anaesthetic breathing systems and IVFT
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
37 Terms
what is the aim of general anaesthesia
ensure patient is in a state of controlled unconsiousness with associated analgesia and muscle relaxation
important stages of anaesthesia
pre-operative assessment
premedication
induction of anaesthesia
maintenance of anaesthesia
recovery from anaesthesia
what should pre-op assessment incl
history and clinical exam which may provide info on health status of patient and highlight any potential factors which may impact the risk of anaesthesia to your patient and so your choice of anaesthetic drugs
ensure you have venous access to patient
aim of premedication
reduce anxiety ]ease handling patient
smooth induction
smooth maintenance
smooth recovery
reduce dose of anaesthetic drugs required
provide pre-emptive analgesia
following premedication what agents are used
injectable agents - propofol
inhalation agents - isoflurane
intravenous agents
used to induce anasthesia
easy to administer
provide rapid, smooth induction
generally short acting, allow enough time for vet to intubate patient and connect them to anaesthetic circuit for maintanence of anaesthetia
then anaesthesia commonly maitained by saturating oxygen with appropriate level of inhalation agent
require metabolism to deactivate and allow patient to fully recover from general anaesthesia
maintanence agents
volatile liquids which vapourise and saturate oxygen to controlled level
concentration of vapour within oxygen devlivered to patient can then be increased or decreased to deepen or lighten the level of anaesthesia
benefit of using inhalation agent = delivery of oxygen and rapid change depth of anaesthasia by adjusting conc of gas delivered
caesing of inhalation agent allows patient to regain consciousness
recovery period
associated with greatest risk of morbitdity and mortality in anaesthesia
2 major types of breathing systems
rebreathing system
non-rebreathing system
rebreathing systems
allow patient to rebreath expired gas
contains higher levels of CO2 whcih must be extracted before patient rebreaths economical but high resistance so only suitable for patients over 15kg
non-rebreathing systems
should not allow patient to rebreath expired gas
expired gas must be flushed out circuit before patient takes nect inhale so utilise a higher fresh gas flow rate
less economical but have low resistance so suitable for patients <25kg

adapter to connect ET tube
designed so can only be connected to ET tube so cant incorrectly connect to anaesthesia machine

expiratory valve
also called adjustable pressure limiting or APL valve

resevoir bag
allows us to undertake intermittent positive pressure ventilation should patient stop breathing
should have capacity of at least twice the normal tidal volume of patient
fresh gas tubing
delivers gas from anaesthetic machine to patient
commonly green
expired gas tubing
takes expired gas away from patient and is white in image

soda lime canister
removes CO2 from expired gas rendering it safe to be rebreathed
soda lime changes colour when reacts with CO2 allowing us to detect when canister is saturated and needs soda lime to be changed
will have gaps of air between granules = inter-granular volume - usually half canisters capacity , should be at least twice the maximium tidal volume of animal
max tidal volume = 2-3 times normal resting tidal volume
bodily fluid compartments
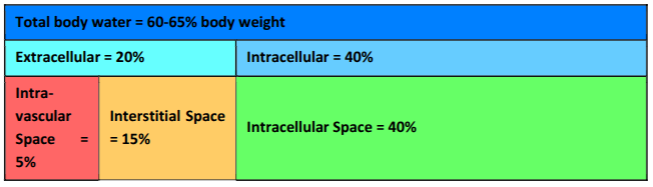
semipermeable membranes that separate body compartments
capillary membrane - between intravascular space - freely permeable to water and electrolytes but not macromolecules
cell membrane - between interstitial space and cell - freely permeable to water
fluid movement accross them is goverend by hydrostatic pressure - move low ti high
hydrostatic pressure affected by osmotic and oncotic pressure
osmotic created by solutes such as electrolytes, glucose and urea
oncotic created by proteins
types of fluid
crystalloids - contain water, NaCl and other solutes - available in multiple concentrations, reffered to as tonicity of solution= describes the effective concentrations of solution when compared to plasma
colloids - contain water, starch, NaCl and other solutes - contain macromolecules which tend to be retained in intravascular spce and exert osmotic effect = retention of fluid in intravascular space
protein-based solutions incl non-oxygen carriers - plasma and oxygen carriers such as whole blood
movement of fluid between intravascular and interstitial space depends on tonicity of fluid administered
isotonic - no net movement
hypotonic = net movement from intravascular space → interstitial
hypertonic = net movement from interstitial space → intravascular
isotonic solutions commonly administerd to dehydrated patients e.g diarrhoea or vommiting or in shock
hypertonic administered to patient in shock to rapidly increase circulating blood volume but never to dehydrated patient
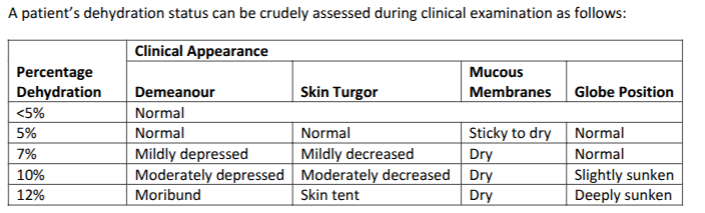
dehydration
associated with loss of fluid from intravascular and interstitial space
to correct it need to calculate volume of isotonic fluid required to restore body fluid to normal
consider - maintanence requirements, current deficit, ongoing losses
shock
circulatory shock caused by hypovolaemia, a loss of fluid from intravascular space = emergency situation
immediate treatment required to increase intravascular volume so CO can be maintained
shock can be with or without dehydration e.g
road accident = shock without dehydration
chronic diarrhoea = shock with dehydration
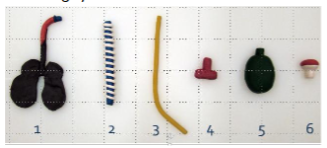
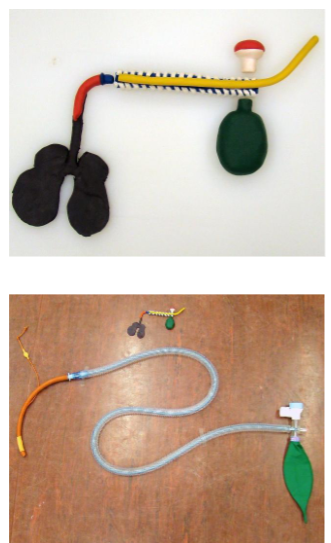
1. Connection to ET tube
2. Expired gas tubing
3. Fresh gas tubing
4. (T-connector)
5. Reservoir bag
6. Expiratory valve

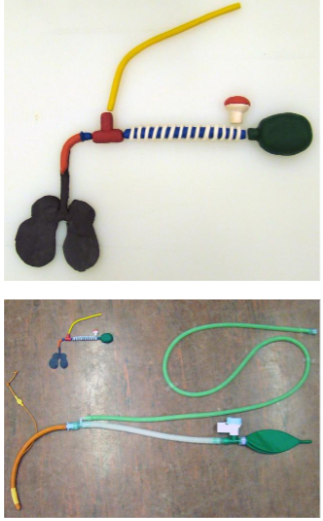
mapleson A
used in patients >10kg
Fresh gas enters the system from the anaesthetic machine and fills the reservoir bag.
• At the start of inspiration, the lungs are empty, the reservoir bag is full and the breathing system is full of fresh gas.
• At the end of inspiration, the patient has breathed in. There is fresh gas in the breathing system and the lungs and the reservoir bag has decreased in size
• During expiration the lungs reduce in size forcing expired gas back into the tubing.
• By the end of expiration, the reservoir bag is full of gas displaced from the tubing by expired gas.
• During the expiratory pause, fresh gas continues to enter the breathing system but cannot re-enter the lungs.
• Pressure within the system is now high enough to open the expiratory valve. Fresh gas continues to flow into the system and therefore expels expired and dead space gas through the expiratory valve
very efficient for spontaneously breathing patients as resevoir bag is filled with fresh gas
presence of expiratory valve at patient end of system can provide challenges for ops around head
can make manual ventilation challenging
considered inefficient for IPPV
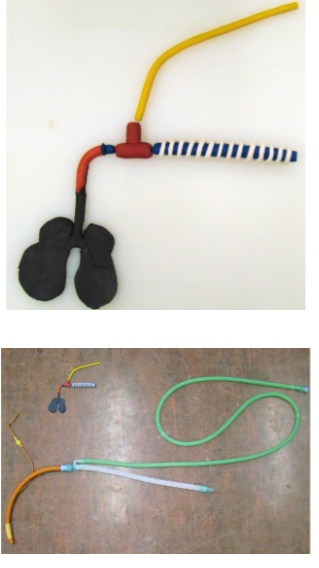
mapleson D
used in patients <10kg
Fresh gas enters the breathing system from the anaesthetic machine
• At the start of inspiration, the lungs are empty, the reservoir bag is full and the breathing system is full of fresh gas.
• At the end of inspiration, the patient has breathed in. There is fresh gas in the breathing system and the lungs and the reservoir bag has decreased in size
• During expiration the lungs reduce in size forcing expired gas back into the expired gas tubing
• By the end of expiration, the reservoir bag is full of gas displaced from the expiratory tubing by the expired gas
• During the expiratory pause, fresh gas continues to enter the breathing system but cannot re-enter the lungs.
• Pressure within the system is now high enough to open the expiratory valve. Fresh gas continues to flow into the system and therefore expels expired and dead space gas through the expiratory valve, so at the
next breath the animal will only breathe in fresh gas
less efficient than magill as require higher gas flow rate in order to ensure expired gas is cleared from resevoir bag prior to next inspiration
more suitable for performing IPPV than magill
Mapleson E
used in patients <10kg
Fresh gas enters the breathing system from the anaesthetic machine
• At the start of inspiration, the lungs are empty, and the breathing system is full of fresh gas.
• At the end of inspiration, the patient has breathed in. There is fresh gas in the breathing system and the lungs.
During expiration the lungs reduce in size and the flow of fresh gas in the fresh gas tubing means expired and dead space gas is forced into the expiratory tubing.
• By the end of expiration, the expiratory tubing is full of expired and dead space gas.
• The continued flow of fresh gas during the expiratory pause increases the pressure in the system and forces expired gas out of the tubing. Remember there is no expiratory valve in this system
has very low resistance = suitable for small patients
least efficient class of breathing system so high fresh gas flows required to clear expired gas from tubing
doesnt has resevoir bag so IPPV couldnt be performed if patient stops breathing
scavenging waste gases is hard
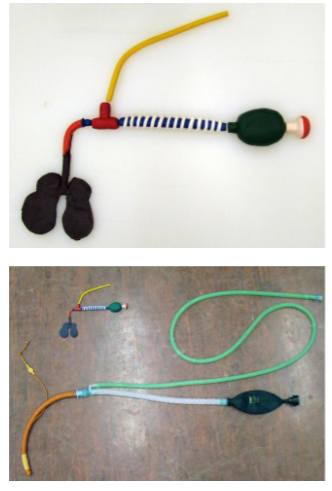
Mapleson F
connector on resevoir bag is not expiratory valve
used in patients <10kg
Fresh gas enters the breathing system from the anaesthetic machine
• At the start of inspiration, the lungs are empty, the reservoir bag is full and the breathing system is full of fresh gas.
• At the end of inspiration, the patient has breathed in. There is fresh gas in the breathing system and the lungs and the reservoir bag has decreased in size
• During expiration the lungs reduce in size and the flow of fresh gas in the fresh gas tubing means expired and dead space gas is forced into the expiratory tubing.
• By the end of expiration, the expiratory tubing contains expired and dead space gas and the reservoir bag is full.
• The continued flow of fresh gas during the expiratory pause increases the pressure in the system and forces expired gas out of the system via the reservoir bag. So that the patient will only breathe fresh gas during the next breath. Remember there is no expiratory valve in this system
low level resistance = suitable for small patients
resevoir bag can be used for IPPV
least efficient = high gas flows required to flush expired gas from system via resevoir bag
appropriate scavenging from system hard due to open bag set up

parallel lack
used in patients >7kg
Fresh gas enters the breathing system from the anaesthetic machine
• At the start of inspiration, the lungs are empty, the reservoir bag is full and the breathing system is full of fresh gas.
• At the end of inspiration, the patient has breathed in. There is fresh gas in the breathing system and the lungs and the reservoir bag has decreased in size
• During expiration the lungs reduce in size forcing gas back into the breathing and the flow of fresh gas in the fresh gas tubing means expired and dead space gas is forced into the expiratory tubing.
• By the end of expiration, the expiratory tubing contains expired and dead space gas.
• During the expiratory pause, fresh gas continues to enter the breathing system but cannot re-enter the lungs.
• Pressure within the system is now high enough to open the expiratory valve. Fresh gas continues to flow into the system and therefore expels expired and dead space gas through the expiratory valve.
Efficient for spontaneous breathing as the reservoir bag is filled with fresh gas. The expiratory valve has been moved away from the patient, compared to the Magill, meaning that surgery around the
head would be less challenging and it is easier to adjust the valve if the patient requires ventilation.
not suited to prolonged IPPV, as it allows for build-up of CO2 in the system in the same way as the Magill.
Co-axial bain
used in patients >10kg
fresh gas enters breathing system from anaesthetic machine
at start of inspiration lungs are empty, resevoir bag full and breathing system full of fresh gas
end of inspiration patients has breathed in, fresh gas in breathing system and lungs and the resevoir bag has decreased in size
during expiration lungs reduce in size forcing expired gas back into expired gas tubing
by end of expiration the resevoir bag is full of gas displaced from expiratory tubing by expired gas
during expiratory pause fresh gas continues to enter breathing system but can’t reenter lungs
pressure within system is high enough to open expiratory valve. fresh gas continues to flow into system and expel expired and dead space has through expiratory valve, so next breath animal will only breath fresh gas
can be used for IPPV
modification of tubing allows for extension of fresh and expired gas tubing without increased resistance in system so allows for good anaesthetic machine positioning
due to co-axial of tubing theres potential for inner tube disconnection = lead to extensive rebreathing of expired gas
check tubing before each use and additional leak testing to test integrity of inner tube required on top of standard leak testing

circle system- rebreathing system
used for patients >15kg
Fresh gas flows into the system from the
anaesthetic machineDuring inspiration the one-way expiratory valve closes and the inspiratory valve opens.
Gas flows from the reservoir bag to the patient via the inspiratory tubing
During expiration the lungs reduce in size forcing expired gas back into the circuit.
The inspiratory valve closes and gas flows into the breathing bag via the expired gas tubing.
The CO2 is absorbed by the soda lime.
During the expiratory pause, the pressure is at its highest in the circuit and excess gas will exit the system via the expiratory valve
Only a single turn of the expiratory valve is required when setting up the circuit in order that excessive amounts of gas are not lost from
the system.
The advantages of rebreathing systems, such as the circle, include conservation of heat and moisture in respired gases; the efficiency of the
system due to low fresh gas flow rates required and the ability to perform IPPV easily.
However, the resistance in the system is high so it cannot be used for small patients, the need to replace soda lime and the slower
change in anaesthetic depth when the anaesthetic gas concentration is changed are potential disadvantages of this system.
what to consider when calculating the flow rate required for non-rebreathing systems
patients minute volume
breathing system being used
minute volume
volume of gas patient is expering per minute
approx 200ml/kg/min
based on tidal volume 10ml/kg and respiratory rate of 20 breaths/min
if respiratory rate is higher it will increase minute volume
flow rate required for rebreathing systems
10-50ml/kg/min
tend to start with initial flow rate of 2-4l/min for first 10 mins to clear circuit of air then reduce to 0.5-1l/min for maintenance
if flow rate too high
not an issue for patient but wasteful as fresh gas comprising O2 and inhalational agent expelled unecessarily
if flow rate too low
expired alveolar gas wont be completely removed from system dueing expiratory pause and gas with increased levels CO2 will be rebreathed by patient
treatment of dehydration fluid therapy calculations
administered intravenously over 24hrs via continuous rate infusion using gravity or infusion pump, patient should be monitored and reevaluated over period incl HR, RR and mucous membranes and pulse quality
maintanence requirement = 2ml/kg/hr or 50ml/kg/24hr
deficit = volume in ml = % dehydration(0.05-0.12) x bodyweight(kg) x 1000
ongoing losses - estimate volume lost each time - 4ml/kg/episode x weight(kg), estimate frequency of loss over 24hr period e.g vomit 4 times a day, volume in ml = volume of loss per episode(ml) x frequency of loss per 24hrs
from this calculate volume per min and drip rate
treatment of shock fluid therapy calculations
initial treatment incl bolus administration of isotonic crystalloid fluids
fluids should be administered as quick as possible but often restricted by size of catheter placed to increase rate -
apply 2 IV catheters
apply pressure to fluid bag to force fluid into intravascular space rather than relying on gravity
bolus of 10-20ml/kg should be administered over 15-30mins
following administration re-evaluate patient - checl HR,RR, mucous membranes
if still in shock repeat bolus
monitor throughout - too much = pulmonary oedema
once normal circulatory volume restored switch to continuous rate infusion of fluids at appropriate rate