FSF Module V (Muscle and Nerve Tissue)
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
Whta is CNS and PNS
CNS- brain, spinal chord
PNS- peripheral nerves, associated ganglia, connections to CNS
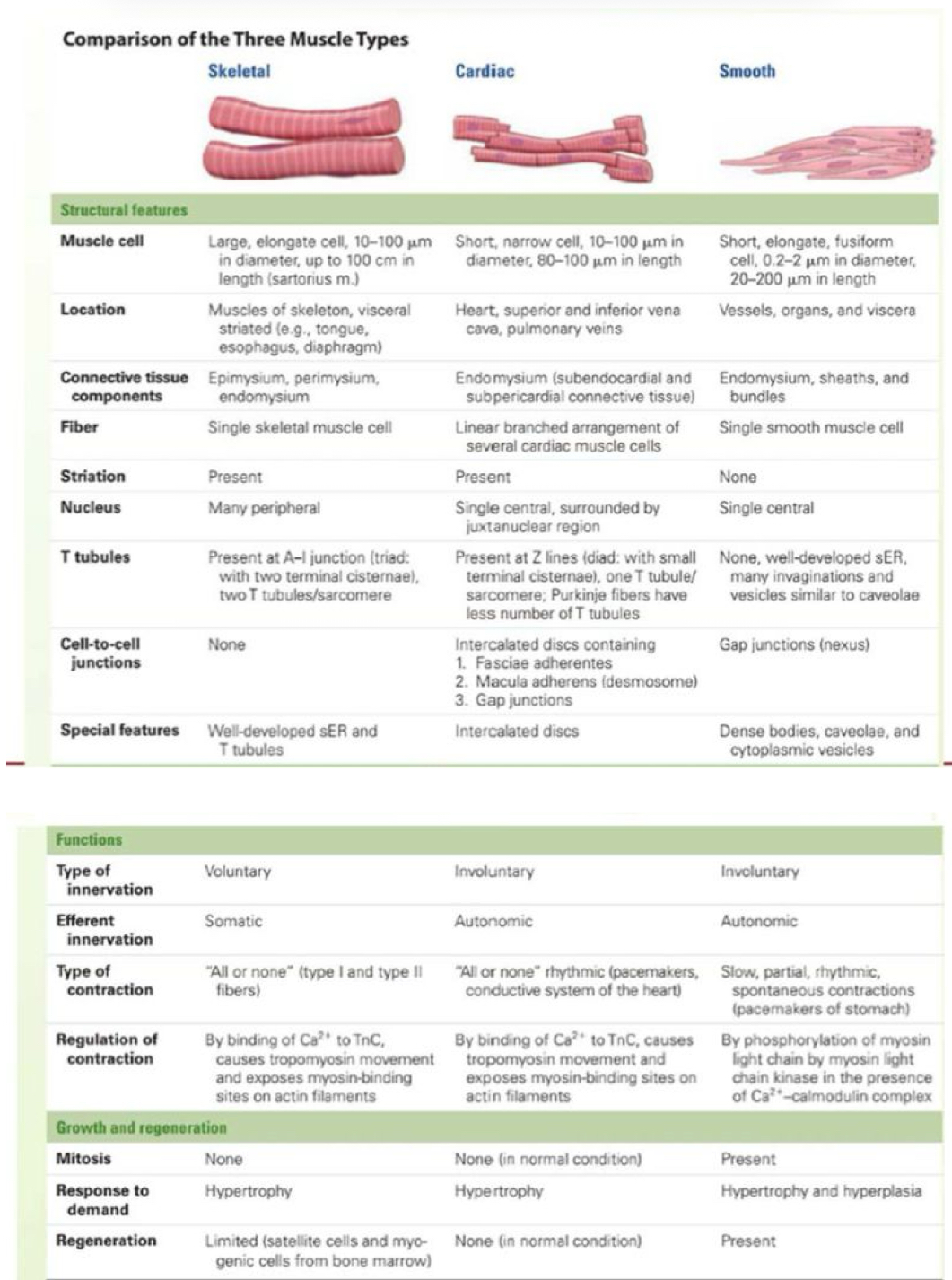
What is th classification fo muscle types?
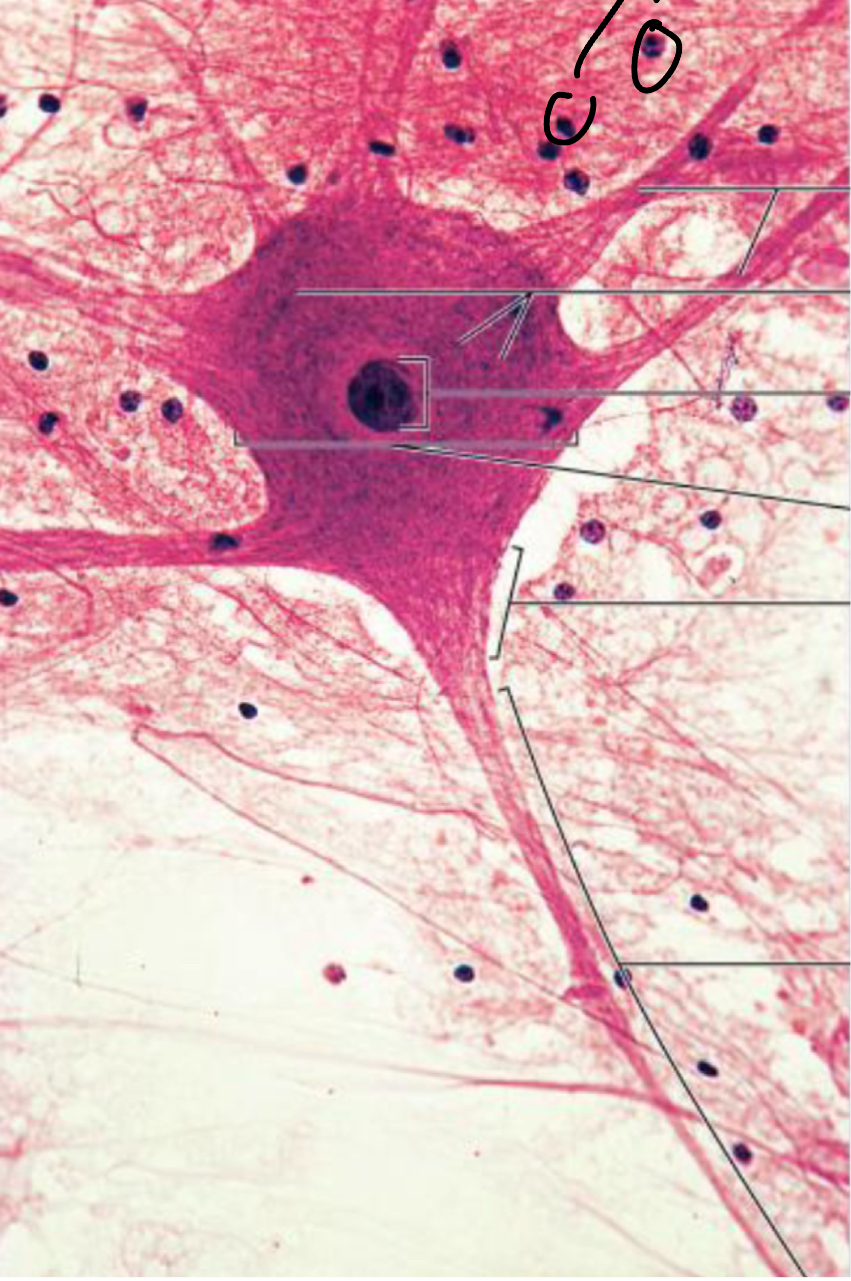
Label this neuron:
What are the two nerve cell types?
Neurons: large, functional unit responsible for electrical impulses
Supporting cells (nueroglia): support, nurture/protect neurons central+peripheral neuroglia
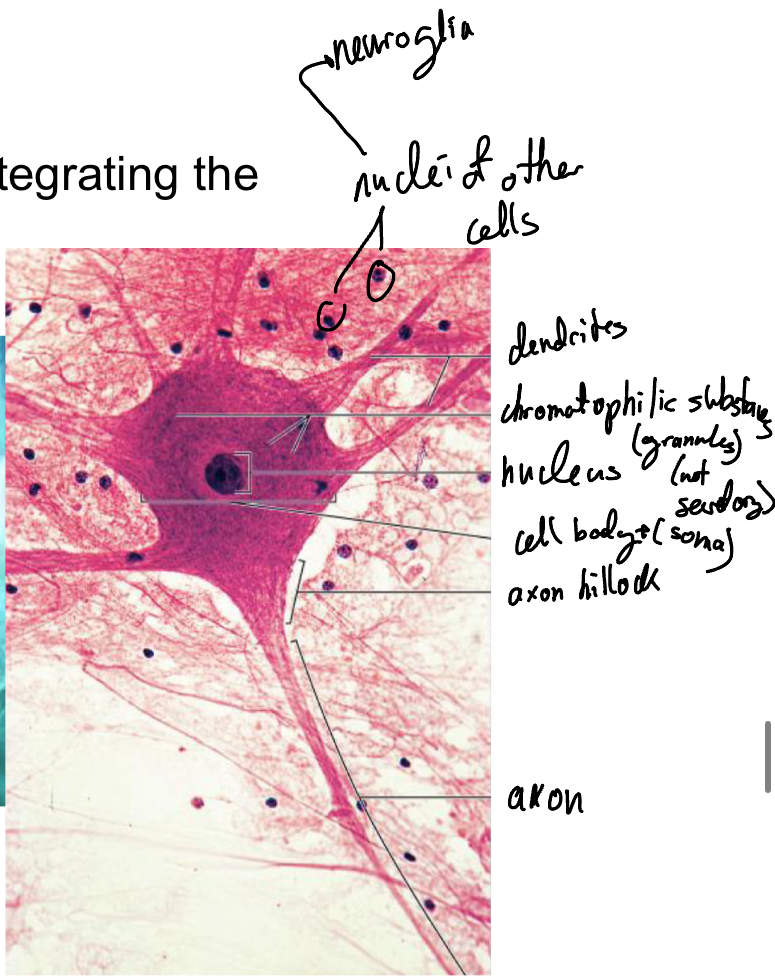
In the top image identify which are the nueroglia and axons (white matter) and which are the nueron nuclei (gray matter) in the spinal chord
The inner (darker region) gray matter (PNS and CNS) of the spinal chord has the neuron nuclei while the white matter (paler) outside contains the neuron axons and nueroglia

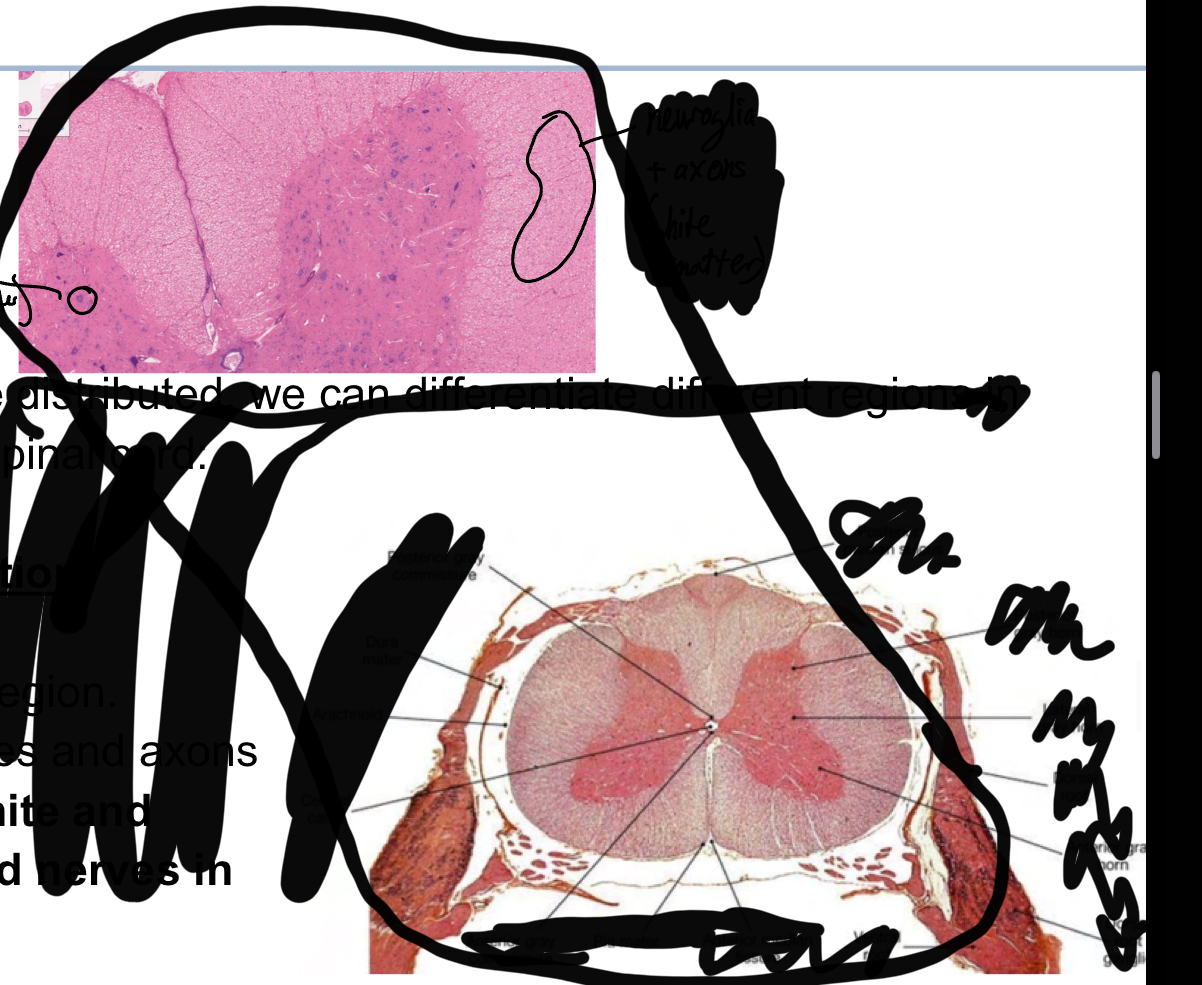
What are th different types of neurons?
Sensory neurons: receive infor and conduct impulses to CNS for processing and analysis
Interneurons: conduct info and connect neurons (specifically sensory to motor and vice versa) (most abundant type we have)
Motor nuerons: transmit info from CNS to motor cells/effector cells to extert response (muscle/glands)
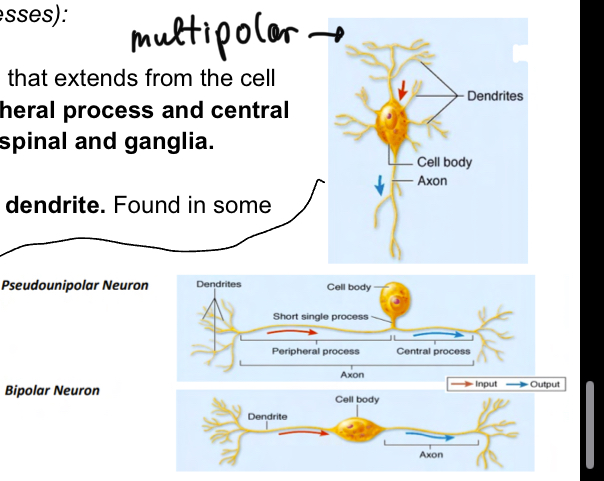
What are the different neurons?
pseudounipolar neurons: single process that extends from cell body branching into peripheral process and central process (not veyr abundant found mainly in spinala dn ganglia)
Bipolar: single axona dn dendrite, not veyr abudant found in sensory organs
Multipolar: usual model of neuronwith many dendrites, single axon, most abundat type.
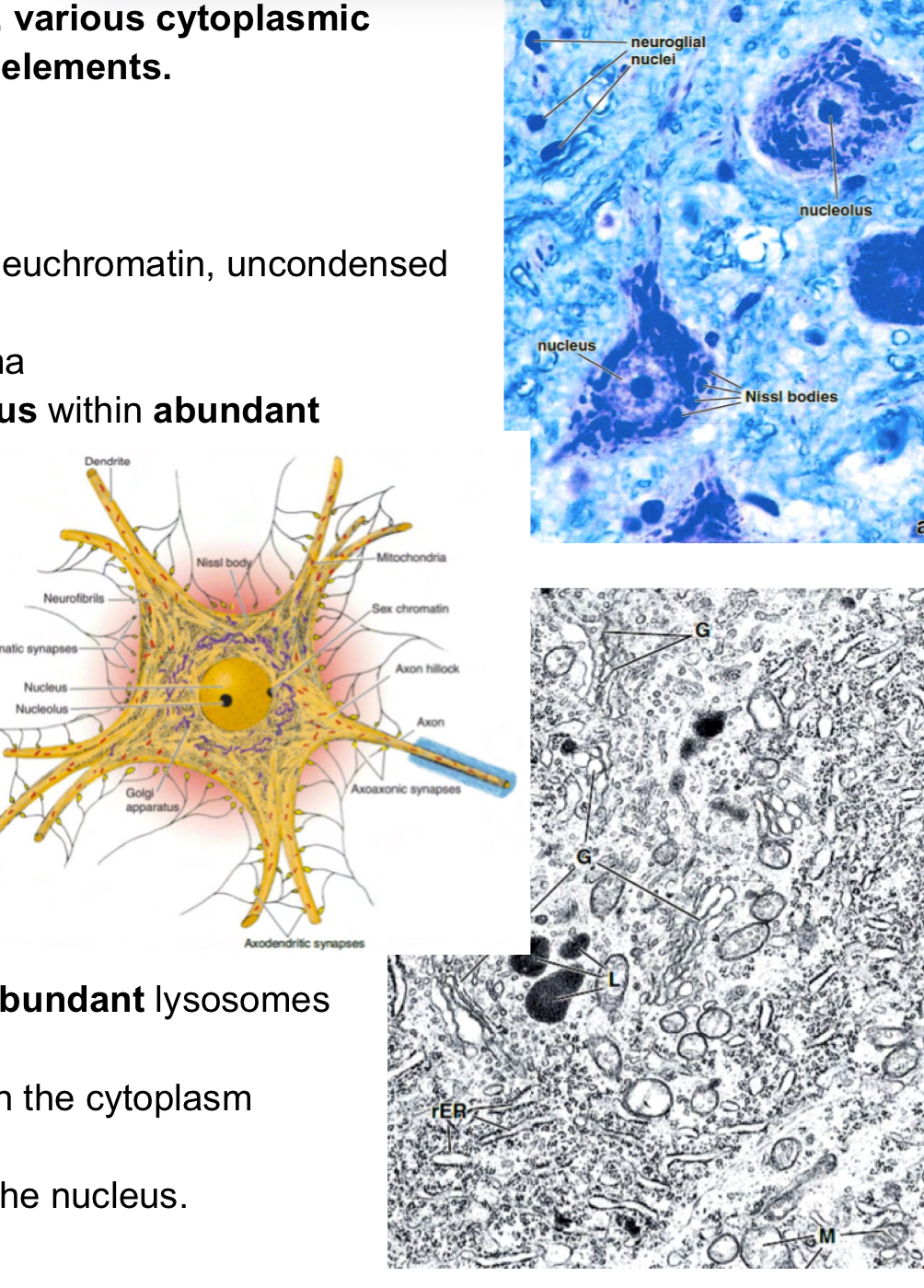
Describe the components of the nueral soma.
Nucleus: has euchromatin (pale uncondense)
Nissl bodies: granular structures with polyribosomes and RER, stain basophilic (purple)
Lysosomes
Mitochodnria
Golgi
Inclusions
Lipofuscin-containing granules: formed by residual bodies of lysosome (incres in number with age)
Lipid droplets (occasionallly present)
Melanin-contsining droplets
Cytoskeleton
nuerofilament (10nm)
Microtubules (24nm)
Microfilaments (6nm)
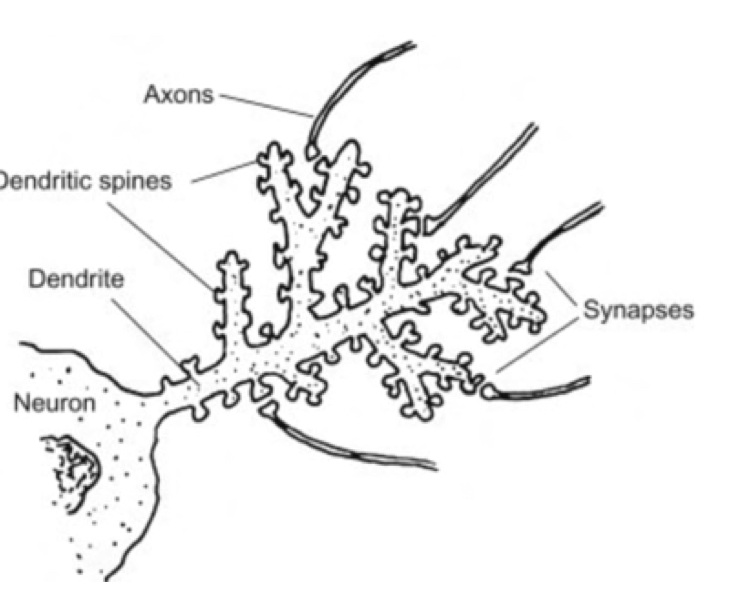
Describe neuronic dendrites
Recieve stimuli from senosry cells, converting them into electrical impulses transmitted to soma (not action potnetials yet). Branches contain different spine swhich increase area availbale for synapse transmission (decrease with poor age+nutrition) ***has many mitochondria
Dscribe axon structure:
Axon hillock, no nissl bodies, lots of microtubules and nuerofilaments wth mitochondria and vesicles (here elctrical pulse generated)
Axon, has surroudning plasmam membrane( axolemma), cytoplasm alled axoplasm, no RER or golgi, lots of cytoselton and SER and elongated mitochondria. Protected in generalby glial cels because it is thin and more fragile+ can be up to 1m long
Axona transport systems
anterograde trasnport: cell bodyto axon terminals, regenration of vesicles and proteins, MAPs like kinesin play important role in this
Retrograde transport: axon terminal to body, recycling r materials, Dyenin plays important role in this.
Recognize neurons under microscope:

What are Astrocytes with reference to neurons?
Largest of neurglial cells
Blood brain barrier: Surround blood vessel thru extended pedicles (vascular feet) reinforcing the blood-brain barrier to regulate exchange +passage from blood to brain stoma. Formed by tight junctions between adjacent endothelial cells, astrocytes reinforce these junctions by connecting trhu anchoring junctions
Surround neurons, taking ions after having compelted their function+suplying energy fr metabolism
In contat w/ meninges (pia mater), protective barrier between pia mater and nervous tissue
In brain, astrocytes form scar tissue (glial scar) after injury to CNS
Can be protoplasmic:
gray matter, short processes, intermediate filaments, mainly form blood brain barrier
Fibrous:
white matter, long slder processes, many intermediate filaments

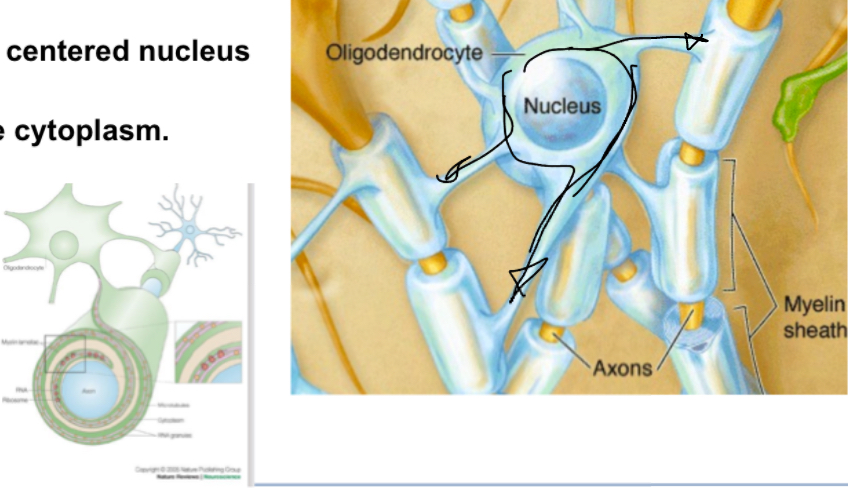
What are oligodendrocytes with reference to nuerons?
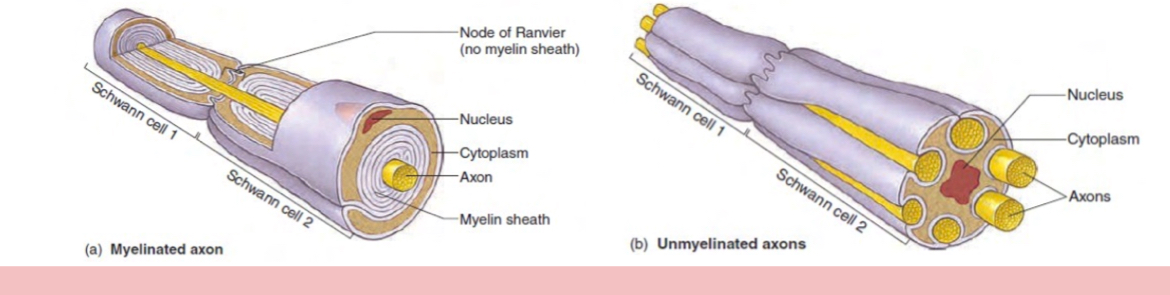
Protect axons of neurons found in white and gray matter, have small condense nucleus and short process… surround axon and create concentric layers of myelin, aiding in eletrical trnamission speeds, each oligodendrocyte can myelinate several axons at once.
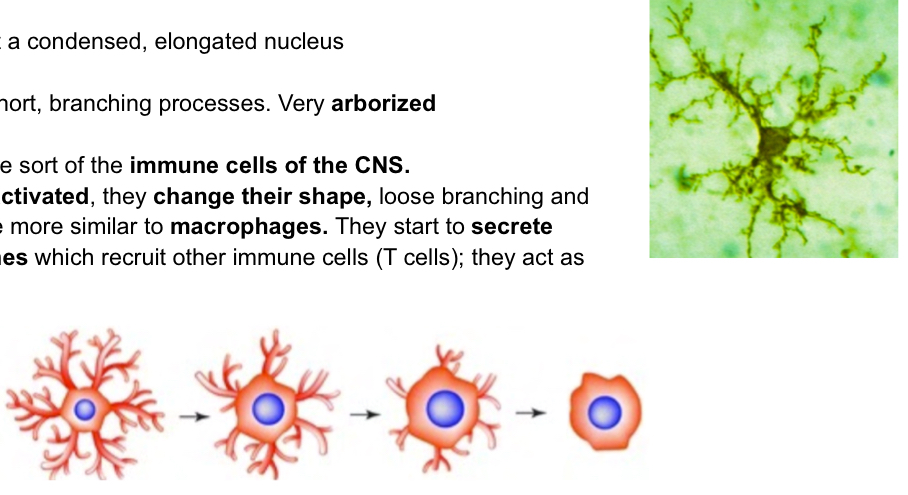
What are microglial cells with reference to neurons
Similar to astocyte sudner microscoep, phagocytic cells. Arborized, immune cells of CNS.. when activated they change shape, becoming liek macrophages and secreting cytokines to recruit other immune T cells (act as APCs (antigen presenting cells)
What are ependymal cells with reference to neurons
Derived form nueroepithelium, line nueral tube and brain ventricles, some contain cilia (move cerebrospinal fluid), some contribute to formation of choroids plexus (tissue that lines ventricles of brain in innermost meninges (pia mater)
What are Schawnn cells with reference to nuerons
Similar to oligodendrocytes, protecting and isolating neurons but doing so in the PNS. Oligodendrocytes are flat cells (with basement membrane), few mitochondria and small golgi region.. form myelinated covers and unmyelinated covers (schawnn cells just surround axons)-single schwann cell can only insulte a single axon
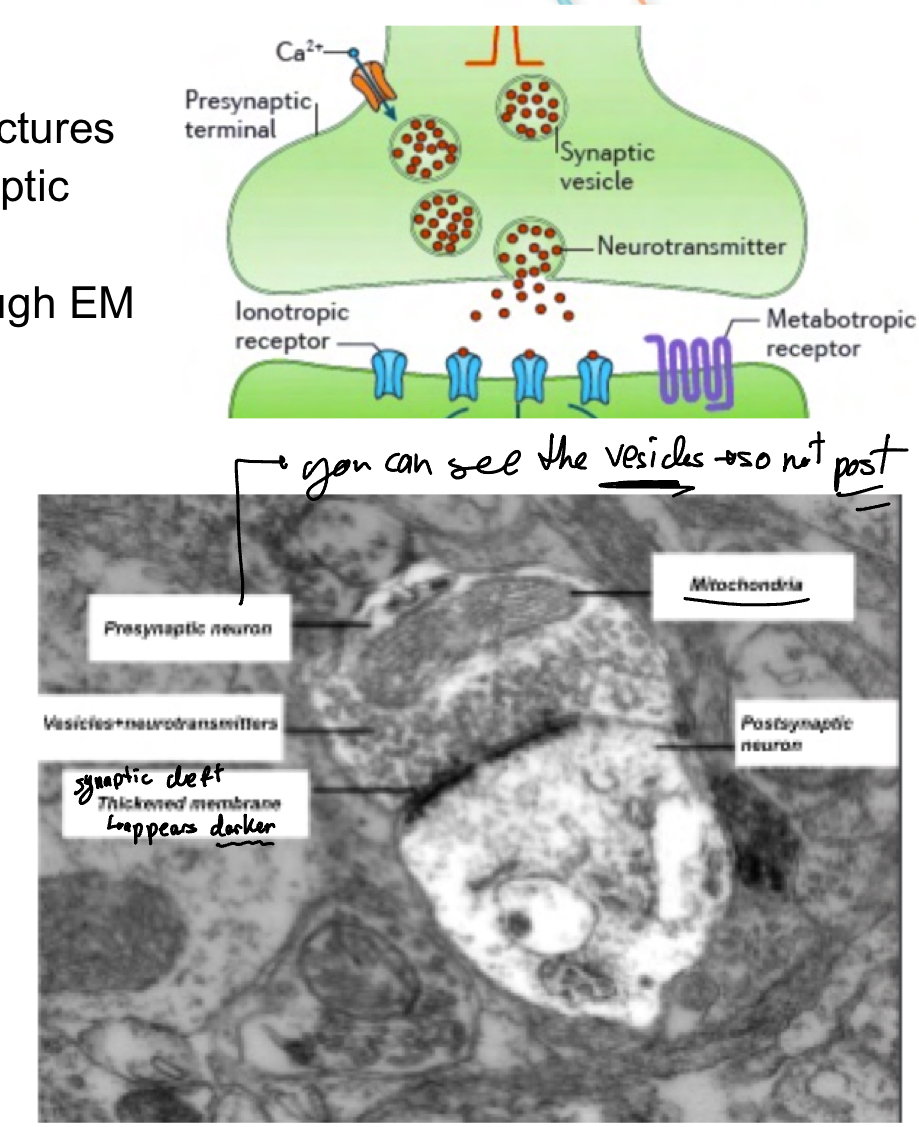
What are the three types of synapses?
Axodendritic synapses: axon dendrite
Axosomatic: axon soma
Axoaxonic: between 2 axons (much less common)
Electrical synapses can be bidirectional (faster)while electrical are more common and unidirectional
This is synaptic cleft under microscope:
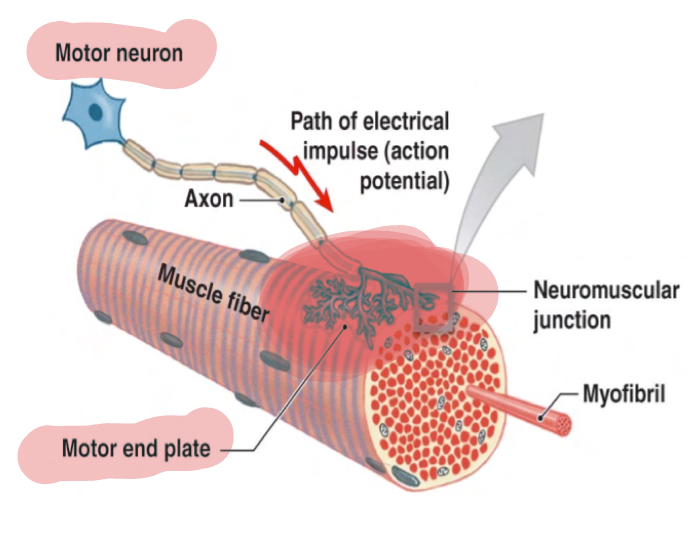
What is a neuromuscular junction?
A type of synapse in which an axon innervates muscle (called motor unit), with the motor end plate connected to the muscle which is where the different synapses take place, we can see that they branch into sveveral axon terminals. The motor end plates in the postsynaptic membrane have junctional folds which are deep invaginations of the muscle of ell plasma membrane (sarcolemma) whihc increase surface area for the neruotransmitter (ACh) to interact
How does myelin sheath get formed?

Keep this image in mind and know how to identify:
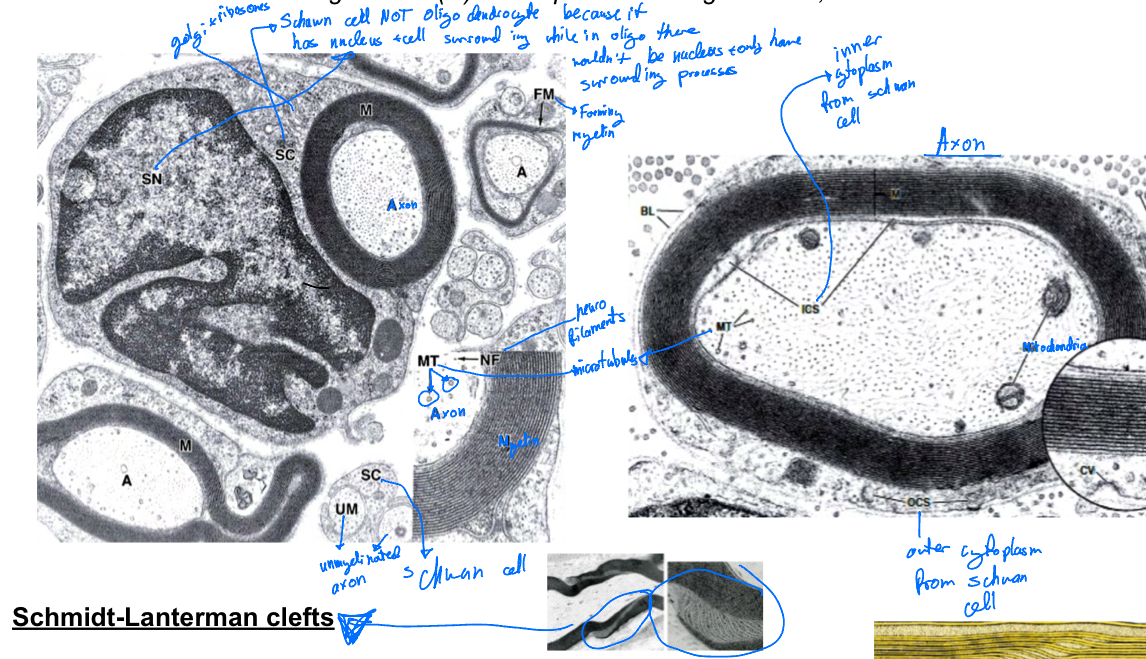
What are Schmidt-Lanterman clefts?
Incisions in myelin know as shcmidt-lantermn clefts that allow for communication between innner and outer cytoplasm to take place.
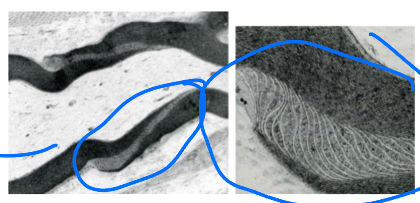
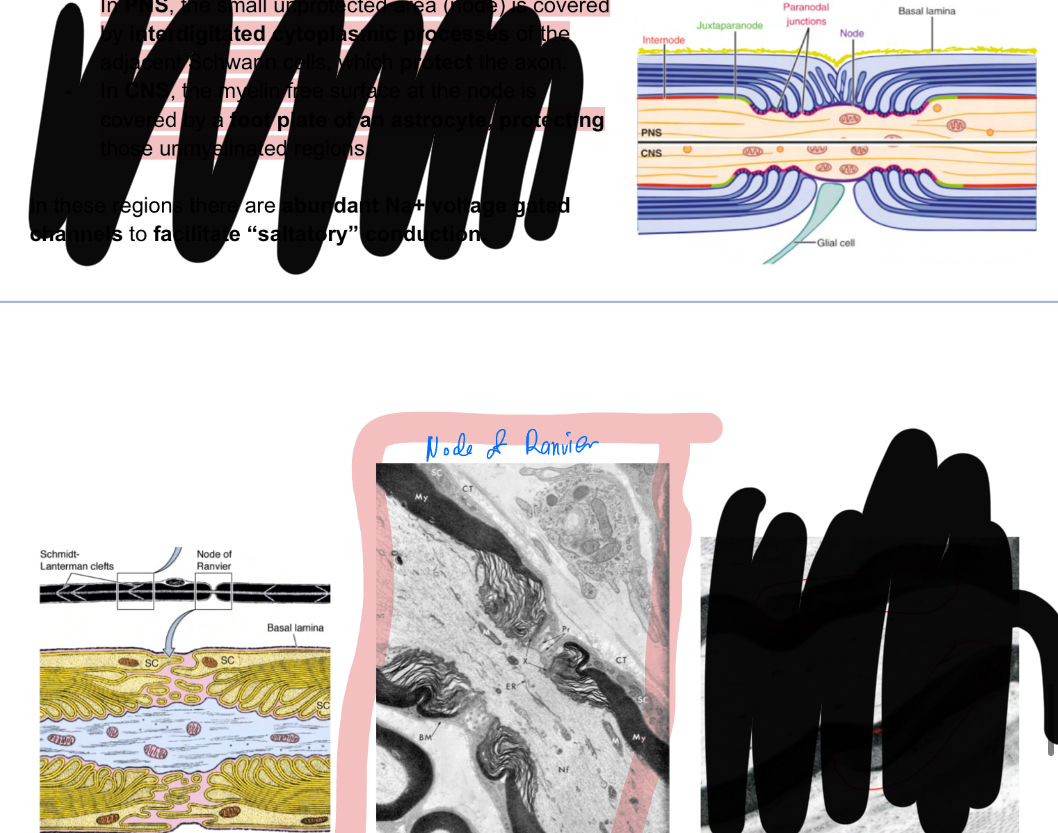
Whata re the nodes of ranvier?
In PNS: node is covered by interdigitated cytoplasmic processes of adjacent schawnn cells protecting axon
In CNS: myelin free surface covered by a foot plate of astrocytes, protecting unmyealinated regions.
Internodes is the space between node of ranvier
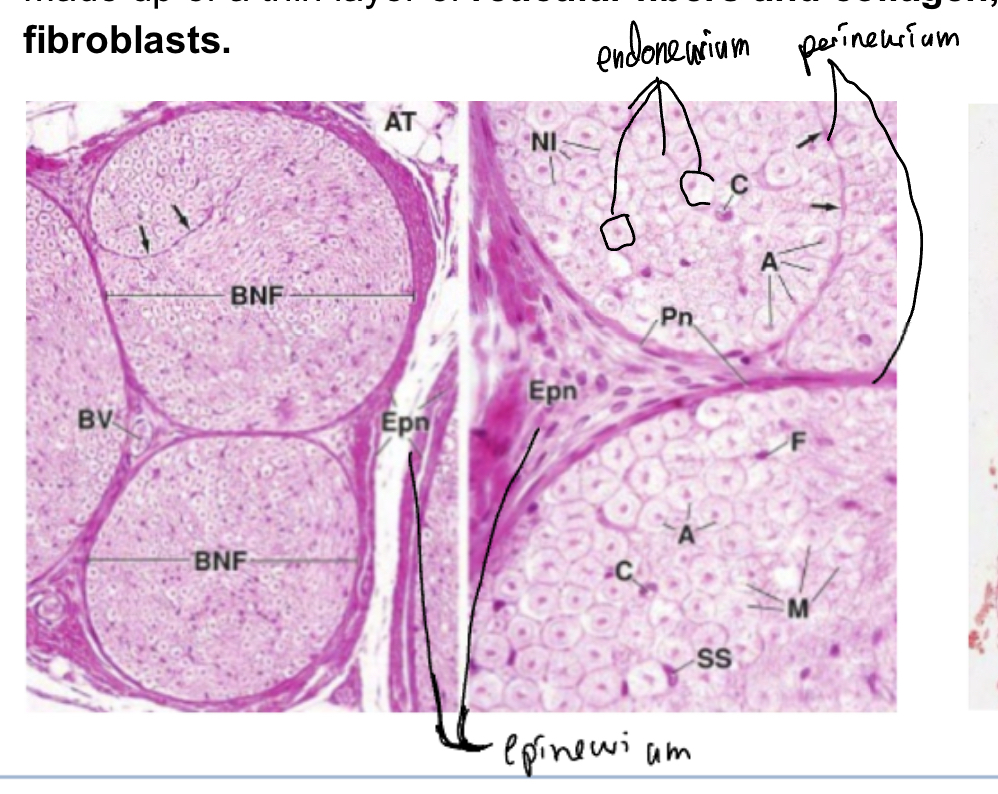
Explain structure of the nerves
They are cordlike bundles made of nerve fibers surrounded by connective tissues, seen in microscopy as white is myelin surrounding the nerves. Conatins the following:
Epinerium: Outermost, consisting of dense fibrous connective tissues, often embedded in adipose tissue
Perinerium: surroduns each bundle of nerve fibers, made up of speacialized connective tissues which block+regulate trhu tight junctions (form blood-nerve barier)
Endoneurium: surrunds each individual nerve fiber, made of reticular fibers and collagen, containign some fibroblasts.
The nerves are axons+supporting cells and the gnaglia is the neuronal bodies
In the spinal cord and cerebellum where is the white or grey matter?
What are ganglia?
Encapsulated aggregations of neuronal cell bdies (soma) outside the CNS+ abundant small glial cells (satellite cells) surroudning them
The nerves are axons+supporting cells and the gnaglia is the neuronal bodies

What are the meninges?
Membranous coverings of brain and spinal cord, formed by connective tissue, protecting inner nerve tissue. 3 layres
Dura Mater: outermost, lines bony skull and close to vertebrae
Arachnoid Mater: intermediate, abutting the dura
Pia Mater: innermost, high vascular, directly on brain surfaceand spinal cord.
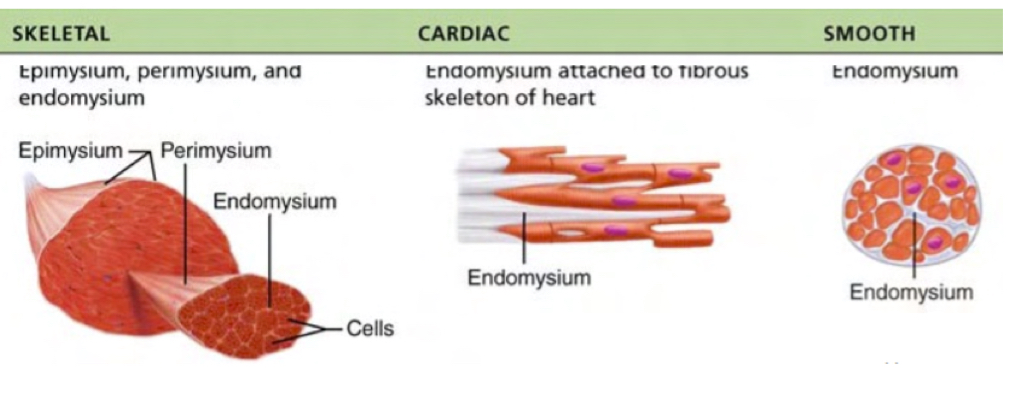
Explain the organization of connective tissue in muscles
Epimysium: surrounds entire muscle and forms a connecion between skelatl muscle and other muscles and tendons, which also connect to bones,.
Perimysium: connective tissue around each muscle bundle
Endomysium: surrounds each individual muscle cell
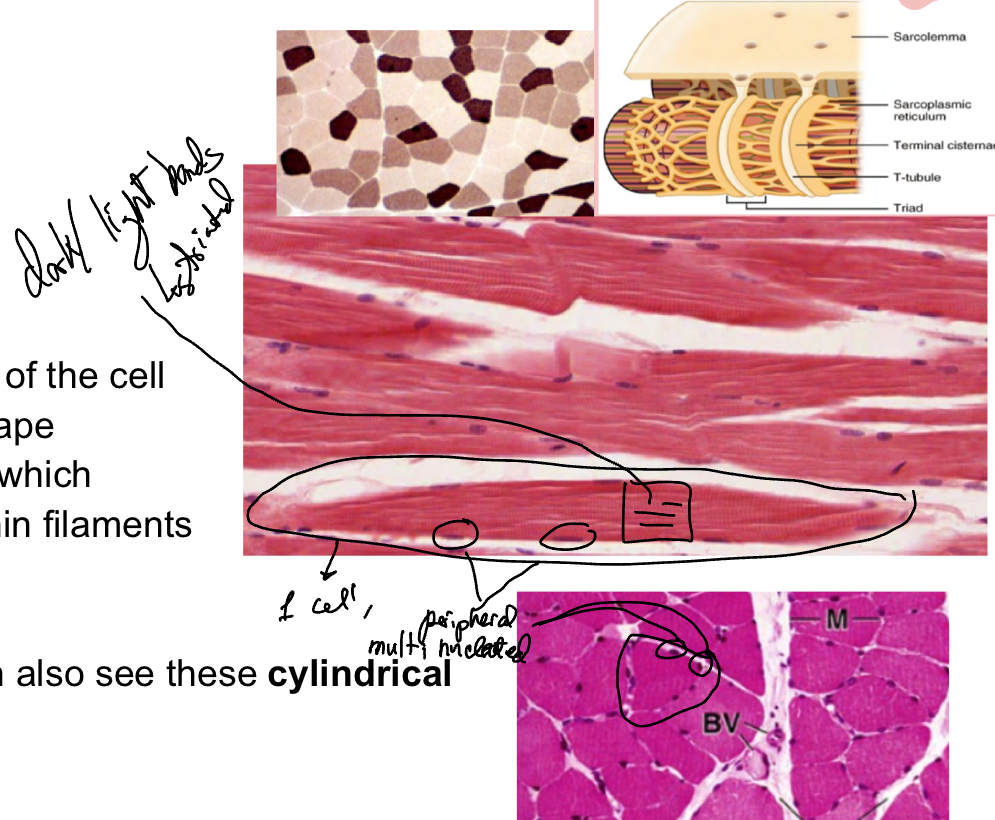
Label these images of skeletal muscle.. and what are skeletal muscle cell characteristics?
multinucleated, on periphery
Long large cells
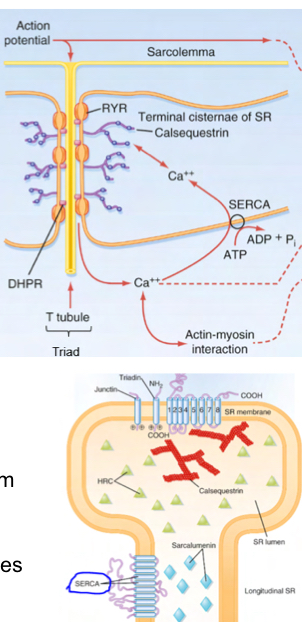
Basement membrane known as sarcolemma, forms deep invagination known as T-tubules. T-tubules together with terminal cisternae (end of sarcoplasmic reticulum) to form triads. Cytoplasm known as sarcoplasm.
Striations which corresponds to myofibrils and thin filaments
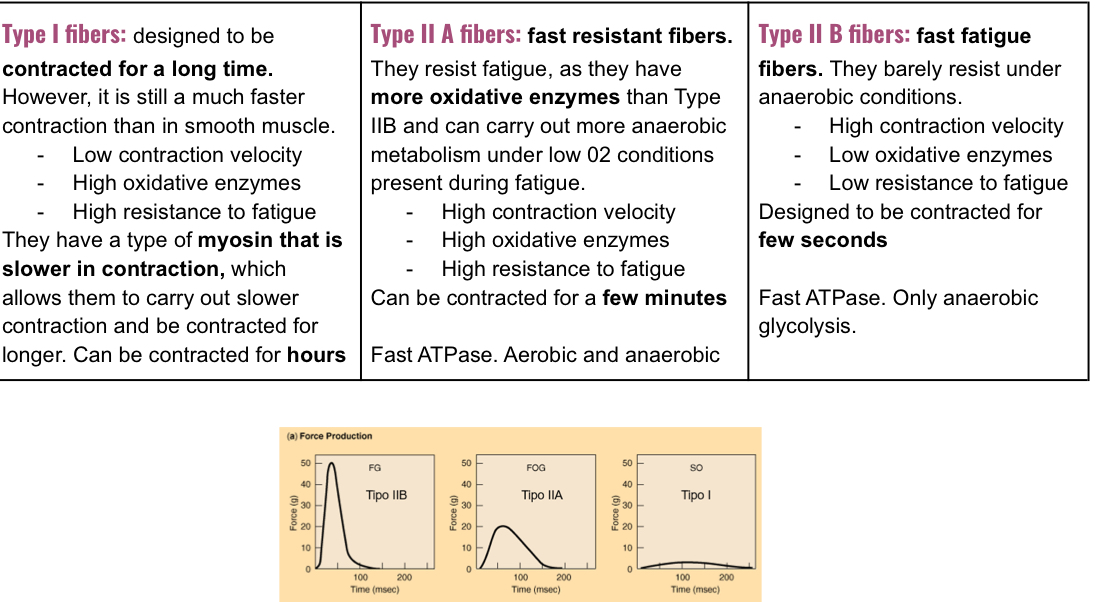
3 different cell types ahve different metabolic compnents, shown by differences in staining:
Red fibers type I: abudnant in myogobin, slow contraction, abundant mitochondria, strong oxidative capcity, more vascularized, thinner less fibers
White fibers (type Ilb): fast contraction but fatigue easily, low myogobin, few mitochondria, fast anaerobic glycolysis metabolism, larger and more myofibrils, less vascularized,
Intermediate fibers (type Ila)
What are the different skeletal muscle type fibers?
You can change between type B to A during resistance training but not between types I and II
When you do force training, you generate more myofibrils in parallel, the dimaete of the muscle fibers increases, having more force but not as much velocity.
How to myofibril growths in skeletal muscle affect strength and velocity?
growth in parallel increases strength
Growth in length increases velocity
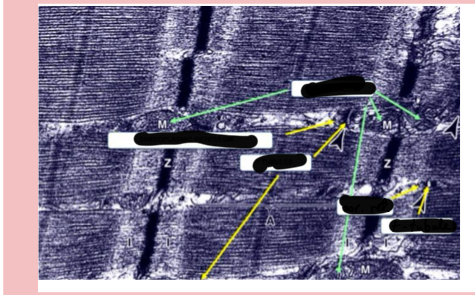
Identify strcutures in the image
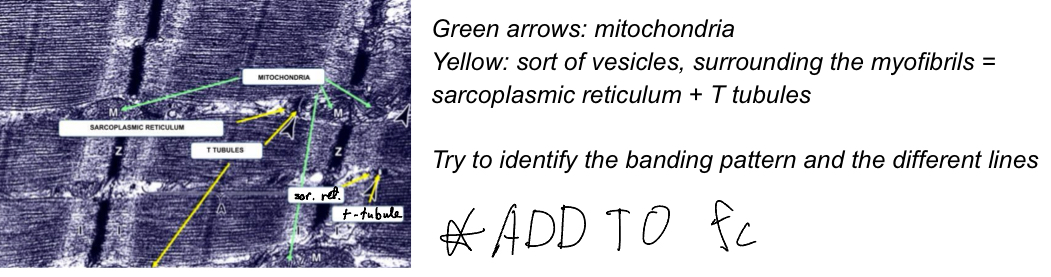
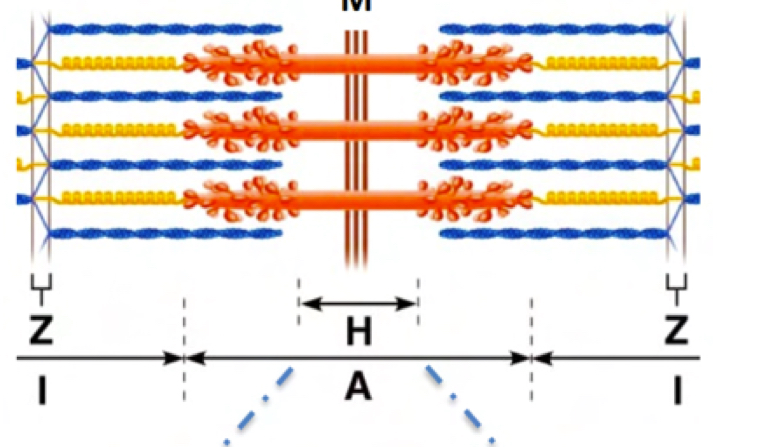
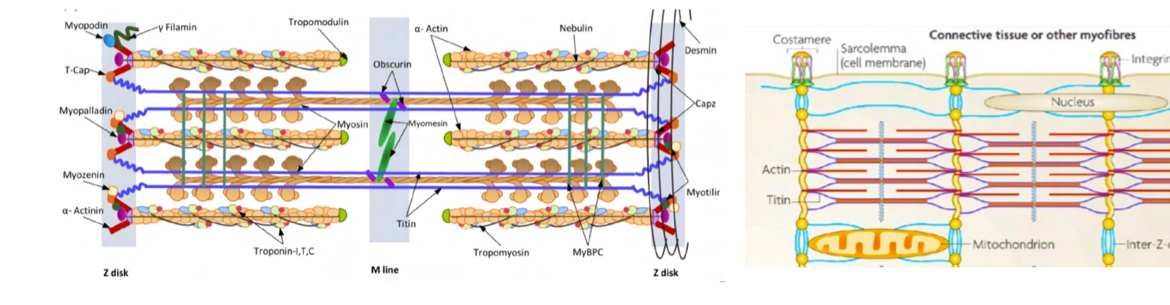
Explain sarcomere structure
Components:
Myosin akes up the thick fillaments in the center
Actin makes up thin filaments attached to Z lines (made up of alpha actinin)
Tropomyosin is on the actin binding sites
Tropnin binds to calcium and reveals active sites of actin (TnT binds troponin complex to tropomyosin, TnI binds to actin and troponin T, TnC binds calcium)
Desmin located at Z disc, binds Z disc to plasma membrane tro transmit contraction of th cell.
Dystrophin: binds actin to cel membrane
Tropomodulin and nebulin are other proteins that help stabilization
M line proteins (myomesin, M-protein, obscurin)
Protein C
Titin: stabilization of thick filaments
Bands:
A band: thin and thick filaments overlap, seen as a dark band. (Actin and myosin)
I band: only thin filaments (actin), seen as light
Z disc:
H bands:inmiddle of A band, bare region of thick filaments, only myosin tails (seen as light)
M lines: dark lines in middle of H zone, corresponding to croos sections between thick filaments
Label this diagram of the sarcomere:
Describe skeletal muscle regeneration
Progenitor cells- satellite cells repair muscle cells int he case of muscle degradation, they become activated under the influence of myogenic regulatory factors and become myoblasts finally differentiating into mature muscle cells.
What are DHP and RYR and SERCA proteins
Allows Ca2+ transmisison
4 DHPR molecules on T tubule changes confromation upon stimulation and act on one RYR, which opens by changing conformation to allow Ca2+ release from cells.
SERCA ats as a calcium pump to pump Ca2+ into the reticulum.
THIS COUPLING ONLY OCCURS IN SKELETAL MUSCLE
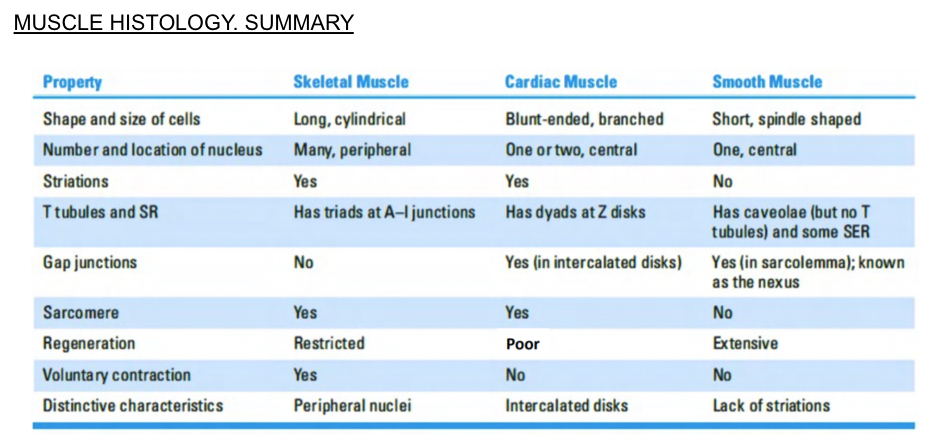
Describe cardiac muscle features
Striated
Self excitatory
Electrically coupled
Nuclei centrally located, multinucleated
Intercalated discs separate the cells and are seen as darker lines.
Striations are more difficult to see (weaker)
Have darker fibrolasts in endomesyum
Abudant mitochondria
Have diads instead of triads- sarcoplasmic reitculum and t tubules at z lines
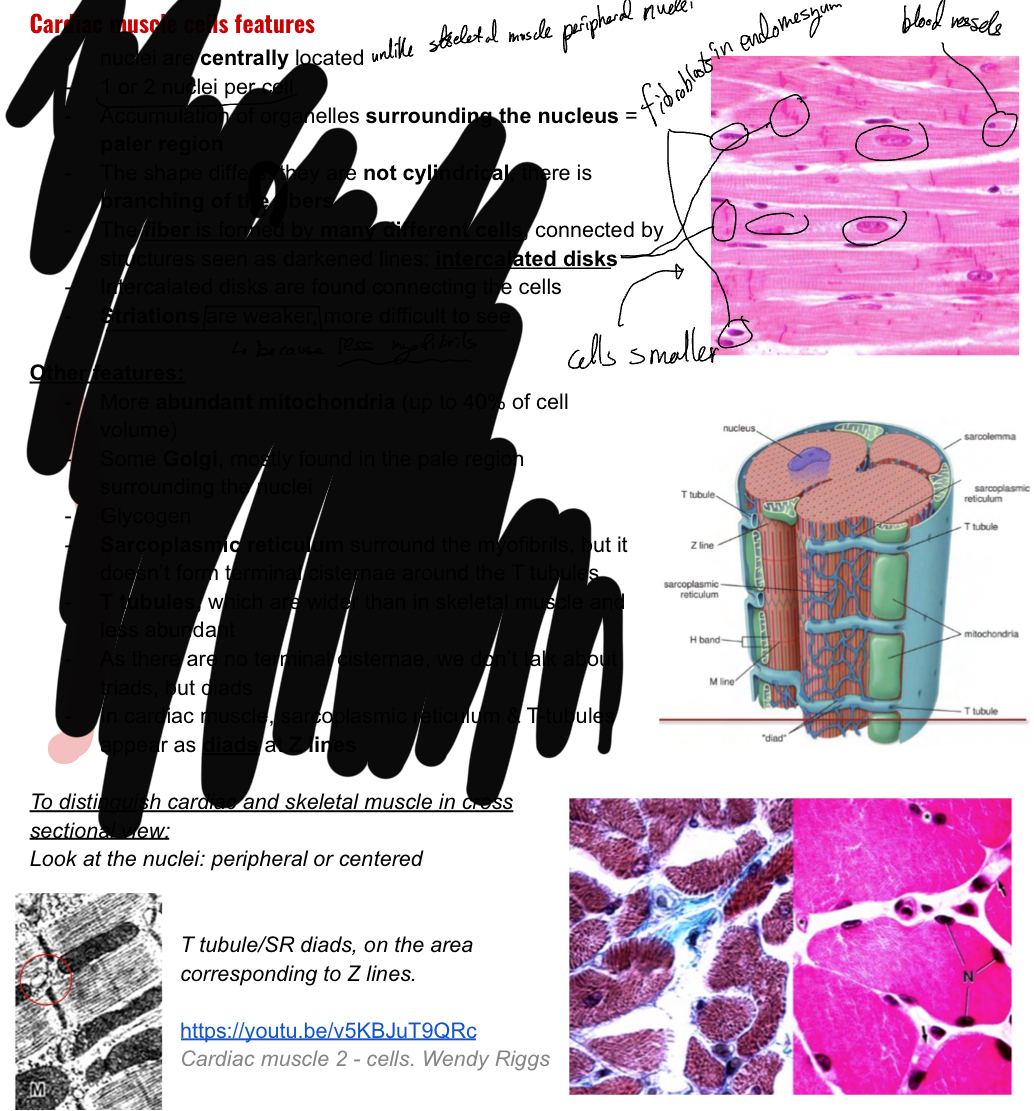
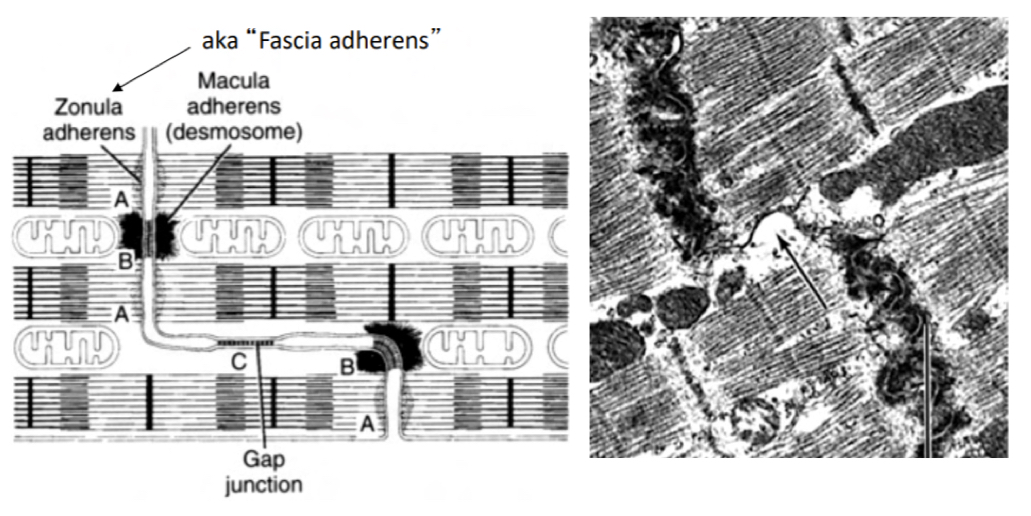
What are cardiac muscle intercalated discs?
They are interidgitated cytoplasmic expansions responsibe for mechanically and electrically coupling heart cells, they are aligned with Z discs, runing transversally (have zonula adehrens and desmosomes- mechanical coupling) and laterally (gap juntcion that transmit electrical signals thru ion transport- electrical coupling)
How is cardiac muscle contraction? In comparison to skeletal muscle?
same.. dependant on Ca2+
Different.. contraction starts thru purkinje fibers and cardiac myocytes- transmitted to mucsle cell thru GAP junctions via electrical coupling (ion trnasport)… calcium enters cell trhu t tubule, tansported to cytoplasm and triggers release of intracellular calcium from SER.
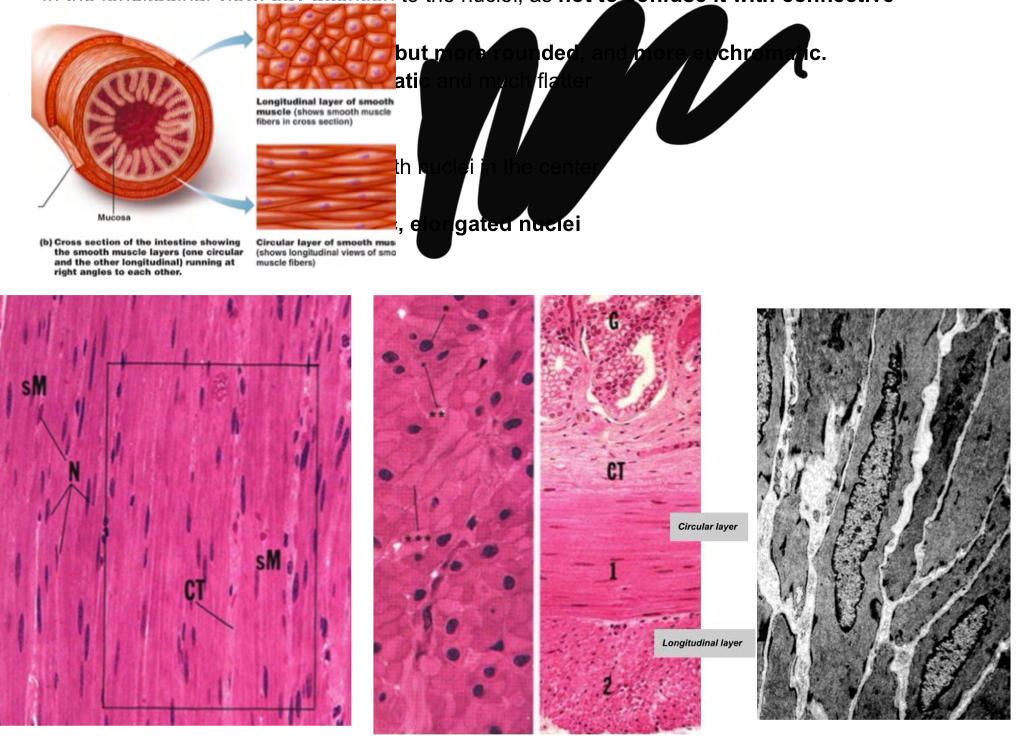
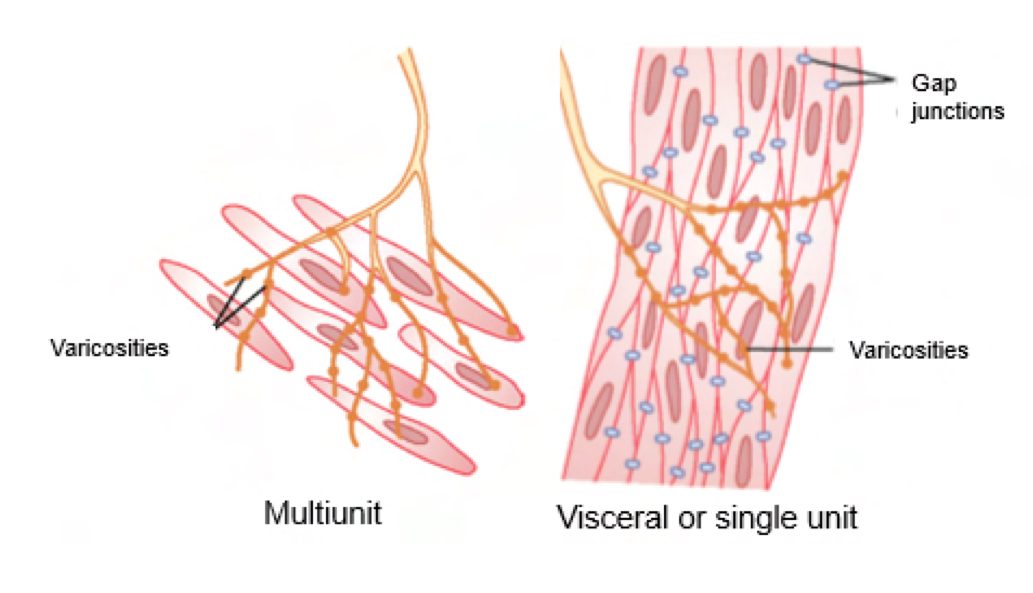
What are smooth muscle chracteristics?
no striations (fusiform)
Each fiber formed by a single cell kkept together by connective tissue and connect thru GAP junctions OR single individual cells innervated each by a separate nerve fiber
surrounded by a basal membrane like endomysium
No t tubules or sarcoplasmic reitculum, insted have pinocytic caveolae and SER in periphery
For non voluntary contraction
modulated by innervation and chemical stimuli,
Slower contraction than skeletal muscle
Organization:
Elongated central nuclei-not to be confsd with those f connective tissue or more heterochromatic and flatter fibroblasts— smooth muscle cells are more euchromatic
Circular layer than runs tranvesally and around and a longitudinal layer that runs along the tube
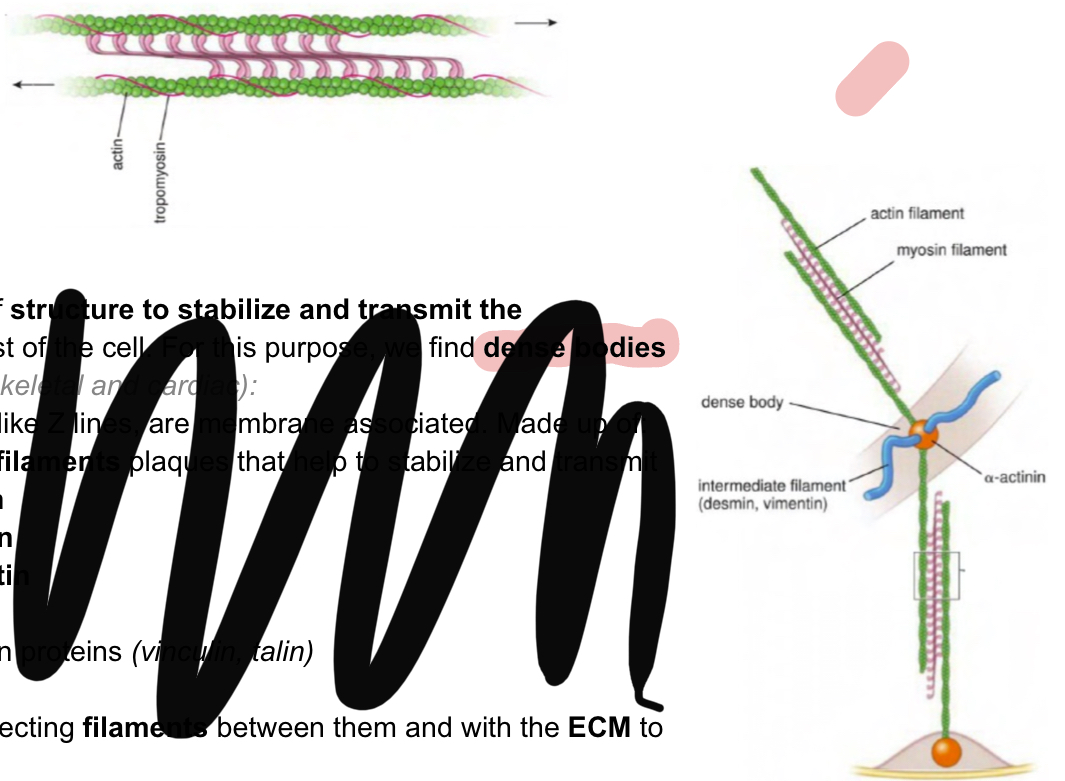
Instead of sarcomeres what can be found in smooth muscle?
contractile fiber
Thin filaments:
actin
Tropomyosin
Caldesmon and calponin (actin binding porteins instead of troponin)
Thick filaments:
smooth musle myosin (no need for troponin to cover active sites since it has low actin affinity)
Side polar orientation— no H zone of central line (look at image)
Dense bodies are membrane associated and act as sort of Z lines to transmit the contraction to the rest of the cell.
Intermediate filaments to stabalize and transmit: Desmin +Vimetin
Alpha actinin
Other adhesion proteins
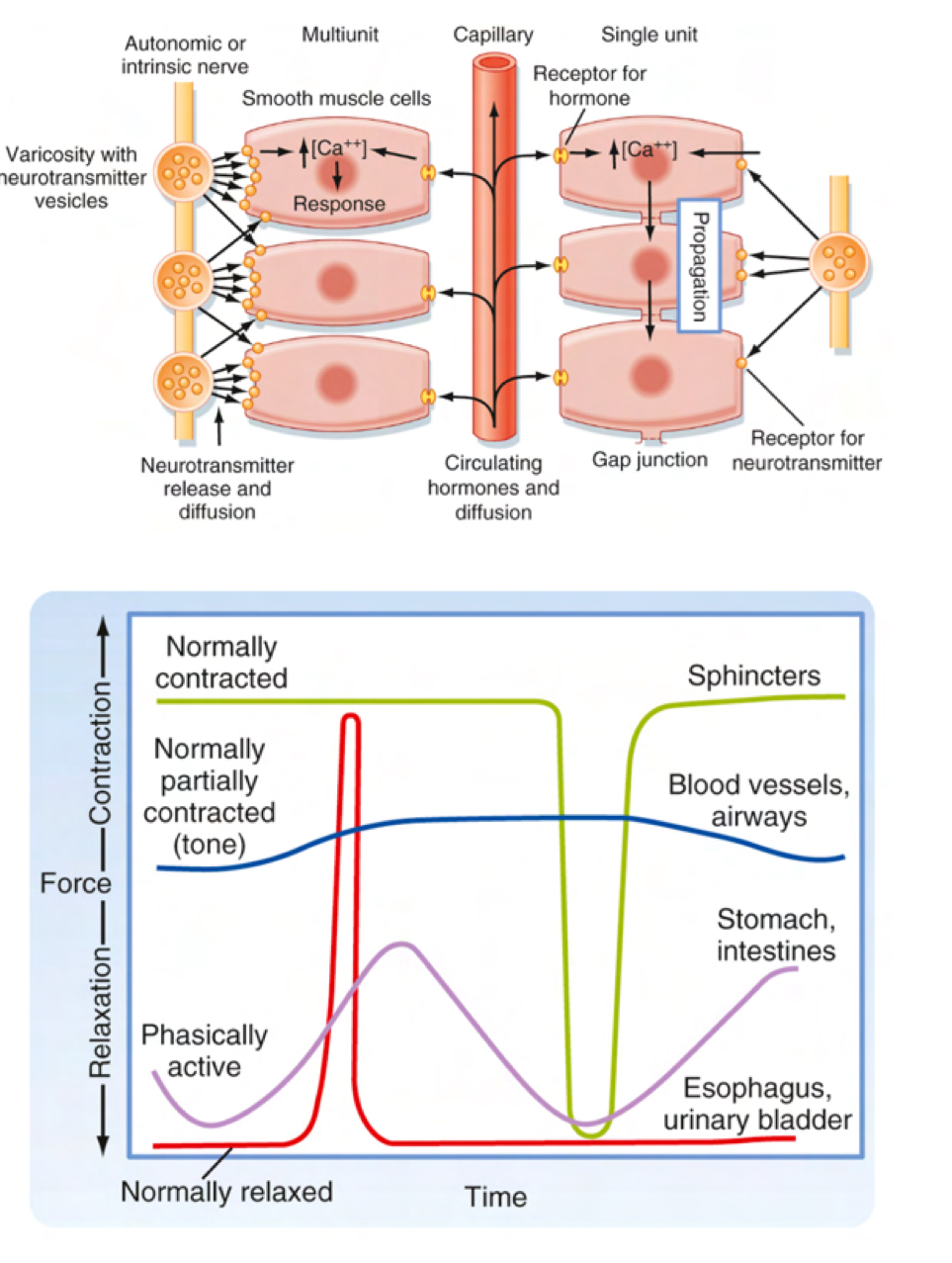
Describe smooth muscle contraction
also Ca2+ dependent
Slower than skeletal muscle contraction no motor end plate, innervation occurs at a distance, therefore instead of synapse regions there are varicosities
Two types of innervation:
Visceral: very few nerve endings, connected thru gap junctions-electrically coupled-rythmic contraction
Multiunti contraction: few gap junctions, every cell individually innervated-more rapid/precise control contractions.
What is the coupling mechanism in smooth muscle cells?
calcium activates an MLCK (myosin light chain kinase), whihc phsophrylates the light chain of myosin- increasinf the affinity of myosin for actin—casues contraction
Since in smooth muscle the binding site is always exposed, the continouos phosphorylation of myosin causes the myosin to bidn to the actin and contract
At the same time there is. Posphatase dephosphorylating myosin to remove its affinity

How does msooth muscle relax?

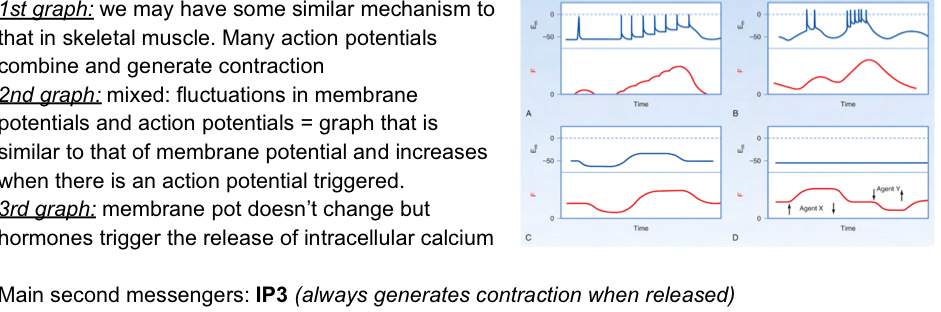
Explain the different patterns of smooth muscle contraction
Because the smooht mscle has so many different mechanism by which to contract, the different mechanism causes different pattenrs
How are long lasting contractions created in smooth muscles?
Neessary for long periods of time— like sphincter (23hrs a day)
since we can control intracellular calcium levels, we can sustain contraction for a long time by keeping intermediate levels of calcium to increase some of the portions of myosin’s affinity for actin
An initial high peak is necessary but after thisit can eb maintained at interediate levels, meaning it does things slower but with alow level of contraction and no excessive energy consumption.

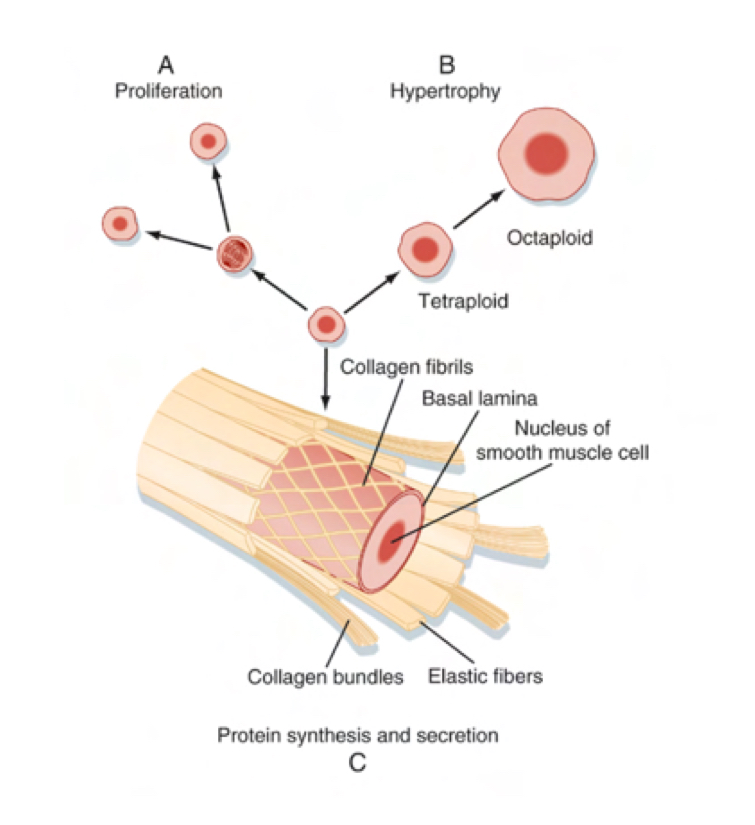
How do the three diff. Muscle types regenrate and growth?
Skeletal:
Increases in size by depostiing collagen (called hypertrophy)
Regenrate thru satellite cells as muscle cell themsleves cannot divide
Restricted
Smooth:
hypertrophy
Cells can divide and proliferate
Mesenchymal cells that differentiate into them (vascular pericytes)
Extensive
Cardiac muscle:
hypertrophy
Circulating progenitor cells that differentiate into them and resident stem cells
Poor
Muscle types summary:
What’s the difference between chemica and eletrical synapses?
Chemical: (in uman body most are like this so we mostly talk abt this)
some delay
NEurotransmitters to excite or inhibit
Unidirectional
Large synaptic cleft
Not necessarly linked to ion channels
Electrical
no delay
Ions
Noinfo changes
Bidirectional
Open chhanel between cells
Minimal intercellular space
Describe the neuromuscular synapse:
Presynaptic bouton:
Sodium potassium volateg gated channels for action potential transmission
Calcium voltage gated channels for muscle contraction— accumulaed calcium exits thru an Na/Ca countertransport pump, one calcium leaves while three Na enter— uses ATP
Neurotransmitter vesicles(ach)
Synaptic cleft
neurotransmitters diffuse trhu cleft an reach postsynaptic muscle fiber
Ach esterase in the cleft breaks down Acetyl choline in the cleft
End plate
hyperdense folds increase surface area, where Ach receptors are located
These nicotinic receptors and ligand-agted and open when two Ach moelcules bind— trigger Na+ influx an local depolarization leading to Na+ volatge gated channels opening- propagate actino ptential
No potassium volatge gated channels as safety mechanism— need a lot of Ach to transmit depolarisation
Sarcollema
specialized membrane surrounding striated muscle fiber with invaginations (more surface area)
Here at teh end plate, no sodium volatge gated channels, hence it propgates electronically not chemically, therefore the amplitude decrease and action potentia will beingin neraby area where those channels can be found (must be -60mV for action potential to take place)
How is Ach stored in vesicles? And releaseD?
Proton pump (ATPase) to maintain low pH, simultaenouesly there is an Ach/proton counter transport- so Ach enters
Vesicle fusion with memebrane and Ach release is mediated by SNARE proteins (Solule NSF attachment Protein receptors).
calcium contacts with synaptotagmin
Synaptobrevin in neurol membrane conacts other proteins which will contact and push vesicles to membrane, causing them to fuse
Also works w/ lysosomes-membrane fusions
Can works in two ways:
Classical: fully integrated due to clathrin
Kiss and Run: no full fusion, release thru fusion pore.

Explain the two main types of postsynaptic receptors
Ionitropic receptors: direct effect, membrane bound that respond to ligand binding by opeening ion channel
Metabotropic receptors: indirect effect, neurotransmitter binds to G-couple receptors, cause secondary messengers to effect— to open ion channels (in same or other parts- unlike ionitropic receptors which is only local) and/ protein synthesis, transciption etc
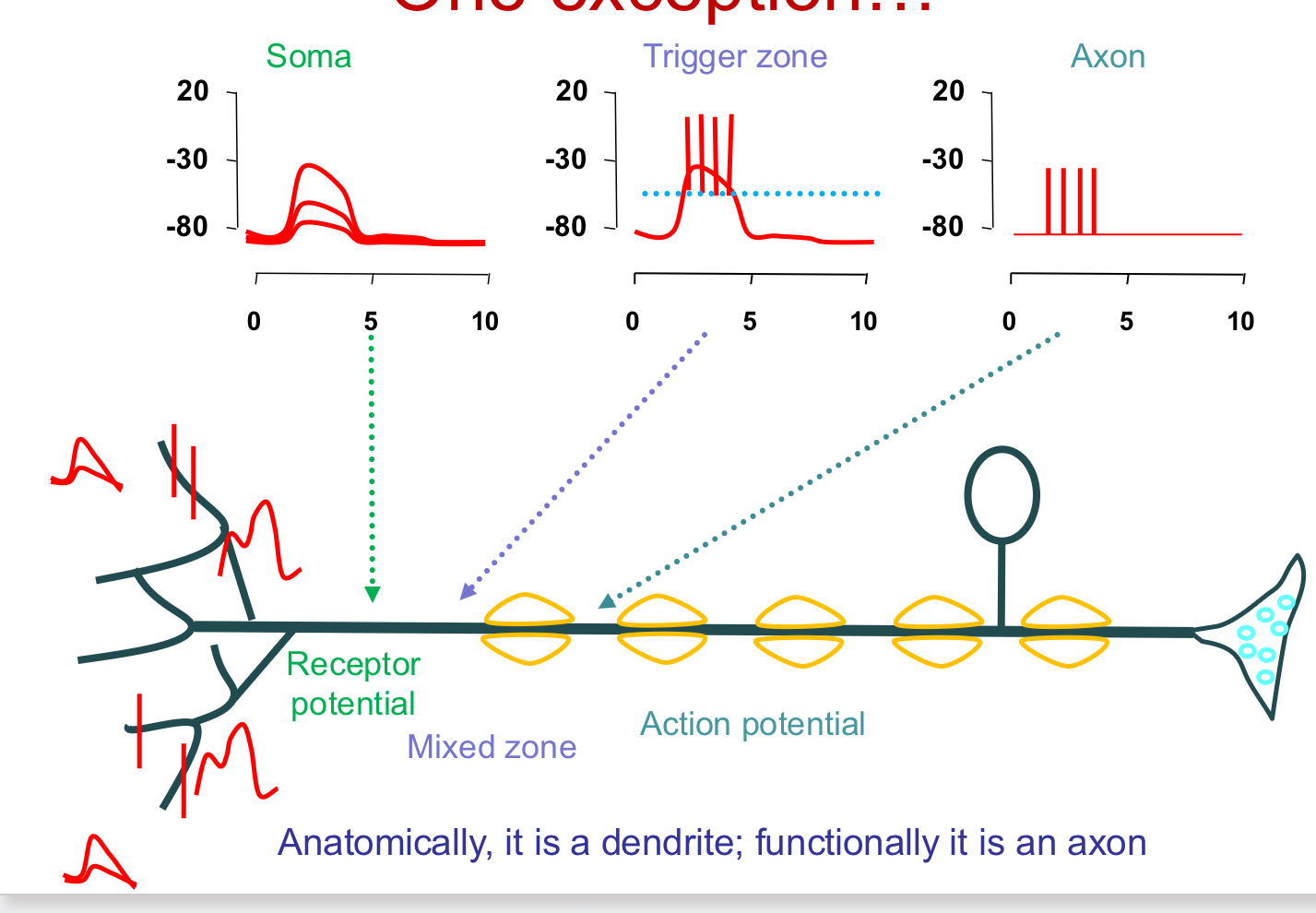
Explain Excitatory vs inhibatory post synaptic potentials
Excitatory(EPSPs):
electronic propagation- decreases w/ distance
propgates homogenusly in all directions
Begins in trigger zone (requires -60 mV)
Use ionotropic and metabotrpic receptors
Retrograde proagation of action potential: goes to soma but can retrograde back into dendrites (since it propagates equally in all directions)- causes neural plasticity via calcium channels
Inhibitory(IPSPs) (redce/block action potnetial firing probability)
ions with equilibrium potential more negative than resting potential are inibitory
Cl- channels: increase Cl- conductance, ECl is 90mV
K+ channels: increase K+ conductance, EK is -95mV
Generated by different receptors
Glycine (tetanus) and GABA via Cl- inhibits ionotropic receptors
5HY2C via IP3/DAG, 5HTA1 via decrease in cAMP, and muscarinic recptor M2 via decrease in cAMP and opening f K+ channels inhibit Metabotropic receptors
Take place near trigger zones
Originate in soma to compensate for the fact that excitatory potentials are more abundant and have a higher amplitude
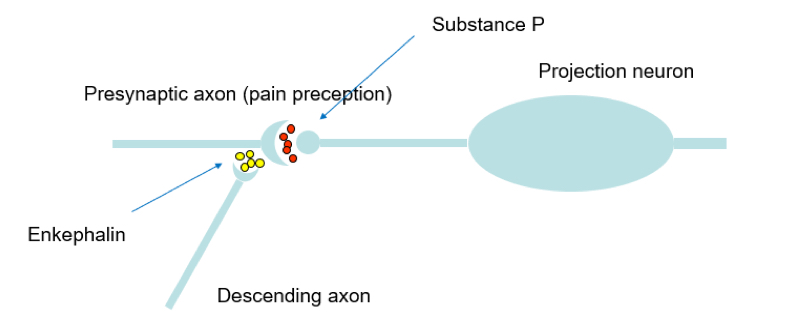
Explain presynaptic inhibition and facilitation
Inhibition:
Small sustained depolarization (ex: enkephalin- as painkiller)
Blocks Nachannels so decrease axonal action potential
Less volatge gate Ca channels opened
NT (neurotransmitter) release reduced
Hyperpolarization
GABA acts on neurons via GABA ceptors to Lower the aperture of C2+volateg gated channels, hence less NT release.
Ca2+ voltage gated chanels blockage
Less Ca entering, less NT release (opiods do this)
Non-Ca mediated Neurtrnamsitter exocytosis block
Facilitation: Potentiate NT release— serotonin does this
Keep this in mind:
What are the three different synapses?

For exam keep in mind:
The calcium from the reticulum is important only, Ca2+ from blood activate K+ channels for membrane potential, hence it is harder to start (regulator) — hypoglycemia causes muscle contraction
For example see
Ok