Exam 4
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
Factor P
Contemporary exercise prescriptions are largely non-purposeful in nature… ie. walking on a treadmill to nowhere- need to get back to going outside and getting activity- Morgan (2001)
Fitness Equipment Sales in America
Makes no sense that we are one of the least fit countries in America, yet we spend the most on equipment (connect to factor p)
Regular leisure-time: Hawaii
Closest to 50% average (target physical activity)… because it’s nice and people walk everywhere (expensive to have car so people actively commute)
Determinants of Physical Activity- Positive
Personal: History of activity (strong)… expected benefits… enjoyment of exercise… intention of exercise… self-efficacy… self-motivation… Environmental: spouse/social support… facility access… physician counseling… geographic region… Physical: choice of type…
Determinants of Physical Activity- Negative effect
Personal: Smoking… Overweight… Blue-collar job (strong)… High CHD risk(strong)… expected barrier/costs… Environmental: perceived lack of time (strong)… Physical: frequency (strong)… duration (strong)… perceived exertion (strong)
Determinants of Physical Activity- no effects
Personal: School sports… Health behaviors… Knowledge of exercise…Attitude… Physical: intensity…
Exercise is maintained when it is reinforced by aspects of the social and physical environment
stimulus control techniques and reinforcement control techniques
stimulus-control techniques
Text someone daily if they’ve gotten workout in (if you respond no it keeps texting you about the benefits of working out)
reinforcement control
contingency management (reward/punishment), goal setting, contracts, and so forth.
Goal Setting
Goals regulate behavior by providing direction, mobilizing effort, and instigating the search for ways to attain them… you can devise a plan that directs activity and emphasizes the link between behavior and outcome… Specific, measurable goals are easier to monitor and make adjustments.
Behavior moves through 5 stages
Prochaska- pre-contemplation (make people aware), contemplation (move people to prepare- inform people how to start), preparation (prompt people to act), action (implement the plan- goal setting-need social support), maintenance (prevent relapse of inactivity)
Processes of change
Cognitive- conscious raising and planning (intention affected by role model, perceived barriers/benefits, and confidence- shaped by, present success, role models, persuasion, and perceived exertion- makes them start and stick to it)
Behavioral- stimulus control and reinforcement control
Relapse prevention
Marlatt & Gordon- designed to help smokers and drug abusers- helped with new exercise programs… you must •Identify situations that put you at high risk for relapse… plan how to avoid/cope in this situation… Put the consequences of not exercising in perspective… Expect and plan for lapses (injuries/vacation)… •Block self-talk and images that focus on the benefits of not exercising… “Abstinence Violation Effect”… enjoy exercise
“Abstinence Violation Effect”
Don’t have an “all-or-nothing” attitude… if you mess up you shouldn’t feel like it’s the end of the world… after you mess up once, yoiu’re more likely to do it again due to shame
Successful interventions- community task force
Informational approaches- communitywide campaigns (had largest effect), point-of-decision prompts (using stairs)
Behavioral and social approaches- school-based physical education, social support interventions in community settings, individually adapted health behavior change
Environmental and policy approaches- creation of or enhanced access to places for physical activity combined with informational outreach activities
Successful interventions programs teach
goal-setting and self-monitoring of progress, building social support for new behaviors, behavioral reinforcement (self-reward and positive self-talk), structured problem solving to maintain the behavior change, prevention of relapse into sedentary behavior.
Physical Activity Interventions- Dishman & Buckworth, 1996
Meta-Analysis of 127 studies (445 effects)-131,000 participants-Overall effect was moderate to large-Mean r = 0.34 (~ 0.75 SD)- Equivalent to increasing success rate from 50% to 67%… effects didn’t differ across gender/age… largest effect= behavior modification, community based, groups, active leisure, mediated delivery, low intensity
Walkability>Driving/Walking>Obesity
10,800 Atlanta adults- Living in walkable neighborhoods (mixed use, grid streets) was related to: More walking for transport, Less driving, Less obesity (Each hour driving = 6% more risk of obesity)
Walking has decreased as obesity has increased, we need to make neighborhoods/cities more walkable and safe
Tips for exercise Success
Choose for enjoyment •Choose for goals (have more than one)•Be comfortable (breathing not heart rate) •Pick a place and time (convenient) (first act of the day) (routine, not drudgery) •Find a buddy •Be flexible (a slip up is not failure) •Short term pleasure, long term gain
What we know about physical activity
Social-Cognitive factors explain 25-40% of physical activity, Genetically transmissible factors explain about 20%, Interventions yield short-term increases in PA by 20-35%
What we don’t know about adherence
Patterns of natural change within people, Impact of environmental change, Impact of genes, Personal mediators and moderators of change, Interaction of culture, environment, and adaptability on choice
Angina Pectoris
Severe, constricting pain in the chest… often behind the sternum, but also common in the left shoulder and down the inside of the left arm or in the throat or neck. Less common in both arms, jaw or back… squeezing, crushing or strangling pain or pressure… from fullness or tingling or just noticeable pain to unbearable and excruciating. Sometimes a fear of imminent death or “angor animi”… best predictor of presence of heart disease… if having angina and coronary artery disease, makes it worse
Not all chest pain is due to cardiac ischemia (heart attack)
Non-ischemic causes aortic aneurysm, pericarditis (inflammation)
Non-cardiac causes: pulmonary disease (e.g., pneumothorax), GI disease - pancreatitis, esophageal spasms (acid reflux)
Convergence
Why angina occurs in different location- inside of your left arm feels like its being crushed during a heart attack… Sensory afferents from the left viscera, chest, shoulder, and upper arm synapse (converge) on the same ascending nerves starting in T1-T5 and projecting to the thalamus… Sensory info from areas such as the neck and hand enter at a different level of the spinal cord, but the nerves from these areas converge on the same primary ascending neural pathway
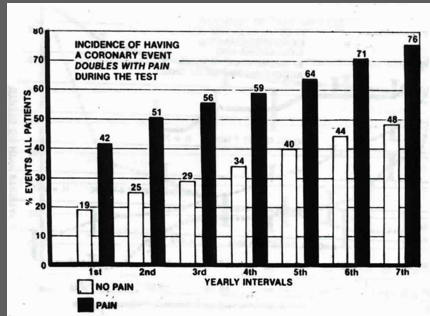
Probability of reoccurrence
If you have a heart attack event- disease progression- doubles in people with chest pain/depression… if you have both you have twice the risk (50% more) of having an additional event… males have a higher risk… more pain/higher chance of event
Stable angina
refers to individuals who repeatedly experience pain during exercise at approximately the same rate pressure product (RPP = HR x SBP). RPP is highly correlated with the work of the heart and myocardial oxygen consumption. (PREDICTABLE)… You will get exercise prescription to stay below the zone the heart rate that causes you the pain
Unstable angina
angina at rest or that occurs with minimal physical activity, or that has recently changed from being stable to being more severe, prolonged or frequent. (wouldn’t want this because its unpredictable)
Stress test
tells you severity of disease- getting worse/staying the same/or better via the yearly test… can tell from chest pain ratings… lower heart rate= same pain rating… arteries are more clogged- worsening heart disease
Syndrome X
5-20% of people who undergo diagnostic angiography after exhibiting evidence of exercise-induced cardiac ischemia and experiencing angina are found to have normal coronary arteries and no other apparent cause for the chest pain (they are okay)
silent ischemia
Painless episodes- They cant feel the pain, they don’t stop what they’re doing, dead… hypertension can stop the feeling of pain too, they start having a heart attack and can’t feel it muscle of the heart stops working and they die
regional myocardial ischemia
occurs (demand for oxygen exceeds supply) due to increased work of the heart not being matched by adequate flow - often due to a reduction of flow in the coronary arteries
cardiac ischemia
causes a need for anaerobic glycolysis in order to produce energy to keep the heart muscle functioning… glycolysis causes an increase in the regional concentration of a hydrogen ions; ischemia also stimulates the production of lactate and other noxious biochemicals… What to do in case of heart attack- Stop what you’re doing, call the paramedics, and take Asprin, don’t move
Brain activation during angina
Periaqueductal grey, Hypothalamus, Thalamus, Pre-frontal cortex, Anterior cingulate cortex
Importance of pain
Muscle pain is a prevalent clinical problem… Muscle pain reduces quality of life… Muscle pain may contribute to inactivity and the associated reductions in health
Chronic Pain Prevalence
2016- 20.4% US adults had chronic pain (8%=high impact pain)- older age=higher prevalence… women (34%) are more likely to report pain than men (27%)… 18-24 are least likely to report chronic pain (7.0), 25-44 is (13.2%), middle aged adults age 44-64 and 64-85 (27.8%) report pain, and adults age 85 and over are the most likely to report chronic pain (33.6%)… costs $560 billion to $635 billion for Americans
Pain
an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage (subjective/emotional)… not always porportional to actual tissue damage
Nociception
Differs from pain… The sum of neurochemical events involved in the identification of and reaction to a noxious stimulus (tissue threatening or tissue damaging)… can occur without pain and pain can occur in the absence of evidence of tissue damage.
Nociception system
The neurobiological apparatus for providing the brain with information about actual or potential tissue damage
Nociceptors
Free nerve endings that increase their firing rate in response to noxious stimuli… Two types of axons - Type A and Type C fibers… High density in skin, muscle, & viscera (None in the brain)… located primarily along the walls of the arterioles and in the surrounding connective tissue… can cause chronic pain if damaged
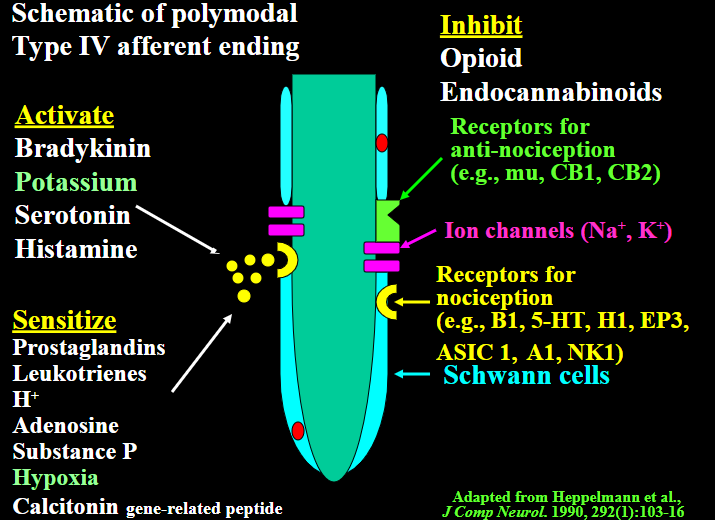
Polymodal Type IV afferent ending
Activates pain- Bradykinin, Potassium, Serotonin, Histamine… Sensitizes pain- Prostaglandins, hydrogen ions, Hypoxia… Inhibits pain- opioids, endocannabinoids
Major Ascending Spinal Tracts
Spinothalamic tract: sensory cortices, hypothalamus
Spinoreticular tract: locus coeruleus
Spinomesencephalic tract: PAG, amygdala, anterior cingulate
What activates when the brain is in pain?
Thalamus, S1 & S2 - somatosensory, Insular cortex - cardiovascular, Prefrontal & parietal - cognitive, Anterior cingulate - affect/attention
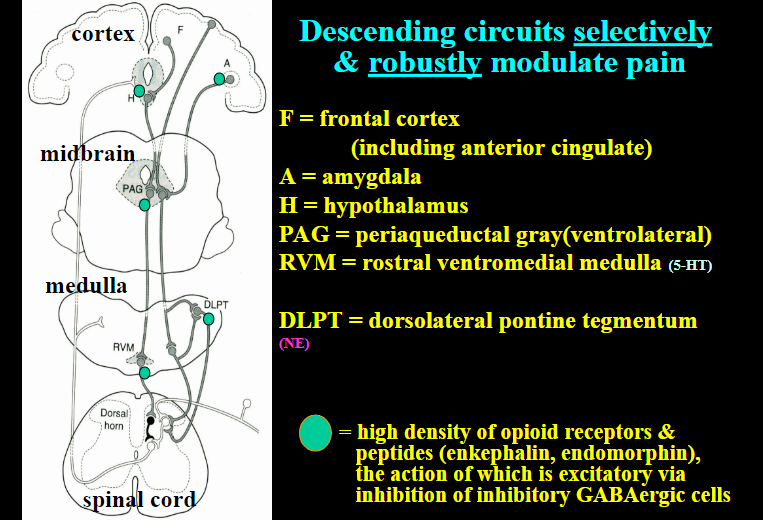
Descending circuits
selectively & robustly modulate pain… this about only one track being able to go up to the brain so the other pain cant travel… Nerves descending from the RVM and DLPT inhibit nociception directly, and indirectly by exciting inhibitory interneurons
Control over brain activation
Individuals can gain voluntary control over activation in a specific brain region given appropriate training, that voluntary control over activation in rACC leads to control over pain perception, and that these effects were powerful enough to impact severe, chronic clinical pain
Measures of pain
Pain threshold - min. stimulus… Pain tolerance - max. stimulus
Pain intensity - how much? Pain affect - how unpleasant? Pain location - where? Pain quality - hot, sharp
Measurement tools of pain
McGill Pain Questionnaire (Melzack 1975) MPQ… Visual analog scale… Descriptive differential scale (Gracey 1988)… Nociceptive flexion reflex (Hugon, 1973; Willer, 1977)
Nociceptive flexion reflex (Hugon, 1973; Willer, 1977) (R-III)
Withdrawal reflex… The time course of the response, determined by the threshold and amplitude of skeletal muscle activation…
Factors reducing threshold: repeated stimulation over short period of time – increasing duration of the stimulus from .1 msec to .6 – anticipation of an intense noxious stimulus – an intense (70 mA) sural nerve stimulation – obesity – negative mood
Factors increasing threshold: Acetaminophen - electro acupuncture – Codeine - hypnotic suggestion of analgesia - positive mood – Ibuprofen - hypertension – increase w/ age, time of day (pm) – Ketoprofen - Caffeine – Morphine - chewing gum – Nefopam hydrochloride - gastric & slow rectal distension – slow wave and REM sleep - sweet taste
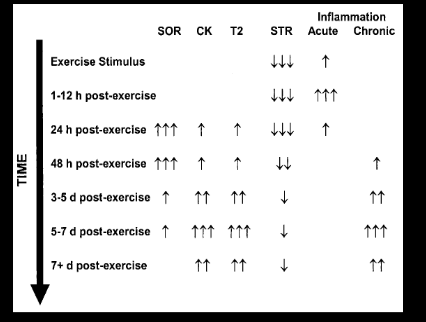
Delayed onset muscle pain
the day you exercise you have acute pain, but the pain really sets in 5-7 days afterDD
Hypoalgesia
decreased sensitivity to painful stimuli, or diminished pain in response to a normally painful stimulus
Do different athlete groups process pain differently?
Contact sport athletes had a higher pain tolerance as they could withstand the pain longer than athletes in non contact sports/non-athletes
Potential factors for manipulation experiments
Muscle/core temperature, Muscle hydrogen ions, Prostaglandins, Opioid receptors, Adenosine receptors, Cognition, CAFFEINE, naloxone
Experiments manipulating cognitive factors
Hypnosis-Prolonged rhythmic behavior of chewing
suppresses nociceptive responses via the 5-HT descending inhibitory pathway… Dissociation- had a higher performance (more min) than control
Sweet Taste Influences Pain Sensitivity
20 females and 14 males college age- 3 days of testing pain threshold and nociceptive flexion reflex… found people who had sugar had significant increase in NFR score (13.1%) & pressure(6.5%)/cold(20.4%) pain threshold
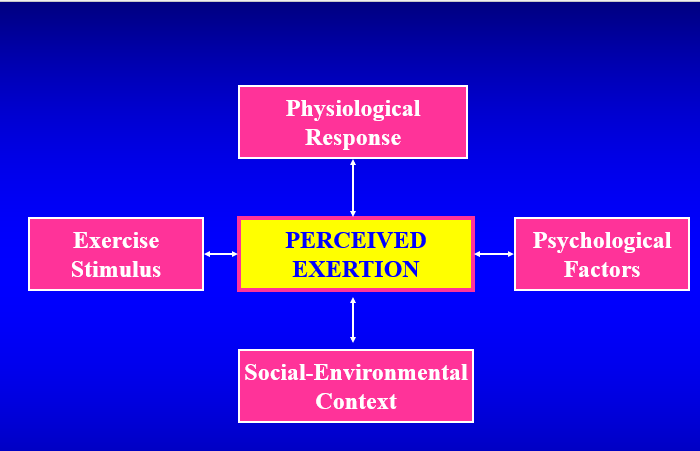
What is perceived exertion?
•Subjective detection and interpretation of the intensity of effort or strain during exercise (dif from fatigue/pain)… •Factors such as breathing, pain, fatigue, sweating, and muscular force come together to make overall feeling of effort
Gunnar Borg
founder of perceived exertion concept- developed first scale
Psychophysics
•Scientific field which studies the perception of physical stimuli… •Study of a subjective response (perceived exertion) to an objective stimulus (exercise)
Sensation
•passive process of detecting a stimulus following stimulation of a sensory organ
Perception
active process of interpreting sensory information
Scaling
measurement of sensation by the assignment of numbers to describe or differentiate perceptual events (nominal-ID number, ordinal-1st,2nd,3rd, interval-thermometer, ratio-ruler)…
Ratio Scales
Yields most accurate description of relationship between stimuli/perceptions… type of scale: Cross-modality matching, Magnitude estimation, Magnitude production… problem! inter-individual comparisons not possible
Cross-modality matching
observer matches the apparent intensities of stimuli across two sensory modalities, as when an observer adjusts the brightness of a light to indicate the loudness of a variable stimulus sound…magnitude production/estimation are both this…
Magnitude Production
The subjects adjust the magnitude of a stimulus to match a numerical value given by the experimenter.
Estimation task
subject assigns a number to represent the intensity of a reference stimulus and then uses that number to rate following stimuli
Production task
subject adjusts the intensity of a stimulus to approximate a given proportion of the reference stimulus
Weber’s Law
a linear relationship exists between a stimulus and a response… •the ratio between the change in the stimulus required to produce a jnd and the stimulus is equal to a constant fraction (K)… as the stimulus increases, the jnd increases at a constant rate
Fechners law
•proposed that the relationship between a stimulus and a response was not linear… •the jnd or response (R) increases logarithmically as the stimulus increases
Steven’s Power Law
•the sensation of a stimulus grows as a power function of the stimulus… •each stimulus (light, sound, exercise) has a power function… •the magnitude of the response (R) is equal to a constant (k) multiplied by the intensity of the stimulus (S) raised to the nth power
Borg’s Modified Power Law
•Borg modified Steven’s Law for perceived exertion by adding 2 terms: a : perceptual noise b : stimulus threshold… •this adjusts for factors which may influence a person’s resting perception and initial perception of effort… As power output increases linearly, the perception of how intense the exercise stimulus feels grows exponentially.
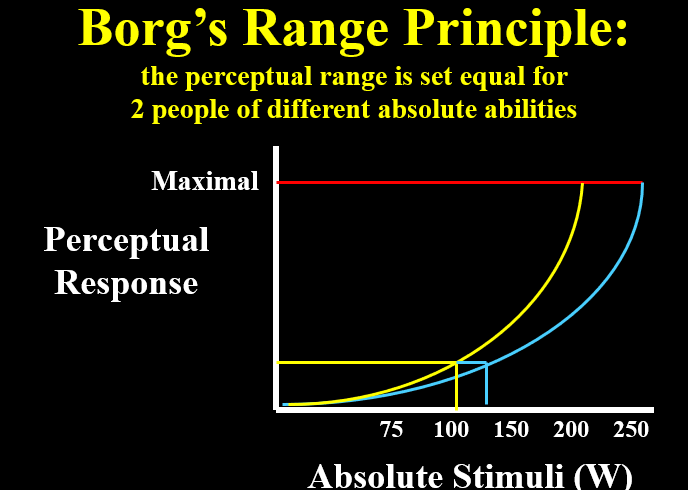
Borgs Range Principle
•Assumes that all people have the same perception at a subjective maximum intensity (varies by person) •All people have the same perception of “maximal effort” and “no effort” •The perception of “hard” is the same for everybody •Allows for comparison of RPE’s among individuals
Differentiated/local ratings of perceived exertion
•ratings obtained for a specific body part or region (ex: legs)
Global ratings of perceived exertion
ratings of an individual’s overall perception of effort
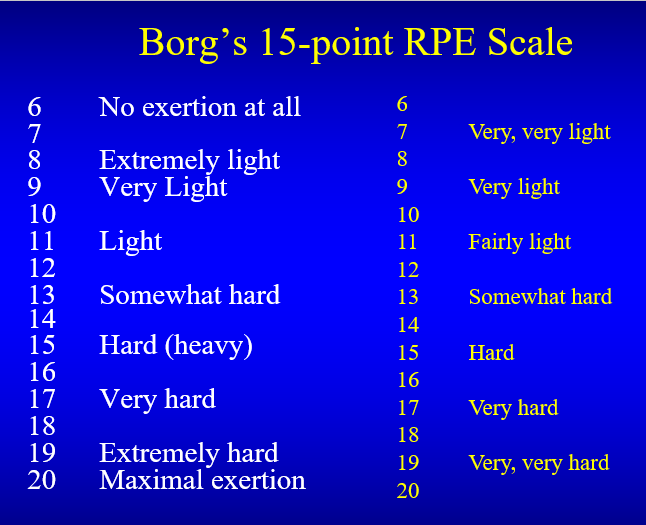
Borg’s 15-point RPE Scale
•Most common and useful for most applications… Interval/ordinal category scale… numbers range from 6-20 with attached verbal anchors… constructed to give HR estimates from 60 bpm (rest) to 200 bpm (maximum)… HR = RPE x 10 [+ 20 to 30 bpm correction]… yields a linear function…
Problems: ceiling effect… not a ratio scale
![<p><span>•Most common and useful for most applications… Interval/ordinal category scale… numbers range from 6-20 with attached verbal anchors… constructed to give HR estimates from 60 bpm (rest) to 200 bpm (maximum)… HR = RPE x 10 [+ 20 to 30 bpm correction]… yields a </span><strong><span>linear </span></strong><span>function…</span></p><p><span>Problems: ceiling effect… not a ratio scale </span></p>](https://knowt-user-attachments.s3.amazonaws.com/0f635ea3-26a6-494f-95d0-833517651e21.png)
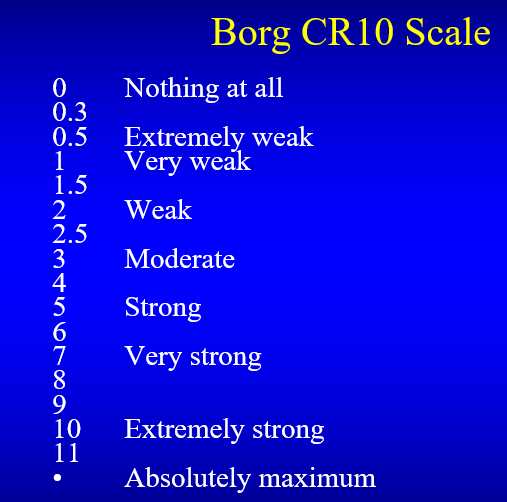
Borg CR10 Scale
•often a research tool… category-ratio scale… numerical scaling (0-10) with free-floating endpoint and verbal anchors… allows perceived exertion to follow a power function… not limited by ceiling effects
Proposed Physiological Mediators
•Heart Rate •Oxygen Uptake (relationship can be altered by thermal stress, change in blood lactate, and training) •Lactate (RPE 13-15-lactate threshold reached)- all three previous objective variables are correlated with RPE (not directly sensed)… •Temperature regulation (core body temp- not sensed, and skin temp- sensed) •Catecholamines (hormones released from adrenal medulla (regulates emotional response/blood glucose/glycogen) in response to stress- increase with exercise) •Muscular contraction •Ventilation (people can detect it- RPE 13-15)
Signals from skeletal muscle that contribute directly to RPE
Force = Ib & tension… Stretch = Ia & II… Pressure = Type III… Noxious biochemicals = Type IV H+, bradykinin, 5HT (serotonin)... Skin & muscle temperature = Type III and some IV
Sensory Pathways for Perceived Exertion
Dorsal-Column Medial Lemniscal System… Thalamus somatosensory cortex… Force, stretch, pressure, vibration
Anterolateral System (Spinothalamic tract etc.)… Amygdala, ACC, locus coeruleus… Nociception & temperature
Muscular Contraction
•feedforward mechanism- motor (efferent) commands are simultaneously transmitted to the working muscle and the sensory cortex in the brain •feedback mechanism - transmits sensory (afferent) information regarding tension, velocity, and position from peripheral receptors in the muscle to the sensory cortex •feedforward-feedback mechanism - combined mechanism allows the complex processing and adjustment of afferent and efferent information
Psychological Influences
•Anxiety, depression, and neuroticism are associated with errors in rating perceived exertion •increased somatic perception is associated with increased RPE •extroverted individuals may give lower RPE’s and prefer to exercise at higher intensity •hypnotic suggestions of increased or decreased workload have been shown to influence RPE and ventilation
Psychosocial and Contextual Cues
•Cultural and social influences –shape attitude toward physical activity –may influence general rating style
•Setting –characteristics of the scale administrator (gender, attractiveness) –exercise context (competition, research, medical evaluation) –exercise environment (outdoor, laboratory, hospital)
Factors of RPE
Valid because: It is moderately-to-strongly correlated to objective measures of exercise intensity, and most importantly, Experimental manipulations in exercise intensity, physical capacity or relevant psychological states result in appropriate changes in RPE.
Potential invalidity: Practice… Faking… Poor perceptual ability
Use of RPE
•serve as a subjective indicator of peak intensity •monitor the progression of the test and act as a cue to prepare the administrator for test termination •monitor changes in power output following exercise training •monitor individuals with health conditions •aid in communication among labs and clinics
ASCM exercise prescription- heart rate
10% of people meet this- 3-5 days/week… 20-45 minutes/session… 50-85% VO2max… Assumes that HR and VO2 is linear when actuality underestimate VO2peak at lower percentages and overestimate VO2peak at higher percentages of HR reserve…
Problems: •Large degree of variation in maximal HR •Difficulty in palpating and counting HR •Influenced by medication or emotional state
Exercise Prescription: Perceived Exertion
•RPE 12-16 typically corresponds to 50-85% VO2max •3 practice trials appear to be sufficient to enable a person to accurately produce a prescribed intensity based on RPE •preferred exertion - when a person is allowed to choose an exercise intensity, resulting RPE’s are typically in the range of 11-14 (below lactate threshold); may have important implications for promoting exercise adherence
Limitations: Liars… Some lack perceptual abilities (kids under 10… psychopathology)… GXT estimation vs production (If you test people on a bike then put them on a treadmill there is a little difference (mode specificity))