Micro 9 | Gram-Negative Bacteria I
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
68 Terms
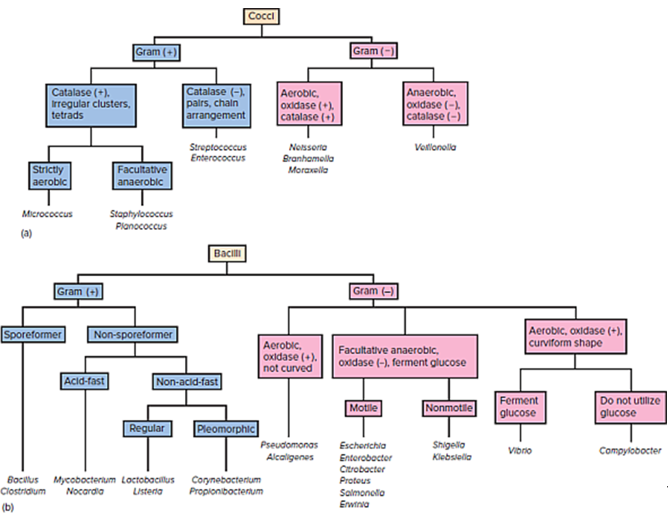
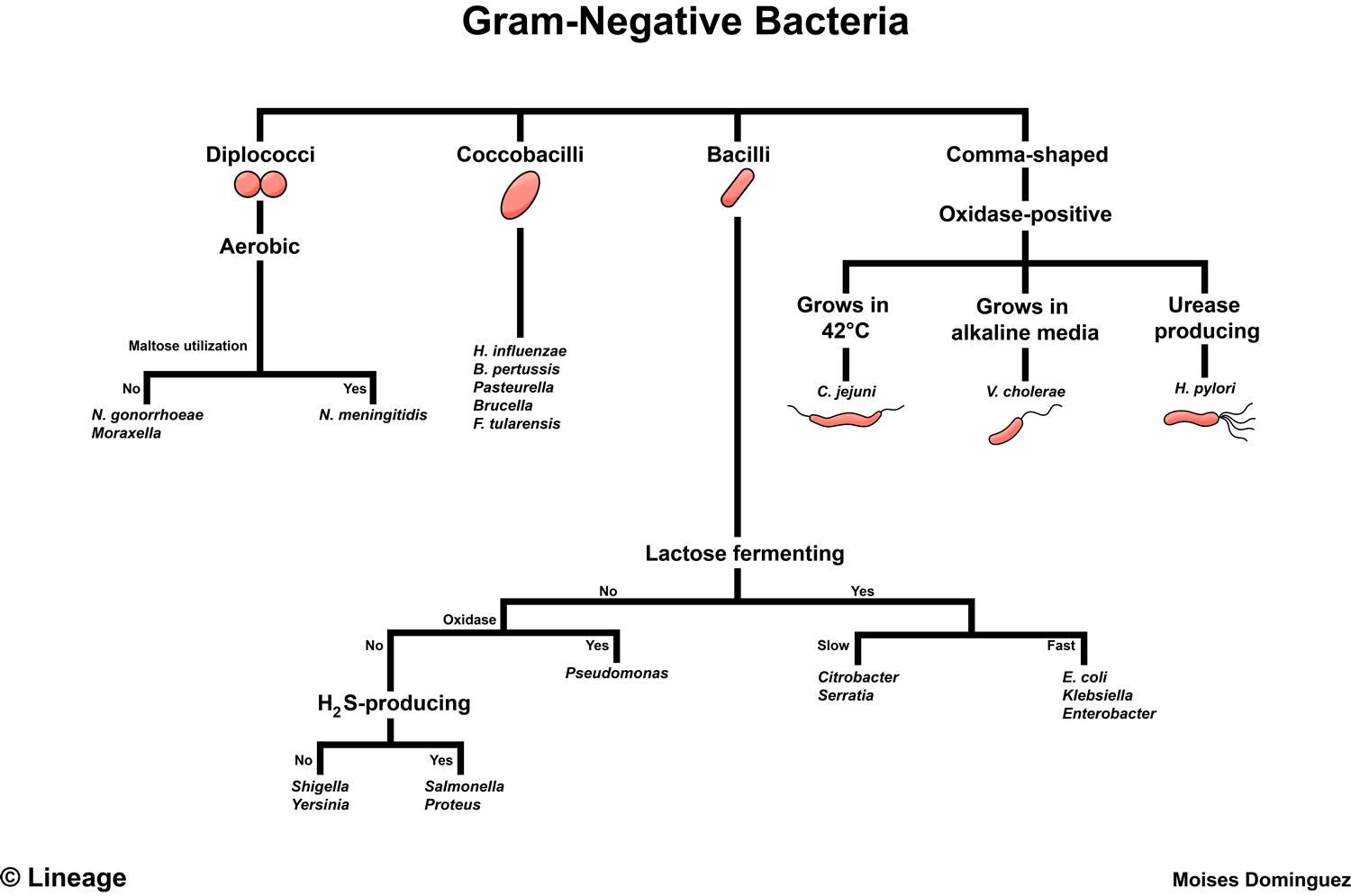
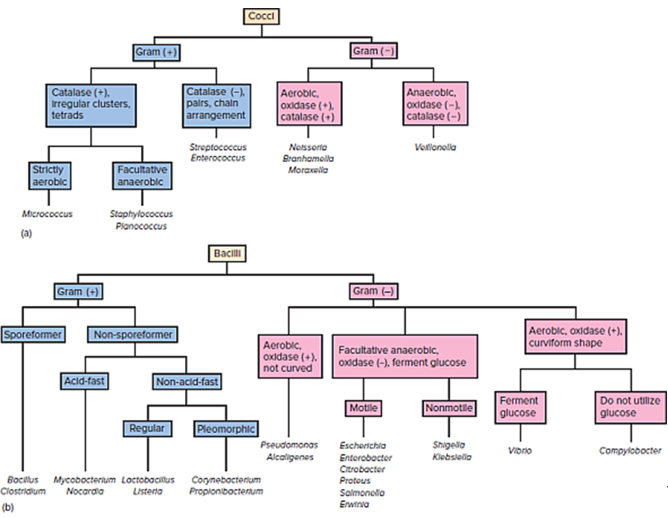
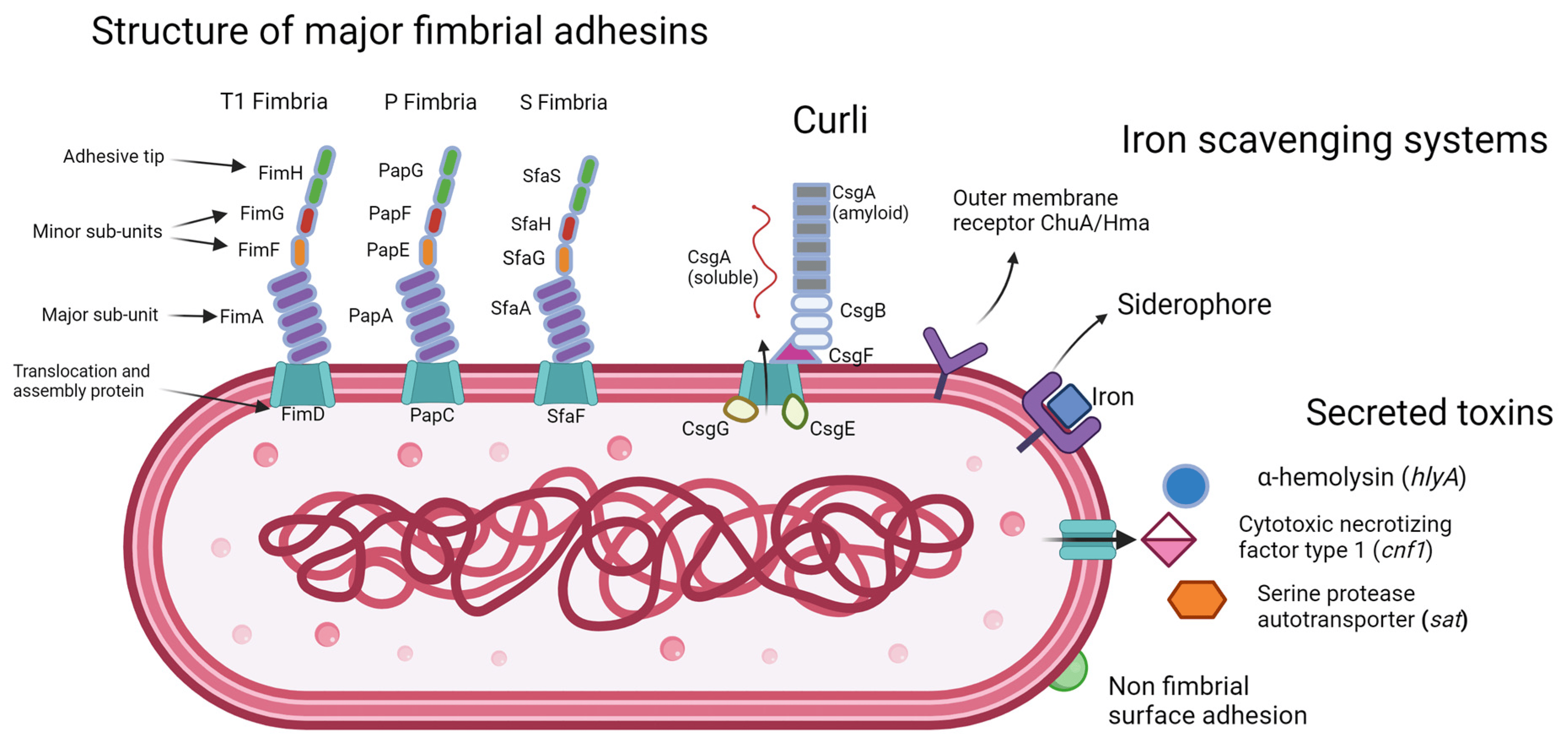
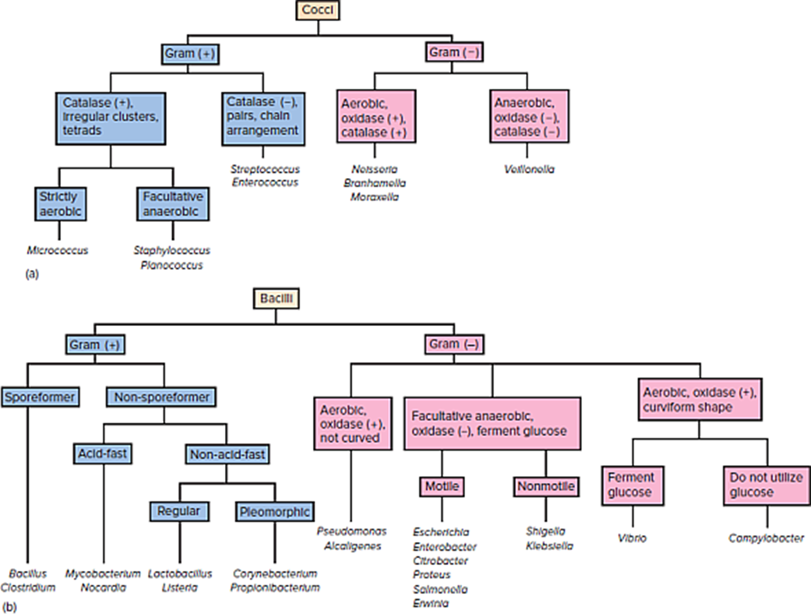
Gram Negative Algorithm
What is LPS, and why is it important?
A bacterial endotoxin that triggers strong immune responses, leading to inflammation, fever, and hypotension.
What are the three main components of LPS?
Lipid A (toxic part), polysaccharide core, and O antigen (for serotyping).
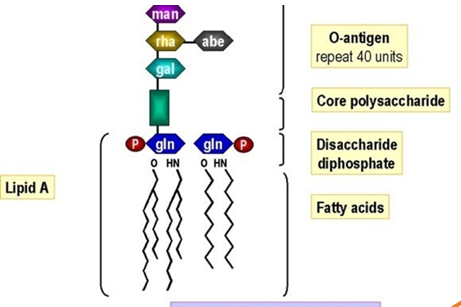
How does LPS activate the immune system?
LPS binds to TLR4 on macrophages, triggering cytokine release (IL-1, IL-6, TNF-α), leading to fever and low blood pressure.

What is lipo-oligosaccharide, and how is it different from lipo-polysaccharide?
LOS is a form of LPS that lacks the O antigen, making bacteria more susceptible to immune system attack.

Which gram negative bacteria are some of the most medically relevant bacteria?
Enterobacteriaceae
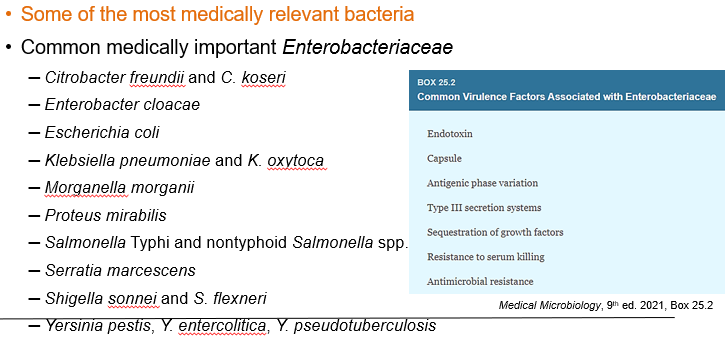
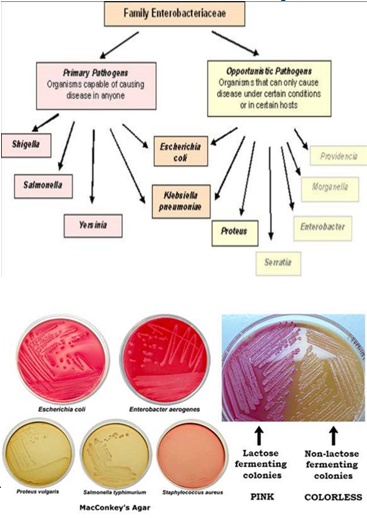
Enterobacteriaceae is a family of Gram-negative bacilli. What are some of the characteristics of this bacteria?
Some species have a capsule.
Most are motile, except Shigella and Klebsiella.
They are facultative anaerobes.
They ferment glucose, producing acid.
They reduce nitrates to nitrites.
They are oxidase-negative.
They are non-fastidious (can grow in simple media).
They grow on bile salt-containing media like MacConkey’s agar.
What type of bacteria is Escherichia coli? Gram positive or Gram Negative?
It is a Gram-negative rod with LPS (endotoxin, O antigen).
How do you diagnose/identify E. coli?
Through culture, Gram stain, and biochemical tests.
What are the key biochemical features of E. coli?
Ferments lactose
Indole positive
Oxidase negative
Motile due to flagella

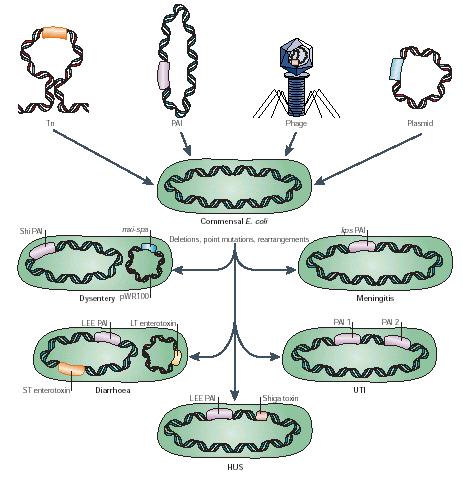
What makes E. coli capable of causing different diseases?
It expresses different virulence genes, which can be transferred via mobile genetic elements.
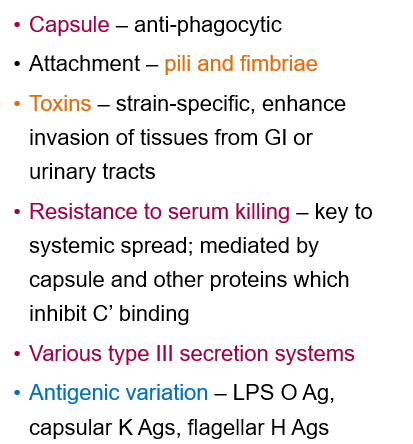
Virulence factors of E. coli?
Capsule prevents phagocytosis (immune evasion).
Pili and fimbriae help attach to host cells.
Strain-specific toxins that enhance tissue invasion, facilitating infection in the gastrointestinal and urinary tracts.
What are the two major pathogenic types of E. coli, and how do they cause disease?
EPEC (Enteropathogenic E. coli) causes diarrhea by altering intestinal cells.
UPEC (Uropathogenic E. coli) causes UTIs by attaching to the bladder and damaging cells.
Target population of Enteropathogenic E. coli?
Infants (before microbiome is established); now rare in developed countries
How is Enteropathogenic E. coli transmitted?
Through the fecal-oral route.
What are the main symptoms of an Enteropathogenic E. coli infection?
Watery diarrhea with mucus, fever, nausea, and vomiting.
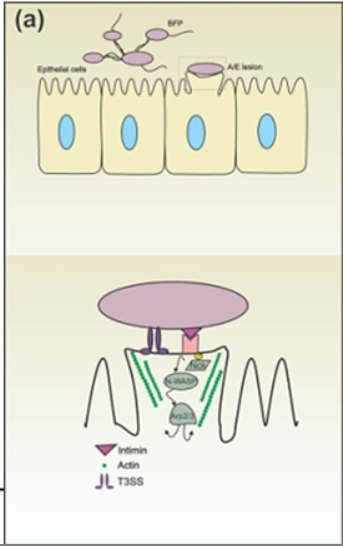
How does Enteropathogenic E. coli attach to intestinal cells?
Using bundle-forming pilus and Intimin/Tir proteins.
Intimin/Tir proteins are virulence factors in Enteropathogenic E. coli that help the bacteria attach to intestinal cells, disrupting their function and causing diarrhea.
What is the effect of Enteropathogenic E. coli on the intestine?
It disrupts the cytoskeleton, forming pedestal-like lesions, leading to cell destruction and reduced absorption.
Mnemonic to remember Enteropathogenic E. coli
"EPEC sits on a Pedestal" → EPEC creates pedestal-like lesions on intestinal cells by rearranging the cytoskeleton. This disrupts cell function and absorption, leading to diarrhea.
"EPEC affects Pediatrics" → EPEC primarily infects infants and young children before their gut microbiome is fully developed.
What is the function of Intimin and Tir proteins in EPEC infection?
Tir is injected into the host cell membrane and binds to Intimin on EPEC, creating a strong attachment that enables bacterial colonization and cellular damage.
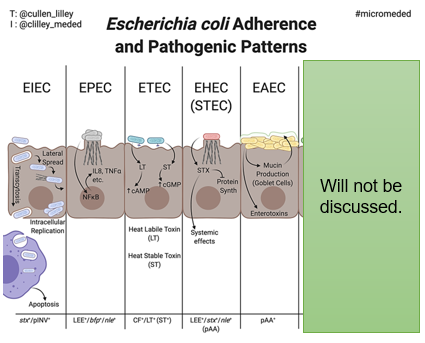
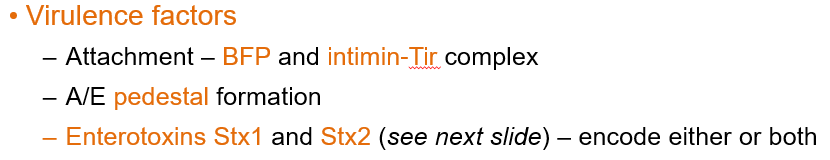
Pathogenesis of Enteropathogenic E. coli?
EPEC uses bundle-forming pili to attach to the intestinal cells.
The Type III secretion system (T3SS) injects bacterial proteins like Tir into host cells.
Tir inserts into the host membrane and binds to Intimin on EPEC, strengthening attachment.
Actin rearrangement creates pedestal-like structures, disrupting the cell surface.
Loss of microvilli reduces nutrient absorption.
EPEC weakens the connections between cells, causing fluid leakage.
Bacterial adhesion blocks fluid absorption, leading to watery diarrhea.
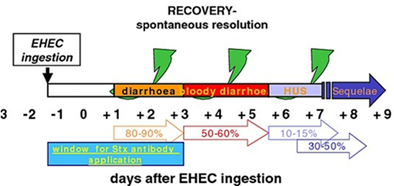
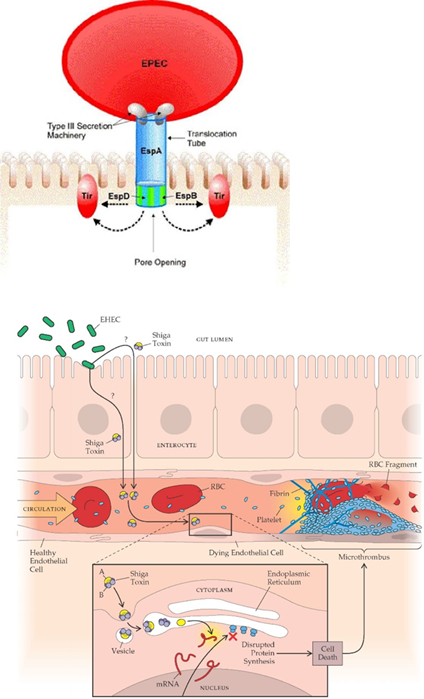
What is Shiga Toxin-Producing E. coli?
STEC, also called EHEC (Enterohemorrhagic E. coli), is a strain of E. coli that produces Shiga toxins, leading to severe gastrointestinal symptoms like bloody diarrhea and, in some cases, hemolytic-uremic syndrome
How is Shiga Toxin-Producing E. coli transmitted?
Through contaminated food (undercooked meat, unwashed vegetables), contaminated water, and person-to-person contact.

What are the symptoms of Shiga Toxin-Producing E. coli infection?
Starts 1-4 days after exposure, lasting 5-10 days.
Abdominal cramps, watery diarrhea → bloody diarrhea.
Can lead to hemorrhagic colitis and hemolytic-uremic syndrome (HUS) (kidney failure risk).
O157:H7 is the most common U.S. strain.
Presentation of Shiga Toxin-Producing E. coli?
Hemorrhagic colitis
Most common serotype of Shiga Toxin-Producing E. coli?
O157:H7 is the most common in the US
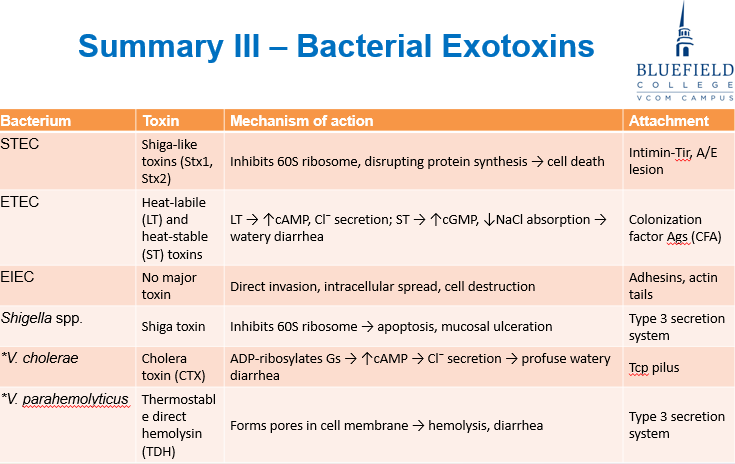
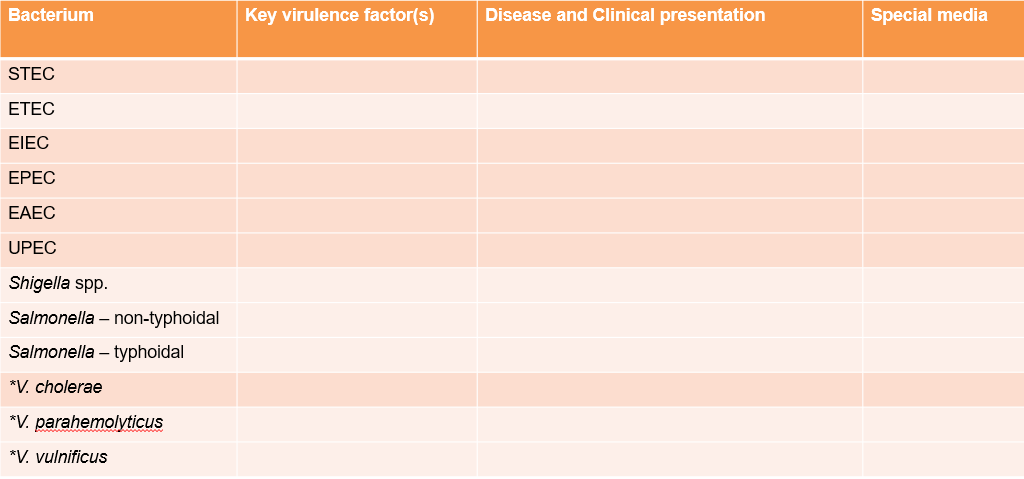
Virulence factors of Shiga Toxin-Producing E. coli?
Uses BFP and intimin-Tir for attachment.
Forms an A/E pedestal to disrupt intestinal cells.
Produces Shiga toxins (Stx1 and Stx2), which damage blood vessels and can cause severe disease.
Pathogenesis of Shiga Toxin-Producing E. coli?
EPEC attaches to intestinal cells using BFP (bundle-forming pili) for initial contact.
Uses a Type III Secretion System to inject Tir into the host cell.
Tir integrates into the host membrane and binds Intimin on EPEC, creating a stronger attachment.
Changes in actin form pedestals under the bacteria, leading to effacement (A/E lesions) and loss of microvilli.
Disrupts tight junctions, leading to fluid loss and diarrhea.
Intestinal cell death and damage to fluid absorption worsen diarrhea.
What is Enterotoxigenic E. coli?
A strain of E. coli that causes traveler's diarrhea by producing enterotoxins that disrupt fluid absorption in the intestines.
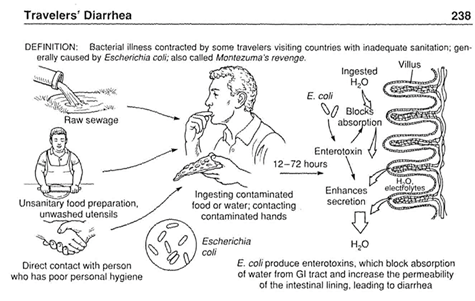
How is Enterotoxigenic E. coli transmitted?
ETEC spreads through contaminated food, water, or direct contact with infected individuals, often due to poor hygiene.
What symptoms does ETEC cause?
Watery diarrhea, sometimes accompanied by nausea, vomiting, and mild fever.
Virulence factors of Enterotoxigenic E. coli?
Fimbriae help bacteria attach to the intestinal lining.
Heat-labile (LT) enterotoxin and Heat-stable (ST) enterotoxin disrupt fluid balance, leading to diarrhea.
Pathogenesis of Enterotoxigenic E. coli?
E. coli uses fimbriae (colonization factor antigens) to stick to the intestinal lining.
Produces two toxins:
Heat-labile toxin (LT) increases cAMP, leading to chloride (Cl⁻) and water secretion.
Heat-stable toxin (ST) increases cGMP, reducing sodium (Na⁺) and water absorption.
Increased ion movement into the intestine causes massive water efflux, leading to watery diarrhea.
Unlike other diarrheal diseases, ETEC does not cause inflammation or cell damage—just fluid loss.
What is Enteroinvasive E. coli?
EIEC is a strain of E. coli that invades intestinal epithelial cells, causing an inflammatory diarrhea similar to Shigella infections.
How is EIEC transmitted?
Transmitted through contaminated food and water, often associated with poor hygiene and unsanitary conditions.
Presentation of Enteroinvasive E. coli?
Dysentery; Fever, abdominal cramps, inflammatory diarrhea with mucus and blood
Virluence factors of Enteroinvasive E. coli?
EIEC invades intestinal cells.
Avoids destruction by escaping from vacuoles inside host cells.
Moves between cells, causing tissue damage and inflammation.
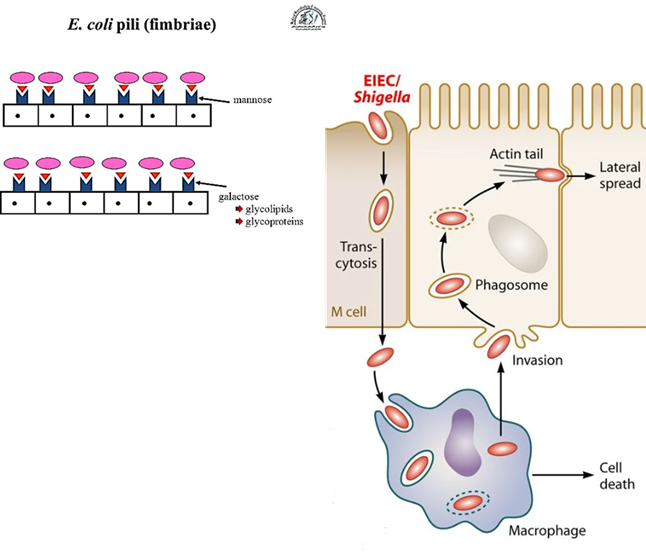
Pathogenesis of Enteroinvasive E. coli?
EIEC attaches to M cells in the intestines using pili and fimbriae.
The bacteria are taken up by M cells and transcytosed to the basolateral side.
Resident macrophages engulf EIEC but cannot destroy it.
EIEC lyses the phagosome using plasmid-encoded toxins.
The bacteria induce macrophage apoptosis, escape, and infect neighboring epithelial cells, leading to inflammation and diarrhea.
How is Enteroaggregative E. coli transmitted?
Through contaminated food, such as desserts and salsa, leading to gastrointestinal infection.
Symptoms/ Presentation of an Enteroaggregative E. coli infection?
watery and mucoid diarrhea, with bloody diarrhea occurring in 10-30% of cases, often without fever.
How long does EAEC infection typically last?
3-7 days but may become persistent in children and immunocompromised individuals (like HIV patients).
Virulence Factors of Enteroaggregative E. coli?
EAEC produces biofilms, which allow bacteria to attach to intestinal cells, making it more resistant to clearance.
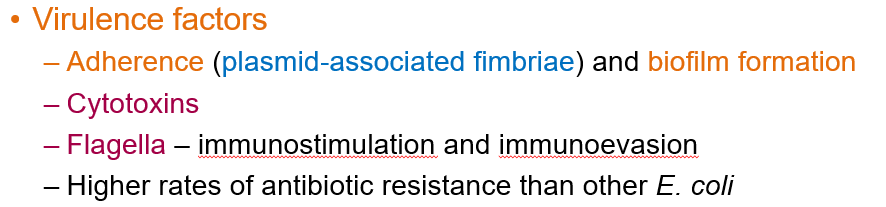
Pathogenesis of Enteroaggregative E. coli?
EAEC adheres to intestinal cells using aggregative adherence fimbriae, forming a "stacked brick" lesion.
EAEC produces biofilms, helping it evade the immune system and block nutrient and water absorption.
EAEC produces toxins, although their exact mechanism is not fully understood.
EAEC flagellin binds to TLR5 receptors, stimulating IL-8 and cytokine production, contributing to diarrhea.
Increased mucus production, biofilm accumulation, and bacterial aggregates lead to prolonged diarrhea, which can cause malnutrition and stunted growth, especially in children.
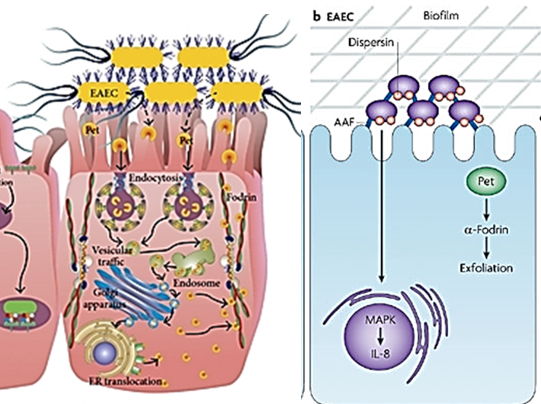
Which variant of E. coli is responsible for most cases of UTIs?
Uropathogenic E. coli
How is Uropathogenic E. coli transmitted?
Bacteria colonize the colon, spread to the perineal region, and ascend into the urinary tract.
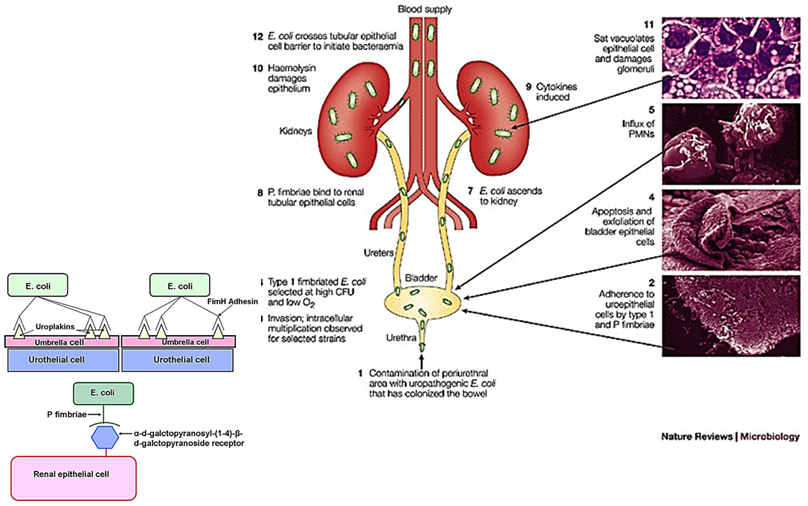
Virulence factors of Uropathogenic E. coli?
FimH – Helps UPEC bind to the bladder and migrate up the urinary tract.
P pilus – Associated with progression to kidney infections (pyelonephritis).
Biofilm formation helps UPEC survive in the urinary tract.
Flagella expression increases when UPEC reduces FimH and P pili, promoting bacterial movement and spread in the urinary tract, which can lead to kidney infections (pyelonephritis).
What are the major pathogenic species of Shigella?
S. dysenteriae (severe but rare)
S. flexneri (severe)
S. sonnei (mildest and most common)
S. boydii (mild and rare)
How is Shigella identified based on its bacterial characteristics?
A Gram-negative facultative anaerobe, oxidase negative, non-motile, and does not ferment lactose or produce H₂S.
What is the natural reservoir for Shigella?
Humans are the only reservoir for Shigella; it has no environmental or animal reservoir.
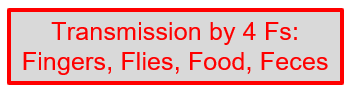
How is Shigella transmitted?
Via the "4 Fs"—Fingers, Flies, Food, and Feces—mainly through poor hygiene and contaminated hands.
What are the symptoms of Shigella infection?
It starts with watery diarrhea and progresses to dysentery (abdominal cramps, blood, mucus, and PMNs in stool in severe cases).
How is Shigella diagnosed?
Involves Hektoen enteric agar, biochemical profiling, and NAAT testing for toxin genes.
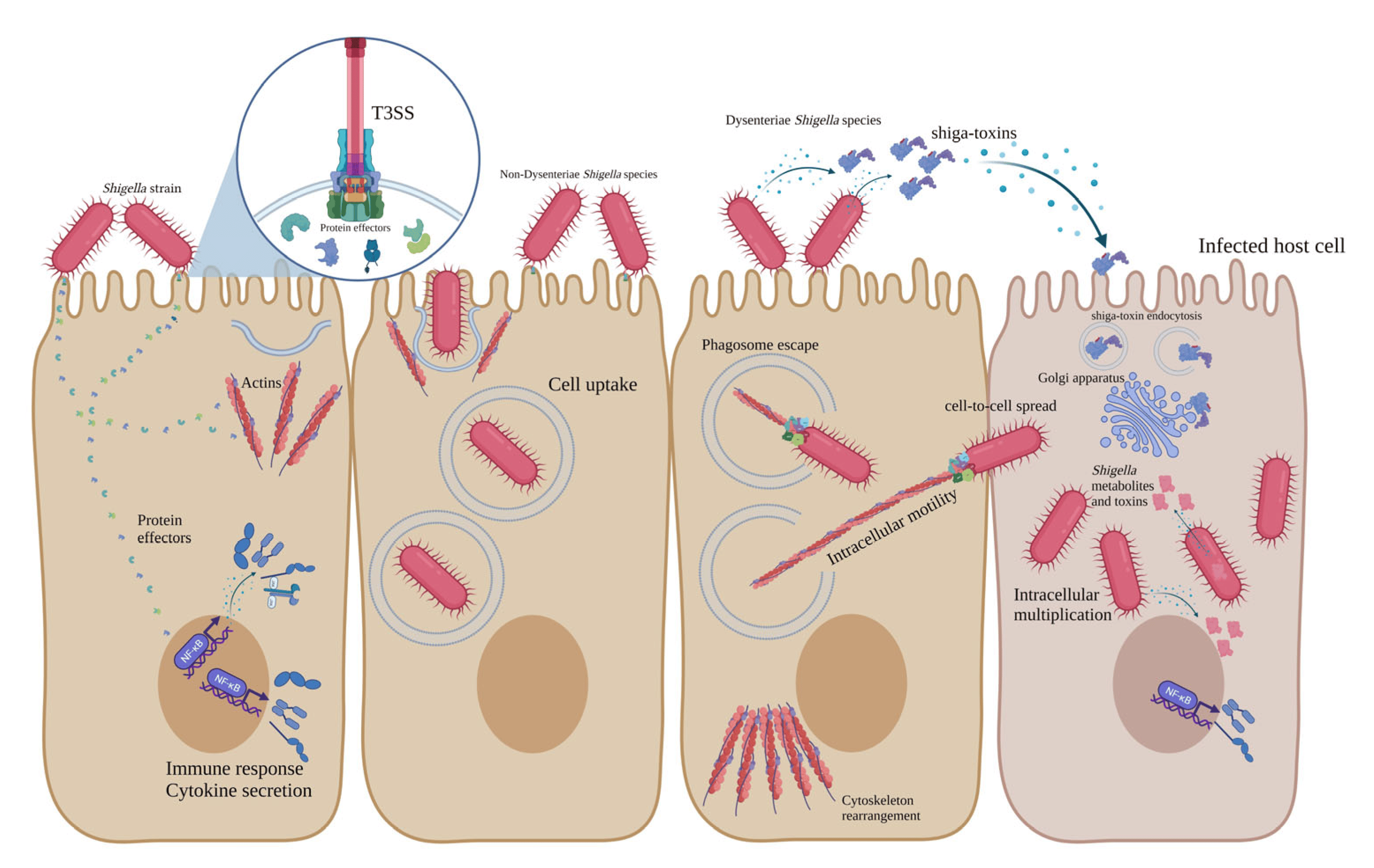
Virulence factors of Shigella species?
Invasion is the key virulence factor; even strains with minimal Shiga toxin can cause disease if they successfully invade M cells.
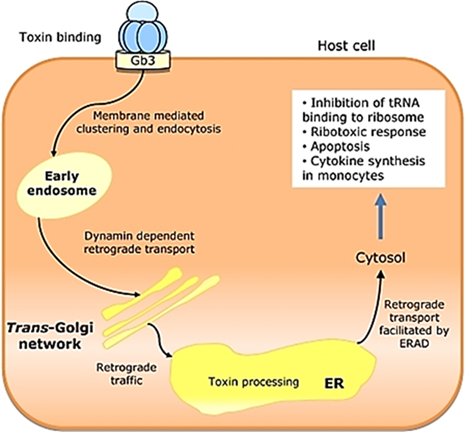
Shiga toxin (A/B enterotoxin) works by binding to Gb3 glycolipid, then transferring the A subunit to the 60S ribosome, where it depurinates the ribosome, stopping protein synthesis and leading to cell death.
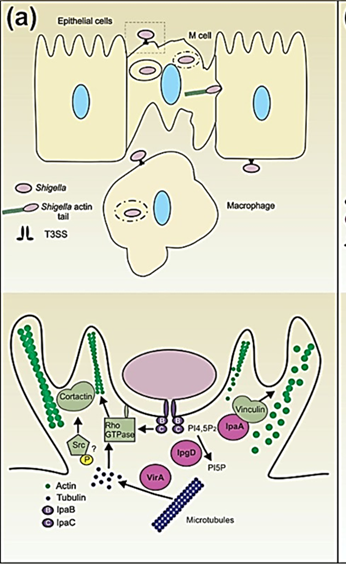
Pathogenesis of Shigella?
Shigella binds to M cells, injecting bacterial proteins that disrupt the cytoskeleton, causing endocytosis.
Once inside, Shigella escapes the endosome and replicates in the cytoplasm.
Bacteria move cell-to-cell using actin tails, avoiding the bloodstream (no hematogenous spread).
Shigella induces apoptosis in immune cells (macrophages), causing inflammation.
High levels of IL-1 and PMN recruitment break down cell connections, leading to tissue damage.
The destruction of intestinal cells results in bloody diarrhea with mucus and PMNs (polymorphonuclear cells).
What is Salmonella?
A Gram-negative, motile bacillus that can cause foodborne illnesses and systemic infections.
How is Salmonella diagnosed?
Does not ferment lactose
Oxidase negative
Produces H₂S (hydrogen sulfide)
Grows on Hektoen enteric agar
What are the main species of Salmonella that cause human infections?
S. typhimurium, S. enteritidis, S. paratyphi, and S. typhi
What role do animal reservoirs play in Salmonella infections?
Many animals carry Salmonella in their intestines, and the bacteria can spread to humans through contaminated food, water, or direct contact.
Virulence factors of Salmonella?
Capsule helps Salmonella evade the immune system by preventing complement activation and phagocytosis.
Hematogenous spread occurs through invasion of the GI tract via M cells in Peyer’s patches, followed by intracellular infection in macrophages.
Salmonella can survive in macrophages by inactivating the acidic environment of the phagosome.
Pathogenicity islands encode invasion proteins (Ssps) and a Type III secretion system, helping Salmonella enter and manipulate host cells.
Lipopolysaccharide (LPS) plays a key role in immune evasion and inflammation.
What bacteria cause non-typhoidal Salmonella infections?
Salmonella typhimurium and Salmonella enteritidis are the main causes.
Pathogenesis of Non-Typhoidal Salmonella?
Binds to M cells using fimbriae (FimA and FimH).
Uses a Type III secretion system (pathogenicity island I) to inject proteins, leading to actin rearrangement and endocytosis.
Proteins from pathogenicity island II prevent lysosome fusion and acidification, allowing bacterial survival and replication.
Bacteria are released, multiply in the lamina propria, and spread within the GI epithelium.
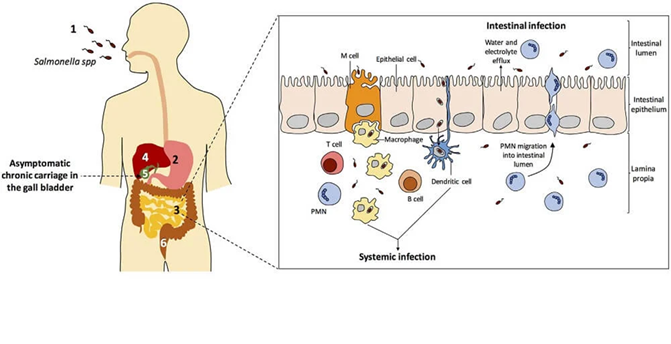
What is Typhoidal Salmonella?
Unlike non-typhoidal Salmonella, which mainly causes food poisoning with diarrhea and vomiting, typhoidal Salmonella invades the bloodstream and affects multiple organs, leading to typhoid or paratyphoid fever.
Typhoidal Salmonella primarily cause systemic infections rather than localized gastroenteritis.
What bacteria cause typhoid and paratyphoid fever (Typhoidal Salmonella)?
Salmonella typhi and Salmonella paratyphi
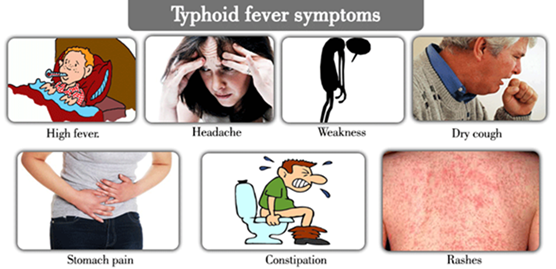
Clinical presentation of Typhoidal Salmonella?
"Rose rash" on the trunk in ~30% of cases, lasting 3-4 days.
Gastrointestinal symptoms: Starts with constipation, then progresses to diarrhea.

How can someone spread Salmonella typhi without showing symptoms?
Some people can carry Salmonella typhi in their gallbladder without showing symptoms, but they can still spread the bacteria to others through their stool, as seen in the case of Typhoid Mary.
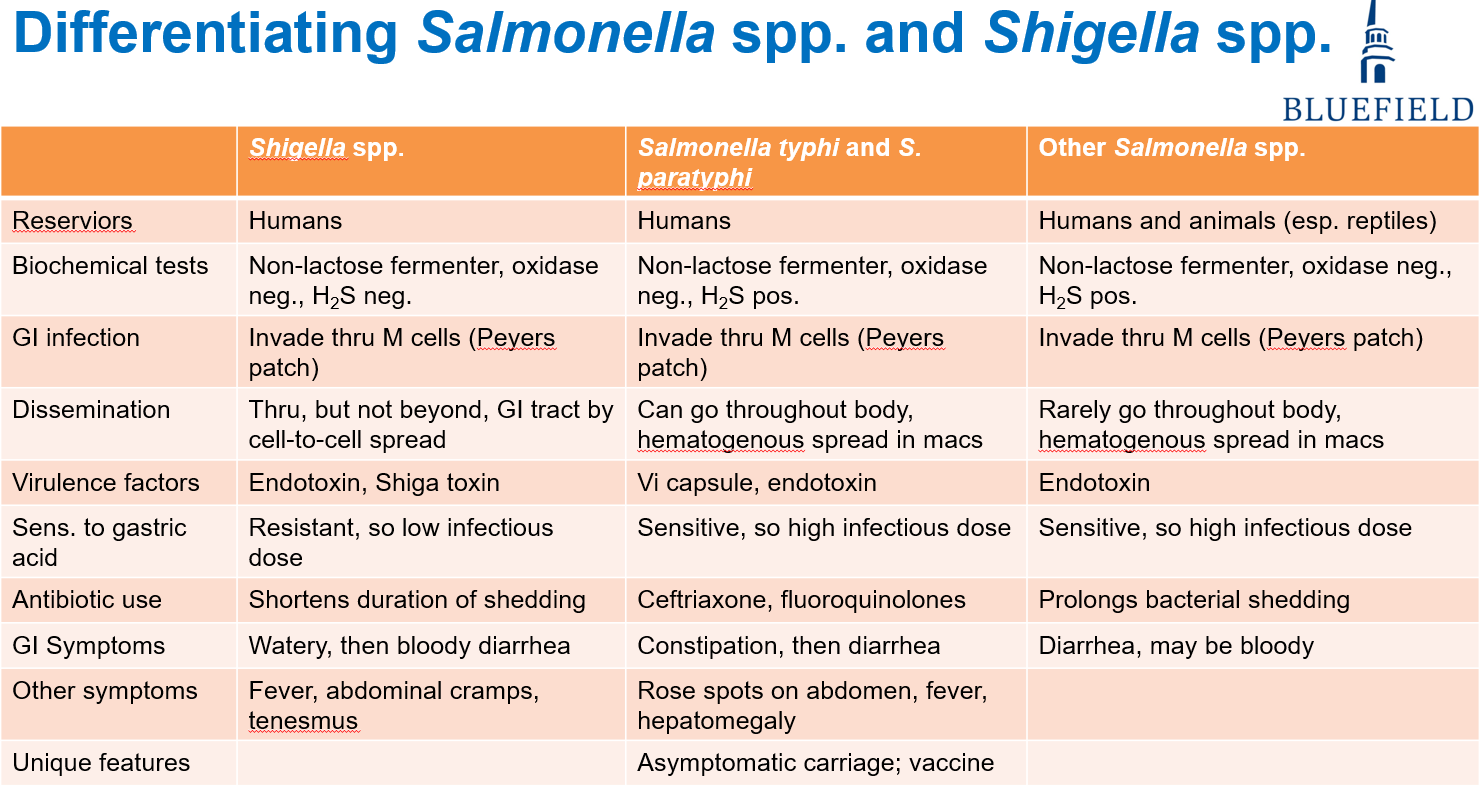
Differences between Salmonella (non-typhoidal vs typhoidal) versus Shigella?
Non-typhoidal Salmonella: Causes gastroenteritis, spreads through contaminated food (poultry, eggs), and remains localized in the GI tract.
Typhoidal Salmonella (S. typhi, S. paratyphi): Causes typhoid/paratyphoid fever, spreads systemically via the bloodstream, and can colonize the gallbladder (e.g., Typhoid Mary).
Shigella: Causes shigellosis (dysentery), spreads via fecal-oral route, invades intestinal epithelial cells, and leads to bloody diarrhea with mucus and PMNs. It requires a low infectious dose compared to Salmonella.
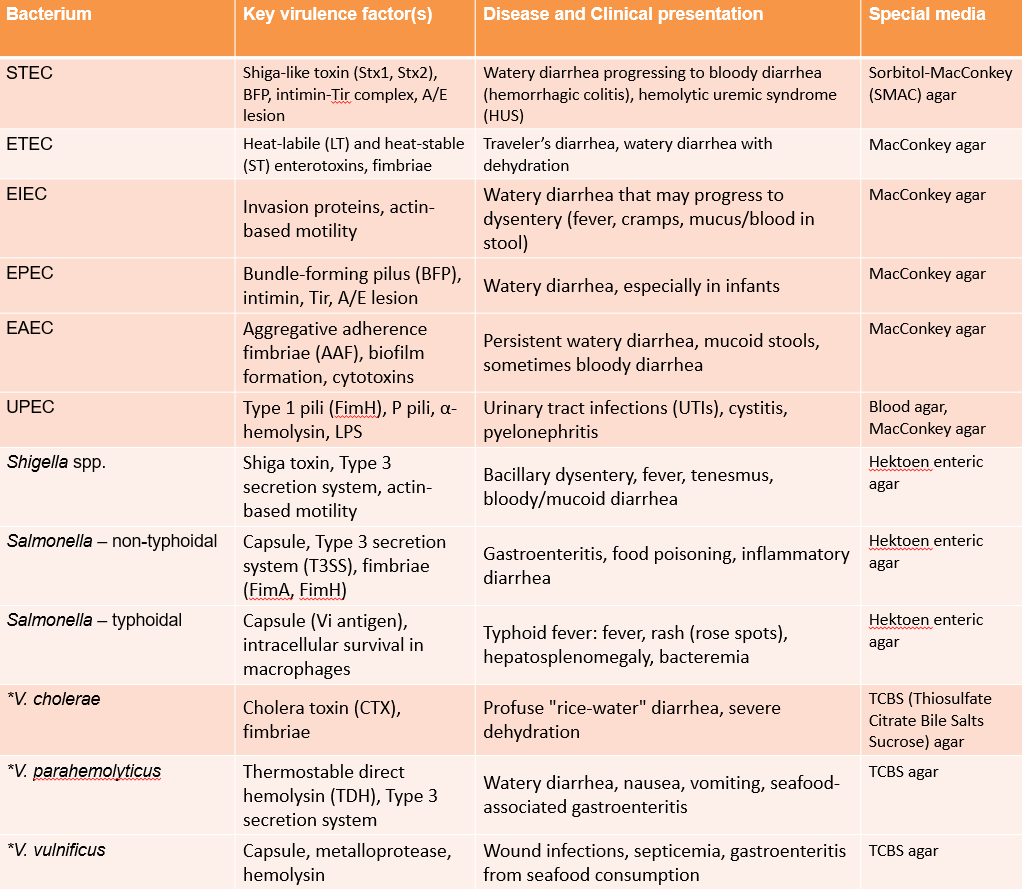
Bacterial Exotoxins