HTHSCI 2HH3 - Microbiology of Pathogenic Factors
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
54 Terms
normal flora
do not produce disease under normal conditions as long as it stays where it belongs, resident microbiota permanently colonize host, transient microbiota temporarily colonize the host
factors that determine distribution and compositions
nutrients, physical and chemical factors, mechanical factors, other “host” factors
nutrients
Secretory and excretory products of cells, bodily fluids, food in GI tract
physical and chemical factors
Temperature, pH, O2, CO2, salt, sunlight
mechanical factors
chewing, flow of saliva and peristalis of GI tract, mucous and ciliary action of respiratory system
other “host” factors
age, nutritional status, disability, stress, hygiene, lifestyle, geography, occupation
where are microbiota located?
upper respiratory tract, upper digestive tract, lower digestive tract, male and female urinary and reproductive systems, eyes and skin
microbial antagonism
normal flora benefits the host by preventing growth of pathogenic microbes as it competes with the pathogen for nutrients, produces substances harmful to the pathogen, and manipulates the host environment (increase or decrease pH and O2 levels)
microbial antagonism - E. coli in the gut
E. coli produces bacteriocins which are proteins that inhibit the growth of closely related species of bacteria like salmonella and shigella
How can infection/disease result?
when the balance between normal flora and a pathogenic microbe is altered (microbial antagonism fails). For example, large exposure to a pathogen
Factors that disrupt microbial balance
age, antibiotic use, changes in hygiene, nutritional status
microbial antagonism - C. diff
C. diff causes a range of GI symptoms from mild diarrhea to severe, or even fatal colitis, presence of normal flora in the large intestine inhibits the growth of C. diff (remains in endospore form). Antibiotic-mediated destruction of the GI normal flora creates an environment conducive to C. diff growth, resulting in disease
When do opportunistic infections occur
Microbes from the host normal flora move from their normal habitat, causing
disease
Escherichia coli gains access to other body sites such as the urinary tract causing urinary tract infections
The host’s immune system is weakened/compromised - Pneumocystis jirovecii causes pneumonia in the immunocompromised patient, but has no effect on healthy individuals
Changes occur in the composition of the host normal flora
Shift in the relative abundance of microbes (due to antibiotic therapy) creates opportunity for one species to thrive and cause disease
microbial mechanisms of pathogenesis (how pathogenic microorganisms cause disease)
contact/exposure, adherence, evasion of host defenses and penetration, damage of host cells, transmission
portals of entry
Mucous membranes
Conjunctiva
Upper respiratory (nose and mouth), gastrointestinal, and genitourinary tracts (placenta)
Skin
When unbroken, the skin serves as an almost impenetrable barrier, however some bacteria can gain access to the body via natural openings in the skin (e.g., follicles, sweat gland ducts)
3. Direct deposition beneath mucous membranes or skin
Trauma (punctures, wounds, cuts), surgery, invasive procedures, IV lines, broken skin, insect bites
what is the most common portal of entry?
upper respiratory tract from touching face and nose
adherence
Means by which a pathogen attaches itself to host tissues at portal of entry
Accomplished by cell surface molecules located on the pathogen called “adhesins” binding specifically to surface “receptors” located on the cells of host tissues
Adhesins are host specific and tissue specific - there must be adhesin, Rc match
Mechanisms of adhesion also contribute to the evasion of host defenses
Use bacterial structures, adherence proteins, and glycocalyx
bacterial structures
Adhesins are present on the fimbriae and flagella of many pathogenic bacteria
P-fimbriae on pyelonephritogenic E. coli (kidney infection) adhere to a specific galactose dissaccharide found on the surface of uroepithelial cells, responsible for 90% of all urinary tract infections (UTIs)
adherence proteins
M proteins produced by Streptococcus pyogenes (GAS); appear as hair-like projections from the cell surface - mediates attachment of bacteria to epithelial cells of the host - many subtypes, some more strongly associated with specific diseases than others
glycocalyx
If well organized and firmly attached to cell wall, referred to as a “capsule”
K1 capsule associated with strains of Neisseria meningitidis type B (most common circulating strain as vaccine is not widely administered and not covered under OHIP)
Binds to epithelial cells of the ventricles and vascular endothelium of the brain, causing meningitis
If unorganized and only loosely attached to the cell wall, referred to as a “slime layer”
Facilitates the formation of biofilms
biofilms
Colony of bacteria that adheres to surfaces (living and non-living) via a slime layer (glycocalyx)
Teeth, medical catheters, heart valves, hip replacement components, contact lenses, industrial food equipment, etc.
May involve multiple bacterial species and consist of many layers antibiotics
Contribute to chronic infections
Shelters microorganisms from host defences; highly resistant to disinfectants and antibiotics - antibiotics can only kill most superficial layer therefore bacteria can continue causing infection
Few treatments available, surgical intervention often required
If a pathogenic bacteria loses their ability to make adhesins they become …
avirulent
capsule
impairs phagocytosis, preventing phagocytic cell from adhering to the microbe, thereby increasing the virulence of the pathogen. With time, the host will produce antibodies against the capsule
bacterial species that possess a capsule are … virulent than those without
more; bacteria without a capsule can be easily dealt with most of the time
cell wall
M proteins increase virulence by helping bacteria resist phagocytosis by WBC e.g., Streptococcus pyogenes
Mycolic acid present in the cell wall of Mycobacterium tuberculosis increases virulence by helping the microbe resist digestion by phagocytes
Streptococcus pneumoniae avoid destruction by host immune system by producing a capsule, which makes undetectable by the host immune system
coagulase
Coagulate fibrinogen in the blood to form fibrin
Fibrin clot protects the bacteria from phagocytosis, and isolates the microbe from other defenses of the host - clot made of own host material making it undetectable
Produced by some Staphylococci spp. (coagulase + or - staph)
kinase
Degrades fibrin, and thus digest clots formed by the body to isolate the wound and clots created by the bacteria as protection from phagocytosis (to get deeper into host tissues and wound)
Streptokinase produced by Streptococcus pyogenes
Staphylokinase produced by Staphylococcus aureus
How do coagulase and kinase faciliate a microbes’s ability to evade host defenses?
bacteria produce coagulase
clot forms protecting bacteria
bacteria later produce kinase, dissolving clot and releasing bacteria as well as facilitating microbe entry into host tissues
How are facultative intracellular bacteria able to survive in immune cells?
Escaping phagosomes before fusing with host cell lysosomes
Preventing phagosomes-lysosome fusion
Reducing effectiveness of toxic
compounds within lysosome
4. Producing cell walls resistant to lysosomal proteases
disseminated infection
bacteria is able to leave portal of entry and travel elsewhere in the body
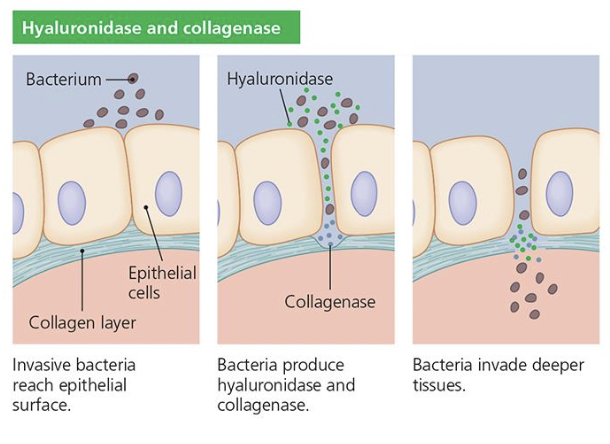
hyaluronidase
Degrades hyaluronic acid, a polysaccharide that holds host cells together, allows bacteria to penetrate deeper into host tissues
collagenase
Degrades collagen fibers at the base of superficial tissues and allows bacteria to move deeper into the host
How do hyaluronidase and collagenase help with penetration of host tissues?
invasive bacteria reach epithelial surface
bacteria produce hyaluronidase and collagenase
bacteria invade deeper tissues