Ch. 4 Overview of Tissue Types and Their Functions
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
130 Terms
Tissue
A group of cells that usually have a common origin in an embryo and function together to carry out specialized activities.
4 basic tissue types
epithelial, connective, muscle, nervous
Histology
The study of tissues.
Epithelial Tissue
Covers surfaces, lines cavities, and forms glands. Enables interaction with internal and external environments.
Connective Tissue
Supports and protects the body, binds organs, stores energy (fat), and provides immunity.
Muscular Tissue
Specialized for contraction and force generation, producing heat in the process.
Nervous Tissue
Detects changes and responds with electrical signals (nerve impulses) to activate muscles and glands.
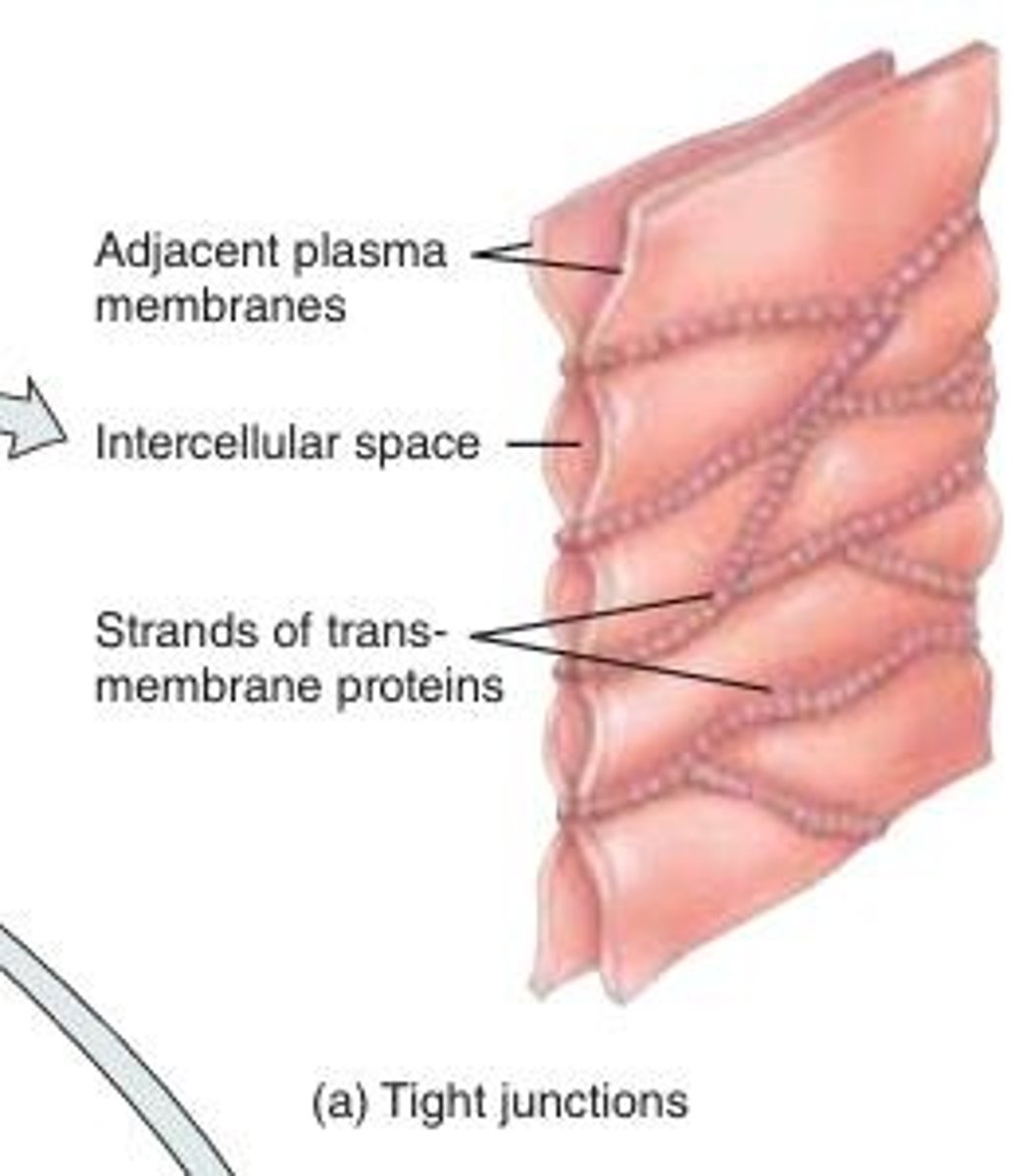
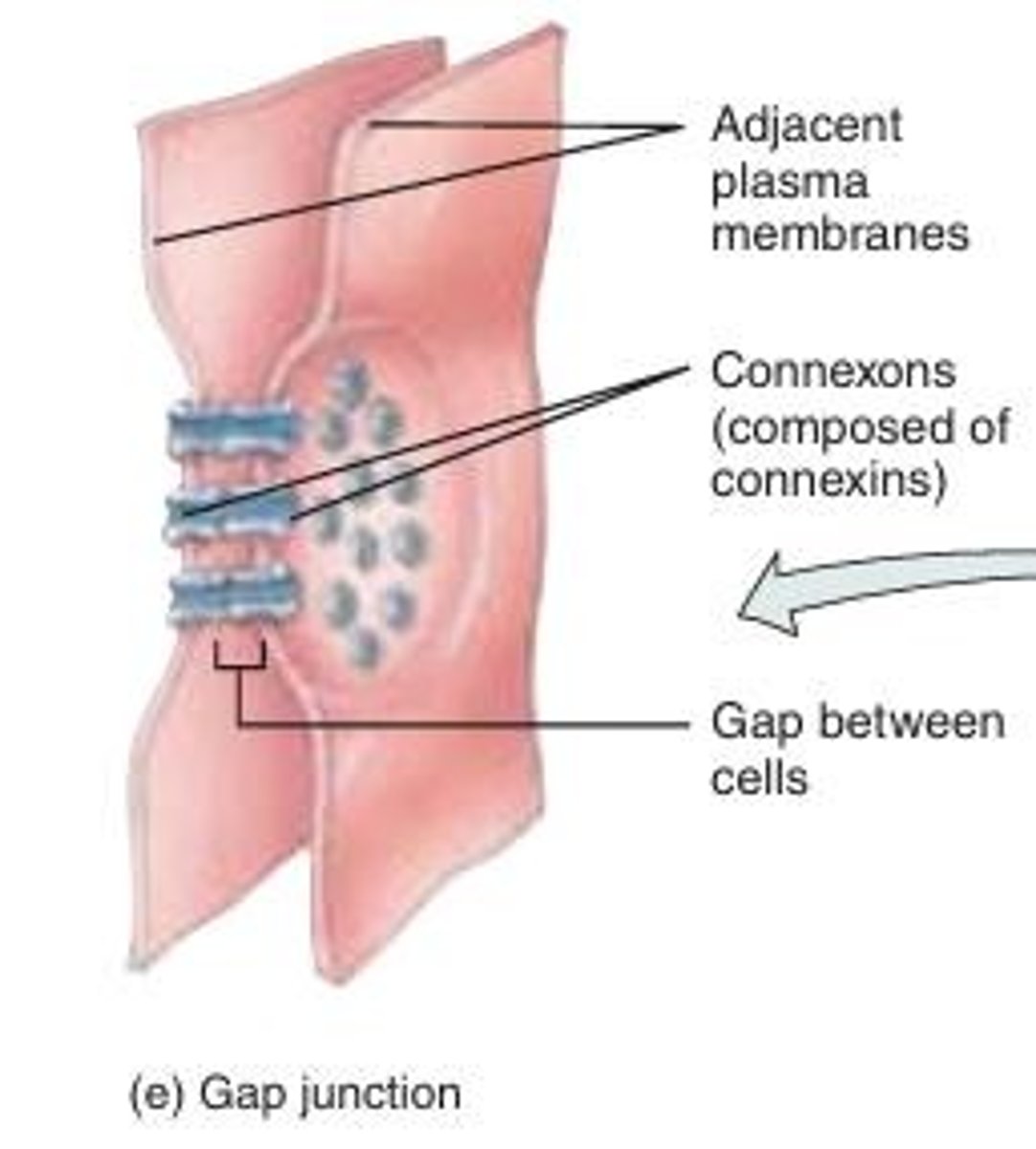
Cell Junctions
Contact points between the plasma membranes of tissue cells that provide structural support, facilitate communication, and regulate the passage of substances between cells
5 major types: tight, adherens, desmosomes, hemidesmosomes, and gap.
Tight Junctions
Consist of weblike strands of transmembrane proteins that fuse together the outer surfaces of adjacent plasma membranes to seal off passageways between adjacent cells
Cells of epithelial tissue that lines the stomach, intestines, and urinary bladder have ______.
They inhibit the passage of substances between cells and prevent the contents of these organs from leaking into the blood or surrounding tissues.
Ziplock bag = nothing gets in or out
Stitching cells together
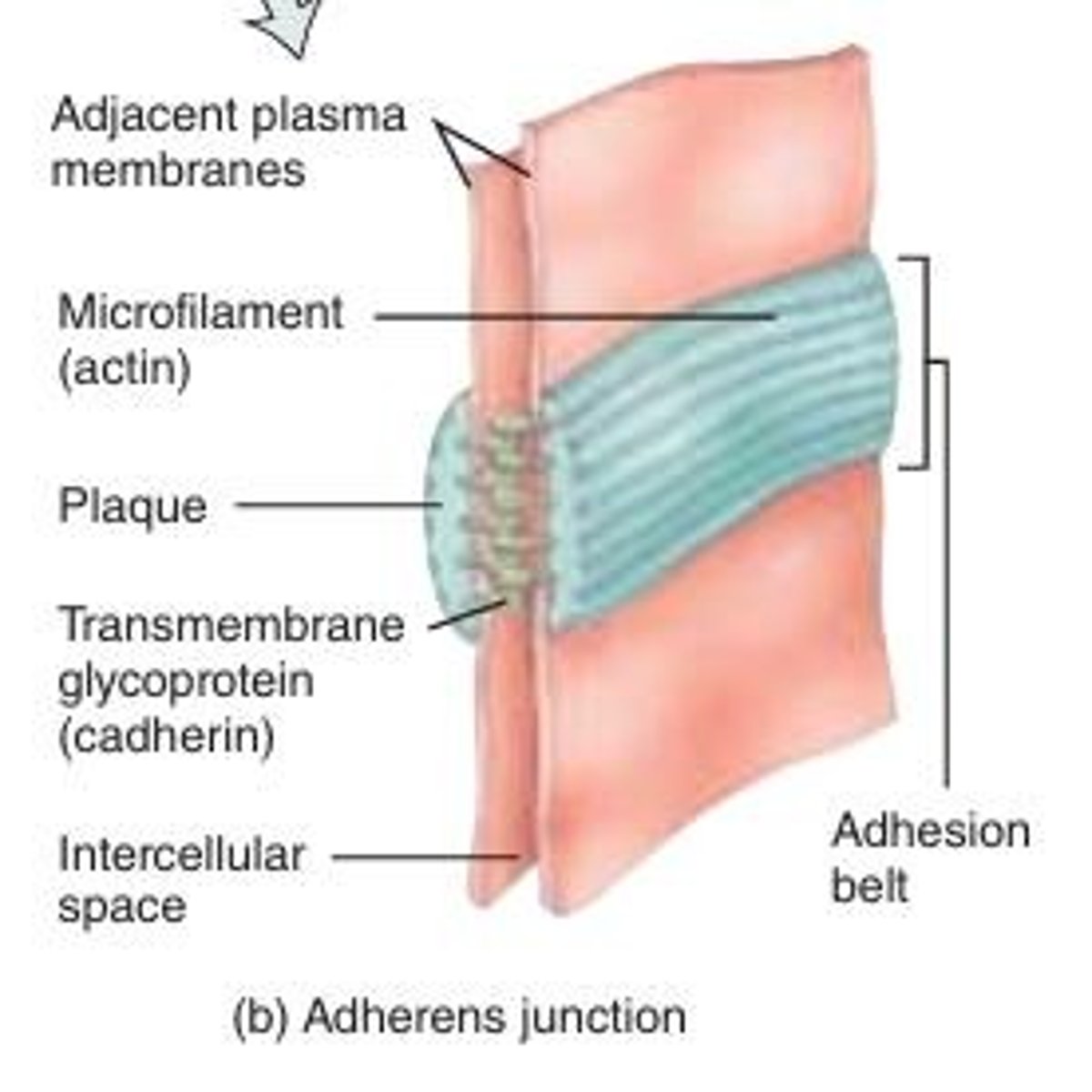
Adherens Junctions
Contain plaque, a dense layer of proteins on the inside of the plasma membrane that attaches to membrane proteins, helping epithelial surfaces resist separation during various contractile activities.
transmembrane glycoproteins called cadherins join cells together by connecting to cadherins of adjacent cells.
Works as a belt to hold your cells together (resist separation) during contractile activities
more flexible connection like a belt (needs flexible strength)
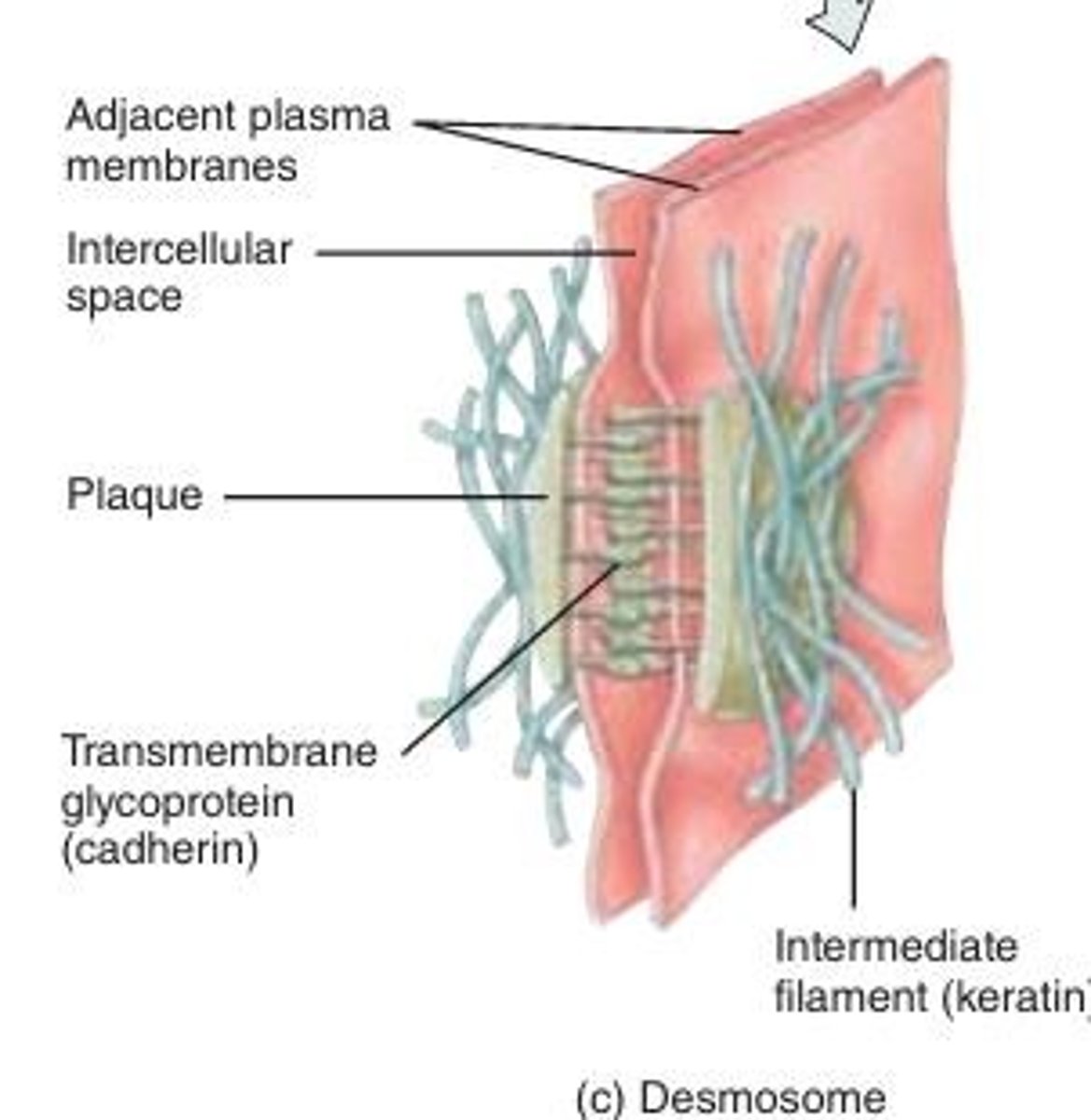
Desmosomes
Similar to adherents, plaque and cadherins are used but connected to intermediate filaments (keratin) inside the cell. They prevent cells from separating under tension.
prevent epidermal cells from separating under tension and cardiac muscle cells from pulling apart during contraction. Found in the skin and cardiac muscle (highly stretched tissues)
Resisting pulling forces
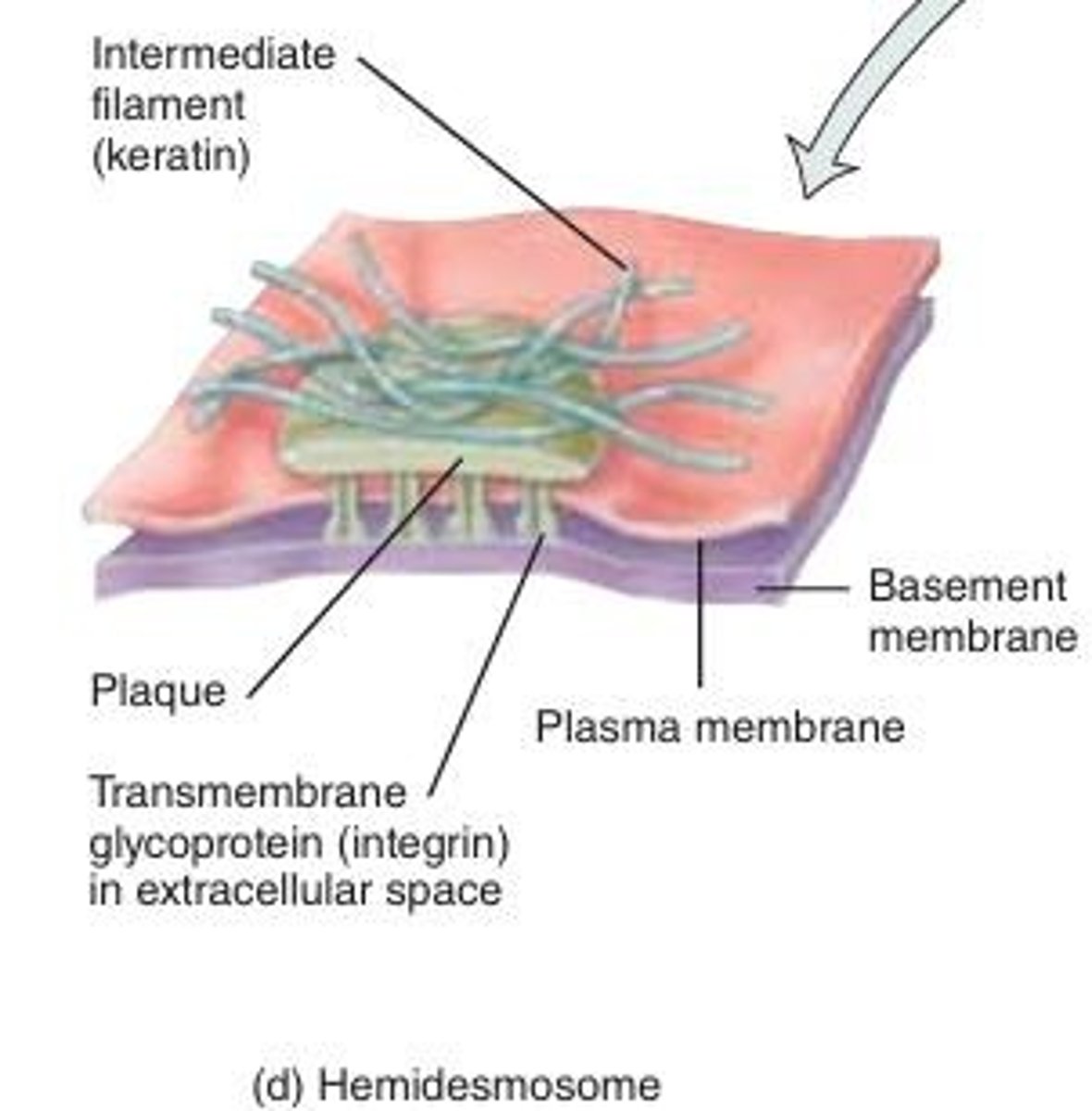
Hemidesmosomes
Anchor cells to the basement membrane using integrins and laminin. anchor cells not to each other but to the basement membrane.
Gap Junctions
Formed by connexins, creating channels (connexons) that allow the passage of ions and small molecules between cells.
- ____ allow the cells in a tissue to communicate. This is necessary for nutrient transfer in avascular tissues (e.g., lens, cornea) and embryonic development.
- enable nerve or muscle impulses to spread rapidly among cells.
- Allows stuff through
Extracellular Matrix
The network of proteins and other molecules outside of cells that influences the characteristics of a tissue. provide structural and biochemical support to surrounding cells. supports and regulates tissues
Bone
A hard tissue that provides structural support and protection for the body.
Blood
A liquid tissue that transports nutrients, gases, and waste products throughout the body.
Plaque
A dense layer of proteins on the inside of the plasma membrane that attaches to membrane proteins in adherens junctions.
Cadherins
Transmembrane glycoproteins that join cells together in adherens junctions.
Intermediate Filaments
Cytoskeletal components that desmosomes connect to in order to prevent cell separation under tension.
Connexins
Proteins that form gap junctions, creating channels for communication between cells.
How does epithelial tissue get blood supply? what type of cell junction is involved?
- epithelial tissues are avascular and get blood supply from neighbouring connective tissues
- gap junctions allow nutrients to move between cells in avascular tissues.
Phagocytes
A type of cell that can move freely within a tissue.
Epithelial Tissue
a fundamental tissue type in the body, characterized by closely packed cells arranged in continuous sheets, with minimal intercellular space (tightly packed together).
primary functions include protection, secretion, absorption, and excretion.
forms boundaries between organs and the external environment.
3 types of surfaces in epithelial cells
1. apical (free) surface
2. lateral surface
3. basal surface
Apical Surface
- faces either the body surface, a body cavity, the lumen (interior space) of an internal organ, or a tubular duct that receives cell secretions.
- They may contain cilia or microvilli (increase the surface area for absorption)
- the most superficial layer
Lateral Surfaces
face the neighbouring cells on either side (side by side)
contain cell junctions such as tight junctions, adherens junctions, desmosomes, and/or gap junctions to keep the cells glued together. they do not contain the hemidesmosome junction because they do not attach to a basement membrane
Basal Surface
adhere to extracellular materials such as the basement membrane via hemidesmosomes
deepest layer of epithelial cells
Basement Membrane
an extracellular membrane
acts as a filter, controlling which substances pass between epithelial and connective tissues.
anchors the epithelium to connective tissue, provides a surface for epithelial cell migration during growth and healing, and restricts larger molecules from passing through
two main layers: basal lamina & reticular lamina
plays key role in connecting epithelial tissue to connective tissue
Basal Lamina
A layer of the basement membrane closest to the epithelial cells.
contains proteins such as laminin, collagen, glycoproteins, and proteoglycans.
The laminin molecules adhere to integrins in hemidesmosomes and thus attach epithelial cells to the basement membrane
Reticular Lamina
a layer of the basement membrane closest to the connective tissue and contains proteins such as collagen produced by connective tissue
Epithelial Tissue Vascularity
has its own nerve supply but is avascular. It relies on the blood vessels of the adjacent connective tissue to bring nutrients and remove wastes through diffusion.
Functions of Epithelial Tissue
The primary functions of epithelial tissue include protection, secretion, absorption, and excretion
Acronym: P SAFE
Epithelial Tissue Location
Epithelial tissue almost always forms surface layers and is not covered by another tissue, with an exception being the epithelial lining of blood vessels (because blood is considered connective tissue)
Cilia and Microvilli
Epithelial cells may contain these organelles, which increase the surface area for absorption.
Extracellular Matrix in Connective Tissue
Connective tissues have a large amount of extracellular material that separates cells that are usually widely scattered.
Protection (Function of Epithelial Tissue)
Epithelial tissue protects underlying tissues from mechanical stress, abrasion, water loss, UV radiation, and invasion by foreign substances.
Secretion (Function of Epithelial Tissue)
Many epithelial cells specialize in secreting substances like mucus, hormones, and enzymes.
Absorption (Function of Epithelial Tissue)
The epithelium lining the gastrointestinal tract absorbs nutrients.
Excretion (Function of Epithelial Tissue)
Epithelium in the urinary tract excretes waste products.
Filtration (Function of Epithelial Tissue)
Epithelial tissue participates in the filtration of blood in the kidneys.
Covering and Lining Epithelium
Forms the outer lining of the skin and some internal organs, and the inner lining of blood vessels, ducts, body cavities, and various systems.
Classified by:
1. arrangement of cells in layers
2. cell shapes
covering and lining epithelium: types of cell layers
a. simple epithelium
b. stratified epithelium
c. pseudostratified epithelium
Simple Epithelium
Single layer of cells for diffusion, osmosis, filtration, secretion, and absorption.
Stratified Epithelium
Multiple layers of cells for protection in areas of wear and tear (ie skin)
Pseudostratified Epithelium
Appears multilayered but is a single layer.
Often ciliated
It appears to have multiple layers of cells because the cell nuclei lie at different levels, and not all cells reach the apical surface; it is actually a simple epithelium because all its cells rest on the basement membrane.
covering and lining epithelium: cell shapes
a. squamous
b. cuboidal
c. columnar
d. transitional
Squamous Cells
Flat and thin cells that allow for the rapid passage of substances.
Cuboidal Cells
Cube-shaped cells that may have microvilli and function in secretion or absorption.
Columnar Cells
Column-shaped cells for protection, secretion, and absorption; may have cilia.
Transitional Epithelium
Changes shape from squamous to cuboidal and back in response to stretching (ie bladder)
Glandular epithelium
a type of epithelium that secretes substances into ducts, onto a surface, or into the blood
Two types: endocrine & exocrine
Endocrine glands
Secrete hormones which enter interstitial fluid and then diffuse into the bloodstream without flowing through a duct. Because they reach the bloodstream, they have systemic effects.
Exocrine glands
Glands that secrete products into ducts that empty onto a surface.
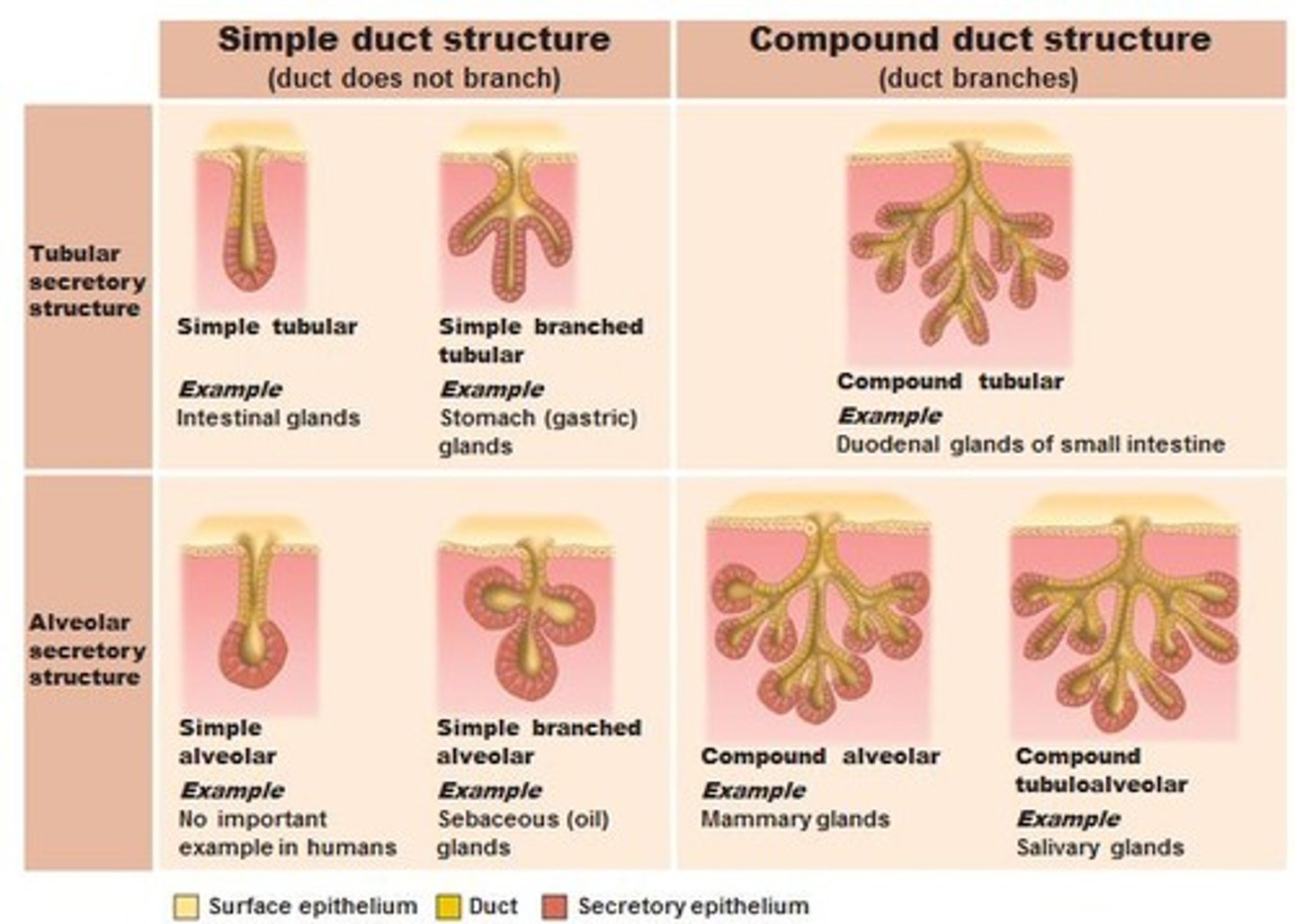
Structural Classification of Exocrine Glands
unicellular and multicellular
Unicellular exocrine glands
Single-celled exocrine glands, such as goblet cells. Goblet cells secrete mucous
Multicellular exocrine glands
Glands composed of many cells that form a distinctive structure or organ.
Multicellular glands categorization
classified by:
(1) whether their ducts are branched or unbranched and
(2) the shape of the secretory portions of the gland.
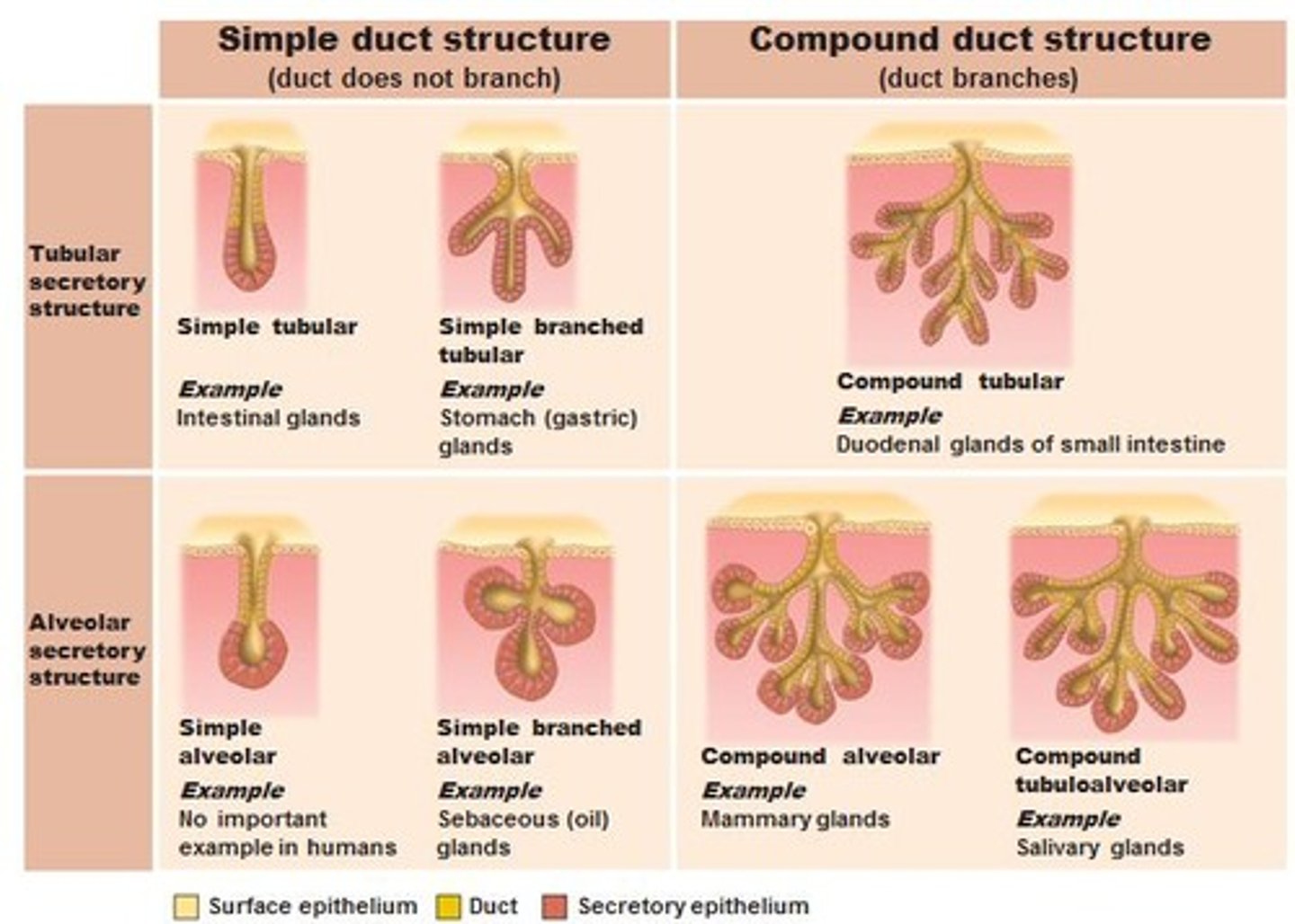
Simple gland
A gland whose duct does not branch.
Compound gland
A gland whose duct branches.
Tubular glands
Glands with tubular secretory parts.
Acinar glands
Glands with rounded secretory portions.
Tubuloacinar glands
Glands that have both tubular and rounded secretory parts.
Simple tubular gland
A simple gland with a straight tubular secretory part.
Simple branched tubular gland
A simple gland with a branched tubular secretory part.
Simple coiled tubular gland
A simple gland with a coiled tubular secretory part.
Simple acinar gland
A simple gland with a rounded secretory portion.
Simple branched acinar gland
A simple gland with a branched rounded secretory part.
Compound tubular gland
A compound gland with a tubular secretory portion.
Compound acinar gland
A compound gland with a rounded secretory portion.
Compound tubuloacinar gland
A compound gland with both tubular and rounded secretory portions.
Multicellular exocrine glands classification
Classified by duct branching (simple vs. compound) and shape of secretory portion (tubular, acinar/alveolar, or tubuloacinar).
Functional Classification of Exocrine Glands
based on how their secretions are released. Each of these secretory processes begins with the endoplasmic reticulum and Golgi complex working together to form secretory vesicles that contain the secretory product
1. Merocrine
2. Apocrine
3. Holocrine
Merocrine glands
Glands that release secretions via exocytosis, synthesized on ribosomes attached to rough ER, processed by the Golgi complex, and released in secretory vesicles.
Salivary glands, pancreas
Apocrine glands
Glands that release secretions by pinching off the apical portion of the cell.
Mammary glands
Holocrine glands
Glands where the entire cell ruptures and becomes the secretion.
Sebaceous glands
Connective tissue
Abundant and widely distributed tissue that binds together, supports, and strengthens other body tissues.
Functions of connective tissue
- Binds together, supports, and strengthens other body tissues
- protects and insulates internal organs
- compartmentalizes structures such as skeletal muscles
- serves as the major transport system within the body (blood, a fluid connective tissue)
- is the primary location of stored energy reserves (adipose, or fat, tissue)
- is the main source of immune responses.
Components of connective tissue
Consists of extracellular matrix (consists of protein fibers and ground substance) and cells.
Extracellular matrix
The material located between widely spaced cells in connective tissue, consisting of protein fibers and ground substance.
Connective tissue cells
Derived from mesenchymal cells; immature cells are called '-blasts' and mature cells are called '-cytes'.
Type of cell "-blasts"
immature cells (ie., fibroblasts, chondroblasts, osteoblasts)
secrete the extracellular matrix
Type of cell "-cytes"
Mature cells, (i.e. fibrocytes, chondrocytes, osteocytes)
maintain the extracellular matrix.
Fibroblasts
Large, flat cells that move through connective tissue and secrete fibers and ground substance.
Macrophages
Phagocytes that develop from monocytes, a type of white blood cell, which destroy bacteria and cell debris by phagocytosis.
Plasma cells (plasmocytes)
Cells found in many places in the body but most reside in connective tissue, especially in the gastrointestinal and respiratory tracts
Develop from B lymphocytes and secrete antibodies that attack and neutralize foreign substances.
Mast cells (mastocytes)
involved in the inflammatory response, the body's reaction to injury or infection and can also bind to, ingest, and kill bacteria. They produce histamine, which dilates small blood vessels during inflammation and kills bacteria.
Adipocytes
Fat cells or adipose cells that store triglycerides and are found below the skin and around organs.
Leukocytes
White blood cells that migrate from blood into connective tissue in response to certain conditions, such as infection.
For example, neutrophils gather at sites of infection, and eosinophils migrate to sites of parasitic invasions and allergic responses.
Ground Substance
The component between cells and fibres
supports cells, binds them together, stores water, and provides a medium for the exchange of substances.
Hyaluronic acid
A viscous, slippery polysaccharide that binds cells together, lubricates joints, and helps maintain the shape of the eyeballs.
Hyaluronidase
An enzyme produced by white blood cells, sperm cells, and some bacteria that breaks apart hyaluronic acid, making the ground substance more liquid.
Adhesion proteins
Proteins responsible for linking components of the ground substance to one another and to the surfaces of cells.
Fibronectin
The main adhesion protein of connective tissues that binds to both collagen fibers and ground substance, linking them together.
Three different types of protein fibers embedded in the matrix between the cells:
1. collagen
2. elastic
3. reticular
Collagen fibers
- very strong and resist pulling or stretching, but they are not stiff, which allows tissue flexibility.
- found in most connective tissues, especially bone, cartilage, tendons (which attach muscle to bone), and ligaments (which attach bone to bone).
Elastic fibers
- Fibers consisting of elastin surrounded by fibrillin, which adds strength and stability.
- strong but can be stretched up to 150% of their relaxed length without breaking.
- have the ability to return to their original shape after being stretched (elasticity).
- Found in skin, blood vessel walls, and lung tissue
- "elastic band"
Reticular Fibers
- Mesh like network
- Support blood vessel walls and form networks around the cells
- Produced by fibroblasts
- much thinner than collagen fibers and form branching networks
- provide support and strength.
- plentiful in reticular connective tissue, which forms the stroma (supporting framework) of many soft organs, such as the spleen and lymph nodes.
- These fibers also help form the basement membrane.
Classification of Connective Tissues
1) Embryonic connective tissues
- Mesenchyme
- Mucous connective tissue
2) Mature connective tissues
a. Connective tissue proper
- Loose
- Dense
b. Supporting connective tissue
- hyaline cartilage
- Bone tissue
c. Liquid connective tissue
- blood tissue
- lymph
Mesenchyme
Embryonic connective tissue found in embryos and fetuses that forms almost all other connective tissue types.
Mucous (Mucoid) Connective Tissue
Embryonic connective tissues found in the umbilical cord; provides support.