Ischaemic Heart Disease - basic
1/107
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
108 Terms
What is the leading cause of death globally?
Cardiovascular disease (CVD).
How many people were estimated to have died from CVDs worldwide in 2016?
Approximately 17.9 million people.
What percentage of all global deaths in 2016 were due to CVDs?
About 31%
What proportion of CVD deaths are caused by heart attacks and strokes?
Around 85%.
According to the World Health Organization (WHO) and British Heart Foundation (BHF), how often does a CVD-related death occur in the UK?
On average, every 3 minutes.
How many people in the UK are currently living with cardiovascular disease?
About 7.4 million people.
Which organisation provides detailed statistics on cardiovascular disease in the UK?
The British Heart Foundation (BHF) – CVD Statistics UK Factsheet 2020.
Which groups are included in the UK death rate statistics for heart and circulatory diseases?
Males, females, and both combined.
What is ischaemia?
Ischaemia is a restriction or reduction in blood flow to tissues.
What can prolonged ischaemia eventually lead to?
Tissue hypoxia (reduced oxygen) or anoxia (absence of oxygen).
What is hypoxia?
A condition in which there is a reduced level of oxygen in tissues.
What is anoxia?
A condition where there is a complete absence of oxygen in tissues.
Can hypoxia occur without ischaemia?
Yes, hypoxia can occur without ischaemia.
Give examples of conditions that may cause hypoxia without ischaemia.
Anaemia and respiratory disease.
How do anaemia and respiratory disease cause hypoxia?
They reduce the oxygen content of arterial blood, leading to decreased oxygen delivery to tissues.
What is ischaemic heart disease (IHD)?
A group of clinical syndromes characterised by myocardial ischaemia.
What causes myocardial ischaemia in ischaemic heart disease?
An imbalance between the heart muscle’s blood supply and its oxygen demand
What is meant by “inadequate perfusion” in IHD?
It refers to an insufficient blood flow to meet the metabolic needs of the heart muscle.
What are the key consequences of inadequate myocardial blood supply in IHD?
Insufficient oxygen supply and reduced nutrient availability.
Besides reduced oxygen and nutrients, what other problem occurs in IHD due to poor perfusion?
Inadequate removal of metabolic end products from the myocardium.
What is the underlying pathophysiological feature of all forms of ischaemic heart disease?
Myocardial ischaemia resulting from reduced coronary blood flow or increased myocardial demand.
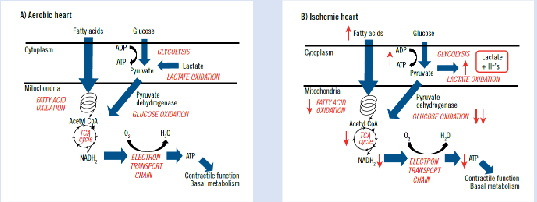
What type of organ is the heart in terms of energy metabolism?
The heart is an aerobic organ
How energy-dependent is the heart compared with other organs?
It is one of the most energy-dependent structures in the body, requiring around 6 kg of ATP per day.
How is most of the ATP in the heart produced?
Through aerobic mitochondrial respiration and oxidative phosphorylation.
Why does the heart require continuous aerobic ATP production?
To maintain adequate ATP pools for its constant mechanical and electrical activity.
What are the main cellular processes in myocardial cells that require ATP?
Membrane transport systems (e.g., Na⁺/K⁺-ATPase to maintain membrane potential)
Sarcomere contraction (via myosin ATPase)
Sarcomere relaxation (via Ca²⁺ transport by PMCA and SERCA pumps)
What happens to myocardial metabolism when heart rate and contractility increase?
Myocardial metabolism increases to meet the higher energy demand.
Under what conditions do cellular ATP levels decrease in the myocardium?
i) When there is insufficient oxygen for aerobic ATP production, or
ii) When ATP utilisation exceeds ATP synthesis.
How is ATP usage distributed in myocardial cells?
Approximately 66% is used for contraction, and 33% for ion pumps.
Through which process is ATP primarily generated in the myocardium?
Through oxidative phosphorylation.
What are the main energy substrates used by the heart under resting conditions?
Fatty acids, glucose, and lactate.
Under resting conditions, what proportion of the heart’s energy is supplied by fatty acids?
Approximately 60–90%.
Under resting conditions, what proportion of the heart’s energy is supplied by glucose and lactate?
Around 10–40%
After a high-carbohydrate meal, which substrate is primarily used by the myocardium for energy?
Carbohydrates, mainly glucose
During exercise, which substrate becomes an important substitute for glucose in ATP production?
Lactate.
Why is lactate an important energy source during exercise?
It can be efficiently oxidised by the myocardium to generate ATP when glucose demand increases.
What happens when the coronary circulation cannot deliver enough metabolic substrates to the heart?
The heart cannot sustain aerobic metabolism
Why is the myocardium unable to maintain aerobic metabolism during hypoxia?
It cannot extract sufficient oxygen from the blood
What does a reduced partial pressure of oxygen within the tissue indicate?
Hypoxia.
How does hypoxia affect mitochondrial respiration and oxidative metabolism?
Both are reduced due to the lack of oxygen.
What causes insufficient coronary flow in hypoxic conditions?
Inadequate flow to maintain cardiac function at rest, or
A limited ability to increase flow during exercise.
What happens when the myocardium’s energy requirements exceed mitochondrial energy generation?
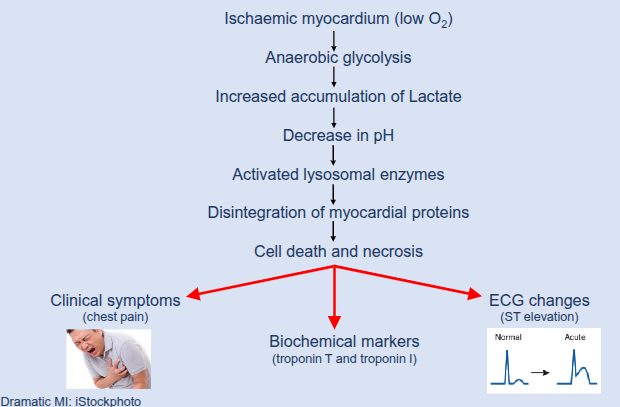
The heart shifts from aerobic metabolism to anaerobic glycolysis.
What metabolic pathway does the myocardium rely on during hypoxia to generate ATP?
Anaerobic glycolysis.
What is the main limitation of anaerobic glycolysis compared with aerobic metabolism?
It produces much less ATP and leads to lactate accumulation.
What energy source does the myocardium use during anaerobic metabolism?
Glycogen.
Why is glycogen an inadequate long-term energy source for the myocardium?
It has a limited supply and is rapidly depleted.
What happens to pyruvate produced by glycolysis during anaerobic conditions?
It is not readily oxidised in the mitochondria.
What is the fate of pyruvate in the cytosol during anaerobic metabolism?
It is rapidly converted into lactate
How does lactate metabolism differ between aerobic and ischaemic conditions?
In aerobic conditions, lactate is taken up from the blood.
In ischaemia, the myocardium produces lactate.
How does anaerobic glycolysis compare to aerobic metabolism in terms of ATP production?
It produces much less ATP.
Can anaerobic glycolysis fully compensate for the loss of oxidative phosphorylation?
No, it cannot.
What is the overall energy state of the ischaemic myocardium?
It has a negative energy balance with a progressive loss of high-energy phosphate reserves (e.g., ATP and creatine phosphate).
What metabolic changes occur during myocardial ischaemia?
Hydrolysis of adenine nucleotides and increased lactate production, leading to acid accumulation.
What effect does increased acid production have on myocardial tissue?
It causes a decrease in tissue pH.
What factors determine the rate and magnitude of phosphate depletion and pH reduction during ischaemia?
The degree of reduction in blood flow and the functional state of the myocardium.
What happens to cellular homeostasis during myocardial ischaemia?
It becomes disrupted due to accumulation of lactate and hydrogen ions (H⁺), leading to a fall in intracellular pH.
How does a fall in intracellular pH affect cardiac function?
It reduces the contractile work of the myocardium.
What can occur if the hypoxic state persists for a prolonged period?
Cell death due to severe ATP depletion.
What is the main energy-related cause of cell death in prolonged myocardial ischaemia?
A critical decrease in ATP levels.
Alterations in myocardial energy metabolism
Ischaemic Heart Disease – Biochemical Changes
What is ischaemic heart disease, and what causes it?
Ischaemic heart disease arises from hypoxia due to decreased blood flow to the myocardium, usually caused by narrowing or blockage of the coronary arteries. It results from coronary artery disease and is often referred to as coronary heart disease.
What is cardiovascular disease (CVD)?
Cardiovascular disease is a group of disorders affecting the heart and blood vessels, including coronary heart disease, cerebrovascular disease, peripheral arterial disease, and conditions such as deep vein thrombosis and pulmonary embolism.
What is coronary heart disease and what are its main pathological causes?
Coronary heart disease refers to the stenosis (narrowing) or blockage of a coronary artery, which can lead to acute coronary syndromes due to sudden loss of blood supply to the heart muscle. Underlying pathologies include coronary spasm, coronary microvascular dysfunction, dissection, intramural haematoma, thrombus or embolus, and atherosclerosis.
What is a coronary artery spasm and what are its key features?
A coronary artery spasm is a sudden occlusive vasoconstriction of a segment of a coronary artery, causing a marked reduction in coronary blood flow. It can occur at rest or be triggered by effort or stress, may arise at both significant and non-significant coronary stenoses, and can involve multiple segments (multifocal spasm).
What is coronary microvascular dysfunction and how does it contribute to ischaemic heart disease?
Coronary microvascular dysfunction affects small coronary vessels (<500 μm) that regulate myocardial perfusion. It involves structural and functional abnormalities of the microcirculation, leading to impaired coronary flow responses to vasodilator stimuli. It often occurs alongside obstructive coronary artery disease and contributes to the development of ischaemic heart disease.
What is spontaneous coronary artery dissection (SCAD) and who does it commonly affect?
Spontaneous coronary artery dissection (SCAD) is an uncommon emergency condition in which a tear forms in a coronary artery, restricting blood flow to the heart. It most often affects women in their 40s and 50s, though it can occur at any age or in men, and typically occurs in individuals who are otherwise healthy with few conventional risk factors for heart disease.
What is a coronary intramural haematoma and how does it occur?
A coronary intramural haematoma occurs when blood accumulates within the media of the artery wall, displacing the internal elastic membrane inward. It may develop spontaneously or during percutaneous coronary intervention. Proposed mechanisms include intimal tears due to weakening of the coronary artery wall and bleeding from the vasa vasorum.
What is a thromboembolism and how does it cause obstruction?
A thromboembolism occurs when a blood clot, known as an embolus, travels through the bloodstream and becomes lodged in a blood vessel, blocking its lumen and obstructing blood flow.
What is atherosclerosis and how does it affect the coronary arteries?
Atherosclerosis is characterised by inflammation and the buildup of fatty deposits (plaques) along the innermost layer of arteries. The plaques develop gradually over many years and, in the coronary arteries, can reduce or block blood flow to the heart.
Healthy endothelium

Endothelial Activation/Dysfunction
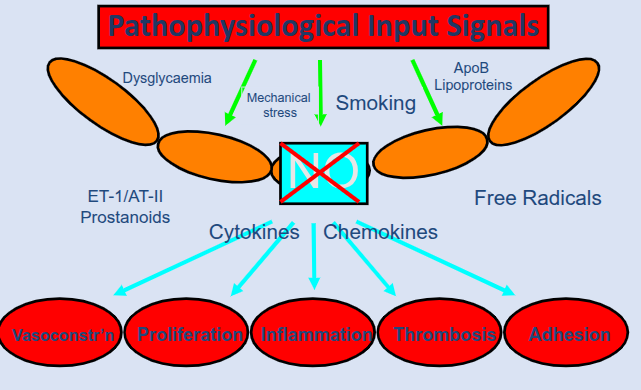
Where does disturbed blood flow commonly occur in arteries?
In areas of high curvature or downstream of bifurcations, such as coronary bifurcations
What type of stress do endothelial cells experience in regions of disturbed flow?
Disturbed shear stress.
How does disturbed shear stress affect endothelial nitric oxide synthase (eNOS)?
It reduces eNOS production, leading to decreased nitric oxide availability.
What is the effect of reduced eNOS production on vascular function?
It results in impaired vasodilatation and reduced endothelial cell repair.
How does disturbed flow influence oxidative stress in endothelial cells?
It increases reactive oxygen species (ROS) levels
What are the consequences of increased ROS in endothelial dysfunction?
Greater endothelial permeability to lipoproteins, enhanced leukocyte adhesion, and increased apoptosis.
How does disturbed flow affect the vessel wall structure?
It promotes smooth muscle cell (SMC) proliferation and collagen deposition, contributing to plaque development.
What are the major risk factors for atherosclerosis-related endothelial dysfunction?
Hyperlipidaemia, smoking, hypertension, and diabetes
Are the risk factors for atherosclerosis evenly distributed throughout the circulation?
Yes, but plaques develop only at specific sites where blood flow is disturbed
Where in the arteries do atherosclerotic plaques most commonly form?
At arterial branches and sites of curvature.
What characterises the blood flow in areas prone to plaque formation?
Low and disturbed wall shear stress, with complex changes in flow speed and direction.
What cellular responses play a central role in the initiation and progression of atherosclerosis?
The responses of vascular endothelial cells (ECs) to mechanical stimuli such as shear stress.
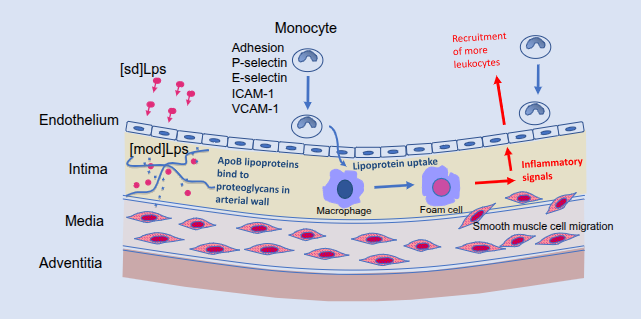
Atherosclerotic plaque initiation I
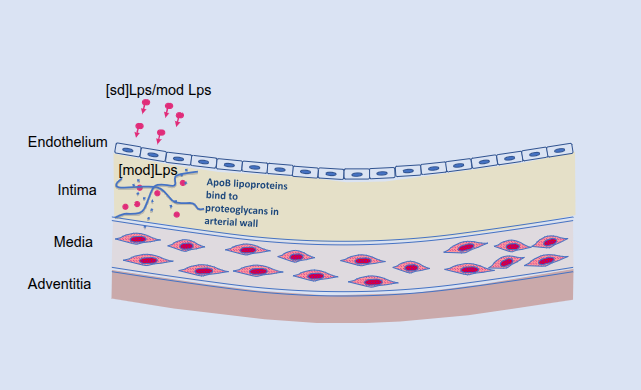
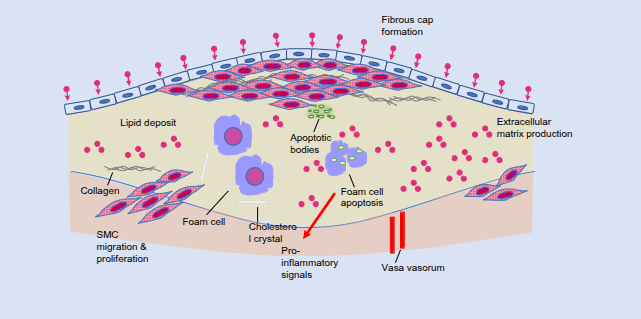
Atherosclerotic plaque initiation II
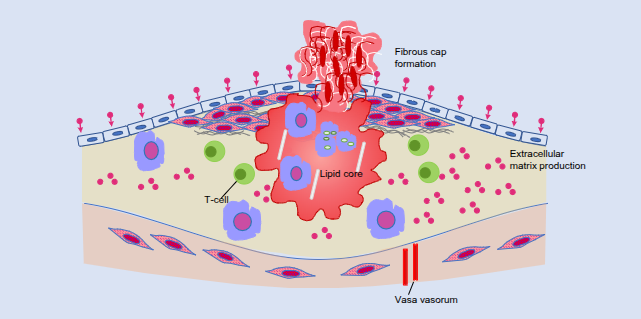
Atherosclerotic plaque progression
How does coronary atherosclerosis develop over time?
It is a slow, progressive process that can take many years before clinical ischaemic symptoms appear
On what factors does the manifestation of coronary heart disease depend?
The duration, severity, and acuity of ischaemic episodes.
What is angina?
Angina is a recurring discomfort or pain in the chest that usually lasts only a few minutes.
How does angina differ from a heart attack?
Unlike a heart attack, angina does not cause permanent damage to the heart muscle.
What is stable angina and when does it typically occur?
Stable angina occurs often during exercise or emotional stress, when heart rate and blood pressure increase, raising myocardial oxygen demand.
What is unstable angina and when can it occur?
Unstable angina can occur at rest or during sleep, or with minimal physical exertion, and may progress to a myocardial infarction.
Why can unstable angina be more dangerous than stable angina?
Because it can occur unpredictably and may lead to a heart attack.
Atherosclerotic plaque progression II
What defines a myocardial infarction (MI) according to the 2018 universal definition?
MI is defined by myocardial necrosis caused by myocardial ischaemia, with five clinical subtypes depending on the underlying pathophysiological mechanism.
What causes myocardial necrosis in all subtypes of MI?
Reduced blood flow leading to myocardial ischaemia.
How does the adult mammalian heart respond to loss of myocardial cells after MI?
It has a very limited capacity to regenerate, so lost cells are replaced by a fibrotic scar.
What happens to the surrounding myocardium after scar formation post-MI?
The surrounding myocardium undergoes remodelling.
What is the long-term consequence of myocardial remodelling after an infarct?
It eventually leads to impaired cardiac function.