ceutics parenterals 1
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
drug delivery involves delivering a drug at ________________ rate to desirable site to treat disease
therapeutically effective
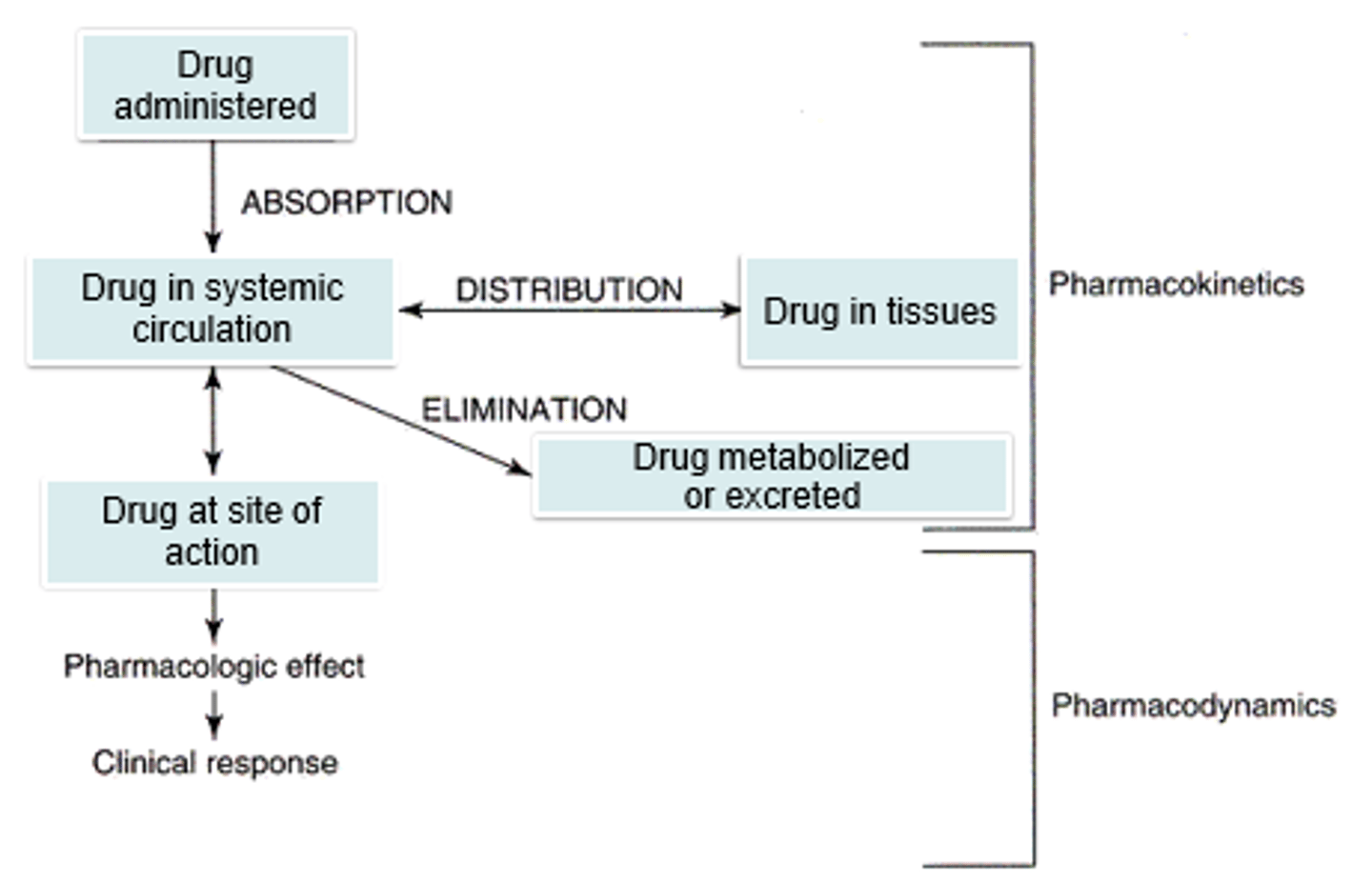
compare and contrast pharmacokinetics and pharmacodynamics in drug preparation
kinetics= what body does on drug
-where?how much? how often?
dynamics= what drug does to body
-effects of drug
both: plasma concentration
goals of drug delivery
1. low degradation
2. target Site deployment (less side effects)
3. therapeutic Window drug level
4. Predictable controllable release rates
5. patient Compliance by reducing dose frequency
DS W PC
7 factors influencing route of administration of drug delivery
1. ease (difficulty swallowing? nausea?
2. site of action (local vs systemic)
3. onset of action (oral?sublingual?IV?)
4. duration of action (controlled, immediate, IV..)
5. metabolism/excretion
6. quantity of drug (small vs large)
7. toxicity
ESOD M QT
how does difficulty swallowing/ nausea impact route of administration choice
difficulty swallowing= avoid solid in favor for liquid
nausea= avoid oral routes
t/f: drugs meant for systemic administration still have specific sites of action
true
local use vs systemic use
local= site specific application
systemic= absorption into blood then to target
do liquids or tablets have faster onset of action?
liquids= meds more available for absorption
do sublingual or oral tablets have quicker onset of action?
sublingual=> med bypasses stomach, goes straight to bloodstream
examples of topical medications with quick onsets of action
-applied to skin
-inhaled into lungs
-instilled into eye
duration of action
The length of time the concentration of a drug in the blood or tissues is sufficient to elicit a response. (in therapeutic level)
how long do CR/ER drugs last? IR?
CR/ER: 12-24hrs
IR: 4-6hrs
which drug route allows for sustained duration
IV infusion
which injections last longer? IM/SC or IV?
IM/SC
how does quantity of drug impact choice of drug route?
small amount of API= tablet with a lot of diluent
large quantity= use IV (diluted in blood)
which method is used to deliver a large amount of drug systemically
IV injections/infusions
first pass effect
The initial metabolism in the liver of a drug absorbed from the gastrointestinal tract before the drug reaches systemic circulation through the bloodstream.
how does age and disease affect choice of drug delivery
older patients usually have less effective drug metabolism and elimination
= usually given lower dose
= potential accumulation and toxicity
toxicology
study of toxic effects of drugs on body
t/f: very little difference exists in the therapeutic vs toxic blood level
true
what is parenteral administraton
injection or infusion by means of a needle or catheter inserted into body
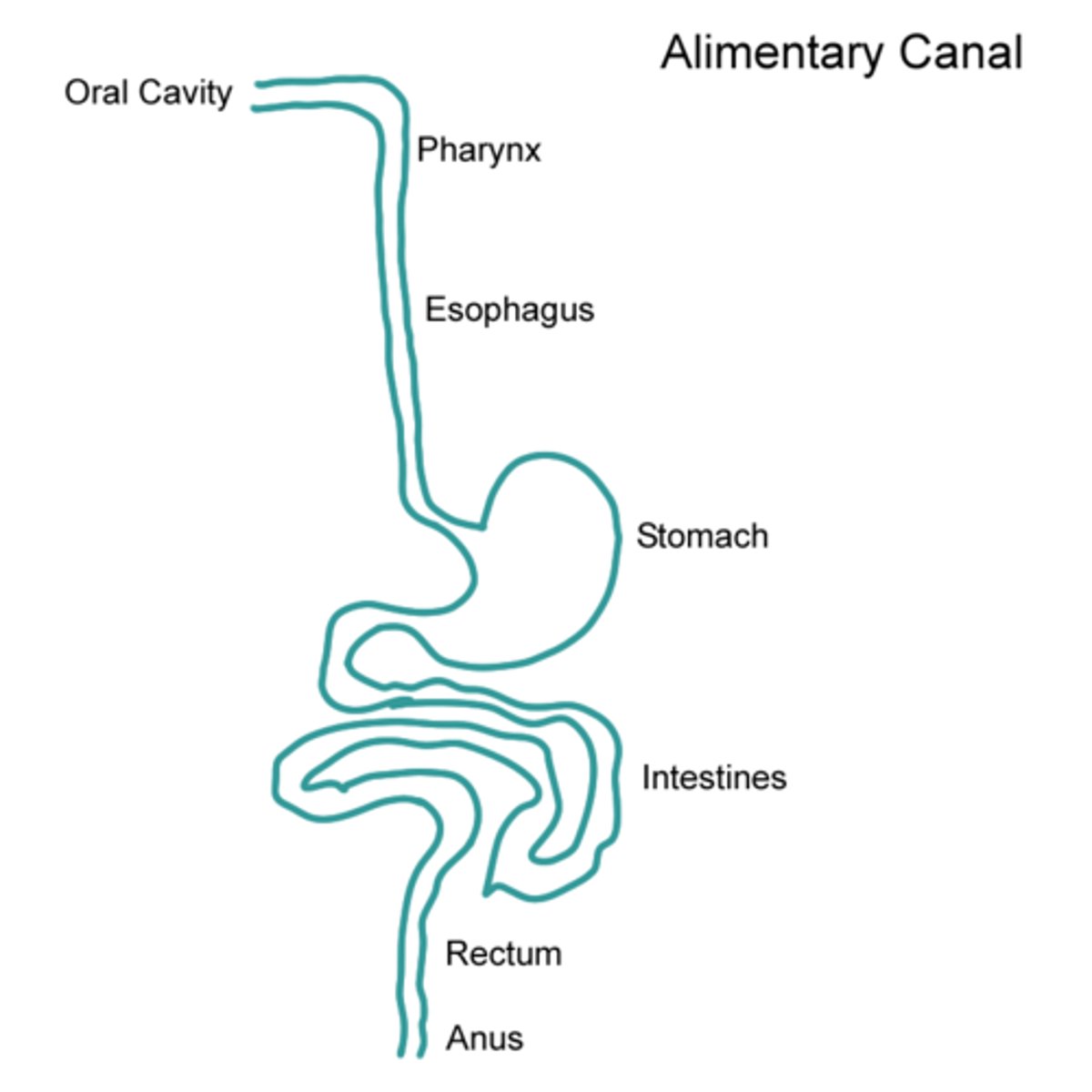
greek definition of parenteral
para= outside
enteron= intestine
parenteral route of administration bypasses the _________
alimentary canal
to ensure sterility, parenterals are prepared using...
1) aseptic technique
2) special clothing (gown,mask..)
3) laminar flow hoods
ASL
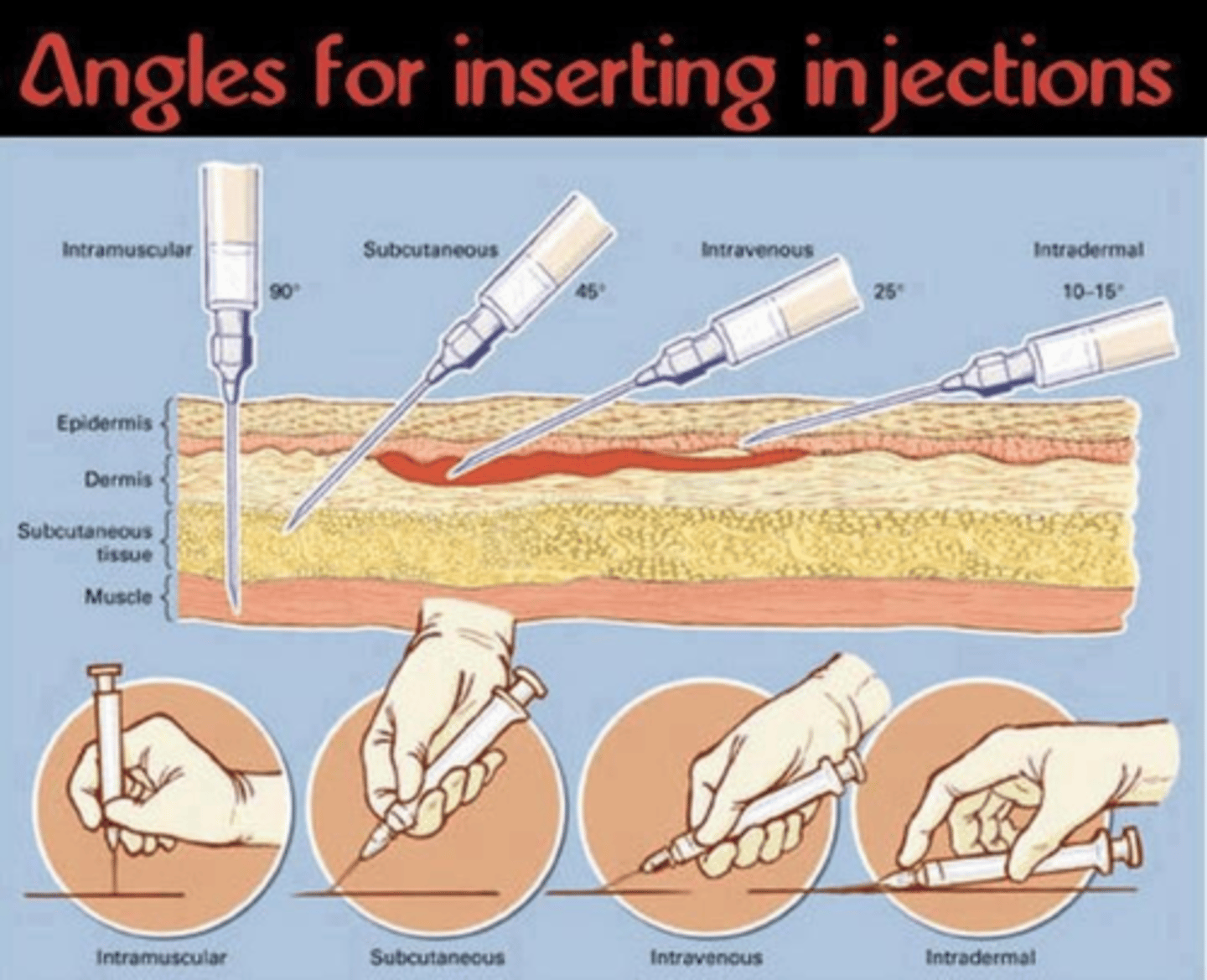
what are the 5 routes of parenteral drug administration
1.IV= into vein
2. IM= into muscle
3. SC= under skin
4. ID= into skin
5. IP= into peritoneal cavity
advantages of IV route
1. Fastest method for giving systemic drugs
2. Provides fluids, electrolytes, nutrition
3. Provides higher concentration of drug to bloodstream (serious bacterial infections)
4. Continuous amount of needed medication (no fluctuations)
5. Infusion rate can be adjusted
what is the fastest route for giving systemic drugs
IV
which route is preferable for continuous amounts of medications with no fluctuations
IV
disadvantages of IV route
1. Injury from needle insertion
2. Potential for introducing toxic agents, microbes, pyrogens
3. Impossible to retrieve once given
compare rate of onset and duration for SC, IM, and IV
SC: longer onset and longest duration (low blood supply)
IM: longer than IV (higher blood supply)
IV: fastest onset and shortest duration (into blood)
T/F: IM/SC can be used for medications not active orally
true
parenteral preparations are usually what dosage forms?
solutions and suspensions
which route of drug administration must be free of air bubbles and why?
IV; introduction of air and matter might cause embolism, vessel blockage, or painful rxn
IV injections must be given at what angle
15-20
describe the proper needle length, gauge, angle, and volume for IM injection
22-25 gauge, 1/2 to 1 inch, 90 degree angle, less than 3mL
T/F: absorption of IM drugs is predictable and used for emergency situations
false. IM absorption is unpredictable and not recommended for unconscious patients (IV is predictable and preferred)
t/f: IM injections can be used to give antibiotics, vitamins, iron, and vaccines
true
which route is used for TB skin test
ID; upper forearm
which route is used for allergy skin tests
ID; usually on back
where are ID injections given
into capillary-rich layer just below epidermis (local anesthesia, diagnostic tests, immunizations)
which injection route is used for epi, heparin, sumatriptan, and vaccines
subcutaneous
which angle, gauge, length, and volume of needle should be used for SC injections
45 degree angle, 25-26 gauge, 3/8 to 5/8 inch, less than 1.5mL
why should less than 1.5mL be used for SC injections
to avoid pressure on sensory nerves causing pain and discomfort
which factors may influence the choice of parenteral route of administration
onset or duration of action, setting where drug is to be administered
describe the types of vehicles used for parenteral drugs
-viscous, water-miscible vehicles (ex: aqueous gelatin, polyvinylpyrrolidone)
-water-immiscible, water-repelling agents (ex: vegetable oil)
parameters manipulated in the design of parenteral controlled forms
1. route of administration
2. drug delivery systems
3. particle size
4. chemical modification of drug
t/f: parenteral medications often need coadministration of vasoconstricters
true (lowers blood flow to increase drug duration at specific site)
3 classifications of parenterals based on mode of delivery
1. injectables (solutions/suspensions)
2. implants
3. infusion devices (pumps)
summarize the 3 types of solutions made for parenteral injections
1. aqueous (high viscosity)
2. aqueous complexed formulations (IM)
3. oil solutions (IM)
example of viscous, water miscible vehicles for parenterals
gelatin or polyvinylpyrrolidone
example of water-immiscible vehicles and water-repelling agents for parenterals
water-immiscible: vegetable oils
water-repelling: aluminum monostereate
what are high viscosity solutions used for in parenterals?
1. molecular weight >750Da
2. water soluble drugs
3. with gel agents/ viscosity enhancers
how are complexed aqueous formulations given
IM (aq)
how is drug release for oil solutions in parenterals controlled
controlled by partitioning of drug out of oil into surrounding into aqueous medium
how are oil solutions/suspensions in parenterals administered?
IM (oil)
how can aqueous suspensions be given
IM or SC
for aqueous parenteral suspensions, solid concentration should be? particle size?
concentration: 0.5-5%
size: <10 micrometers
compare length of drug action of oil suspension, aqueous suspension, and oil solution
oil suspensions have longest drug action. drug particles must dissolve then partition from oil solution to aqueous medium
penicillin G procaine in vegetable oil is an example of
oil parenteral suspension
release of water soluble drugs can be slowed by presenting it as what form of parenterals?
oil suspension
what is a microsphere and how is drug released controlled
-matrix of drug in polymer
- first order process, dissolution/degradation of matrix
small matrices release drugs at a ___slower?faster?___ rate
faster
examples of polymers used in microspheres
polylactic acid, polylactide coglycolide
microsphere vs microcapsule
microsphere: drug matrix-> dissolution (first order)
microcapsule: drug centrally located within shell-> dissolution or diffusion; for potent drugs
for potent drugs, are microspheres or microcapsules preferred
microcapsules (steroids, peptides, antineoplastics)
-> more controlled release
polymers used for nanoparticles/nanospheres
polyacrylic acid, polyglycolic acid
what are nanoparticles used for
targeted therapy (cancers)
niosomes
closed vehicles formed in aqueous media from NONIONIC surfactants (similar to liposomes)
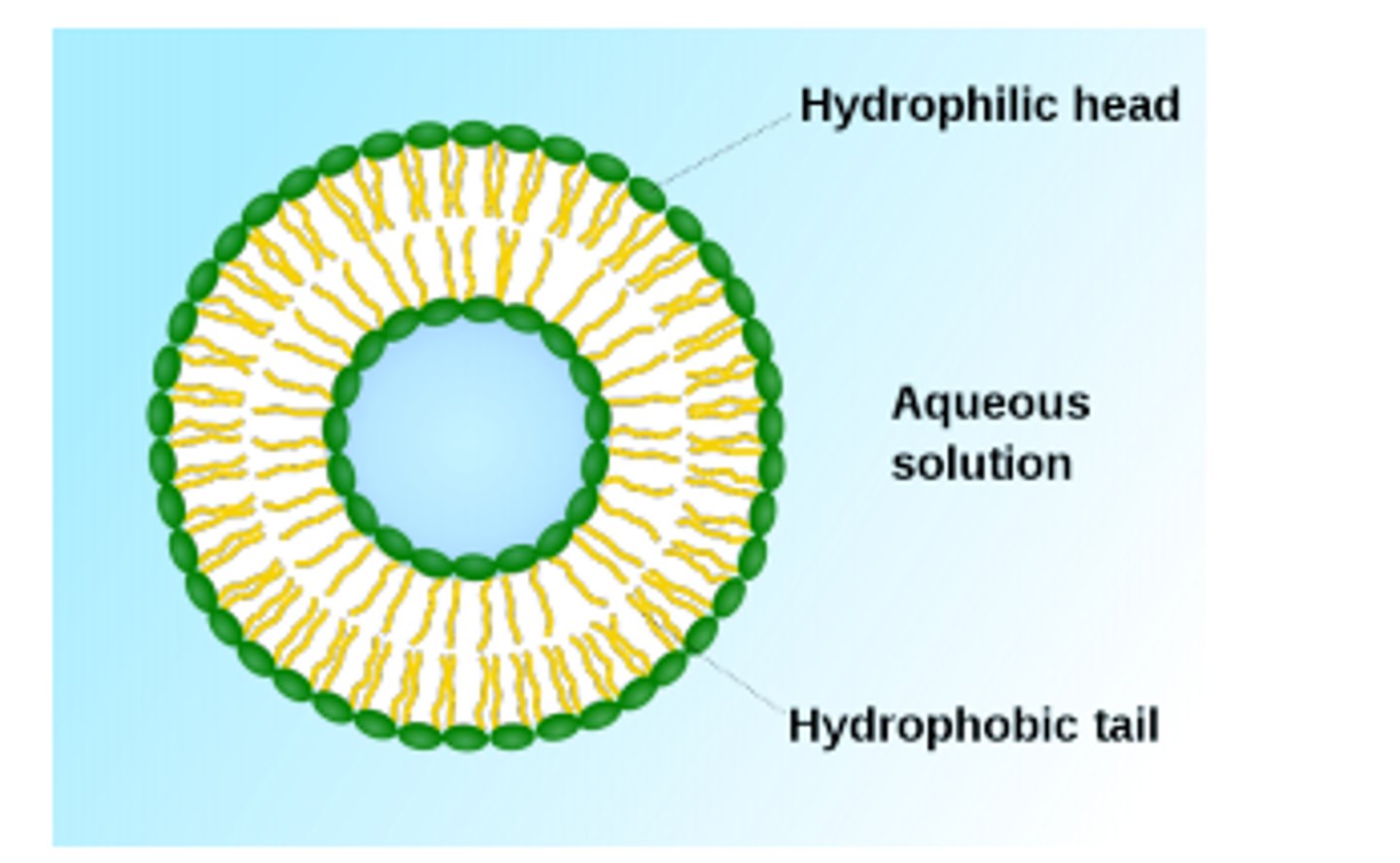
liposomes are? which lipids are used?
-spherical vesicle of lipid bilayers enclosing aqueous compartment (water soluble drugs)
- phospholipids, sphingolipids, glycolipids, sterols
liposomes can be given by which routes
IM and SC, can be IV for targeted delivery (cancers)
type 1 vs type 2 scFV conjugation to liposomes
type 1: scFv directly attached onto liposome (sterically hindered0)
type 2: scFv conjugated via flexible spacer (ex: PEG)
these are immunoliposomes with drug inside

properties of resealed erythrocytes for drug delivery
-biodegradable, biocompatible,nonimmunogenic
-circulate intravascularly for days, carry large amounts of drugs
-easy drug loading
-damaged= removed by liver
t/f: resealed erythrocytes can carry large amounts of drugs and stay in circulation for days
true
what factors may influence the choice of an injectable parenteral DDS
1. size of formulation
2. loading of drug
3. action and setting where drug is to be targeted or delivered