Communication Disorders in Adults Midterm
1/162
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
163 Terms
Neurogenic communication disorder
A problem with communication as a result of damage to the brain or other part of the nervous system
Where do SLPs treat adult disorders?
hospitals
acute care facilities ex: intensive care
rehabilitation facilities
outpatient rehabilitation facilities
skilled nursing facilities
home health care
home and community
Cognition
Ability to process thought
Speech
Sounds the mouth makes to produce words
Language
Words, symbol set used to communicate meaning; usually verbal, written, or signed
Receptive or expressive
Deficits in language
Does not imply deficits in cognition
e.g., A person may be able to think clearly, but not be able to put those thoughts into words
Deficits in cognition
Does not imply deficits in language
e.g., A person may only be able to produce disordered thoughts, but every disordered thought may be perfectly organized into language and produced verbally via speech
Healthy aging
Normal changes that occur with aging, ex: wrinkles, hearing loss; speech and voice remain overall typical
What remains intact for healthy aging?
Orientation
sustained attention
divided attention for basic tasks
long term memory
procedural memory
executive functions for ADLs
processing functional verbal language
overall comprehension
What usually declines for healthy aging?
Slight non-pathological decline:
selective attention
divided attention for complex tasks
short-term memory
working memory
processing of verbal language slows, though remain entirely functional
reading slows, though remains entirely functional
word finding of proper names and confrontational naming
Pathological aging
Changes that occur due to a particular disease or disability
Communication
Fundamental to an older persons’ quality of life to:
express themselves
maintain social connections
function independently
learn new things
adapt to changes
Potential barriers to communication for the elderly
physical isolation
sensory losses
diminished power/influence
retirement, lack of purpose
lack of transportation
health issues
gradual reduction of support systems
Etiology
Underlying medical cause of a symptom of deficit
Etiologies of neurogenic communication disorders
stroke
TBI
tumors
surgical trauma
degenerative disorders
infectious diseases
Idiopathic etiology
Deficits of symptoms that are of an unknown or obscure origin
Damage to the CNS or PNS
Results in communication, cognition, language, and behavior deficits; determined by site and severity
Stroke
Known as a cerebrovascular accident (CVA), occurs when brain tissue is permanently destroyed or temporarily does not function due to decreased or absent blood supply to affected brain tissue
3rd leading cause of death in US
can occur w/in any area of the brain of brain stem
factors that increase likelihood of strokes
tobacco use, physical inactivity, A-Fib, HTN (hypertension), CAD (coronary artery disease)
Anoxia
Complete lack of oxygen to a cell
Hypoxia
Partial, insufficient loss of oxygen to a cell
What are the 2 types of strokes?
Ischemic
Hemorrhagic
Ischemic stroke
Blockage in the arterial system, occurs when a blood vessel in the brain is occluded. 3 types of ischemic strokes:
thrombotic
embolic
transient ischemic attack (TIA)
Ischemic core/infarct
Location of the focal damage to tissue w/in the brain following the stroke
Ischemic penumbra
Area of tissue that, although it has lost the appropriate level of blood supply to function, still receives enough collateral blood flow from other vessels to stay alive
Surrounds the ischemic core
damage to the penumbra can be reversed w/in 2 to 4 hours of medical attention
Thrombotic stroke
An occlusion of blood vessels w/in the brain, usually due to atherosclerosis, occurs when:
a thrombus forms
interrupts flow w/in the brain
Embolic stroke
Occurs when:
embolus lodges w/in a blood vessel inside the brain
A mass traveling through the circulatory system, lodges in a blood vessel in the brain
cuts off blood circulation to a part of the brain
Transient ischemic attack
TIA, or mini-stroke
small ischemia in the brain that resolves itself w/in 24 hours
does not cause permanent deficits unless TIAs are recurring
may be a warning sign of a larger oncoming stroke
Hemorrhagic stroke
Compromised artery resulting in bleeding, occurs when:
a blood vessel w/in the brain ruptures
blood spills into the brain
deprives a part of the brain of blood flow
Typical causes of hemorrhagic stroke
high blood pressure aka hypertension (HTN)
engaging in high periods of physical activity
have a history of hemorrhagic stroke
experience alcohol abuse
onset symptoms:
severe headache
nausea
vomiting
3 mechanisms of damage due to hemorrhagic stroke
blood supply to a portion of the brain has been interrupted due to a burst/broken blood vessel
blood spilling out into the brain tissue where it does not belong causes damage
intracranial pressure increases due to the continued release of blood into the brain or between the surface of the brain and the cranium
Aneurysm
Weakness in the wall of the artery results in abnormal stretching or ballooning out of the wall of a blood vessel, symptoms include:
severe headache
nausea
vomiting
blurred vision
sensitivity to light
seizures
loss of consciousness
Traumatic brain injury
Serious and life-threatening brain damage,
result of an external and forceful event (not due to disease, stroke, seizure, surgery)
common causes: falls, motor vehicle accidents (MVA), violent assault, being struck by an object
immediate impact ranges from mild concussion to coma to death
language + cognitive deficits are varied and complex
depends on what areas of the brain were damaged and to what extent
common in children ages 4 yrs and under to sustain a TBI
Opioid-related brain injury
Anoxic/hypoxic brain injury
severity depends on extent and length of oxygen deprivation
damage is diffuse
toxic brain injury
damage to the brain induced by high levels of toxins in the body
common in opioid abuse and CO2 poisoning
Brain tumors
Neoplasm, abnormal growth of cells in the brain, serves no purpose to the body
the name of brain tumors reflect the types of cells they are composed of primary or secondary tumors
Infection
Can damage CNS and PNS
may be viral, fungal, bacterial, parasitic
examples: encephalitis, HIV/AIDS, Creutzfeldt-Jakob disease (mad cow)
impacts cognition, motor, and language
depends on site, nature, and damage of infection
Seizures
Sudden, often periodic, abnormal levels of electrical discharge occurring in the brain, caused by:
stroke
TBI
tumor
surgical trauma
infections
epilepsy
Nervous system
central nervous system: brain and spinal cord
peripheral nervous system: cranial and spiral nerves
What are the three gross divisions of the brain?
Cerebrum, brainstem, cerebellum
Cerebrum
The major portion of the brain that’s filled with ridges and valleys; houses our consciousness, language, cognition, organizes body movements, and other complex cognitive functions
cerebral cortex
subcortex structures: basal ganglia, limbic system, thalamus
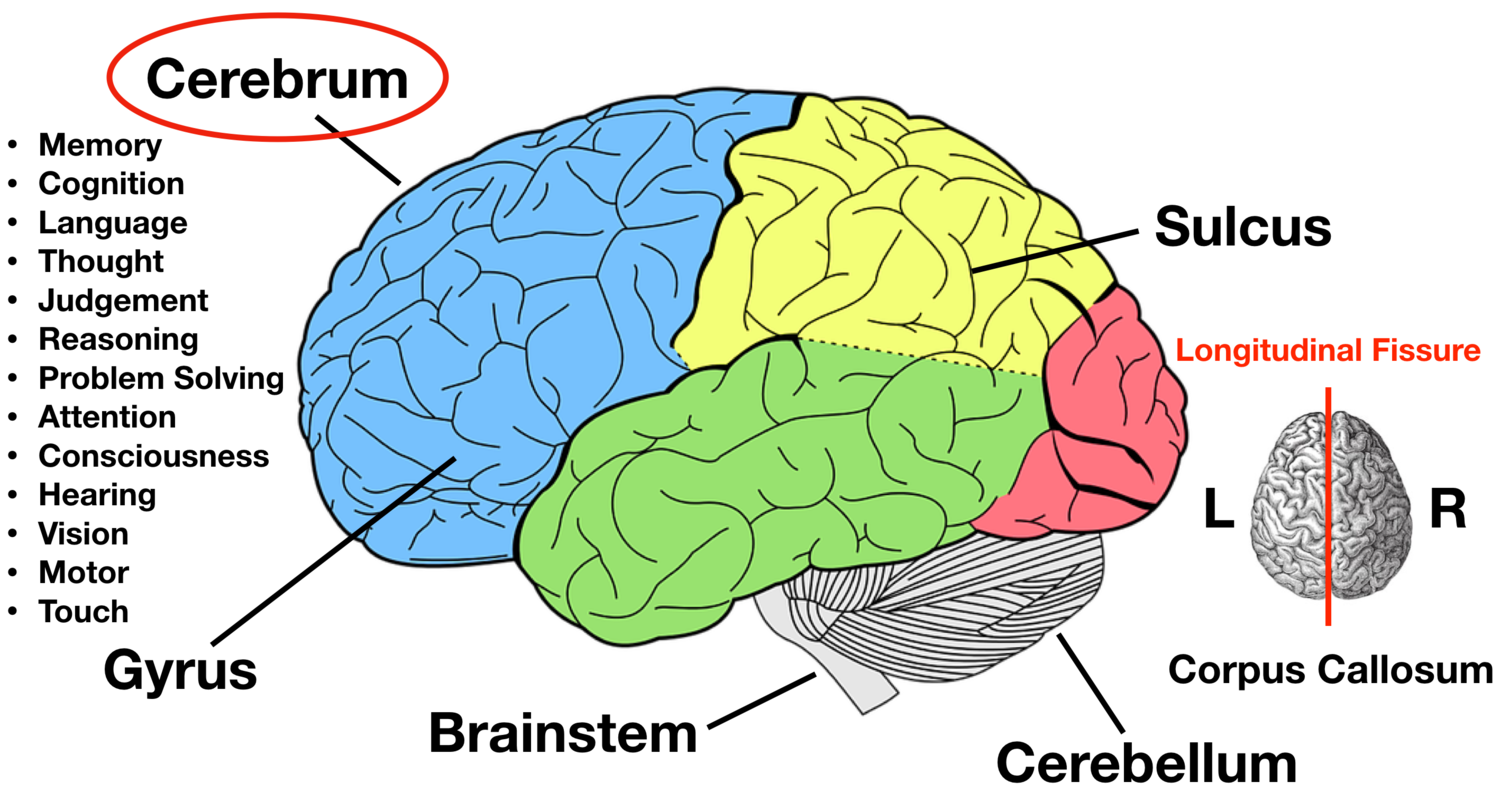
Longitudinal fissure
runs from the front to the back along the brain
divides the brain into left and right halves
Corpus callosum
connects the right and left hemispheres through white matter
located at the base of the cerebral hemispheres
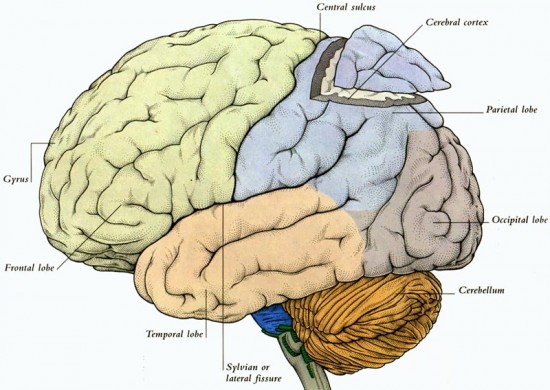
Cerebral cortex
The surface tissue and most superficial layer of the cerebrum made up of gray matter (cell bodies); is divided into 4 lobes
Grooves and bulges in cortex
sulci: small
fissures: large
bulges: gyri
Cerebral lobes
Frontal, parietal, temporal, occipital
Frontal lobe
Anterior aspect of both hemispheres, contains:
primary motor cortex
Broca’s area
prefrontal cortex
Primary motor cortex (motor strip)
posterior gyrus of frontal lobe just anterior to the central sulcus
left primary motor cortex send motor plans to speech muscles
damage near base of motor strip often creates apraxia of speech
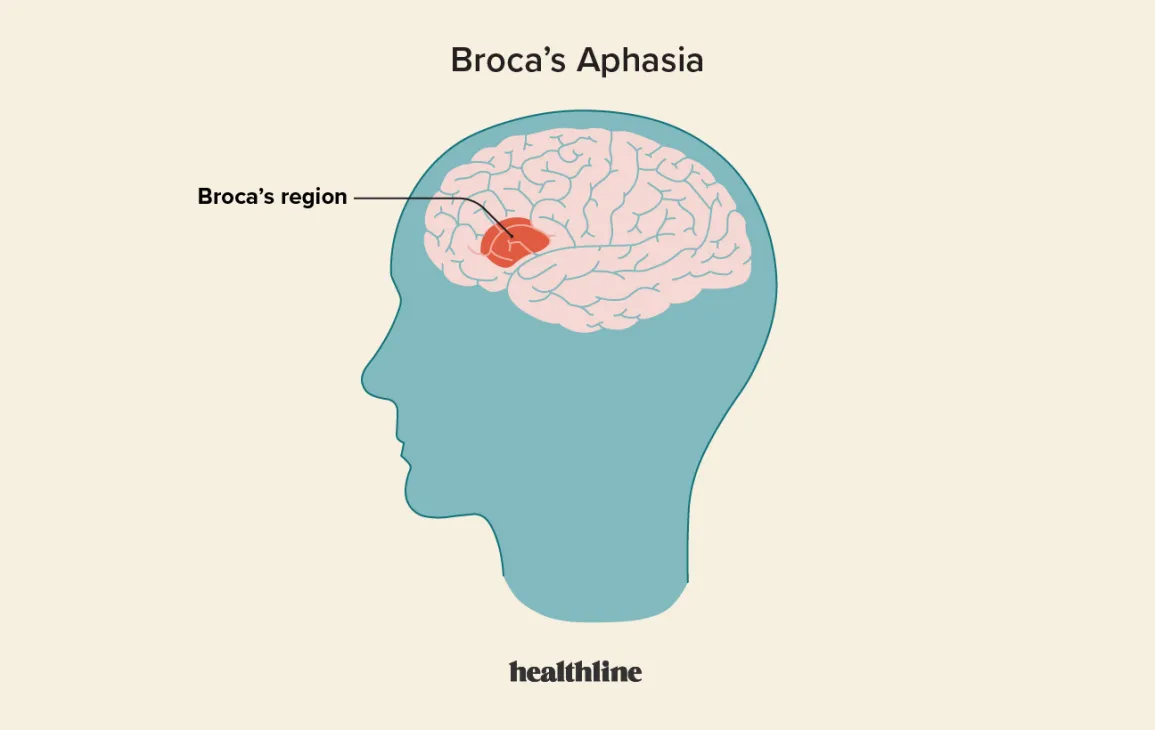
Broca’s area
inferior frontal gyrus
one hemisphere, located in the left frontal lobe
damage results in Broca’s aphasia
expressive language impairment
Pre-frontal cortex
Critical for executive functioning and personality
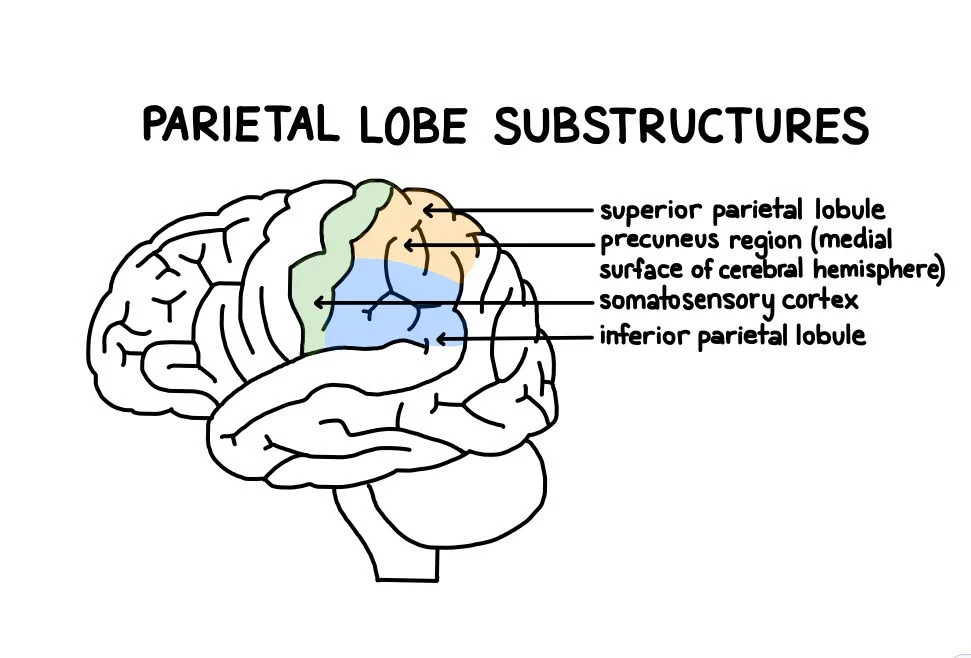
Parietal lobe
Primary sensory cortex (sensory strip)
first gyrus of parietal lobes
receives tactile + proprioceptive (somatic) information
left sensory cortex receives sensory info from the right side of the body
right sensory cortex receives sensory info from left side of the body
Temporal lobe
inferior to lateral sulcus
hearing center
located in upper half of anterior two thirds of temporal lobe
left primary auditory cortex
auditory comprehension of verbal language
right primary auditory cortex
comprehension of environmental sounds and music
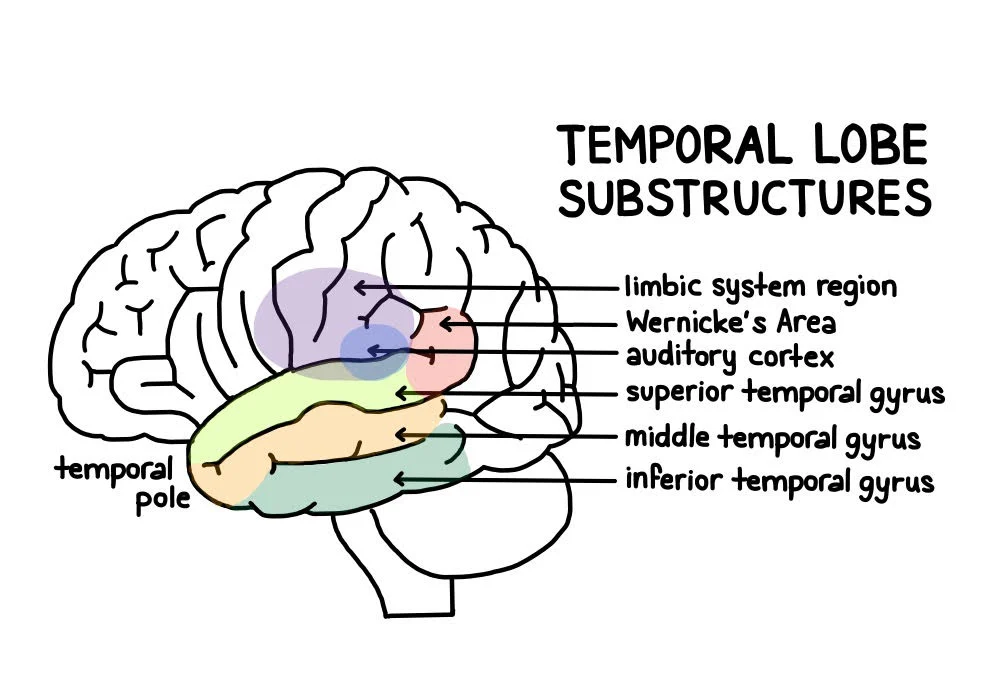
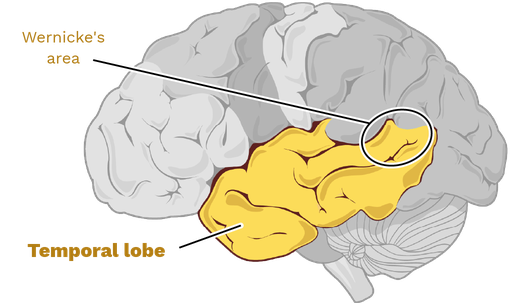
Wernicke’s Area
posterior part of superior temporal lobe
important for attaching meaning to sensory input
damage results in Wernicke’s aphasia
receptive language impairment
Hippocampi (“seahorse”) of limbic system
located in the inferior and medial sections of temporal lobes
moves experiences from short-term memory into long-term memory
needed to learn new information
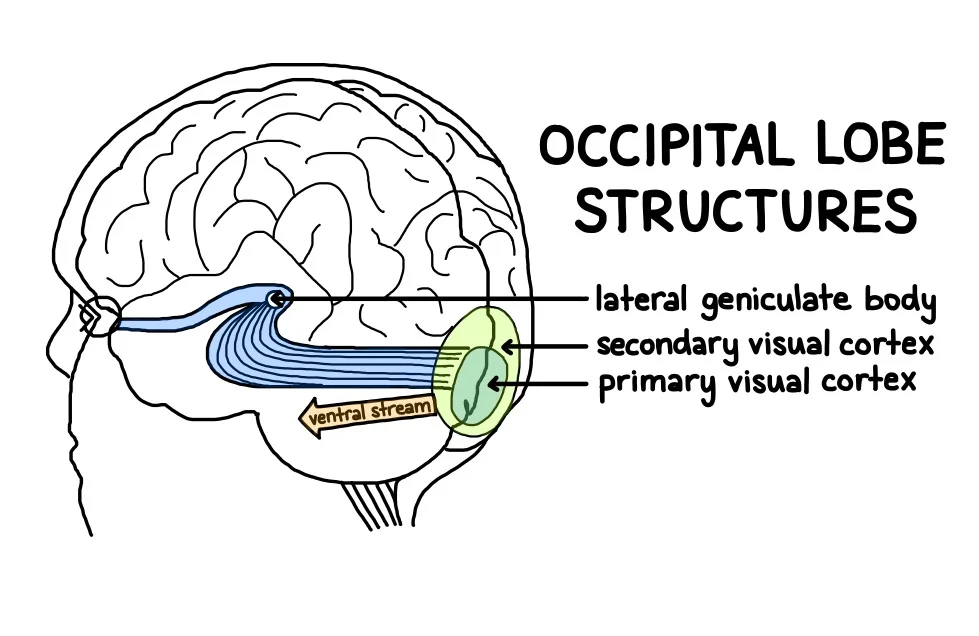
Occipital lobe
The most posterior sections of the cerebrum that are dedicated to receiving and processing neural impulses related to vision
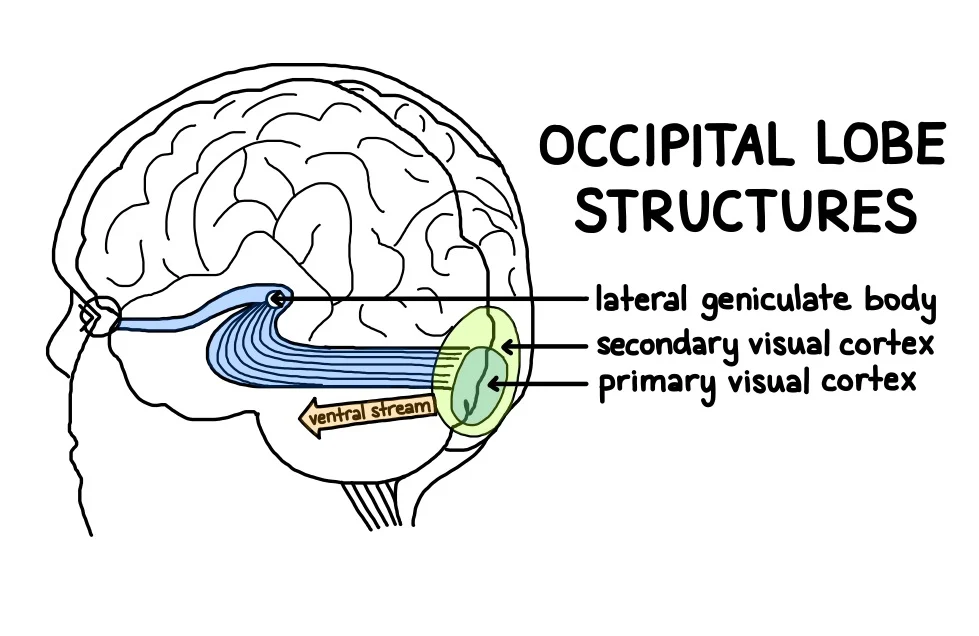
Primary visual cortex
located on the most posterior section of the occipital lobe
receives visual information from the eyes
each visual cortex receives and processes information from the contralateral visual field
transmits visual information anteriorly to visual association (parieto-occipital) area for processing
Subcortex
Responsible for function usually beneath the level of awareness
refines motor plans
regulates heartbeat, breathing, arousal, and sleep/wake cycle
coordinates viscera and digestive system
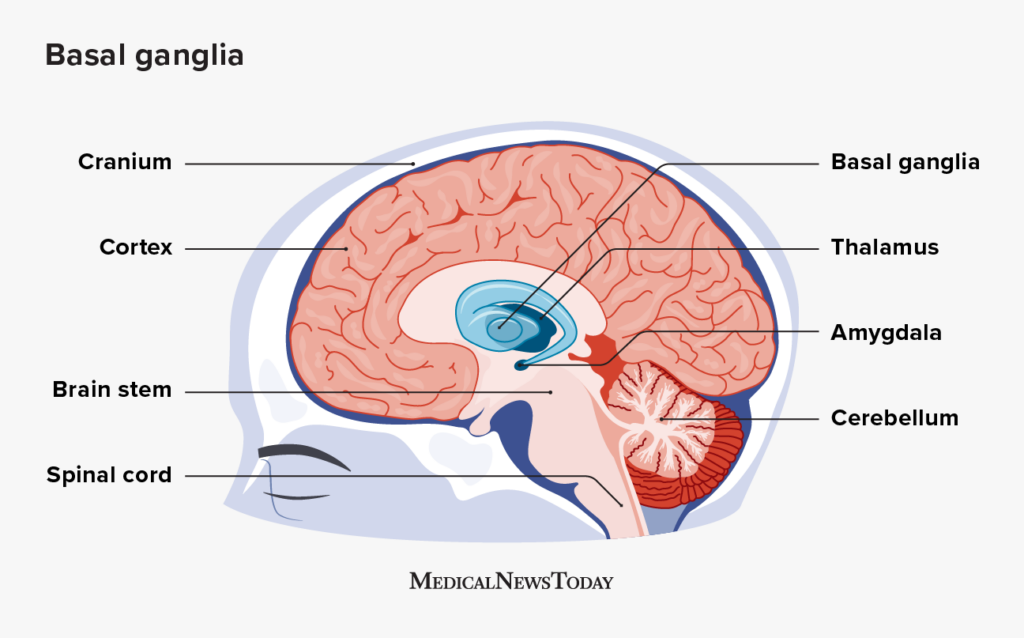
Primary structures of the subcortex
basal ganglia - motor control/inhibition
limbic system - memory + emotional control
thalamus - sensory relay station
cerebellum - fine-tuning motor output
brain stem - home of the CN
Basal ganglia
Group of subcortical structures located within the cerebral hemispheres on either side of the thalamus; plays a role in initiation of movement, muscle tone maintenance, and inhibition of extraneous movements
Includes substructures such as:
caudate nucleus, putamen, globus pallidus
Limbic system
A number of subcortical structures responsible for sense of pleasure, mating, and feeding behaviors, fight-or flight response, emotions, emotional memory, and sense of motivation. Some structures include:
hippocampi
medial temporal lobe
LTM (storage)
amygdala - emotional control center
emotions and memory
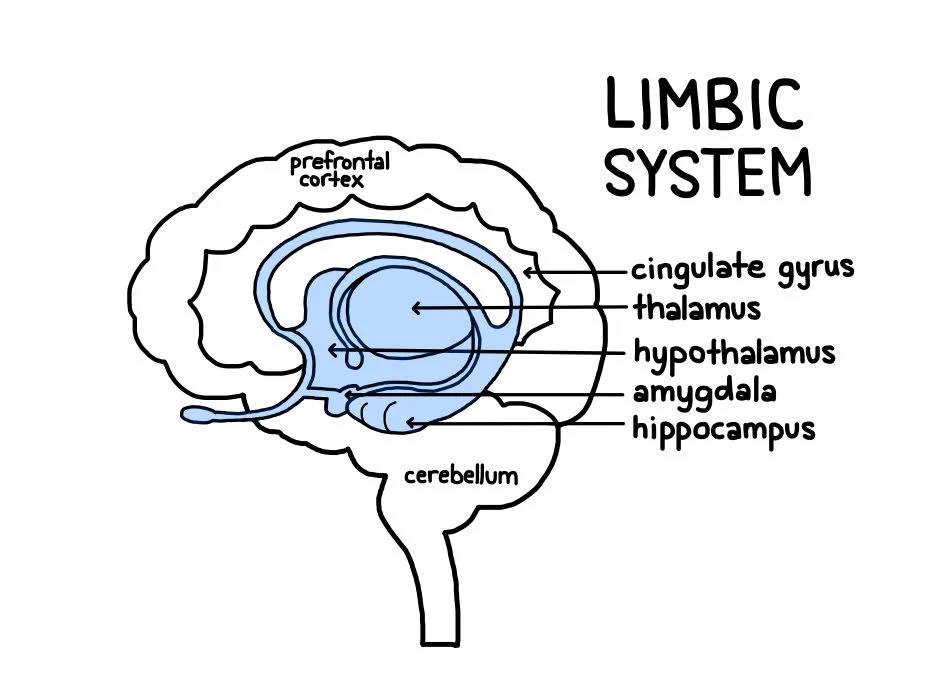
Thalamus
sits on top of the brain stem, under the cerebral hemispheres
functions as a sensory relay station
receives afferent sensory information being transmitted from the body (except olfaction) and directs it to the appropriate part of the brain for processing
receives the motor plans the cerebellum has checked for errors and sends the refined plans for motor execution
Cerebellum
known as “little brain”
Divided into 2 hemispheres
hemispheres connected by the vermis
vermis receives info about the body from projections through the pons
attached to the pons via peduncles
superior, middle, and inferior peduncles
works as an error control device, detect and correct errors in motor plans
makes sure body movements are coordinated and free of errors
monitors the intent of motor plans and compares them to what the body is actually doing
if an error occurs, the cerebellum alters the force, timing, and sequencing of muscle contractions
ataxia
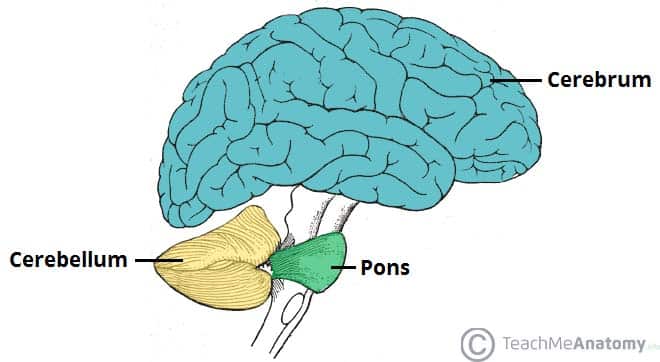
Brainstem
Structure that connects the spinal cord to the brain
What are the 3 main divisions of the brain?
midbrain - houses substantia nigra
pons - attaches cerebellum to the rest of CNS
medulla - many motor fibers decussate here to other side of the body
lesion w/in the CNS above medulla often creates contralateral hemispheres/hemiplegia
lesion along spinal cord below medulla creates ipsilateral hemispheres/hemiplegia
reticular formation
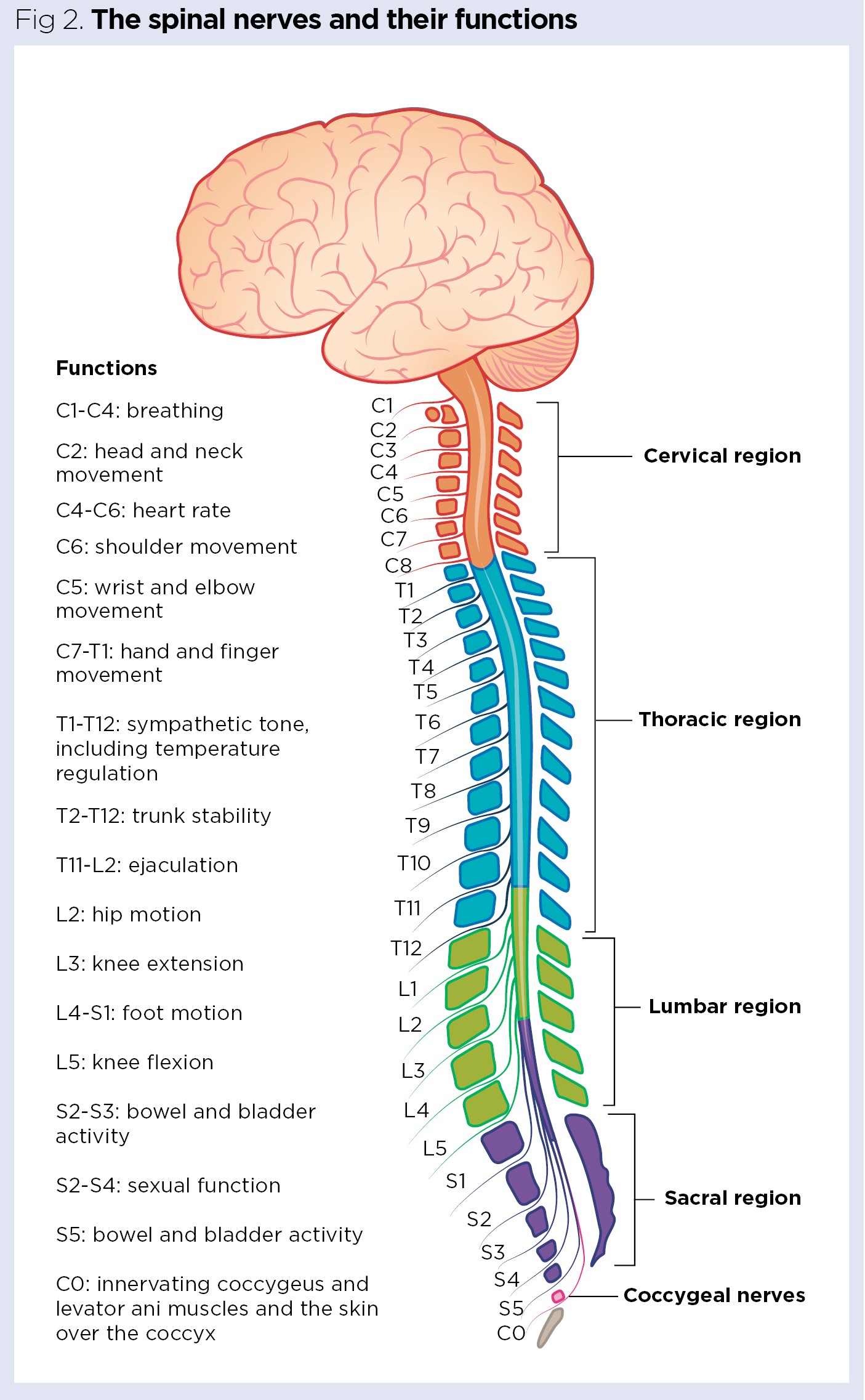
Spinal cord
Bundle of white and gray matter in the spinal column
transmits sensory (afferent) information from the body to the brain and motor (efferent) info from the brain to the body
begins at the medulla
spinal cord breaks up into loose strands of nerves called the cauda equina
White matter
Region of fiber tracts (myelinated axons), tracts that connect parts of nervous system
Gray matter
Cell bodies
Peripheral nervous system
Carries sensory and motor info to and from the body and CNS , spinal and cranial nerves
Spinal nerves
Controls the trunk, arms, and legs of the body, connects the spinal cord to muscles, organs, or glands
31 pairs of spinal nerves originate w/in the gray matter of the spinal cord and course out of vertebral column into soft tissues
no direct role in speech except for phrenic nerve
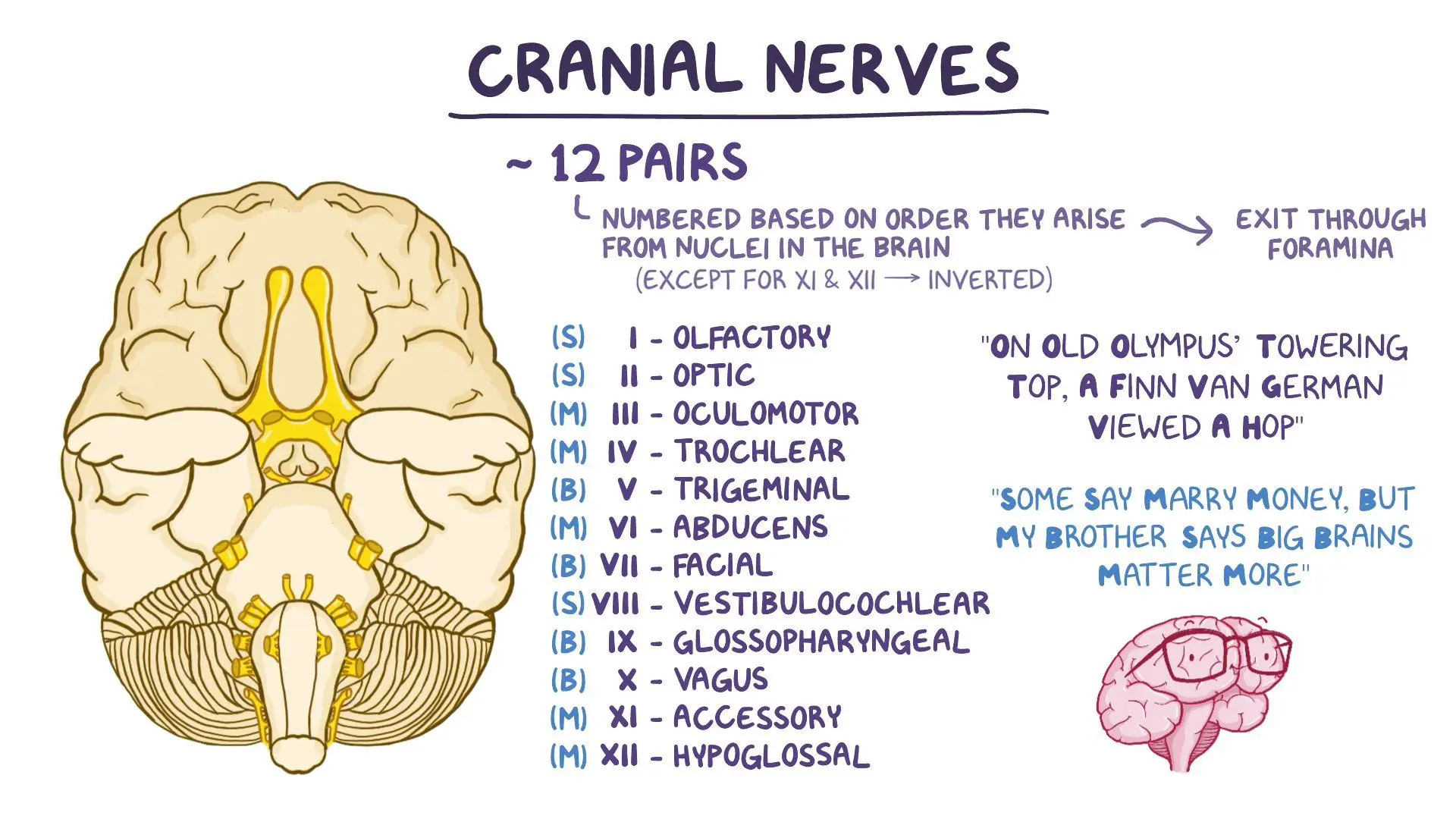
Cranial nerves
Innervates the muscles of the head, face, and neck; connects the muscles and structures of the head, face, and neck to the CNS
12 paired nerves
all either motor, sensory, or mixed motor-sensory
CN I Optic Nerve
Conducts sensory signals from eyes/retina
optic chiasm - the point where the left and right optic nerves come together and medial fibers decussate
optic radiations
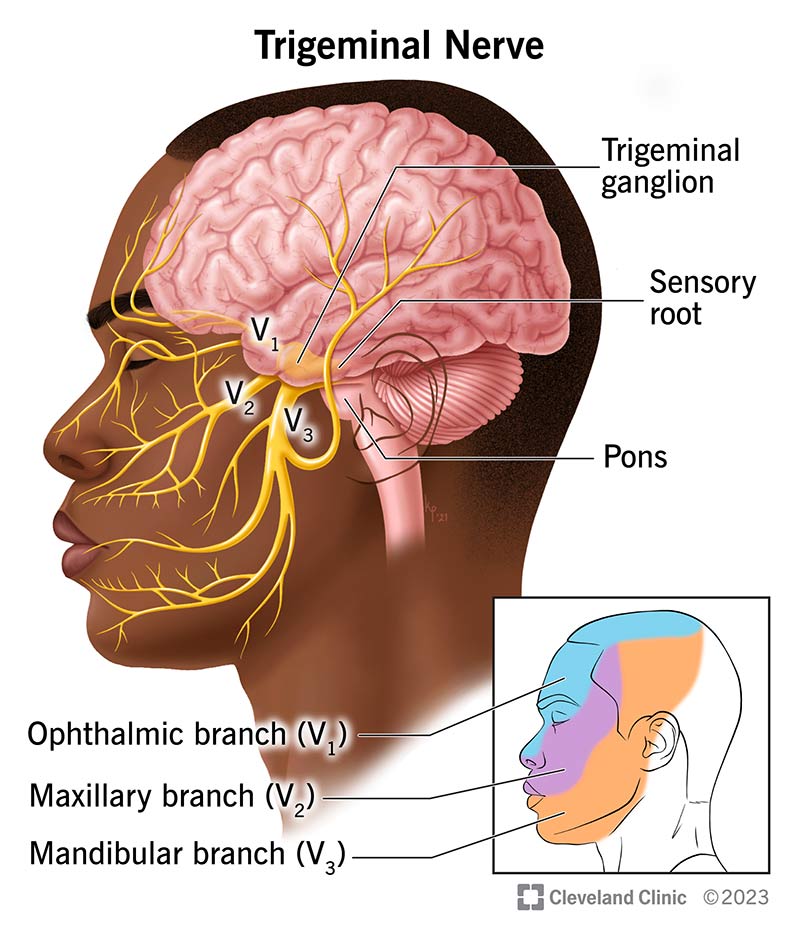
CN V Trigeminal Nerve
Mixed motor-sensory nerve, splits into 3 branches:
ophthalmic: sensory
sensory info from upper face, forehead, scalp to CNS
maxillary: sensory
sensory info from teeth, upper lip, buccal, nasal cavities, sides of face to CNS
mandibular: motor-sensory
sensory info from lower teeth, lower gums, bottom lips, portions of tongue to CNS
motor info to muscles for mastication
CN VII Facial Nerve
Mixed motor-sensory nerve
motor info to the face
sensory (taste) info from anterior 2/3 of tongue
Has four branches
temporal, zygomatic
motor info to muscles of the upper face
bilaterally innervated
buccal, mandibular
motor info to muscles of the lower face
unilaterally innervated
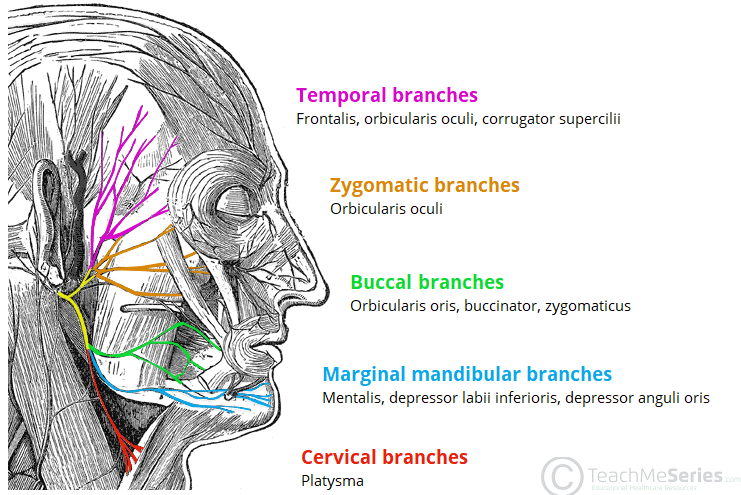
Bilateral innervation
Receives motor plans from both contralateral and ipsilateral hemispheres, protective redundancy allows body part to still function if one cerebral hemisphere is damaged
Unilateral innervation
Receive motor plans from the contralateral hemisphere of motor movement, no protective redundancy
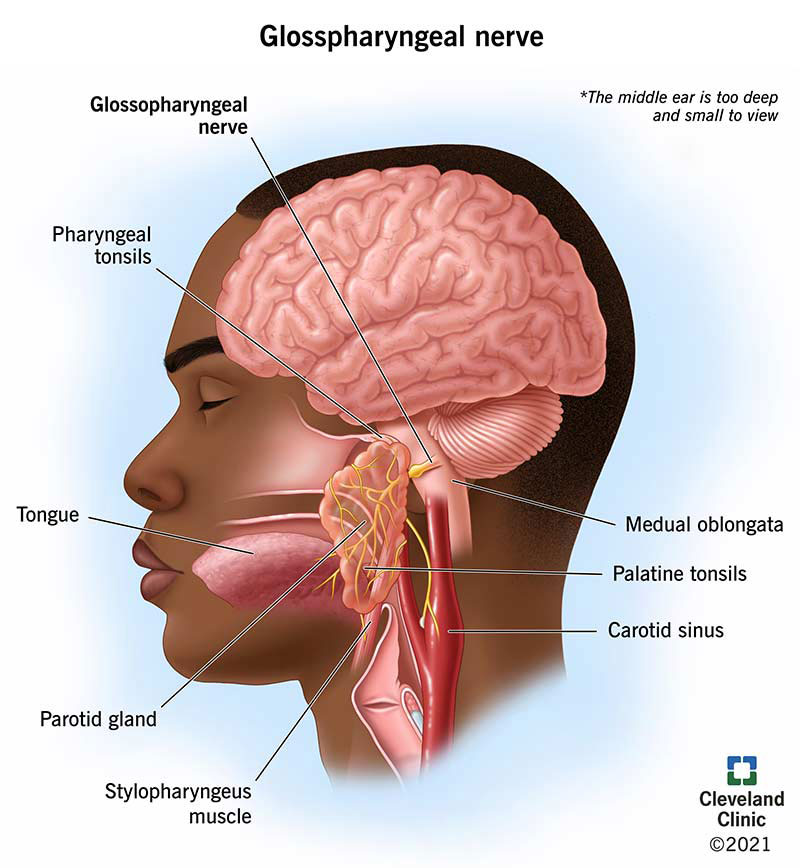
CN IX Glossopharyngeal Nerve
Sensory and motor functions:
sensory (taste) from posterior 1/3 of tongue
motor to muscles of pharynx for swallowing and parotid gland for saliva
CN X Vagus Nerve
Also known as “the wanderer”, both sensory and motor functions:
innervates muscles of the soft palate, pharynx, and larynx through various branches
important for speech/voice
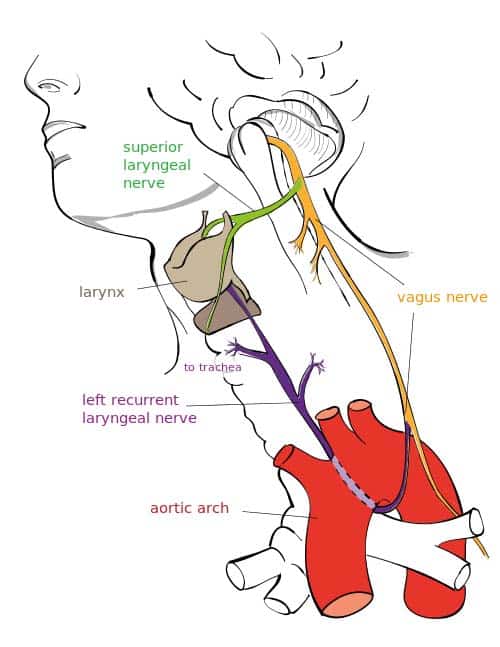
Pharyngeal branch
Innervates portions of pharynx for swallowing and elevates velum for non-nasal sounds
Superior laryngeal nerve (SNL)
intrinsic branch - sends afferent info from inside larynx to CNS
extrinsic branch - innervates cricothyroid muscle
Recurrent laryngeal nerve (RLN)
right RLN = passes under right subclavian artery
left RLN = passes under arch of aorta
both recur into neck/larynx and innervate muscles for adduction and abduction of vocal cords
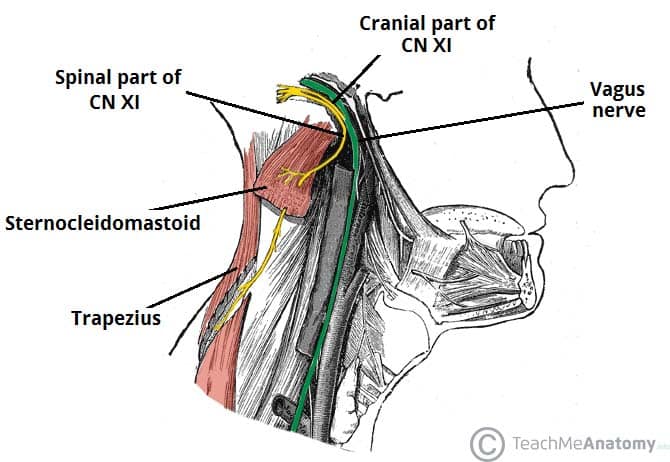
CN XI Accessory Nerve
Only motor function:
cranial component works as an accessory of the vagus nerve
spinal component innervates muscles of the neck/shoulders
sternocleidomastoid - bilateral innervation cerebral cortex
trapezius - unilateral innervation
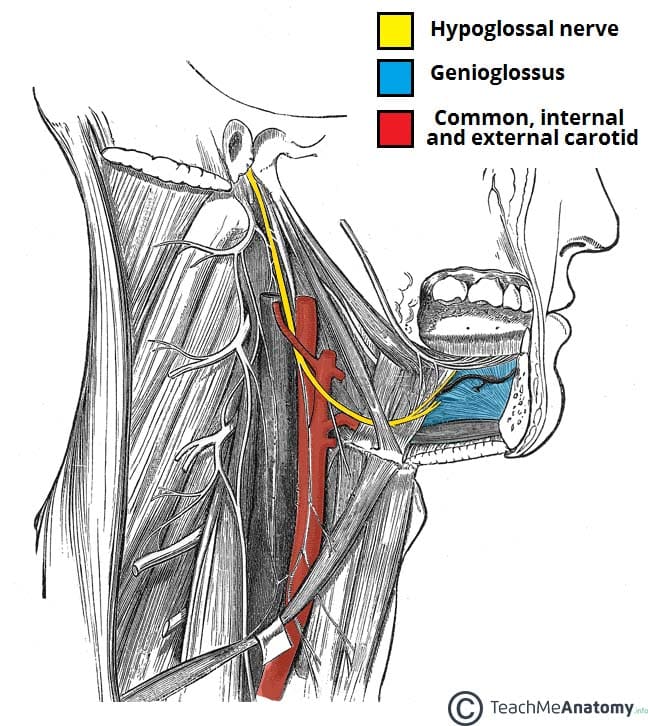
CN XII Hypoglossal Nerve
Motor functions
innervates all intrinsic muscles of the tongue
fine motor movements of tongue
innervates most extrinsic muscles of the tongue
gross motor movements of tongue
Ataxia
Manifests as poorly controlled and poorly coordinated movement that is lacking in smoothness; complex movements are often disintegrated and broken down and executed in their component parts
Cerebral hemispheres
Each hemisphere is responsible for different cognitive and motor functions
Vascular System
Made up of the vessels that carry blood and lymph fluid through the body:
Aorta - Common carotid artery
internal carotid - majority of blood goes to the brain
anterior cerebral artery
middle cerebral artery
external carotid
Vertebral artery
posterior cerebral artery
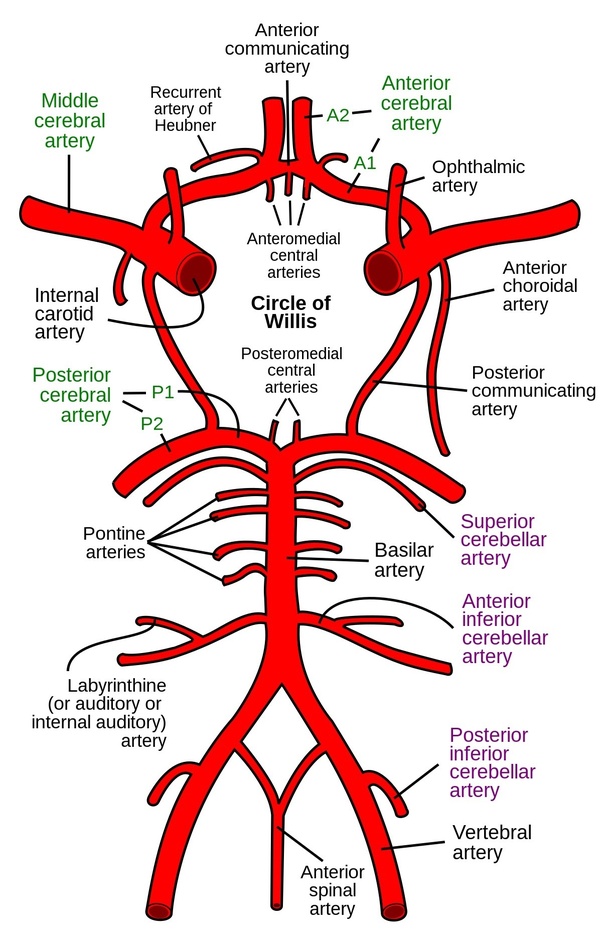
Deficits associated with ACA lesions
Paralysis
contralateral hemiplegia of leg only
cognitive + emotional changes
apraxia of gait
incontinence of bowl + bladder
Deficits associated with MCA lesions
contralateral hemiplegia
hemianopsia
visual field cut
aphasia
apraxia
upper motor dysarthria
Deficits associated with PCA lesions
hemianopsia
visual agnosia
difficulty with labeling or identifying objects
Deficits associated with Vertebrobasilar system
Brainstem blood supply
Dysarthria
Dysphagia
Locked in syndrome (LIS)
Arousal difficulties
Cerebellar blood supply
Ataxic dysarthria
Wernicke’s aphasia
Good speakers, poor communicators
Damage to this area and surrounding:
occlusion of inferior/posterior branches of MCA to posterior 1/3 of superior gyrus of temporal lobe
Characteristics:
Poor comprehension
Neologisms (jargon)
Semantic + phonemic paraphasias
Logorrhea
Empty speech
Loss of pragmatic skills
Minimal motor involvement of extremities
Transcortical sensory aphasia
Transcortical sensory: L Parietal watershed
Occlusion to anterior area between MCA and posterior cerebral artery (PCA) posterior to Wernicke’s area at the temporo-occipital-parietal area
Characteristics:
Poor auditory comprehension
Relatively intact reception
Fluent speech with semantic paraphasias
Visual deficits
Conduction aphasia
Conduction: L supramarginal gyrus + atcuate fasciculus
Supramarginal gyrus of parietal lobe, posterior to sensory cortex and above Wernicke’s area damaging arcuate fasciculus leaving Broca’s and Wernicke’s genrally okay
Characteristics:
Fluent speech
Intact auditory comprehension
Repetition inordinately impaired relative to other deficits
Phonemic paraphasias
Anomia
Aware of errors
Self repair/correction attempts
Anomic aphasia
Damage anywhere w/in the language areas
L angular gyrus
Characteristics:
Fluent speech
Intact receptive language
Disproportionately severe anomia
Crossed aphasia
Lesion to a right hemisphere that creates aphasia, the consequent contralateral hemiparesis/hemiplegia leaves R hand (usually dominant writing hand) motorically intact
Assessment of aphasia
Case history - demographic info, medical chart
Assess/observe communication and speech - observe residual language, compensatory strategies, connected speech
Administer standardized test - ex: BDAE, WAB-R
Cognitive evaluation - cognition, language, and communication are intertwined,
Some level of cognitive deficits almost universally present in those with aphasia
Attention, working memory, STM
4 primary modalities of language
Auditory comprehension
Verbal expression
Visual comprehension (reading)
Written expression (writing)
and possibly non-verbal communication
Aphasia therapy
Spontaneous recovery is up to 6 months post-onset
therapy during aphasia will facilitate spontaneous recovery
3 categories of therapy approaches:
restorative, compensatory, social
Restorative approach
Based on neuroplasticity
ability of the brain to change itself to take on new functions and to compensate for damage to another part of the brain
Melodic Intonation therapy - uses intact melodic/prosodic processing of the right hemisphere to cue word retrieval in the left hemisphere
Constraint-induced therapy - combats learned non-use
Errorless learning - avoid the practicing of errors
Compensatory strategies
Strategies that focus on helping a patient function despite their deficits
AAC
low tech - gestures, draw, point to pictures on a communication board
high tech - programmable voice generating computers such as Lingraphica, apps for iPhones, iPads
Social approaches
Communication partner training
targets changing the behavior of those in the environment of individuals with aphasia to facilitate the communication of those with aphasia
Group therapy
increases hope, psycho-social emotional support, pragmatic skills, and confidence as speaker
may also focus on goals unaddressed by individual therapy
Aphasias
multimodality deficit in communication, affecting language-based modalities
acquired neurologic impairment of language
NOT a disorder of development
NOT due to sensory or motor disorder
Can a child have aphasia? Yes, through brain tumors, TBI, stroke, etc.
Expressive language deficit
Difficulty in formulation or production of verbal, written, or gestural language
Due to lesions at or near Broca’s area
lesions anywhere w/in anterior portion of left cerebral hemisphere may cause expressive deficits