GI physiology 1: Upper GI tract
1/181
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
182 Terms
What are the 6 major functions of the mammalian GI tract?
ingestion of food
secretion of fluids and digestive enzymes
mixing and movement of food and wastes through the body
digestion of food into smaller pieces
absorption of nutrients
excretion of wastes
What direction does movement in the GI tract go in?
unilateral
What are the clinical terms used to describe the parts of the GI tract?
upper and lower
What are the embryological terms used to describe the parts of the GI tract?
upper/fore, mid, lower/hind
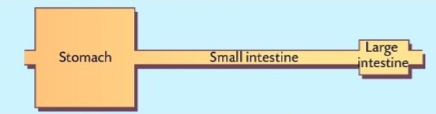
What animals does this relate to?
carnivores
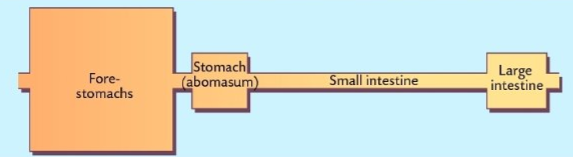
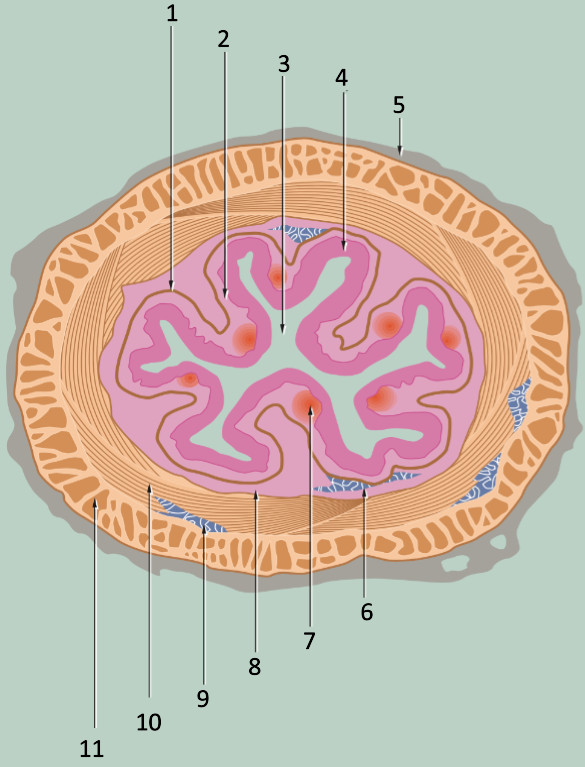
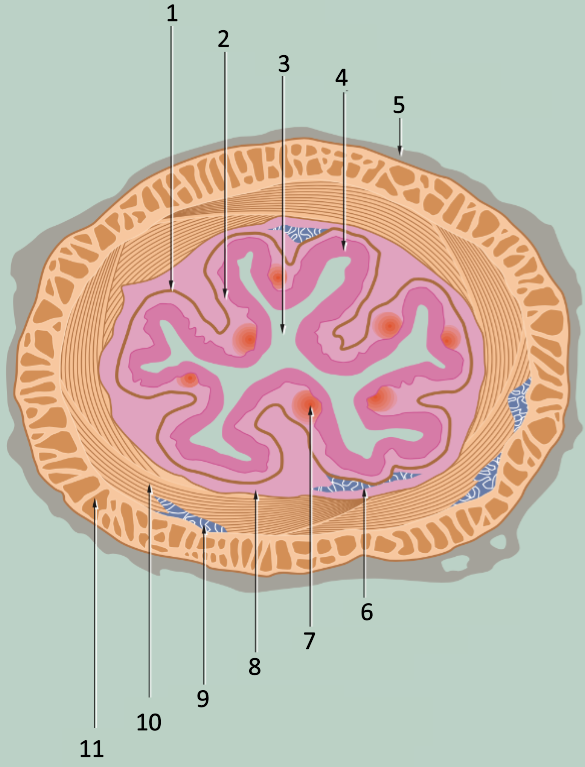
What animals does this image relate to?
ruminants
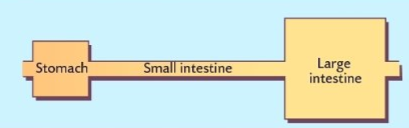
What animals does this image relate to?
simple-stomached herbivores
What do herbivores utilise for digestion?
microbial fermentation
Why do herbivores utilise microbial fermentation?
structural carbohydrates not digested by mammalian enzymes
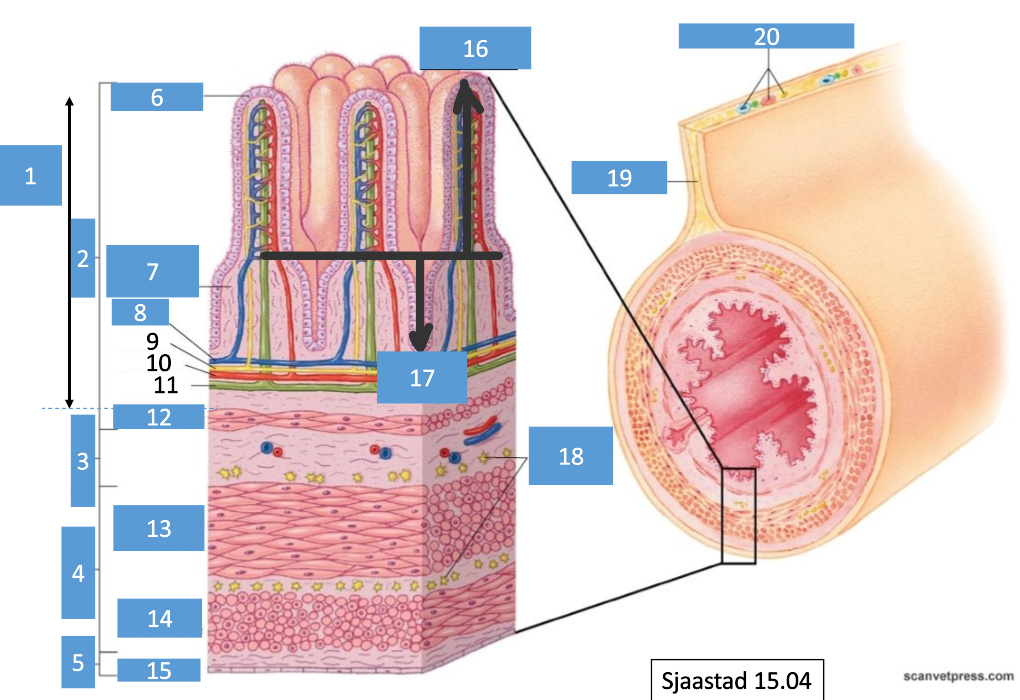
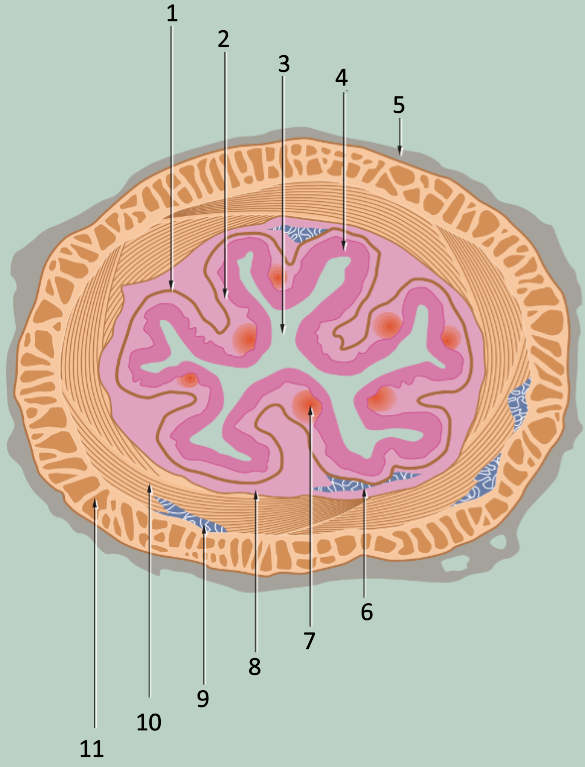
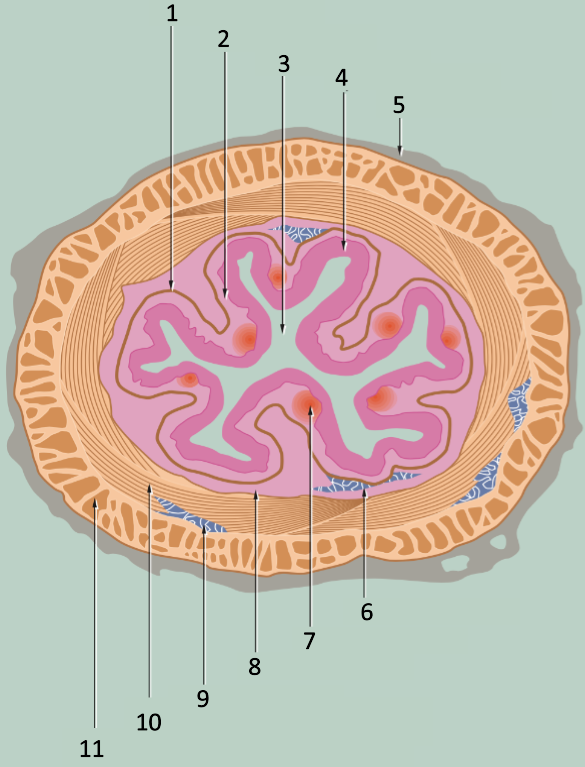
1
lamina propria
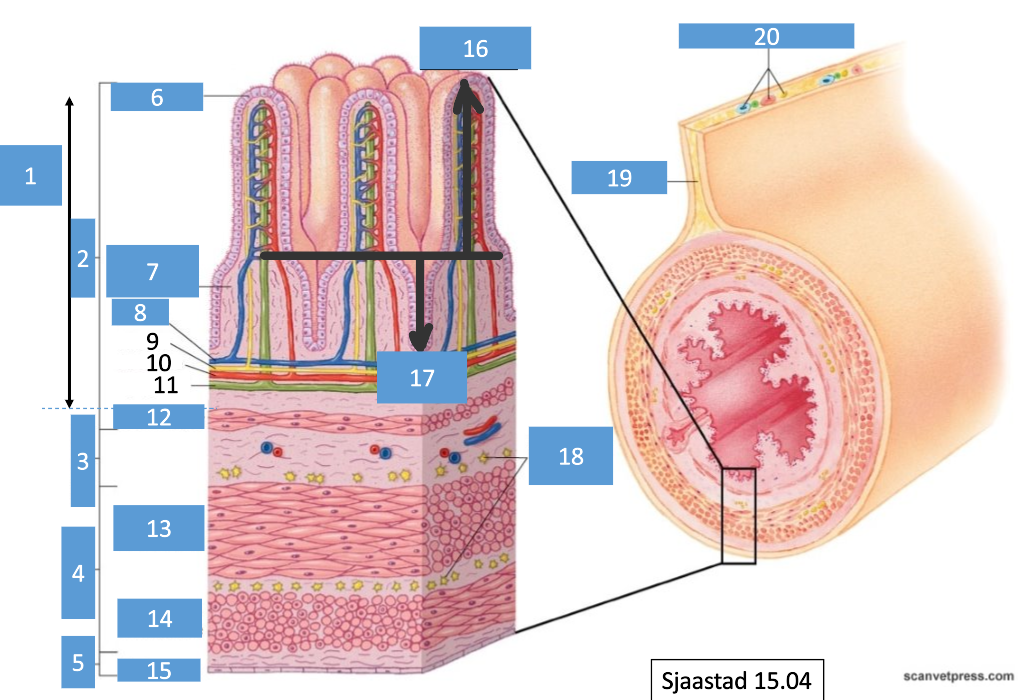
2
mucosa
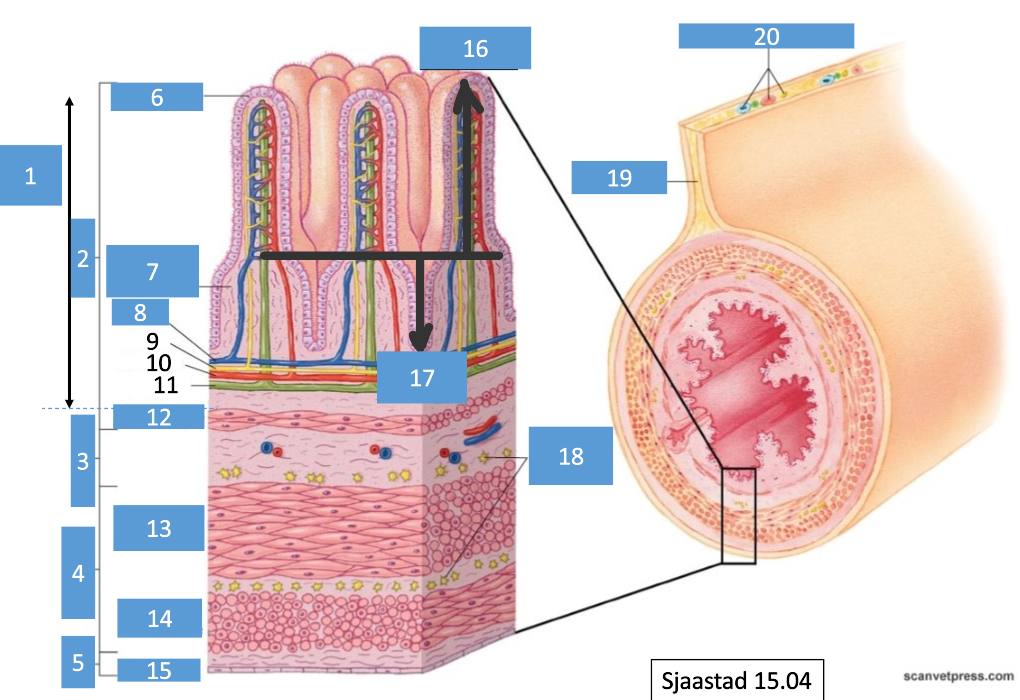
3
submucosa
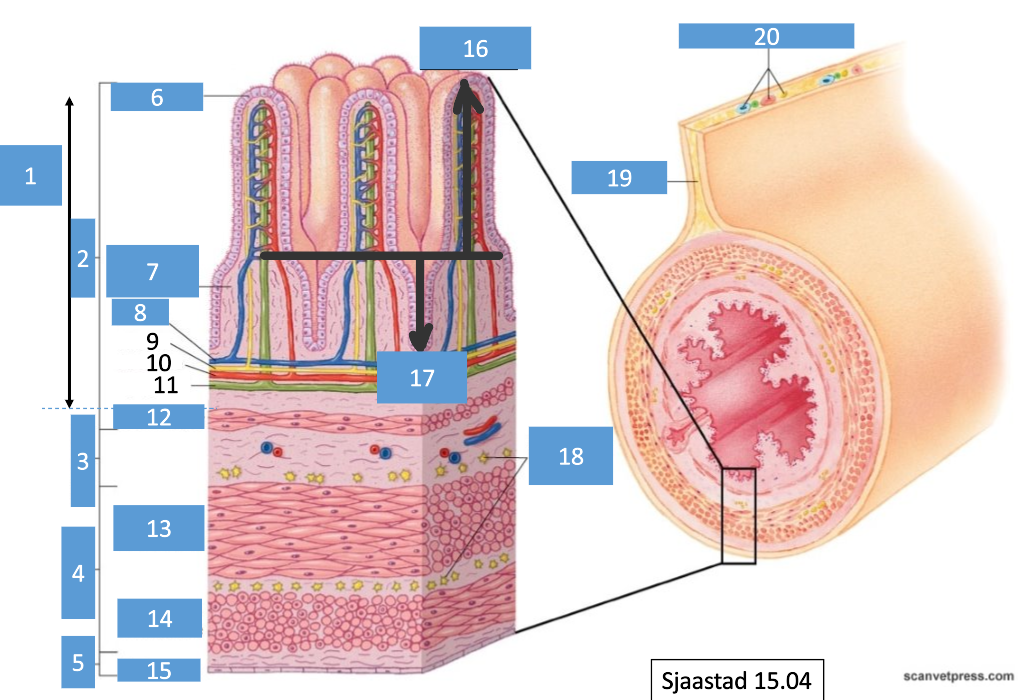
4
muscularis
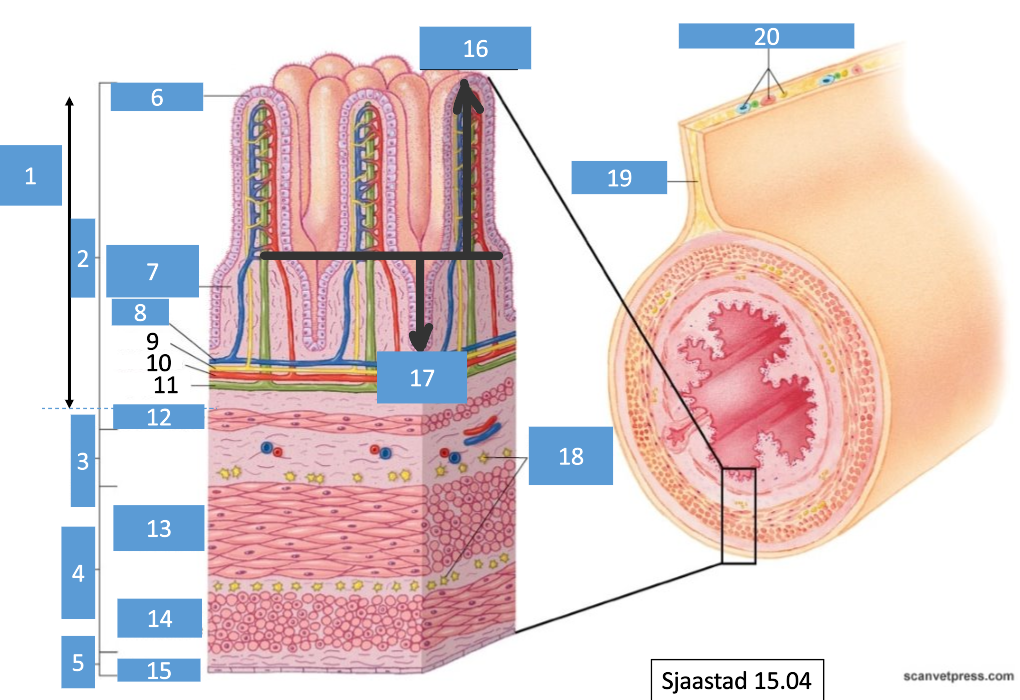
5
serosa
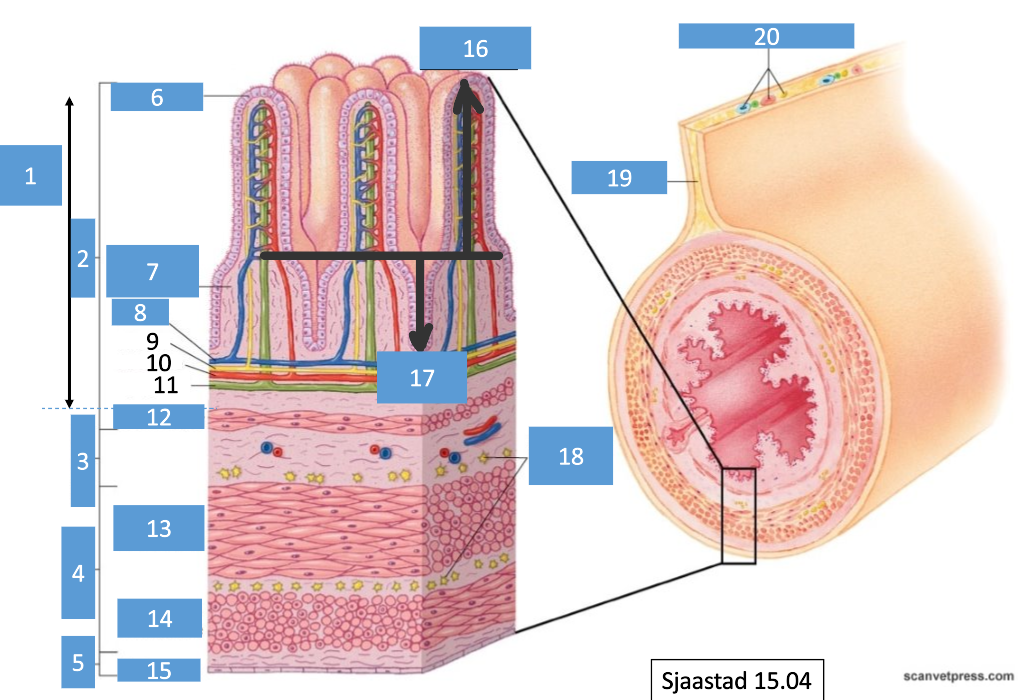
6
epithelium
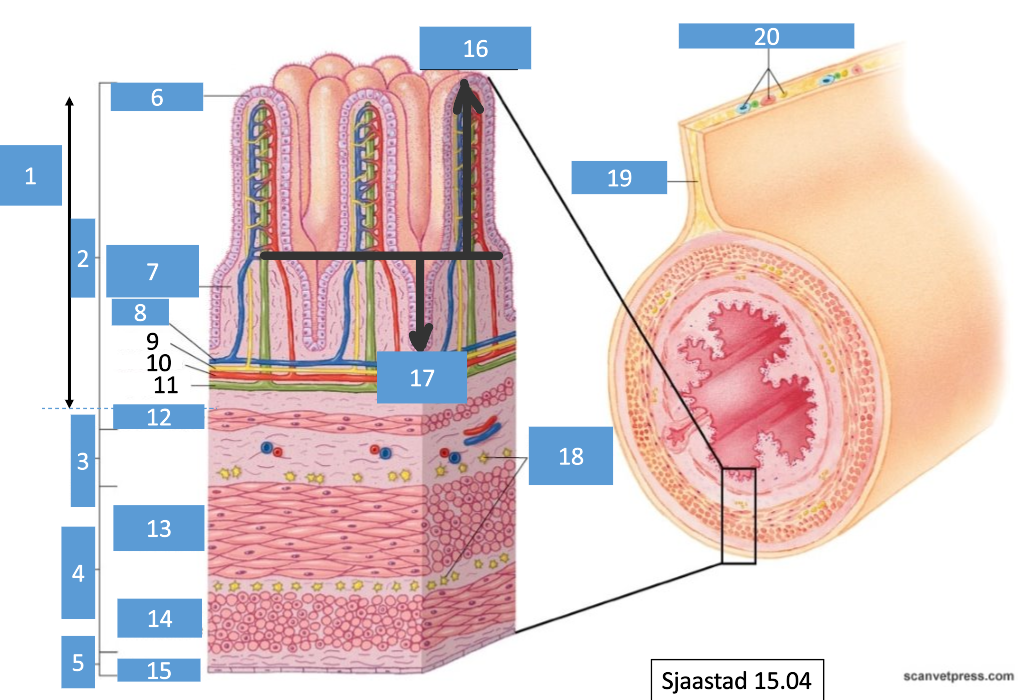
7
connective tissue
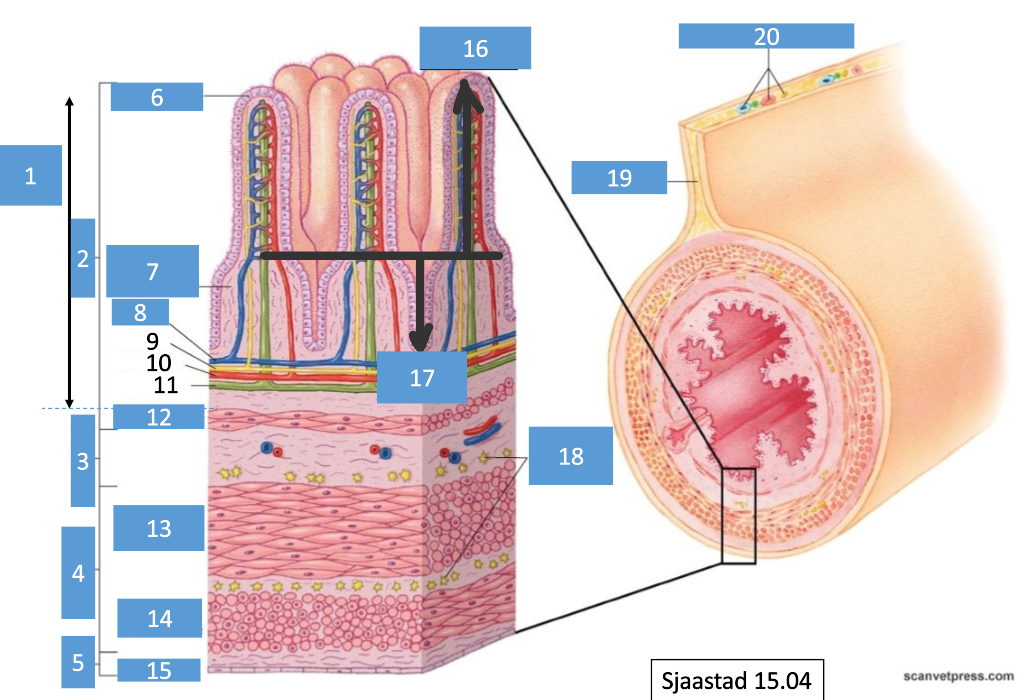
8
venule
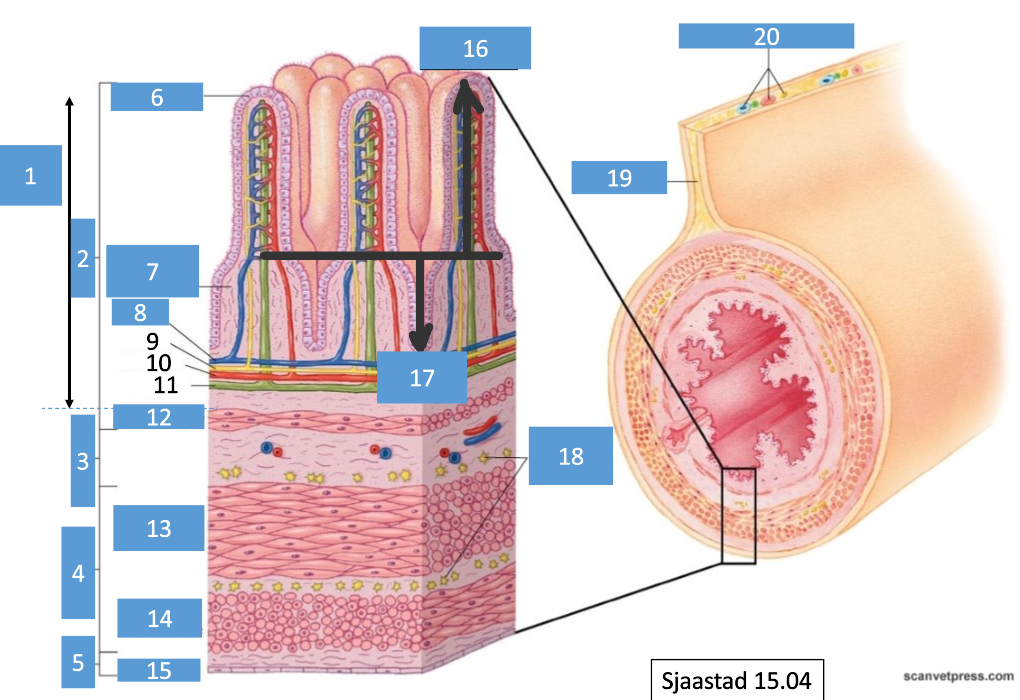
9
nerve
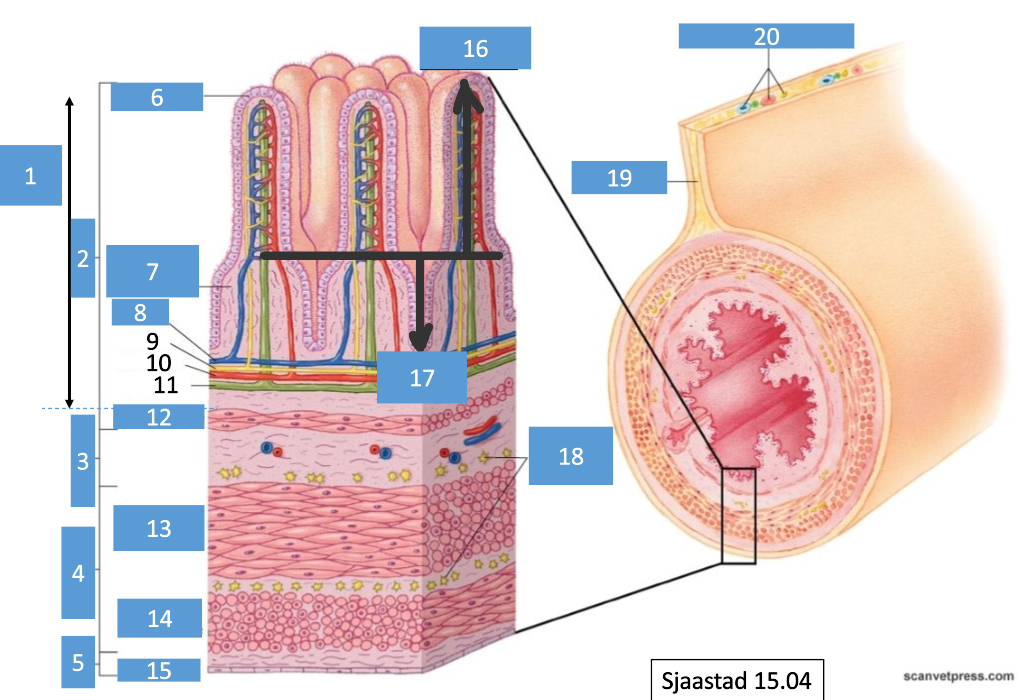
10
arteriole
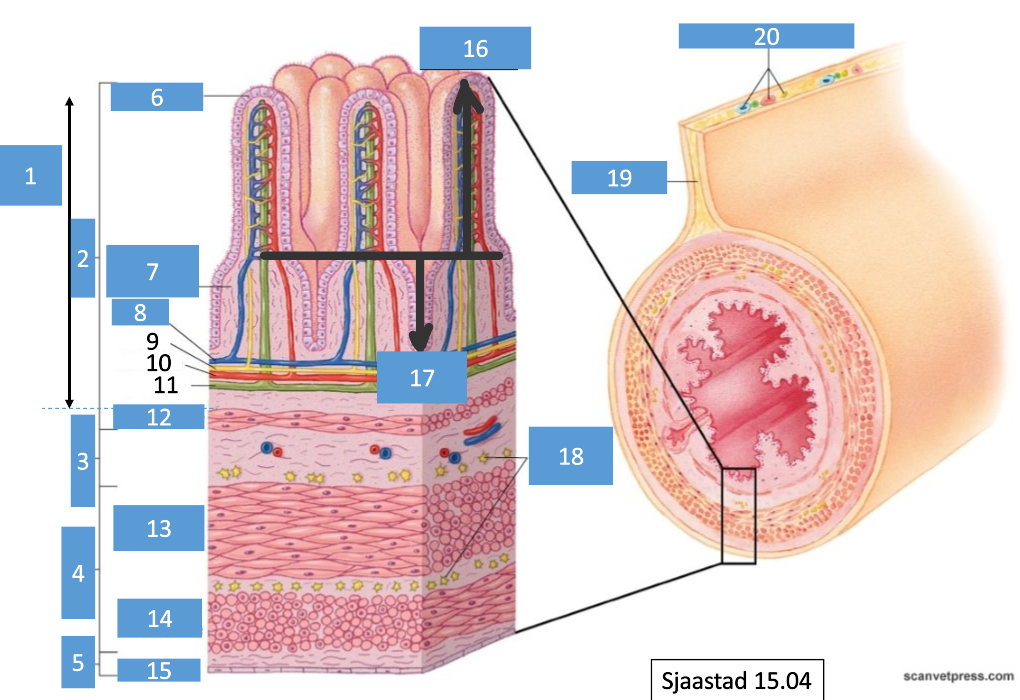
11
lymphatic
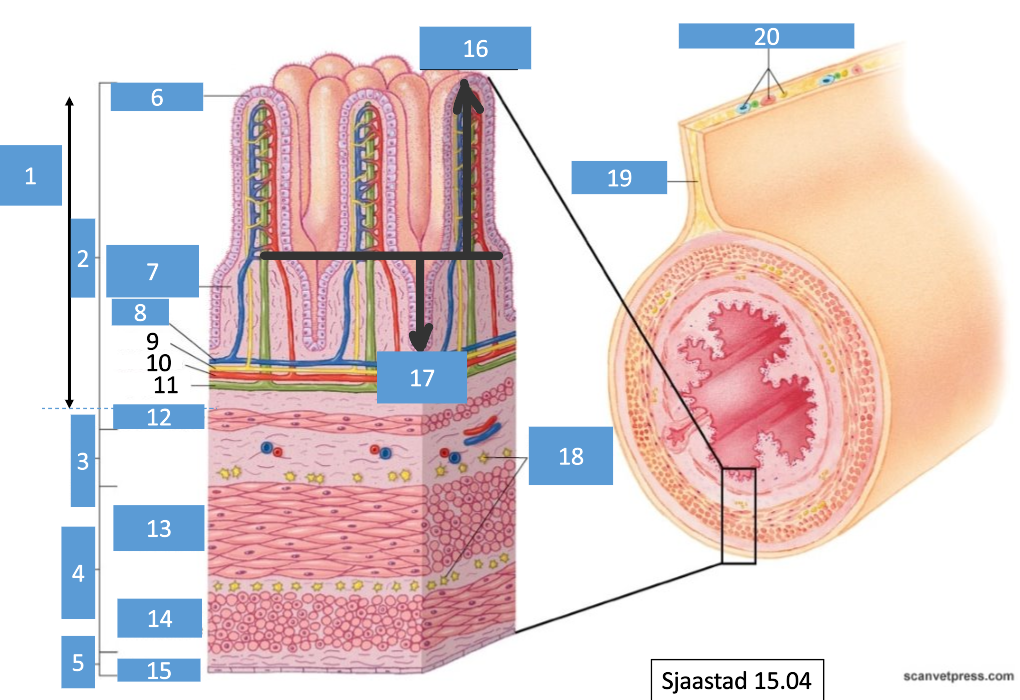
12
muscle layer
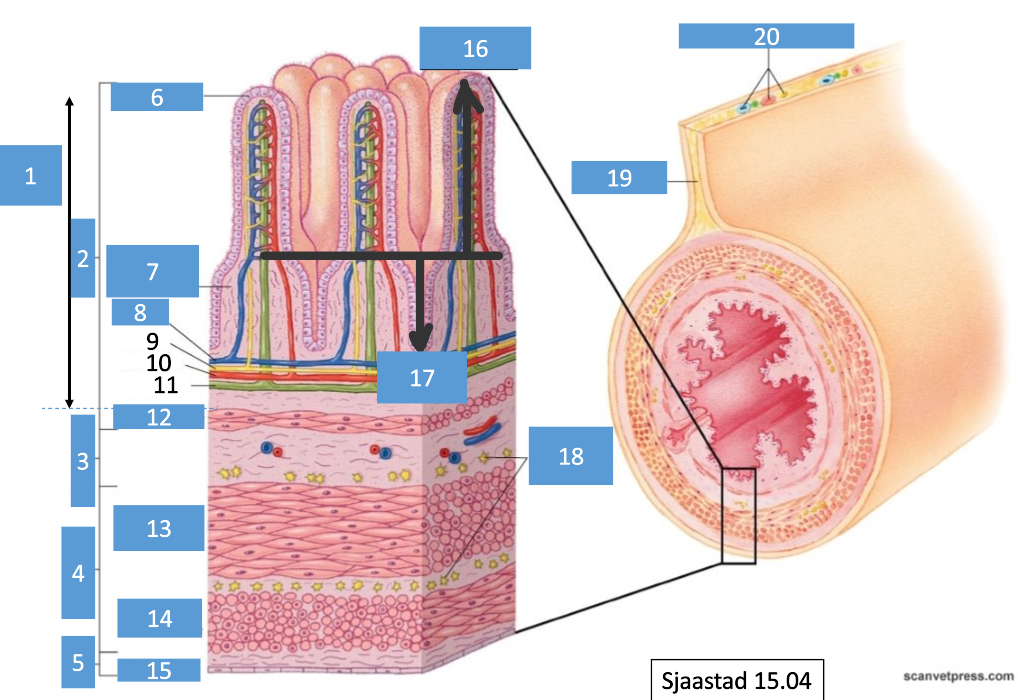
13
circular musculature
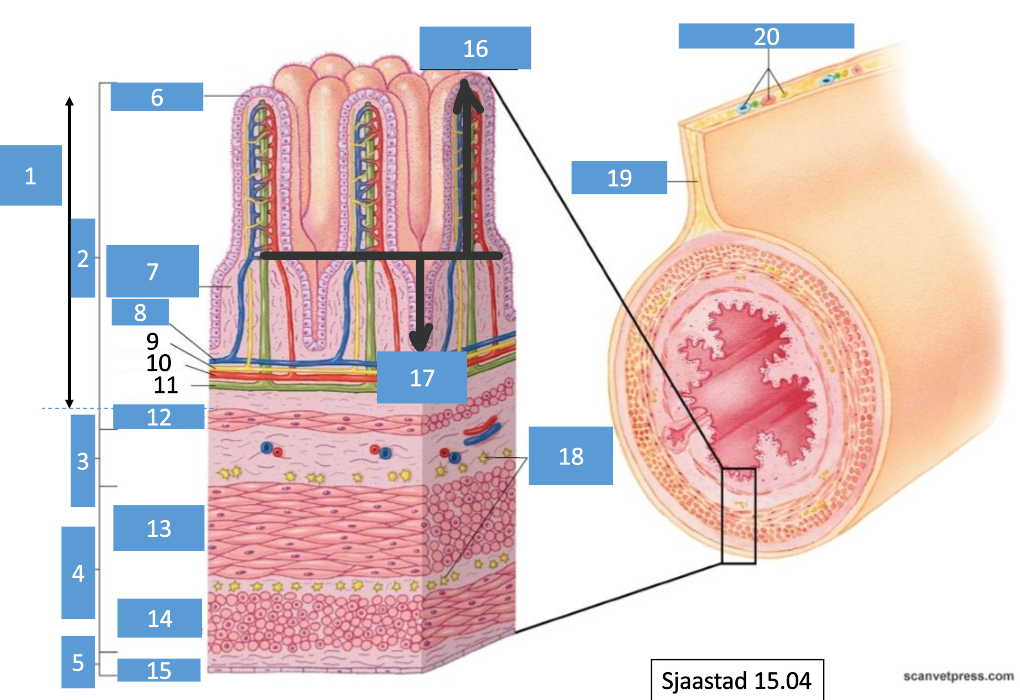
14
longitudinal musculature
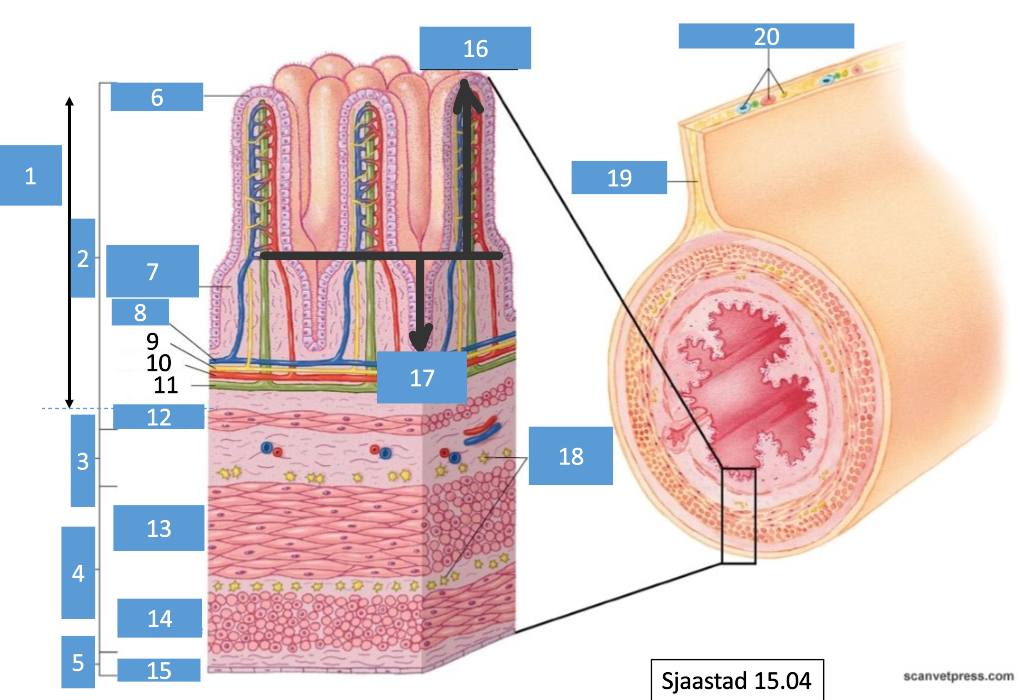
15
peritoneum
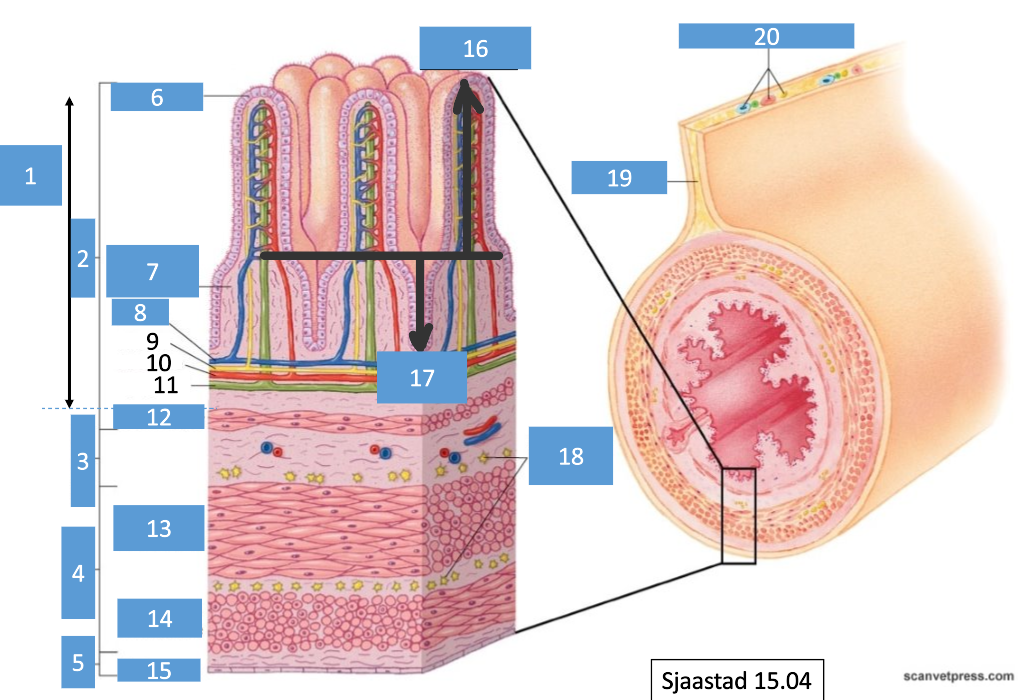
16
villus
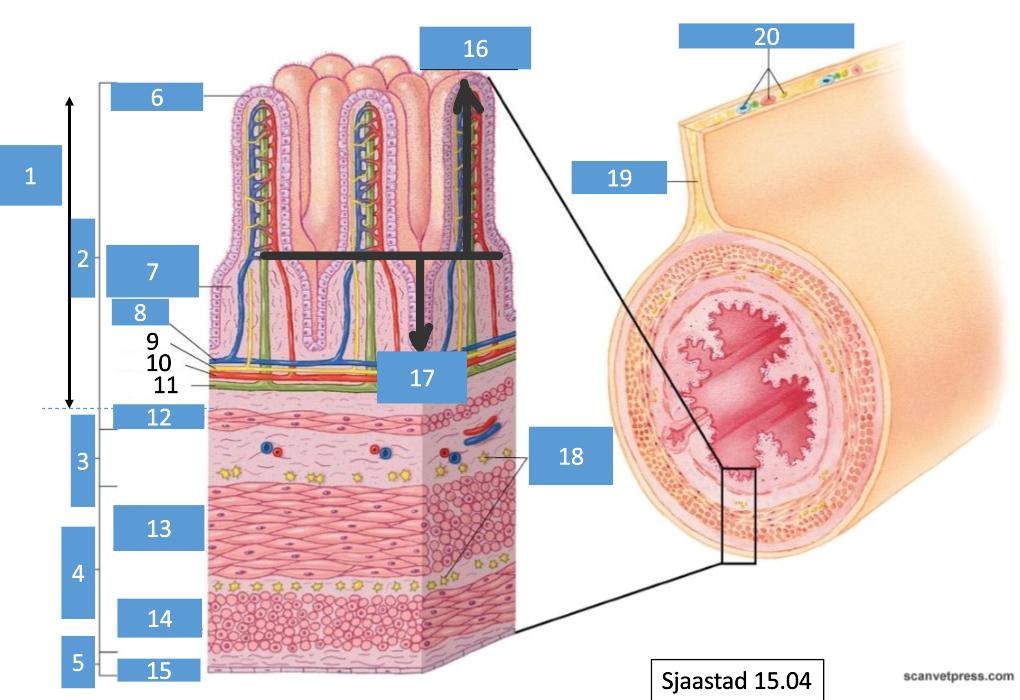
17
crypt
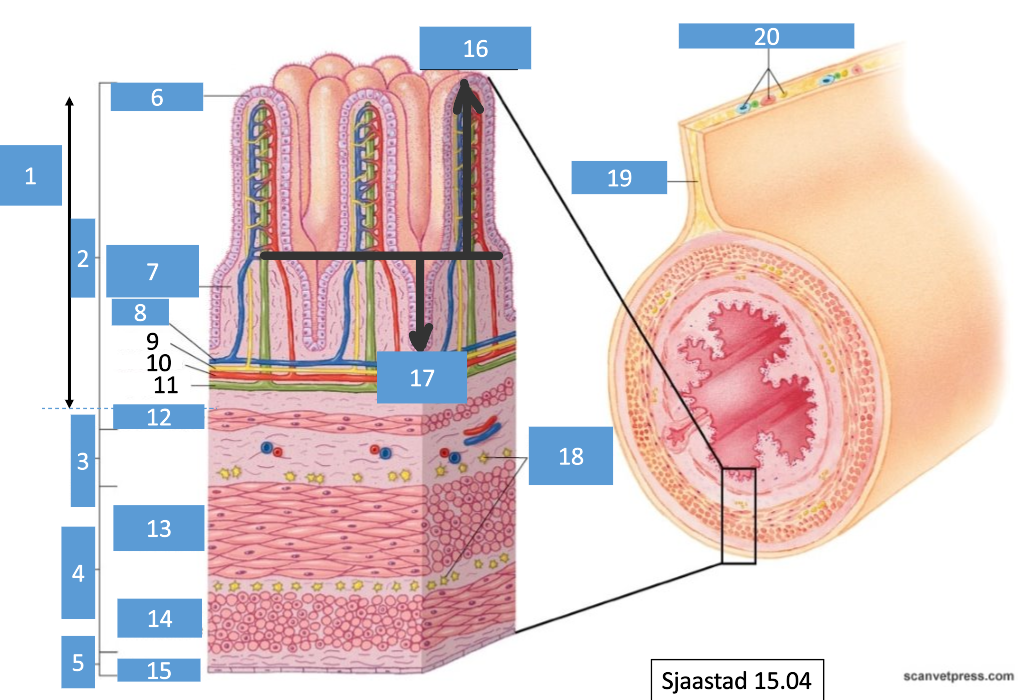
18
network of nerve cells
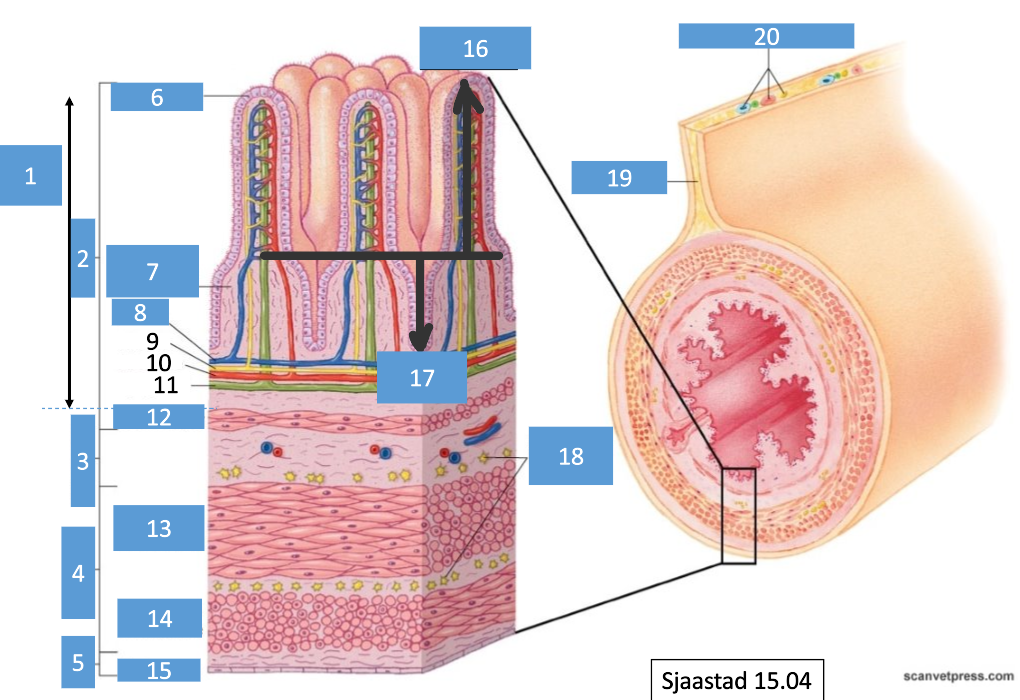
19
mesentery
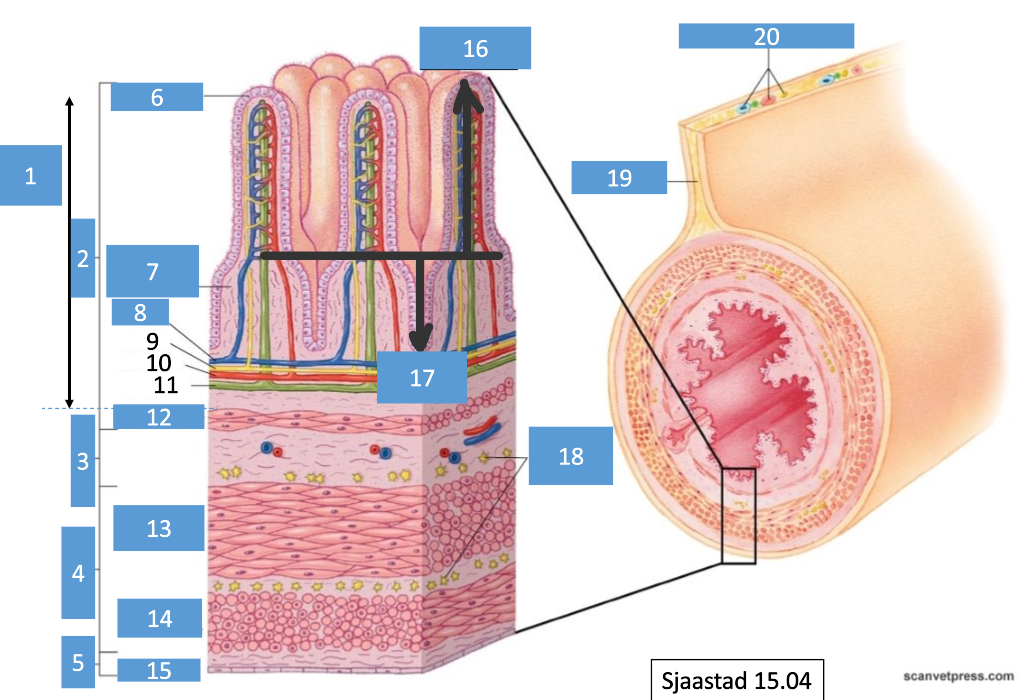
20
nerve and blood vessels
Do the crypts secrete or absorb?
secrete
Do the villi secrete or absorb?
absorb
What does the circular muscle layer do to GI tract?
contract to decrease diameter
What does the longitudinal muscle layer do to the GI tract?
contract to shorten length
What are the 4 distinct functional layers of the GI tract?
mucosa, submucosa, muscularis propria and adventitia
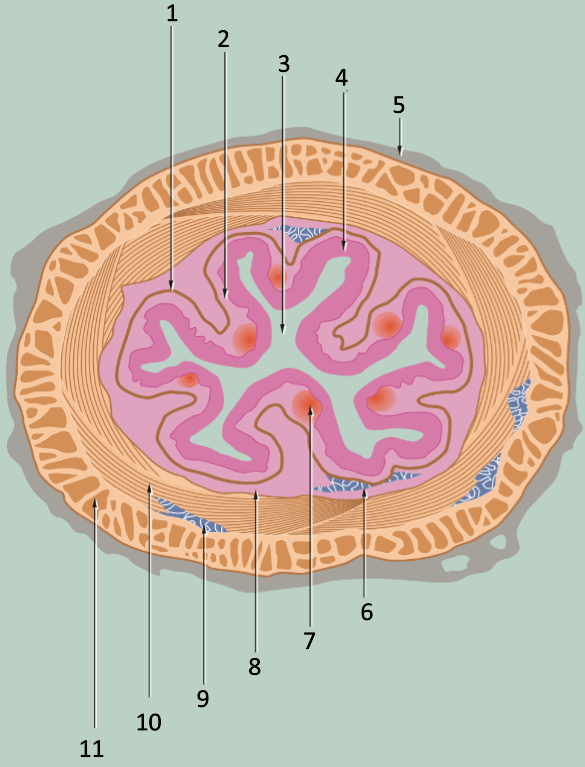
1
muscularis mucosae
2
lamina propria
3
lumen
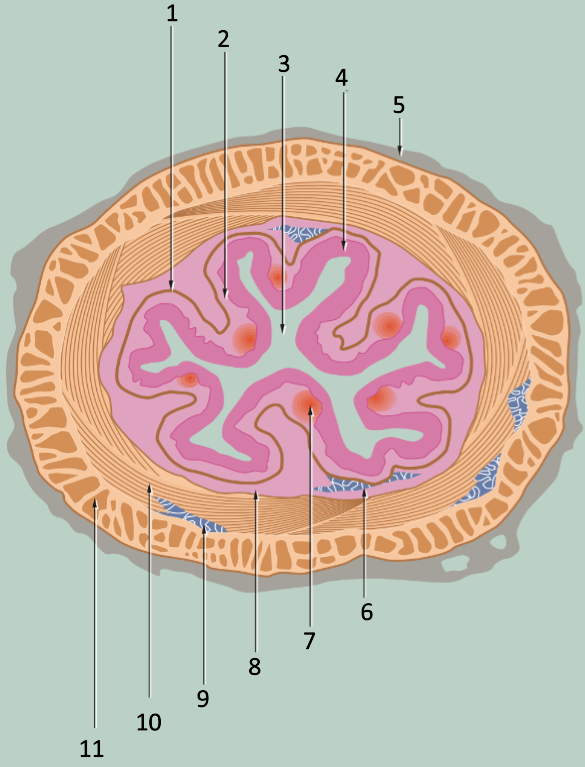
4
epithelium
5
adventitia
6
submucosal plexus
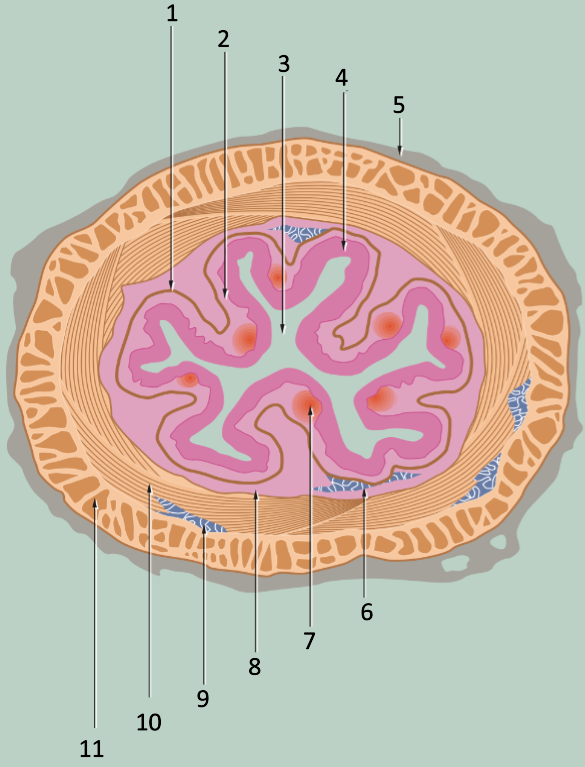
7
lymphoid aggregate
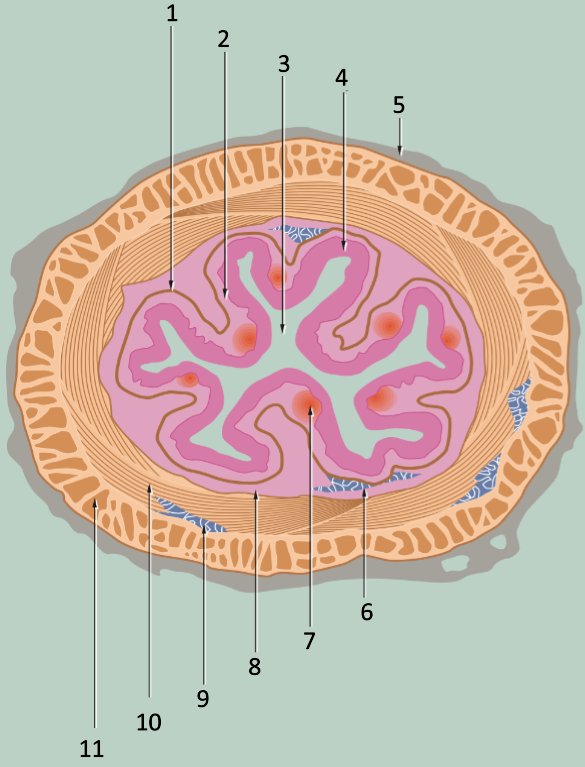
8
submucosa
9
myenteric plexus
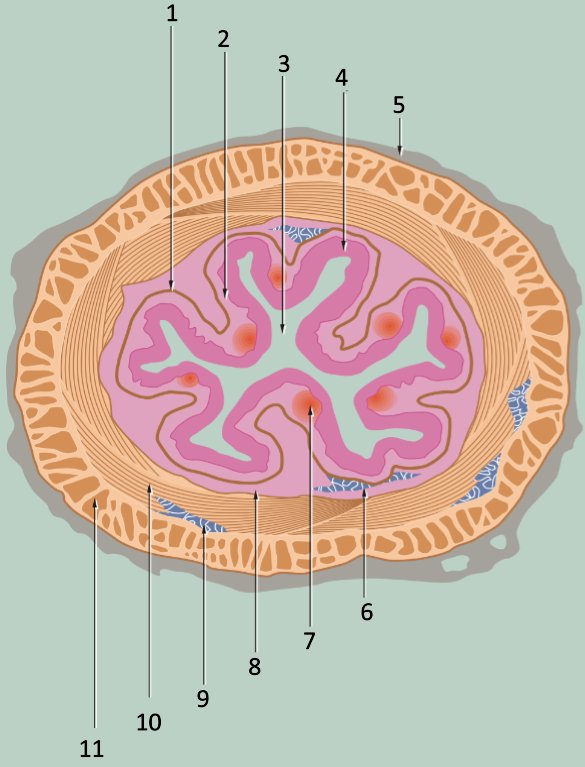
10
muscularis propria: inner circular layer
11
muscularis propria: outer longitudinal layer
What 3 components make up the mucosa?
epithelium, lamina propria, muscularis mucosae
What does the muscularis mucosae do?
produce local movement and folding of mucosa
submucosa
layer of loose collagenous connective tissue supporting mucosa & containing larger blood vessels, lymphatics and nerves
muscularis propria
smooth muscle usually arranges as inner and outer longitudinal layer
What are the 2 layers of the muscularis propria the basis of?
peristaltic contraction
Adventitia
outer layer of loose supporting tissue conducts major vessels, nerves and contains variable adipose tissue
In the gut, what is the adventitia (serosa) lined with?
simple squamous epithelium
What increases the surface area in the GI epithelia?
folding of mucosa
villi
microvilli
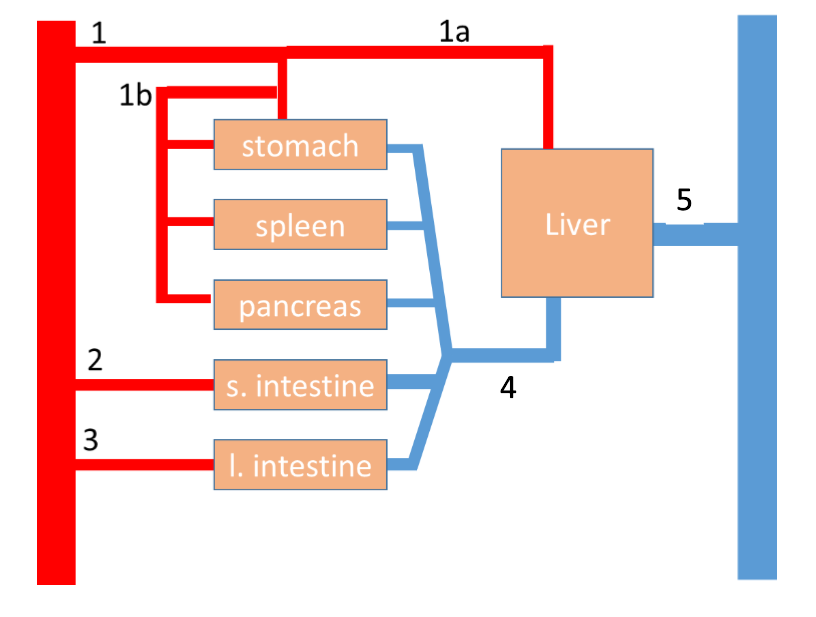
1
celiac artery
2
cranial mesenteric artery
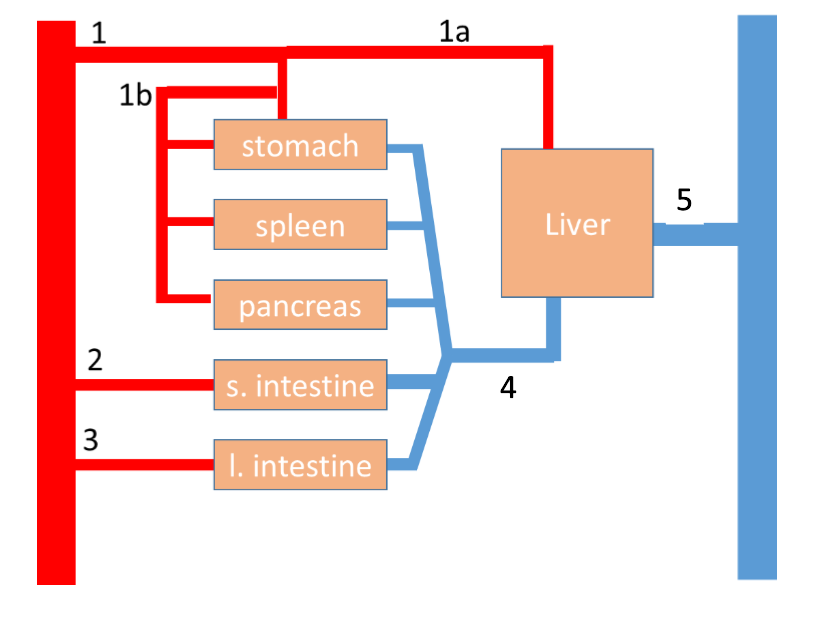
3
caudal mesenteric artery
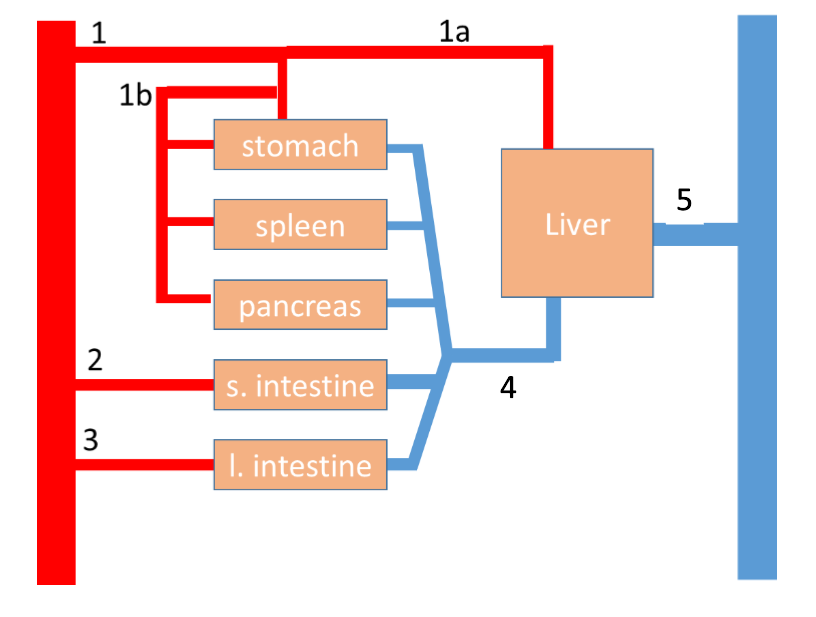
4
hepatic portal vein
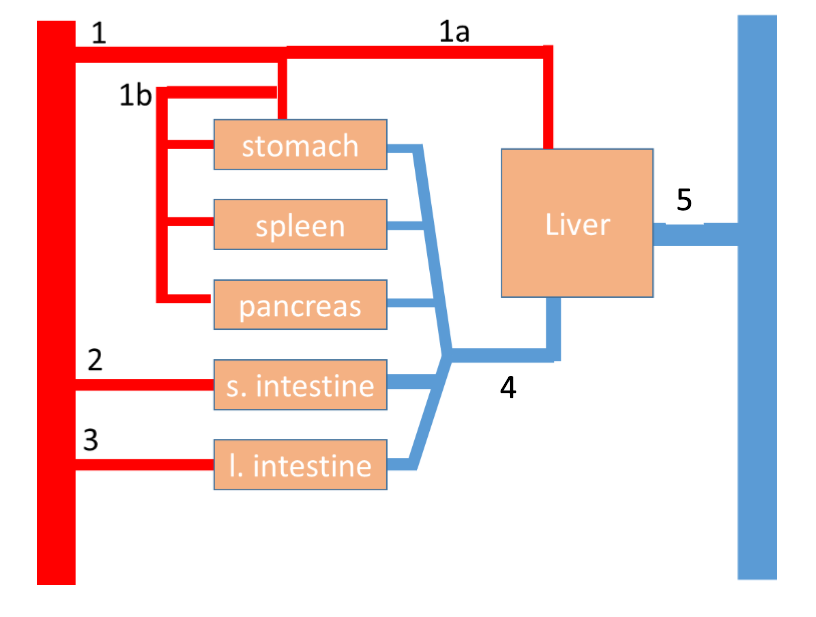
5
hepatic vein
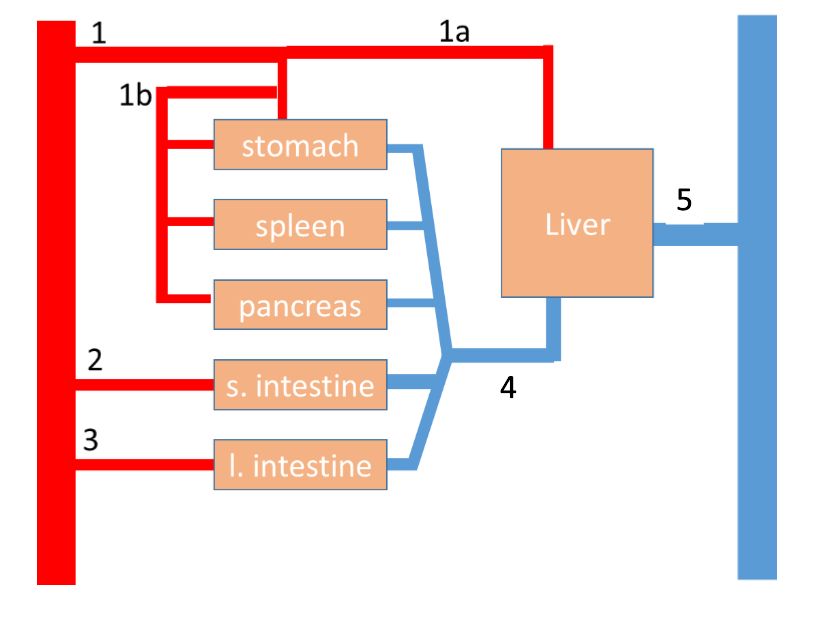
1a
hepatic artery
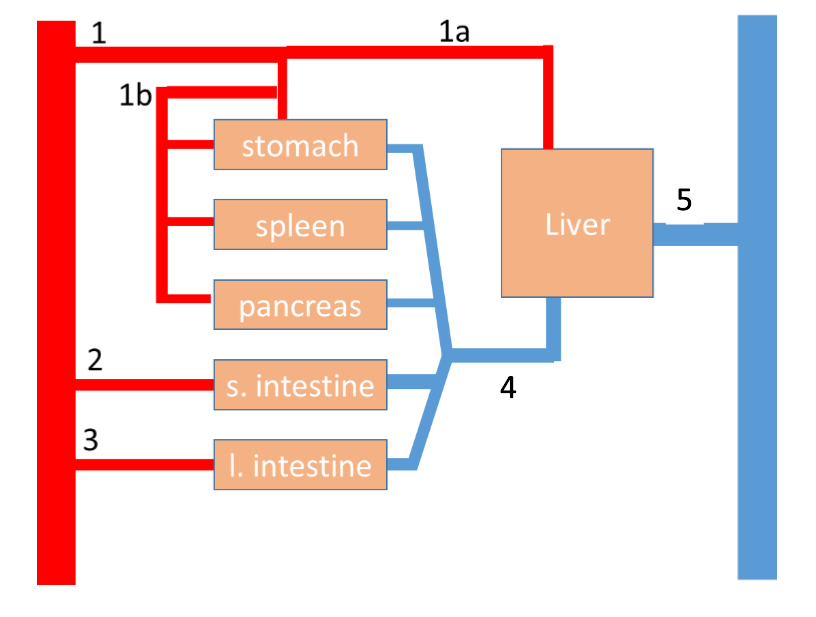
1b
splenic artery
What 3 things is the function of the GI tract coordinated by?
nervous systems
paracrine substances
hormones
What are the 3 nervous systems that the function of the GI tract is coordinated by?
central, autonomic and enteric
Enteric NS
nervous tissue within wall of gut
What are the 2 types of reflexes involved in the nervous control of the GI tract?
long and short
Where do paracrine substances act?
locally
Where do hormones act?
secreted into blood to act systemically
What type of control/nervous system is involved with long reflexes?
CNS
What nervous system controls are involved with short reflexes?
enteric
What kind of tissue is involved in the motor activity of the GI tract?
contractile tissue (smoot muscle)
What does motility relate to?
function (mixing, propulsion, etc)
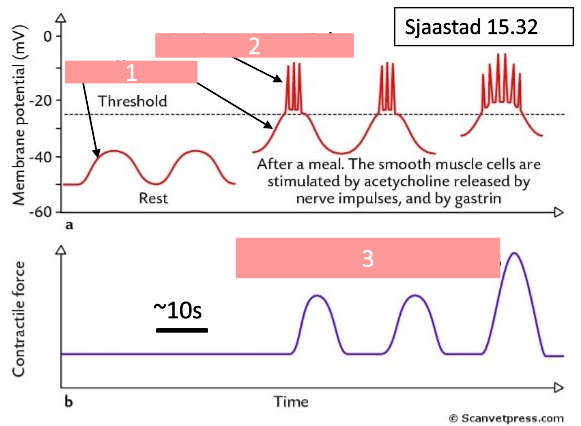
1
oscillations
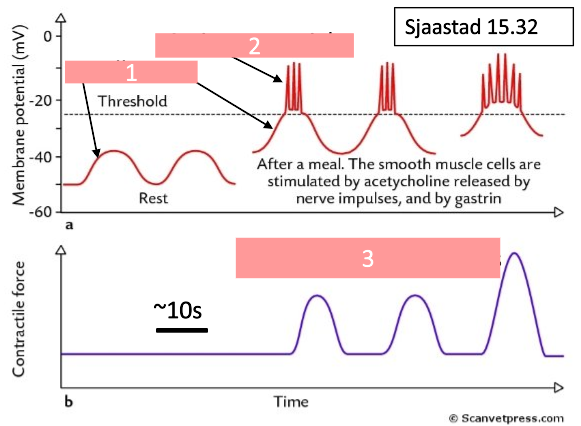
2
action potentials
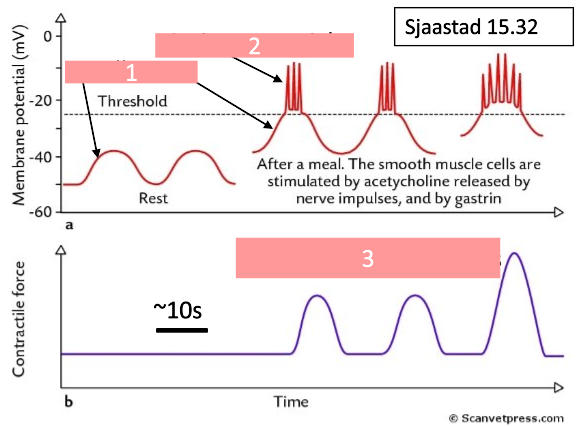
3
slow wave contractions
When do slow waves not reach the threshold?
if fasted
When are slow waves activated/stimulated?
after a meal
What happens after a meal that causes smooth muscle to be stimulated?
acetylcholine is released by nerve impulses, and gastrin release
What is motility regulated and coordinated by?
enteric NS, hormones, ANS
What waves are involved in stomach motility?
slow waves
What are the features of motility in the small intestine?
segmentation (minute rhythm) and peristalsis
In the stomach, how many small waves are there per minute?
2/4
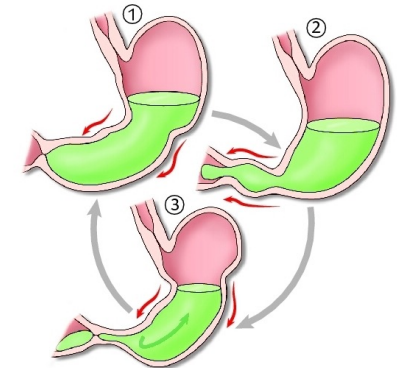
What are the 3 main steps in stomach motility?
propagate from fundus to plyorus
breaks up food
moves material to duodenum
What factors stimulate the stomach emptying?
distension of stomach
peptides in stomach
What does distension of the stomach do that stimulates the stomach emptying?
increase activity of stretch-sensitive sensory cells
increase contraction of smooth muscle cells
emptying increases
What does peptides in the stomach do that stimulates the stomach emptying?
increase gastrin
increase contractions of smooth muscle cells
emptying increases
What factors inhibit the stomach emptying?
high peptide conc
high pressure
high osmolarity
low pH
high fat content
What does high fat content do that inhibits the stomach emptying?
increase release of hormones from duodenal epithelium
What happens due to high peptide conc, high pressure, high osmolarity and low pH that inhibits the stomach emptying?
increase activity of sensory cells in duodenum
(CNS) increase sympathetic activity & decrease parasympathetic activity of nerve fibres to stomach
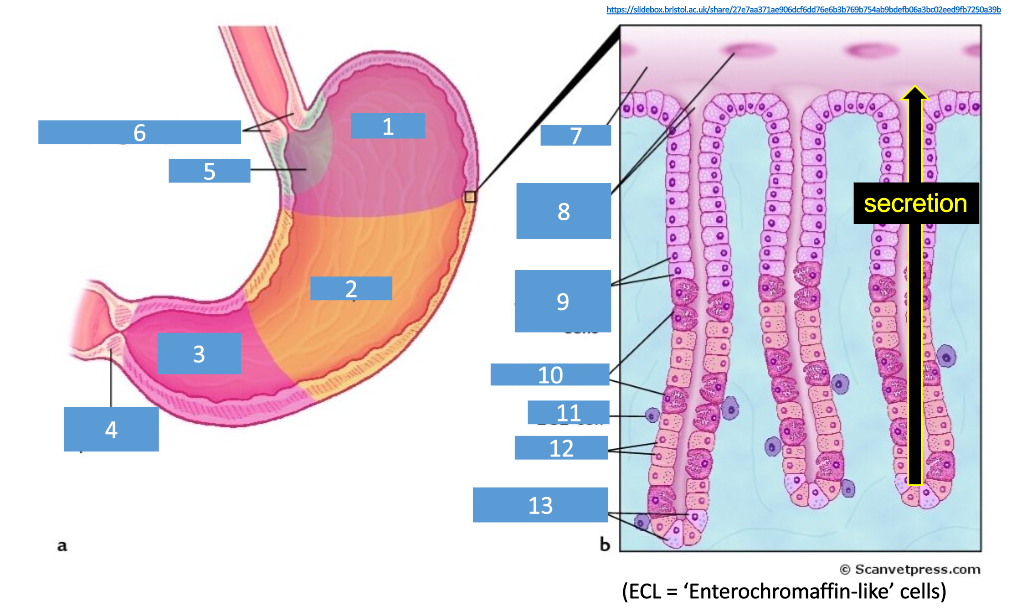
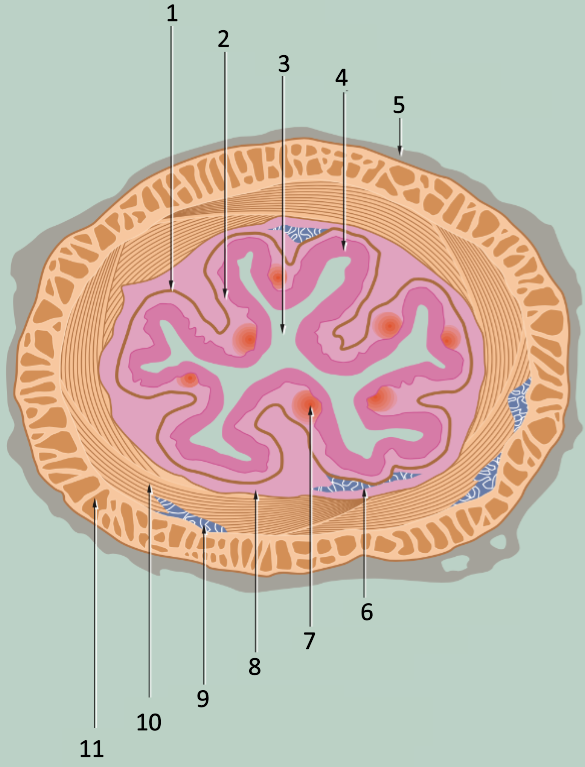
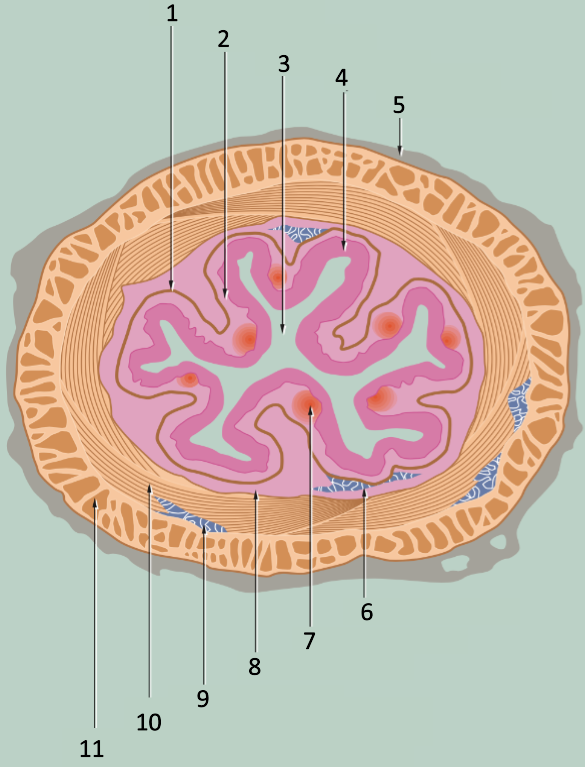
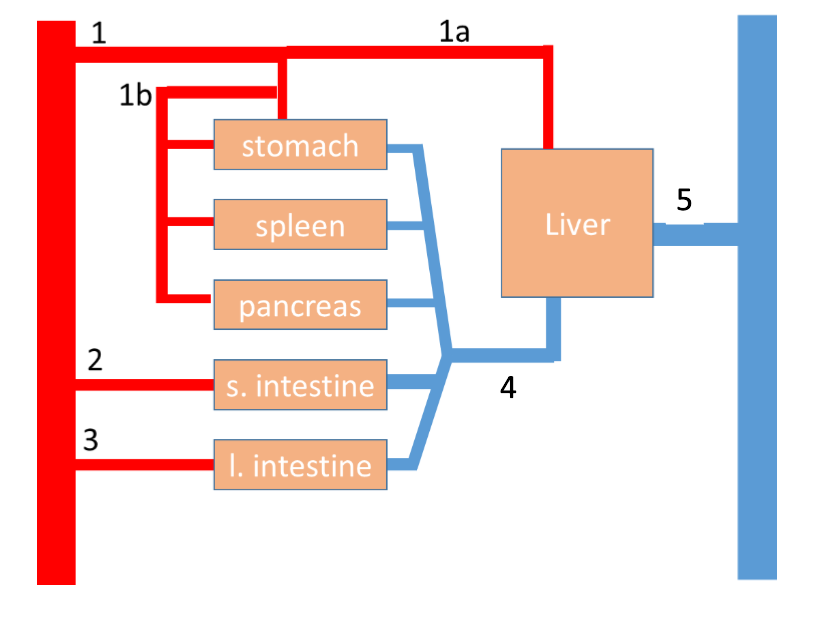
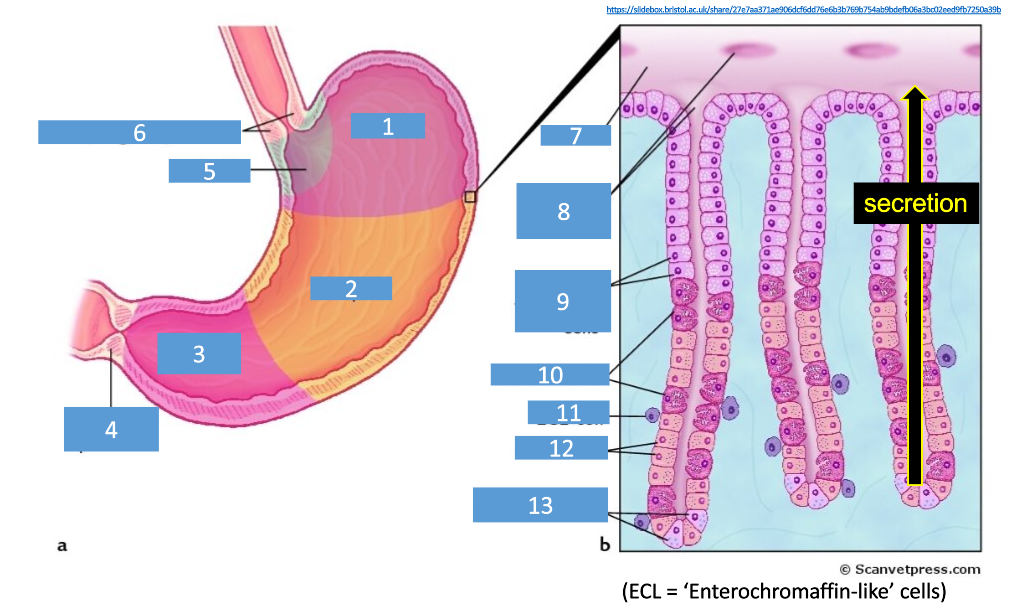
1
fundus
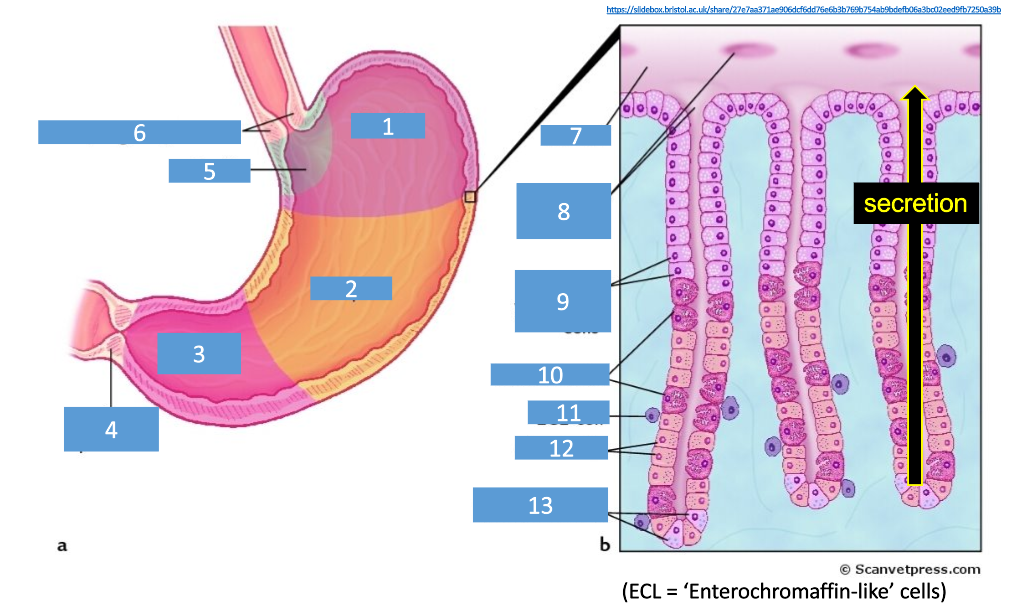
2
corpus
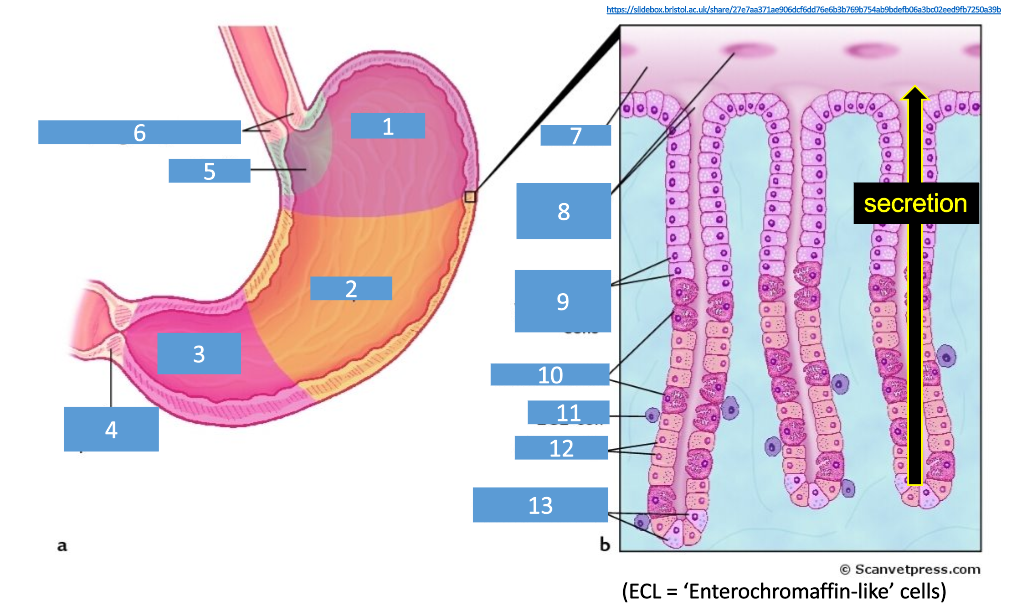
3
pylorus/antrum
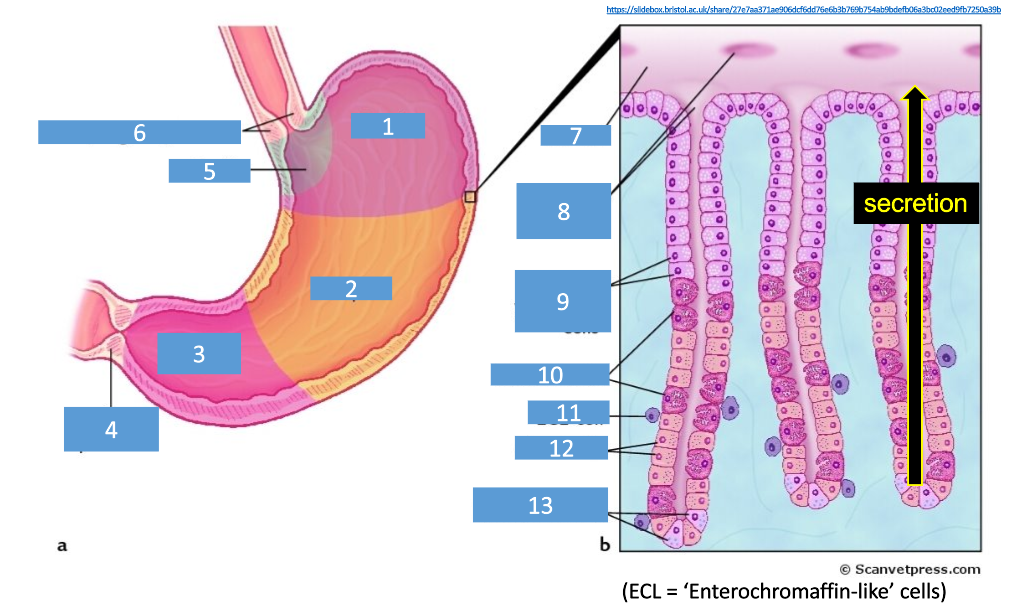
4
pyloric sphincter
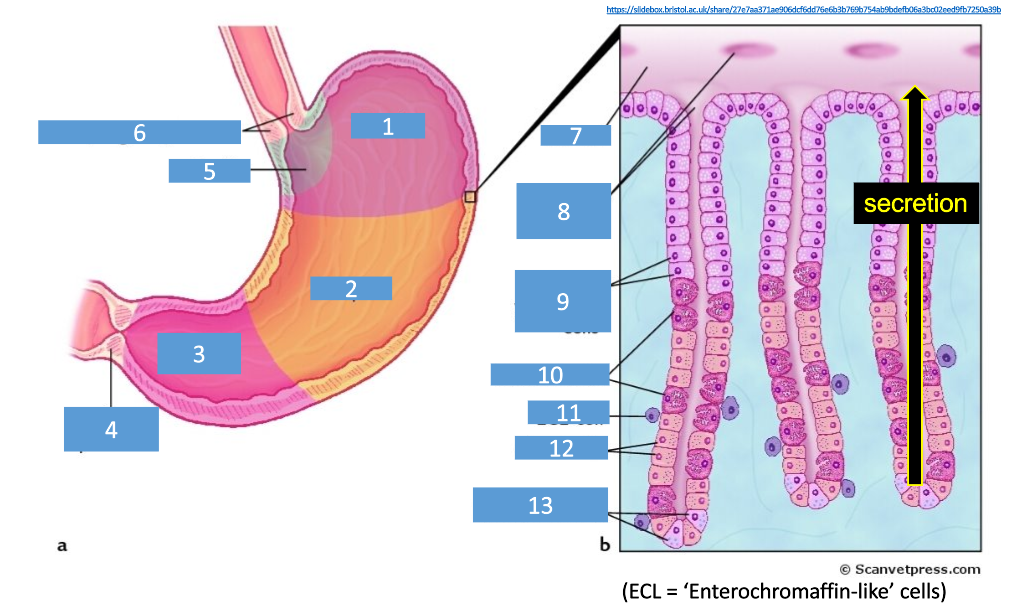
5
cardia
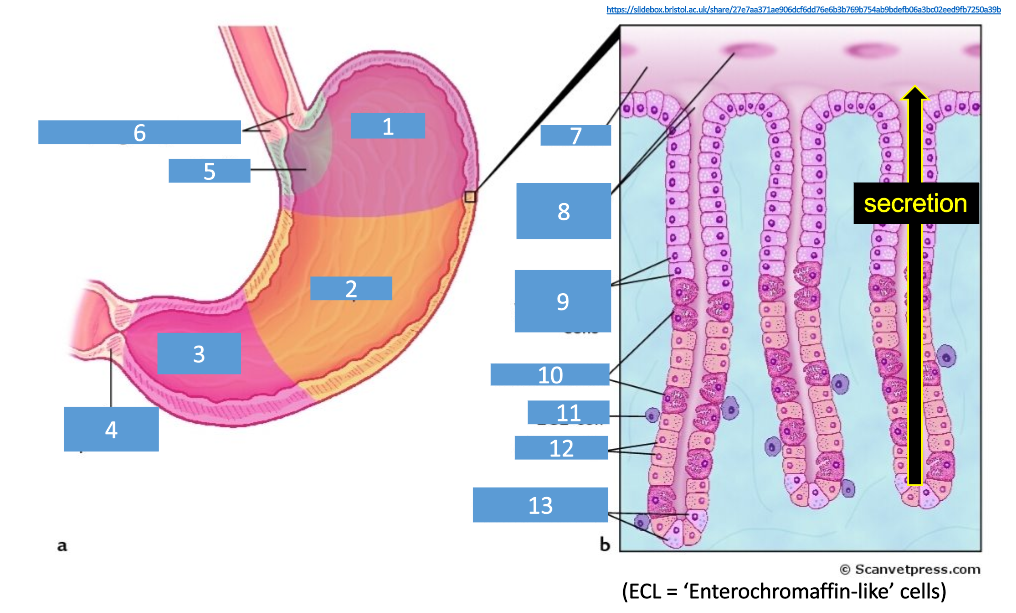
6
esophageal sphincter
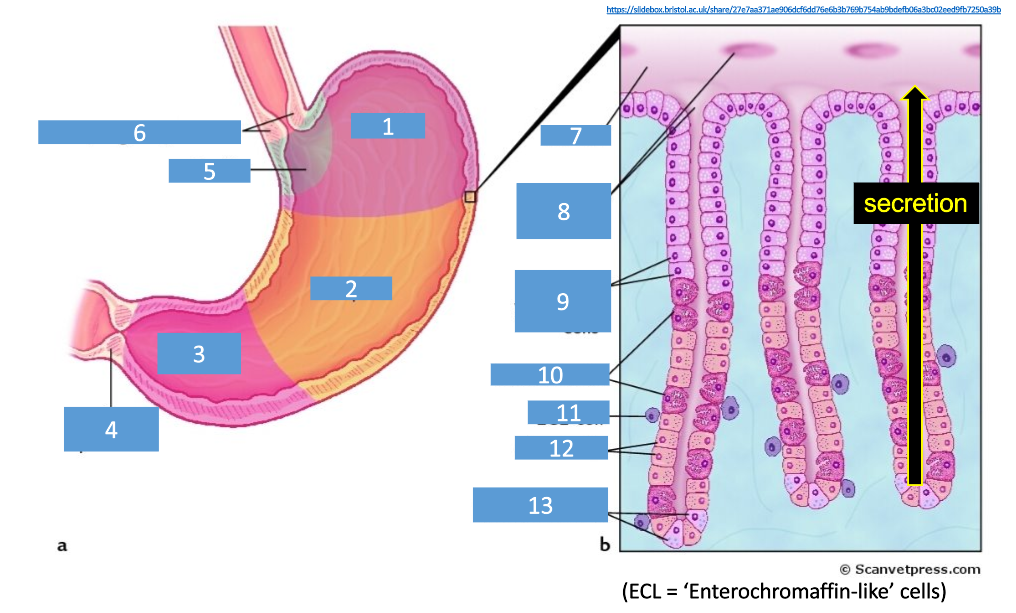
7
lumen
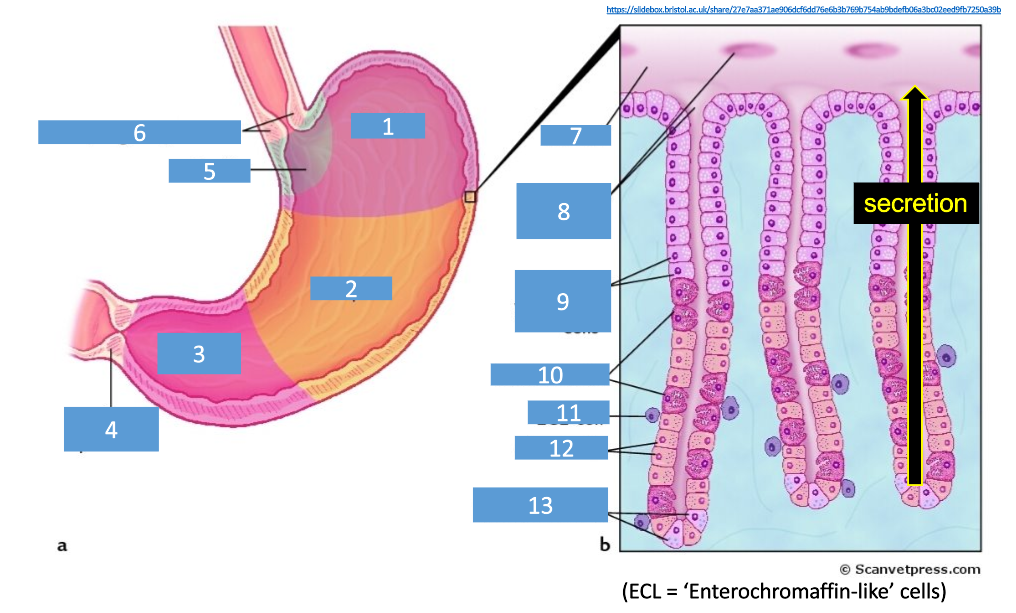
8
gland entrances
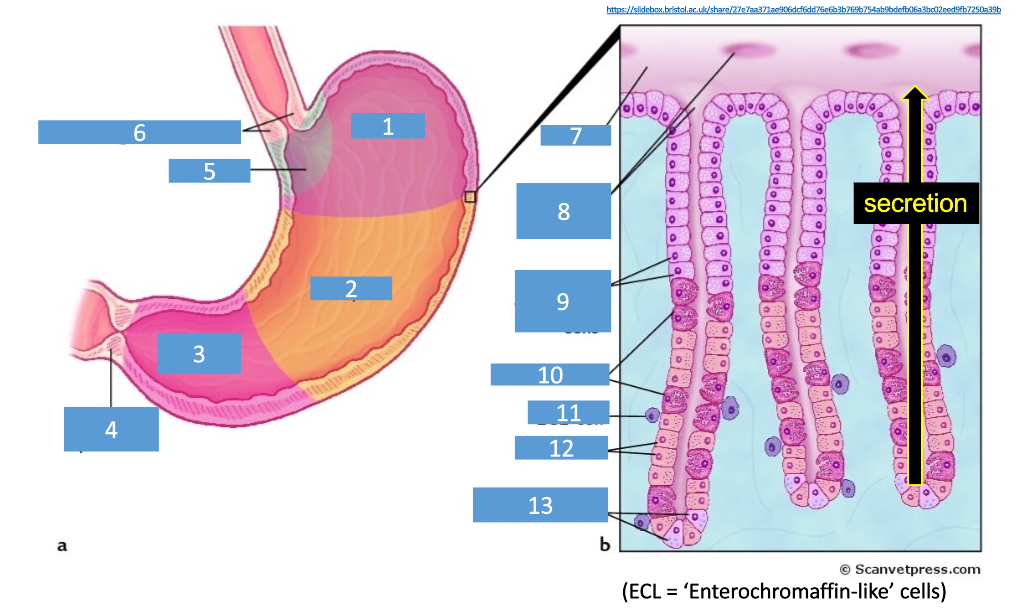
9
mucin-producing cells
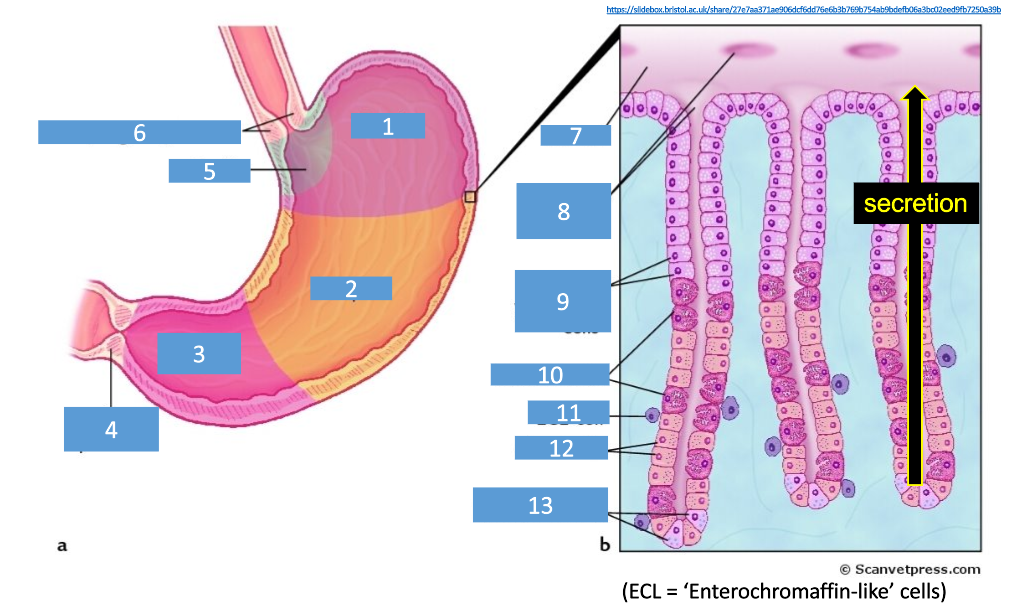
10
parietal cells
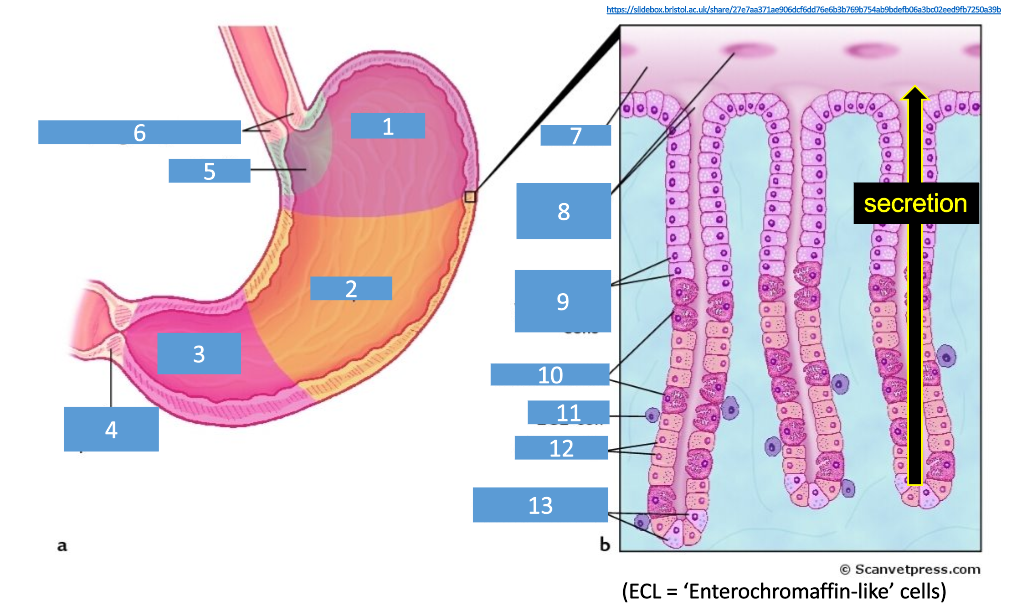
11
ECL cell (enterochromaffin-like cells)
12
chief cells
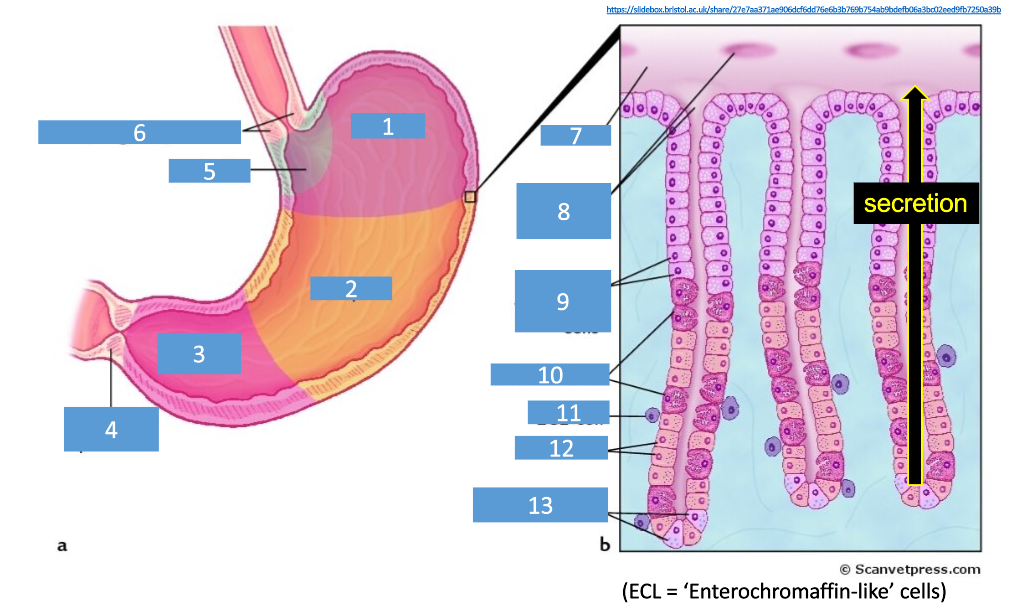
13
endocrine cells