NUR 317 - Seizure Disorders
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Seizure
Sudden and abnormal electrical discharge of neurons in brain, interrupting normal function
May accompany other disorders or occur spontaneously without apparent cause
Seizure vs epilepsy
A seizure is a one time event while epilepsy is multiple seizures (aka seizure disorder)
Causes of seizure
Systemic
Hypertension
Stroke epilepsy
Lupus
Pre-eclampsia
Brain infection
Brain tumor
Brain injury
Metabolic
Acidosis
Electrolyte imbalances
Sodium, blood glucose
Hypoxemia
Substance use or withdrawal
Medications
Illicit drugs
Alcohol
Poisoning
Dehydration or water intoxication
Fever
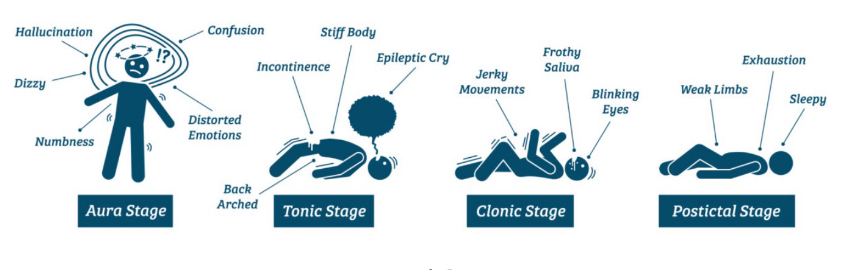
Phases of seizures
Prodromal phase
Aural phase
Ictal phase
Tonic phase
Clonic phase
Postictal phase
Can last hours to days
Generalized seizures
Seizures occur over both sides of the brain
Awareness impaired a few seconds to several minutes
30% of people with epilepsy have generalized seizures
Tonic-clonic seizures
Characterized by loss of consciousness and falling (if standing)
Body stiffens (tonic) with subsequent jerking of extremities (clonic)
Cyanosis, excessive salivation, incontinence, and tongue or cheek biting may occur
Generalized seizures postictal phase
Muscle soreness, fatigue
Patient may sleep for hours
May not feel normal for hours to days
No memory of seizure
Tonic seizures
Sudden onset of increased tone in the extensor muscles
Sudden stiff movements
Most often occur in sleep
Affects both sides of the body
Patients will fall if they are standing
Usually lasts less than 20 seconds
Patient usually stays aware
Clonic seizures
Begin with loss of awareness and sudden loss of muscle tone
Rhythmic limb jerking, that may or may not be symmetric, follows
Clonic seizures are rare
Atonic seizures
Also called drop attack
Involves sudden, brief loss of muscle tone
Begins suddenly with the person falling to the ground
Typically lasts less than 15 seconds
Brief loss of consciousness and brief post-ictal confusion
Great risk for head injury - often protective helmets are needed
Typical absence seizures
Staring spell
Person is usually unresponsive when spoken to
Lasts only a few seconds
Often goes unnoticed
Multiple episodes per day when untreated
Atypical absence seizures
Staring spell with other manifestations
Eye blinking
Jerking movements of the lips
Often lasts more than 10 seconds (up to 30 seconds)
Gradual beginning and end
To adulthood
Focal seizures
(Formally called partial seizures or partial focal seizures)
Seizures occur in one hemisphere of the brain
Manifestations based on function of area of brain involved
60% of people with epilepsy have focal seizures
Motor focal seizures
Atonic (loss of tone)
Tonic (sustained stiffening)
Clonic (rhythmic jerking)
Myoclonic (irregular, rapid jerking)
Some people show strange behavior - Lip smacking or other repetitive, purposeless actions (automatisms)
Non-motor focal seizures
Emotional manifestations - fear or joy, strange feelings
Racing heart
Goose bumps
Waves of heat or cold
Focal awareness
Conscious, alert
Unusual feelings or sensations
Sudden and unexplainable feelings of joy, anger, sadness, or nausea
May hear, smell, taste, see, or feel things that are not real
Focal impaired awareness
Loss of consciousness or alteration in awareness
Eyes remain open but cannot interact
May display strange behaviors
Automatisms
Ex. person counting money will continue counting, person walking will continue walking without awareness
Difficulty remembering recent actvity
Lasts 1-2 minutes, but patient may be fatigued after and not return to activity for hours
Status epilepticus
Continuous seizure activity or when seizures recur in rapid succession without return to consciousness between seizures
Neurons become exhausted and cease to function
Permanent brain damage can result
Any seizure lasting > 5 minutes
Neurologic emergency
Refractory status epilepticus
Continued activity despite 1st and 2nd line therapy
Nonconvulsive status epilepticus
Long or repeated focal impaired awareness seizures
Convulsive status epilepticus (CSE)
Prolonged and repeated tonic-clonic or other motor seizures
Can cause ventilatory insufficiency, hypoxemia, cardiac dysrhythmias, hyperthermia, and systemic acidosis
Can be fatal
Complications of seizures
Effect on lifestyle is most common complication of seizure disorder
Depression
Social stigma still exists
Ineffective coping
Discrimination
Driving sanctions
Diagnostic studies for seizures
Comprehensive health history
Including accurate description of seizures
EEG
May help determine type of seizure and pinpoint seizure focus
Many patients do not have abnormal findings
Magnetoencephalography in conjunction with EEG
Greater sensitivity for detecting small magnetic fields generated by neuronal activity
Other
CBC, serum chemistries, liver and kidney function
UA to rule out metabolic disorders
CT or MRI to rule out structural lesions
Seizure interprofessional care
Most seizures
are self-limiting
rarely cause bodily injury
Immediate medical care for:
Status epilepticus
Significant bodily harm
First-time seizure
Seizure disorders are primarily treated with antiseizure drugs
Prevent seizures with minimal drug side effects
Cure is not possible
Seizure mediation therapy
Medications stabilize nerve cell membranes and prevent spread of the epileptic discharge
Initiate therapy with a single drug
May need combination of drugs
Usually no more than 2 medications
Therapeutic ranges are guides
Newer drugs do not require serum drug levels
Seziure medication therapy patient teaching
Patients need to:
Take medication(s) regulalry and continuously (often for life)
Understand importance of following the specific drug regimen
Know what to do if a dose is missed
Broad spectrum seizure medication therapy
Gabapentin (Neurontin)
Topiramate (Topamax)
Lamotrigine (Lamictal)
Tiagabine (Gabitril)
Levetiracetam (Keppra)
Zonisamide (Zonegran)
Pregabalin (Lyrica)
Additional treatment for focal seizures
Status epilepticus medication therapy
Initially, rapid-acting IV lorazepam (Ativan) or diazapam (Valium)
Followed by long-acting drugs
Primary drugs for treatment of generalized tonic-clonic seizures
Phenytoin (Dilantin)
Carbamazepine (Tegretol)
Divalproex (Depakote)
Primary drugs for treatment of generalized non-motor and myoclonic seizures
Ethosuximide (Zarontin)
Divalproex (Depakote)
Clonazepam (Klonopin)
Primary drugs for treatment of focal seizures
Carbamazepine (Tegretol)
Lamotrigine (Lamictal)
Levetiracetam (Keppra)
Seizure medication side effects
Common side effects often involve the CNS and include:
Diplopia
Drowsiness
Ataxia
Mental slowing
Seizure medication therapy considerations
Can medication be given 1-2X/day?
Medications should be routinely reviewed and adjusted as needed
If weaning is to occur the patient must:
be seizure free for a prolonged period (e.g. 2-5 yrs)
have a normal neurologic examination
have a normal EEG
Serizure gerontologic considerations
Many experience a 1st single seizure
More responsive to antiseizure drugs
More likely to experience side effects at lower doses
Don’t excrete medications as well
Medication sondierations
Do not give phenytoin in patients with liver issues
Carbamazepine increases bone and cognitive issues
Seizures surgical therapy
Must have a defined site of origin
Surgical resection of that area
Laser ablation
Radiosurgery
Hemispherectomy (for severe cases)
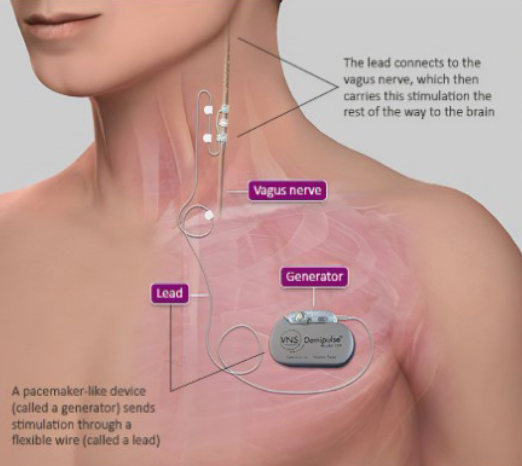
Vagal nerve stimulation seizure therapy
Adjunct to medications when surgery is not feasible
Exact mechanism not known
Thought to interrupt synchronization of epileptic brain-wave activity and stop excessive discharge of neurons
Seizure diet therapy
Ketogenic diet has been effective in controlling seizures for some
High-fat, low carbohydrate diet
Ketones pass into the brain and replace glucose as an energy source
Equally effective in children and adults
Seizure nursing assessment - triggers
Sleep deprivation
Flashing lights
Illness
Dietary changes
Certain medications
Missed medications
Specific foods (caffeine)
Alcohol
Etc
Seizure nursing assessment - prior to seizure
Aura
Mentation changes
Abnormal behaviors
Etc
Seizure nursing assessment - during seizure
Onset of seizure
Activity -
*body parts involved
*sequence of movement
*autonomic signs
Etc
Seizure nursing assessment - after seizure
Bitten tongue, soft tissue damage
Abnormal respiratory rate
Weakness, paralysis, ataxia (postictal)
Absent or abnormal breath sounds
Airway occlusion
Incontinence
Etc
Seizure patients hospital care
Seizure pads on bed rails
Bed rails up, bed in lowest position
Resuscitation equipment at bedside
Oxygen equipment at bedside
Suction equipment at bedside
In event of a seizure:
Observe, maintain patient safety and document
Ensure ABC’s and Safety:
Maintain patent airway
Support head
Protect - turn to side, loosen constrictive clothing, ease to the floor
Do not restrain patient or place any objects in their mouth
Post-seizure care
Ensure safety and continue assessments
Neuro assessments
Assess for injuries
Allow for periods of rest and sleep
Seizure nursing interventions and care
Emotional support and identification of coping mechanisms
Does patient have a medical alert bracelet or ID card?
Seizure response service dog
Seizure safety measures
Wear helmet if risk for head injury
Carpeting in home/on stairs
Protective padding/cushions on sharp corners, handles, faucets, etc.
Seizure education
Promote general health habits (diet, exercise)
Instruct to avoid excessive alcohol, fatigue, and loss of sleep
Assist to identify events or situations precipitating seizures and avoid if possible
Education regarding prevention of recurring seizures
Adherence to medication, do not adjust dose without physician instruction
Keep routine appointments
Teach family members emergency management