BTEC Applied Science Unit 5
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
Function of the Right Pulmonary Artery
Carried deoxygenated blood to the right lung
Function of the Aorta
Carries oxygenated blood from the left ventricle to the rest of the body
Function of the Left Pulmonary Artery
Carries deoxygenated blood to the left lung
Function of the Left Pulmonary Vein
Carries oxygenated blood to heart from left lung
Function of Semilunar Valve
prevent backflow of blood from aorta to ventricles
Function of the Atrioventricular (Bicuspid) Valve
Prevent backflow of blood from Left Ventricle to Left Atrium
Function of the Septum
Cardiac muscle that divides the left and right side of heart
Function of Purkinje Fibres
Carry nerve impulses to ventricles to ventricles to aid contraction
Function of the Inferior Vena Cava
Carries deoxygenated blood from the lower body to the heart
Function of the Bundles of His
transmit impulses from AV Node to ventricles
Function of Atrioventricular (Tricuspid) Valve
Prevent backflow of blood from Right Ventricle to Right Atrium
Function of Sinoatrial Node (SA Node)
The pacemaker of the heart, which is responsible for the regular contraction of the heart muscle.
Function of the Right Pulmonary Vein
Carry oxygenated blood to the heart from right lung
Function of the Superior Vena Cava
Carry deoxygenated blood from upper body to Right Atrium
Step 1 of Blood Flow(deoxygenated)
Aorta relax and fill with blood from Superior and Inferior Vena Cavae
Step 2 of Blood Flow (deoxygenated)
Atria Contract (Atrial Systole) which forces AV valves open and blood moves through to fill ventricles
Step 3 of Blood Flow(deoxygenated)
AV Valves close shut to prevent backflow
Step 4 of Blood Flow (deoxygenated)
Ventricles contract (Ventricular Systole) - increases pressure
Step 5 of Blood Flow (deoxygenated)
The pressure causes semilunar valves to open and blood flows into pulmonary arteries (deoxygenated) The pressure in arteries closes the SL valves to prevent backflow.
What happens to the process of blood flow for oxygenated blood?
The process for deoxygenated is reversed.
Blood enters from Pulmonary Veins, into Left Atrium and is forced through to Left Ventricle through the Bicuspid Valve. The ventricle contracts and forced blood through the Sl Valve into the Aorta where it is pumped around the body.
The formulae for cardiac output?
Cardiac Output = Heart Rate X Stroke Volume
What is the Cardiac Cycle?
The process of pumping blood around the heart, once oxygenated blood is received from lung.
Step 1 of the cardiac cycle
Blood drains from Left Atrium from Pulmonary Vein. This is cardiac diastole (heart fills with blood).
Step 2 of the cardiac cycle
The raising of blood pressure in Left Atrium forces Bicuspid Valve to open.
Step 3 of the cardiac cycle
The contraction of Left Atrium (atrial systole) forces blood through the AV valve into the Left Ventricle.
Step 4 of the cardiac cycle
When the Left Ventricle is full (Ventricular Diastole) the ventricles contract (Ventricular Systole).
Step 5 of the cardiac cycle
The pressure caused by Ventricular Systole causes AV Valve to shut and causes SL valves to open. Blood is forced up into the Aorta.
What happens to the right side of the heart in the cardiac cycle?
The process is exactly the same for deoxygenated blood.
The Structure of Arteries
Thick wall, smooth muscle and elastic fibres. They are also lined with endothelial cells in a narrow lumen.
The Structure of Capilliaries
Very thin wall with a small lumen.
The Structure of Veins
A thin wall, with very little smooth muscle or elastic fibres. The lumen is wide and there are valves.
Function of Arteries
To withstand high blood pressure as they carry blood away from heart. They must be able to change the diameter of lumen with the blood flow. The walls must be able to stretch when blood is pumped through and be able to recoil back to size. Therefore the surface must be low friction.
Function of Capillaries
There needs to be rapid exchange (diffusion etc) between blood and tissues hence the thin wall. They also link arteries and veins.
Function of Veins
Be able to pump blood to heart under low blood pressure. They do not stretch or recoil due to low bp. They act as a reservoir so have a large volume. Valves prevent the backflow of blood.
What is the ABO blood system?
A blood type classifying system dependent on A and B antigens/antibodies.
Type A Blood
Anti-B Antibodies
A Antigen
Type B Blood
Anti-A Antibodies
B Antigens
Type AB Blood
NO Antibodies
A Antigen and B Antigen
Type O Blood
Anti-A Antibodies and Anti-B Antibodies
NO Antigens
What is deemed as Universal Donor?
Type O Rh Negative blood is deemed as this.
Why is type O Rh-negative the "universal donor"?
It can be donated to all other blood types because it contains no A/B or rhesus antigens. This means that no antibodies will attack it and agglutinate the blood.
When is O Rh-negative blood used?
Only in ermegnecies as normally the patient will receive blood with same Rh and ABO group as their own.
What is the Rhesus System?
Classifies blood as Rh-positive or Rh-negative.
How is Rh-negative blood present in human?
An inherited blood protein is not present on Red Blood Cells.
How is the Rh negative (Rh-) different?
does NOT contain the protein and is RECESSIVE
Rh-Rh- = Rh-
What type of blood can Rh-positive people receive?
Rh-negative blood only.
What type of blood can Rh-negative people receive?
Only Rh-negative CANNOT receive Rh-positive blood.
Factors which can increase CVD
Diet
Smoking
Age
Inactivity
Genetics
High Blood Pressure
Diet
There is a correlation between dietary habits and CVD. Lipoprotein and salt levels, if high will impact cholesterol levels and cause fatty deposits.
Smoking
There is a correlation and causation between smoking and CVD as the chemicals cause damage to walls of arteries which causes them to constrict and lower blood flow.
Gender
Oestrogen in females offers protection from CVD. This is because it decreases LDL cholesterol levels (bad cholesterol). After menopause females face a higher risk as this protection is reduced.
Age
Older people lose elasticity and width of arteries which decreases blood flow to heart.
Inactivity
lack of physical activity and exercise will lead to an increased blood pressure. High bp causes the arteries to narrow as plaque builds up and blood flow is therefore reduced.
Genetics
Can inherit high bp, poor metabolism of cholesterol and easily damaged arteries. These all affect blood flow to heart.
High Blood Pressure
This should not be above 140 mm Hg systolic and 90 mm Hg diastolic. High BP will damage arteries and increase risk of CVD.
3 types of CVD Treatments
Anti-hypertensive (diuretics/ calcium channel blockers)
Statins
Transplantation and Immunosuppression
Positives of Anti-hypertensive (diuretics/ calcium channel blockers) treatments
It reduces Blood Pressure, reducing damage to arteries.
Positives of Statins
Reduces LDL as the enzyme is inhibited in the liver.
Positives of Transplantation and Immunosuppression
The heart is able to function properly.
Negatives of Anti-hypertensive (diuretics/ calcium channel blockers) Treatment
There side effects such as occasional dizziness, nausea and cramps.
Negatives of Statins
Tiredness, Sleeplessness, Nausea, Headaches, Weakness and Fatigue
Negatives of Transplantation and Immunosuppresion
Risk of rejection and these reduce immunity to other diseases so there is an increased risk of infection.
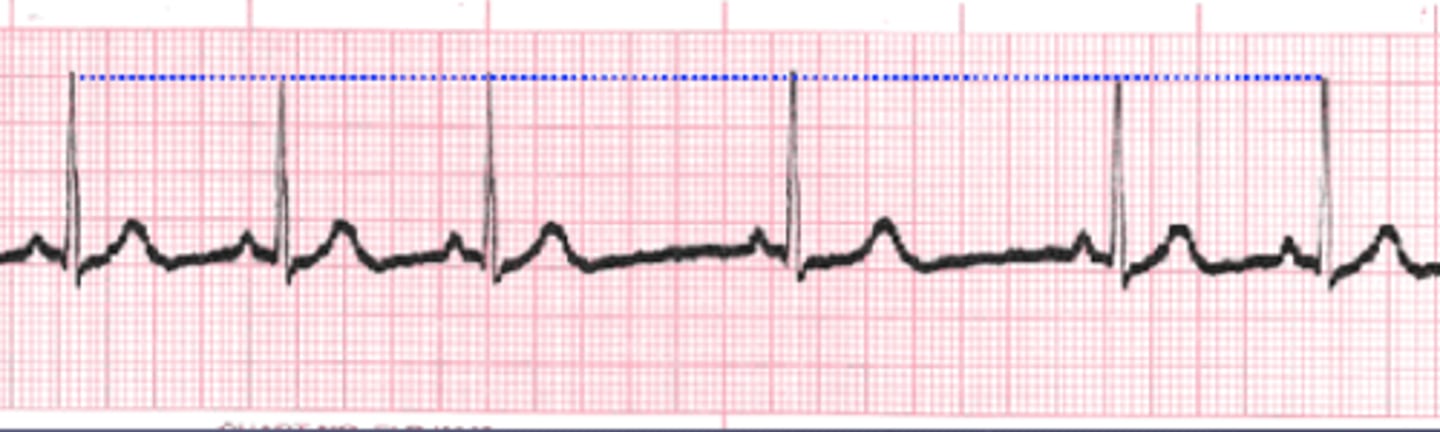
Electrocardiograms
These are tests that record the electrical activity of the heart and the results are published on a graph known as an electrocardiogram.
An abnormal reading means that CVD conditions or other heart problems can be diagnosed.
What are the parts of an ECG?
The P Wave
The QRS Complex
The T wave
The P Wave
indicates atrial depolarization in both left and right atrium. This means there is atrial contraction (atrial systole)
The QRS Complex
Includes The Q Wave, The R Wave and The S Wave
All 3 waves occur in rapid succession
This complex indicates that the myogenic impulse is travelling across the ventricles to initiate ventricular depolarisation (ventricular systole).
The T Wave
This indicates Ventricular Repolarization (Ventricular Diastole).
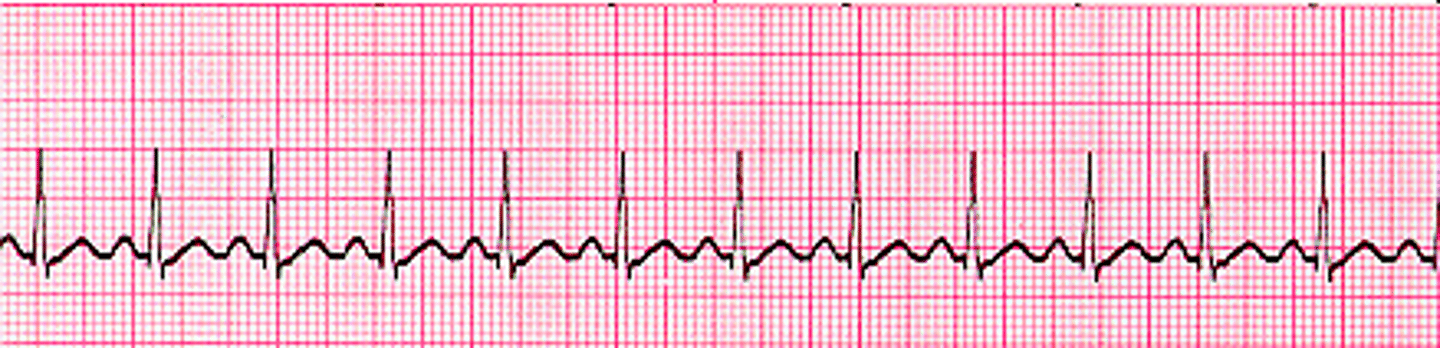
What is a normal rhythm of the heart?
60-100 bpm.
What is the bpm of Bradycardia?
less than 60 bpm.

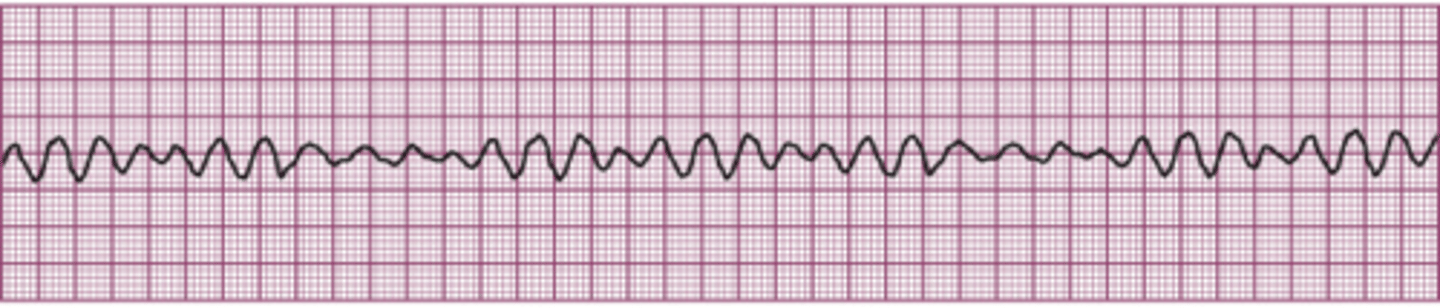
What is the bpm of Ventricular Fibrillation?
A very irregular ventricular rate.
What is the bpm of Sinus Arrhythmia?
Normal beats but they are triggered at irregular intervals.
What is the bpm of Tachycardia?
More than 100 bpm.
What happens in the practical?
Caffeine is added to Daphnia to observe the change in heart rate.
Why is caffeine used?
It is a known stimulant that may affect the heart.
Why are Daphnia used?
They are very abundant in supply
Are easily obtained
They are also easily transparent so the heart can be seen.
They have a simple nervous system so the ethical issues are low.
Why aren't humans used?
There is a complex nervous system
Needs dissection
Cannot kill for experiment
Can give consent
Ethical issues of using Daphnia
Simple nervous system
No dissection needed
Abundant in nature
Bred for fish food
CANNOT GIVE CONSENT
Limitations of using Daphnia
They are not humans, so any conclusions made, must be thoroughly considered before linking to humans.
What steps must be taken to ensure the experiment is successful?
The daphnia must be immobilised
All the variables must be controlled.
The heart rate must all be measured the same
Immobilise Daphnia Step
These needs to be done to ensure a successful experiment
Cotton wool submerged in a small dish of solution is used to trap Daphnia.
Controlling the Variables
Temp must be monitored to maintain it, this is done with a thermometer in the water.
The daphnia should all be the same size and age.
Ensuring that all the variables are controlled means that the experiment is repeatable.
Measurement of heart rate
Can be done by placing dots in paper in a S shape to avoid overlapping or repeatedly adding on a calculator.
Variables
Temperature
Age/size/sex of Daphnia
Aspects of pre-treatment (water type, habitat type, time out of habitat).
Safety Measures
Do not mix water and electric
Wash hands after handling daphnia.
What is the ideal temperature?
If the investigation is to investigate the effect of a substance (caffeine) the temp must be constant.
An unconstant temp could affect the heart rate.
25C is a suitable temp in this investigation as it ensures a high level of activity without enzyme denaturing.
Alveoli
The air sacs of the lungs in which the gas exchange of oxygen and carbon dioxide takes place ,this is through diffusion.
Co2 out of blood into alveoli to be exhaled.
O2 into blood for respiration.
Alveolar fluid surrounds the alveoli.
This is known as Pulmonary Surfactant which helps to reduce surface tension of alveoli. As well as maintain a moist surface to assist in diffusion.
The surface contains phospholipids which aid with this.
Pathway of Air into Lungs
Nose/Mouth
Pharynx
Epiglottis
Larynx
Trachea
Bronchi
Bronchioles
Alveoli
Pleural Membranes
A serous membrane that lines the rib cage.
Outer pleural membrane = lines outside of lungs.
The space between lungs and rib cage is filled with fluid, which reduces friction and increases lubrication.
The Pleural Membranes provide protection too.
These membranes allow the expansion of lungs without damage.
Features of the Gas Exchange System
Large Surface Area - 500-700 mil alveoli (70-100m2)
A thin gas exchange surface - one cell thick with squamous epithelium which assists diffusion.
A good blood supply - through the capillaries which allows efficient, continuous gas transfer.
It is important for continuous gas transfer to aid in maintaining the high conc. gradient of both gases.
The Concentrations of Gases (O2 and CO2)
In Alveoli
- High conc of O2 and a low conc of CO2
- O2 dissolves in moisture so moist surfaces of alveoli help this to happen.
In Blood
- Low conc of O2 in blood. This means that there is a conc grad. between blood and alveoli. So O2 diffuses from alveoli to blood. (high to low conc).
- High conc of CO2 in blood. So there is a conc grad. between blood and alveoli.
So CO2 diffuses down conc grad (high to low) from blood to alveoli.
Ventilation (Inhalation)
1. Diaphragm contracts and moves down to flatten.
2. If more O2 is needed then, the external intercostal muscles contract and move rib cage up and out to accommodate more O2.
3. The volume of the thoracic cavity increases.
4. An increase in volume causes a pressure decrease in the thoracic cavity which then is lower than outside.
5. Air then rushes in down a pressure gradient.
Ventilation (Exhalation)
1. Internal Intercostal Muscles contract and move the rib cage in and down.
2. The abs contract and push diaphragm back to dome shape.
3. The volume of thoracic cavity decreases.
4. A decrease in volume = increase in pressure compared to outside.
5. Air is forced out.
In Alveoli
- The elastic fibres shrink and increase pressure to force air out.
Mechanical Ventilation
The use of a mechanical ventilator to assist breathing.
Air is pumped into trachea through endotracheal or tracheostomy tube.
This increases pressure which then allows air to flow in.
The pressure drops to zero which allows lungs to exhale air.
A punctured lung - the effects
A hole in a lung would cause a hole in the thoracic cavity.
Air would enter the thoracic cavity and increase the pressure outside the lungs.
HOWEVER
The pressure would also increase in the lungs, so there is no pressure difference and air would neither flow in or out.
Spirometer
A device used to measure aspects of the lungs.
The patient breathes in and out of an airtight container which makes the device move up and down.
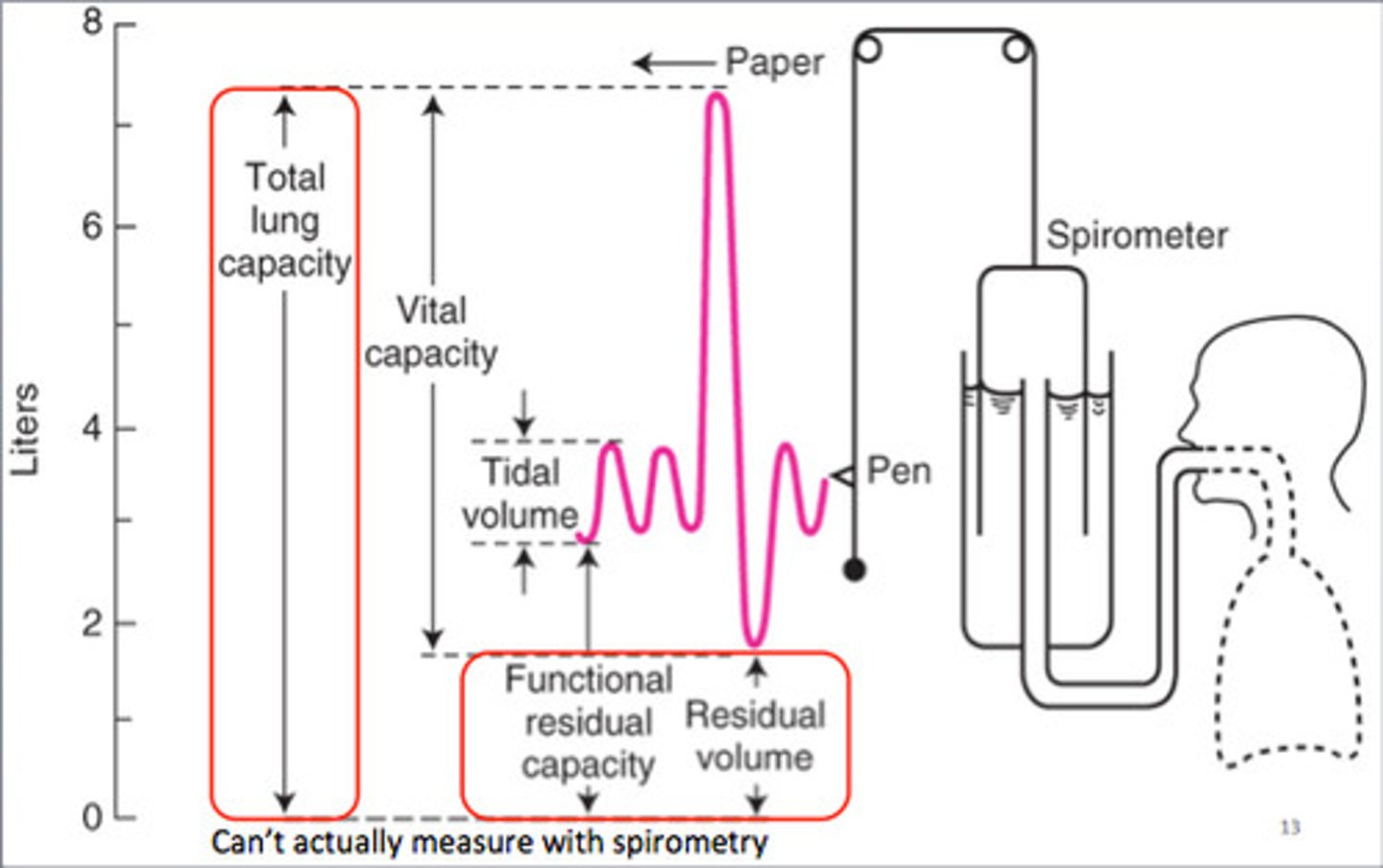
Parts of a spirometry graph
Tidal Volume
Expiratory Reserve Volume
Residual Volume
Vital Capacity
Total Lung Capacity
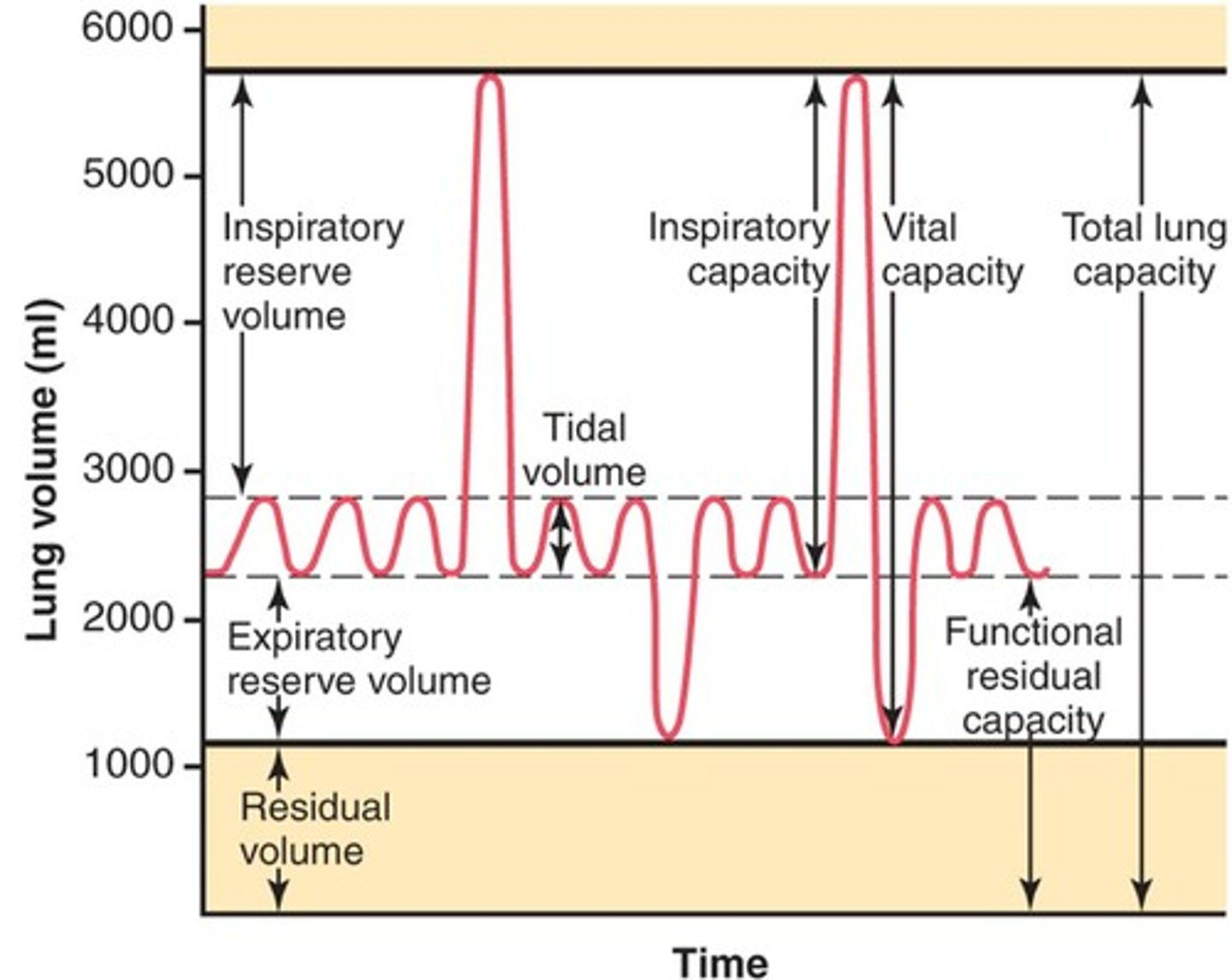
Tidal Volume (TV)
amount of air inhaled or exhaled with each breath under resting conditions
Expiratory Reserve Volume (ERV)
Amount of air that can be forcefully exhaled after a normal tidal volume exhalation
Residual Volume (RV)
Amount of air remaining in the lungs after a forced exhalation
Vital Capacity (VC)
The difference between the minimum and maximum volume of air in the lungs (TLC-RV).
So the volume between full inspiration (TLC) and full exhalation(RV).