5. Skeletal System
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
5 functions of skeletal system
1. Support
2. Protection
3. Movement
4. Mineral storage: Calcium and phosphorous
5. Hematopoiesis (Blood cell formation)
Protection (skeletal system function)
Bones Protect the brain
The cranium completely surrounds and protects the brain from injury.
What does hematopoiesis mean?
blood cell formation
hematopoiesis (skeletal system function)
blood cell formation
Red marrow is responsible for hematopoiesis.
Yellow marrow stores fat
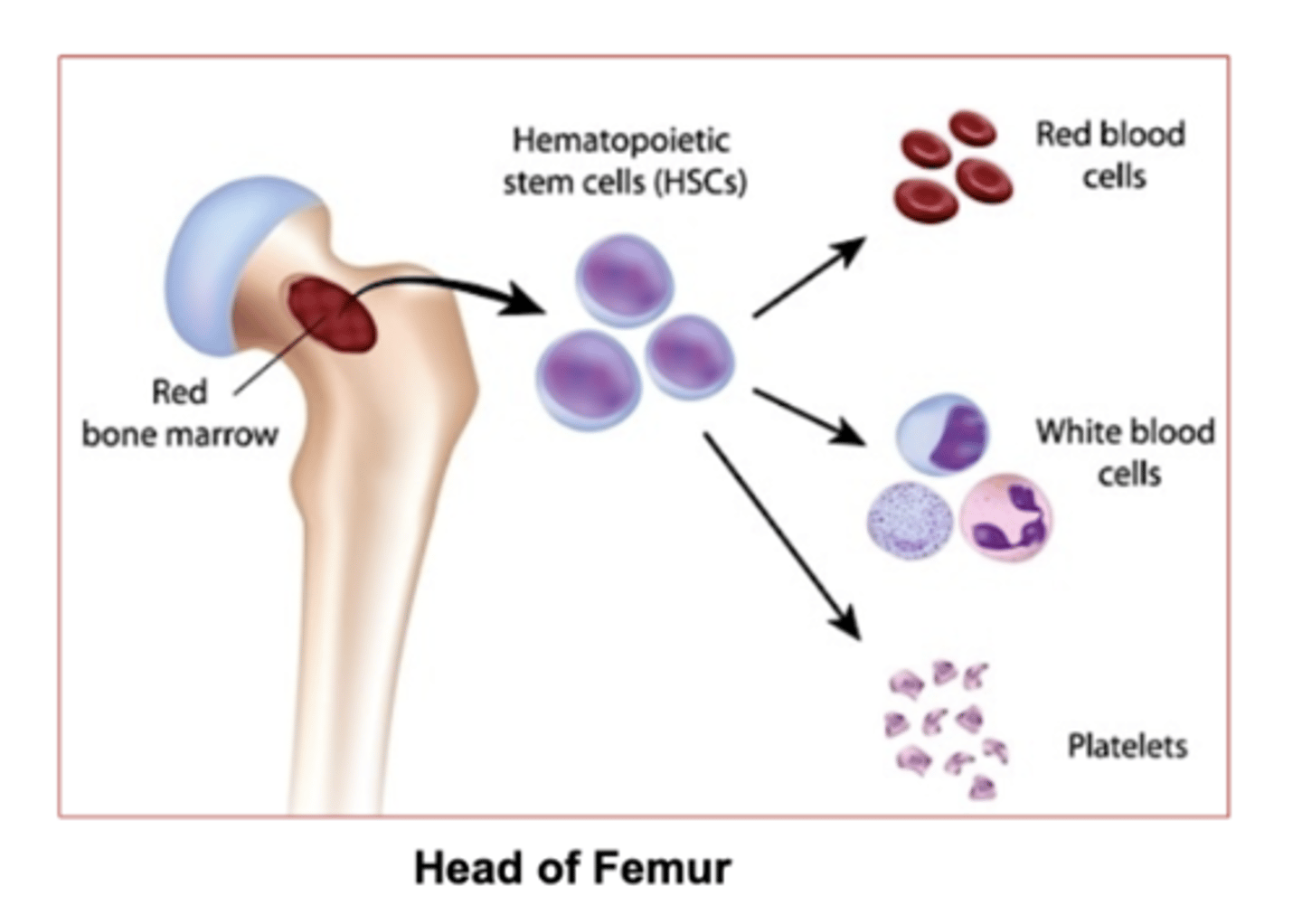
Which marrow is responsible for hematopoiesis (red blood cell formation) ?
red bone marrow
which marrow stores fat?
yellow bone marrow
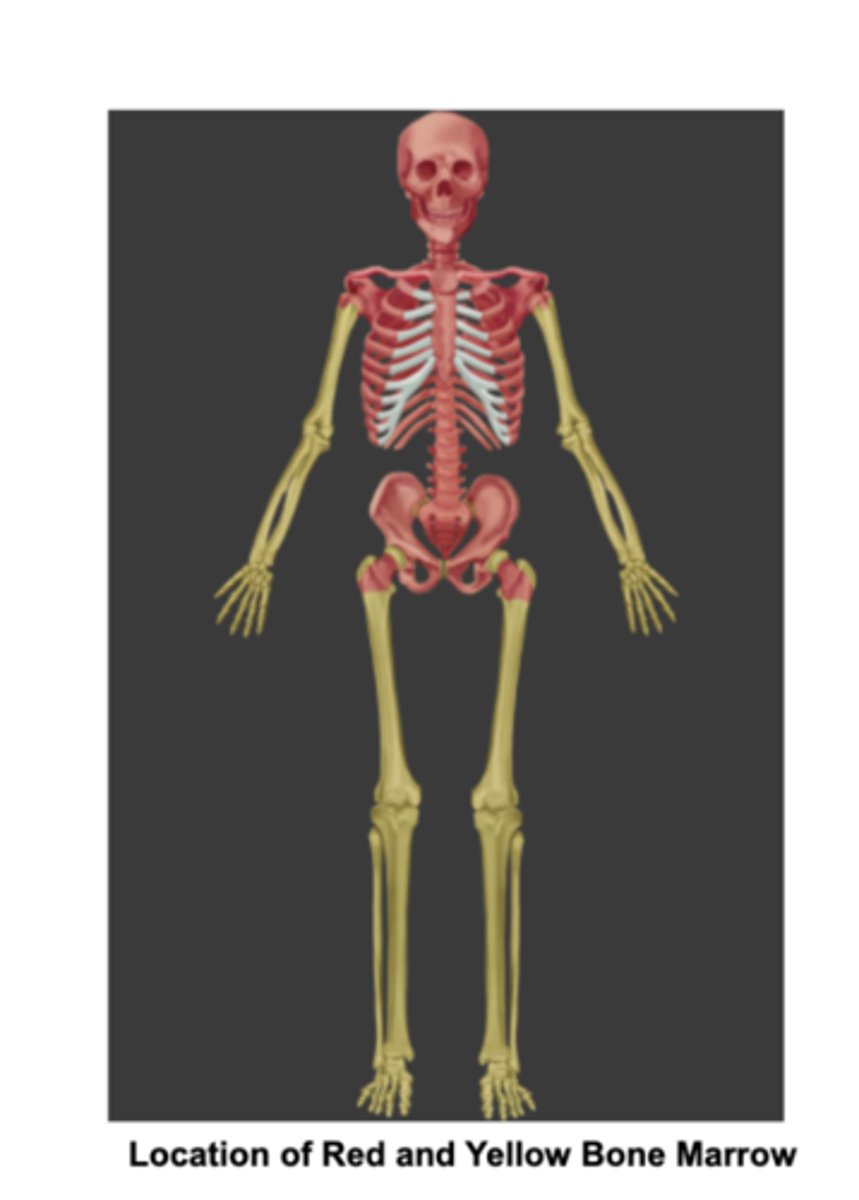
Which bones contain Red bone marrow in adults:
Flat bones and the ends of the femur and humerus.
(epiphyses = the end of long bones)
what does epiphyses mean?
the rounded ends of long bones, also containing the articular cartilage.
Where is yellow bone marrow in adults?
in the medullary cavity of long bones.
the limbs
2 Bone marrows in adults
Red bone marrow- in Flat bones, the ends of the femur and humerus.
yellow bone marrow- found in the medullary cavity of long bones,
what is the medullary cavity?
The inner space of long bones.
Its filled with bone marrow
Whats the medullary cavity filled with?
Bone marrow
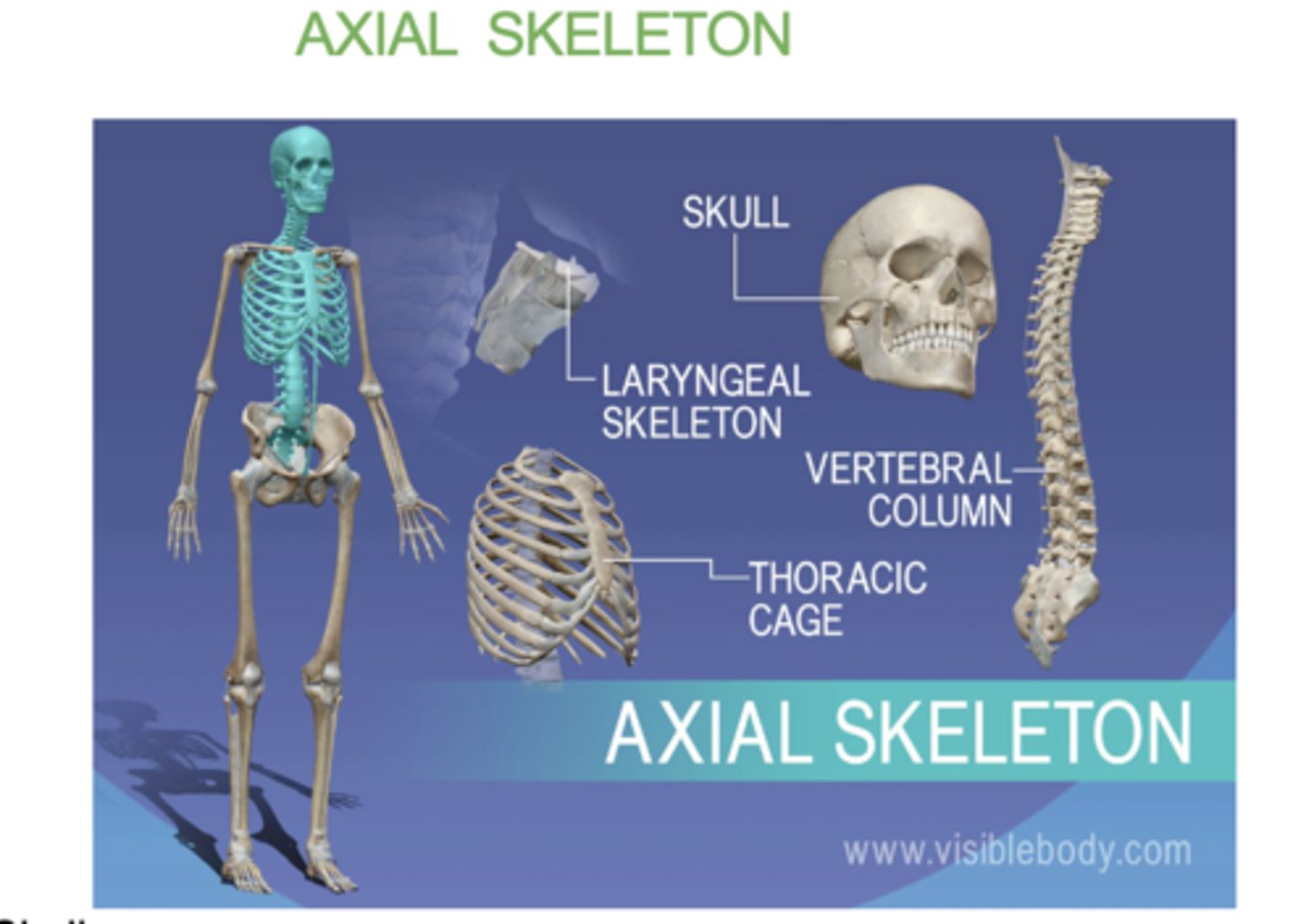
what does the axial skeleton consist of?
-skull
- verterbral column
- sternum
- ribs
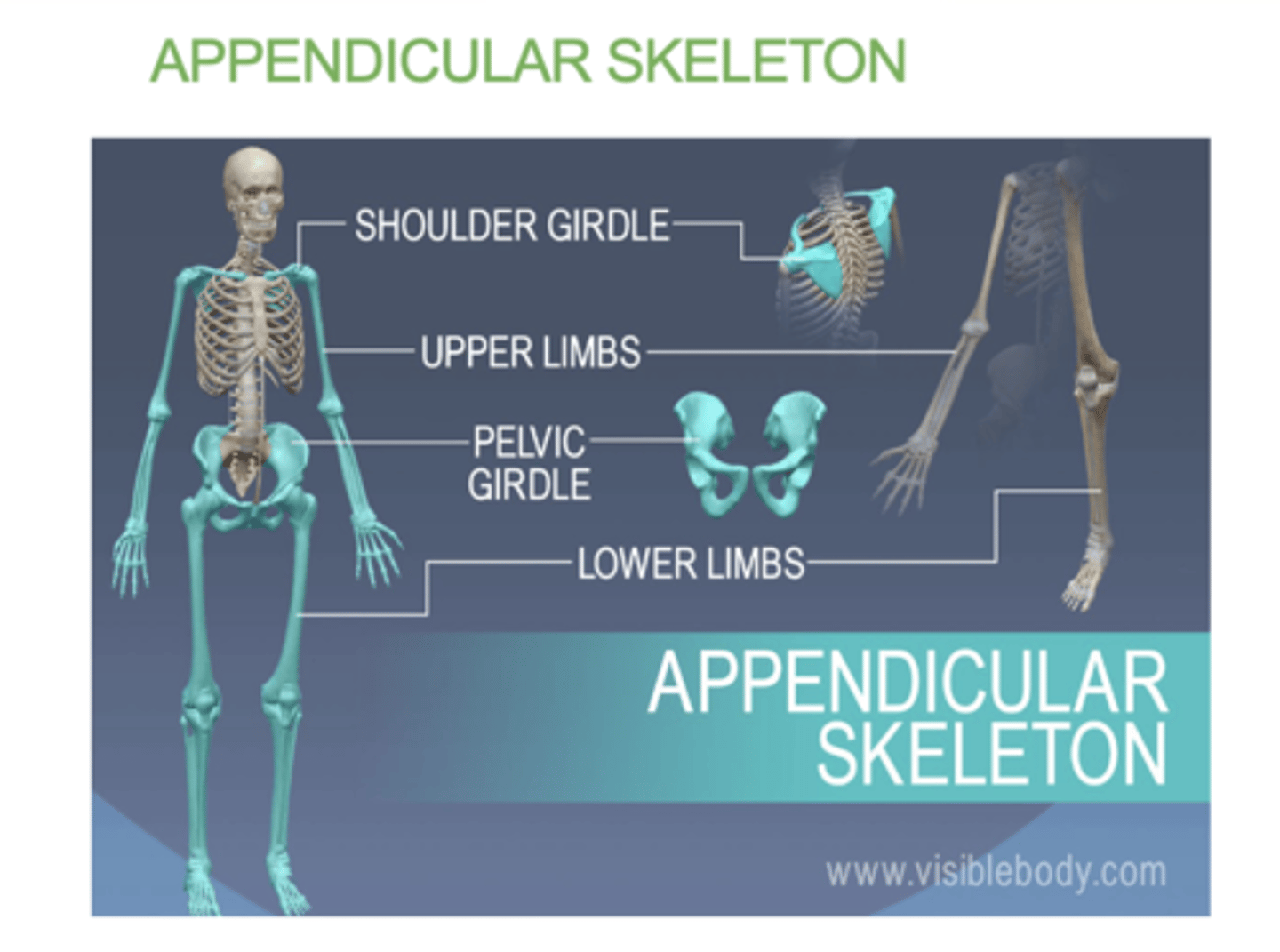
what does the appendicular skeleton consist of?
(Appendicular = Attachments)
• Shoulder girdle
• Upper limbs
• Pelvic girdle
• Lower limbs
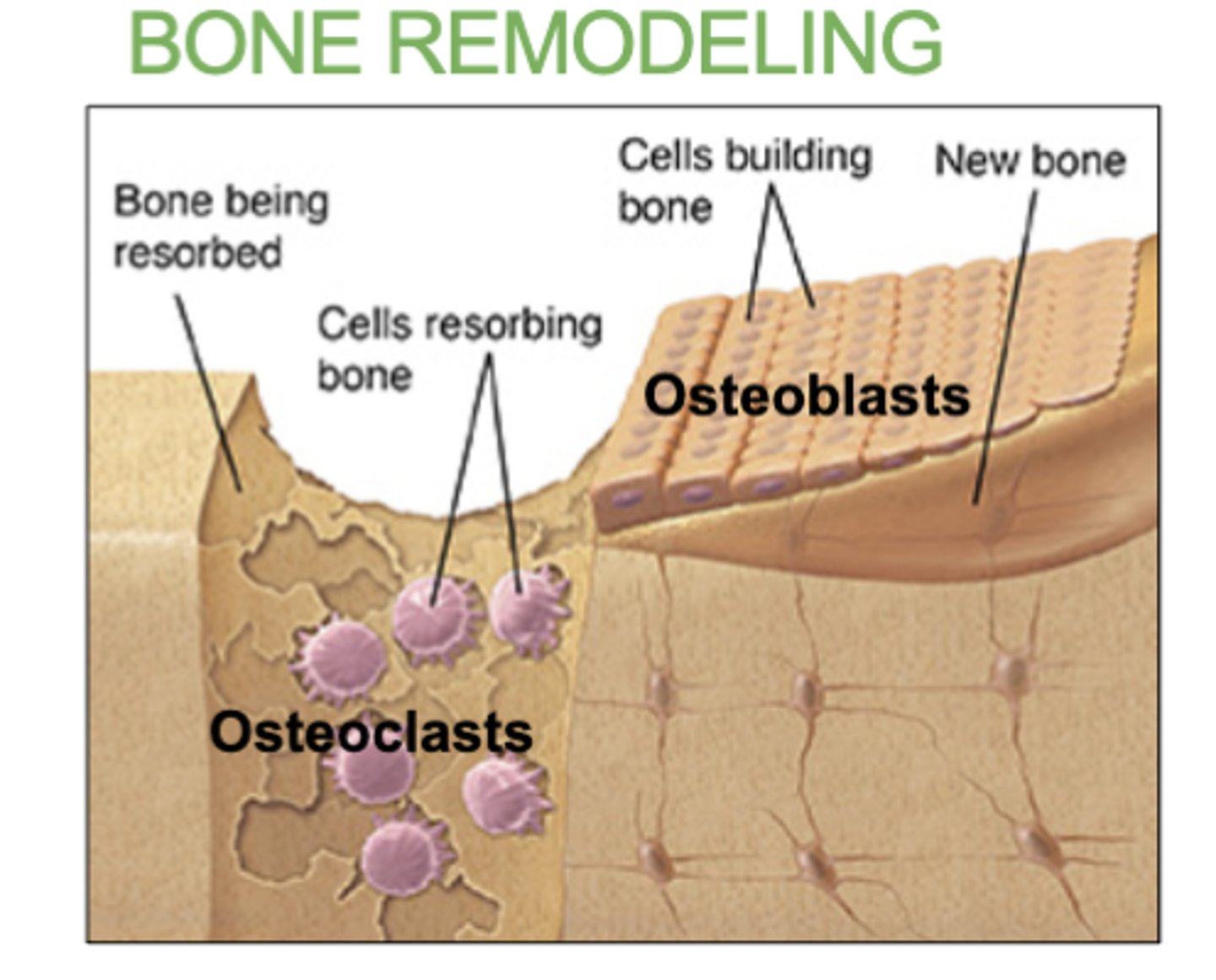
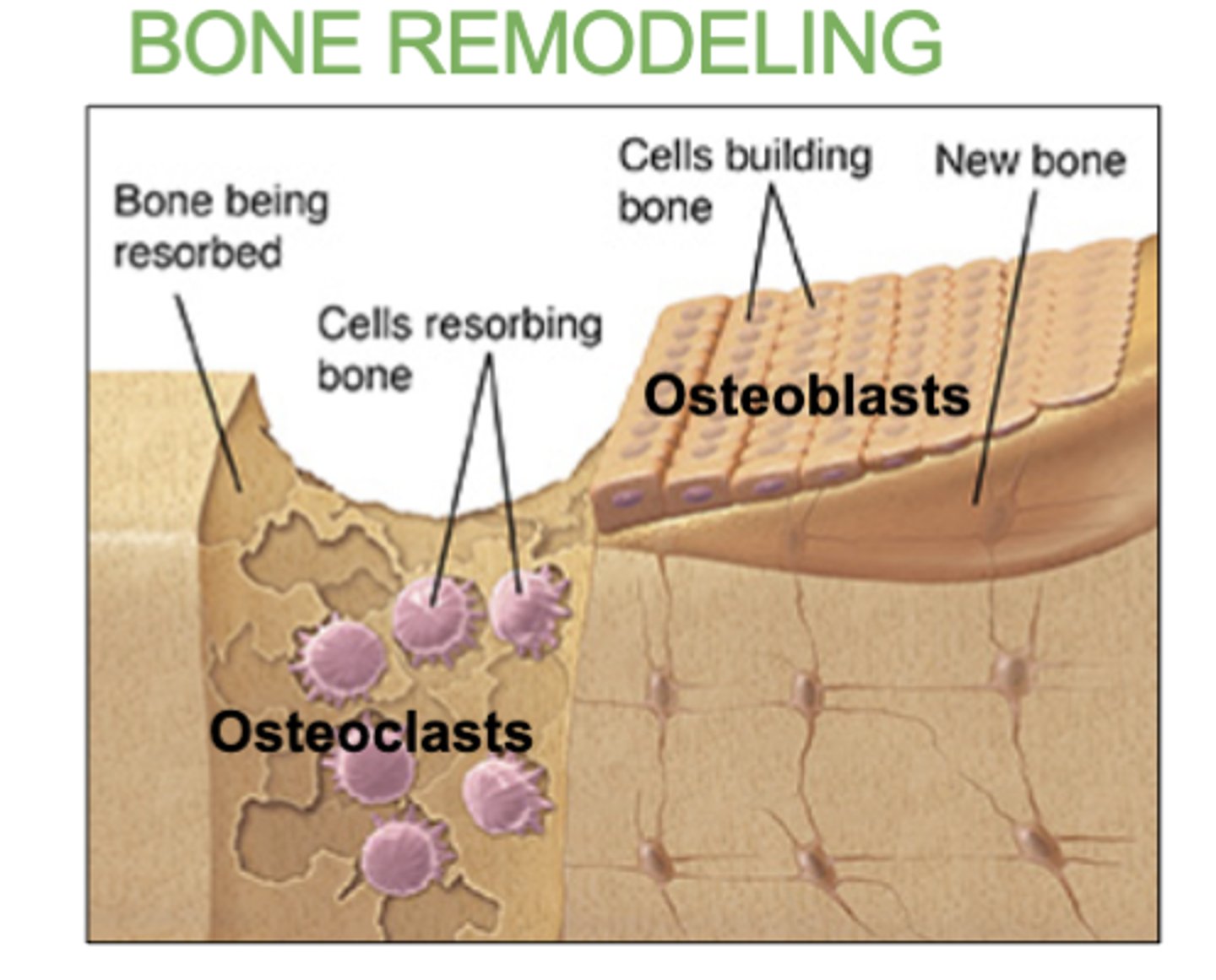
4 bone cells within bones
a) Osteogenic cells: Stem cells that develop into osteoblasts.
b) Osteoblasts: Bone-forming cells. Lay down bone matrix and collagen fibers. They will mature into osteocytes.
c) Osteocytes: Mature bone cells .
d) Osteoclasts: Bone destroying cells. Break down bone for remodeling and release of calcium. Responsible for bone resorption. (completely seperate cell, does not have to do with the other)
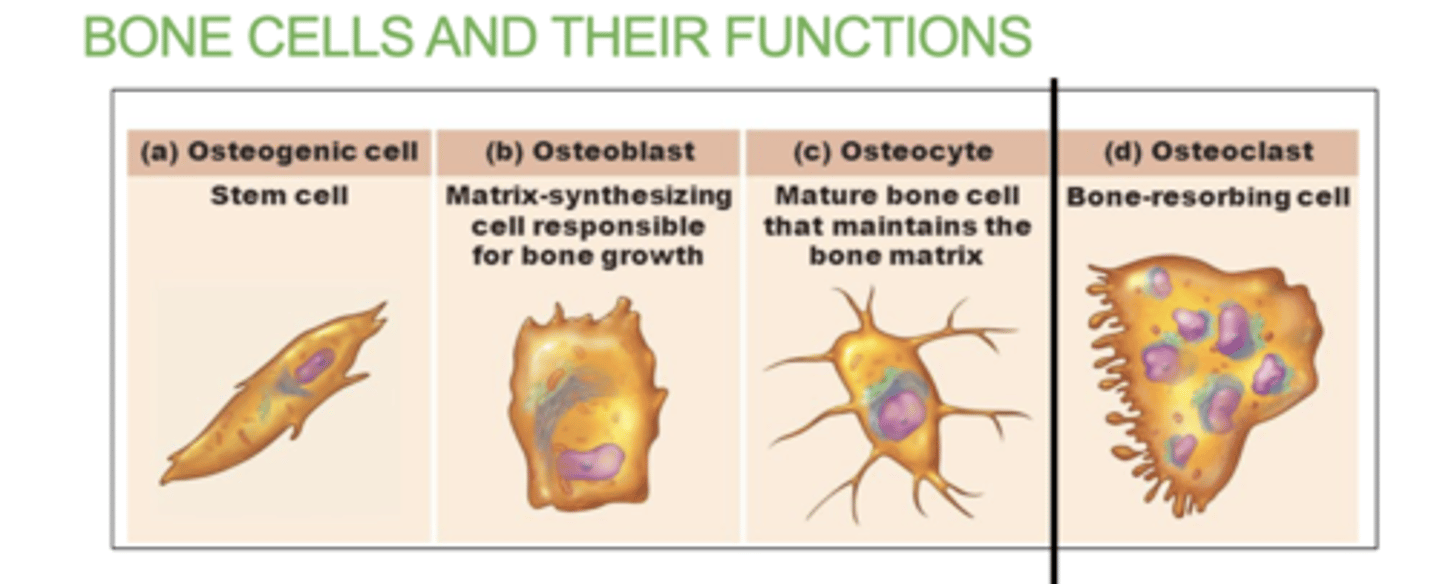
what does the Osteogenic cells do?
They contain stem cells that develop into osteoblasts.
What does the Osteoblasts cells do?
they are responsible for "building bone"
They Lay down bone matrix and collagen fibers. They will mature into osteocytes.
What are Osteocyte cells?
they are mature bone cells.
What do Osteoclast Cells do?
"claws bones"
Break down bone for remodeling and release of calcium.
Osteoclasts in diaphysis will break down bone forming the medullary cavity
Which bone cell will break down bone in the diaphysis and form the medullary cavity?
The Osteoclast cells
5 structures in the anatomy of long bone
- Epiphysis (spongy bone): end of long bone
- Diaphysis (compact bone): middle segment of bone
- Articular cartilage: cartilage that covers both ends of joins ( top and bottom epiphysis)
- Epiphyseal line: the line between epiphysis and diaphysis. An indication that growth in length is complete
-Medullary cavity - space filled with bone marrow
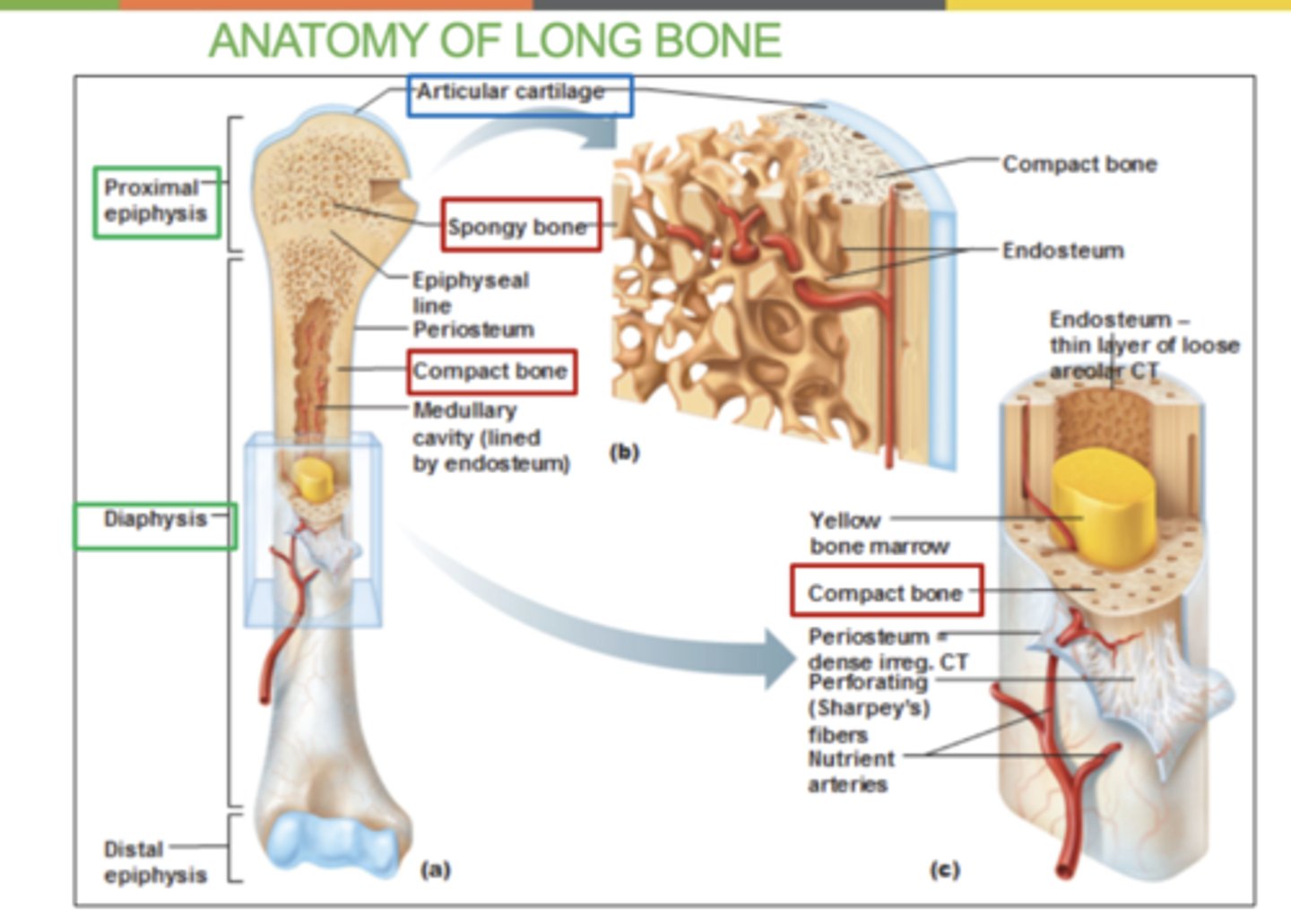
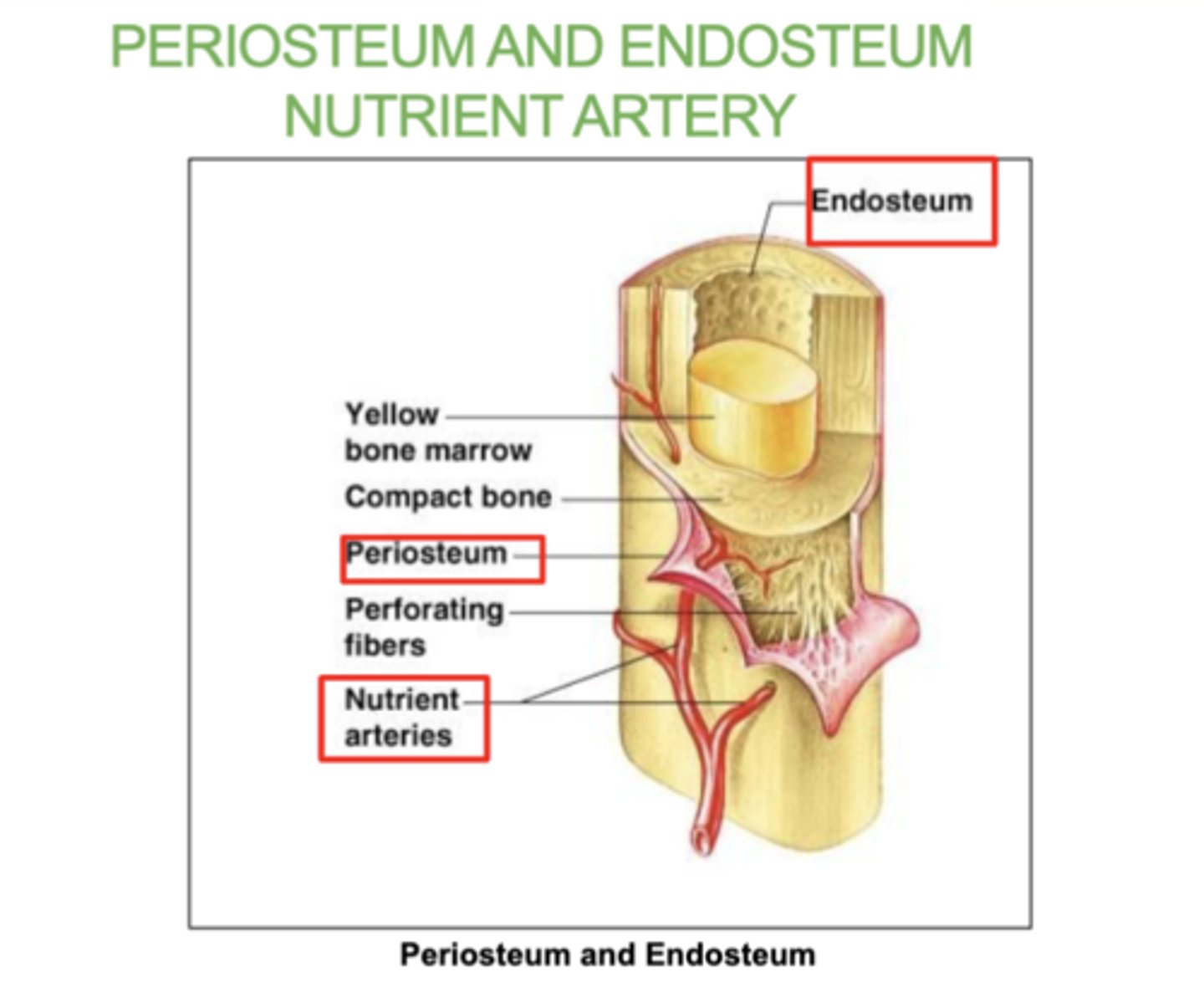
What is the periosteum?
A thin layer of tissue that covers the outside of bones
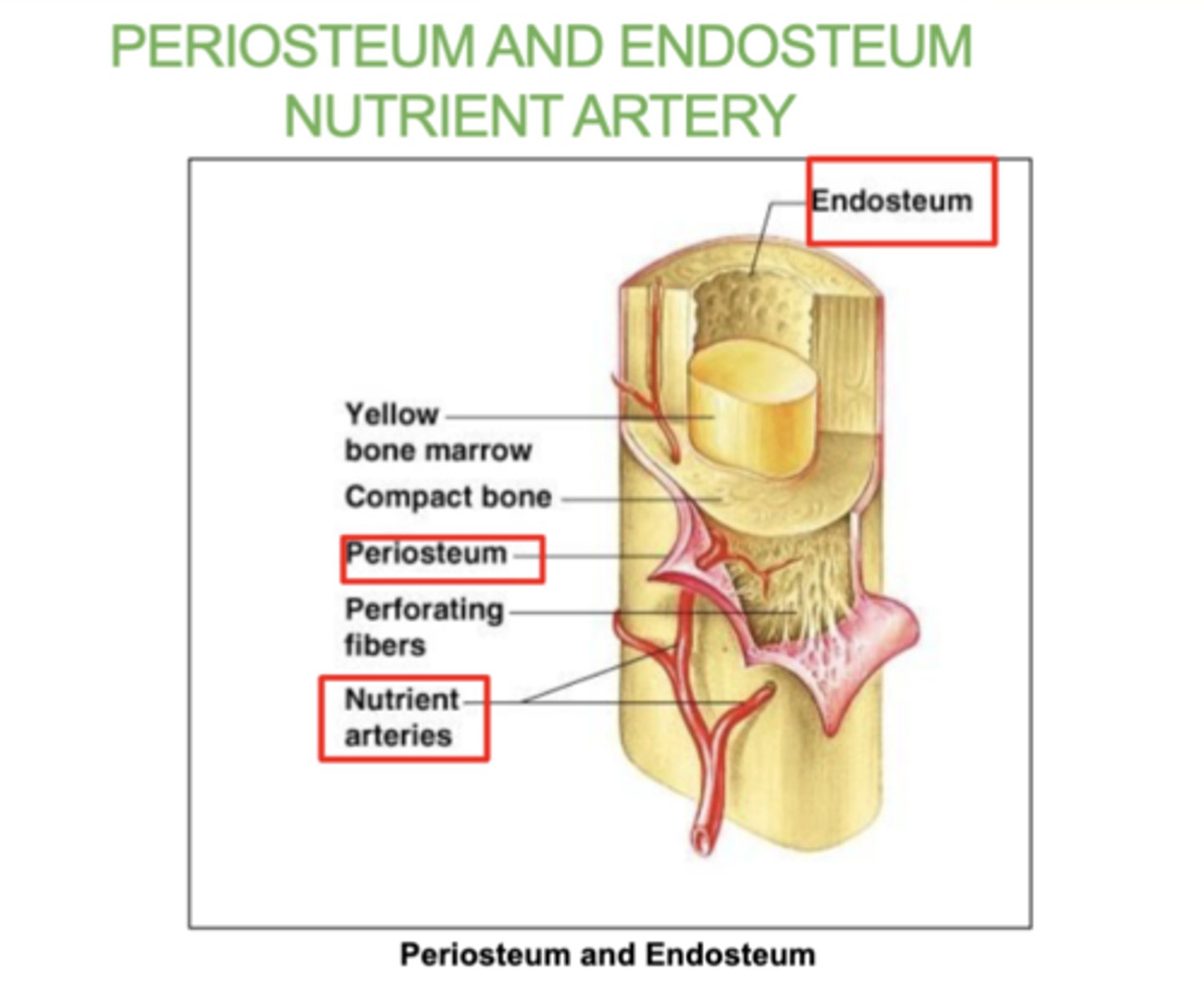
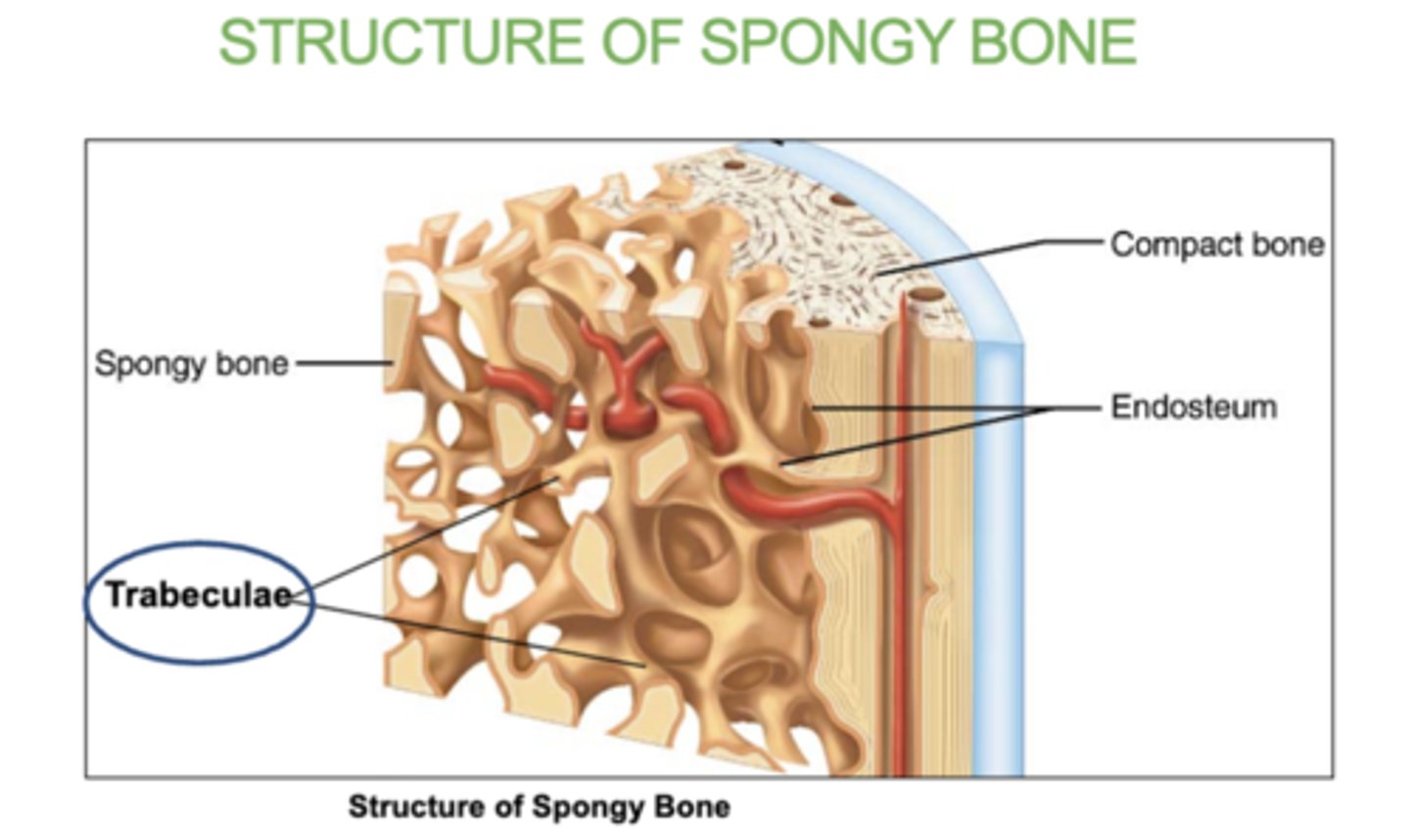
what is the Endosteum?
A thin tissue lining the inside of bones.
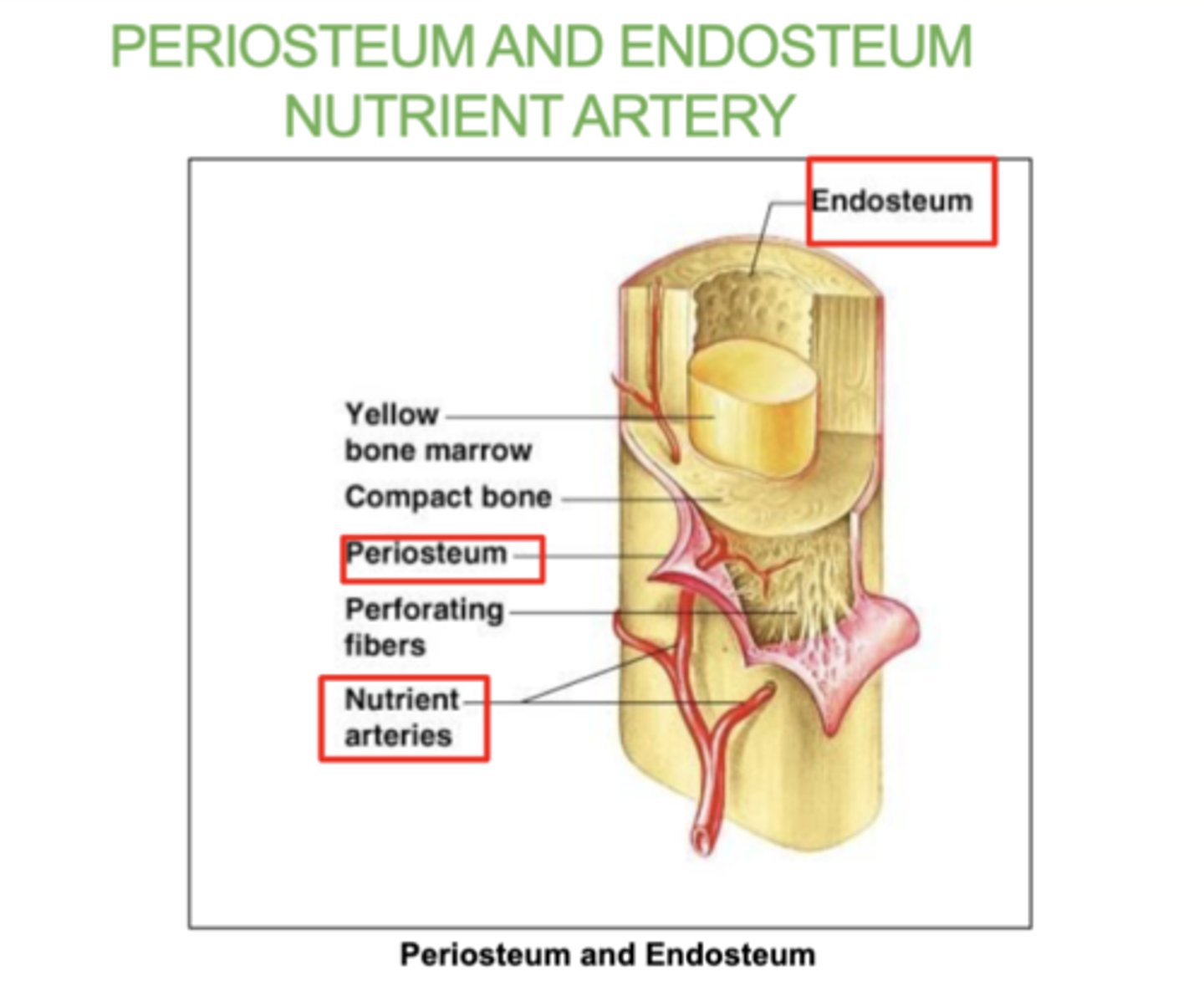
what is the Nutrient artery?
The blood vessel that supplies nutrients to the bone.
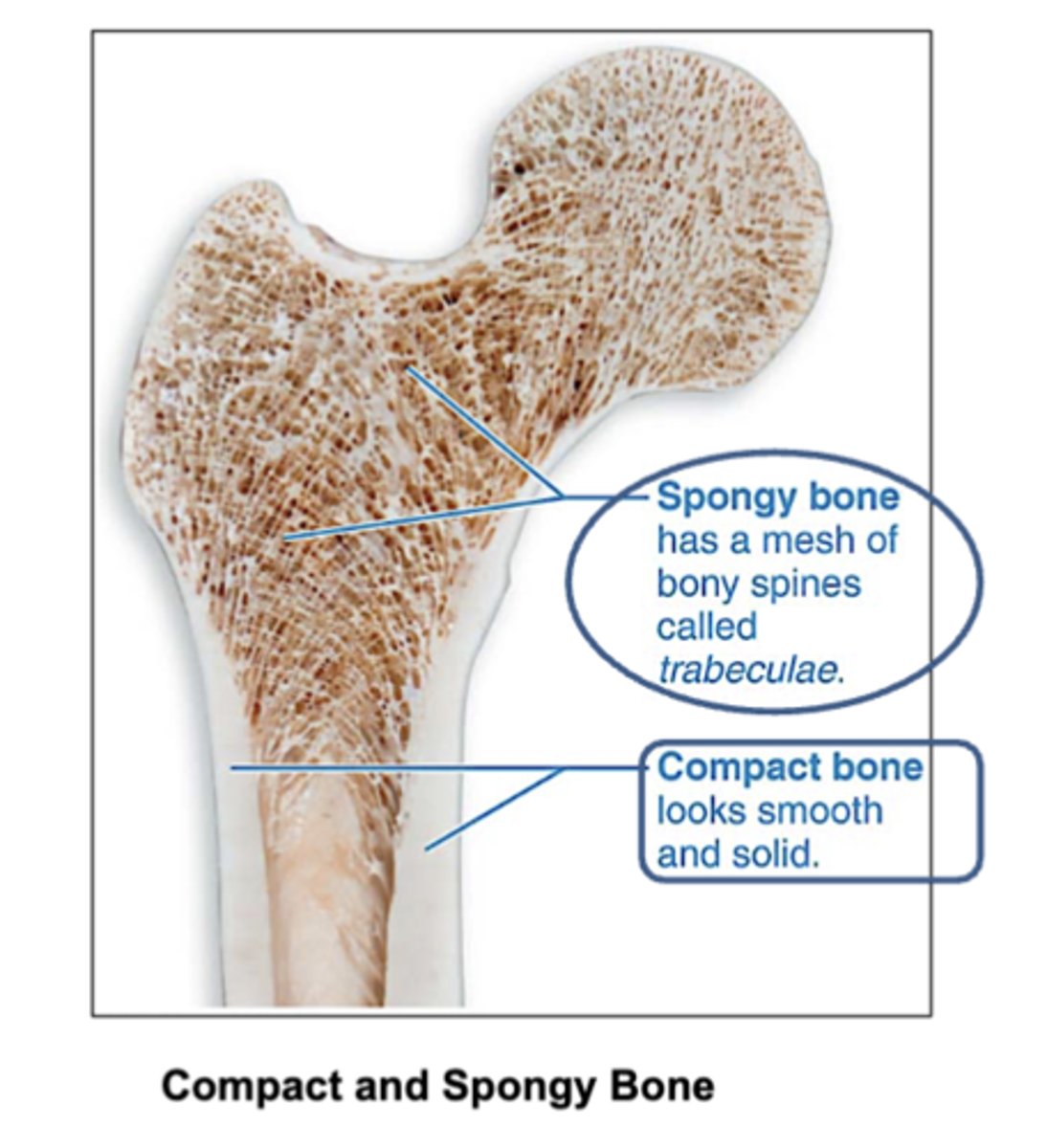
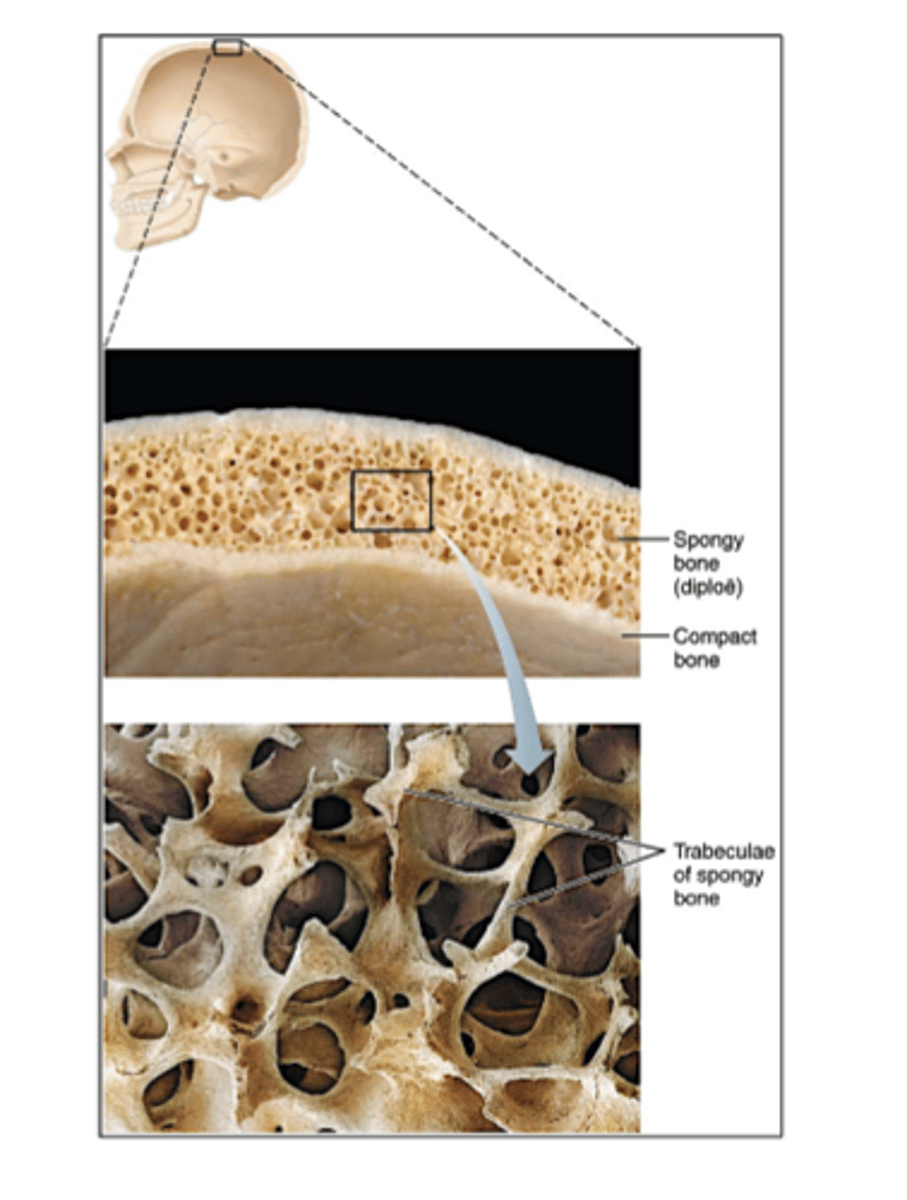
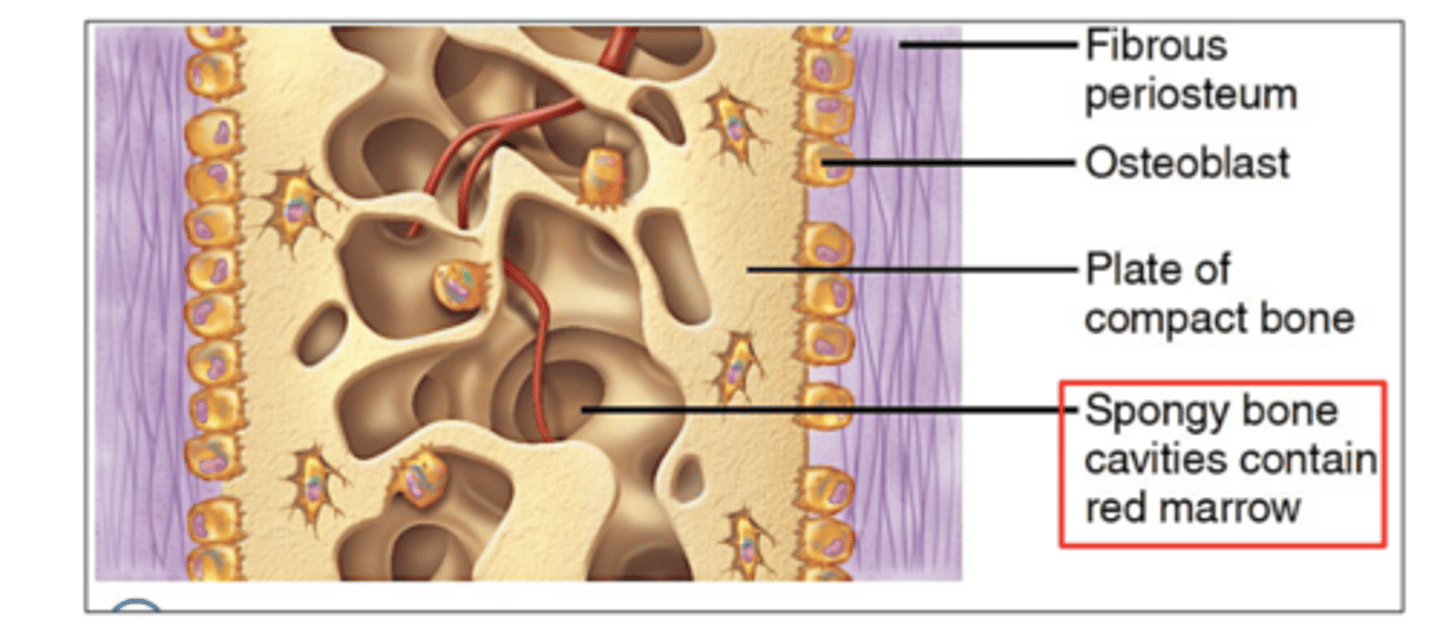
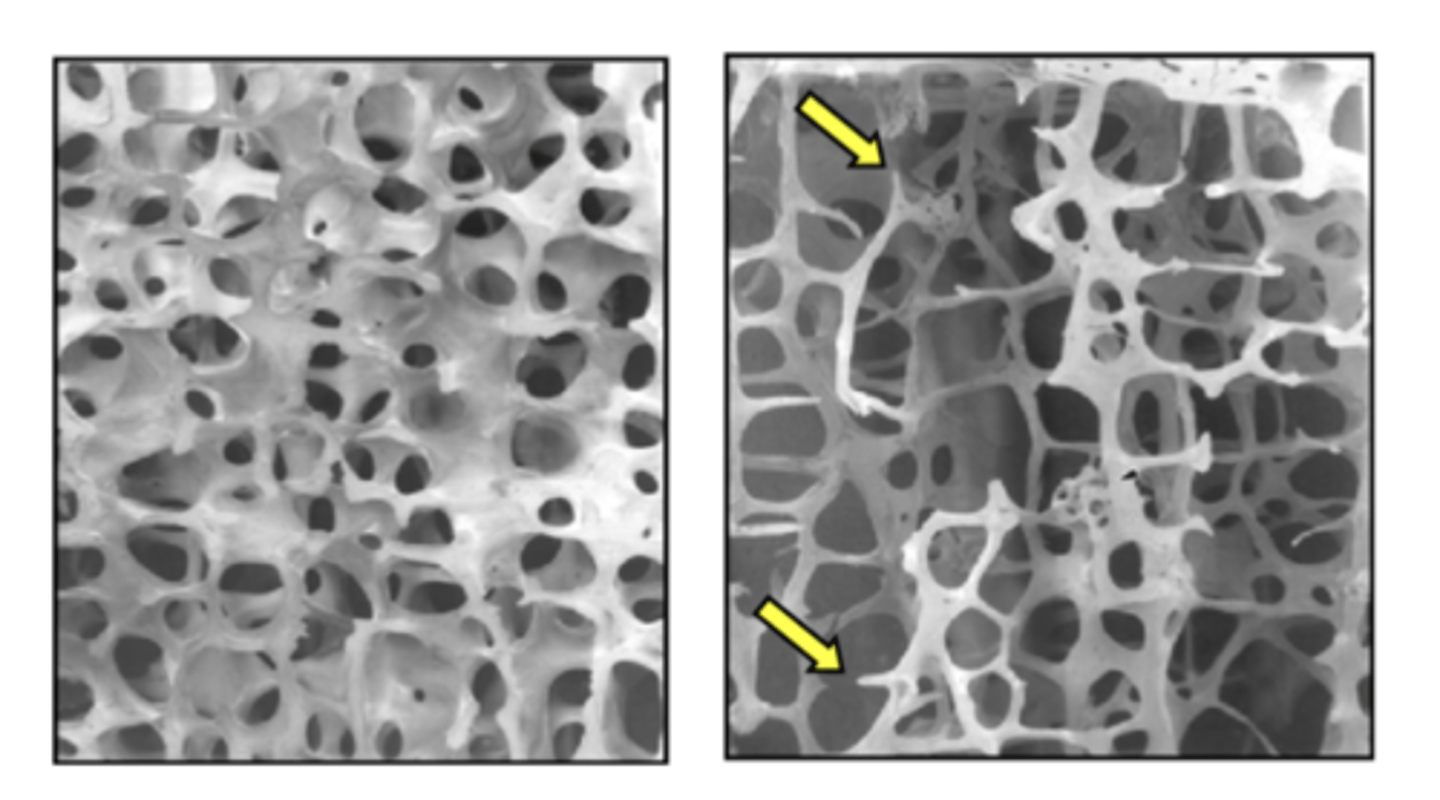
Location of compact and spongy bone?
Compact bone: Found on the outer layer of bones. (looks smooth and solid)
Spongy bone: Found inside bones, mainly at the ends of long bones.
And in flat bones like the ribs, vertebrae and skull bones.
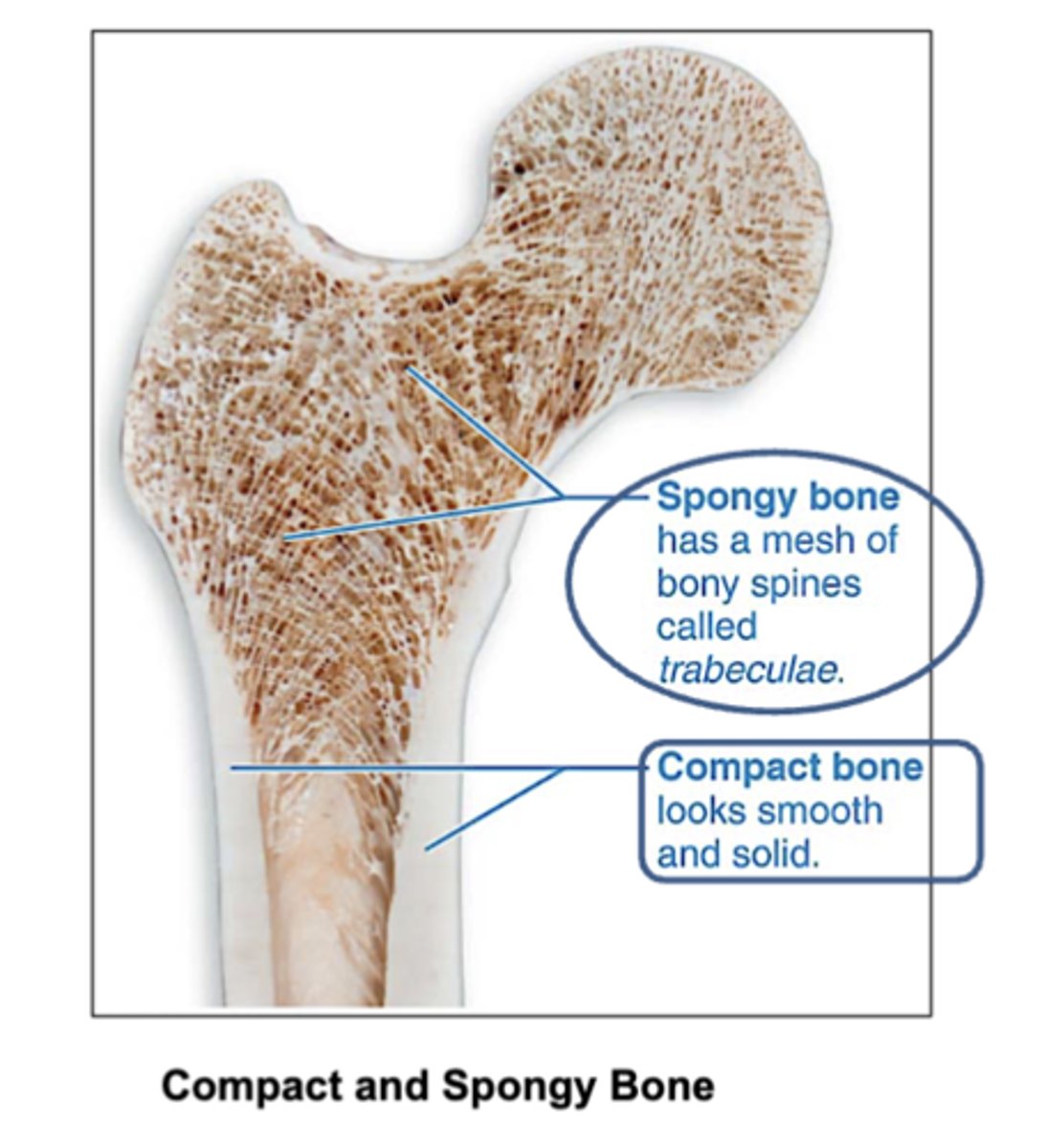
How does compact bone look?
smooth and solid
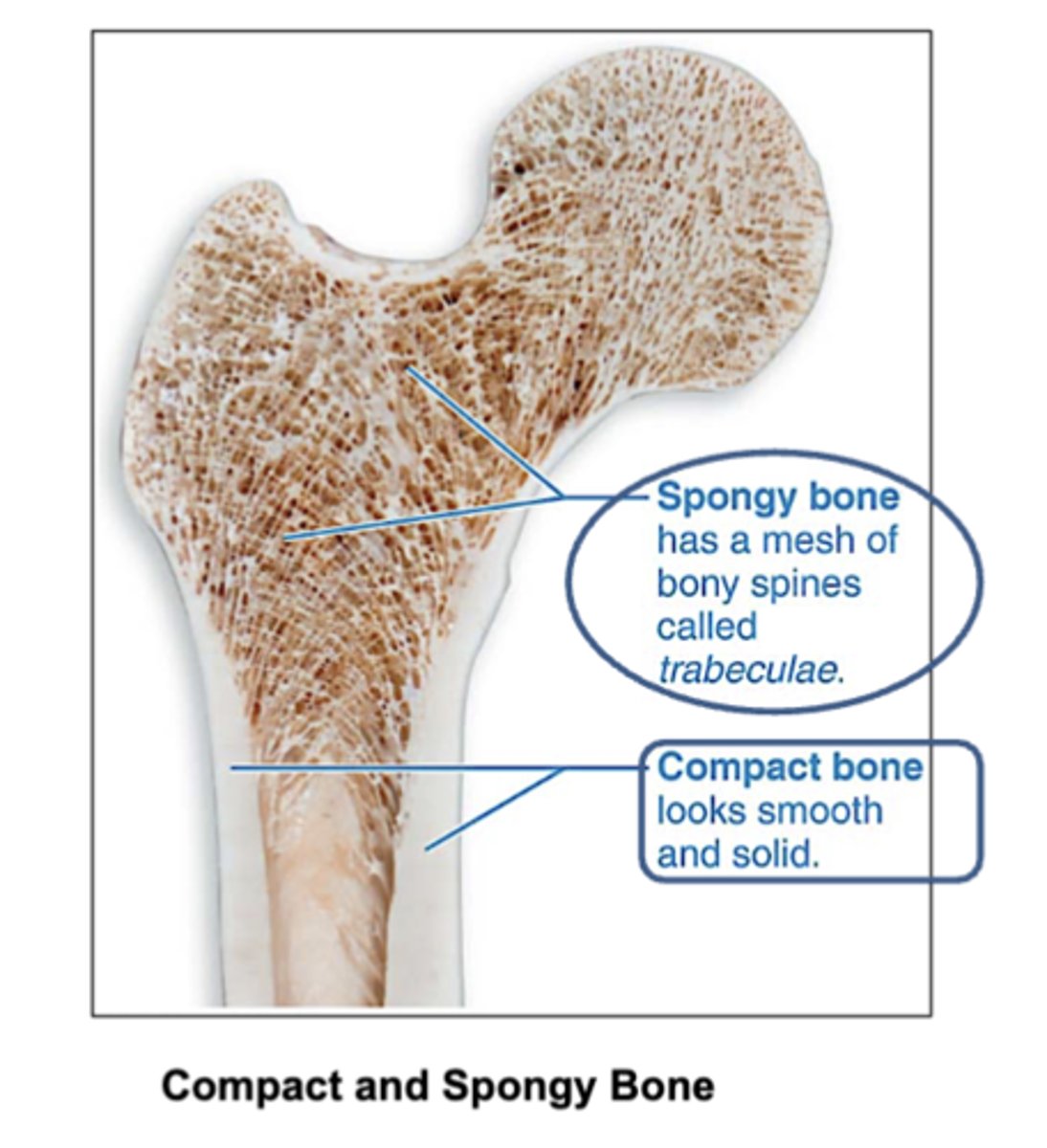
What are spongy bones made of?
trabeculae that contain the osteocytes.
Red marrow fills the spaces.
What fills in the inside of spongy bones?
red bone marrow
where is spongy bone found?
in epiphyses (ends )of long bones and in flat bones such as ribs, vertebrae and skull bones.
What is trabeculae?
the small, needle-like structures that form the network in spongy bone.
Inside of them is the red bone marrow.
3 Structure of compact bone:
- Osteon: basic unit of compact bone. there's a canal in between each osteon.
- Bone lamellae: basic structure of compact bone. concentric rings/layers of collagen fibers and bone matrix .
- Central canals and Perforating canals: contain blood vessels and nerves
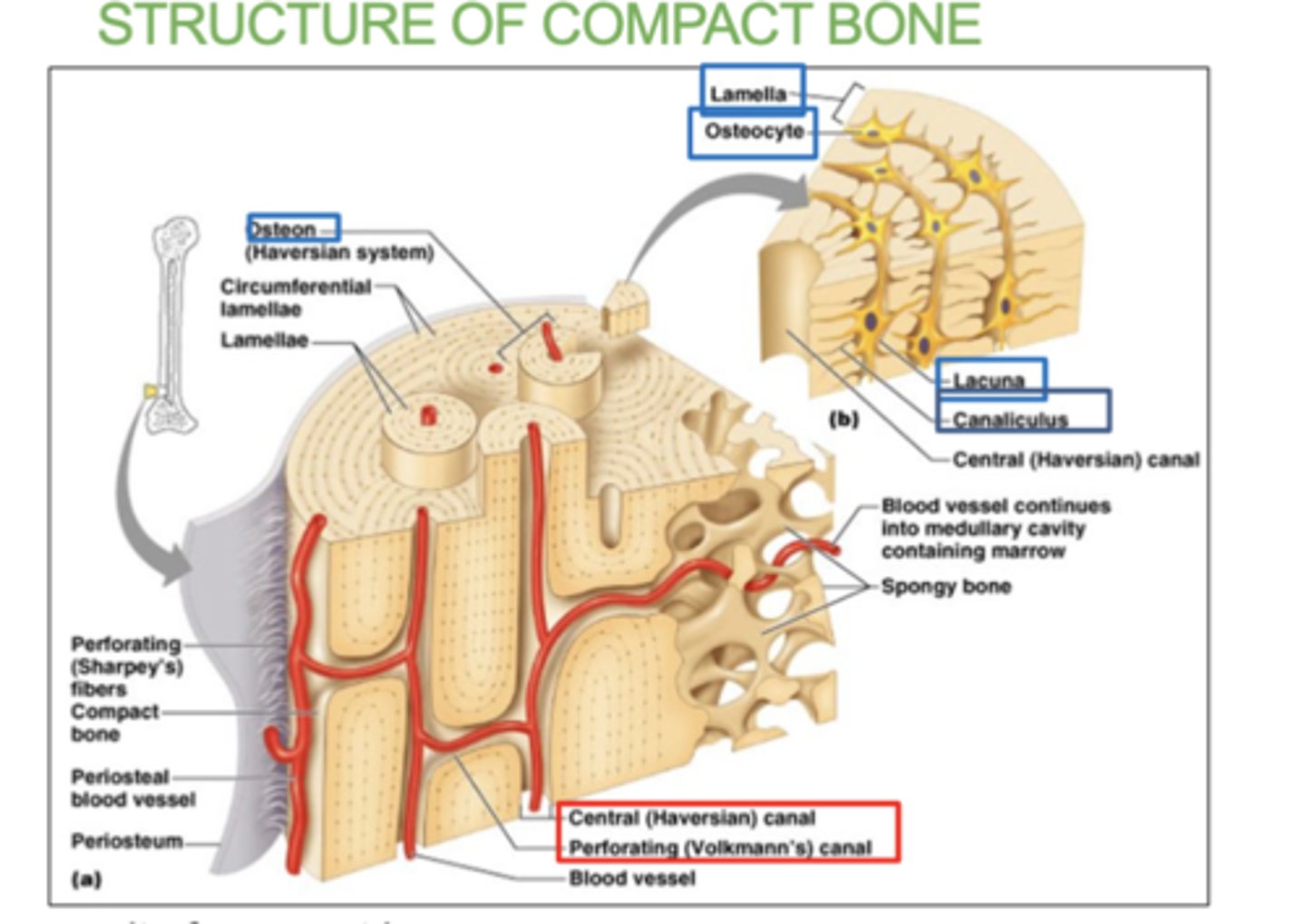
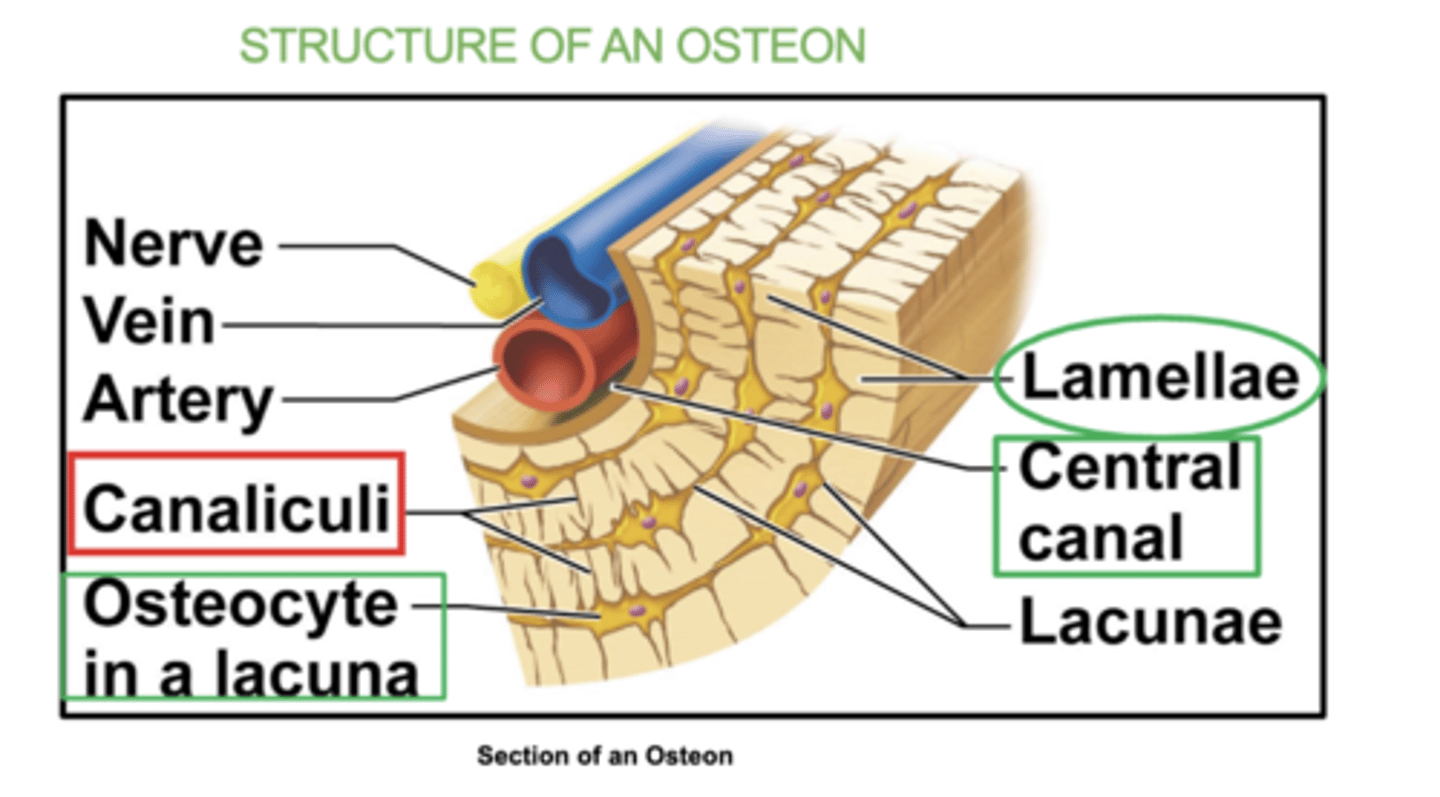
4 Structures of an Osteon:
(all in the osteon)- osteocyte, lacuna, lamellae, & canaliculi
Each osteocytes sit inside hollow spaces called lacuna.
Very thin hair-like canals called canaliculi radiate from each lacuna and allow osteocytes to communicate.
They eventually connect to the central canals
what is an osteocyte?
a mature bone cell that helps maintain bone tissue.
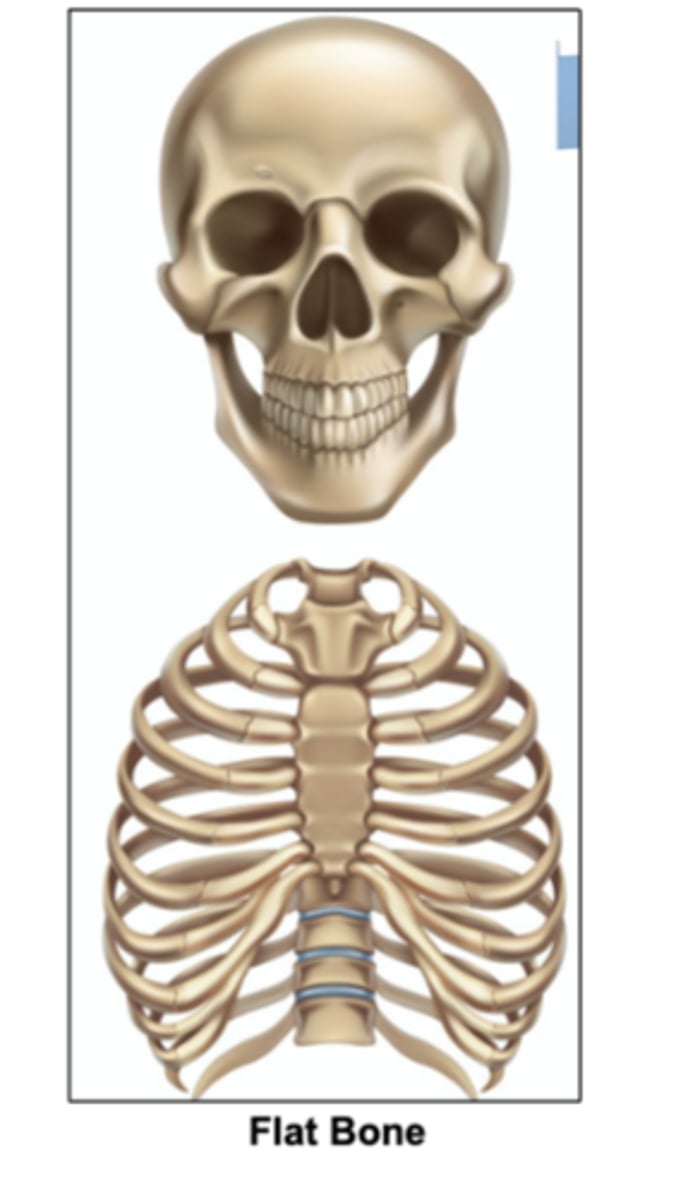
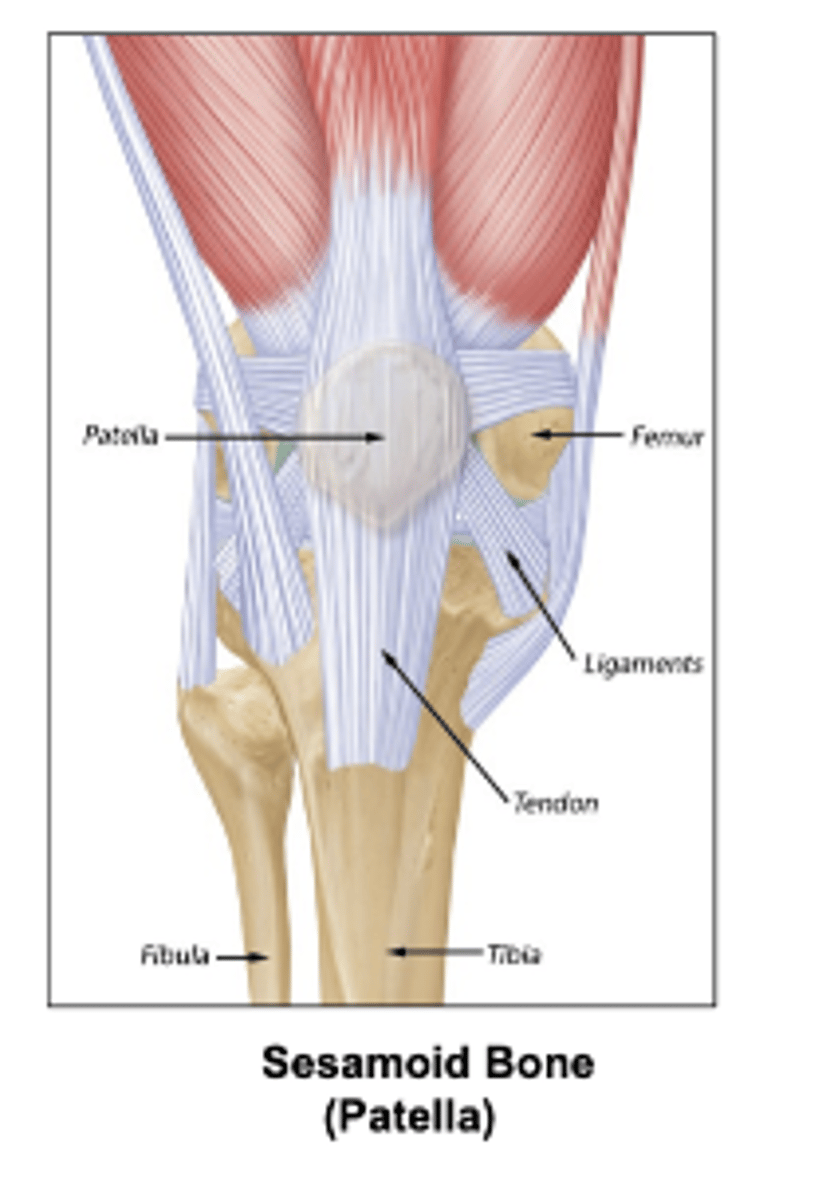
Some types of bones shapes are:
Long, short, flat irregular, irregular, and sesamoid (bone embedded within a tendon).
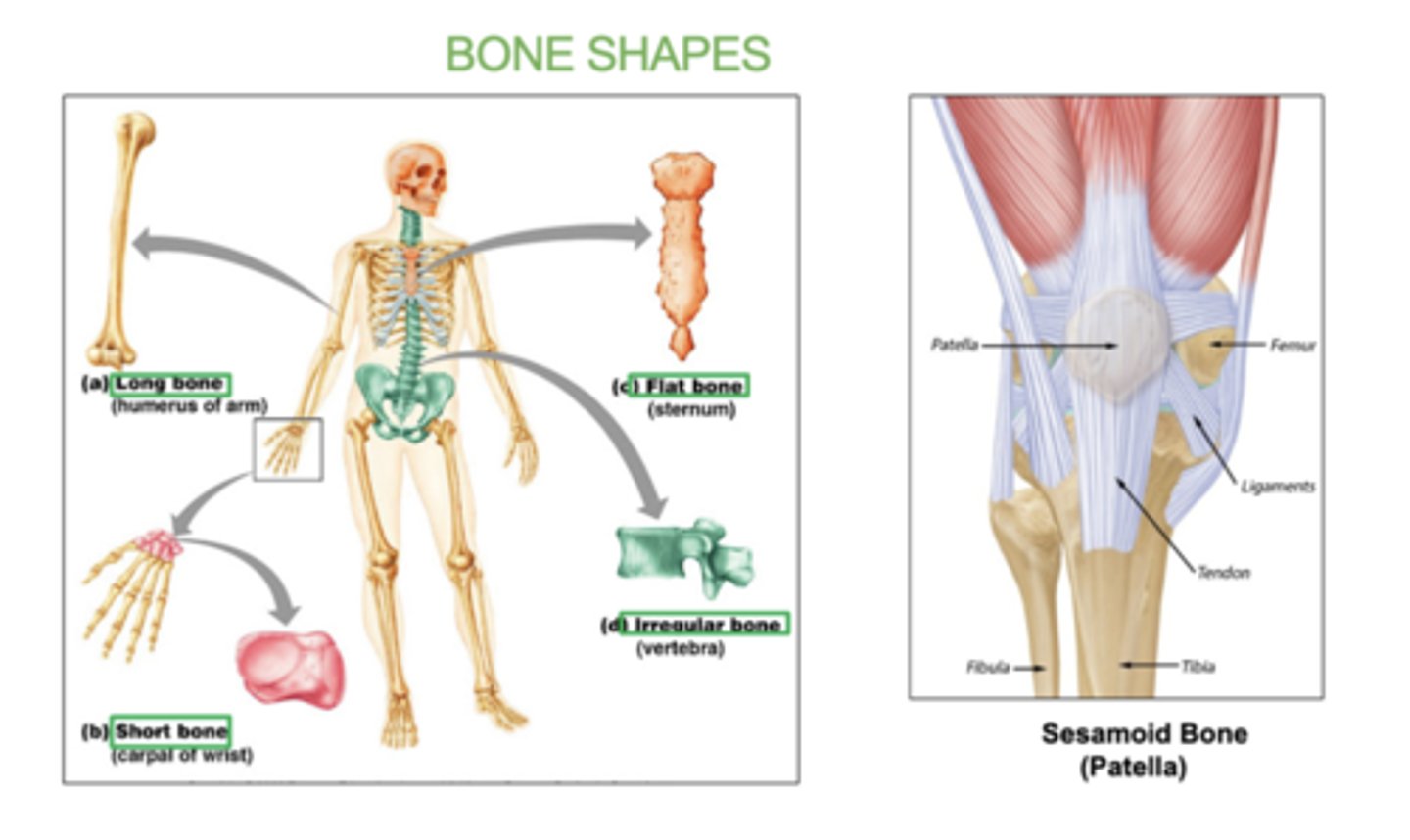
examples of long bones:
(all limbs)
femur, humerus, radius, ulna, tibia, fibula
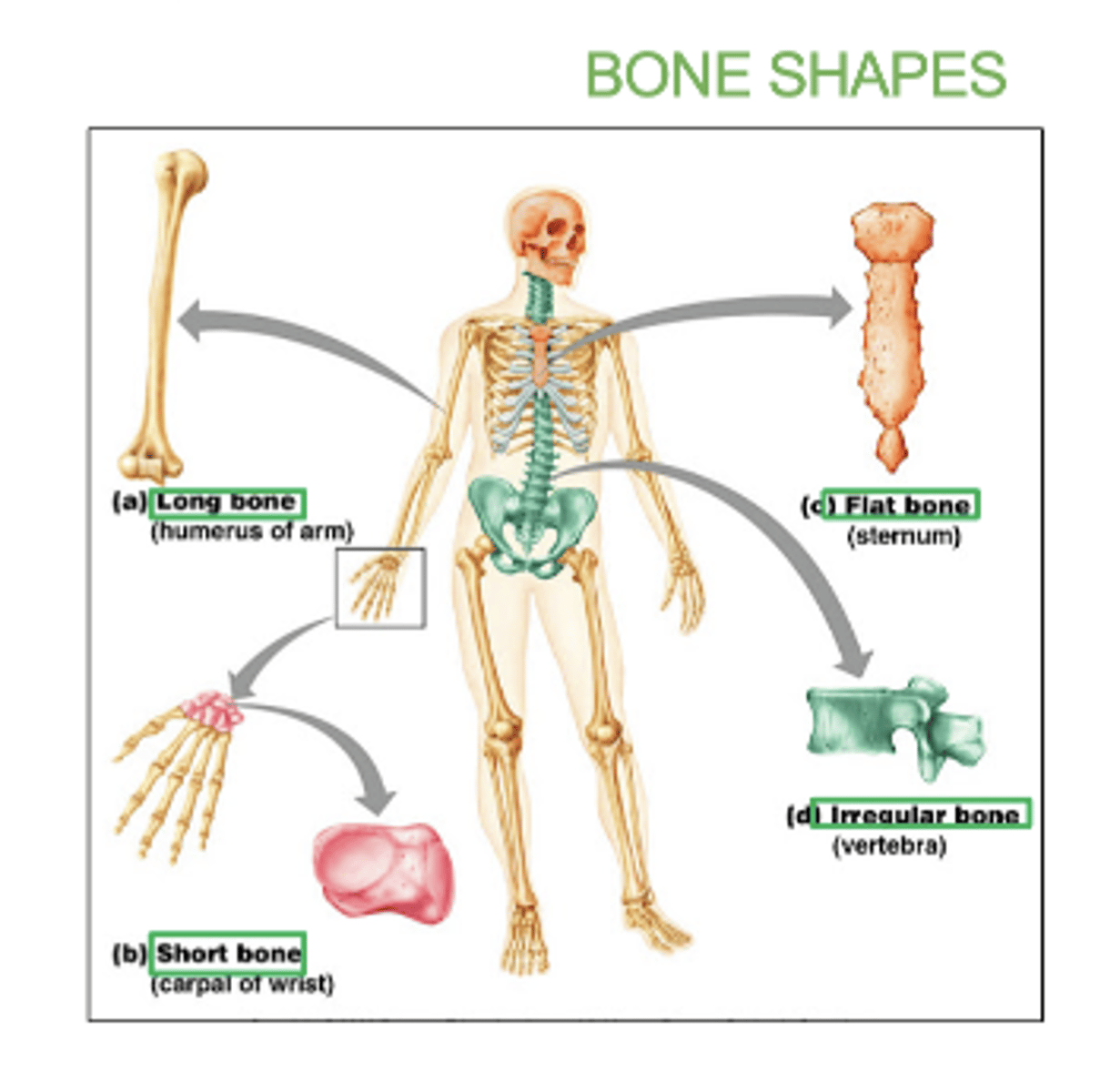
examples of flat bones:
skull, ribs, sternum, & scapula
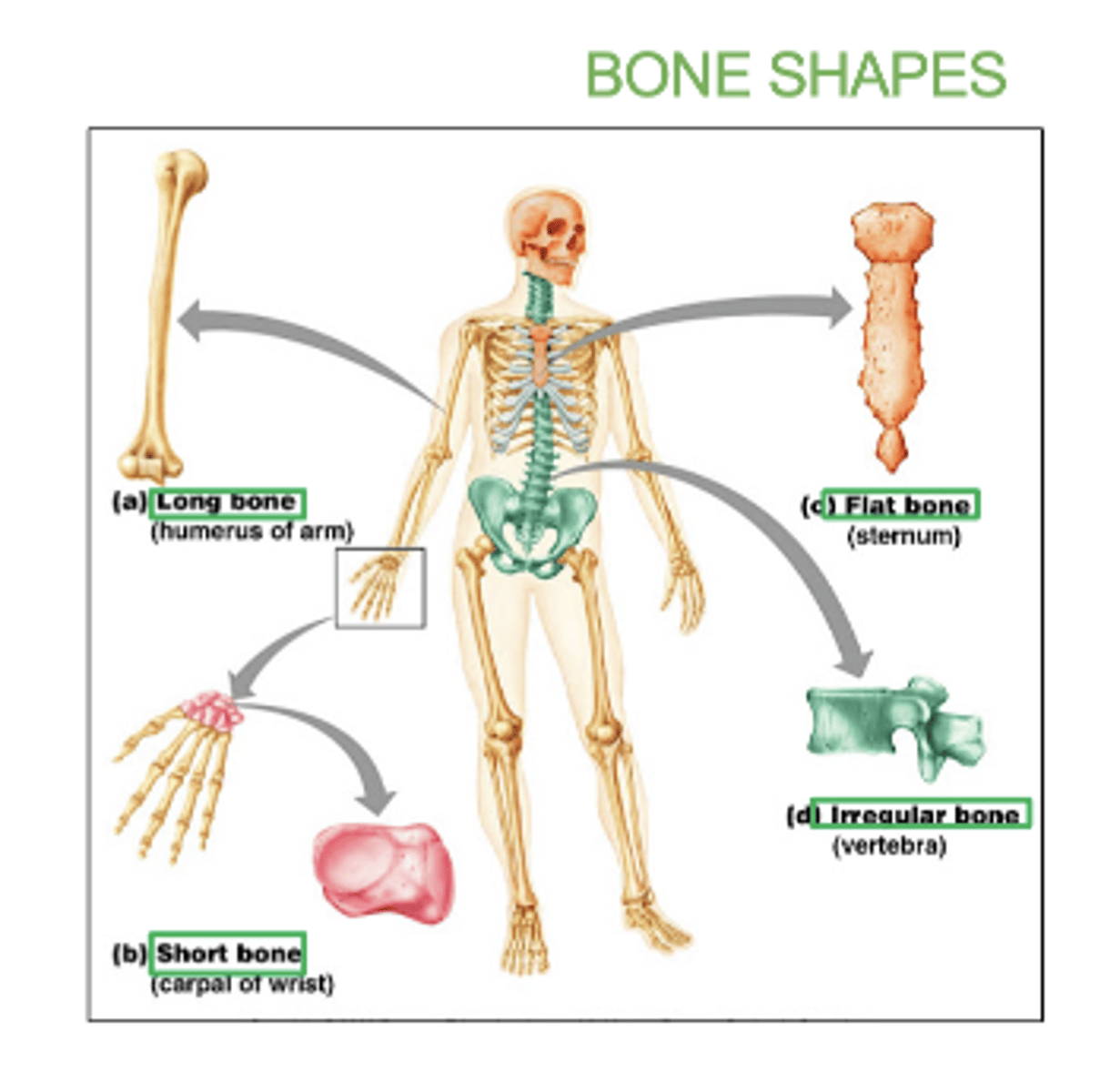
examples of short bones:
carpals and tarsals
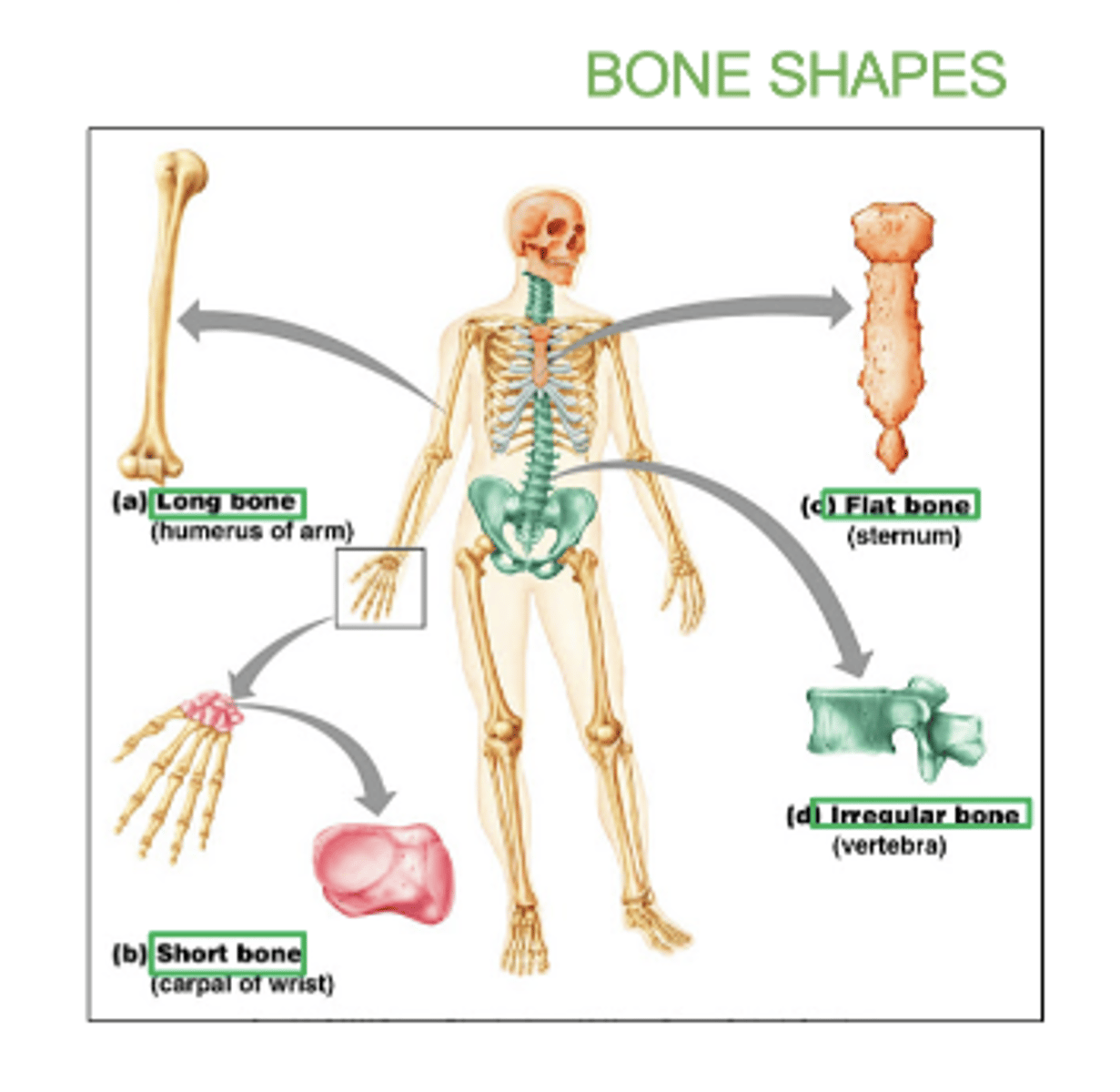
examples of irregular bones:
vertebrae and hip bones
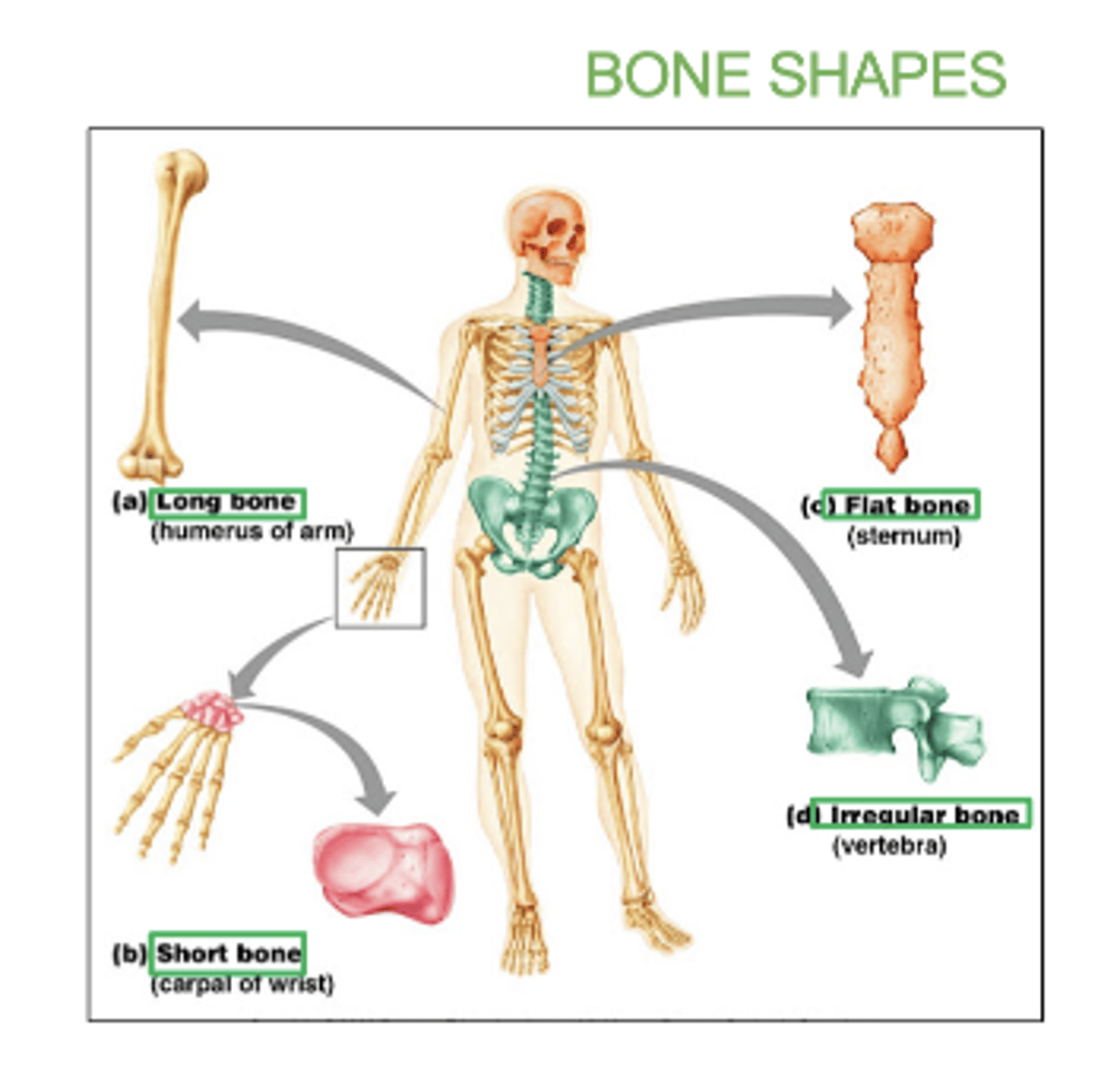
examples of sesamoid bone:
patella
All _____ bones contain spongy bones.
flat
What is bone ossification?
the process by which bone tissue is formed
- either by replacing cartilage or developing directly from connective tissue.
What is intramembranous ossification?
-Bone develops from mesenchyme (embryonic connective tissue)
-Forms flat bones (skull, clavicles) which are mainly spongy bone.
-Multiple ossification centers fuse
what's mesenchyme (embryonic connective tissue)?
the tissue found in embryos that develops into different types of connective tissue in the body, including bone, cartilage, and blood.
what does embryos have to do with bone ossification?
Embryos are where bone ossification begins.
-During early development, the bone starts forming from embryonic connective tissue (mesenchyme) or cartilage, leading to the creation of the skeletal structure.
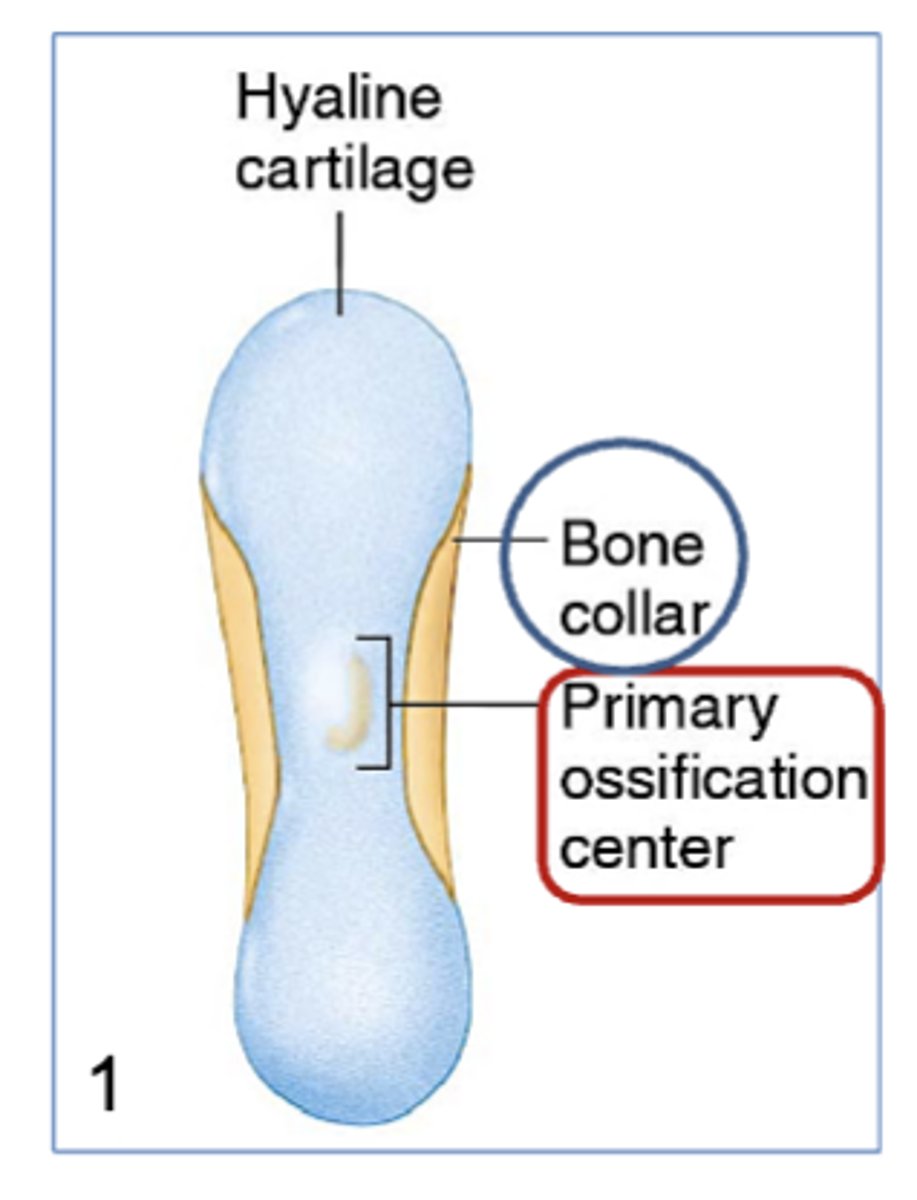
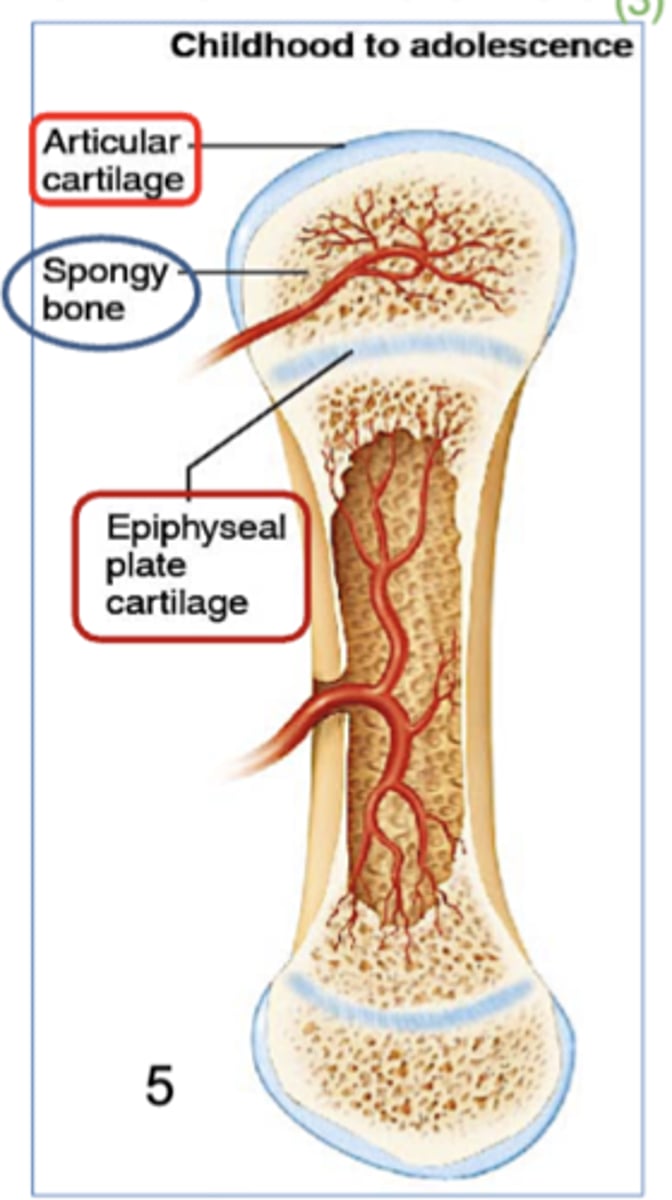
What is Endochondral Ossification?
-Bone replaces hyaline cartilage.
-Occurs at long bones and forms compact bone.
-Primary and secondary ossification centers.
What does it mean when you see an epiphyseal line?
That the bone is done growing.
What does it mean when you see an epiphyseal plate?
the growth in length of long bone NOT done.
What's hyaline cartilage?
- a smooth, glassy type of cartilage found in joints, ribs, nose, and the respiratory system.
- provides support and flexibility.
what is flat Bone Intramembranous Ossification?
the process by which flat bones (like the skull and clavicles) form directly from soft mesenchymal tissue ( embryonic connect tissue) without a cartilage model.
This process creates spongy bone in the center, with a thin layer of compact bone surrounding it.
What is usually surrounding spongy bone?
a thin rim of compact bone
Process of Intramembranous Ossification (4 steps)
Osteoblasts Secrete Tiny Spaces, Forming Compact bone.
1. Ossification Centers form
2. Secretion and Calcification of Osteoid Tissue
3. Trabeculae/Spongy Bone From along w/ formation of Periosteum
4. Spongy bone filling with bone marrow and Formation of Compact Bone
Step 1 of Process of Intramembranous Ossification
1. Ossification Centers form
Mesenchymal cells in the embryo change into osteoblasts and group together to form ossification centers where bone development begins
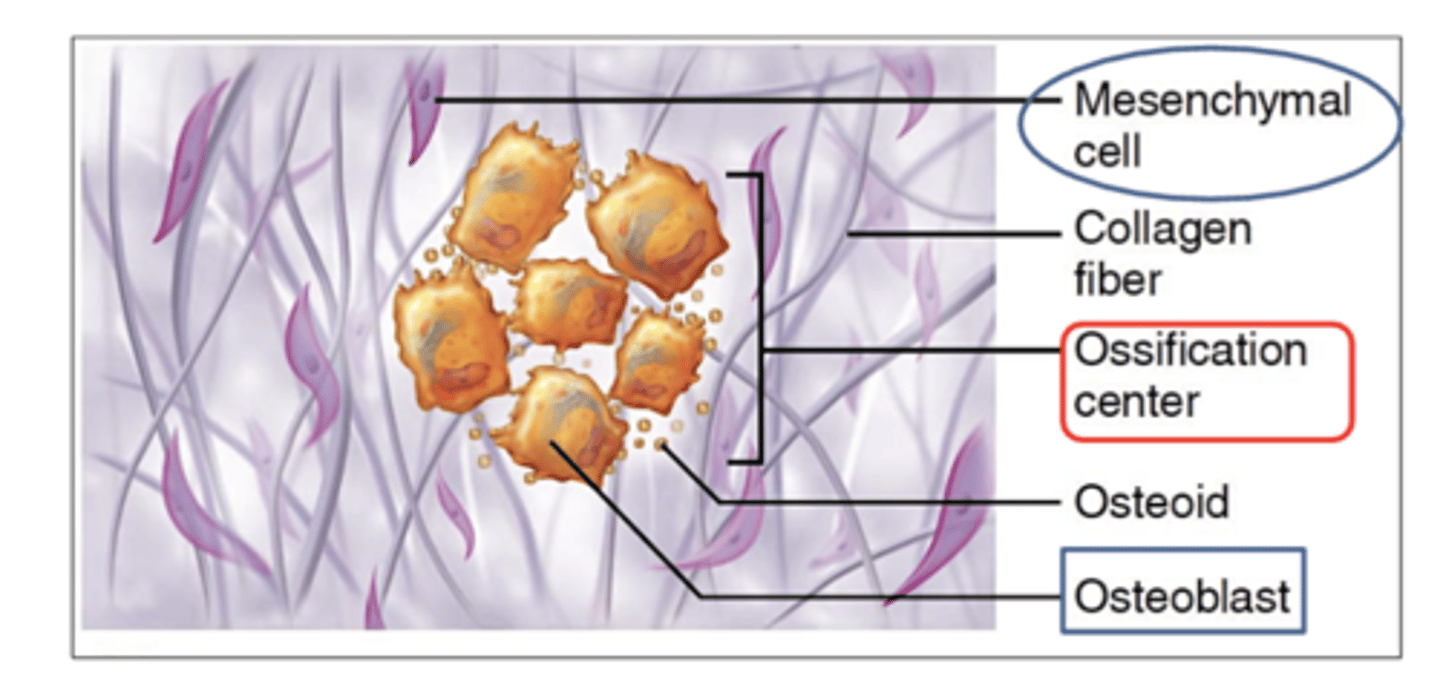
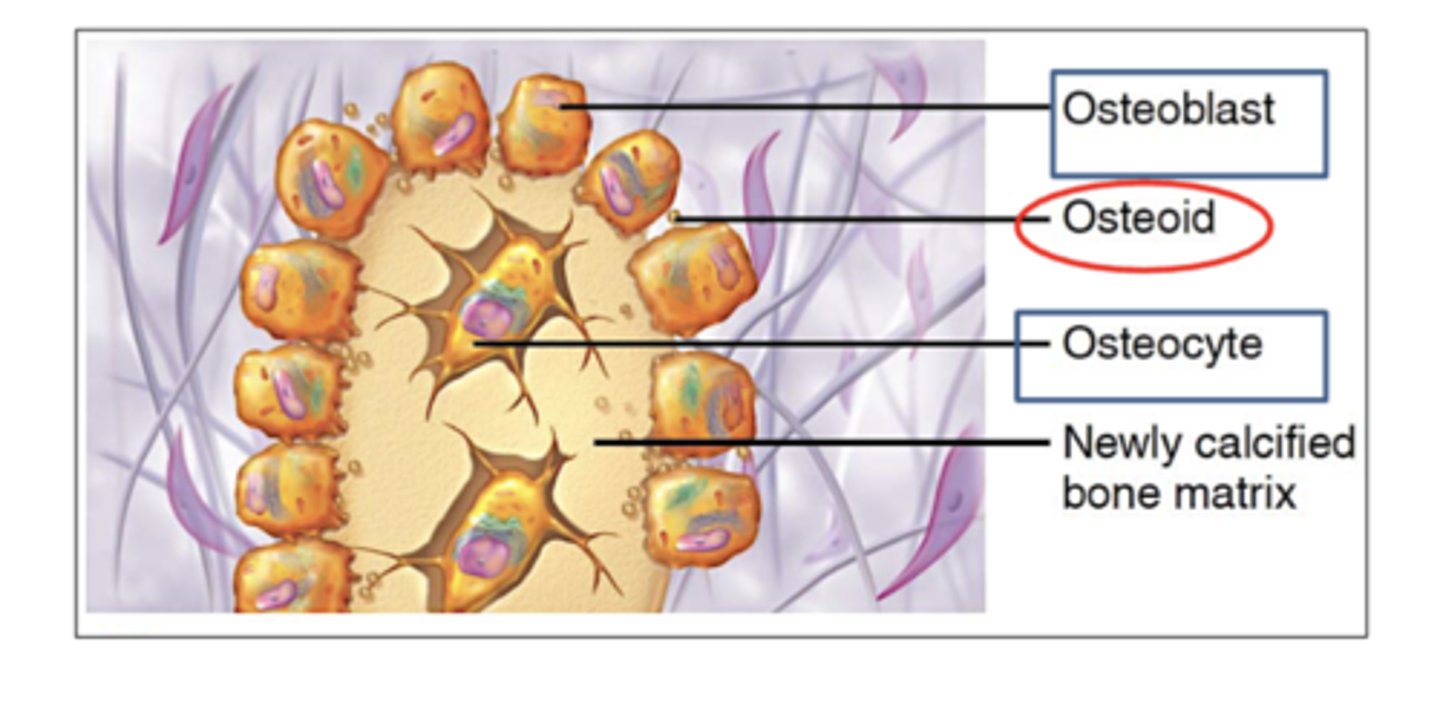
Step 2 of Process of Intramembranous Ossification
2. Secretion and Calcification of Osteoid Tissue
Osteoblasts secrete osteoid tissue (bone matrix)
As osteoblasts continue secreting osteoid, some of them get trapped and surrounded by the matrix.
THEN these trapped osteoblasts become osteocytes.
The trapped osteoid matrix inside also then becomes calcified
(filling with calcium and hardening)
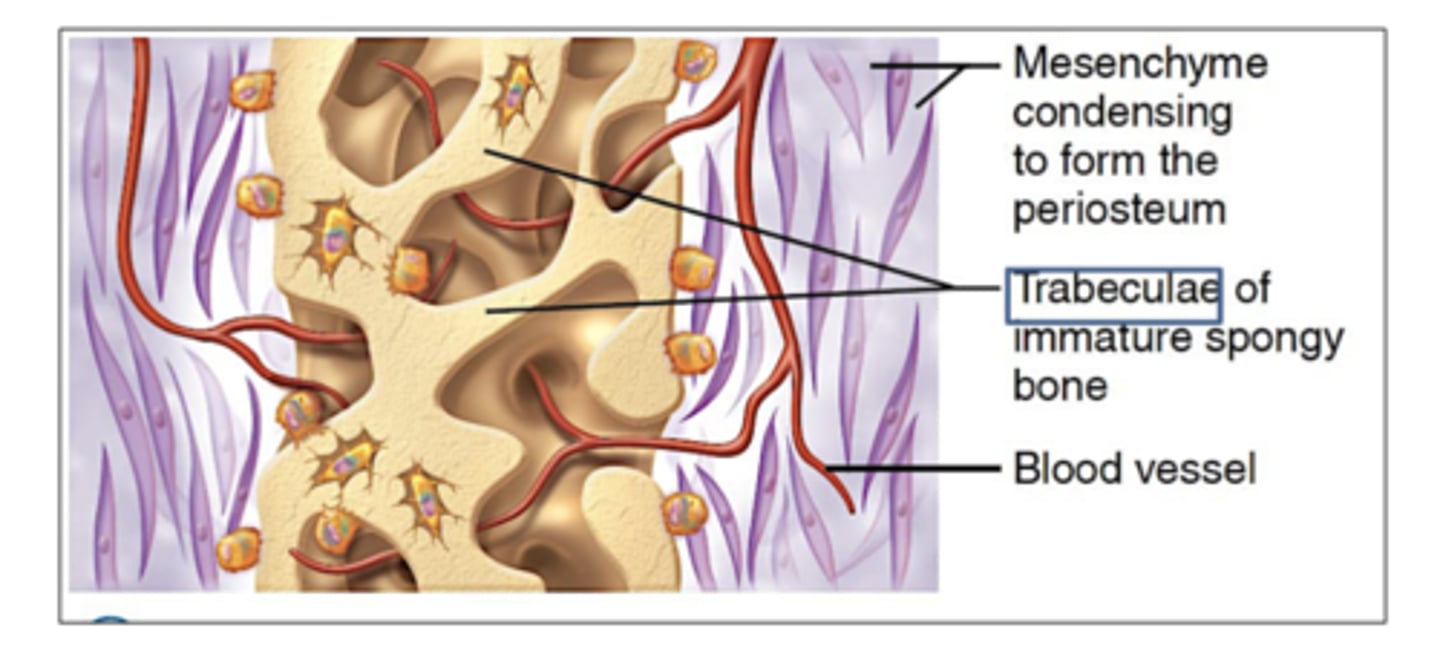
Step 3 of Process of Intramembranous Ossification
3. Trabeculae/Spongy Bone From along w/ formation of Periosteum
The calcified osteoid forms a network of trabeculae, creating spongy bone around blood vessels.
The outer mesenchyme condenses to form the periosteum (bone’s outer lining).
Step 4 of Process of Intramembranous Ossification
4. Spongy bone filling with bone marrow and Formation of Compact Bone
Spongy bone matures and fills with bone marrow.
then, a thin layer of compact bone develops beneath the periosteum for strength.
What's Osteoid tissue?
what osteoblasts secrete to build bones.
unmineralized bone matrix (made of collagen and proteins) that osteoblasts produce
Endochondral ossification process (5 steps)
1) Bone collar forms around the diaphysis, and the primary ossification center forms
2) The bony collar reduces blood flow to the inside of the cartilage, cutting off nutrients to the chondrocytes, causing them to break down.
3) Osteoblasts replace chondrocytes with spongy bone, surrounded by compact bone.
4) Osteoclasts create the medullary cavity; blood vessels bring osteoblasts to form spongy bone and the secondary ossification centers
5) Once complete, hyaline cartilage remains as articular cartilage and in the epiphyseal plate.
Whats bone matrix?
osteoid tissue (or bone matrix) which is what what osteoblasts secrete which later calcifies (hardens) as calcium deposits fill it, forming solid bone tissue.
Step 1 of the Endochondral ossification process?
1) Bone collar forms around the diaphysis, and the primary ossification center forms
Step 2 of the Endochondral ossification process?
2) The bony collar reduces blood flow to the inside of the cartilage, cutting off nutrients to the chondrocytes, causing them to break down.
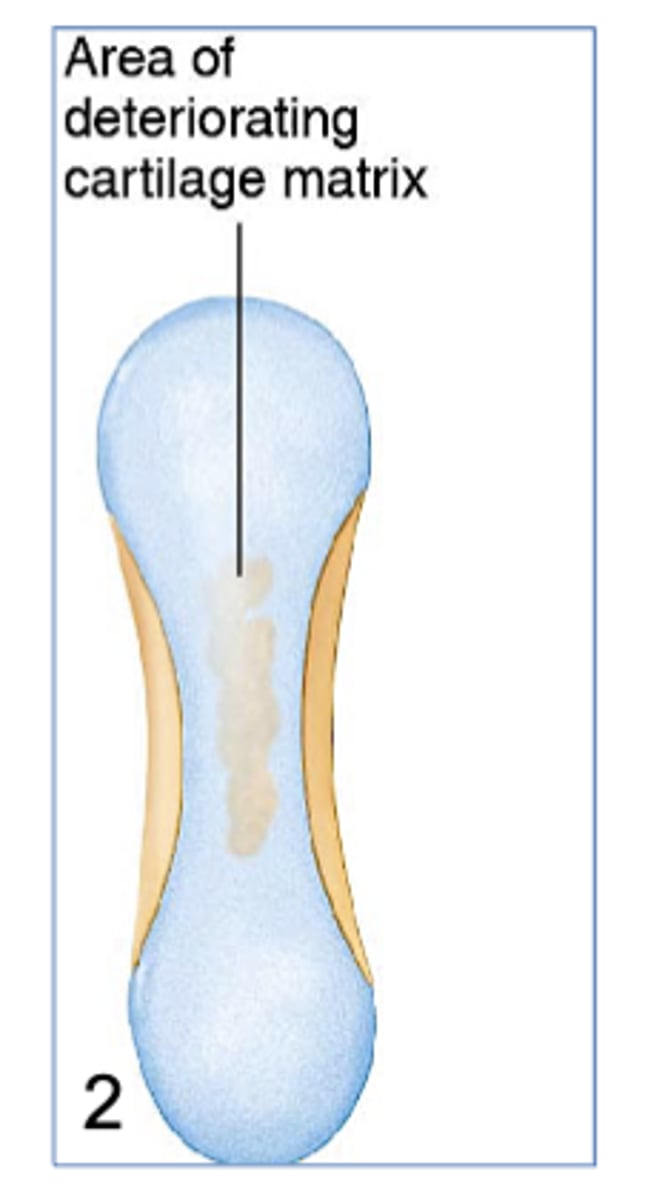
Step 3 of the Endochondral ossification process?
3) Osteoblasts replace chondrocytes with spongy bone, surrounded by compact bone.
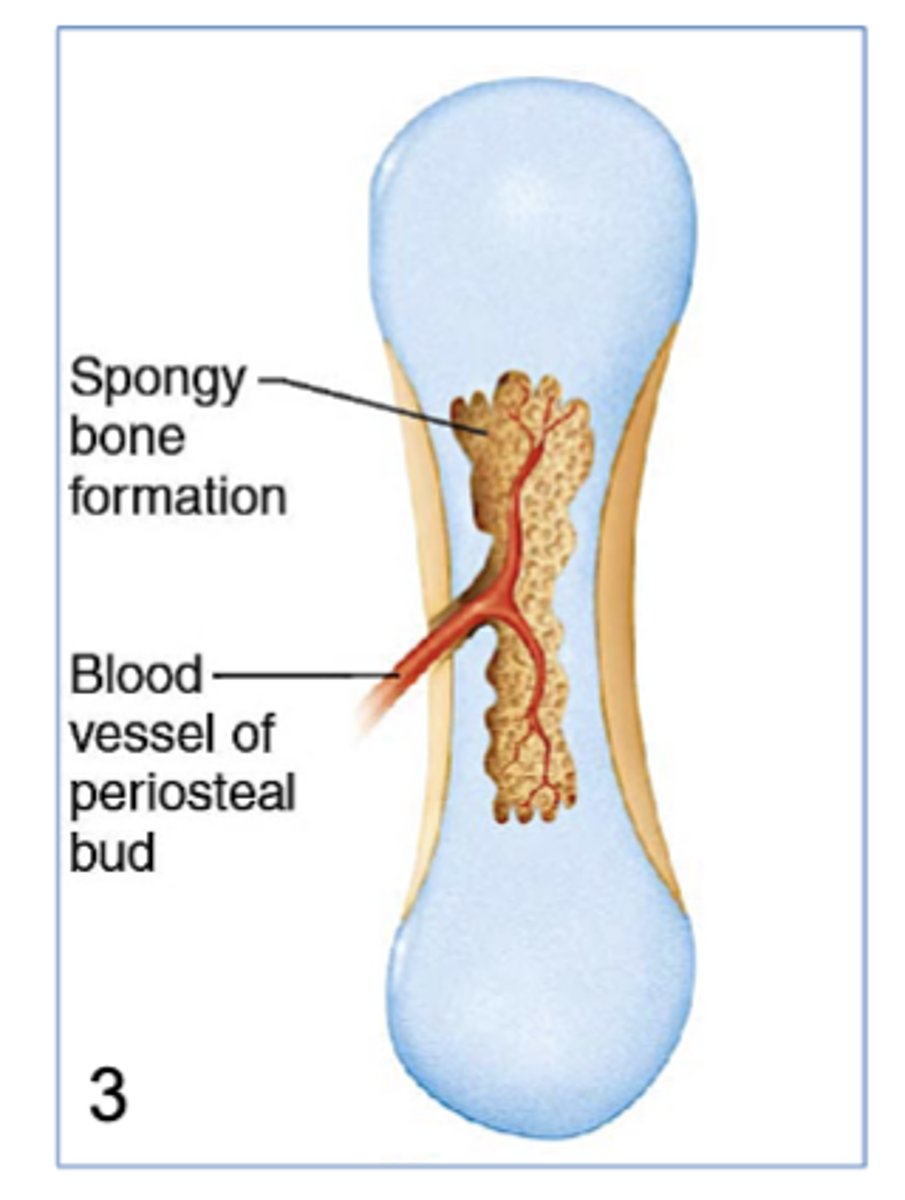
Step 4 of the Endochondral ossification process?
4) Osteoclasts create the medullary cavity; blood vessels bring osteoblasts to form spongy bone and the secondary ossification centers
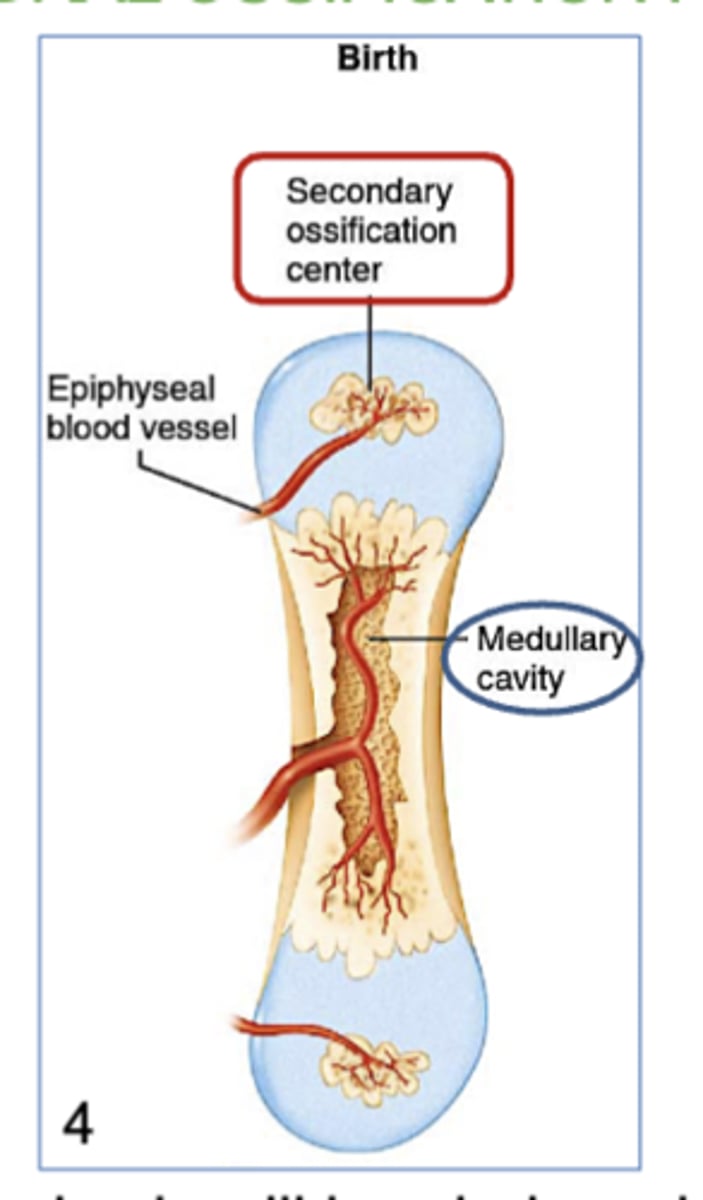
Step 5 of the Endochondral ossification process?
5) Once complete, hyaline cartilage remains as articular cartilage and in the epiphyseal plate.
What Are Ossification Centers?
the specific areas where bone formation begins during ossification.
These centers are where osteoblasts start producing bone tissue, either directly from mesenchyme (intramembranous) or by replacing cartilage (endochondral).
Where does hyaline cartilage remain at the end of endochondral ossification?
it covers the epiphysis forming the articular cartilage and in the epiphyseal plate.
what does fetal primary ossification centers mean?
Its the first areas where bone begins to form (ossification centers) .
At around 12 weeks of fetal development,
These centers replace cartilage with bone.
(part of endochondral ossification)
When/where does Endochondral ossification start?
in the embryo, at 12 weeks.
what are Cartilage cells called?
chondrocytes
Appositional growth of bone (definition)
when bones grow in width.
the process by which deeper lamellae (layers of compact bone) are broken down by osteoclasts, recycled and replaced by new bone secreted by osteoblasts.
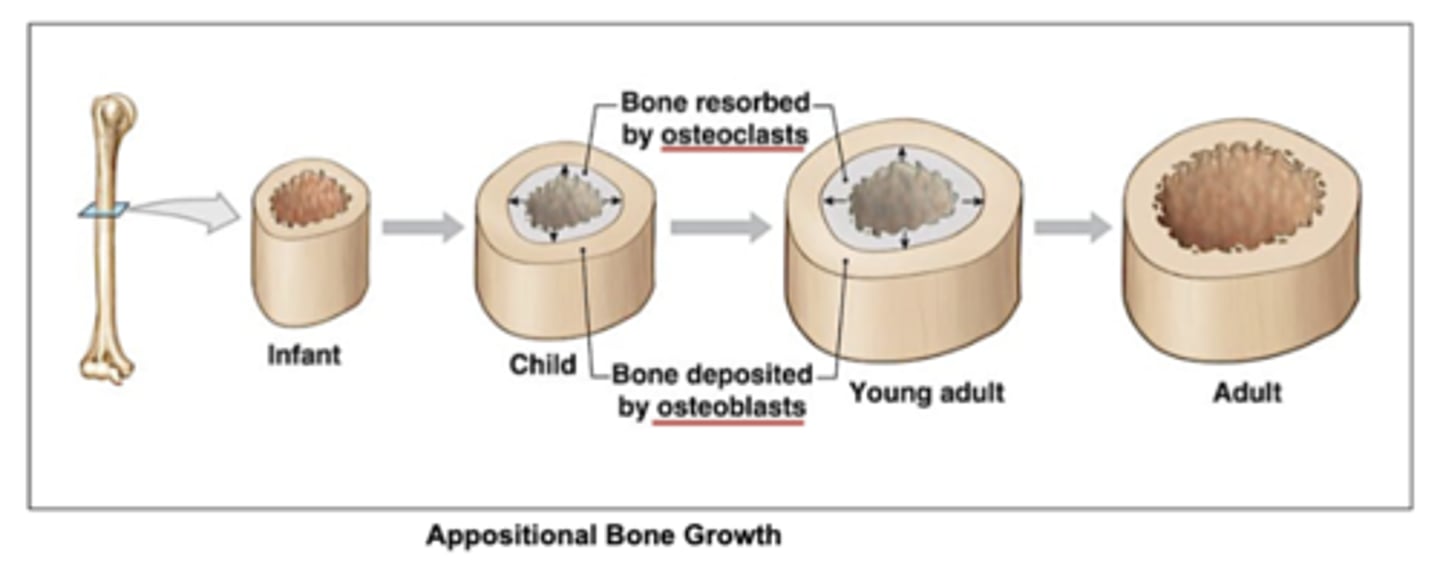
what is lamallae?
layers of compact bone.
concentric rings of bone matrix that form around the central canal in an osteon (bone unit).
Where does longitudinal bone growth occur?
at the epiphyseal plates.
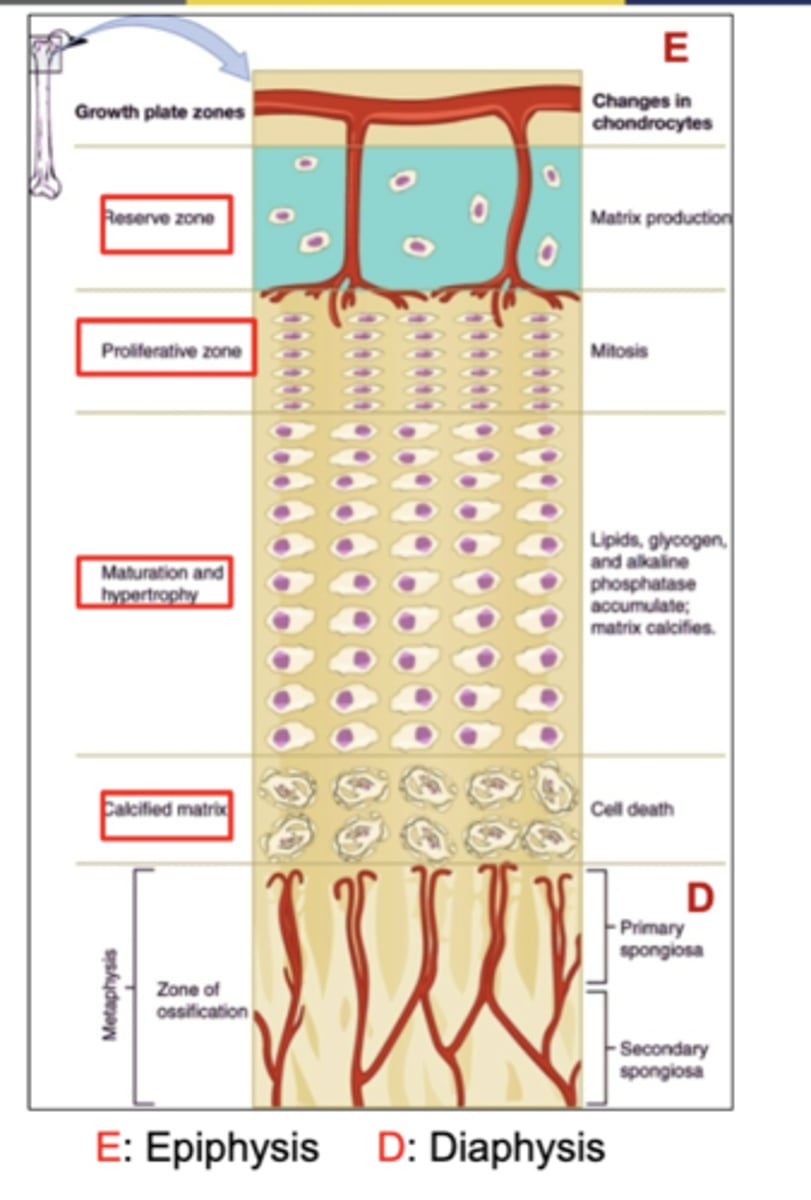
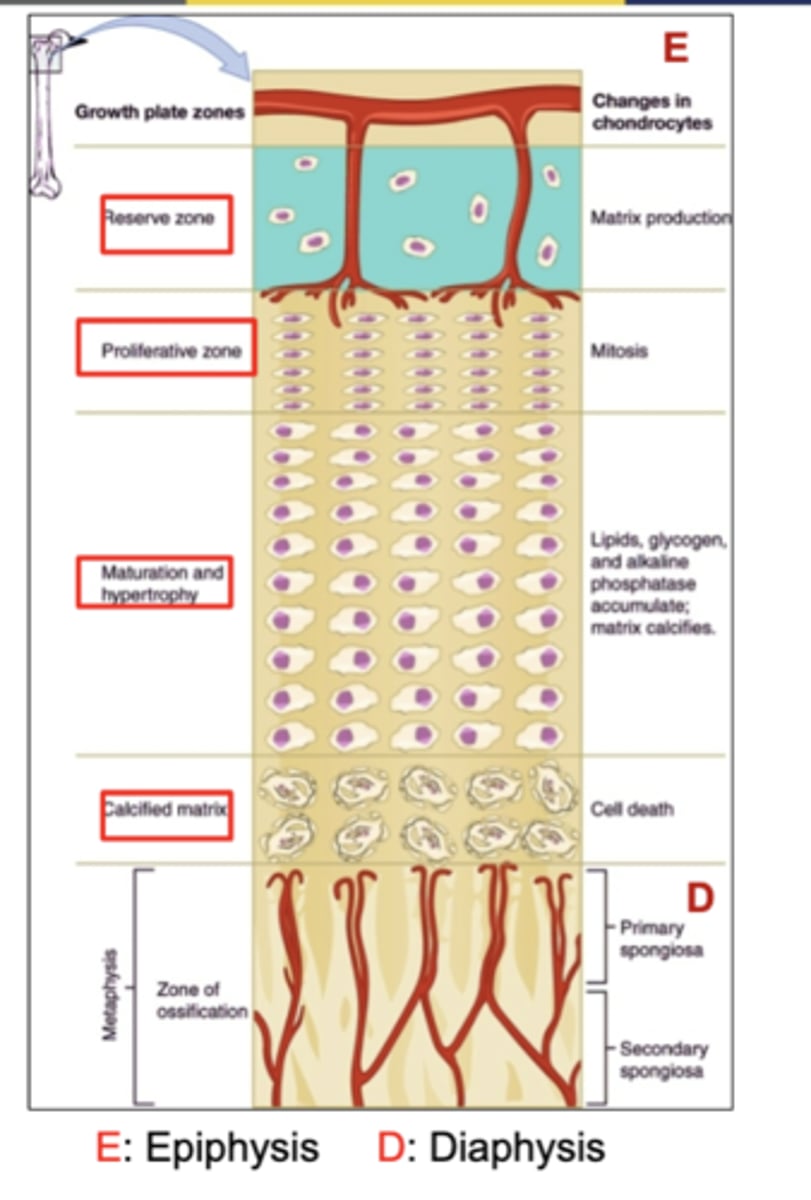
the 4 zones of growth for longitudinal bone growth?
reserve
proliferation
maturation and hypertrophy
calcified matrix
What happens in the "Reserve Cartilage" zone?
(a zone of growth for longitudinal bone growth)
(Reserve - Resting)
It is the resting cartilage zone, where cells are not actively dividing.
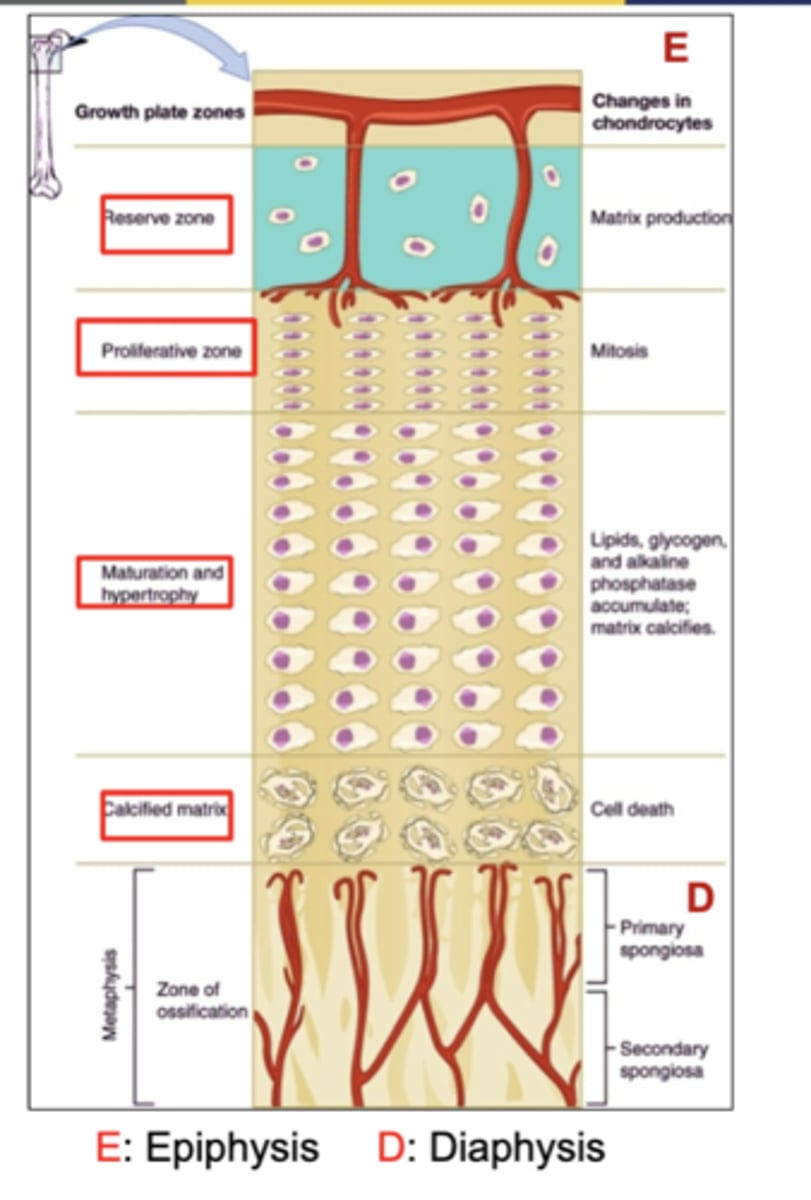
What happens in the "Proliferation" zone?
(a zone of growth for longitudinal bone growth)
(proliferation = mitosis, new cell life)
Chondrocytes actively divide by mitosis.
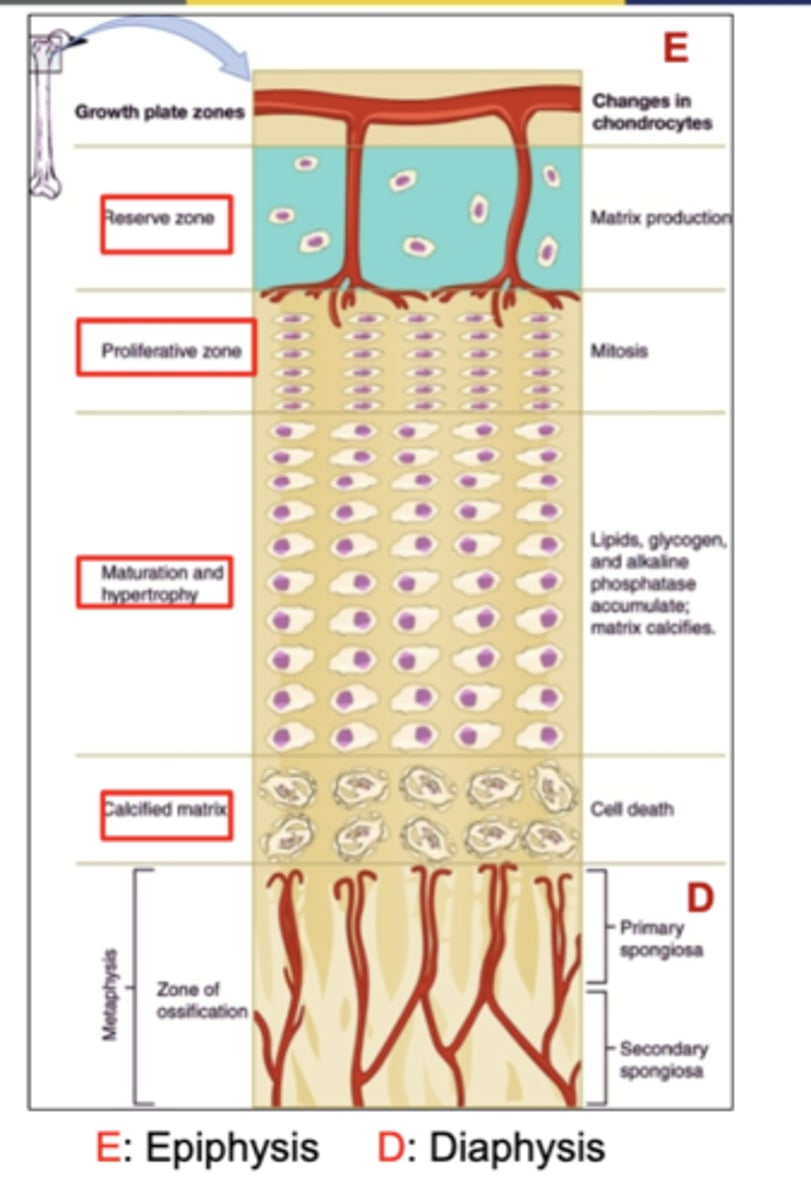
What happens in the "Maturation and Hypertrophy" zone?
(a zone of growth for longitudinal bone growth)
(hyper - too much)
Chondrocytes enlarge too much.
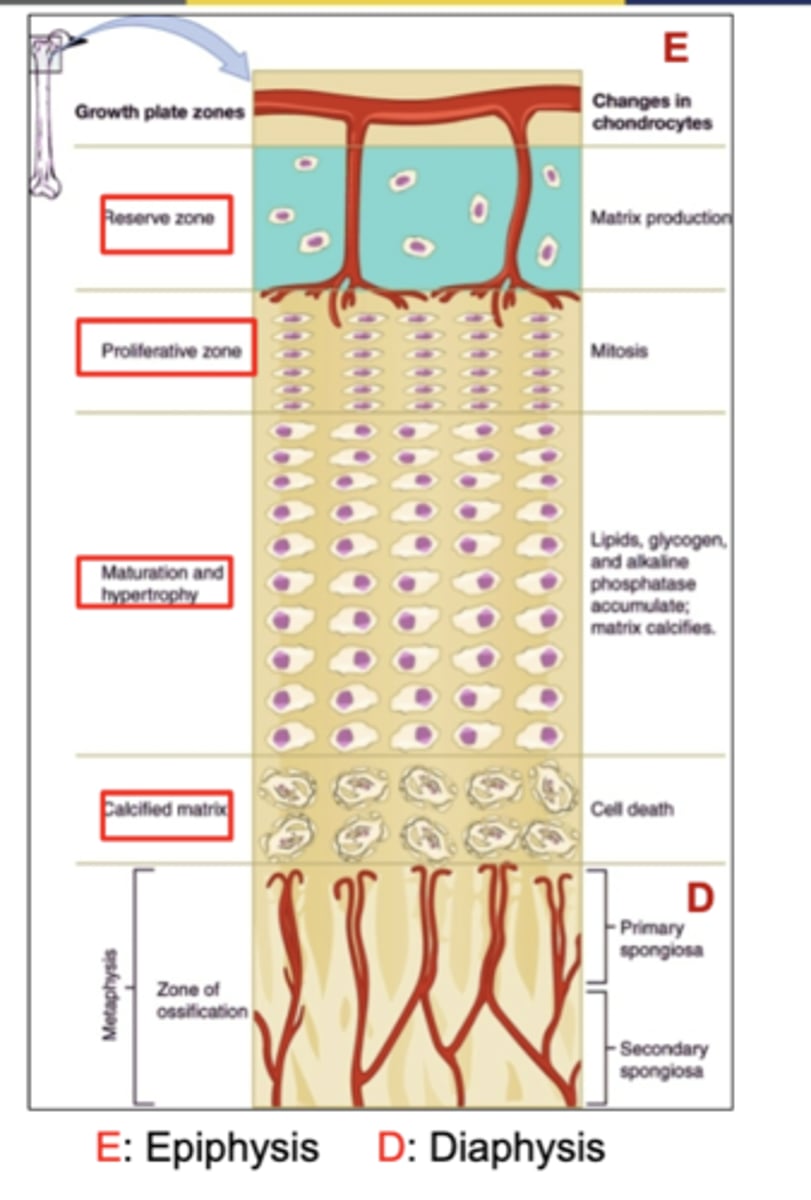
What happens in the "Calcified Matrix" zone?
(a zone of growth for longitudinal bone growth)
(Calcified Matrix- Cell Moves on)
Chondrocytes die, and osteoblasts replace them with bony matrix.
What stimulates epiphyseal plate activity, specifically during infancy and childhood?
Growth hormones
they're the main stimulus for longitudinal bone growth.
What are chondrocytes?
Cartilage cells
located in lacunae.
What is bone remodeling?
the process of resorption (breaking down) of old bone by osteoclasts and deposition of new bone by osteoblasts.
(Our skeleton is replaced about every 10 years)
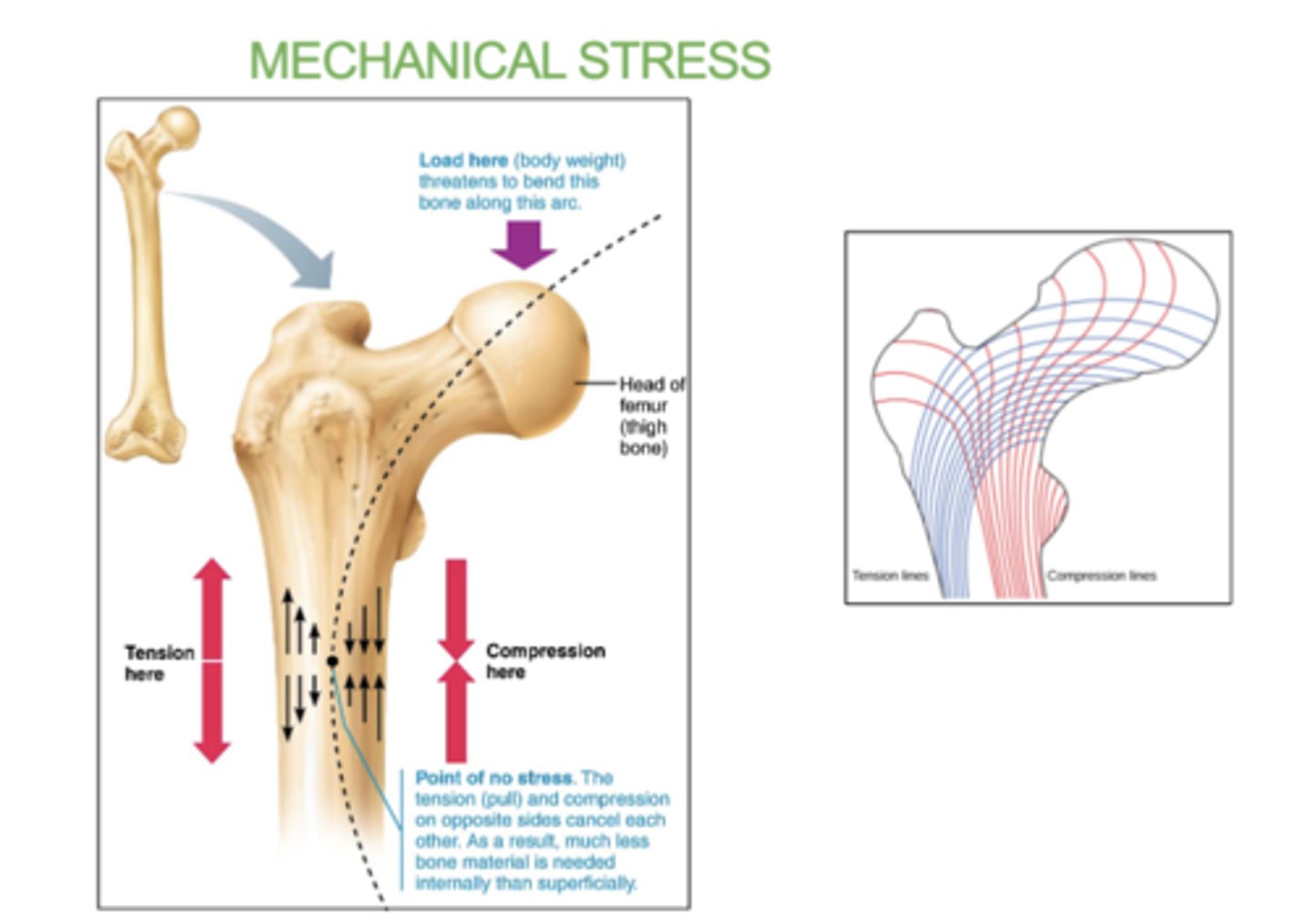
What 4 factors control bone remodeling?
1) Mechanical stress (e.g., weight-bearing exercise)
2) Hormones (e.g., Calcitonin and PTH)
3) Diet (e.g., calcium)
4) Vitamins (e.g., Vitamin D for calcium absorption)
What is mechanical stress in bone remodeling?
When Mechanical stress (from weight-bearing exercise) along bending and stress lines stimulates the bone.
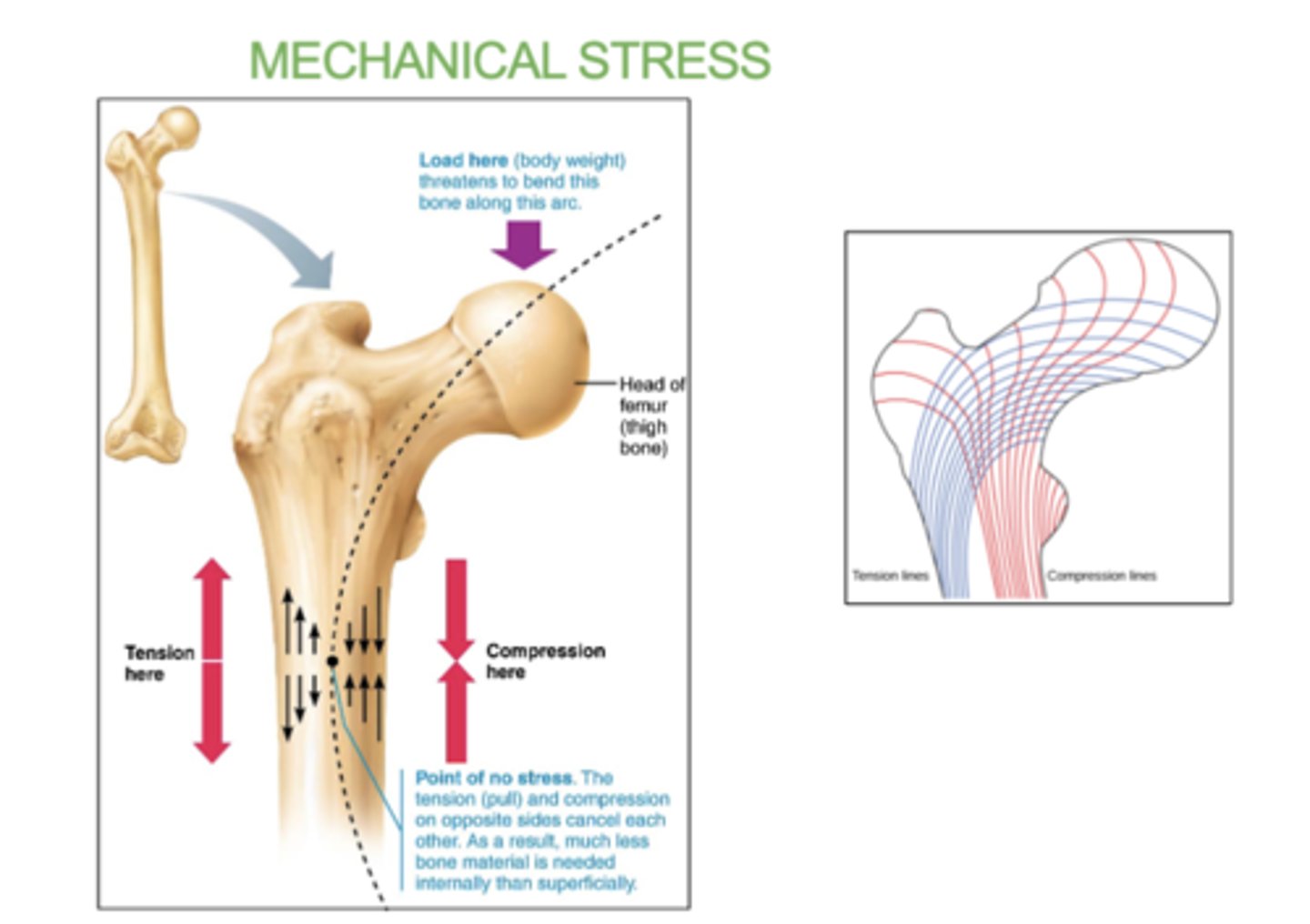
How does mechanical stress affect bone remodeling?
Mechanical stress determines where bone remodeling will occur.
diff between bone stress and mechanical stress?
- Bone Stress refers to strain or pressure placed on bones, which can be positive (stimulating growth) or negative.
-Mechanical Stress refers to the force applied to bones from activities like weight-bearing exercise. generally beneficial because it stimulates bone remodeling and strengthening.
!! these both help prevent osteoporosis.
What is Calcium homeostasis?
the process by which the body maintains a stable level of calcium in the blood and tissues, regulating its release and storage in bones, kidneys, and intestines.

What happens when blood calcium levels are low?
When blood calcium is low, parathyroid hormone (PTH) is released, activating osteoclasts and inhibiting (stopping) osteoblasts.
(this one is bad since it can lower bone density and lead to osteoporosis because Osteoclasts is degrading our own bone matrix)

What happens when blood calcium levels are high?
When blood calcium is high, hormone calcitonin is released, activating osteoblasts and inhibiting (stopping) osteoclasts.

What is osteoporosis?
a condition where decreased bone density can lead to fractures.
why can the release of too much parathyroid hormone (PTH) when calcium levels are low end up being dangerous?
because the constant activation of osteoclasts breaking down the bones can lead to low bone density or OSTEOPOROSIS.
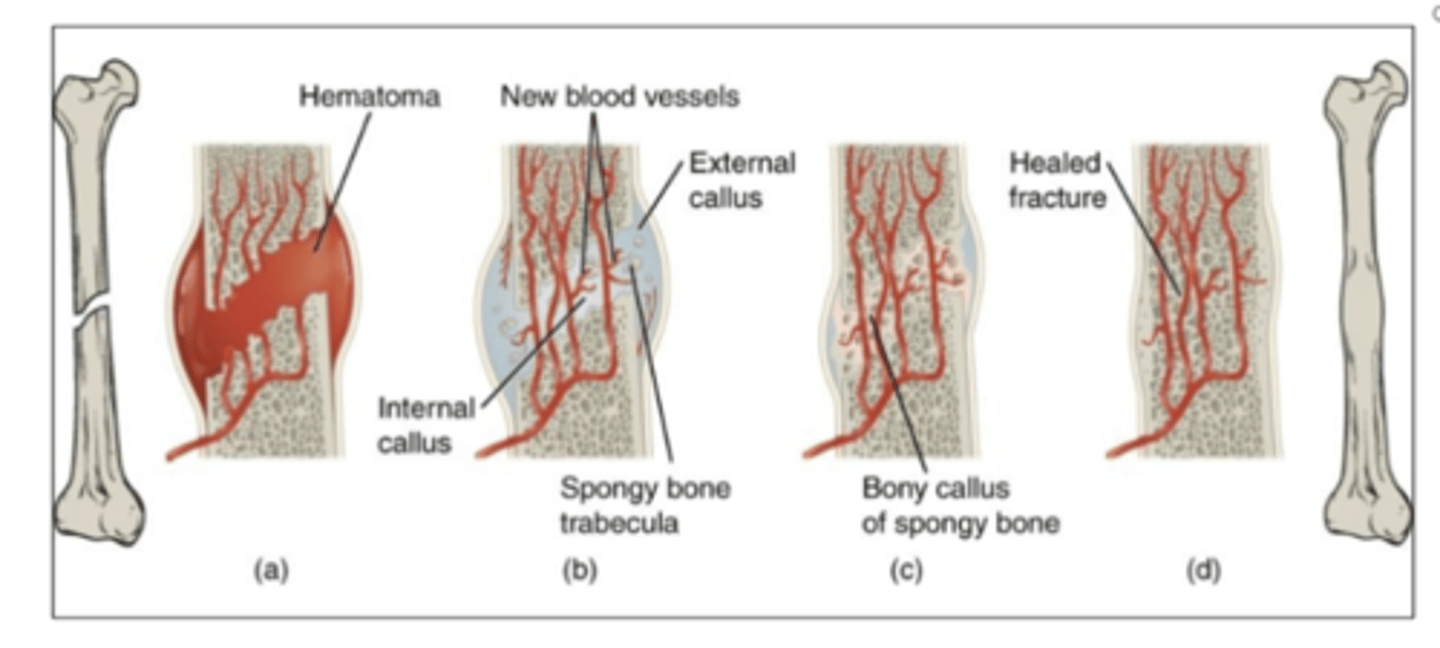
What are the 4 steps in fracture repair?
1. A hematoma forms.
2. Internal and external callus of cartilage forms
3. Cartilage of the callus is replaced by trabecular bone.
4. Remodeling occurs.
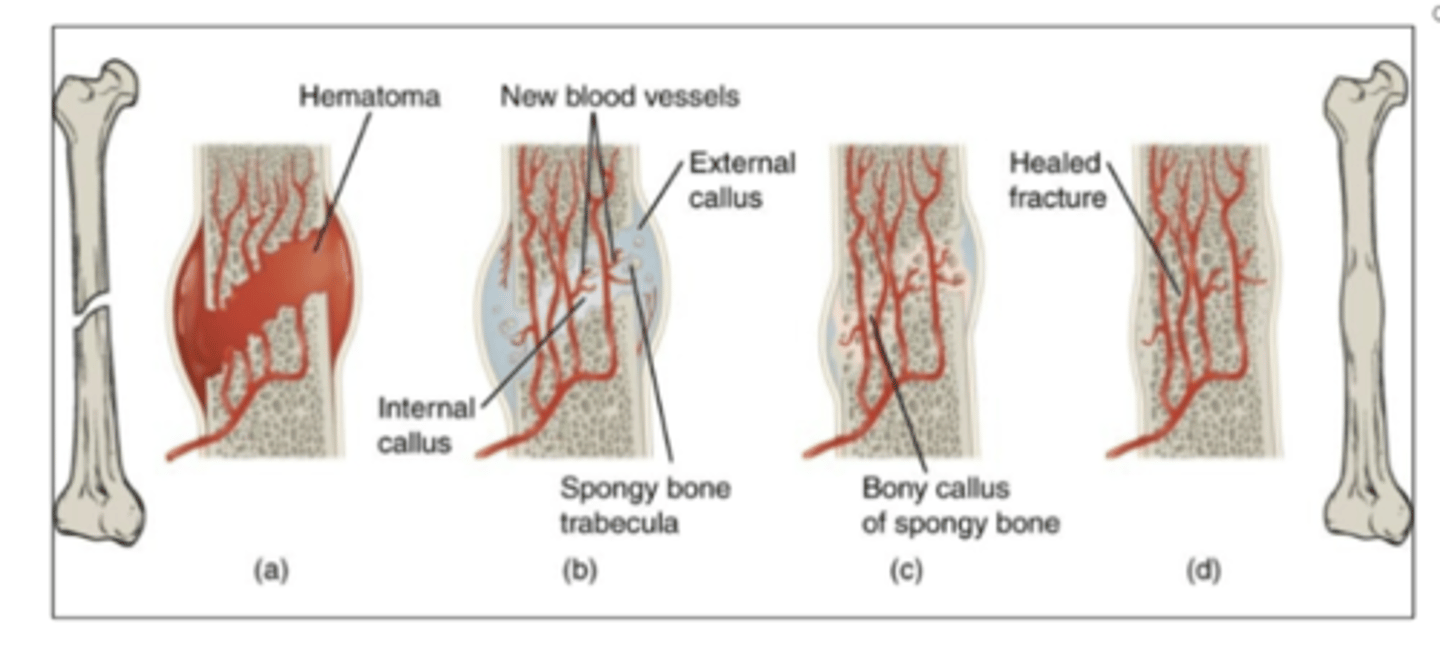
What is the 1st step in a fracture repair?
A hematoma forms.
- a blood clot forms around the fracture to stop the bleeding.
What is the 2nd step in a fracture repair?
Internal and external callus of cartilage forms.
-blood clot gets slowly eaten by macrophages and replaced with cartilage by fibroblasts and chondroblasts.
What does callus mean in fracture repair?
a patch of tissue that first forms to hold everything together.
- soft callus is made of cartilage and forms first to hold the broken bone together.
- hard callus forms when osteoblasts replace the cartilage with new bone, making the fracture stronger.
What is the 3rd step in a fracture repair?
Cartilage of the callus is replaced by trabecular bone
-cartilage gets replaced with spongy bone by osteoblasts
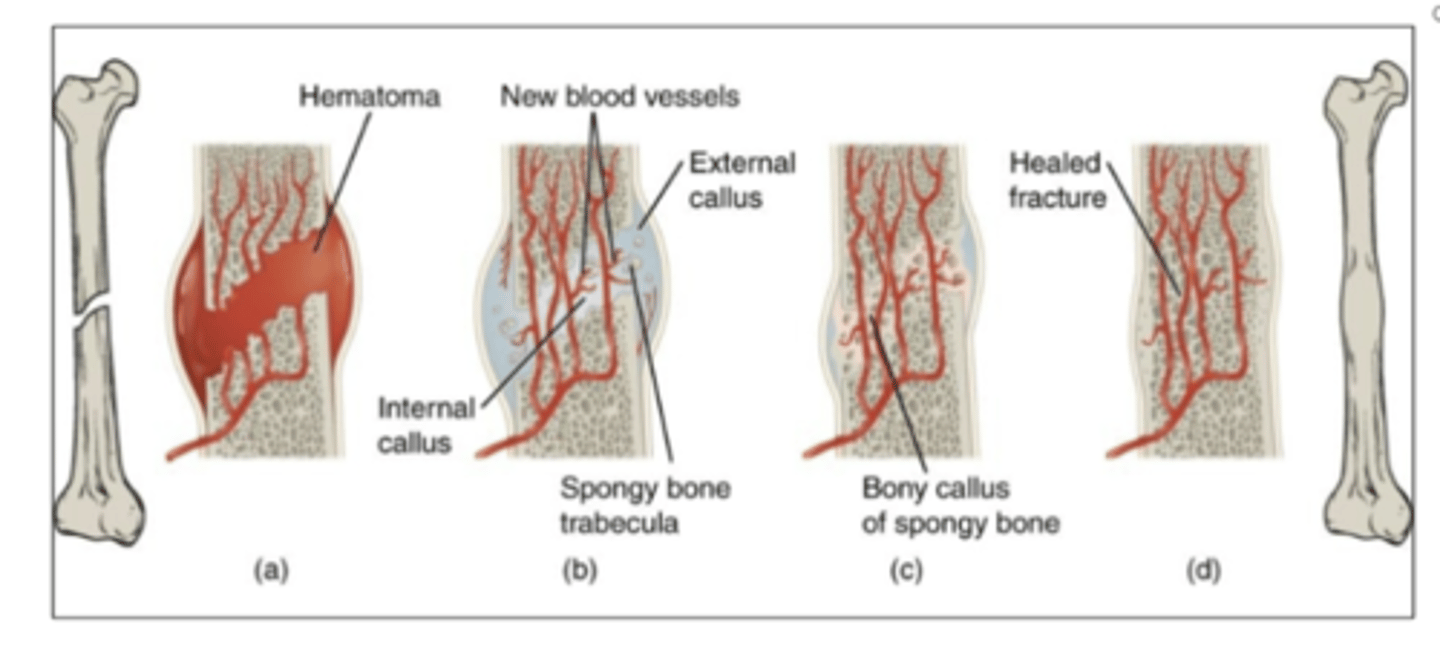
What is the 4th step in a fracture repair?
Remodeling occurs.
-compact bone gets replaced by spongy bone and
Bone has technically healed!!
(takes really long to happen)
what are macrophages?
immune cells that clean up/eat dead cells and debris to create a healthy environment
( Also seen in deep dermis wound healing step 2 )
Bone stress will trigger bone resorption (breaking down) and osteoporosis.
true or false
FALSE
(resorption -> breaking down)
Bone stress (like weight-bearing exercise) actually stimulates bone formation (building) not resorption.
Osteoporosis occurs due to lack of mechanical stress, leading to increased bone resorption (break down) and decreased bone density.
What does bone stress stimulate ?
bone resorption or bone formation?
bone formation.
overtime bones become denser and stronger in response to regular stress, reducing the risk of fractures and osteoporosis. (bone remodeling)