Geriatrics & Death & Dying
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
120 Terms
Clinical problems in aging
In younger adults individual diseases tend to have a more distinct pathophysiology with well-defined risk factors
Diseases in older persons may have a less distinct pathophysiology and are often the result of failed homeostatic mechanisms
Population aging emerged as a worldwide phenomenon for the first time in history within the past century
Governments and societies—as well as families and communities— now face new social and economic challenges that affect health care
While the number of children has remained relatively stable, explosive growth has occurred among older populations (especially among the oldest)
The number of persons aged 80–89 years more than tripled between
1960 and 2010
Top two deaths in the US
Heart disease
Cancer
Active Dying is measured in
Days
Terminal illness is measured in
Weeks to months
How to prevent or stop the death rattle?
Anticholernergic agents (scopolomine)
Position change
What are clinical signs of decreased cardiovascular?
Decrease in cardiac output (despite tachycardia)
Decrease in blood pressure
Shunting of blood to core
Decreased peripheral perfusion
Peripheral & central cyanosis
Skin mottling
Loss of peripheral pulses
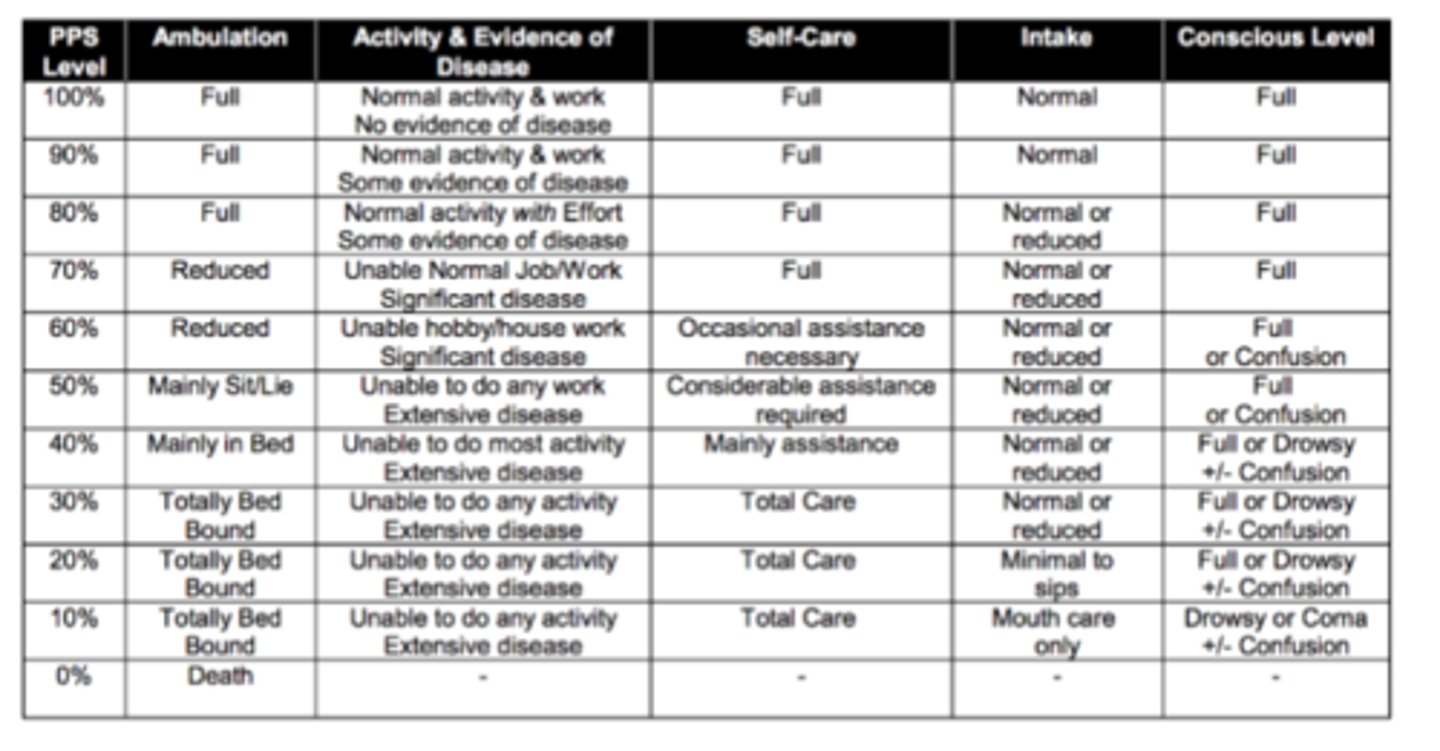
What does the palliative performance scale measure?
30% or below is bad
a positive finding
at 30%
completely physically reliant
still consuming food and water
full, drowsy, or confusion LOC
Activity
Ambulation
Intake
Consciousness
What are drugs or palliative drugs used to help with confusion and restless during death?
Dopamine
Why does withdrawing liquids and food help in death?
Reduce discomfort, continuing liquids + food does not prolong life
Major issues with aging
Increasing disability (difficulty with ADLs)
Cognitive impairment
Increased use of healthcare resources/ increased health expenditures
Expenditures increase with age, degree of disability, and are highest in the last year of life
What are ADLs (activities of daily living)
basic self-care activities
personal hygiene
dressing / undressing
eating
transferring from bed to chair & back
voluntarily controlling urinary & fecal d/c
using the toilet
moving around (vs. being bedridden)
What are IADLs (instrumental activities of daily living)
tasks that are not necessary for fundamental functioning but permit an individual to live independently in a community
according to Erickson’s stage of life, this is “ego integrity vs despair”
doing light housework
preparing meals
taking medications
shopping for essential items (e.g. groceries, clothing)
using the telephone
managing money
using technology (new!)
When do you spend more one care?
The last year of your life
What is the Erikson Stage for aging adults?
Ego integrity vs Despair
What are geriatric syndromes
common conditions found in older adults that tend to be multifactorial & do not fall under discrete disease categories, including:
delirium
gait d/o's / falls
chronic pain
urinary incontinence
anorexia / malnutrition
cognitive impairment
chronic pain
disability
disease susceptibility / comorbidity
decubitus ulcers
sleep d/o's
4 domains (systemic effects) of aging
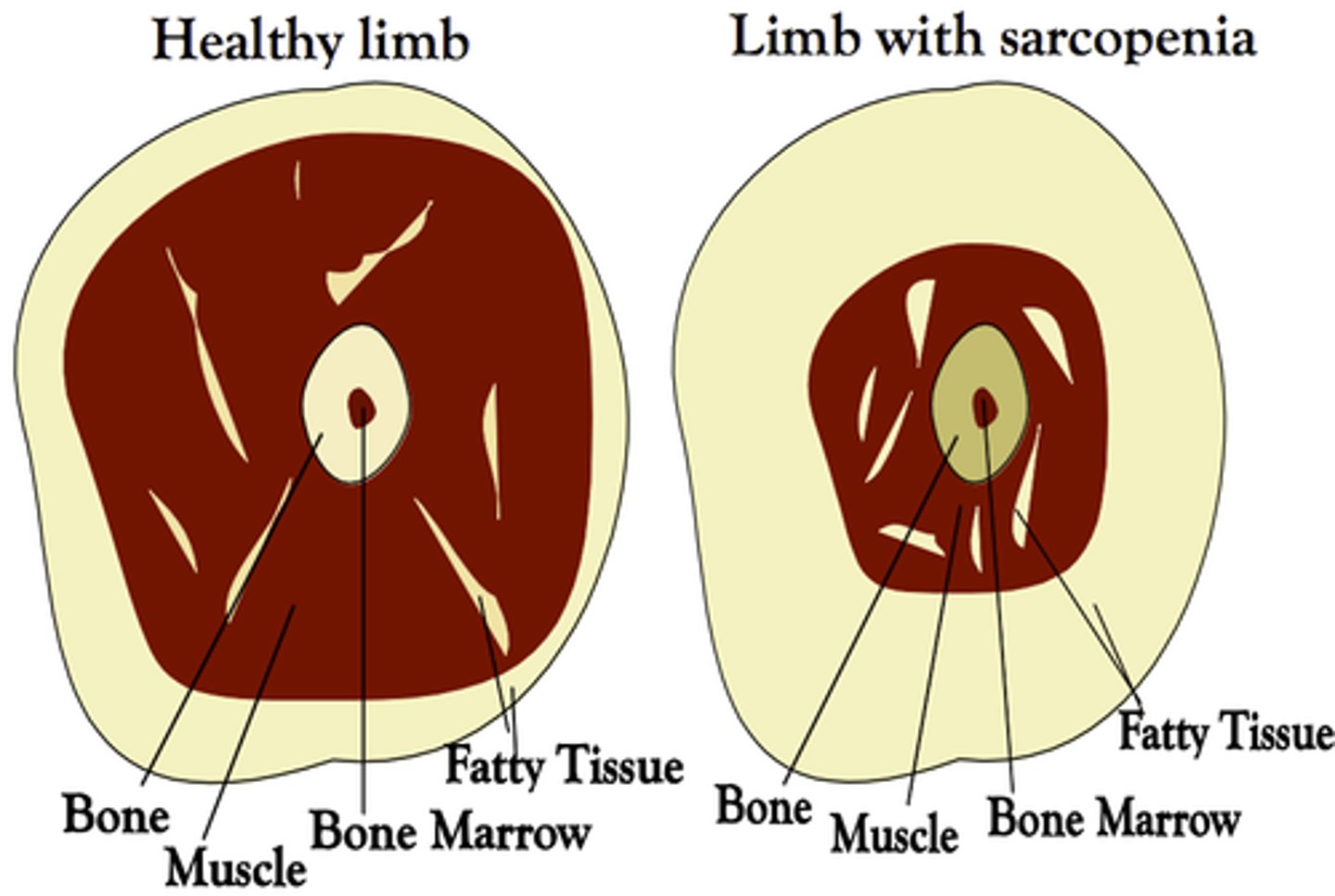
body composition
lean body mass declines (muscle and visceral organ tissue) → body fat increases
balance between energy availability & energy demand
becomes imbalanced with age → fatigue
decline of signaling networks (e.g. endocrine & nervous systems) that maintain homeostasis
neurodegeneration
Domain: body composition
This might be the most evident & and inescapable effect of aging
Caused by disruptions in links b/t synthesis, degradation, & and repair that normally serve to remodel tissues
Influenced by aging, illness, lifestyle factors (e.g. physical activity, diet)
Assessment: body composition
PE → muscle strength testing (isometric, isokinetic), anthropometrics (weight, height, BMI, waist circumference, arm & leg circumferences, skin folds)
labs → biomarkers (24-hr creatinuria OR 3-methyl-histidine)
imaging → CT & MRI, DEXA
other → hydrostatic weighing
Manifestations: body composition
body weight ↑ through childhood, puberty, & adulthood until late middle age
body weight begins to ↓ in
male-bodied people 65 - 70 y/o
female-bodied people somewhat later
fat mass ↑ in middle age then ↓ in late life
so may be slightly overweight may better to enter last stage of life
lean body mass (predominantly muscle + visceral organs) ↓ steadily after 3rd decade
faster in fast-twitch (used in long runs)
waist circumference continues to ↑ through lifespan
suggests that visceral fat continues to accumulate
muscle strength ↓ with age → ↑ weakness
strong independent predictor of mortality
bone strength ↓ with age from progressive demineralization / architectural modification → ↑ risk for fractures
true or false: Muscle strength is a strong independent predictor of mortality.
true
prevention:
low-impact strength training has been shown to ↓ muscle atrophy & weakening of bones
body awareness-strengthening activities (e.g. yoga, Tai Chi) shown to ↓ falls
In skeletal muscle, atrophy that occurs as we age is greater in _____-twitch than in _____-twitch fibers.
fast, slow
true or false: Male-bodied people tend to lose bone mass at a younger age & more quickly than female-bodied people.
false
Rationale: Female-bodied people tend to lose bone mass at a younger age & more quickly than male-bodied people (i.e. reach threshold of low bone strength that ↑ fracture risk sooner).
What kind of fat is responsible for most of the pathologic consequences of obesity?
visceral
What constitutes "energy demand" for the body?
the energy required to complete tasks of daily life PLUS compensate for any kind of chronic condition that requires energy expenditure to maintain homeostasis
Assessment: balance between energy availability & energy demand
self-reported questionnaires re: physical activity, sense of fatigue, exercise tolerance (including sexual activity)
PE → performance-based tests of physical function
imaging → magnetic resonance spectroscopy
other → resting metabolic rate, treadmill testing (of O2 consumption during walking), objective measures of physical activity (e.g. accelerometers, double-labeled water)
Manifestations: balance between energy availability & energy demand
fitness ↓ → ↓ activity tolerance
energy production / consumption (measured by VO2) ↓ progressively & rate of ↓ is accelerated in persons who are sedentary / those affected by chronic illness
BMR ↓
only partially explained by ↓ in metabolically active lean body mass
individuals with chronic illness expend more energy in resting state → higher RMR, weight loss observed with illness
old age + chronic illness + physical impairment all ↑ energetic cost of motor activities
What is fitness?
max possible energy production over an extended period of time
This declines with age
How are energy production & consumption measured?
indirectly via oxygen consumption (VO2)
Why do sick, older individuals often consume all of their available energy performing their most basic ADLs?
because of the ↑ energetic cost of motor activities (i.e. despite available energy levels being lower, chronically ill people require more energy both at rest AND during all physical activity)
*why these individuals are often fatigued, mostly sedentary
Domain: decline of signaling networks that maintain homeostasis
reflexes & homeostatic mechanisms start to fail including
hormonal signaling via endocrine system
electrical signaling via nervous system
signaling that involves cytokine release and immune function
changes develop in parallel and affect one another
Assessment: decline of signaling networks that maintain homeostasis
labs → nutritional biomarkers (e.g. vitamins, antioxidants), baseline levels of biomarkers & hormone levels, inflammatory markers (e.g. ESR, CRP, IL-6, TNF-ɑ)
other → stress response, response to provocative tests (e.g. OGTT, Dexamethasone test)
Manifestations: decline of signaling networks that maintain homeostasis
Changes in body composition cause (& are, in turn, worsened by) changes in hormonal & cytokine / adipokine regulation of energy balance
example: ↑ fat mass (esp. visceral) → metabolic syndrome → ↓ testosterone, ↑ inflammation
↑ fat mass → insulin resistance
Altered leptin / adiponectin → neurodegeneration
- ↓ testosterone, ↑ inflammation, ↓ IGF-1 (associated with aging) → ↓ in muscle mass / strength
Changes in hypothalamic & autonomic functioning affect nearly all homeostatic maintenance systems
Domain: neurodegeneration
changes in structure & function of nervous system that are thought to be compensatory (attempt by NS to reorganize & compensate for aging) why significant ↓ in function is not always seen in older individuals
early detection of pathological decline requires careful screening / testing!
Assessment: neurodegeneration
PE → objective assessment of gait, balance, reaction time, coordination; standard neurologic exam, including assessment of global cognition
imaging → MRI, fMRI, PET, other dynamic imaging techniques
other → evoked potentials, electroneurography, electromyograph
Manifestations: neurodegeneration
brain atrophy occurs after 60 y/o, proceeding at varying rates in different parts of brain
less coordination b/t brain regions
less localization of cortical activity during tasks requiring executive function
spinal cord changes occur after 60 y/o → ↓ motor neurons, myelin damage
ANS changes → changes in CV & splanchnic function
In older individuals with mild cognitive impairment, atrophy has been found mostly in what 2 regions of the brain?
prefrontal cortex & hippocampus (most important regions for executive function)
true or false: Brain pathology typically associated with specific neurodegenerative diseases has been found upon autopsy in individuals who had normal cognition (as assessed by extensive testing in year prior to death).
true
Rationale: Not all individuals whose brains undergo neurodegenerative histological changes (e.g. amyloid plaques & neurofibrillary tangles typical of Alzheimer’s disease) will experience associated cognitive changes. Research show that learning things and engaging can cause this phenomenon
As the number of motor neurons in the spinal cord decreases with age, the motor neurons that survive compensate via __________ & service to larger / smaller (select one) motor units.
↑ branching, larger
as motor units become larger, they ↓ in # at rate of ~1%/yr (starting after 3rd decade)
contributes to ↓ in fine motor control & manual dexterity
What is frailty?
physiologic syndrome characterized by
↓ reserve & diminished resistance to stressors that results from cumulative decline across multiple physiologic systems
that causes vulnerability to adverse outcomes, disability & a high risk of death
state in which a person has extremely low resistance to stress (i.e. exhibits severe weakness)
altered response to tx
a person who is "frail" is “one step away" from acute decline → sign someone is nearing / in their last stage of life
makes someone susceptible to geriatric syndromes
extreme presentation of phenotype of aging
Why wont aging patients show symptoms outside of decreased level of consciousness?
Immune system is suppressed
What is aging phenotype
outward physical manifestations of aging, including:
presence of multiple coexisting conditions & polypharmacy
impaired stress response, including ↑ susceptibility to disease & limited ability to heal or recover after an acute illness
disability
emergence of geriatric syndromes
5 signs of frailty
included in “Frailty Index”, which has been shown to be reliable predictor of (1) survival in a community dwelling older people & (2) survival, length of stay, & d/c location in acute care settings
1. weight loss
2. fatigue
3. impaired grip strength
4. diminished physical activity
5. slow gait
What is the relationship between frailty & chronic or acute stress?
pre-existing chronic diseases (e.g. DM, CHF) may trigger onset of frailty in an aging person → worsening condition / quality of life → death
frailty can mean that any acute injury, disease, or impairment may trigger a rapid decline in health precipitating significant disability or death
ex: older frail adults who fracture bone as a result of falling are at ↑ risk of mortality within 6 months of injury
4 main clinical consequences of Frailty
Ineffective or incomplete homeostatic response to stress
reduced ability to cope with challenges such as acute diseases
ex. being in a hospital → loss of muscle that they can never recover
infx more likely to become septic
Multiple coexisting diseases (multi- or comorbidity) and polypharmacy
Physical disability
Geriatric syndrome
How does the presence of multiple comorbidities & polypharmacy complicate the diagnosis & treatment of older individuals?
drug tx more complex because comorbid diseases may affect absorption, volume of distribution, protein binding, & elimination of many drugs → fluctuation in therapeutic levels & ↑ risk of under- or overdosing
pt’s with many diseases usually have multiple rx’s from various HCPs who don’t communicate
risk of adverse drug rxn’s, drug-drug interactions, & poor compliance ↑ dramatically with # of rx’s & severity of frailty
measures to minimize adverse effects of polypharmacy
always ask pt’s to bring in ALL medications, including rx drugs, OTC products, vitamin / mineral supplements, herbals (the “brown bag test”)
screen for unnecessary drugs → d/c those without clear indication for use
simplify drug regimens in terms of # of agents & schedules (avoid frequent changes in medications, use single daily dose regimens whenever possible)
avoid drugs that are $$$ and/or not covered by insurance whenever possible
minimize # of drugs to those that are absolutely essential & always check for possible drug-drug interactions
ensure pt or available caregiver understand prescribed regimen
provide legible instructions in the pt's primary language
schedule periodic medication reviews (MTM!)
Why should infections be prevented, anticipated, & assertively treated in older adults?
they're more likely to become septic & resolve more slowly than in younger individuals
should be considered when choosing tx & assessing prognosis (e.g. tx plans may need to be modified to enhance tolerance)
hospitalization & bedrest should be avoided
What 3 biomedical measures do physical & cognitive function in older persons predict more accurately than any others?
1. healthcare utilization
2. institutionalization
3. mortality
Disability occurs early / late (select one) in the frailty process
late (after reserve & compensation have been exhausted)
*if not already frail, headed towards frailty
Interventions aimed at preventing & reducing disability in older adults should have a dual focus on both the ___________ & systems needed for __________.
precipitating cause, compensation
example: fall prevention in older adults should ALSO include balance & strength training (both needed for recovery from fall, if it occurs)
Why do older individuals experience decreased food intake?
↓ energy demand (from ↓ physical activity, lean body mass, & rate of protein turnover)
loss of taste sensation
↑ circulating levels of CCK
↓ stomach compliance
↓ testosterone levels associated with ↑ leptin (males)
when present, diet should be liberalized & dietary restrictions should be lifted as much as possible
nutritional supplements should be given b/t meals to avoid interference with food intake at mealtime
true or false: Decreased food intake is more marked in older female-bodied people than their male-bodied counterparts.
false
Rationale: Decreased food intake is more marked in male-bodied older adults.
What are causes of weight loss in older adults?
anorexia
not the same as anorexia nervosa
cachexia* (body wasting)
sarcopenia*
malabsorption*
hypermetabolism*
dehydration*
recent move to long-term care setting
acute illness (often with inflammation)
hospitalization with bedrest for as little as 1 - 2 days
depression
drugs that cause anorexia and/or N/V (e.g. Digoxin, abx)
swallowing problems
poverty with reduced access to food
isolation
*most common and in some combo
What is cachexia?
weakness & wasting of the body due to severe chronic illness
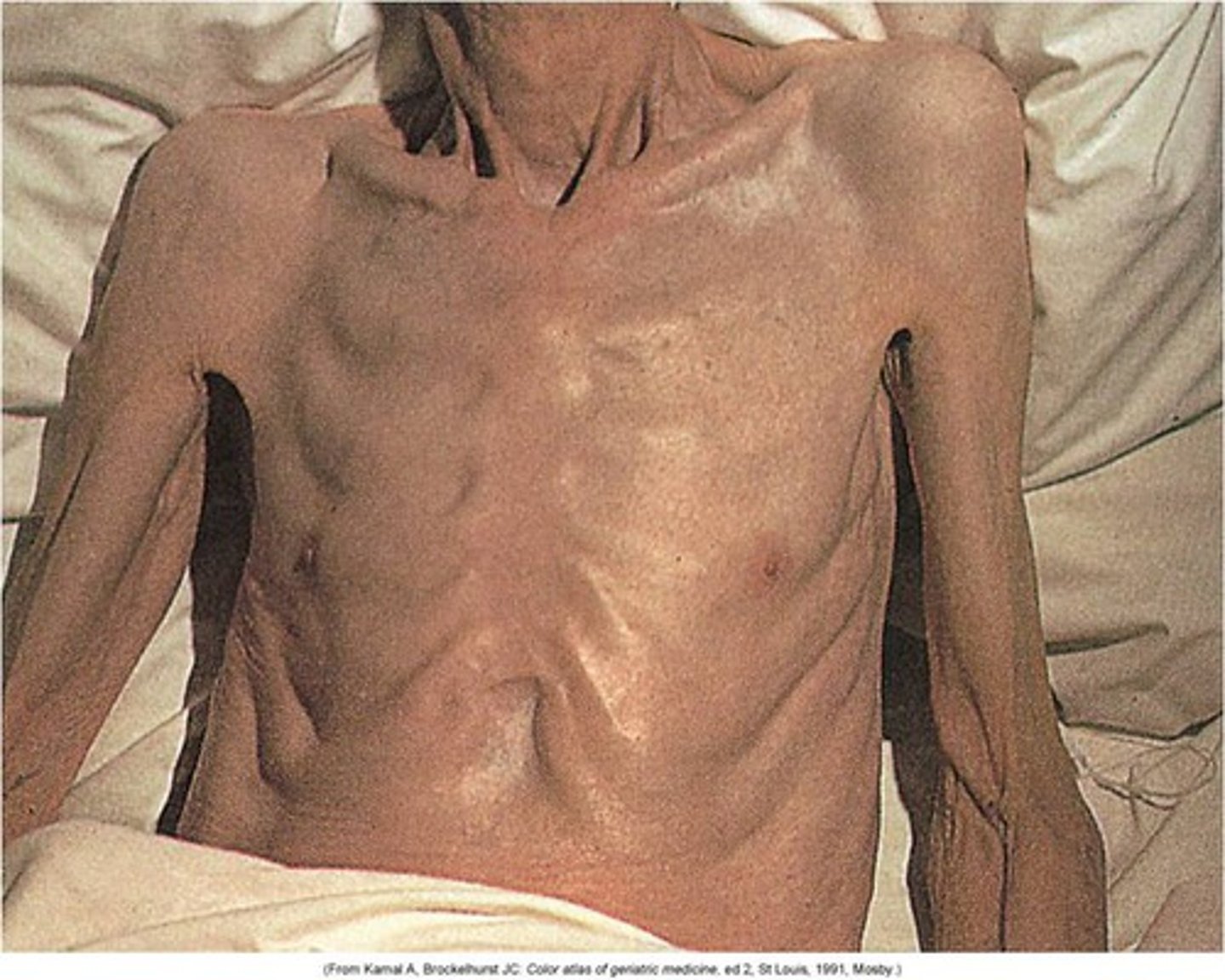
What is sarcopenia?
loss of muscle mass, strength, & function that come with aging
Why should older adult patients' weight be regularly monitored?
because weight loss can be insidious!
should be done both at home & by HCP & maintained in medical record
true or false: There is little evidence that intentional weight loss in overweight older people prolongs life.
true
Rationale: Weight loss after 70 y/o should be limited to persons with extreme obesity & should always be medically supervised.
What are risk factors for gait disorders & falls?
poor muscle strength
neural damage in basal ganglia & cerebellum
DM
peripheral neuropathy
Interventions to prevent & reduce instability & falls in older adults usually require a mix of medical, rehab, & environmental modification approaches, & often include...
medication adjustment
PT
home modifications
vit D supplementation (800 IU daily)
What are risk factors for urinary incontinence?
female-bodied
caucasian
hx of childbirth
obesity
comorbidities
3 types of urinary incontinence
1. stress incontinence
2. urge incontinence
3. overflow incontinence
stress incontinence
failure of the sphincteric mechanism to remain closed when there is sudden ↑ in intra-abdominal pressure (e.g. coughing, sneezing)
causes:
in female-bodied people often d/t insufficient strength of pelvic floor muscles
in male-bodied people almost exclusively 2° to prostate surgery
urge incontinence
sudden sensation of the need to urinate & the inability to control it accompanied by loss of urine
cause: detrusor (bladder) muscle overactivity (i.e. lack of inhibition) d/t loss of neurologic control or local irritation
overflow incontinence
urinary dribbling, either constantly or for some period after urination, d/t overfilling of the bladder
causes:
impaired detrusor contractility d/t denervation (e.g. in DM)
bladder outlet obstruction (e.g. prostate hypertrophy in male-bodied people, cystocele in female-bodied people)
Older female-bodied people are most likely to have what kind of urinary incontinence?
mixed (urge + stress)
What is the first-line treatment for urinary incontinence in older adults?
bladder training associated with pelvic muscle exercises (e.g. Kegel exercises)
What medications associated with urinary incontinence
diuretics
antidepressants
sedative hypnotics
adrenergic agonists / blockers
anticholinergics
CCBs
*whenever possible, d/c these meds in older adults!
What is delirium?
an acutely disturbed state of mind that occurs in fever, intoxication, & other d/o's & is characterized by restlessness, illusions, & incoherence of thought & speech
normal consequence of surgery, chronic disease, or infections in older pt’s
Delirium affects _____ to _____% of hospitalized older adult patients.
15 to 55%
What are risk factors for delirium
dementia
any other condition associated with chronic or transient neurologic dysfunction (e.g. neurologic diseases, dehydration, ETOH use, psychoactive drugs)
sensory (hearing & visual) deprivation
Delirium is an independent risk factor for...
morbidity
prolonged hospitalization
death
frequent features of delirium in older adults
rapid ↓ in LOC with difficulty focusing, shifting, or sustaining attention
cognitive change (e.g. rumbling incoherent speech, memory gaps, disorientation, hallucinations) NOT explained by dementia
PMH suggestive of pre-existing cognitive impairment, frailty, or comorbidity
Tx for acute vs chronic delirium
acute: dementia eval
chronic: cognitive assessment and delirium eval
delirium confirmed → identify and address cause + supportive care + prevent complications + management of s/sx
delirium r/o → r/o depression, mania, and psychosis
What is the most common cause of chronic pain reported by older adults?
MSK d/o’s
neuropathic & ischemic pain also common
Chronic pain in older adults can lead to...
Most common symptom reported by older adults
restricted activity
depression
sleep d/o’s
social isolation
↑ risk for adverse effects of medications
regular analgesic schedules are appropriate & should be combined with non-pharmacologic approaches (e.g. splints, exercise, heat)
According to the CDC, what were the 2 leading causes of death in the USA & Great Britain in 2010?
USA
1. heart disease (24.2%)
2. malignant neoplasms (cancer) (23.3%)
Great Britain
1. malignant neoplasms (28.5%)
2. heart disease (28.3%)
trajectory 1 of death
sudden death (e.g. acute MI, trauma)
trajectory 2 of death
short period of evident decline (e.g. cancer)
trajectory 3 of death
long-term limitations with intermittent serious episodes of illness (e.g. organ failure)
trajectory 4 of death
prolonged dwindling (e.g. frailty, dementia)
*more likely to experience this kind of death with increasing age
What trajectory(ies) to death is/are most common in industrialized countries?
trajectories 3 & 4
For most people, death is a __________, not an event.
process
*as timeline to death gets more abbreviated, there are transitions of care & appropriate changes in location & goal of that care
A person with months to weeks to live is considered to have a __________, while someone with days to live is considered to be __________.
terminal illness ("end of life"), actively dying
Why are vital signs not very helpful with respect to signaling onset of death?
they're highly variable & can remain quite stable until just before the moment of death
*HR is only sign that tends to significantly ↑ (relative to other VS)
What are clinical signs typically seen in last 1 - 3 days of life
- periods of apnea
- Cheyne-Stokes respirations
- respiration with mandibular movement
- death rattle
- dysphagia of liquids
- ↓ LOC
- ↓ performance status
- peripheral cyanosis
- pulselessness of radial artery
- cessation of urine output
What is apneic breathing
prolonged pauses between each breath; also called “brainstem breathing” (compensatory mechanism to relieve acidosis)
criteria for (+): < 30 sec; 30 - 60 sec; > 60 sec
Apneic breathing is a sign of impending death that, on average, has been found to begin roughly how many days before the actual time of death?
1.5 days
What is Cheyne-Stokes respiration?
alternating periods of apnea & hyperapnea with a crescendo-decrescendo pattern
criteria for (+): present
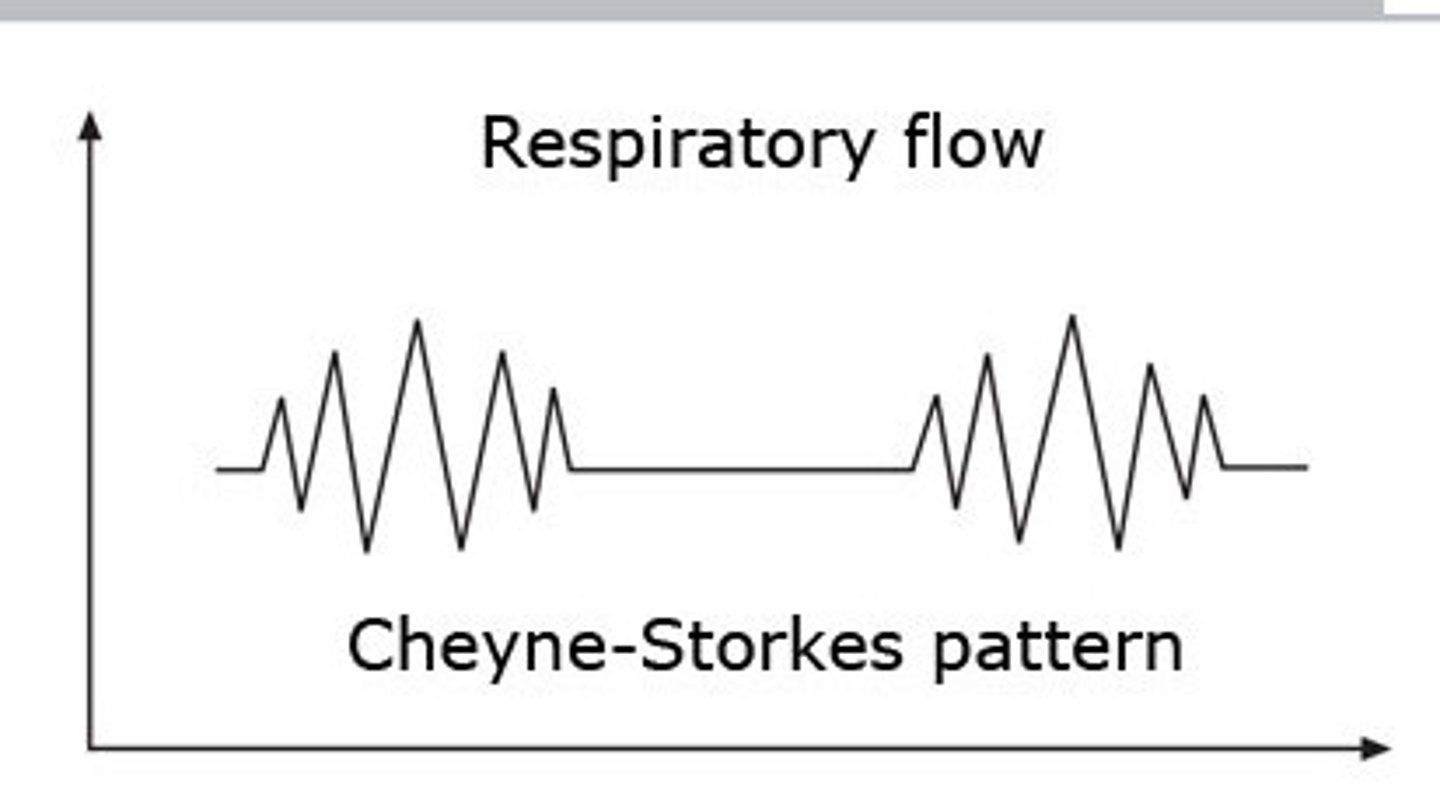
Cheyne-Stokes respiration is a sign of impending death that, on average, has been found to begin roughly how many days before the actual time of death?
2 days
What is the death rattle
gurgling sound produced on inspiration and/or expiration R/T airway secretions that accumulate d/t increasing coma & loss of gag reflex / ability to swallow
criteria for (+): audible if very close; audible at the end of bed; audible > 6 m from door of room
*loved ones may perceive that the pt is choking
*can be improved with enhanced positioning & anticholinergic agents (e.g. Scopolamine)
Scopolamine
anticholinergic agent, antiemetic
SE:
- tachycardia
- dissociation (may be an advantage or disadvantage, depending on the pt)
Death rattle is a sign of impending death that, on average, has been found to begin roughly how many days before the actual time of death?
1.5 days
What 2 common breathing patterns are observed leading up to the time of death?
1. apneic breathing
2. Cheyne-Stokes respirations
Respiration with mandibular movement is a sign of impending death that, on average, has been found to begin roughly how many days before the actual time of death?
1.5 days
dysphagia of liquids
difficulty with fluid intake
criteria for (-): absent
criteria for (+): present
Dysphagia of liquids is a sign of impending death that, on average, has been found to begin roughly how many days before the actual time of death?
7 days
How is decreasing level of consciousness quantified in an individual who is actively dying?
Richmond Agitation Sedation Scale
criteria for (-): -1 to 4
criteria for (+): -2 to -5
Decreased level of consciousness is a sign of impending death that, on average, has been found to begin roughly how many days before the actual time of death?
7 days
How is decreasing performance status quantified in an individual who is actively dying?
Palliative Performance Scale (PPS) to assess function (from 0 - 100%)
criteria for (-): 30 - 100%
criteria for (+): ≤ 30% (bed-bound, completely dependent (i.e. requires total care)
What 5 factors does the PPS take into account?
1. ambulation
2. activity & evidence of disease
3. self-care
4. intake
5. LOC