COPD – pathophysiology, diagnosis, prognosis & treatment
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
Describe key features of COPD
Heterogenous - not only one type
Airway disease (in the lung)
Persistent progressive airflow obstruction
Irreversible
What are symptoms of COPD?
Cough (common)
Sputum
Shortness of breath
Exacerbations
Describe COPD incidence
Top 3 causes of death
90% of deaths occur in low and middle income countries
Deprived populations and 3.5x more likely to suffer from COPD.
Describe COPD pathophysiology
Conditions occur due to abnormalities in:
The airways (bronchitis)
The alveoli (emphysema)
- Alveoli collapse - have lower surface area, so poorer gas exchange
- Chronic bronchitis - bronchitis for at least for 3 months. Cough, sputum production
- Emphysema - the collapse of the alveoli leads to reduced alveolar wall elasticity. Therefore less air can be pushed out upon exhalation.
- Tight smooth muscle airways
It does NOT include fibrosis.
What are the COPD current international and national guidelines?
National: these are the main ones used
- NICE NG 115
- Last updates July 2019
International: Gold initiative for chronic obstructive lung disease
- reported annually
What are risk factors for COPD?
- Main risk factor is smoking
- Patients from lower income backgrounds are more prone to smoke
- Lower income patients are likely to do work involving air pollution like mining
- Underdeveloped lungs e.g. maternal smoking
- Genetics - a1 antitrypsin deficiency (rare cause)
- History of asthma
Describe normal decline of lung function
Lungs are usually fully developed at 25 yrs old.
What happens in childhood and adolescence massively impact lung health.
After 25 yrs old, the lung function naturally declines
When should we consider a COPD diagnosis?
Cough becomes more productive as it becomes more severe.
Chronic cough
Any previous offenders to the organs
Any risk factors e.g. smoking, air pollution, occupational dusts
Recurrent wheezing
Shortness of breath (dyspnoea) which is progressive over time, persistent and gets worse with exercise.
When is COPD usually diagnosed
The earliest point at which airflow obstruction is detected by spirometry is usually when 50% of lung function is gone.
What are differential diagnosis for COPD?
1. Asthma
- variable airflow obstruction
family history
- common in children
- common in patients with eczema, allergy and rhinitis
- symptoms change daily
2. Congestive heart failure
- pulmonary oedema on chest x-ray
- volume restriction shown on pulmonary function tests rather than airflow obstruction
3. Bronchiectasis
- lots of sputum
- bacterial infection
- bronchial dilation on chest-Xray
Describe how to diagnose COPD
COPD diagnosis is determined by:
- Medical, family, social history
- Physical examination
- Assessment tools and questionnaires
- Post-bronchodilator spirometry (if available)
- Clinical diagnosis centres in primary care
- Other tests e.g. chest X-ray, ECG, blood tests, (HR)CT
Risk of lung cancer is x6 in people with COPD, we do an X-ray of chest to eliminate lung cancer
Describe spirometry in relation to COPD diagnosis
It is important to perform a spirometry test for a COPD diagnosis but a spirometry test ALONE is not enough for a COPD diagnosis.
What does spirometry tells us about patient's COPD?
Spirometry measures the FEV1/ FVC ratio.
To indicate COPD, we need an FEV1/ FVC ratio <0.7
This means less than 70% of total air was exhaled in 1 secound. This is a sign of obstruction.
We would expect that all/ most air would get out in 1st second in a healthy individual.
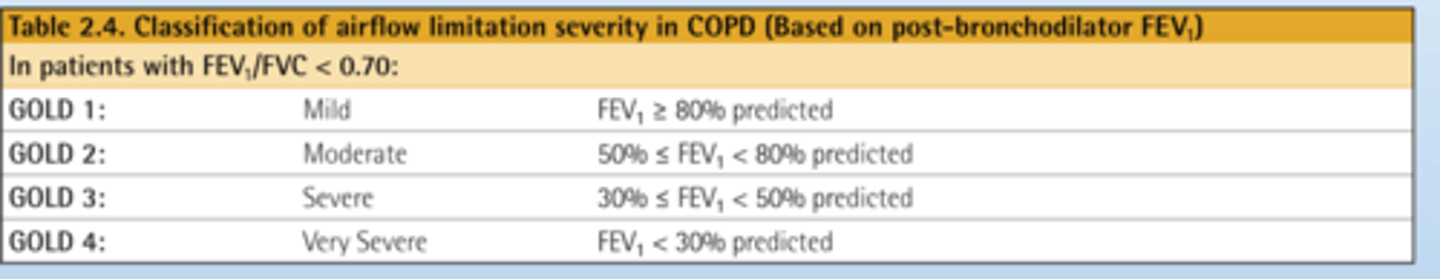
What is the current grading symptom for COPD?
Current grading system:
Gold 1-4
We grade COPD depending on severity.
- We compare FEV1/ FVC ratio to the ratio of a healthy of a patient of the same age, same gender and same height, sometimes ethnicity is also considered (but there may be poor evidence when considering ethnicity).
- We compare that persons score with their predicted score assuming healthy lung function.
Gold 4 Is the most severe COPD. Here FEV ratio is less than 30% of predicted.
What is the role of spirometry?
Spirometry allows us to:
- Diagnose COPD
- Assess severity of airflow obstruction
- Allows follow-up assessment; it can inform therapeutic decisions and identify rapid decline in lung function.
How can we assess COPD severity using questionnaires?
Patients can do these questionnaires
1. Modified MRC dyspnoea scale
- patients grade how breathless they feel (0-4)
2. CAT assessment
- The higher the score, the higher the impact of COPD on a patient's lifestyle.
Describe treatment based grading of COPD
Recently, grading of COPD has changed to A, B and E. We NO LONGER use A, B, C, D classification.
E stands for exacerbations.
We choose treatment for patient based on their symptoms - this is seen by how patient grades themselves (CAT or MRC assessment) and number of exacerbations.
What are the treatment goals for COPD?
1. Reduce symptoms - improve patients life
- Less cough
- Relief of symptoms
- Improve health status
AND
2. Reduce risk of comorbidities
- Prevent disease progression
- Prevent and treat exacerbations - the fewer the flare ups the better. Flare ups reduce lung function.
- Reduce mortality
What are likely comorbidities in patients with COPD?
We must screen patients with COPD for cardiovascular risk assessment (measure using QR4).
Anxiety and depression
Suicide
Patients feel guilt and shame as they believe they caused their symptoms of COPD.
How many people die 1 year after their 1st COPD exacerbation?
1 in 5 people after 1 year since 1st exacerbation.
How many people die 3.6 years after their 1st COPD exacerbation?
After 3.6 years after 1st exacerbation, only 50% survival rate.
Outline initial assessment of patients with COPD
1. FEV 1 - Gold 1-4
2. Symptoms (CAT or MRC questionnaires)
3. Exacerbation history
4. Blood eosinophil count
5. Alpha-1 trypsin
6. Comorbidities
Outline initial management of patients with COPD
1. Smoking cessation
2. Vaccination
3. Active lifestyle and exercise
4. Initial pharmacotherapy
5. Self-management education
- risk factor management
- inhaler technique
- breathlessness
- written action plan
6. Managing comorbidities
Describe smoking cessation strategy
1. Ask if they smoke
- what have they smoked e.g. cannabis is equivalent to smoking 10 cigarettes
2. Advise them not to smoke
3. Assess the willingness of the person quitting smoking
- why do they smoke
4. Assist: help the patient quit by
- making a plan
- social support group
- pharmacotherapy
5. Arrange: schedule a follow up in person or on the phone
Describe pharmacological treatments to assist smoking cessation
1. Cytisinicline (new and NOT for >65 year olds).
- Quit date: 5 days
2. NRT (nicotine replacement therapy)
- the only one for <18 (from 12 years) - most effective when short- and long- acting NRT combined.
- No set quit date
3. Varenicline (as part of the behavioural support programme).
Quit date: 1-2 weeks
4. Bupropion (less effective).
- Quit date: 2 weeks
Other recommended interventions:
- nicotine-containing e-cigarettes • Allen Carr's Easyway
Most smoking-related health problems are caused by other components in tobacco smoke, not by the nicotine.
Describe vaccination as a pharmacological treatment of COPD
The more vaccinations the better. Here are some of the recommended vaccinations for patients with COPD:
- Annual influenza
- Once-only pneumococcal (community acquired pneumonia incidence)
- Covid-19
- DTaP/atpA (pertussis/whooping cough) for those unvaccinated in adolescence
- Zoster (shingles protection) for >50 yrs
Describe pulmonary rehabilitation as a non-pharmacological treatment of COPD
This treatment is for patients who are functionally disabled by COPD (grade B and E).
This cannot be given to people who:
- can't walk
- have unstable angina
- had a recent MI
It aims to strengthen muscles and increase muscle use.
But! A drawback is that it can lead to shortness of breath initially, so patients then associate exercise with anxiety which is not good
Describe the COPD management cycle
1. Review
- symptoms
- dyspnoea
- exacerbation
2. Assess
- inhaler technique
- adherence
- non-pharmacological approached (pulmonary rehab and self-management education)
3. Adjust
- escalate/ de-escalate
- keep same
- switch inhaler device or molecules
We can provide advice for self-management.
Educate patients on how to manage their symptoms e.g. inhalers.
How do we treat group A COPD?
A bronchodilator.
Low symptoms (low CAT or MRC). They have low/ no exacerbations. (PRN - when required)
How do we treat group B COPD?
LABA and LAMA (both bronchodilators).
LAMA - long acting muscarinic antagonist
LABA - long acting beta-agonist
Moderate symptoms but low/ moderate exacerbations.
How do we treat group E COPD?
LABA and LAMA (both bronchodilators).
LAMA - long acting muscarinic antagonist
LABA - long acting beta-agonist
Exacerbations: at least 2 moderate or 1 which led to hospitalisation.
If blood eosinophil is more than 300, we CAN add ICS (inhaled corticosteroid). BUT! In COPD patients, this can increase risk in pneumonia.
What does eosinophil count represent in COPD patients?
The higher the eosinophil count, the higher the number of exacerbations.
What happens if a COPD patient who is on ICS due to a high eosinophil count gets pneumonia?
If patient gets pneumonia after adding ICS, we remove them off the ICS. Then their eosinophil level cut-off for ICS drops to 100.
What treatments could we add on top of LABA or LAMA in COPD patients?
If patients fit a specific criteria, we can also add azithromycin or roflumilast.
Azithromycin cannot be prescribed in smokers - doesn't work.
Roflumilast isn't too effective in COPD, but we have had it for years. This can be given if FEV1 < 50% and patient has chronic bronchitis.
What are some practical points relating to inhaler use and COPD treatment?
1. 2 in 1 or 3 in 1 once daily (e.g. Trelegy and Ellipita) inhalers improve patient adherence and therefore are preferred.
2. Most COPD preventors are DPIs. This should be considered when prescribing a reliever (also give as a DPI to prevent confusion with inhaler technique).
3. Always prescribe by a brand name e.g. Qvar, Trimbow, Fostair because it determines the particle size so that particles impact in the correct place in the lungs.
4. If a patient has COPD AND asthma then treatment for asthma should be followed. Therefore, treatment should ALWAYS contain an ICS.
What are the different oral treatment options for COPD?
1. OCS (oral corticosteroids): not recommended for long term use.
2. Theophylline
- little evidence for use
- narrow therapeutic range
3. Oral mucolytics e.g. carbocysteine and n-acetylcysteine
- can be useful in reducing sputum production
- long term use can cause peptic ulcers
4. Prophylactic antibiotics e.g. azithromycin
- 250mg 3x/week for non-smokers
- strong evidence in preventing eCOPD and improves QoL of patients
- started by a specialist
5. Roflumilast
- anti-inflammatory
- prescribed by a SPECIALIST only
What is classed as a COPD exacerbation?
An event characterised by dyspnoea (shortness of breath) and/or cough and sputum that has worsened over < 14 days.
How do we treat exacerbations in COPD?
SABA/SAMA initially and review and escalate maintenance treatment
We can give a short course of steroids
- 5 days is enough; for this length of time we don't need to ween patients off when it's a one-off two-off course
- BUT, even 1 course of oral steroids increases risk of side effects. But we don't want to remove them when patient is unwell.
Antibiotics for 5 days can be used, when indicated.
This can:
- shorten recovery time
- reduce the risk of early relapse
- reduce treatment failure
- reduce hospitalisation duration
When are COPD patients given COPD rescue packs?
Patients are given rescue packs if they have had at least 1 exacerbation and are still at risk of exacerbations.
After 1 exacerbation, you are at risk of more exacerbations.
Patient should be informed when and how to use them.
Describe problems related to COPD rescue packs
If they have had more than 3 oral corticosteroid/ antibiotic courses a year then they have a greater mortality risk and so this must be investigated further.
A problem with rescue packs for COPD is they are poorly coded in primary care so it is hard to determine how many a patient has received.
What is a new treatment for COPD being investigated?
Biologics are used in COPD patients so long as their eosinophil levels were high (>300) and had severe COPD .e.g monoclonal antibodies such as benralizumab ad mepolizumab.
Anti IL-4 such as dupilumab can also be used if
- Baseline blood eosinophil ≥ 0.3
- Recurrent exacerbations in COPD
What is respiratory failure?
A failure to maintain adequate blood oxygen levels (hypoxia) or increased blood carbon dioxide levels (hypercapnia).
What is type 1 respiratory failure?
Hypoxic
- Inadequate provision of oxygen to the body, leading to hypoxaemia
e.g. Pulmonary oedema, pneumonia, PE, pulmonary fibrosi
What is type 2 respiratory failure?
Hypercapnic
- Insufficient removal of carbon dioxide from the body, leading to hypercapnia
e.g. Chest-wall deformities (e.g., kypho-scoliosis) or trauma, respiratory muscle weakness, COPD, severe obesity
Describe NIV (non-invasive ventilation)
This is used in hospital for patients with exacerbations in COPD with acute respiratory failure.
In stable patients with severe COPD with hypercapnic respiratory failure and obstructive sleep apnoea (type 2 respiratory failure).
It improves ventilatory pressure leading to better gas exchange by reducing:
- respiratory rate
- work of breathing
- severity of breathlessness
- mortality
Describe oxygen in COPD
Oxygen needs to be prescribed (NOT air)
O2 saturation should be checked by pulse oximetry in all breathless and acutely ill patients
For critically ill patient it should be administered immediately
How do we concentration of much oxygen to administer in COPD patients?
In type 2 respiratory failure, in COPD patients, the brain gets used to high level of CO2. Therefore the brain stops reacting to it - becomes less sensitive.
The brain freaks out when there is a high level of O2 administered. This can cause the brain to think it no longer needs to breath.
We never give COPD patients 100% oxygen because a sudden increase in O2 to normal saturations (94-98%) confuses the brain signals to respiratory muscles to breathe slower and shallower. This causes a build-up of more CO2 leading to respiratory acidosis, coma, and death. We only give slow O2 to target oxygen 88-92%
What are the requirements for patients to receive long-term oxygen therapy?
- Must have severe chronic hypoxaemia
- Must not smoke
What are the risks of long-term oxygen therapy?
Respiratory depression, falls from tripping over equipment, burns & fire

How long is long-term oxygen therapy used for daily?
Used minimum 15 hours daily
Describe palliative and end of life care for COPD patients
- Discuss options with patient and family
- Administer opioids, oxygens and fans blowing on patients face to reduce breathlessness
- Nutritional supplementation to improve respiratory muscles and overall health
- Reduce fatigue using: self-management education, mind-body interventions and nutritional support.