Animal Reproduction - Embryogenesis and Development of the Reproductive System
1/71
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
_______ sex determines _______ sex determines __________ sex.
Genetic, gonadal, phenotypic.
external features of reproductive system
external genitalia and secondary sex characteristics.
internal features of reproductive system
urogenital system.
central nervous system components of reproductive system
pituitary gonadotropin secretion and sexual behavior.
female sex chromosome
XX
male sex chromosome
XY
which chromosome determines sex of the offspring?
Y chromosome
zygote
a diploid cell resulting from the fusion of two haploid gametes.
which chromosome is bigger?
X chromosome, contains 3 times as many genes.
SRY gene
sex determining region of the Y chromosome.
genotypic sex determination
sex is determined genetically by the chromosomes.
temperature-dependent sex determination
sex is determined by egg incubation temperature.
embryogenesis
the formation and development of an embryo.
blastocyst
stage of early development in mammals that consists of a hollow ball of cells.
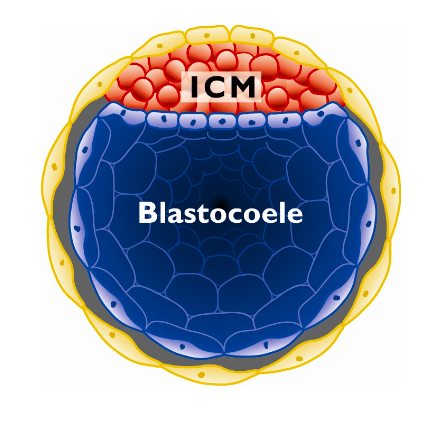
inner cell mass
solid clump of cells in the blastocyst that becomes the embryo.
trophoblast
outer layer of blastocyst that becomes the placenta.
when do cells begin to differentiate?
early blastocyst stage.
morula
ball of 16-32 cells.
what is produced when the two nuclei of the gametes fuse (karyogamy)?
zygote.
what are the three germ layers that the inner cell mass differentiates into during early embryogenesis?
ectoderm, mesoderm, endoderm.
ectoderm
outer germ layer; develops into nervous system, skin, external genetalia, and hair.
mesoderm
middle germ layer; develops into muscle, skeleton, cardiovascular and reproductive system.
endoderm
inner germ layer; develops into digestive system, lungs, and endocrine system.
what two germ layers develop into the entire reproductive system?
mesoderm (internal reproductive system), and ectoderm (external genitalia, hypothalamus, and pituitary).
pituitary gland
endocrine gland at the base of the brain that releases gonadotropins (FSH and LH).
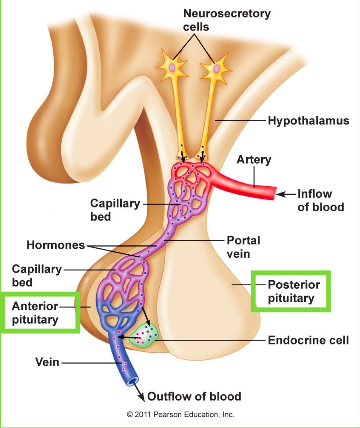
hypothalamus
structure in the brain that triggers the pituitary gland through the release of gonadotropin-releasing hormone (GnRH).
hypophysis
another name for the pituitary gland.
posterior pituitary (neurohypophysis)
derived from neural ectoderm tissue of the brain floor. stores and secretes hormones.
anterior pituitary (adenohypophysis)
derived from ectoderm tissue in the roof of the embryonic mouth. synthesizes and secretes hormones.
the pituitary is derived from which two types of ectoderm tissue?
neural and oral.
hormones secreted by posterior pituitary
oxytocin (milk production) and ADH (antidiuretic hormone).
hormones secreted by anterior pituitary
LH, FSH, PRL, GH, TSH, ACTH.
diverticulum (pituitary)
a sac diverting from a main tube/cavity.
infundibulum (pituitary)
the diverticulum of the brain floor that forms the posterior pituitary.
Rathke's pouch (pituitary)
the diverticulum of the roof of the mouth that forms the anterior pituitary.
how is the pituitary developed?
the infundibulum stretches down towards the Rathke's pouch, which pinches off and regresses from the roof of the mouth when meeting. the two are joined by connective tissue and are then protected by the surrounding developing sphenoid bone at the base of the skull.
sella turcica (turkish saddle)
saddle-shaped depression in the sphenoid bone that protects the pituitary.
hypophysectomy
removal of the pituitary gland.
primordial germ cells (PGCs)
the common origins of spermatozoa and oocytes.
where are PGCs found?
the base of the handgun (near the yolk sac), and migrate up to the genital/gonadal ridge through chemotaxis.
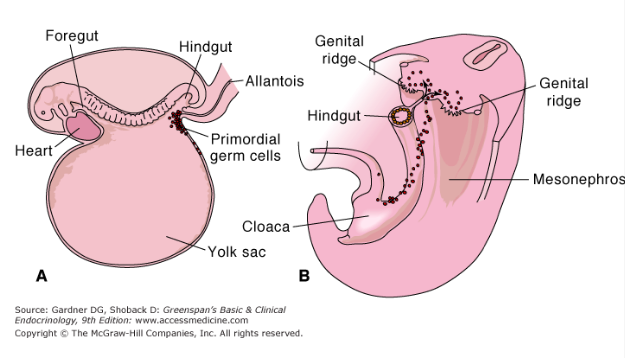
genital/gonadal ridge
area along the dorsal body wall that is the precursor to male or female gonads.
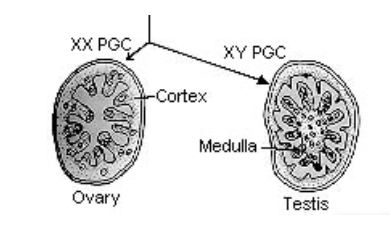
bipotential gonads
indeterminate preliminary gonads that have yet to differentiate towards ovaries or testis.
what happens when PGC arrives at the gonadal ridge?
they divide into millions and stimulate biopotential gonad growth, which differentiate depending on whether the PGCs are XX or XY.
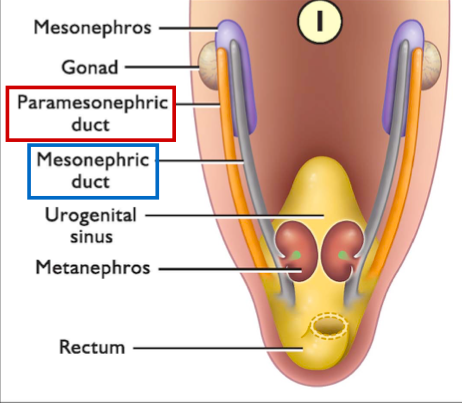
mesonephros
primitive kidney in fetus.
mesonephric duct (Wolffian duct)
forms male reproductive tract.
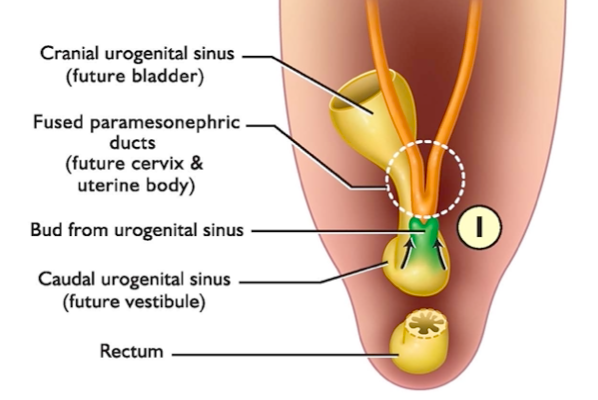
paramesonephric duct (Mullerian duct)
forms female reproductive tract.
indifferent reproductive tract
developing reproductive system that contains both the mesonephric (male) and paramesonephric (female) duct.
what is the result of SRY being present at a biopotential gonad?
testis development -> paramesonephric duct retracts.
what is the result of SRY not being present at a biopotential gonad?
ovary development -> mesonephric duct retracts.
which hormones lead to the development of the male reproductive tract
testosterone and anti-Mullerian hormon (AMH).
anti-Mullerian hormon (AMH)
secreted by Sertoli cells, degenerates paramesonephric duct.
dihydrotestosterone (DHT)
potent androgen that develops penis, scrotum, and accessory sex glands.
why do the testes have to descend into the scrotum, outside the body?
temperature regulation: spermatogenesis occurs at a lower temperature than the human body's core temperature.
gubernaculum
ligamentous cord attached to the bottom of the testis and connect to the scrotal sac.
INSL-3
hormone that causes the gubernaculum to pull the testis.
peritoneum
membrane that lines the abdominal cavity.
inguinal canal
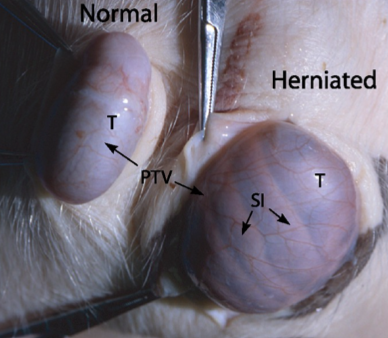
the channel through which the testis descends into the scrotum.
transabdominal phase
first phase of testicular descent in which growth of the fetal body pushes testis against the peritoneum.
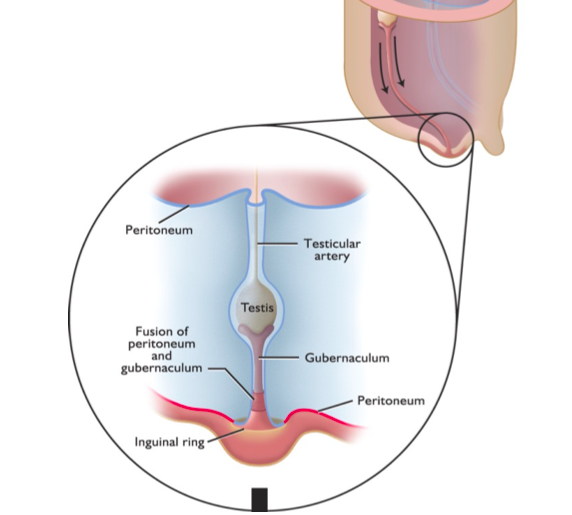
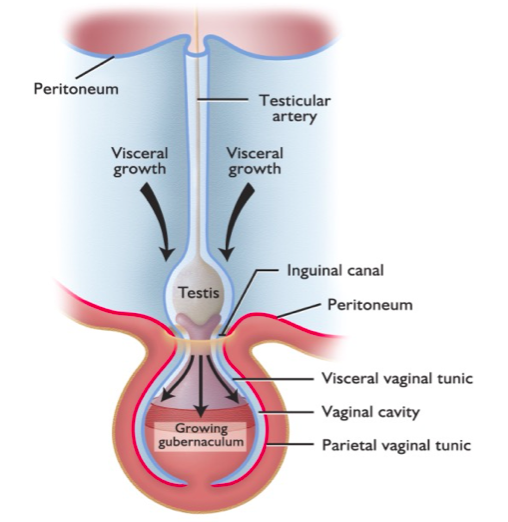
inguinal-scrotal phase
second phase of testicular descent in which the gubernaculum grows rapidly and mechanically pulls the testis into and through the inguinal canal.
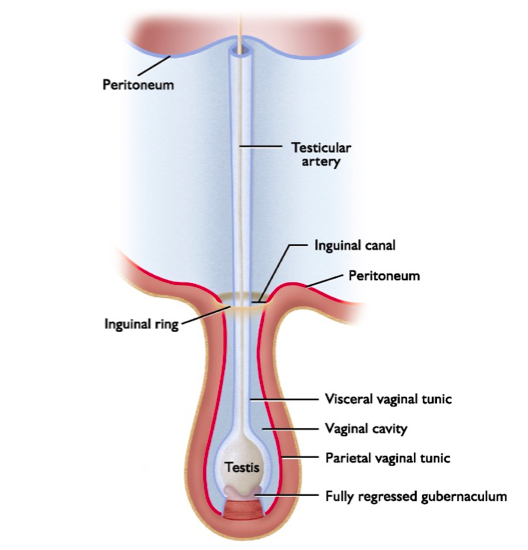
gubernaculum regression
third phase of testicular descent in which the gubernaculum regresses, peritoneum pinches off.
inner peritoneum
visceral vaginal tunic.
outer peritoneum
parietal vaginal tunic.
cryptorchidism
undescended testes.
in which form of cryptorchidism are males completely sterile?
bilateral (both sides).
true or false: cryptorchidism testes still produce testosterone
true.
inguinal hernia
common condition in which the small intestine pushes through the inguinal canal into the scrotum.
when no SRY is present, what do the paramesonephric ducts develop into?
infundibulum, oviduct, and uterus.
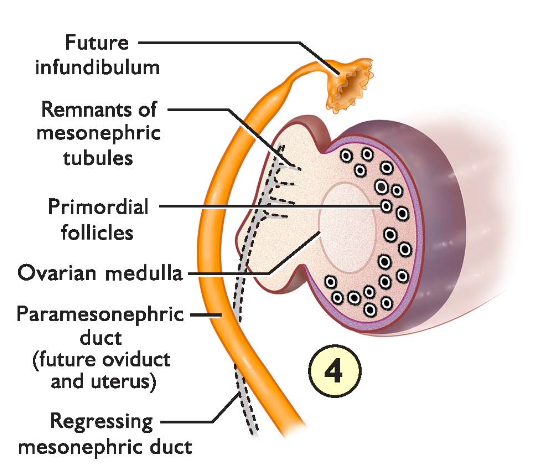
how do the fusion of the paramesonephric ducts affect the uterine structure?
more fusion = less/no uterine horn; less fusion = longer horns.
freemartin cattle
intersex condition in cattle where female cow uterus secretes testosterone, acts like a bull.
how are freemartin cattle developed?
dizygotic male/female twins share a blood flow in utero. testes develop before ovaries thus female embryo is exposed to AMH.
reproductive tract markers of freemartin cattle
small ovaries, no uterine body or cervix, large clitoris.
is sex determined genetically or developmentally?
both.