Lecture 21 - Dialysis
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
what is diffusion
passive movement of solutes from an area of higher concentration to an area of lower concentration until an equilibrium is reached
what is ultrafiltration
process that removes excess fluid from blood during dialysis, relies on pressure differences across a semipermeable membrane
fluid moves from higher to lower fluid pressure gradient
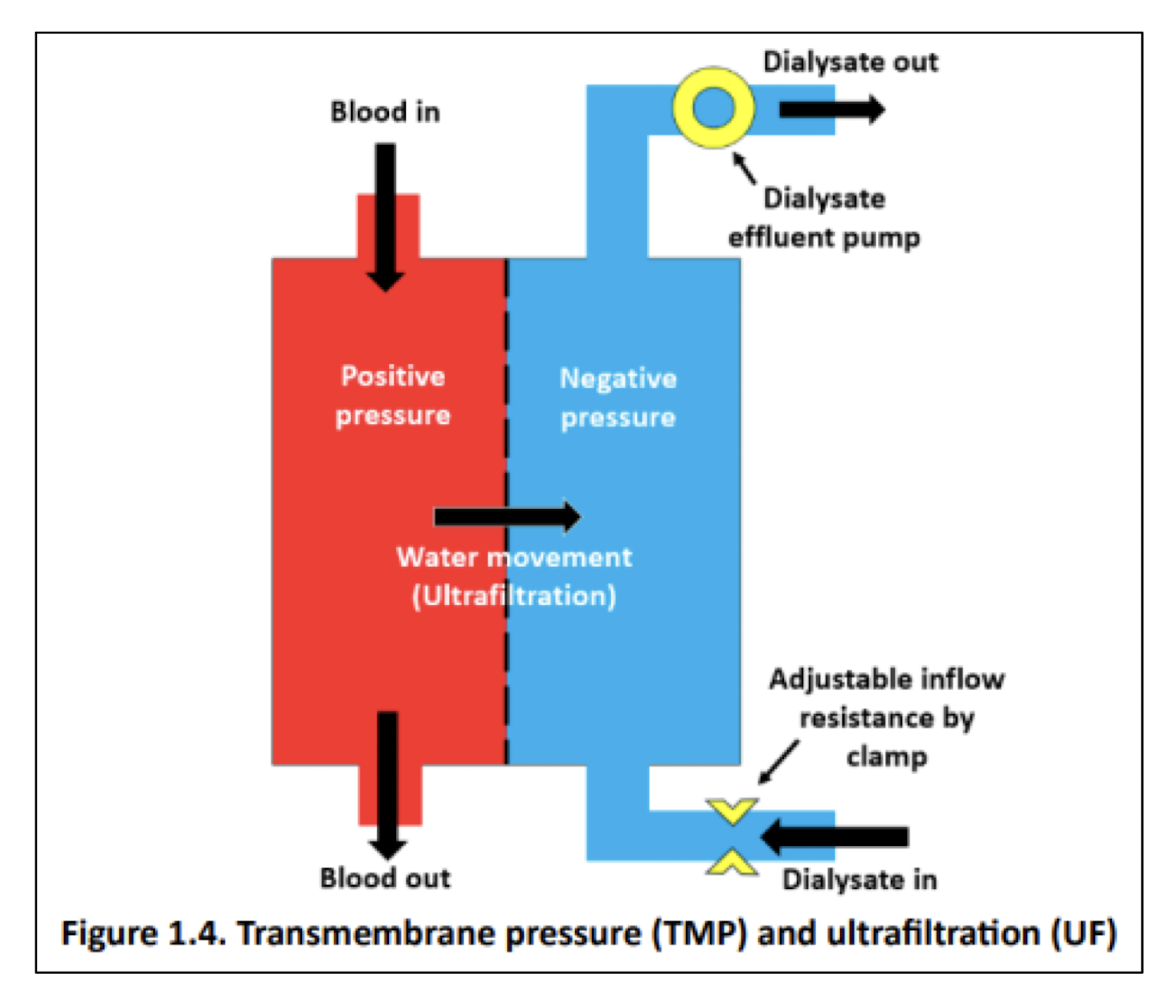
what is ultrafiltration driven by in hemodialysis
hydrostatic pressure
what is ultrafiltration driven by in peritoneal dialysis
osmotic pressure
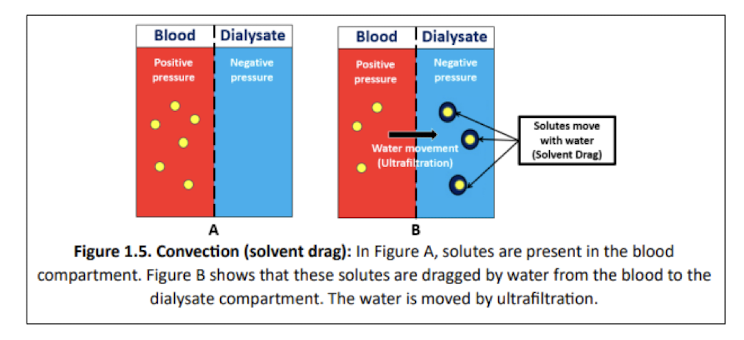
what is convection
passive movement of solutes dissolved in fluid from pressure gradients rather than differences in concentration (solvent drag)
solutes move from area of higher to lower fluid pressure gradient
rate is dependent on molecular size
what principles does hemodialysis use
diffusion
ultrafiltration
limited convection
what principles does peritoneal dialysis use
diffusion
ultrafiltration
convection
what is hemodialysis
blood flows counter-current with dialysate
blood and dialysate are separated by semipermeable membrane → allows for movement of fluid and solutes from blood to dialysate
what is peritoneal dialysis
dialysate is infused into peritoneal cavity
blood and dialysate are separated by peritoneal membrane → acts as semperimeable membrane and allows for movement of fluid and solutes from blood to dialysate
what does the rate of movement of solute depend on
concentration gradient
permeability of membrane
surface area of membrane
length of time that blood and fluid remain in contact with membrane
what are the indications for dialysis in AKI
Acidosis - metabolic acidosis
Electrolyte abnormalities - hyperkalemia
Intoxications - salicylates, lithium, methanol, ethylene glycol, theophylline, phenobarbital
Overload - fluid overload
Uremia - pericarditis, encephalopathy
what are the goals of therapy for dialysis in AKI
maintain fluid and electrolyte, acid-base, and solute hemostasis
prevent further injury to kidney
permit renal recovery
allow other supportive measures
when should dialysis be considered in CKD
patients with GFR <15-20 or risk of renal replacement therapy >40% over 2 years → referred to specialist
balance between prolonging the dialysis-free period to maximize quality of life while trying to facilitate a dialysis-assisted period with minimal complications
should dialysis be initiated early in CKD
no - does not appear to increase survival in CKD patients
early start is associated with increased mortality in patients without diabetes or other comorbidities
starting dialysis at eGFR 14-16 may be associated with 5% reduction in 5 year risk of death (extend life by 1.6 months) compared to starting at eGFR 6-7
when should dialysis be initiated in CKD
if one or more of the following are present:
s/s of kidney failure - neurological attributed to uremia, pericarditis, anorexia, medically-resistant acidosis/electrolyte abnormalities, intractable pruritus, serositis
inability to control volume status or BP
progressive deterioration in nutritional status refractory to dietary intervention
cognitive impairment
initiated based on clinical status rather than specific CrCl (s/s manifest around eGFR 5-10)
what are the goals of therapy for dialysis in end-stage CKD
manage s/s of ESRD
remove uremic toxins and other substances
restore fluid and electrolyte imbalances
re-establish normal pH
what are properties of hemodialysis
most common renal replacement therapy for ESRD
extracorporeal - cleaned outside body
membrane is artificial
can be done in centre or at home
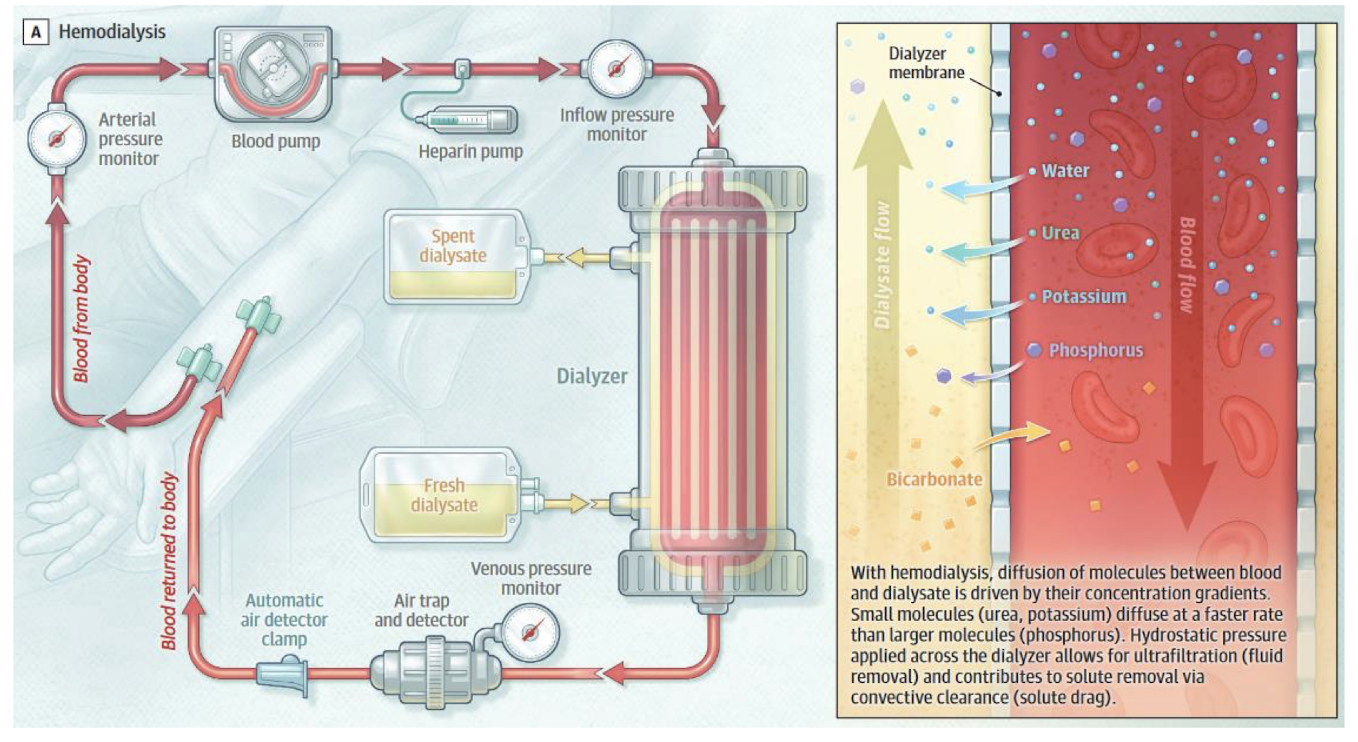
how does hemodialysis clean blood
dialysis machine pumps blood from body towards semipermeable membrane
blood flows counter-current to dialysate (creates larger conc. gradient)
membrane pores allow movement of small molecules, but not large enough for RBCs
solutes removed from blood by diffusion → creatinine, potassium, urea, uremic toxins, drugs
excess water removed by ultrafiltration
bicarbonate moves from dialysate to blood
limited convection
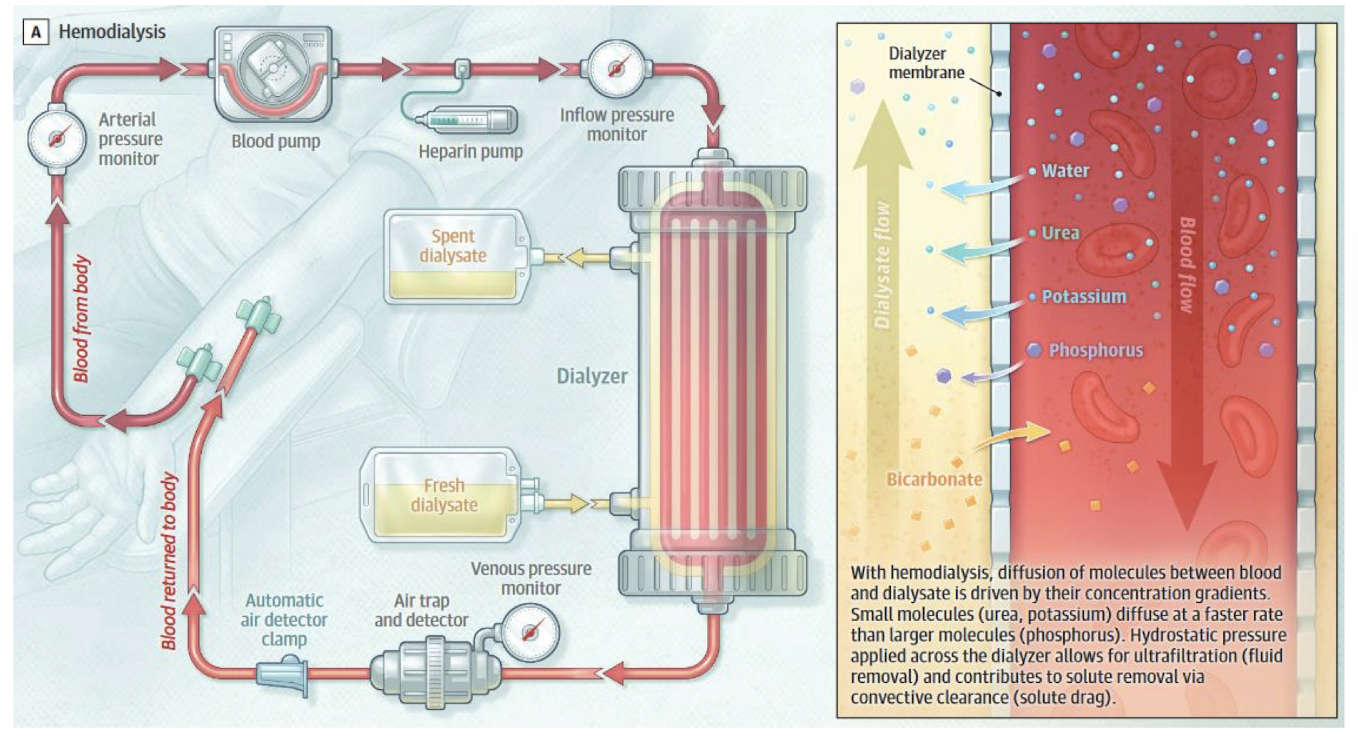
what are the main components of a hemodialysis circuit
vascular access
dialyzer
dialysate
dialysis machine
when is temporary access used for hemodialysis
immediate access required
done via central venous catheter (CVC)
when is permanent access used for hemodialysis
advanced planning
done in arteriovenous (AV) fistula or graft
where is a central venous catheter inserted for hemodialysis
large vein e.g. jugular, subclavian, femoral
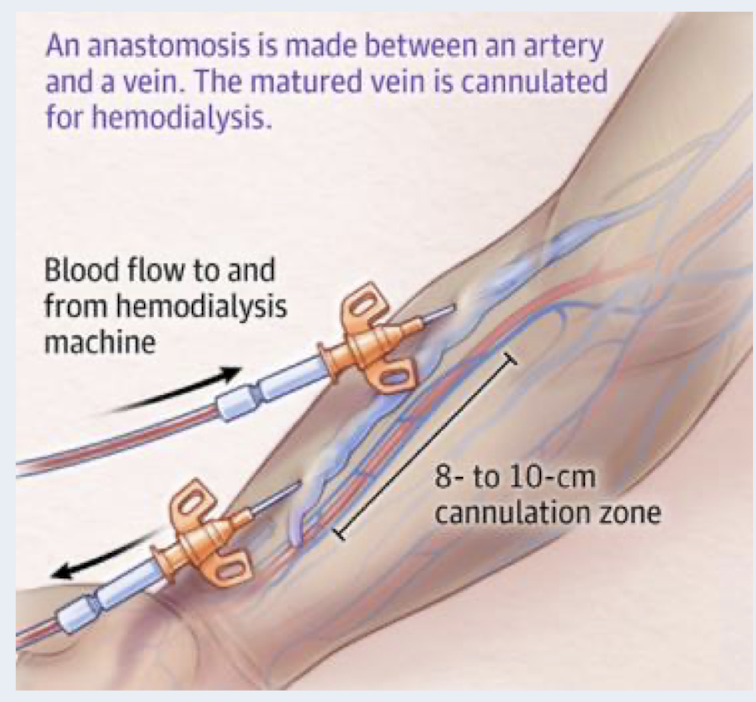
what is an AV fistula
preferred method for permanent access HD
native fistula: surgically created by connecting an artery and vein in the forearm
require 2-6 months for maturation before it can be used for HD
longest survival time of vascular access methods and lower rate of complications
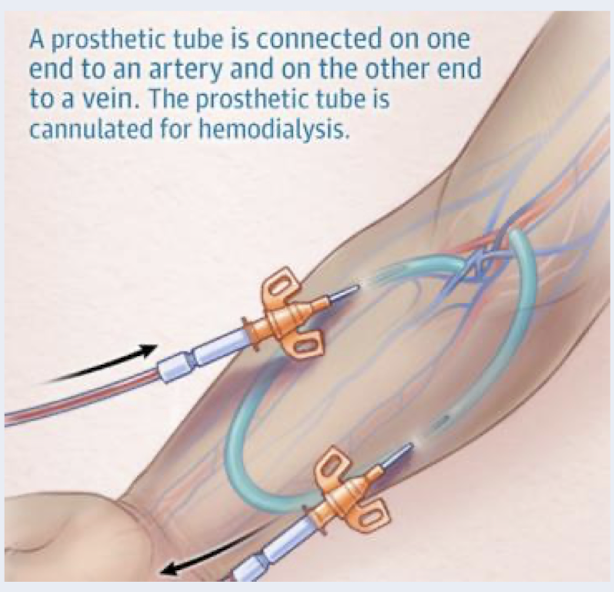
what is an AV graft
synthetic tubing graft is surgically inserted under the skin to connect an artery and a vein
require 2-4 weeks of healing time before it can be used for HD
shorter access survival time, higher rates of infection and thrombosis
what is the dialyzer in HD
filter, artificial kidney
houses semipermeable membrane
larger pores = increased diffusion of solutes
more permeable to water transport = increased ultrafiltration of water
blood flows through one section and dialysate through the other
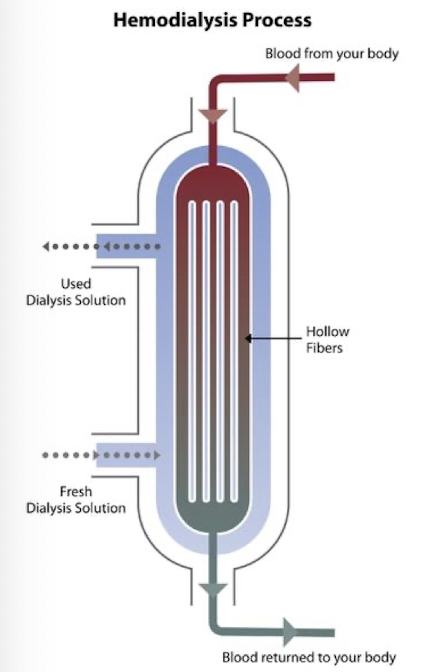
what is the dialysate in HD
cleasing fluid, contains electrolytes, purified water, dextrose
composition can be adjusted based on patient needs
bicarbonate - high concentration allow for movement of bicarbonate into blood
potassium - low concentration to prevent sudden hypokalemia as excess potassium is removed from blood
what does the dialysis machine do in HD
monitors patient for dry weight and BP
controls flow rates or blood and dialysate
controls ultrafiltration
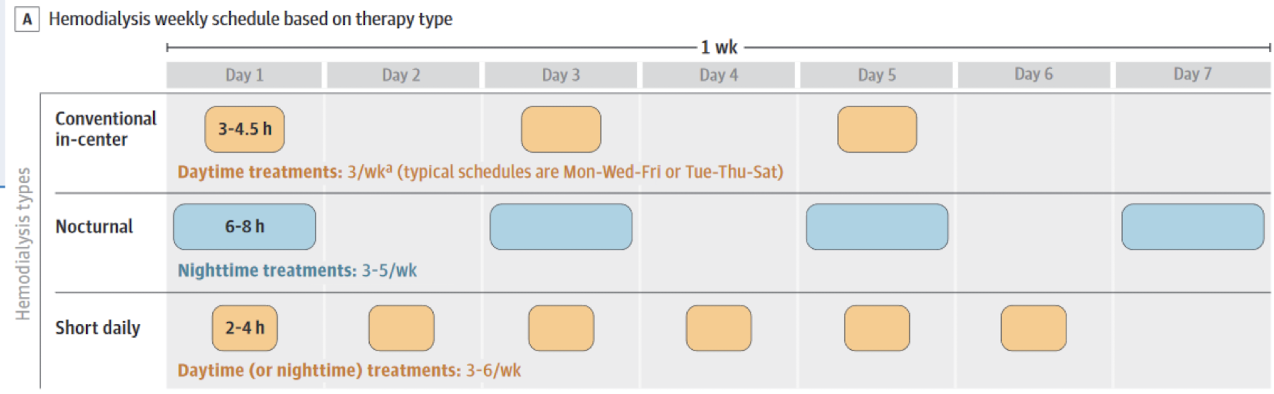
what is a typical in-centre HD schedule
3x/week with each HD run lasting approx. 4 hours

what is a typical home HD schedule
interval and duration of HD
3-6x/week
some patients can do nocturnal HD
what are complications during HD
hypotension
HTN
cramps
N/V
headache
chest/back pain
pruritis
fever/chills
what are infectious complications of HD
access site infections
bacteremia, sepsis
what are non-infectious complications of HD
worsening of existing anemia
thrombosis of AV fistula/graft/catheter
what are advantages of dialysis
higher solute clearance - intermittent treatment
clear parameters → underdialysis detected early
low technique failure rate
homeostasis parameters better corrected than in peritoneal dialysis
close monitoring in centre
what are disadvantages of dialysis
multiple visits per week
disequilibrium, hypotension, muscle cramps are common
infections/thrombosis
decline in residual kidney function more rapid compared to peritoneal dialysys
what is the process of peritoneal dialysis
instillation of dialysate into the peritoneal cavity through the PD catheter
peritoneal membrane = semipermeable membrane between dialysate and blood → abdominal viscera is highly vascularized
solutes are removed from blood across peritoneal membrane by diffusion and convection (solute drag)
excess plasma water removed by ultrafiltration
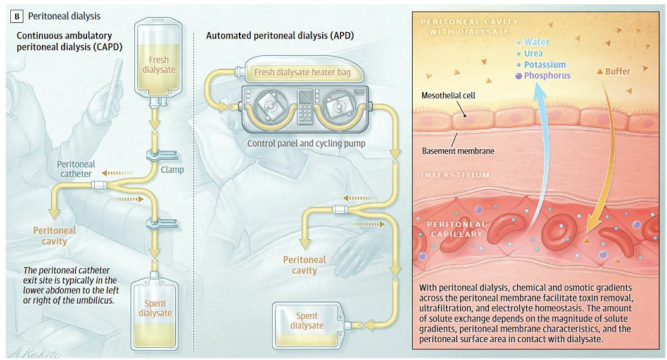
what are the components of PD
access → permanent PD catheter
dialyzer → peritoneum semipermeable membrane
dialysate → PD bag solutions, osmotic agent is dextrose, similar electrolyte composition to serum but no potassium, uses lactate instead of bicarbonate
what are contraindications of PD
absolute: peritoneal adhesions from previous surgeries
relative:
ostomy
severe physical or mental disability
inflammatory bowel disease
lack of appropriate caregiver or inadequate living situation for home dialysis
what exchanges occur in PD
fill → dialysate solution is instilled into the peritoneal cavity (20 mins)
dwell → duration dialysate remains in peritoneal cavity (2 hours)
drain → effluent fluid removed from peritoneal cavity (10-15 mins)
whole process called an exchange
what factors are considered when determining a PD prescription
types → continuous ambulatory PD or automated PD
target dry weight
number of exchanges per day
volume of dialysate to be instilled for each exchange
type of dialysate (dextrose concentration)
dwell duration
what are infectious complications of PD
PD peritonitis → infection within peritoneal cavity
PD catheter exit site infections
tunnel infections
what are non-infectious complications of PD
increased glucose absorption from dialysate → hyperglycemia, increased insulin requirements, hypertriglyceridemia, weight gain, obesity
malnutrition (loss of albumin)
fibrin formation in dialysate
hypokalemia
what are advantages of PD
slow filtration = hemodynamic stability
high clearance of large solutes
better preservation of kidney function
convenient route for drugs like ABX or insulin
freedom from the machine = independence
less blood loss/iron deficiency
no systemic heparization
what are disadvantages of PD
loss of proteins and amino acids
risk of peritonitis
infections
inadequate ultrafiltration with large body size
high rate of technique failure
obesity
hernias, dialysate leaks, hemorrhoids, back pain
what are trends in morbidity and mortality in patients on dialysis
increased hospitalizations and complications
lower life expectancy → 40% 5 year survival
leading causes of death: CV related causes, infections
mortality rates steadily declining
what are impacts of dialysis on quality of life
physical endurance
employment
social life
diet
sex
fatigue
high rates of depression and anxiety
what is the role of the pharmacist in dialysis patients
drug dosing → drug dialyzability, dose adjustments, timing of medications
de-prescribing of nephrotoxic drugs
medication education
management of CKD complications
PD patients → management of constipation, peritonitis
HD patients → management of hypotension
what is drug dialyzability
how much drug is removed from body during dialysis
high = more removed
low = less removed
depends on molecular weight, protein binding, Vd, water solubility, dialysis membrane, blood/dialysate flow rates
what are the general principles of drug dosing in dialysis
renally cleared drugs → dose adjustments
if drug is unaffected by renal impairment (>50% elimination by other routes), typically no adjustments needed
drugs that are toxic and excreted in active form → dose or frequency adjustment to avoid accumulation
drugs highly dialyzed → dosing adjustments, adjust timing (post-dialysis), may require supplementary dosing