Gas Exchange and Transport: Oxygen
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
28 Terms
Describe the two separate blood supplies to the lungs.
1) Bronchial Circulation
Purpose:
Part of the systemic circulation, not pulmonary circulation.
Its main job is to oxygenate the lung tissue itself (the bronchi, bronchioles, and connective tissue) — the lung parenchyma.
Flow:
Bronchial arteries (from systemic circulation, usually off the aorta) supply oxygen-rich blood to lung tissue.
After passing through the bronchial capillaries, most of the blood drains into bronchial veins.
Key point:
Some of the deoxygenated bronchial blood mixes with oxygenated pulmonary venous blood.
This is called an anatomic shunt — a small amount of deoxygenated blood reduces the PO₂ slightly in the blood returning to the heart.
2) Pulmonary Circulation
Purpose:
Part of the low-pressure system carrying blood between heart and lungs for gas exchange.
It’s main job of pulmonary circulation is to carry deoxygenated blood from the heart to the lungs for gas exchange and return oxygenated blood back to the heart.
Flow:
Pulmonary arteries (from right ventricle) carry deoxygenated blood to pulmonary capillaries around alveoli.
Gas exchange occurs: CO₂ leaves blood, O₂ enters blood.
Pulmonary veins carry oxygenated blood back to the left atrium of the heart.
Key points:
Pulmonary arteries carry deoxygenated blood (opposite of most arteries).
Pulmonary veins carry oxygenated blood (opposite of most veins).
Pressures are low compared to systemic circulation, which helps protect the delicate alveolar capillaries.
How do PO2 and PCO2 gradients drive gas exchange?
Principle: diffusion along a partial pressure gradient
Gases move from areas of high partial pressure (P) → low partial pressure (P)
In the lungs:
O₂ diffuses from alveoli → blood because PAO₂ > PvO₂
CO₂ diffuses from blood → alveoli because PvCO₂ > PACO₂
2. Pulmonary circulation specifics
Deoxygenated blood arrives in pulmonary capillaries
PO₂ ≈ 40 mmHg
PCO₂ ≈ 45 mmHg
Alveolar air in the lungs
PO₂ ≈ 100 mmHg
PCO₂ ≈ 40 mmHg
Diffusion occurs:
O₂ moves into blood until arterial PO₂ ≈ 100 mmHg
CO₂ moves into alveoli until blood PCO₂ ≈ 40 mmHg
→ tissues (~40 mmHg) → venous blood (~40 mmHg)
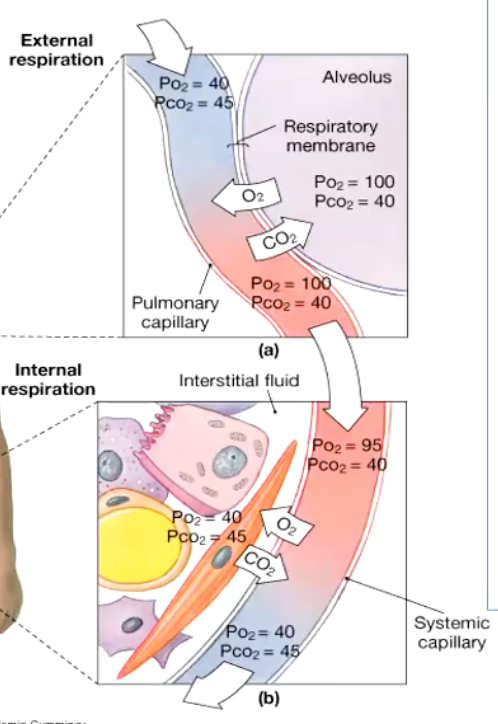
Describe the two processes occurring in the pulmonary and systemic circuit.
1. Pulmonary circuit
Blood enters the lungs via pulmonary arteries (deoxygenated, high CO₂).
O₂ enters the blood from alveoli → arterial PO₂ rises.
CO₂ leaves the blood into alveoli → exhaled.
Cardiac output (CO) determines the volume of blood passing the lungs per minute, which also determines how much O₂ and CO₂ is exchanged per minute.
2. Systemic circuit
Oxygenated blood leaves the lungs via pulmonary veins and travels to tissues.
At tissues:
O₂ leaves the blood → used by cells
CO₂ enters the blood → produced by metabolism
similar volumes of CO2 and O2 move each minute (Which is why it is called gas EXCHANGE).
What is the driving force for gas movement?
Diffusion is the driving force for gas exchange at the respiratory surfaces
All animals have some of the thinnest respiratory membranes to allow good diffusion
What is a gas exchange membrane?
Thin partitioning between internal and external compartments promoting flux of respiratory gases
How does the thickness of blood/water/air barriers change from fish, to amphibians, to reptiles, to mammals, to birds?
What is the respiratory unit?
Respiratory unit = gas exchanging unit: basic physiological unit of the lung consisting of respiratory bronchioles, alveolar ducts and alveoli.
Describe the pressure of gas through the anatomic dead space → the body.
Anatomic Dead Space
PIO2 = 150
PICO2 = 0
Alveoli
PAO2 = 102
PAACO2 = 40
Pulmonary Artery
PVO2 = 40
PVCO2 = 46
Pulmonary Veins
PpvO2 = 102
PpvCO2 = 40
**PI = partial pressure inhaled
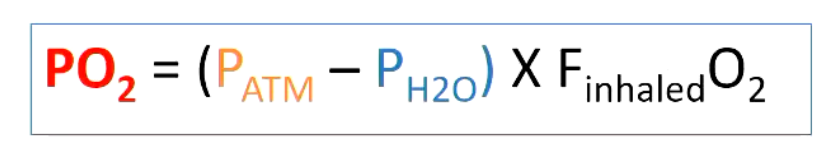
Why does ATM alter partial pressure of O2?
Therefore if atmosphere pressure changes (eg altitude), there will be a change in PO2
• The partial pressure of O2 alters depending on other factors eg atmospheric pressure (Ратм)
• PO, can be calculated by this equation:
PATM in mmHg
FO2 = mole fractional concentration of oxygen in air (0.21 for air), always 21%, unless you change

Why does water vapour molecules alter the partial pressure of O2?
Presence of water vapor molecules, which reduces concentration of O2. PO2 is less in humidified air, PO2 of humidified gas in airways is calculated by (Equation in photo)
• PO, is less in humidified air
• PO, of humidified gas in airways is calculated by:
What is the arterial PCO2?
40
Why does the partial pressure of O2 drop as we arrive in the alveoli?
Air composition vs alveolar air
Atmospheric air (trachea) has a PO₂ ≈ 160 mmHg (21% of 760 mmHg at sea level)
Alveolar air has PO₂ ≈ 100 mmHg
Why the drop? Two main reasons:
2. Moisture in the airways
As air travels down the trachea and bronchi, it becomes fully humidified
Water vapor contributes ~47 mmHg to total pressure
This reduces the partial pressure of O₂
3. Gas exchange in alveoli
Alveoli aren’t empty — they contain:
Residual CO₂ from blood (~40 mmHg)
Some remaining O₂ from previous breaths
The presence of CO₂ dilutes the O₂, lowering PO₂ further to ~100 mmHg
Why does PAO₂ (alveolar PO₂) equal PpvO₂ (pulmonary vein PO₂), and why is this important in hypoxia?
Equilibration: Pulmonary capillary blood equilibrates with alveolar air, so PAO₂ ≈ PpvO₂.
Mechanism: O₂ diffuses down its partial pressure gradient until no difference remains.
Importance in hypoxia:
Low alveolar PO₂ → low pulmonary vein PO₂ → reduced O₂ delivery to tissues.
Highlights that alveolar oxygen sets the maximum systemic oxygen level.
What are the two forms that O2 can be carried in the blood?
i) Dissolved (measured clinically in arterial blood Pa°2) -very small %
ii) Bound to haemoglobin (Hb)
• Haemoglobin (Hb) is major transport molecule for O, found in red blood cells.
• Hb: four heme (iron porphyrin compounds) groups joined to globin protein (two a chains and two ß chains polypeptide chains).
• Each heme group contains iron in the reduced ferrous form (Fe**), which is the site of 0, binding.
Oxygen transport can be modified by what three mechanisms?
1. Concentration of pigment (Hemoglobin conc.)
2. Rate of circulation (cardiac output etc) - how quickly it moves around body
3. O2 affinity of pigment (Hemoglobin)
Describe how the concentration of pigment varies among different species.
Concentration of pigments is very variable
• birds and mammals 15-20ml/100ml
Lower in invertebrates with Hb
• annelid 4-6ml/100ml)
Animals with haemocyanin tends to be even lower
• squids and octopuses 3.7ml/100ml
• crabs/prawns 1ml/100ml
How does the rate of circulation change?
• Circulatory system of mammals and birds operates at leisurely pace at rest
• During exercise O2 demand increases so circulatory system responds
Venous blood becomes much more deoxygenated during exercise than at rest

What factors affect the oxygen affinity of haemoglobin?
• Degree of Hb oxygenation depends on PO2
High PO2 = at lungs (promote uptake onto the haemoglobin)
Low PO2 = at tissues (promote oxygen being pushes off - into the tissues)
What does 100% saturation mean?
All O2 binding sited occupied
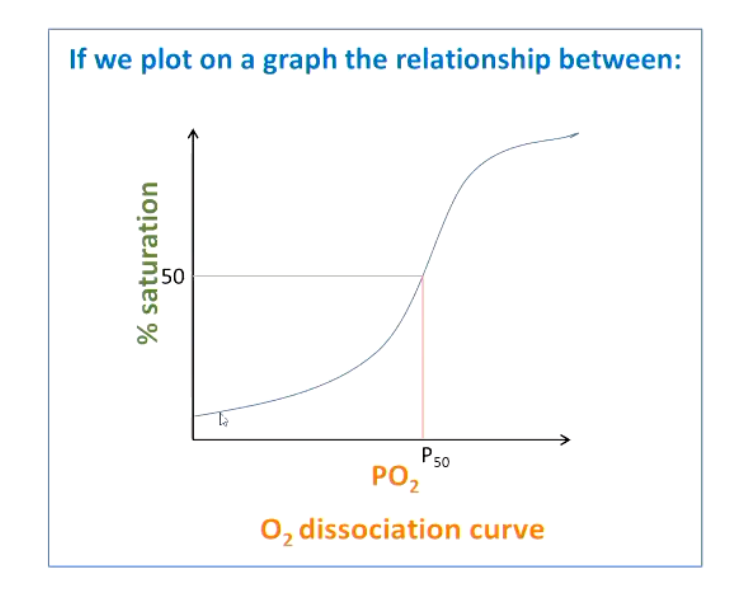
Describe the oxygen affinity curve.
What is P50?
P50 = the partial pressure of 02 at which 50% of pigment is bound to 02
How does the oxygen affinity curve change with hemoglobin and myoglobin?
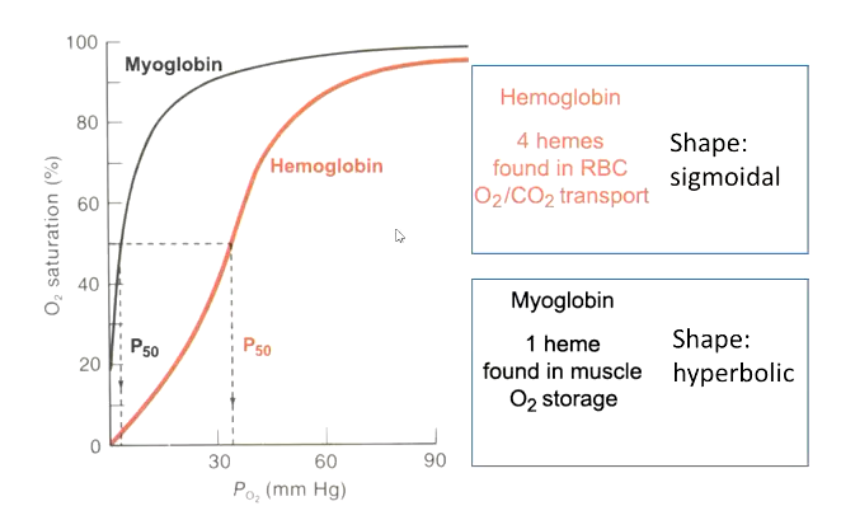
Why does hemoglobin show a sigmoidal curve?
Cooperative binding, binding at one site increased affinity at the remaining sites
Partially oxygenated Hb is more likely to bind O2 than fully deoxygenated molecule
Cooperatively enhances the responsiveness to changes in PO2
Cooperative binding means:
Binding of O₂ to one subunit → increases the affinity of the remaining subunits for O₂
Releasing O₂ from one subunit → decreases affinity of the others
How does oxygen affinity vary?
If oxygen affinity is lowered, how does the curve shift?
Respiratory pigments of various animals vary in their O2, affinity
• Pigments that bind O2 at low PO2 HIGH AFFINITY
• Pigments that require a higher PO2, to bind O2 LOW AFFINITY
Shift to the right, means O2 more difficult to bind to Hb, but easier to release O2
What are the factors affecting O2 affinity?
1. pH and CO2 - The Bohr effect
2. Temperature
3. lons
4. Organic compounds
How does pH or the Bohr effect alter oxygen affinity?
• Oxygen affinity depends on the PCO2 and the pH
Low pH (more acidic) or high CO₂ → stabilizes deoxygenated Hb (T state) → reduces O₂ affinity - right shift
High pH (more basic) or low CO₂ → stabilizes oxygenated Hb (R state) → increases O₂ affinity - left shift
In tissues (high CO₂, low pH from metabolism):
Hb releases O₂ more readily → oxygen delivered to metabolically active cells
In lungs (low CO₂, higher pH):
Hb binds O₂ more tightly → efficient oxygen loading
Enhancing oxygen delivery means lowering oxygen ____.
affinity
How does temperature alter O2 affinity?
• Increase in temperature decreases O, affinity → shift to right
Enhancing O2 delivery to muscles, similar to Bohr effect
How do inorganic ions and organic compounds alter O2 affinity?
3. Inorganic ions O, affinity
• lons in the blood can allosterically modulate O2 affinity of respiratory pigments
• Cl ions in RBCs critical allosteric modulator
They bind to hemoglobin at specific sites → stabilize the deoxygenated (T) state.
Decreases O₂ affinity → Hb releases O₂ more easily to tissues
4. Organic compounds
• 2,3-diphosphoglycerate (DPG) reduces O2, affinity of Hb molecules it binds
2,3-DPG is a molecule produced in red blood cells during glycolysis
• Human Hb continuously exposed to 2,3-DPG so constantly modulated by a "normal" DPG level
• 2,3-DPG is increase by chronic hypoxia, anaemia and acclimation to high altitude