GI 5: Stomach Motility and Secretion
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
41 Terms
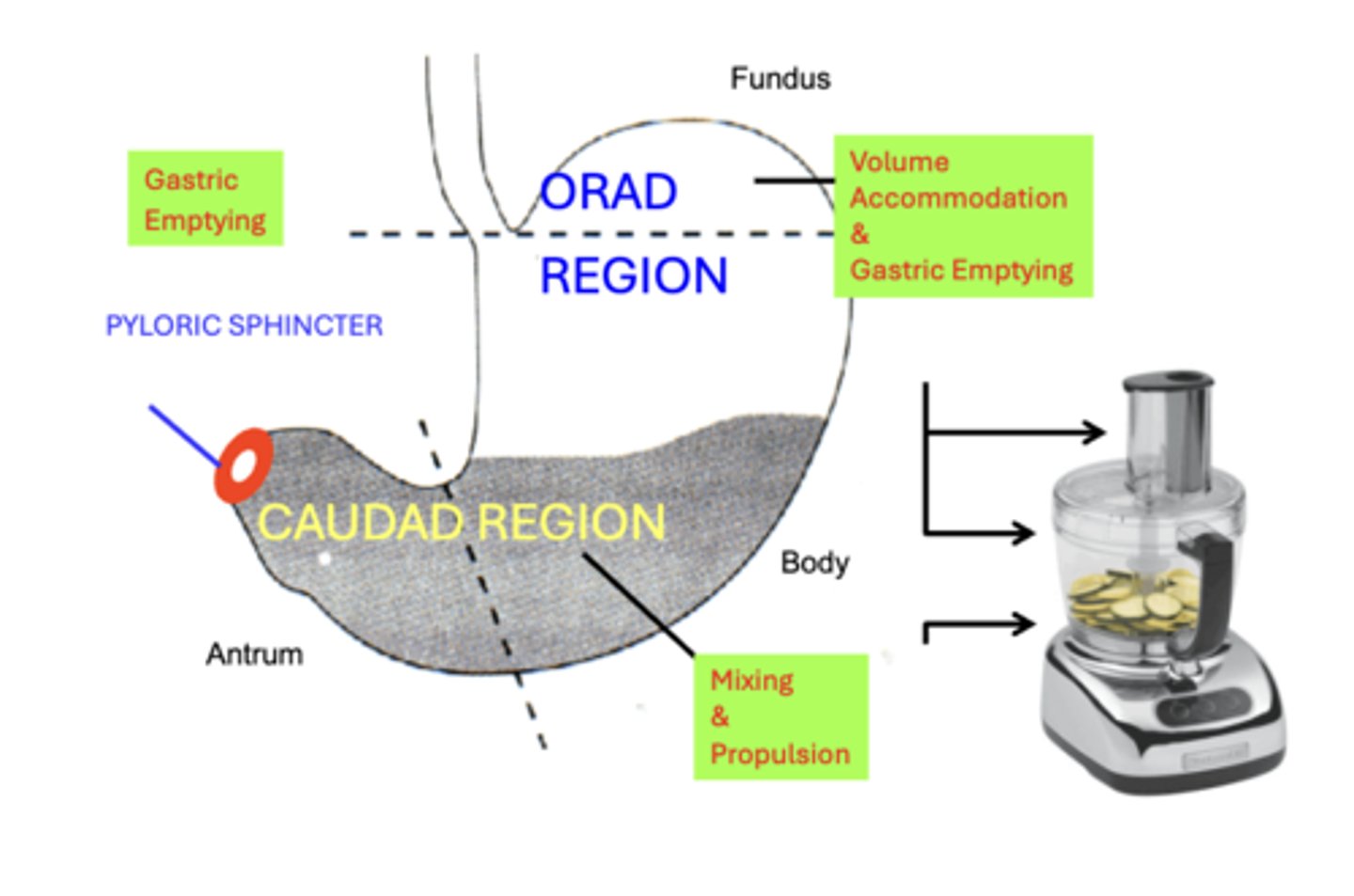
Motility Regions of Stomach
- Orad Region: Volume Accommodation & Gastric Emptying
- Caudad Region: Mixing & Propulsion
- Pyloric Sphincter: Gastric Emptying
Muscle Histology of Stomach
longitudinal & circular smooth muscle layer possessed by most of the GI tract
- unique oblique smooth muscle layer mixing and propulsive
physiologically important histological feature of the stomach
smooth muscle thickness increases caudally
- such that smooth muscle layers are significantly thicker in the caudad compared to the orad region
- difference is related to the specific motility actions of each region
Orad
parts: Fundus and proximal part
motility function: Volume accommodation and gastric emptying
Caudad
parts: Antrum and distal body
motility function: Mixing and propulsion
Pyloric
parts: Pylorus
motility function: Gastric emptying
Factors affecting gastric emptying
Motility activities affecting gastric emptying rate are initiated by neural and hormonal signals from
A. Stomach
B. Duodenum
Factors affecting gastric emptying: Stomach Volume
• Increased gastric filling SPEEDS gastric emptying
• Decreased gastric filling SLOWS gastric emptying
Factors affecting gastric emptying: Duodenum
duodenum exerts the more potent of the regulatory signals
• feedback mechanism involves "sensing" of the chemical and nutrient composition of chyme entering the duodenum by receptors located in the duodenal mucosa
• Receptor stimulation affects gastric emptying through neuro- chemical or hormonal mediators that alter motility activities of the stomach and proximal intestines
Intestinal Chyme properties
1. Food composition
2. Chyme pH
3. Chyme osmolality
Chyme pH
o ↓ pH SLOWS gastric emptying
o When duodenal chyme pH becomes <3.5, gastric emptying rate slows to allow adequate neutralization of duodenal chyme by pancreatic and bile buffers.
Chyme Osmolality
• Isotonic chyme empties MOST RAPIDLY.
• HYPOtonic chyme empties significantly SLOWER
• HYPERtonic chyme empties the SLOWEST
What the significance of controlling gastric emptying?
Slowing or speeding gastric emptying rate in response to gastric filling and chyme properties is primarily to
1. prevent saturation of duodenal digestive (lipid & volume effects)
2. minimize large [Electrolyte] fluctuations (osmotic effects) in the duodenum
Summary of Gastric Emptying
Stomach Volume: (Relatively Weak)
• ↑ Filling: SPEEDS Emptying
• ↓ Filling: SLOWS Emptying
Intestinal Chyme Properties: (More Potent Factors)
• Food Composition:
- Carbohydrate > Protein > LIPID
- Lipid slowing mediated by CCK
• ↑ Acidity (pH < 3.5): SLOWS Emptying
• Osmolality: Isotonic > Hypotonic > Hypertonic
gastric juice composition
1. HCl
2. Pepsin
3. Gastric Lipase
4. Mucus
5. Intrinsic factor
Hydrochloric Acid (HCl)
1. serves an important function as a Bactericidal agent
- Prevents GI Infection
- When acid secretion is impaired, bacterial GI infections increase
2. Denatures Complex Polypeptides into simpler proteins & peptides
3. Pepsin activation
- Pepsinogen → Pepsin (pH < 3)
- Stomach pH = 2
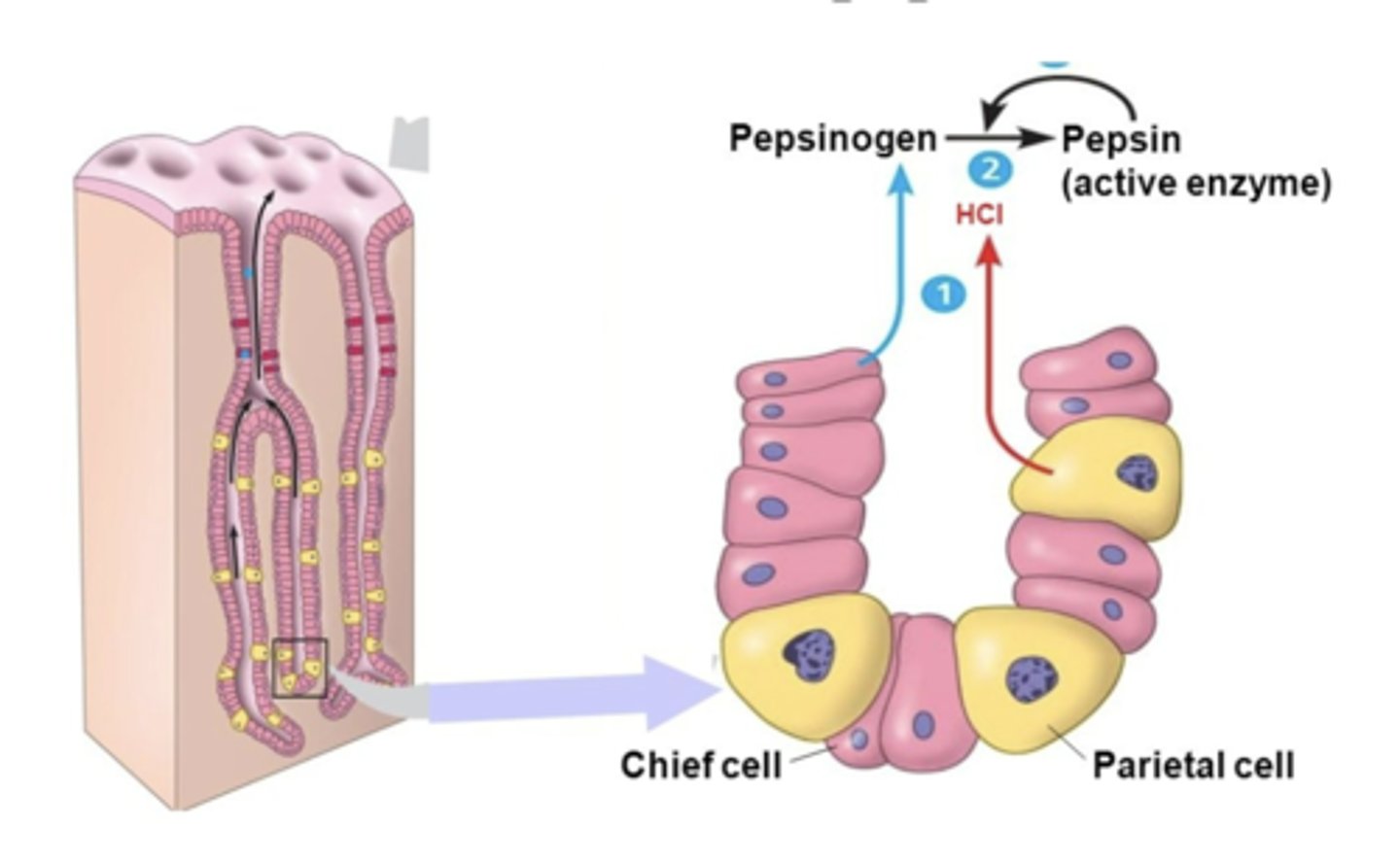
Pepsin
proteolytic enzyme
- Initiates Protein Digestion by splitting interior peptide bonds (endopeptidase)
- Initially secreted as a larger inactive precursor, Pepsinogen
Pepsin activation
Pepsinogen cleavage to active pepsin
- dependent on an intragastric pH < 3, thus requiring HCl secretion
- therefore, Pepsinogen cleavage is typically instantaneous at the normal intragastric pH < 2
- Pepsin itself can also cleave Pepsinogen, amplifying acid activation.
Nevertheless, HCl & Pepsin are NOT essential for normal protein digestion
gastric lipase
enzyme involved in fat digestion
- primarily secreted from the pancreas (some from saliva)
- gastric activity can contribute significantly to overall dietary fat digestion, especially during pancreatic insufficiency
mucus
- lines the gastric lumen and mixes with other secretions
- Lubricates Chyme
- Protects Mucosa from pepsin autodigestion and mechanical injury
HCO3-
Buffers Gastric Acid in association with mucus: The Mucus-HCO3- layer is sometimes referred to as the "Gastric Mucosal Barrier"
intrinsic factor
a mucoprotein that binds vitamin B12 in the stomach
- Forms a complex with other proteins necessary for vitamin B12 Absorption in the ileum
- Pernicious Anemia
- Only Intrinsic Factor Essential
Functions of gastric secretions
1. Initiate Digestion of proteins through acid and proteolytic enzyme production
2. Facilitate Absorption of essential nutrients, specifically Vitamin B12, by the ileum
3. Protect the gastric mucosa from Infection by ingested pathogenic microorganisms as well as possible Damage & Autodigestion from its own production of caustic gastric acid and proteolytic enzymes
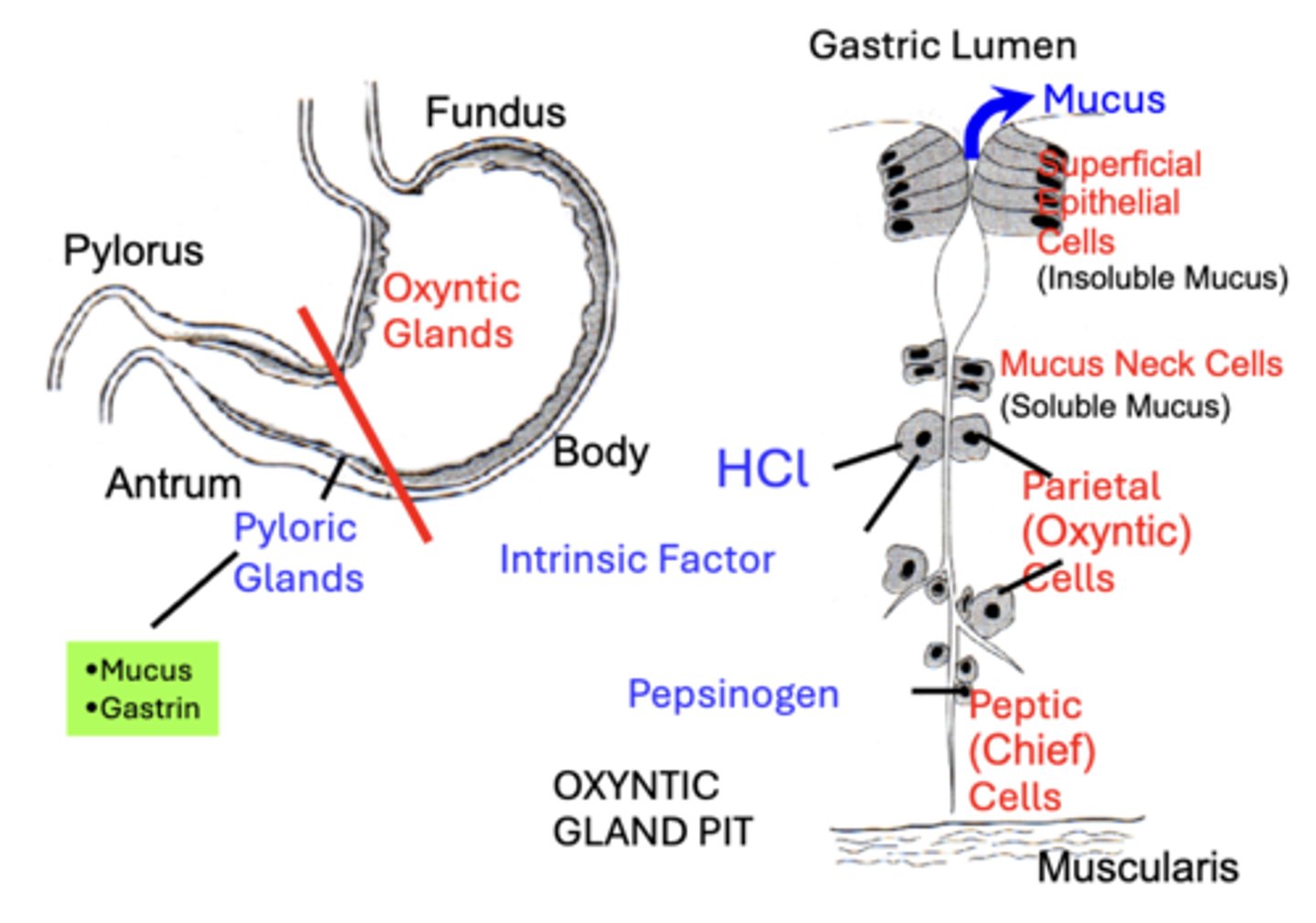
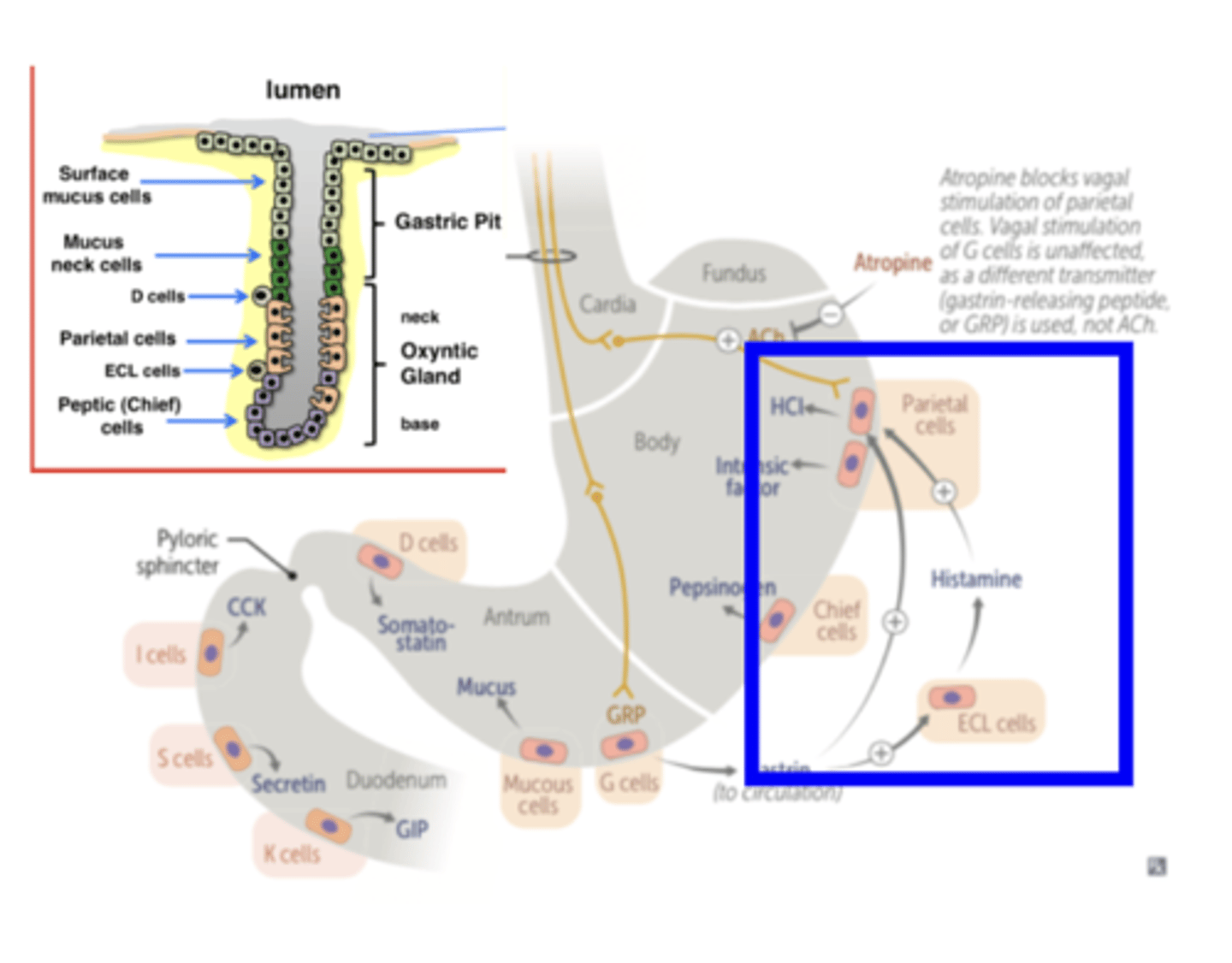
Mucus Neck Cells
secretes soluble mucus
- mixes with ingestate and other secretions to mainly lubricate gastric chyme
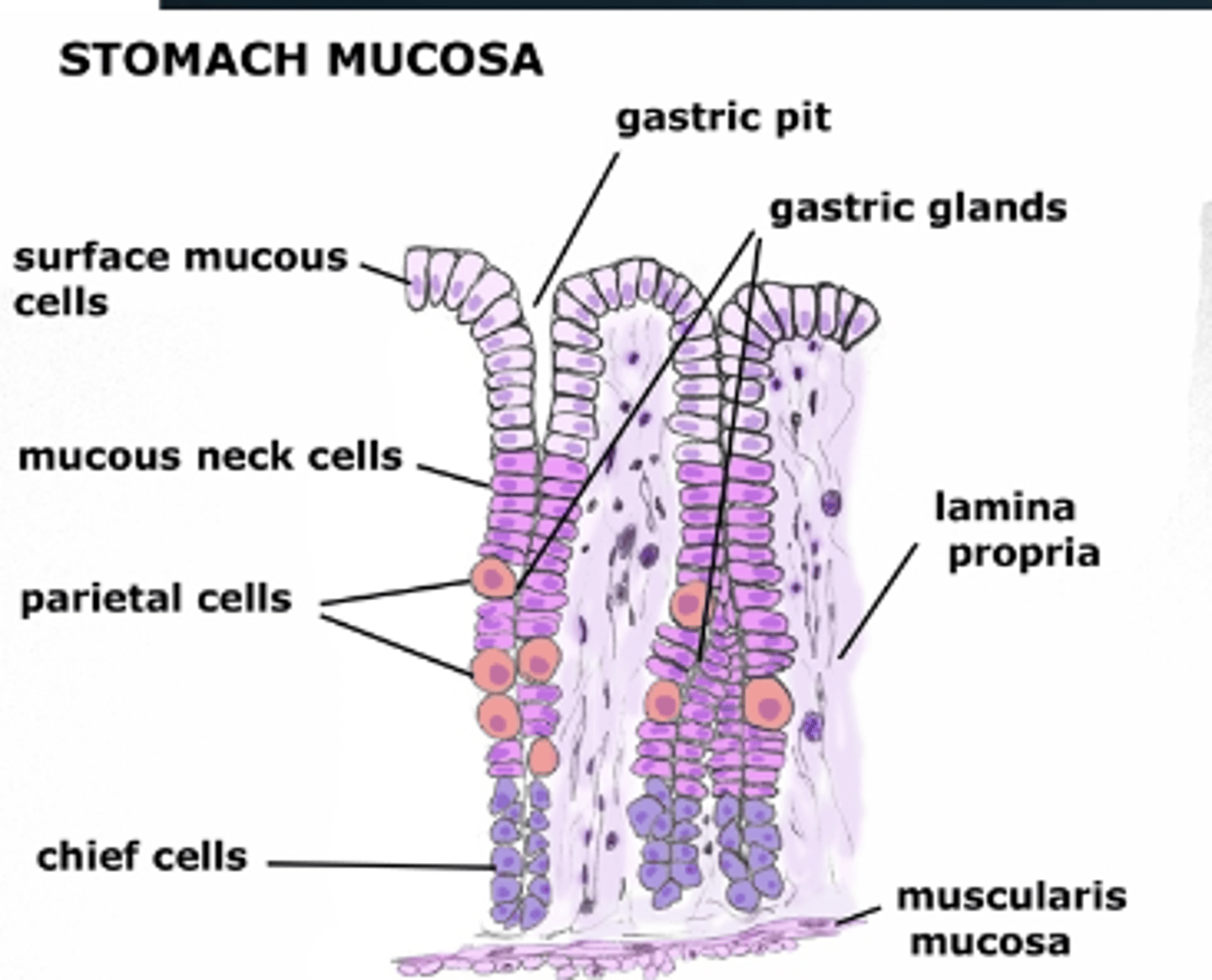
Superficial Epithelial Mucus Cells
• produce insoluble mucus in response to chemical (ethanol) or physical irritation (chyme friction)
• Secreted as a visible thick gel that forms over the mucosal surface
• This unstirred layer traps dead mucosal cells and HCO3- secreted from surface cells, providing a "Gastric Mucosal Barrier" that neutralizes stomach acid and protects the mucosa from mechanical injury and pepsin digestion
Parietal Cells
produce HCl and also Intrinsic Factor in humans
Peptic (Chief) Cells
are the producers of Pepsinogen (some mucus cells)
APUD cells
the main site of G Cells
- produce the GI hormone Gastrin
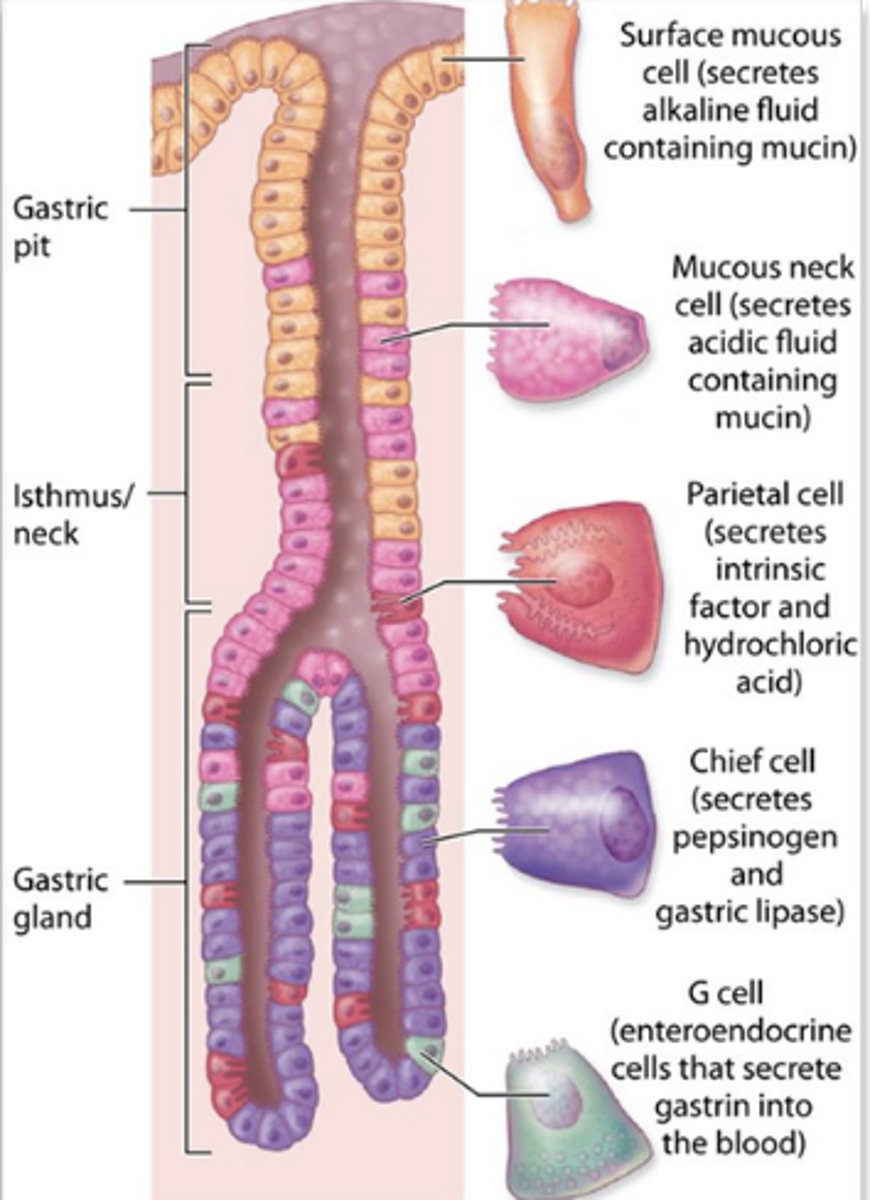
Gastrin
a major regulator of gastric acid secretion
Secretory Anatomy of Stomach
Gastric acid secretion mechanism
H+ & HCO3-: produced by parietal cells from CO2 generated through normal cell metabolism
Parietal cells: are enriched with the catalytic enzyme Carbonic Anhydrase
- HCl secretion from parietal cells into gastric
lumen involves active transport mechanism that depends on several types of membrane electrolyte transporters
(H+-K+)-ATPase: pumps metabolically produced H+ (H+ inside cell) across the Apical membrane in EXCHANGE for luminal K+
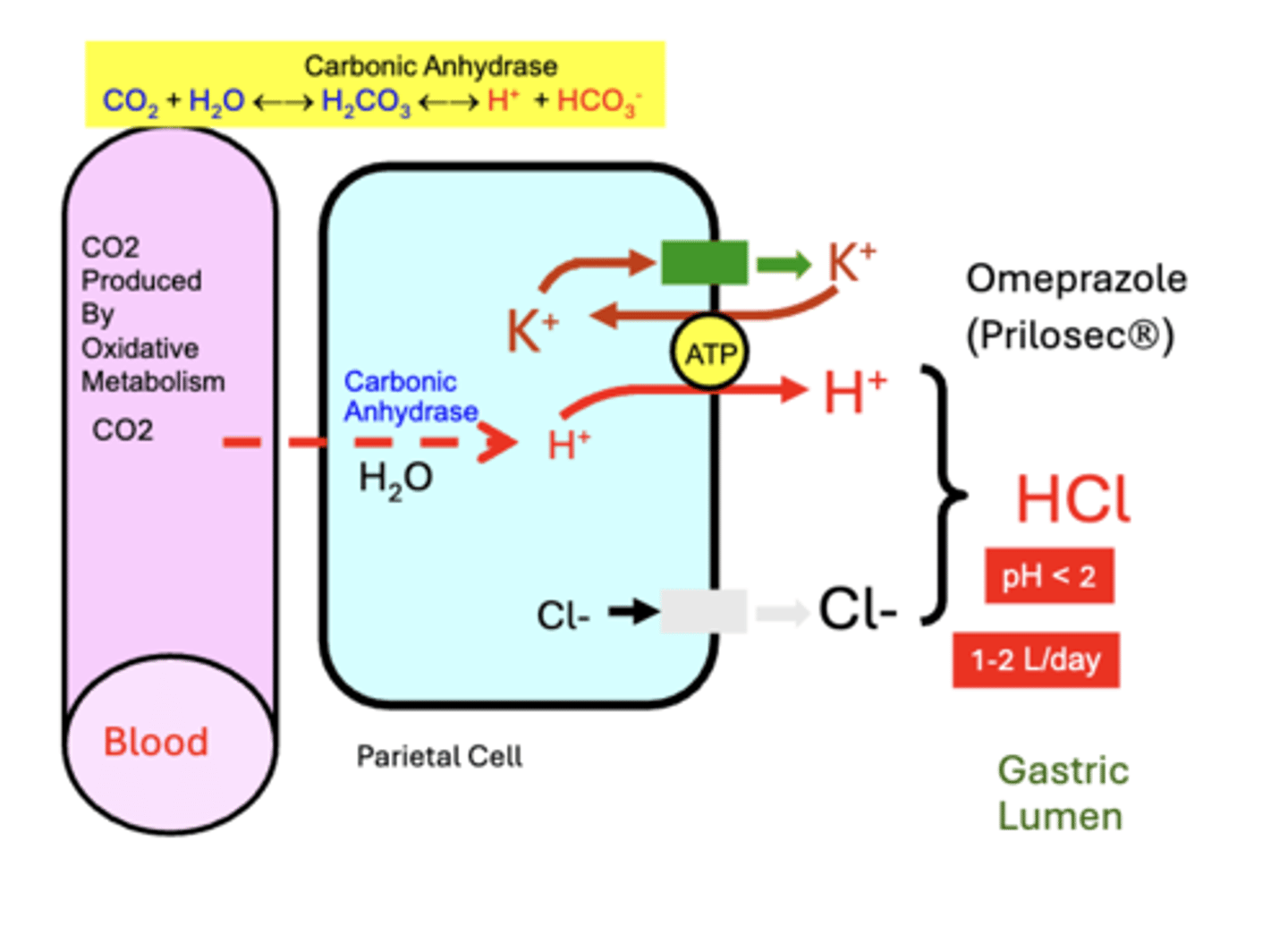
clinical importance of the (H+-K+)-ATPase
it is the pharmacological target of commonly used antacid drugs, such as Omeprazole, used to treat excess acid secretion disorders
Acid Concentration in Gastric Lumen
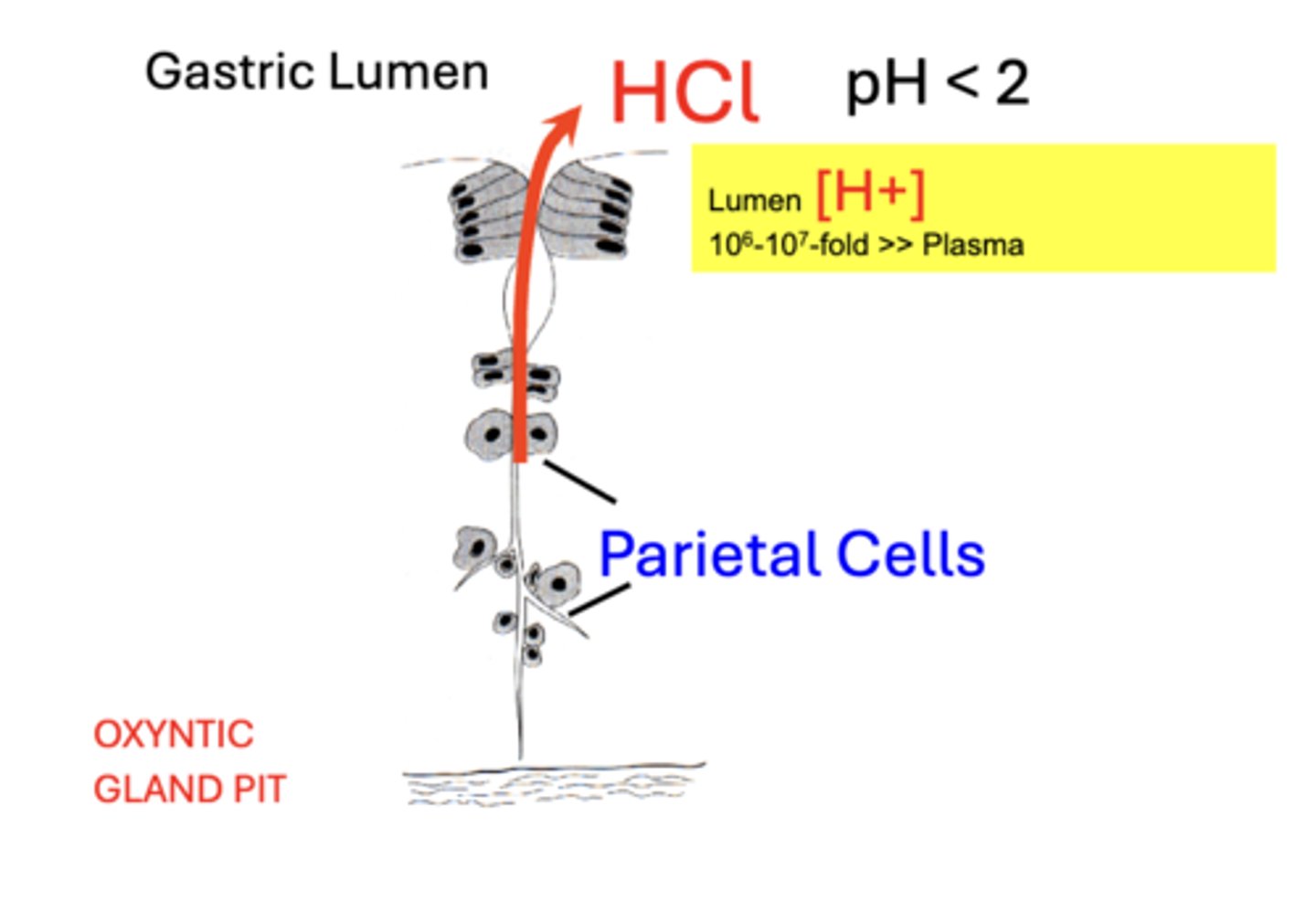
Regulation of acid secretion
Acid secretion from parietal cells is stimulated through:
a. Direct Neural
b. Neuroendocrine
c. Paracrine
acid secretion is also regulated by POTENTIATION
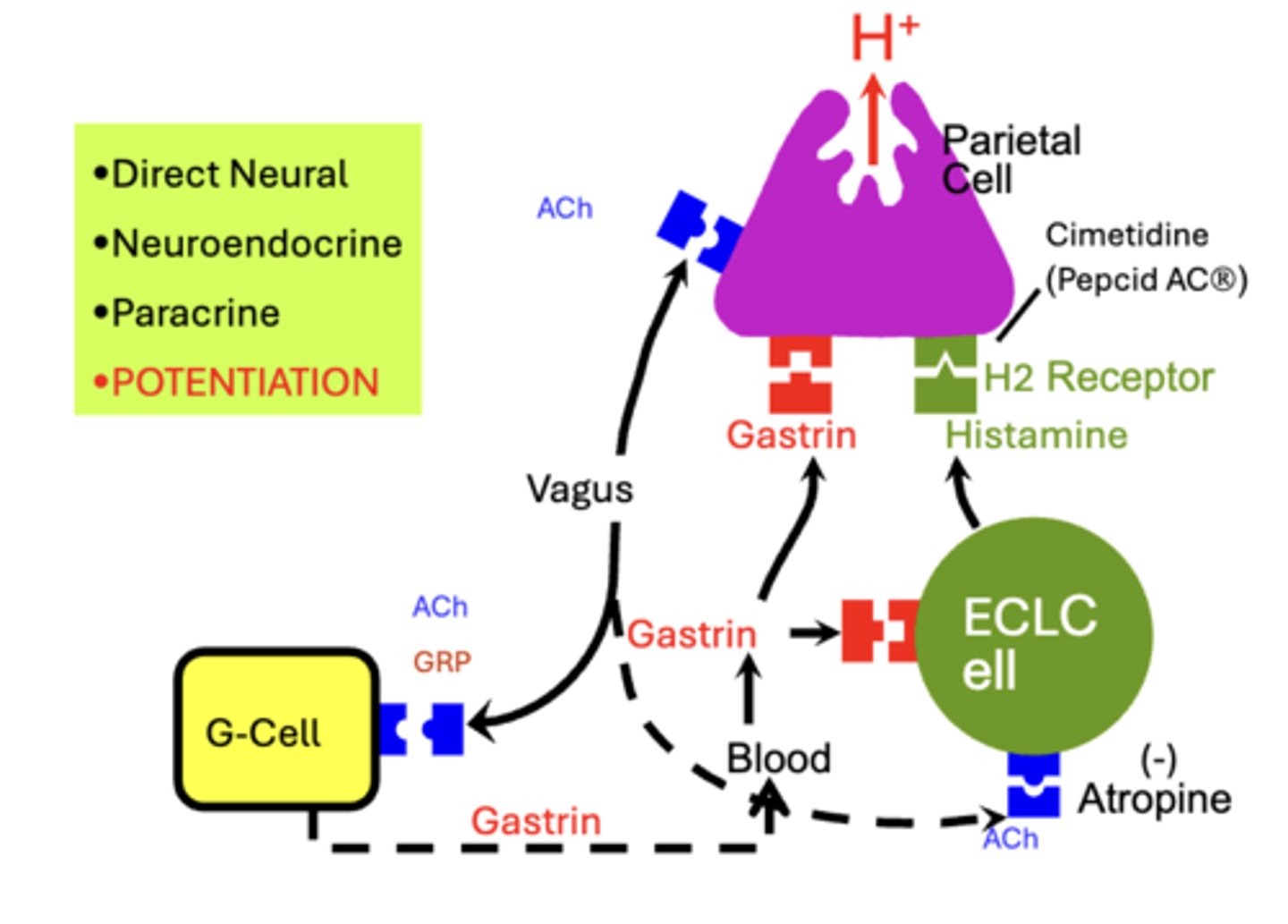
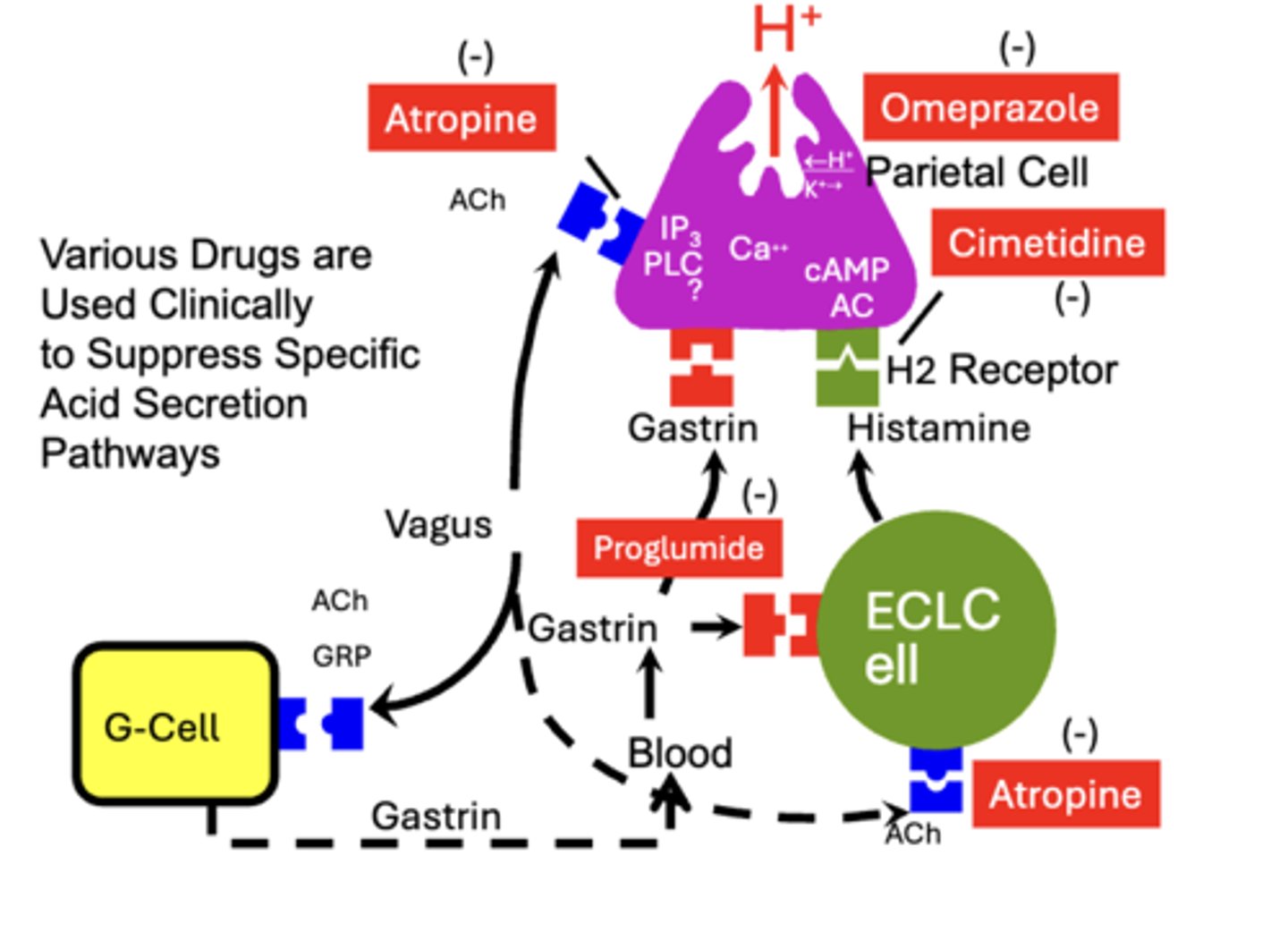
Regulation of acid secretion: Direct Neural
Acid secretion (H+) from Parietal Cells can be increased through direct parasympathetic stimulation by the Vagus nerve
- neurotransmitter acetycholine (ACh) acts through muscarinic receptors
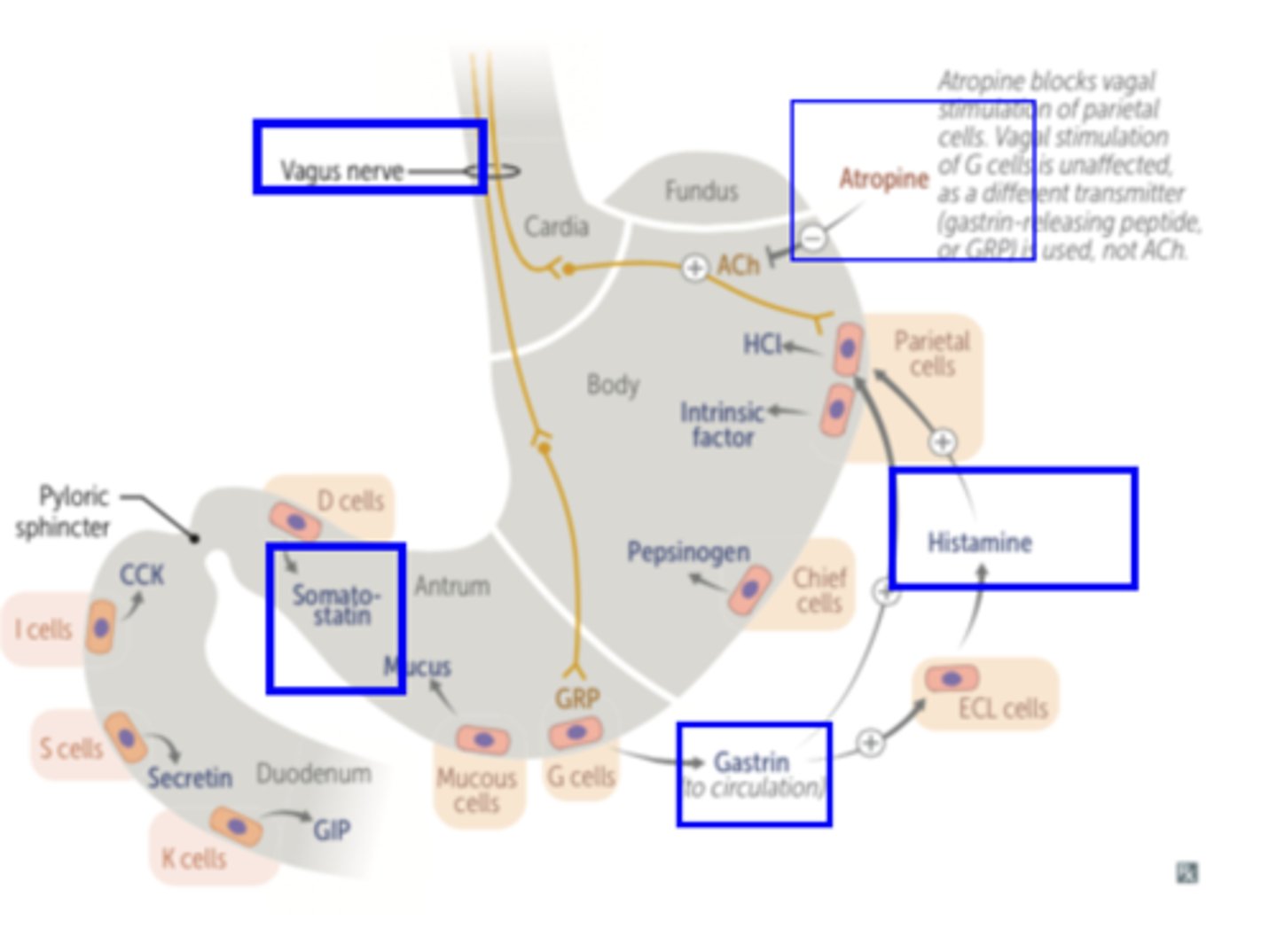
Regulation of acid secretion: Neuroendocrine
GI endocrine hormone Gastrin is secreted from pyloric G-Cells in response to parasympathetic Vagus nerve stimulation
- may be mediated by the neurocrine agent Gastrin Releasing Peptide (GRP) or neurotransmitter ACh
- Gastrin is secreted into Blood and delivered to Parietal Cells where it stimulates H+ secretion
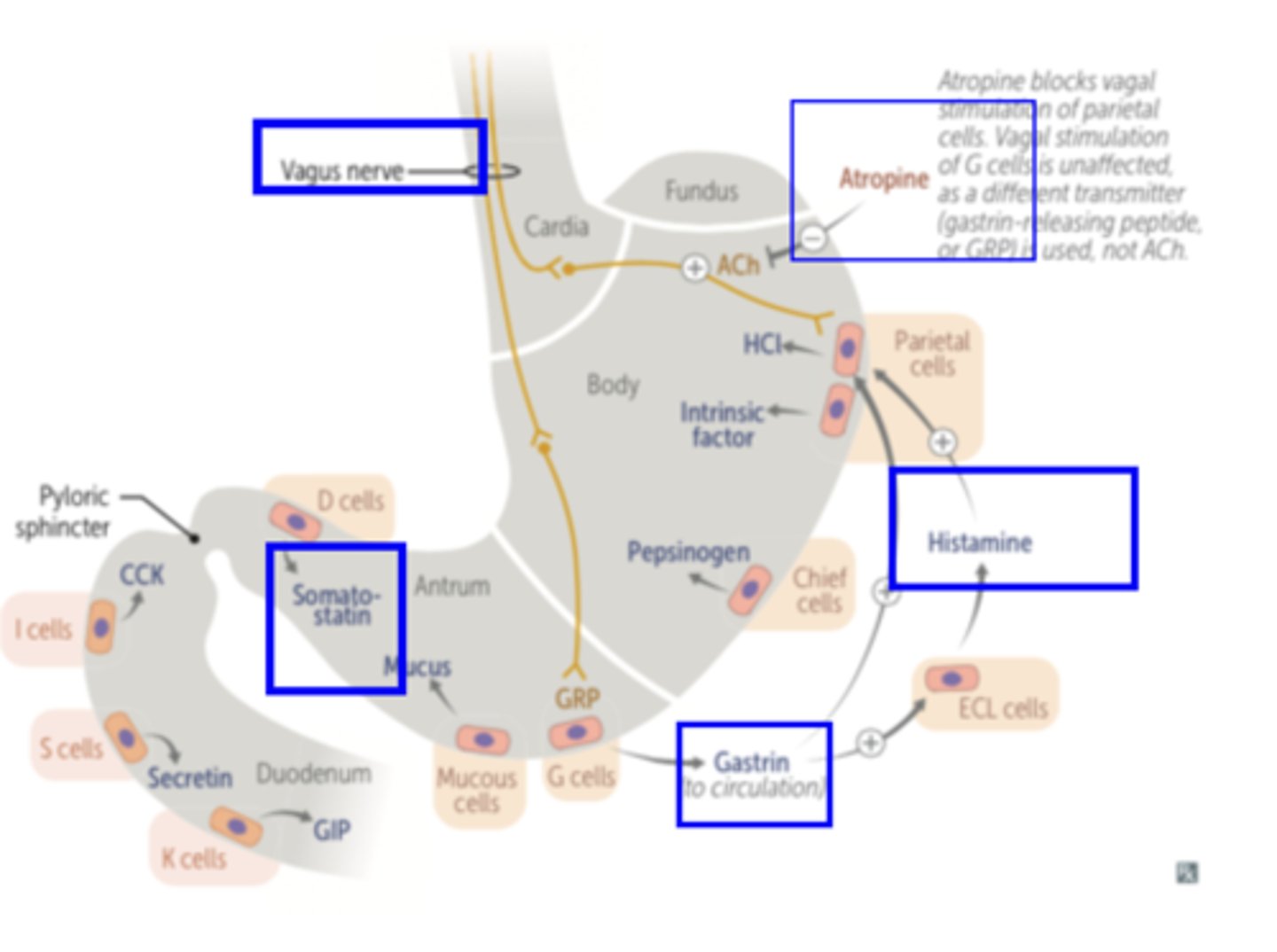
Regulation of acid secretion: Paracrine
Histamine, a paracrine agent, is secreted by mucosal Entero Chromaffin-Like cells (ECL Cells)
- Histamine stimulates H+ secretion through H2 Receptors that activate cyclic AMP (cAMP) via an adenylate cyclase (AC) pathway
- pathway is independent of both vagal and gastrin stimulation
Cimetidine
H2-receptor-blocking drug used to control acid secretion
- inhibit H+ secretion by blocking (-) the stimulatory effect of histamine on parietal cells
- Drugs such as Pepcid AC and Tagamet are trade derivatives of Cimetid
Pharmacological Control of Acid Secretion
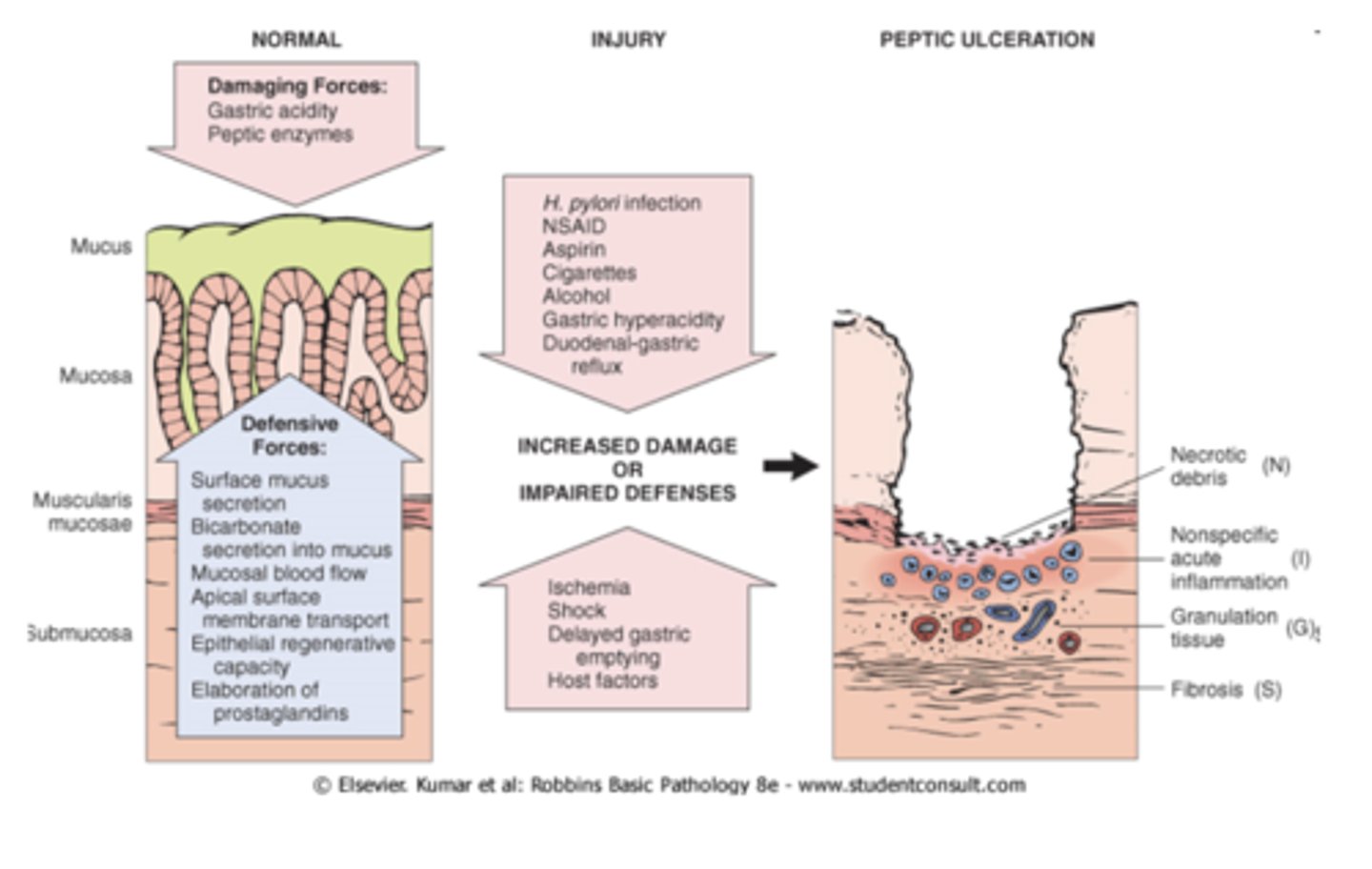
Gastric Mucosal Barrier
alkaline mucus layer
- functions to prevent damage to the gastric mucosa by the highly acidic Gastric Juice and from autodigestion by Pepsin
composed of:
1. Mucus:
- thick viscous
- secreted by gastric glands in copious amounts
- produced by neck cells & surface epithelial cells (Gastric Epithelial Cells)
- stored within cytoplasmic apical granules (Mucus Droplets)
- released by exocytosis to the lumen where it coats the surface of the stomach (Mucus Layer)
2. Bicarbonate: secreted and entrapped by the mucus coat
- makes the mucus layer alkaline (pH 7)
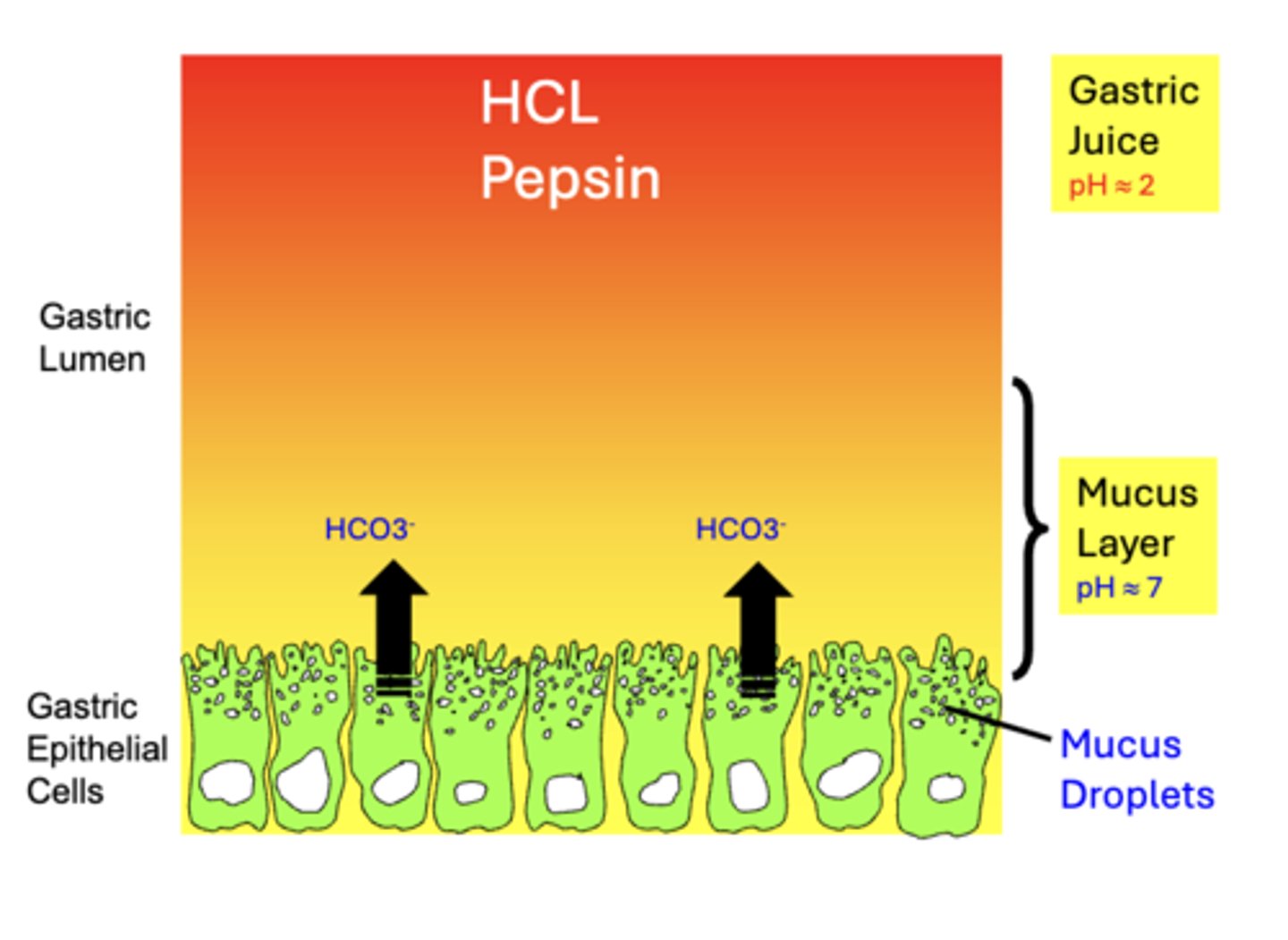
secretion + the gastric mucosal barrier
adequate protection requires normal secretion of BOTH Mucus & HCO3-
- impairment of either may result in mucosal damage and the development of Gastritis and possibly Peptic Ulcer Disease
- various factors can reduce their secretion, including aspirin and other NSAIDS along with some ⍺-adrenergic agonists