14. Anti-amoebic and Anti-malarial Drugs
1/29
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
List protozoal diseases.
Amoebiasis
Giardiasis
Trichomoniasis
Toxoplasmosis
Leishmaniasis
Trypanosomiasis
Define and describe amoebiasis.
Intestinal infection caused by Entamoeba histolytica
Asymptomatic or may present with mild to moderate colitis or as dysentery or as liver abscess
Drug therapy needed for acutely ill patient and asymptomatic patients
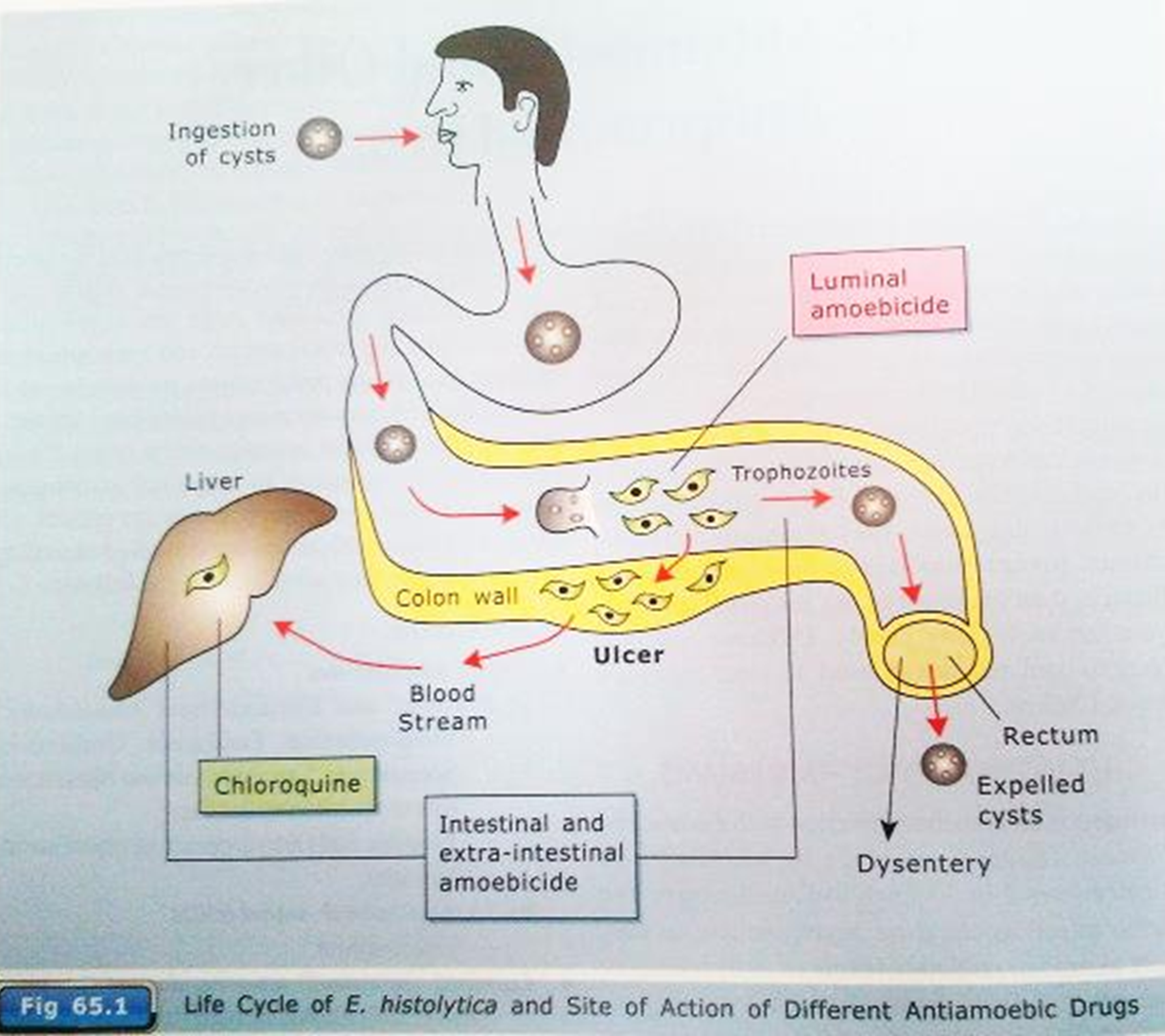
List the types of amoebicides.
Tissue amoebicides (destroy amoeba that have invaded tissue; tissue phase is only secondary to intestinal amoebiasis; hence, in tissues, only trophozoites present not cysts)
Luminal amoebicides
List tissue amoebicides.
Metronidazole
Tinidazole
Ornidazole
Chloroquine
List luminal amoebicides.
Diloxanide furoate
Antibiotics - tetracycline
Tissue Amoebicides
Describe the mechanism of metronidazole.
Forms reduced cytotoxic compounds that bind to proteins and DNA, resulting in death of E. histolytica trophozoites
Tissue Amoebicides
List the adverse effects of metronidazole.
Nausea
Vomiting
Metallic taste
Epigastric distress
Anorexia
Transient neutropenia
Tissue Amoebicides
List the contraindications of metronidazole.
Neurological disease
First trimester of pregnancy (mutagenic potential)
Not to be taken with alcohol - disulfiram-like effects produced
Tissue Amoebicides
List the uses of metronidazole.
Amoebiasis: drug of choice for all forms (intestinal or extraintestinal)
Giardiasis: highly effective
Trichomonas vaginalis: drug of choice
Anaerobic bacterial infections
Pseuodomembranous enterocolitis: drug of choice
Ulcerative gingivitis: drug of choice for acute condition
H. pylori peptic ulcer: used w/amoxicillin or clarithromycin and PPI
Guinea worm infestation: niridazole
Tissue Amoebicides
Describe chloroquine and what it is used for.
Kills trophozoites of E. histolytica and is highly concentrated in liver
Used for hepatic amoebiasis
Tissue Amoebicides
List the adverse effects of chloroquine.
Toxicity is low but adverse effects are frequent and unpleasant:
Bitter taste
May cause nausea
Vomiting
Visual defects
Loss of hearing
Luminal Amoebicides
Describe diloxanide furoate and how it works.
Highly effective luminal amoebicide
Directly kills trophozoites (acute amoebiasis)
Effective against cyst forms of amoeba
Effective in treating asymptomatic carriers of amoebiasis
Not active against tissue trophozoites
Drug of choice for mild intestinal/asymptomatic amoebiasis, and is given after any tissue amoebicide to eradicate cysts
Luminal Amoebicides
List the side effects of diloxanide furoate.
Minimal side effects, well tolerated: flatulence, occasional nausea, and itching
Malarial parasite is a single cell protozoan called Plasmodium. List clinically important species of Plasmodium.
Plasmodium vivax
Plasmodium falciparum
Plasmodium ovale
Plasmodium malariae
Describe malaria and its symptoms.
Incubation period - 7-30 days
Brief prodromal period with symptoms of fever, headache, and myalgia
Symptoms begin with a cold stage (a shaking chill), following by a fever stage (40–41°C) that lasts about 24 hours, and finally a wet stage
The wet stage occurs several hours after the fever, when the body temperature drops quickly to normal and profuse sweating begins; patient is exhausted but well until the next cycle of fever begins
Other symptoms include splenomegaly and anemia
List and describe the 3 basic types of malaria.
Benign tertian (P. vivax and P. ovale): fever every second day
Benign quartan (P. malariae): fever every third day
Malignant tertian (P. falciparum):
cold stage is less pronounced and fever stage is more prolonged and intensified
fever usually continuous or briefly remittent
no wet stage
this type more dangerous because of complications caused by capillary blockage
large no. of RBC parasitized and destroyed = dark urine
Which 2 species of Plasmodium can remain in the liver if not treated properly? What happens when they remain in liver?
P. vivax and P. ovale
Organisms leave liver and reinfect RBC, causing symptoms
Relapsing malaria occurs when there are relapses many years after initial episode of malaria
Describe the life cycle of malarial parasite/Plasmodium.
Complex life cycle
Alternating cycle of asexual division in human beings (intermediate hosts)
Sexual development occurs in female mosquito (anopheline, definitive host)
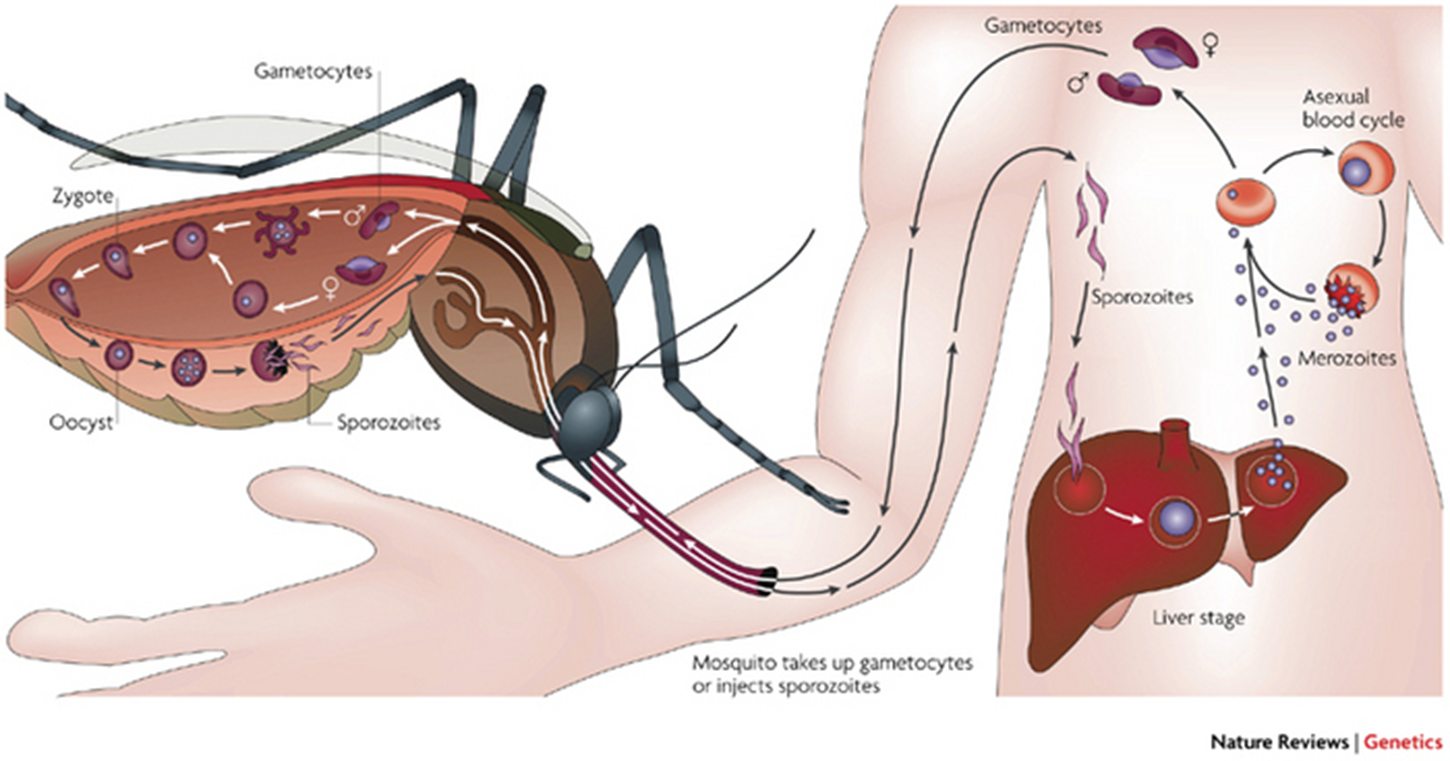
List the objectives of anti-malarial therapy.
Treat and prevent clinical attack of malaria
Completely eradicate the parasites from patient’s body
Reduce human reservoir of infection
List anti-malarial drugs.
Chloroquine
Mefloquine
Proguanil
Primaquine
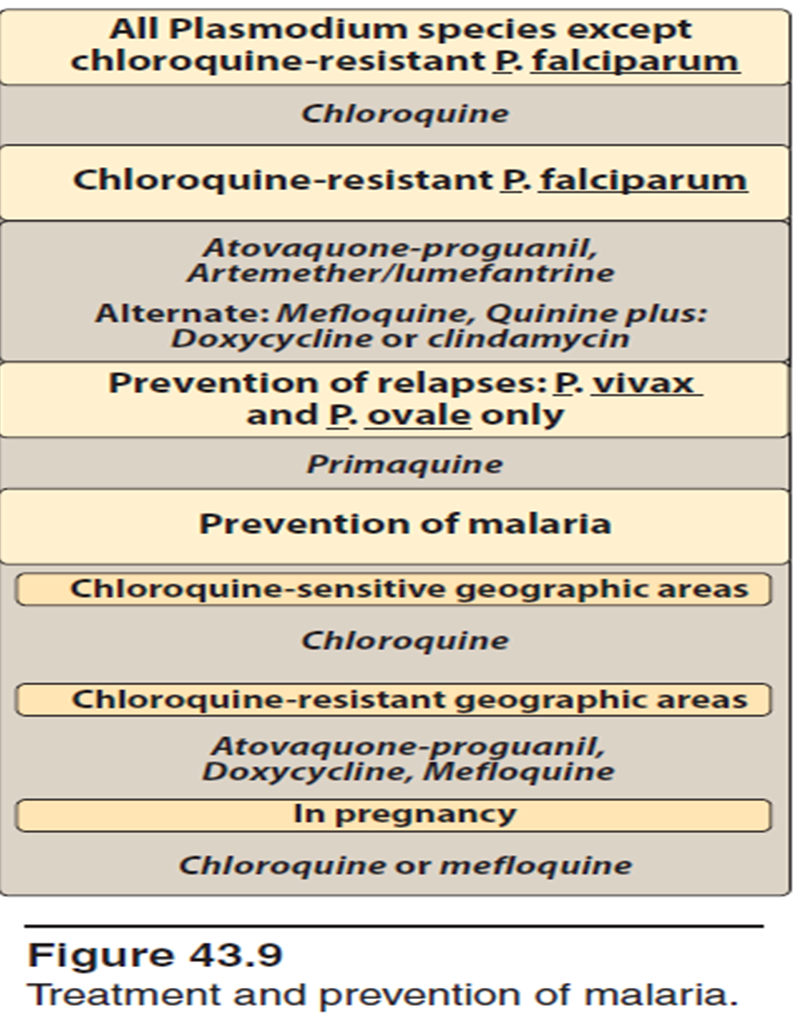
List the clinical uses of anti-malarial drugs.
Causal prophylactics
Suppressive prophylaxis/chemoprophylaxis
Clinical cure
Radical cure
Causal Prophylactics
The ________________ phase (_____) which is the cause of malarial infection and clinical attacks is the target. They prevent __________ of ____________ to _________ within the infected hepatic cells target.
pre-erythrocytic
liver
maturation
sporozoites
schizonts
List causal prophylactics.
Proguanil
Primaquine
Suppressive Prophylaxis/Chemoprophylaxis
Do not affect the _______ phase. Destroy the ___________ released from the _____, so that the development of ____________ stage is prevented. They are mainly blood _______________.
hepatic
merozoites
liver
erythrocytic
schizonticides
When is suppressive prophylaxis employed?
During period of exposure to infected mosquitoes and for some weeks after
List drugs used for suppressive prophylaxis/chemoprophylaxis.
Chloroquine
Proguanil + chloroquine
Mefloquine
Doxycyline
Clinical Cure
The ________ ____________ __________ state of malarial parasite is responsible for clinical symptoms (fever, chills). Hence, blood _______________ can be used to terminate an acute attack of malaria.
asexual erythrocytic schizogony
schizonticides
List drugs used for clinical cure.
Fast-acting high efficacy drugs: chloroquine, mefloquine
Slow-acting low efficacy drugs: proguanil
Faster-acting drugs preferred for P. falciparum
Radical Cure
Eradication of both ________________ and ____________ state of malarial parasite leads to radical cure of malaria. Adequate clinical cure of P. falciparum with ____________ results in radical cure.
exoerythrocytic
erythrocytic
chloroquine
Which drug is used for radical cure?
Primaquine