EKG Interpretation
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
Atrial Rhythms
• Are not classic “P-wave” rhythms, if equal/consistent/nonvarying P-waves are easily identified then the rhythm is NOT atrial in origin
• Atrial rhythms are routinely fast
• Ventricular rates can be controlled (<100) or uncontrolled (>100)
• Ventricular responses and rates can reach up to 220 – 240 ppm
• Ventricular regularity can be regular or irregular, depending on the rhythm:
- AFib, WAP & MAT = ALWAYS IRREGULAR
- Aflutter = Regular or Irregular
- SVT/PSVT, ATach = ALWAYS REGULAR
• QRS-complexes can be Narrow (<0.12 sec) or Wide (>0.12 sec). This is measured using the ECG paper (<0.12 = less than 3 small boxes; <0.12 = greater than 3 small boxes)
Atrial Rhythms & Associated Rates
• A-Fib: Atria Rate >350 – 500; Ventricular Rate >220 – 240 ppm
• A-Flutter: Atrial Rate >250 – 450; Ventricular Rate >220 – 240 ppm
• Atrial Tachycardia: Atria > 220 – 240; Ventricular Rate = Atrial Rate (1:1 ratio)
• Supraventricular Tachycardia: >150 – 160 ppm, even upwards of 220 – 240 ppm; Ventricular Rate = Atrial Rate (1:1 ratio)
• Wandering Atrial Pacemaker (WAP): Atrial Rate <100 ppm; Ventricular Rate = Atrial Rate
• Multifocal Atrial Tachycardia (MAT): Atrial Rate >100 ppm; Ventricular Rate = Atrial Rate
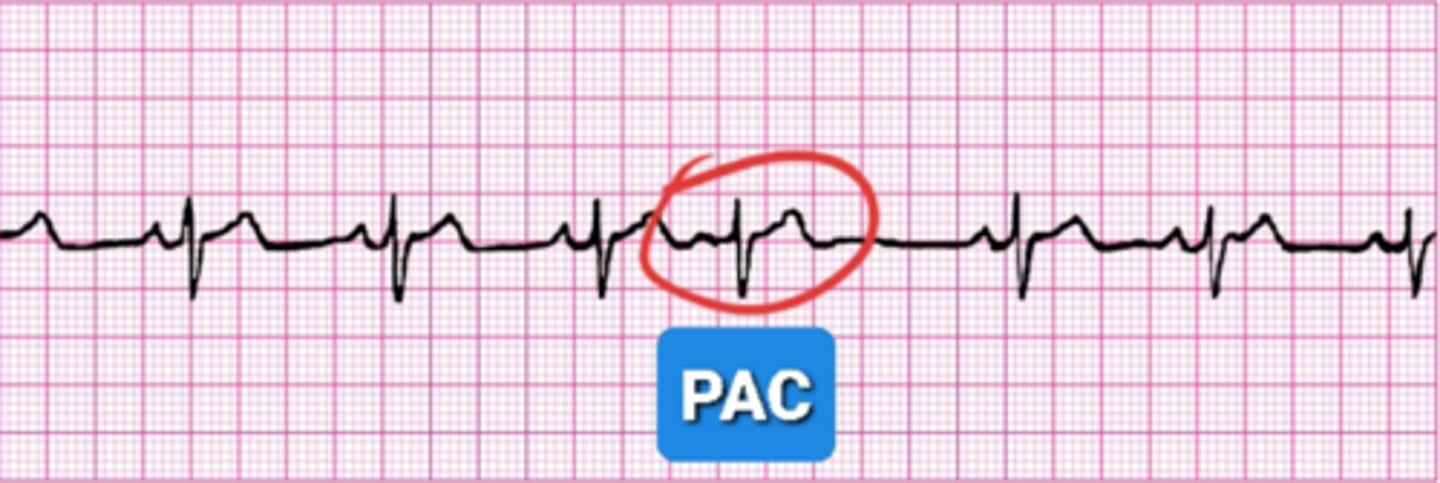
Premature Atrial Contraction (PAC)
Atrial ectopy (not a rhythm) similar to an ill timed hiccup within the atria, or the atria playing a game of interrupting cow.
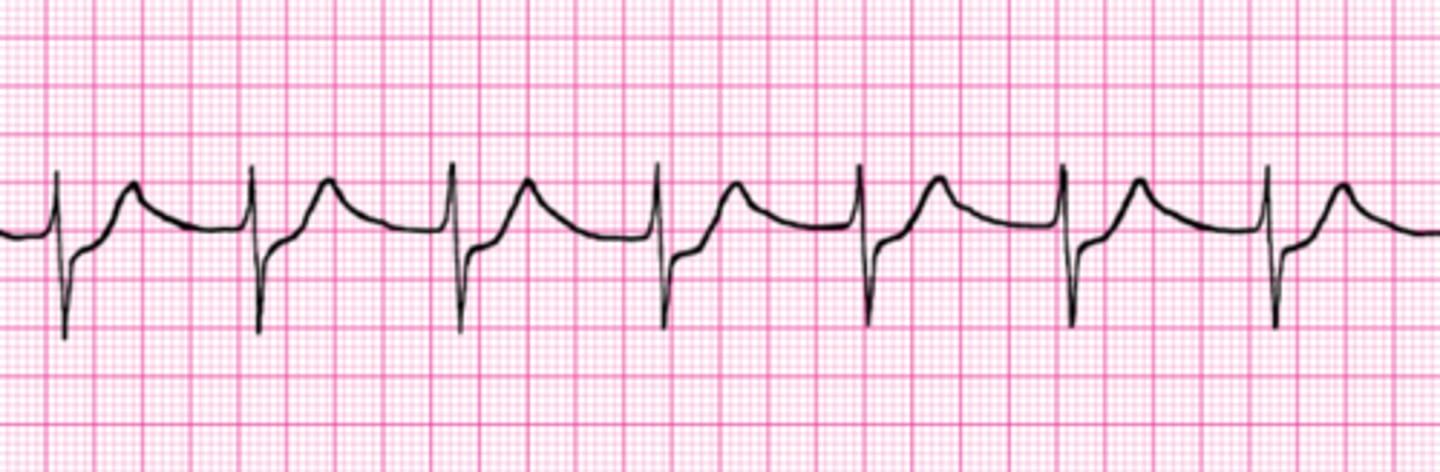
Atrial Fibrillation (A-Fib)
Wavy and chaotic baseline, noted overall irregularity, AFib QRS complexes can be 'wide' or 'narrow'
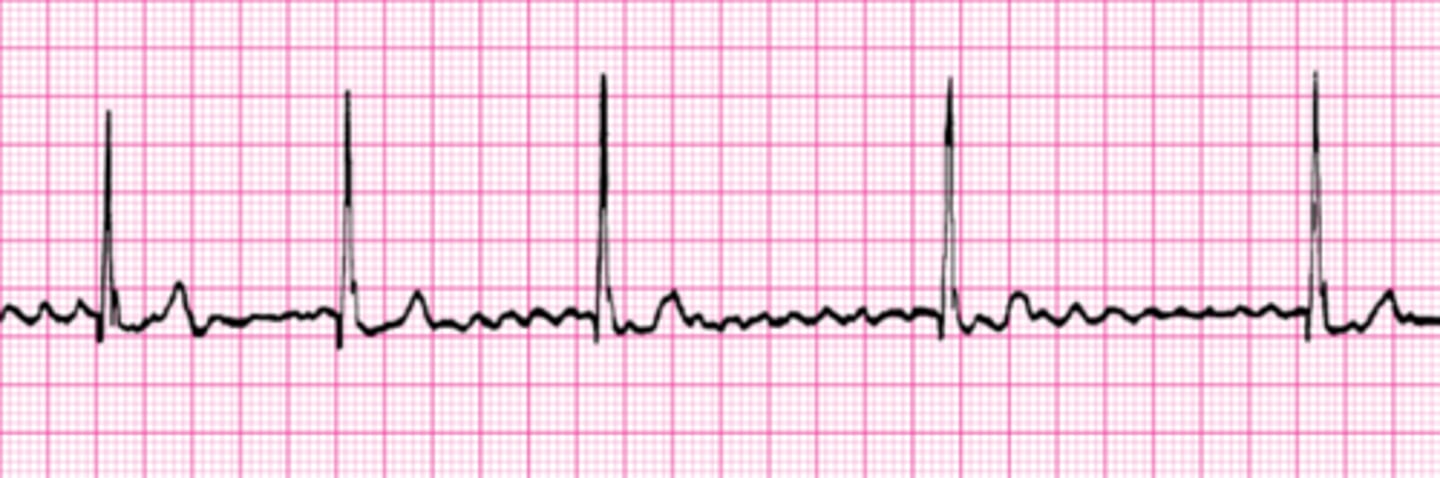
Narrow QRS Complex
<0.12 seconds (3 small boxes)
Wide QRS Complex
>0.12 seconds (3 small boxes)
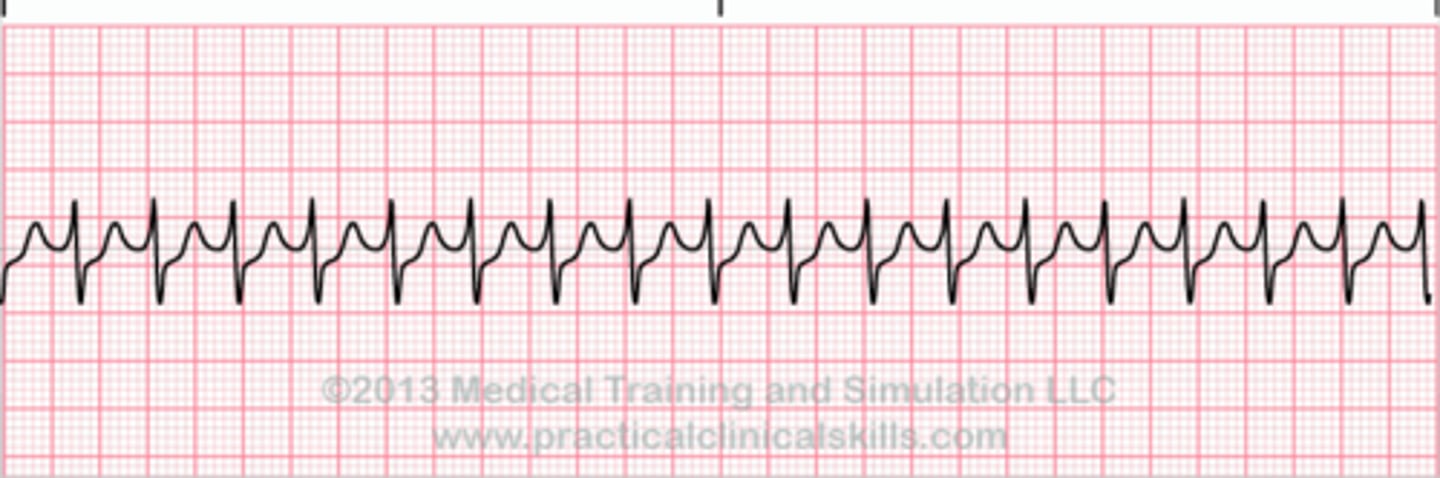
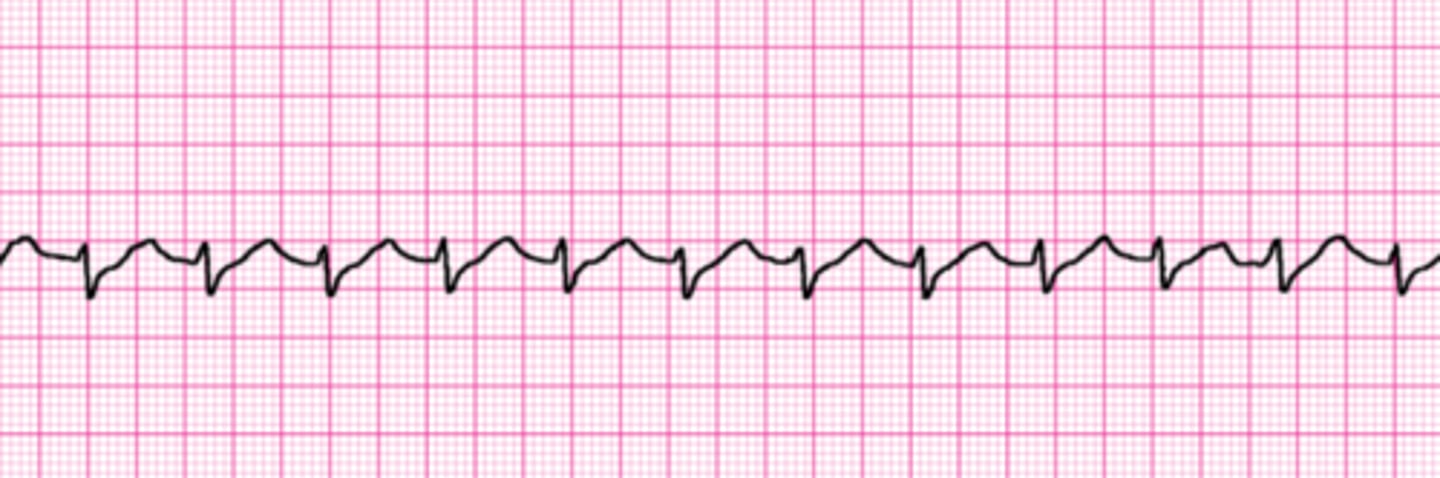
Atrial Flutter (A-Flutter)
Consistent atrial depolarization waves creating "flutter" or "saw-tooth" appearance on baseline.
Can be regular or irregular.
QRS complexes can be 'wide' or 'narrow'
Different ratios (2:1, 3:1, 4:1) possible

Atrial Tachycardia (A-Tach)
Atrial Tachycardia is caused when abnormal electrical signals inersect with signals coming from the SA node.
It can prevent the heart from filling normally and refuse the overall blood flow out of the heart due to rapid rate.
'Teeny-tiny' P's noted, FAST rate, narrow complexes and REGULAR

Supraventricular Tachycardia (SVT)
Abnormal heart rhythm arising from aberrant electrical activity in the heart; originates at or above the AV node
No P's noted, FAST rate, narrow complexes and REGULAR
Multifocal Atrial Tachycardia (MAT)
3 or more varying P-Waves, overall irregular and rate is >100 ppm. Note the DIFFERENT P’s presented.
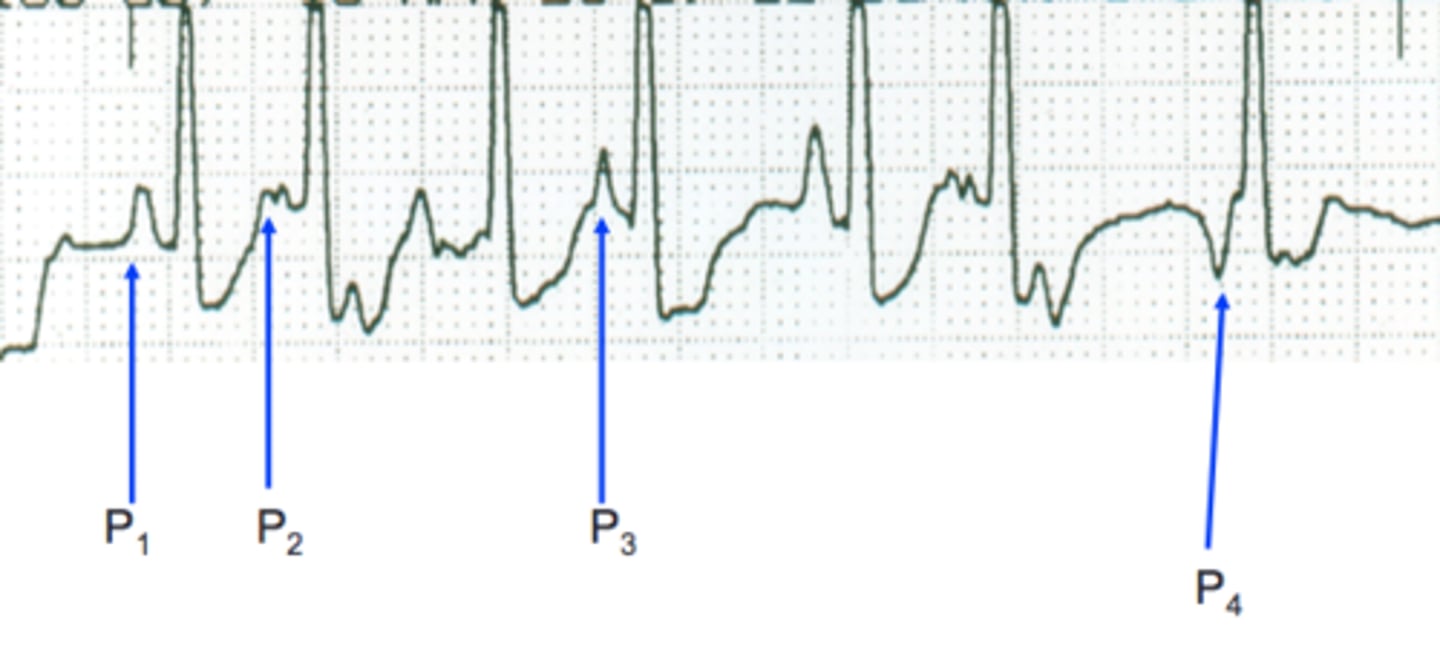
Wandering Atrial Pacemaker (WAP)
3 or more varying P-Waves, overall irregular and rate is <100 ppm. Note the DIFFERENT P’s presented.

Heart Block Key Points
• 1st Degree - PRI is > 0.20sec and 1:1 (P-wave for every QRS-complex)
• 2nd Degree Type I – PRI will INCREASE, QRS’s will drop. Remember phrase: “Going…Going…Going…Gone!”
• 2nd Degree Type II – PRI will remain CONSTANT and QRS’s will drop.
• 2nd Degree High Grade Block – Repetitive QRS complexes are dropped.
• 3rd Degree (Complete Heart Block) – Occurs when impulses are not received from the atria into the ventricles. Atria and ventricles will each depolarize at individual rate
***RATES CAN VARY FOR EVERY TYPE OF BLOCK***
Heart Block Rhythms
When interpreting Heart Blocks, the P-wave is always present which means the Sinus Node is “firing”, so the underlying rhythm is typically “Sinus” in nature. In order to identify a “Heart Block”, find the P-waves! Heart block degree is based on the location of the P-waves and their relationships to the following QRS-complexes and their consistency.
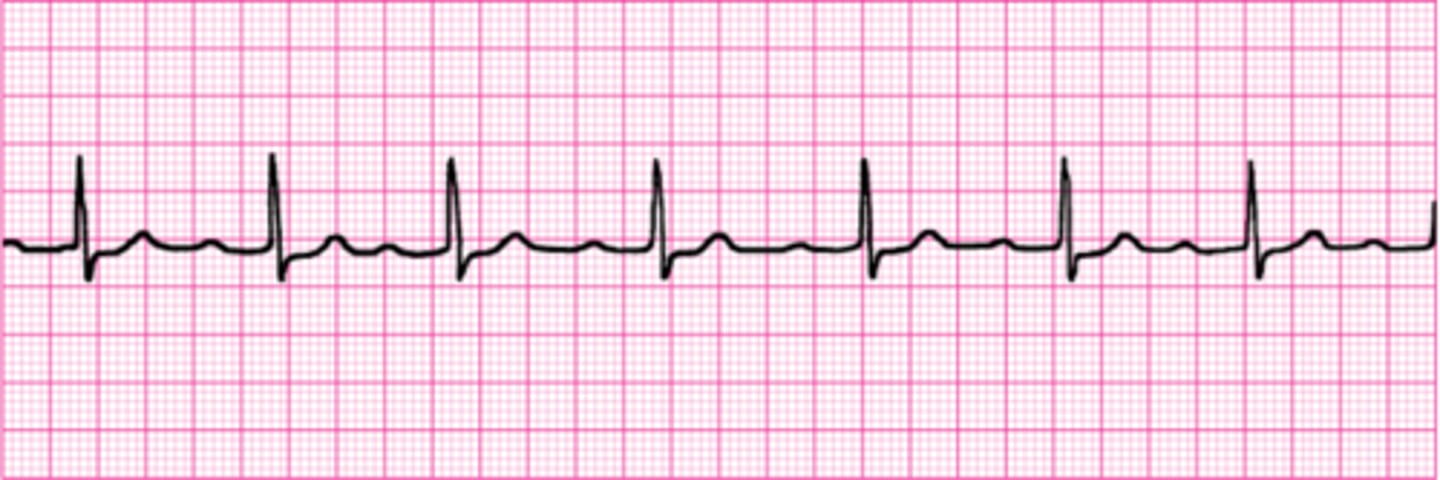
1st Degree Heart Block
Actually only a “delay” so all waves are present on the strip. With a 1st Degree AV Block, there is a P-wave for EVERY QRS-complex. Thus, nothing is “missing” and the PRI is consistently >0.20sec (5 small boxes) as measured on the ECG/EKG paper. Remember, the PRI WILL NOT CHANGE!
2nd Degree Type I Heart Block
Missing QRS-complexes. The PRI will increase, resulting in a "dropped" QRS-complex. The PRI will reset and the process will start all over again. Remember the following phrase: "Going...Going...Going...Gone..." and this will help you remember the process of a 2nd Degree Type I (Wenckebach or Mobitz I). Remember the PRI CHANGES!
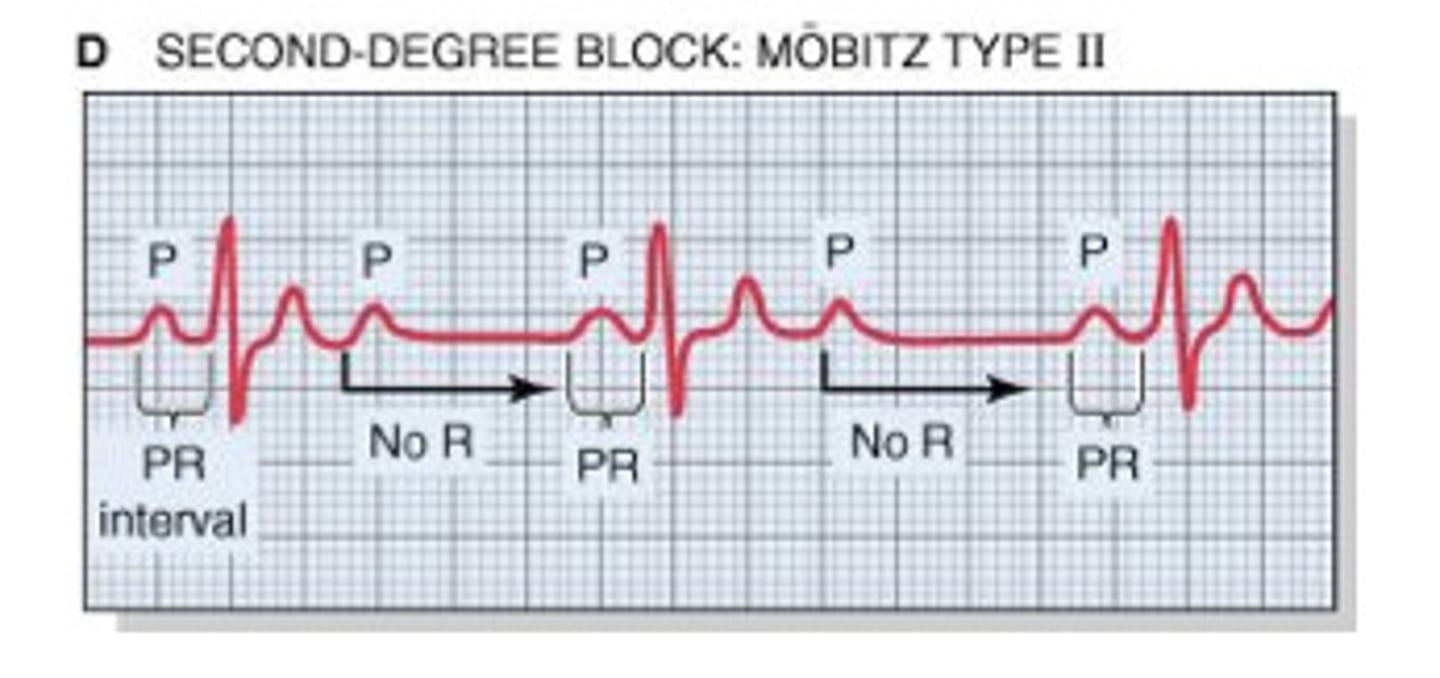
2nd Degree Type II Heart Block
Dropped QR complexes with the PRI remaining CONSTANT. PRI's will remain overall consistent and QRS-complexes are repeatedly drop from the rhythm. Defining characteristic of this heart block is that the PRI WILL NOT CHANGE!
2nd Degree High Grade Heart Block
2nd degree heart block becomes “high grade” when multiple QRS’s are consistently missing from the rhythm. These ratios are given when interpreting and documenting a 2nd High Grade Block:
• 2:1 - 2 P-waves for every QRS-complex present
• 3:1 - 3 P-waves for every QRS-complex present
• 4:1 - 4 P-waves for every QRS-complex present and so on…
Junctional Rhythm
The SA node is nonfunctional, P waves absent, inverted, or follow QRS's.
• Usually slow
• QRS-complexes can be narrow (<0.12 sec) or wide (>0.12 sec).
Junctional Rhythm Rates
• Junctional Escape: 40 – 60 ppm
• Junctional Bradycardia: < 40 ppm
• Accelerated Junctional: 60 – 100 ppm
• Junctional Tachycardia: > 100, upwards of 130 to 140 ppm
Automaticity
•Ability of pacemaker cells to initiate electrical impulse independent of external stimulation.
•Increased electrolytes decrease automaticity
•Decreased K+ and Ca++ in blood increase automaticity
Exitability "irritability"
Ability of cardiac cells to respond to outside stimulation.
Junctional Bradycardia
HR = 38
No apparent P-waves

Accelerated Junctional Rhythm
HR = 71
No apparent P-waves
Junctional Tachycardia
R = 125
No apparent P-waves
Sinus Rhythms
• Rhythms that originate in the SA node
• Upright & Consistent P-waves
• P-waves remain identical (except premature complexes)
• PRI remains constant (0.12 – 0.20 Seconds, or 3 – 5 small boxes on ECG paper)
• 1 P-wave for every QRS-complex (1:1 ratio)
• R to R (QRS to QRS) is typically regular, meaning at equal intervals. Only variations would be for premature/delayed complexes, sinus arrhythmias, or pauses of the SA Node
• QRS-complexes can be Narrow (<0.12 sec) or Wide (>0.12 sec). This is measured using the ECG paper (<0.12 = less than 3 small boxes; <0.12 = greater than 3 small boxes)
• Exception are pauses of the SA node. Sinoatrial Blocks and Sinoatrial Arrests occur, but do not change the underlying sinus rhythm.
Sinus Rhythm Rates
• Normal Sinus Rhythm: 60 to 100 ppm
• Sinus Bradycardia: <60 ppm
• Sinus Tachycardia: >100 ppm (up to 150 – 160, even as high as 180)
• Sinus Arrhythmia: fast or slow, bradycardic, normal, or tachycardic rates. The R to R (from QRS to next QRS) changes in rates typically due to cardio-respiratory response. However, there are instances where this is not respiratory related.
• Sinoatrial Block: rates vary; but periodically PQRS-T complexes are ‘dropped’, but resume normally/on time
• Sinoatrial Arrest: rates vary; but periodically PQRS-T complexes are ‘dropped' but resume at unpredictable intervals
Normal Sinus Rhythm
Ventricular rate: 60-100

Conduction
Ability of a cardia cell to receive and relay an electrical signal
Contractility
Ability of cardiac muscles to contract the heart
Phases of cardiac cellular conduction
Polarized- cells are charged with energy
Depolarized- cells are discharging energy and causing physical contraction
Repolarization- cells are recharging
Electrical conduction of the heart
SA Node --> AV Node --> Bundle of His --> Purkinje Fibers --> Contraction of ventricles
(Stab A Big Pickle)

PPM
Paces per minute
Cardiac output cannot be determined by conductivity, hence "BPM" is incorrect when referring to rates
Bundle branches
DO NOT produce any rhythms, are only the "power lines" between AV and Purkinje fibers
SA node
Pacemaker of the heart
Relays electrical impulses from atria into ventricles
Inherent rate 60-100ppm
Creates P-wave
AV node
Gatekeeper of electrical impulses
Speed bump function, can hold onto electrical impulses to control a rate when SA node fires too quickly
Backup pacemaker; can take over if SA node fails
Inherent rate 40-60ppm
Purkinje fibers
Tertiary pacemaker
Inherent rate <40ppm
Can only sustain cardiac output for short time
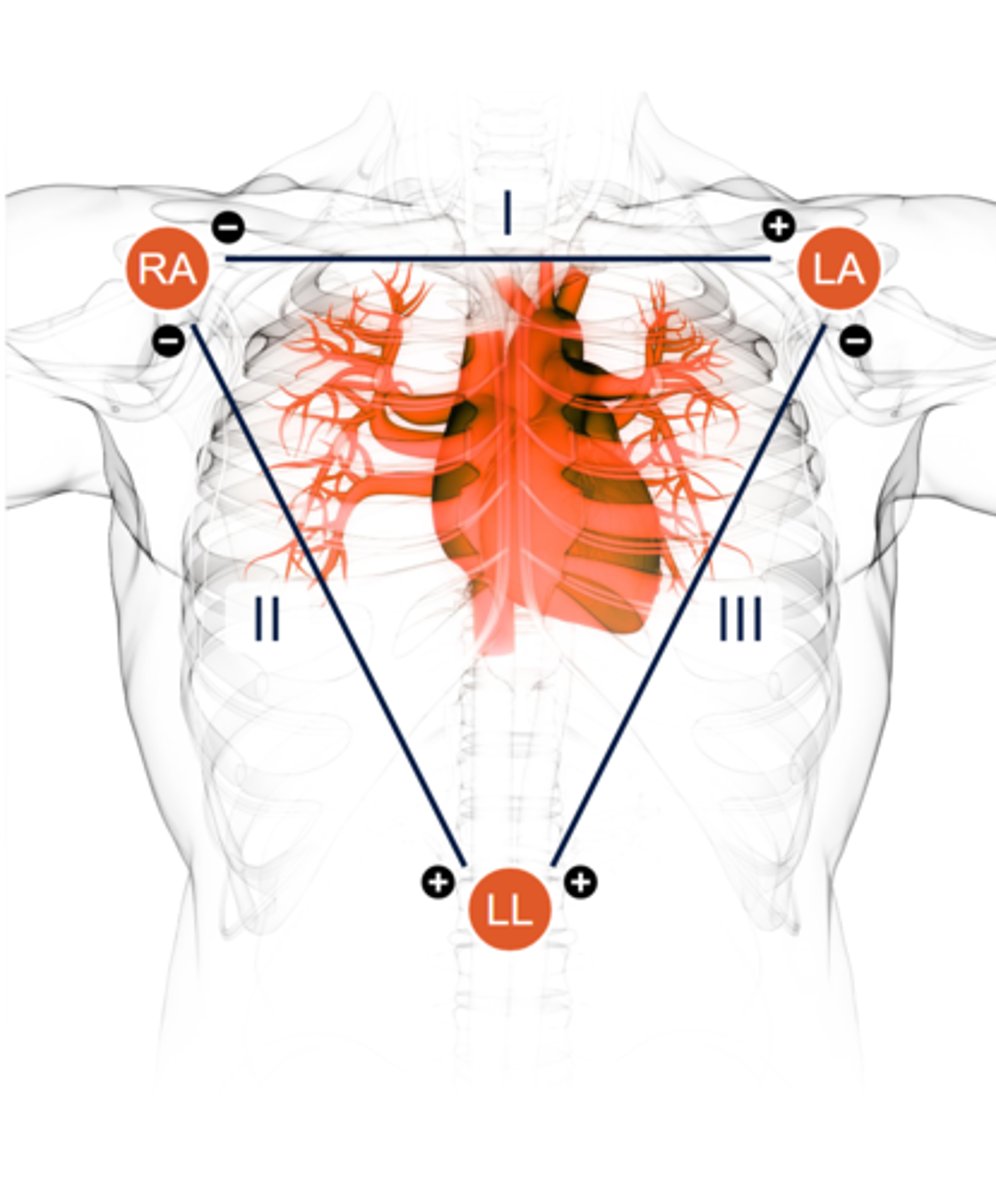
Eintoven's Triangle
Based on triangle formed with LA, RA, LL 9red, black, and white)
Triangle is the basis for limb lead tracings (I, II, III, aVR, aVL, and aVF)
Each lead tracing is bipolar, one positive and one negative
Shows frontal plane of cardiac conduction
Lead Placement Prep
Clean with soap and water if possible
Do not place on bony prominences if possible
If you need to shave, you need to shave!
Alcohol dries the skin AND electrode leading to low quality read
Floating lead
Brown lead (chocolate in your heart)
Traditional placement is right 4th intercostal space
Small EKG box
0.04 seconds
Large EKG box
0.2 seconds
5 Large Boxes
1 second
15 Large Boxes
3 seconds
Sometimes demarked by tic marks
300 Large Boxes
1 minute
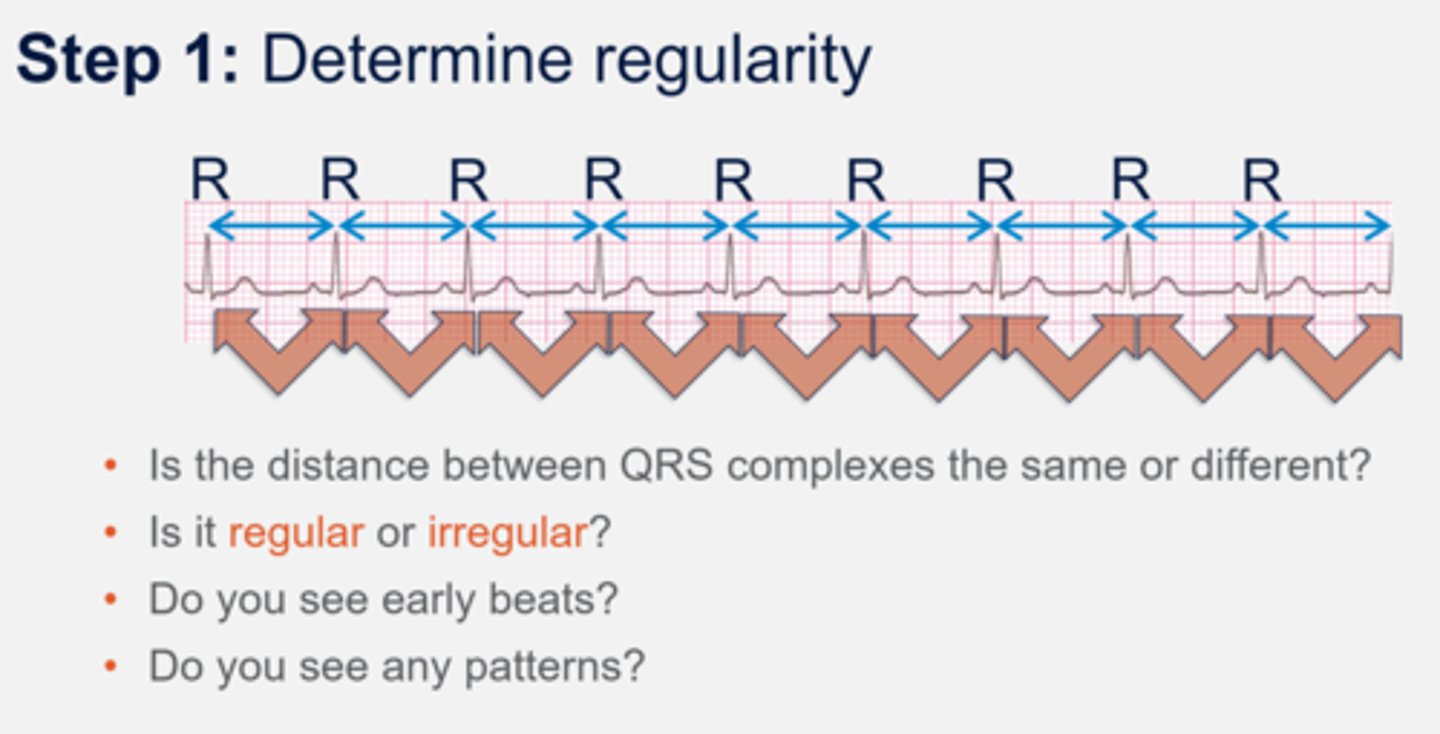
Regular rhythm
Measure the intervals between P to P waves or R to R waves
If the intervals vary by less than 0.06 seconds or 1.5 small boxes, we can consider the rhythm to be regular
Baseline
Represents resting cardiac potential -90mV
Line is most visible when patient is in asystole
P wave
Atrial depolarization (contraction)
Normally from SA node
Usually rounded but can appear pointed, notched, or even biphasic (above and below baseline)
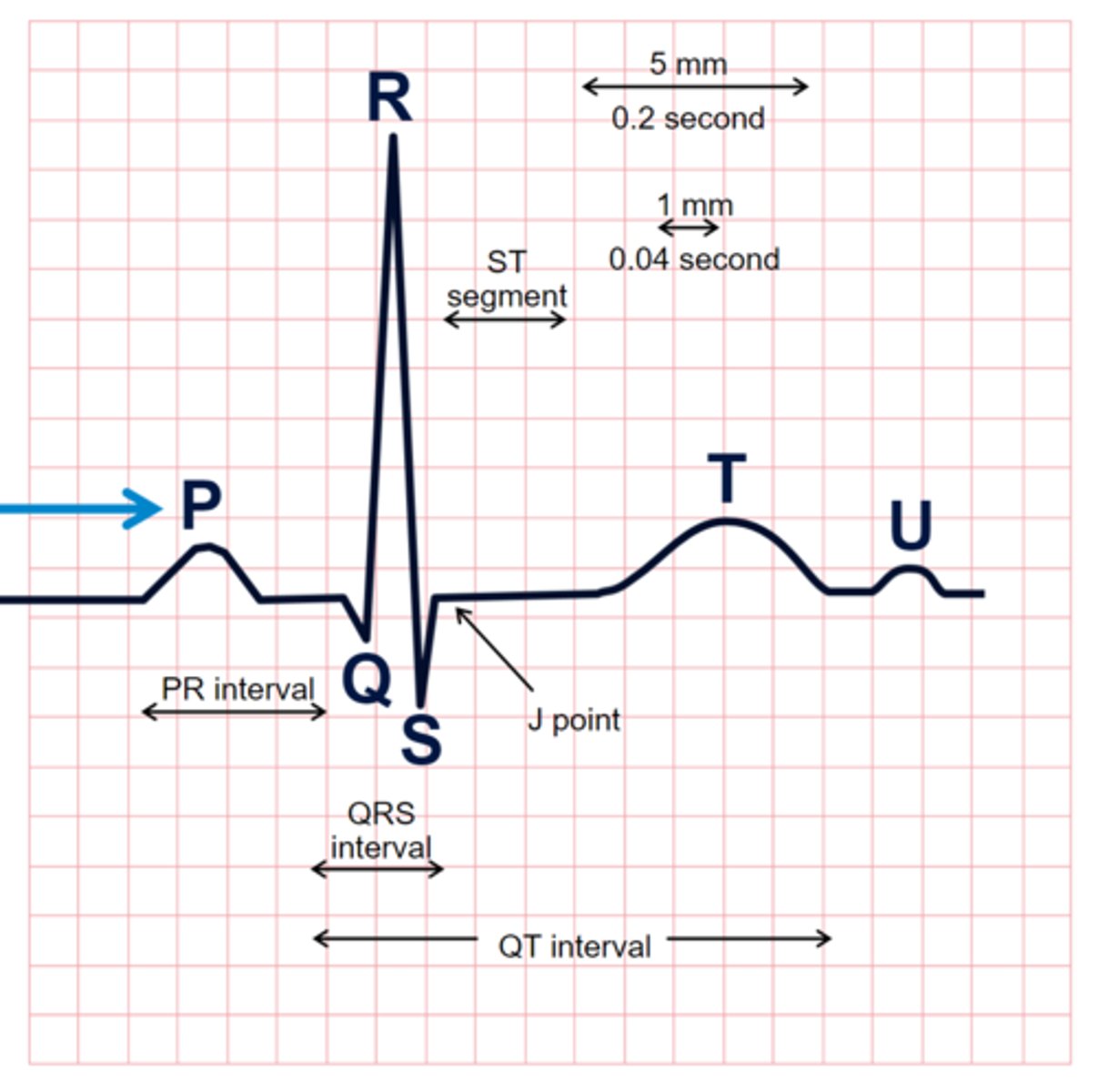
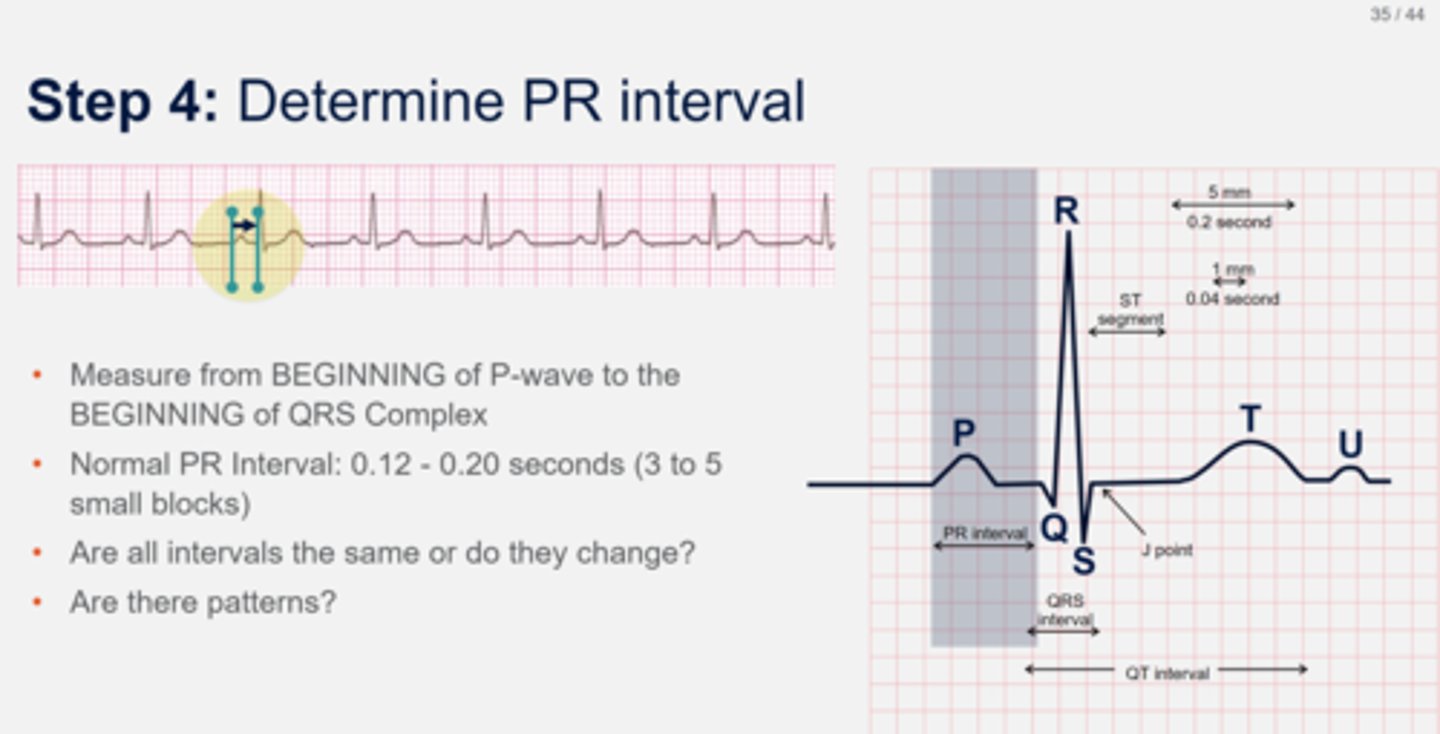
PR interval
Measurement from beginning of P wave to beginning of QRS complex
Normally 0.12-0.20 seconds (3-5 small boxes)
Q wave
First negative deflection of QRS
R wave
First positive deflection of QRS
S wave
First negative deflection after R wave
QRS complex
<0.12 seconds
Even if waves are missing, still referred to as QRS complex
Only complex with straight lines
ST segment
Early stage of repolarization
Measured J point to beginning of T wave
Usually 0.04 seconds (one small box)
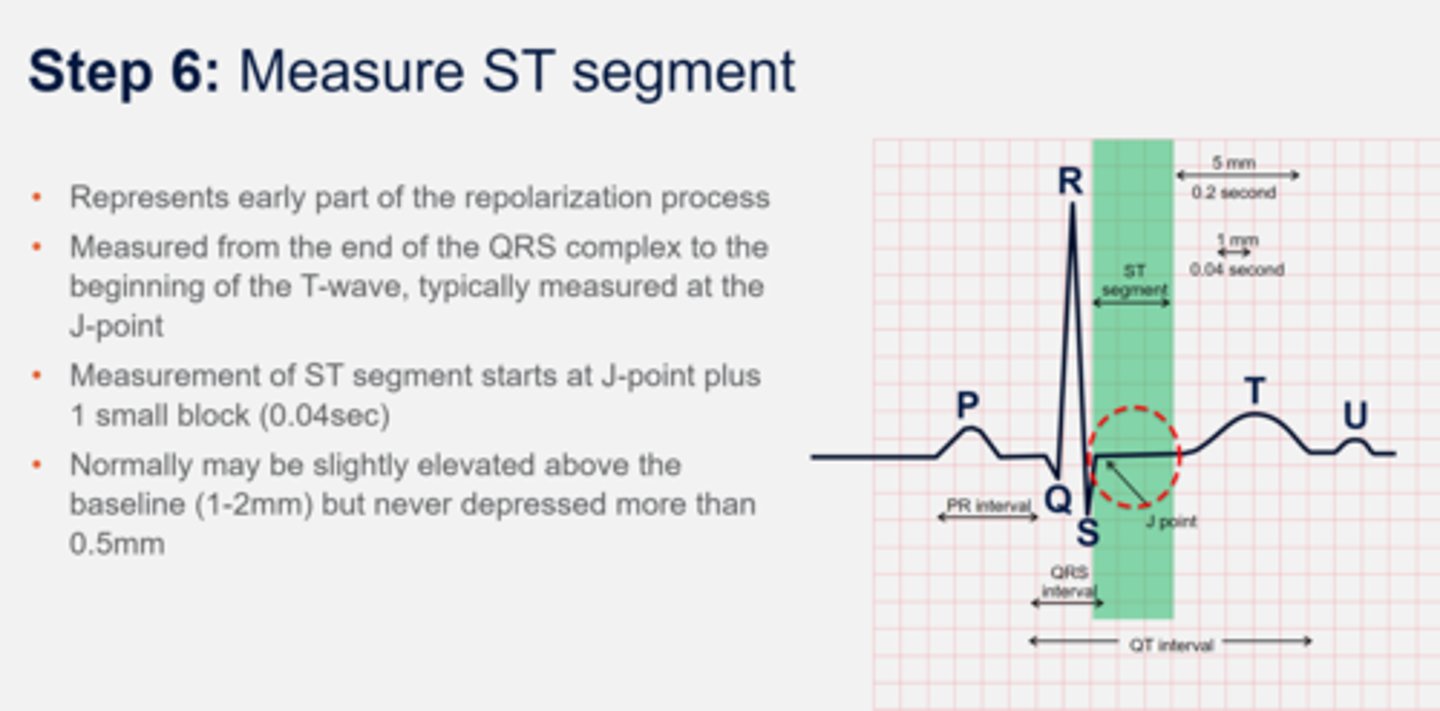
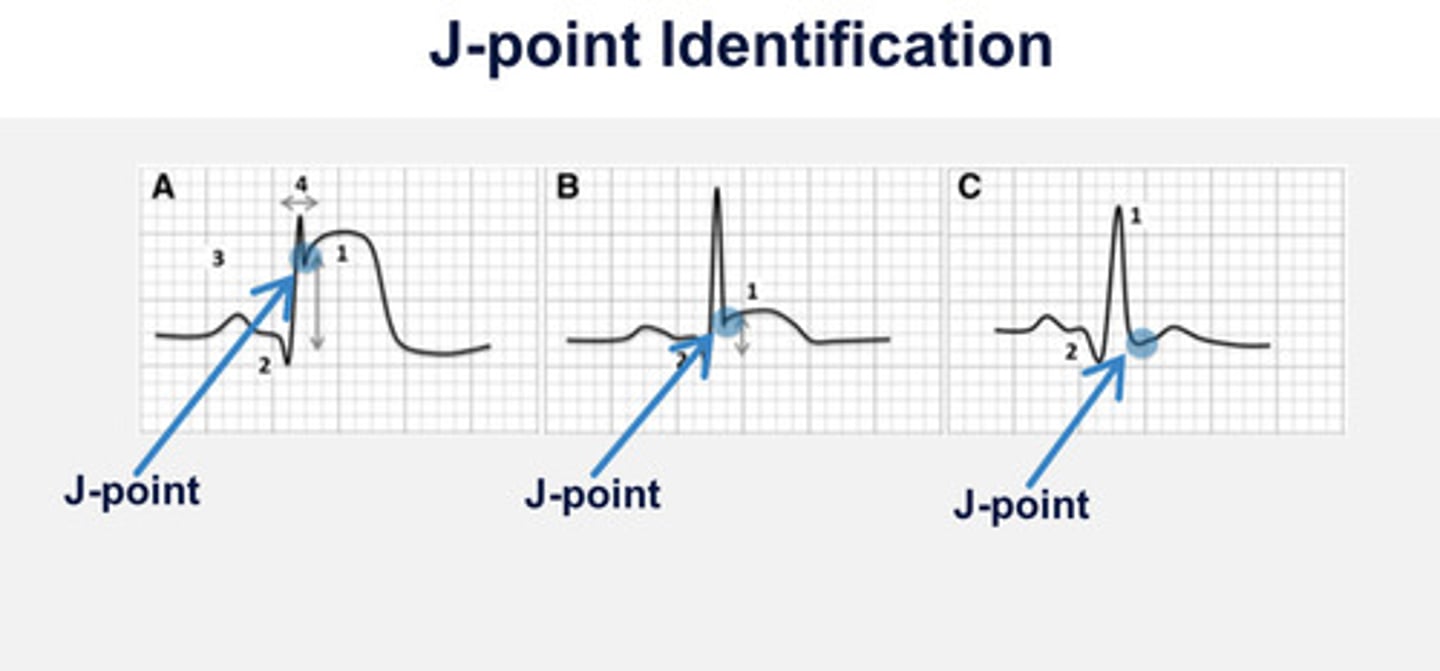
J point
Junction between end of QRS complex and start of ST segment
T wave
Ventricular repolarization and relaxation
Should be pointing in same direction as QRS complex whether positively or negatively deflected
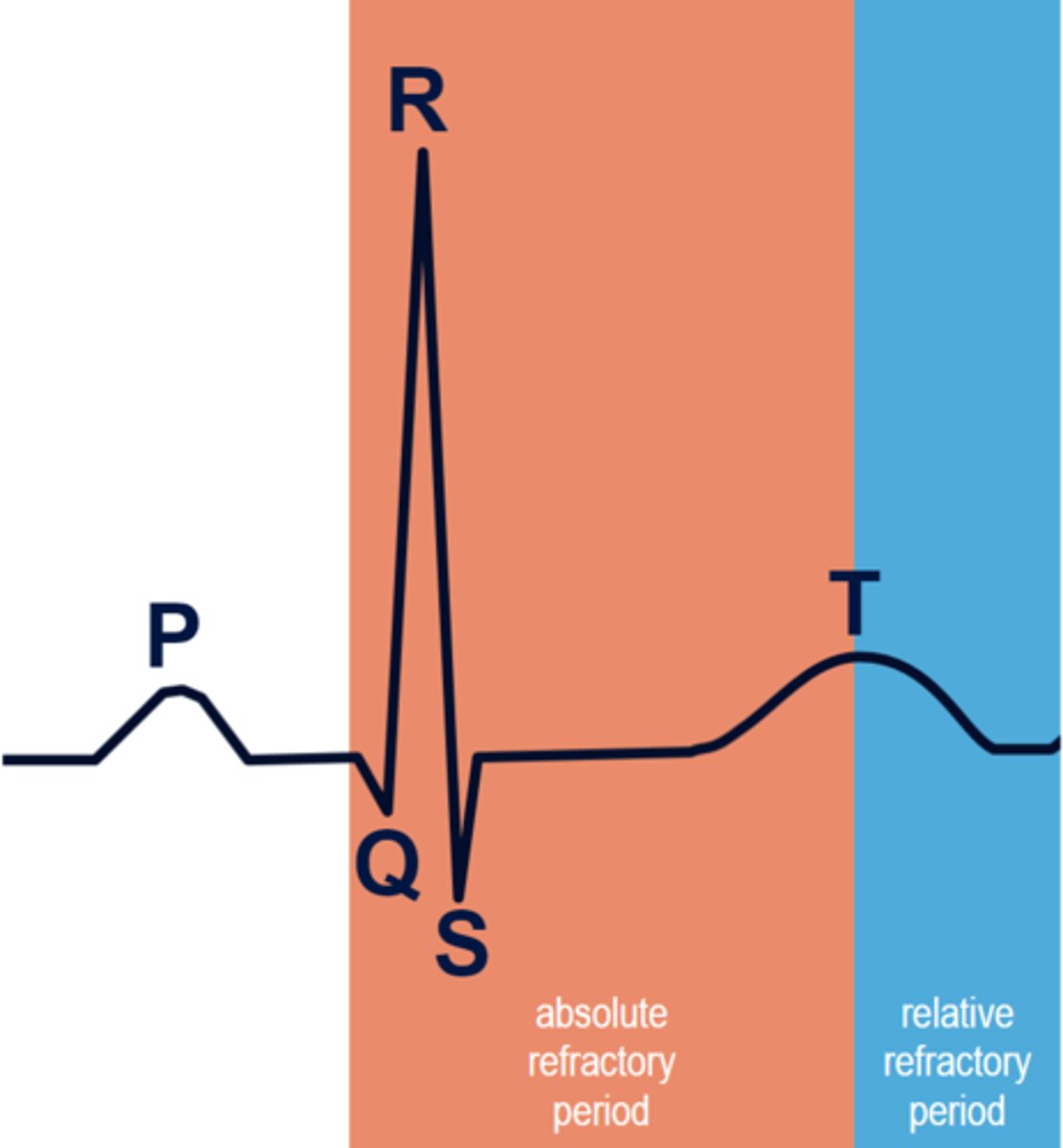
QT interval
Refractory period
Measures from beginning of QRS to end of the T wave
Normally 0.44 seconds or half of the R-R interval (can change based on age and gender)
The longer the QT, the greater chance of ventricular depolarization during ventricular repolarization, resulting in chaotic and lethal rhythm such as Torsade's
QTc interval
Measure of time between start of Q wave and end of T wave in cardiac cycle
Absolute Refractory Period
"Safe zone
Cells cannot be stimulated to conduct an electrical impulse, no matter how strong
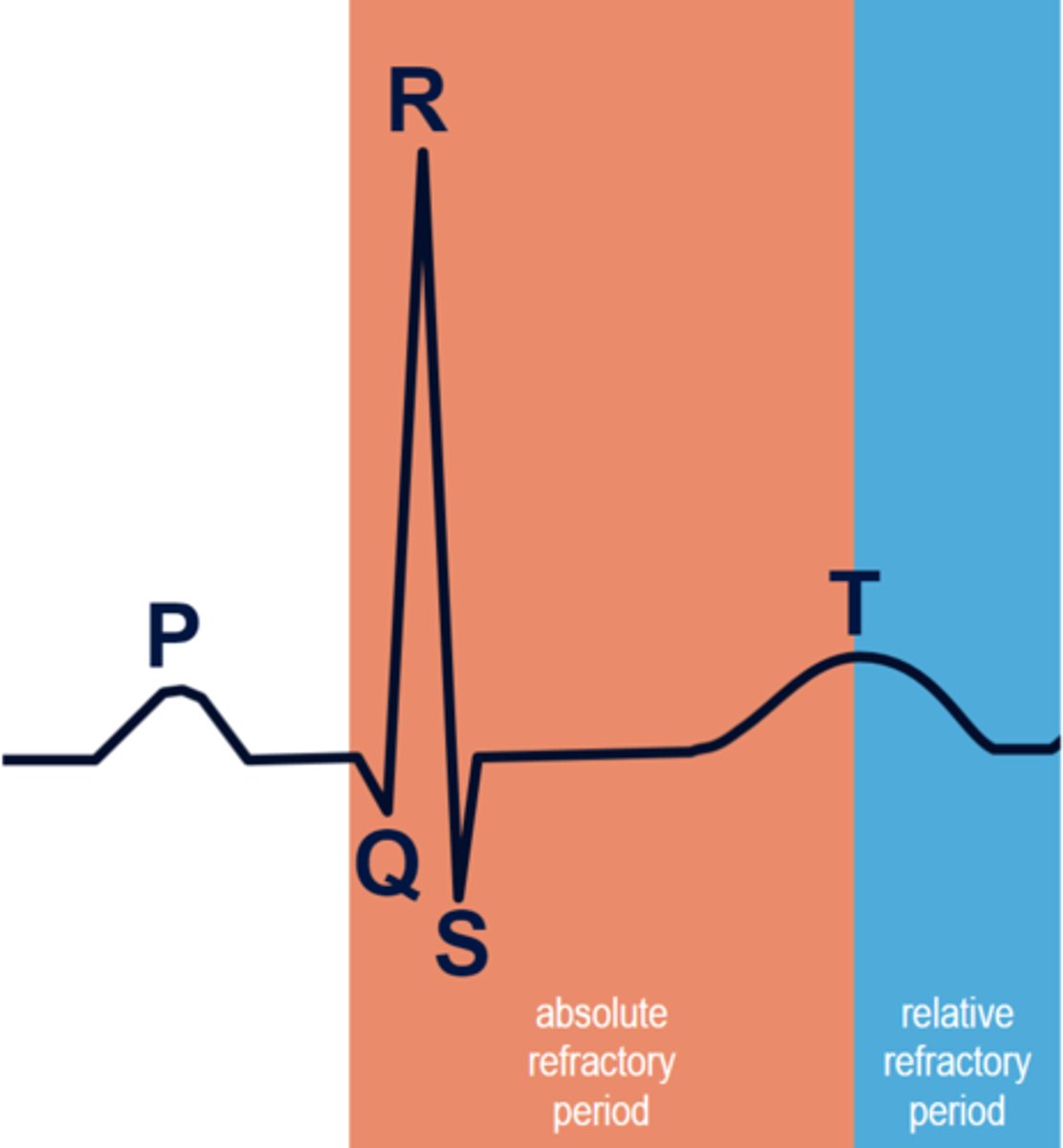
Relative Refractory Period
Danger zone
Cardiac cells can be stimulated to depolarize if the stimulus is strong enough
This is why cardioversion has a sync button to time the shock exactly; shocking during RRP could cause a patient to go into V-fib a lethal rhythm
U wave
Associated with bradycardic rhythms and hypokalemia
Delayed repolarization of Purkinje fibers
Same direction as T wave
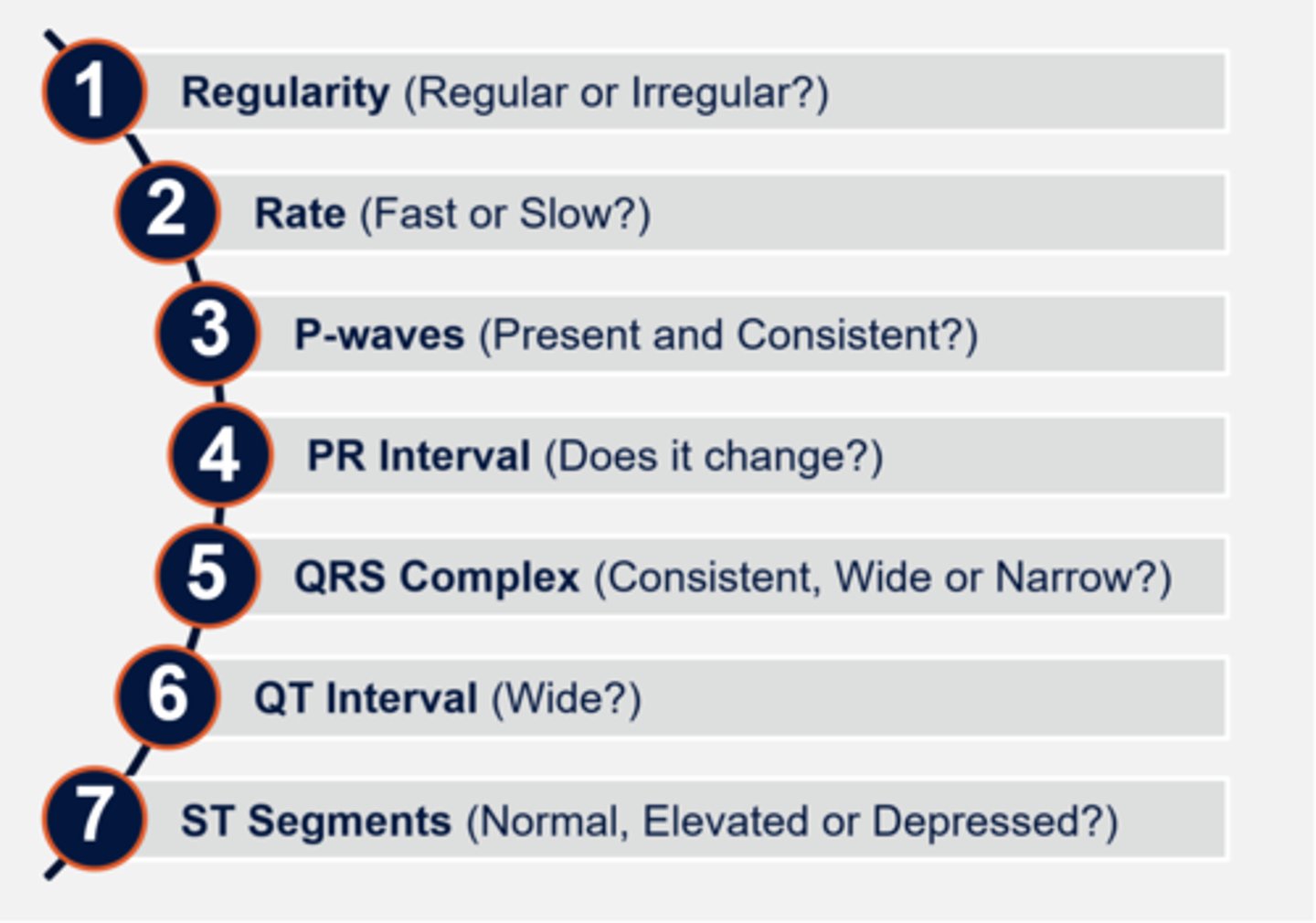
7 Step Interpretation
Regularity
Rate
P waves
PR interval
QRS complex
QT interval
ST segments
1500 Method
Count number of small squares between two consecutive R-waves and divide that number by 1500
Most accurate only if regular rhythm
P-P Interval
Used to determine atrial rate and regularity
Measure from beginning of one P wave to the beginning of the next
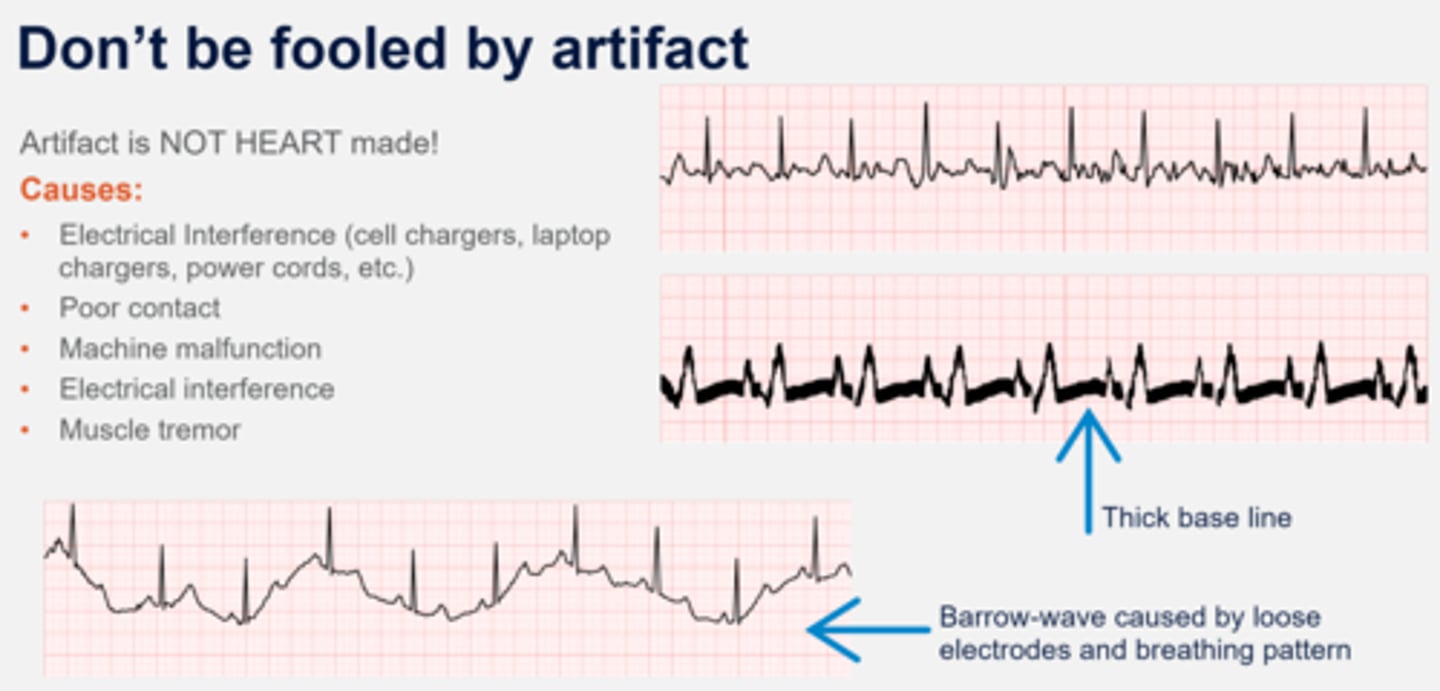
Artifact
Readings produced by external activity rather than cardiac electrical current
J-Point
Point where the QRS complex and ST segment meet