Circulatory and Respiratory Systems Test - Yr 11 ATAR
1/68
Earn XP
Description and Tags
Chapter 4 and 5 for Human Biology
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
69 Terms
Why do humans have a double circulatory system
. right side of heart pumps deoxygenated blood to lungs for oxygenation = pulmonary circulation
. left side of heart pumps oxygenated blood to rest of body (is thicker) = systemic circulation
Describe the hearts chambers
. heart has 4 chambers
. 2 thin walled atria on top: receive blood
. 2 thick walled ventricles underneath: pump blood
—> veins carry blood into atria + arteries carry blood away from ventricles
Describe the locations of valves in the heart
. between the atria + ventricles are atrio-ventricular valves: prevent back flow of blood from ventricles to atria
Left AV valve has 2 flaps = bicuspid/mitral valve
Right AV valve has 3 flaps = tricuspid valve
Also are 2 semi-lunar valves in arteries
Pulmonary valve
Aortic valve
What are the left and right halves of heart separated by?
. the septum
Which ventricle has thinner walls and why?
. walls of right ventricle are 3x thinner than left
—> it produces less force and pressure in the blood as the blood has less distance to travel (lungs only)
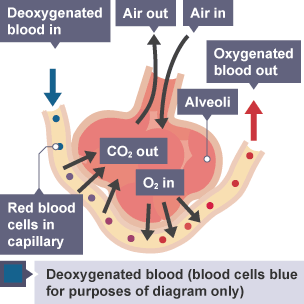
Draw the process of gaseous exchange
. the absorption of oxygen from the air in exchange for CO2 removed from the body, taking place in alveoli of lungs
Process:
Gases move from an area of high pressure to an area of low pressure in diffusion
Oxygen is inhaled and taken to alveoli
Oxygen moves from alveoli into the capillaries + blood
CO2 moves from capillaries in blood into alveoli + exhaled
Blood is now oxygenated + will be transported to rest of the body
What happens when the heart’s cardiac muscle contracts?
. the volume in the chamber decreases, so the pressure in chamber increases, forcing blood out
What type of muscle is the heart?
. cardiac muscle
—> myogenic (contracts on its own without needing nerve impulses)
—> made of myocytes
Stage 1 of Cardiac Cycle: Atrial Systole
Stage 2 of Cardiac Cycle: Ventricular Systole
Stage 3 of Cardiac Cycle: Diastole
What is the lub dub sound of the heart caused by?
lub: the atrioventricular valves closing during ventricular contraction
dub: the semilunar valves closing as the ventricles relax.
Explain how the heart is a double pump
1st: blood is pumped to lungs + returns to heart (via right side)
2nd: blood is pumped to respiring muscles + back to heart (via left side)
—> 1. Deoxygenated blood is pumped from heart to lungs (right side)
—> 2. Blood receives oxygen + pumped back to heart
—> 3. Oxygenated blood then pumped to rest of body (left side)
—> 4. Oxygen leaves blood to be used for respiration in body + blood goes back to heart
Cardiac output
. the amount of blood flowing in a given time
Heart rate x stroke volume = cardiac output
What are the benefits of increased cardiac output during exercise (5) ?
oxygen to muscles faster
glucose to muscles faster
CO2 away from muscles faster
Lactate away from muscles faster
Heat away from muscles faster
Difference between systemic and pulmonary arteries and veins?
Systemic arteries: carry oxygenated blood to rest of body
Systemic veins: carry deoxygenated blood to heart from body
Pulmonary arteries: carry deoxygenated blood to lungs
Pulmonary veins: carry oxygenated blood to heart from lungs
Veins and venules description
function: to carry blood from tissues to heart
—> thin walls since blood at low pressure
—> large lumen to reduce resistance to flow
—> many valves to prevent backflow
—> blood at low pressure: BP naturally decreases as moves from arteries (close to heart) towards veins (further), due to the resistance blood encounters as it flows through the blood vessels
—> blood usually deoxygenated (except pulmonary vein)
Arteries and Arterioles description
function: to carry blood from heart to tissues
—> thick walls with smooth elastic layers to resist high pressure + muscle layer to aid pumping
—> small lumen
—> no valves (except in heart)
—> blood at high pressure: directly connected to heart + force of heart’s pumping action creates high pressure helping blood reach all parts of body
—> blood usually oxygenated (except in pulmonary artery)
Capillaries description
function: to allow exchange of materials between blood + tissues
—> very thin (1 cell thick), permeable walls to allow exchange of materials
—> very small lumen (blood cells distort to pass)
—> no valves
—> BP falls: due to large total cross-sectional area, increased resistance to blood flow caused by small diameter, low velocity of blood flow allowing for efficient exchange of nutrients + waste products
—> blood changes from oxygenated to deoxygenated (except in lungs)
How are ABO blood groups distinguished
. the difference is due to the presence of antigens on the plasma membranes of RBCs + the presence or absence of antibodies in plasma
What happens if someone receives incompatible blood?
. donor antigens react with antibodies in patient’s plasma and an immune response called agglutination can occur
What is agglutination?
. clumping together of RBCs due to the interaction between antigens + antibodies
What is the ABO blood group system?
. a method of classifying blood types according to the antigens on the surface of the RBCs
—> 4 types: A,B,AB,O
—> 2 sugar antigens involved: antigen A and antigen B
How is your ABO blood group determined?
. by your DNA and is thus inherited
. on surface of the RBCs a person may have either antigen A, antigen B, both antigens (AB) or neither antigen (O)
ABO blood compatibilities
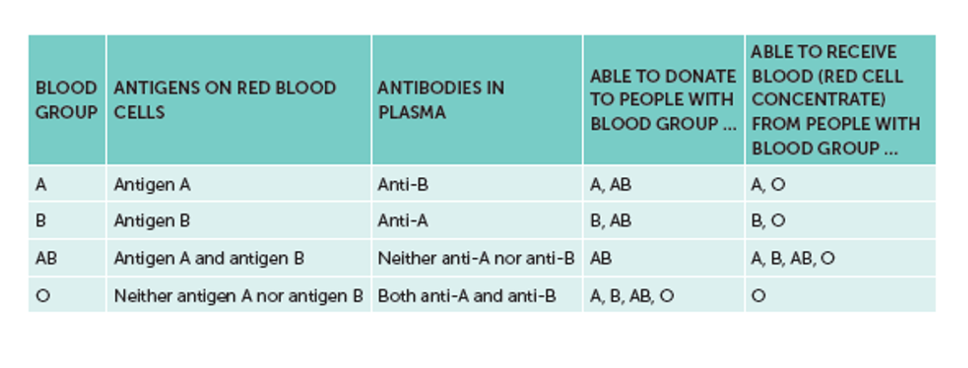
Blood group typing table
The Rhesus factor transfusions table
Lymphatic system’s role in defence
. larger particles (bacteria) are trapped in the meshwork of fibres
—> large phagocytic cells (macrophages) destroy these particles in phagocytosis
. when infection occurs, formation of lymphocytes increases, causing the lymph nodes to become swollen + sore (part of immune response)
3 Functions of lymphatic system
collects + returns excess tissue fluid that has escaped the blood in circulatory system, back to circulation
filter lymph fluid containing pathogens + cell debris and destroy it
Activate the immune system
Difference between lymphatic system and circulatory system
. lymphatic has no RBCs, does not circulate and has no pump
Structure:
—> circulatory:
. blood flows in closed continuous circuit, meaning blood flows continuously within the vessels without leaving the system
. blood is pumped by heart
. consists of heart, blood vessels (arteries, veins, capillaries) and blood
—> lymphatic:
. lymph flows in open circuit from tissues to lymphatic vessels, starting in the tissues and ending in bloodstream, where lymph is returned to circulatory system
. lymph not pumped + flows passively due to muscular contractions
. made up of lymphatic vessels, lymph nodes, and lymph
Function:
—> circulatory:
. distributing O2 nutrients to cells of body
. no immune function
. maintains blood pressure and is directly involved in gas exchange in the lungs
—> lymphatic:
. collecting and removing waste products or excess tissue fluid + absorb fats and fat-soluble vitamins from digestive system
. has an immune response
. maintain fluid balance by returning excess tissue fluid to bloodstream
Breathing (ventilation)
. the process of moving air into and out of the lungs
. purpose is to exchange oxygen + carbon dioxide between lungs and air
Respiration
. the transport of oxygen from the air to the tissues and the transport of CO2 in the opposite direction
External respiration
. the movement of O2 and CO2 between the lungs and bloodstream
Internal Respiration
. the exchange of O2 and CO2 between blood and tissues
How is oxygen transported
. oxygen combines with haemoglobin in RBCs to form oxyhaemoglobin
How is carbon dioxide transported
. most CO2 is transported in the plasma as dissolved bicarbonate ions
The Process of Inspiration
. Breathing in
External intercostal muscles contract, pulling ribs up and out
Diaphragm contracts + flattens downwards
volume of thorax increased
Volume of lungs + alveoli increased
Decreases pressure of air in alveoli (below atmospheric)
Air flows in to lungs to equalise pressure
The process of normal expiration
. Breathing out
External intercostal muscles relax, allowing ribs to fall
Diaphragm relaxes + curves upwards (elasticity returns)
Volume of thorax decreased
Volume of lungs + alveoli decreased
Increases pressure of air in alveoli (above atmospheric)
Air flows out of lungs to equalise pressure
Describe forced expiration
Internal intercostal muscles contract, pulling ribs downward
the abdominal muscles contract, pushing diaphragm upwards
—> gives a larger + faster expiration, used in exercise
Describe what asthma is
. allergic condition that causes difficulty breathing due to a narrowing of the airways
What does asthma occur due to
. smooth muscles contracting, narrowing the airway
. inflammation causing the lining of the airways to thicken, narrowing its diameter
. mucus filling the airway, narrowing the tube
Triggers of asthma
allergic response to allergen
a non-allergic response
. air pollutants, exercise, cold air, infection, anxiety, stress, smoke, some medication
Asthma effect on respiratory system
. much greater resistance to air flow in and out of alveoli, making it difficult to ventilate lungs
—> hard to maintain a diffusion gradient as a result of reduced flow
Symptoms of asthma
difficulty in breathing: due to constriction + inflammation
wheezing sounds: due to air passing through very constricted passages
Tight feeling in chest: a consequence of not being able to ventilate the lungs because of constriction in bronchi + bronchioles
Coughing: a reflex action to obstructed bronchi + bronchioles
What is emphysema
. progressive lung disease involving damage to the alveoli, caused by long-term exposure to irritants
Emphysema causes
. long term exposure to irritating particles in the air taken into lungs (eg: smoke, pollution)
—> smoking, people working in industry + living in cities with high pollution levels
Emphysema effect on respiratory system
. progressive destruction of alveoli + surrounding tissue that supports alveoli
. alveoli lose elasticity, contain more fibrous tissue, break down, and reduces the internal SA for gas exchange
. loss of elasticity in walls of alveoli = lungs constantly inflated + expiration no longer occurs passively but requires active effort
—> inadequate SA for gas exchange
—> difficulty in ventilating lungs
Emphysema symptoms
. breathlessness (dyspnoea) especially during exertion
. chronic cough
. barrel chest (due to hyperinflation)
. fatigue
What is lung cancer
. growth of a tumour in the lungs: a mass of cells in the lung tissue that divides in an uncontrolled way
Lung Cancer causes
. exposure to carcinogens (asbestos fibres, pollutants, smoking)
—> some chemical substances can initiate cancerous growths
—> some chemical substances can promote cancerous growths
—> chemicals in cigarette smoke can initiate AND promote lung cancer
Where does lung cancer commonly begin and what results from this
. in walls of bronchi
. smoke particles irritate mucus membrane resulting in excessive production of mucus
. causes the mucosal cells to divide more rapidly + accumulate (can’t be removed)
—> results in smoker’s cough
—> the trapped mucus can damage alveoli causing emphysema too
What is Pneumonia
. lung infection that causes fluid + mucus to build up in alveoli, causing difficulty breathing
Pneumonia causes
. bacteria, viruses, fungi or other organisms
What response does Pneumonia cause?
The inflammatory response:
. increase in mucus + fluid production in alveoli (obstructs air flow)
. reduces amount of air within alveoli
. reduces gas exchange efficiency
. causes breathing difficulty
What is tuberculosis (TB)
. a lung infection caused by the bacterium Mycobacterium tuberculosis
How is TB spread?
. by droplets (coughs, sneezes, spit) that contain the TB bacteria from an infected person
—> inhaled by others
What happens to respiratory system due to TB
Lung tissue destruction: Cavities, hemoptysis
Chronic inflammation: Scarring, decreased lung elasticity
Bronchial damage: Obstruction, infection risk
Pleural involvement: Fluid build-up, pain
Impaired gas exchange: Shortness of breath, hypoxia
How does the structure of alveoli aid in gas exchange?
1 cell thick epithelial cells + capillaries
Blood capillaries throughout/around them = rich supply of blood + high rate of diffusion
High SA:V ratio
Blood vessels in the heart
Aorta
vena cava
Pulmonary artery
Pulmonary vein
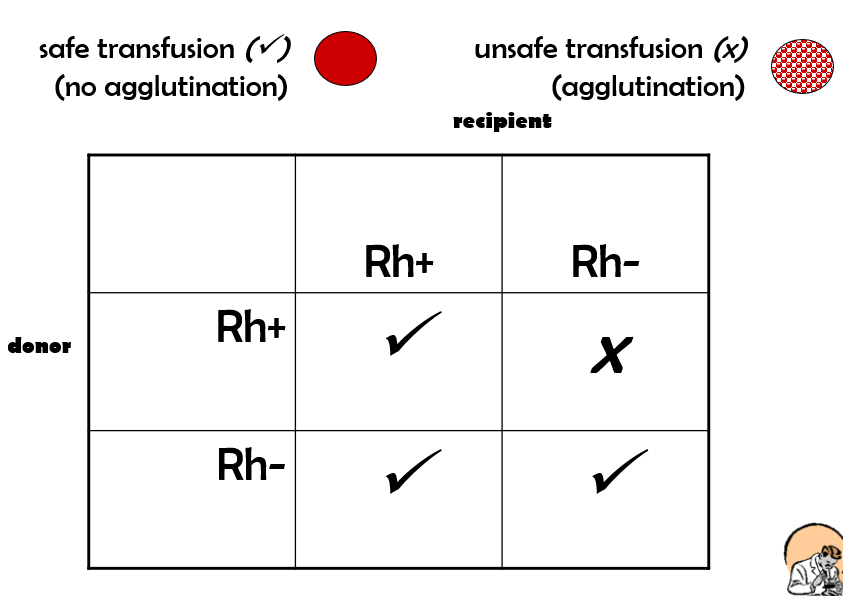
Describe the rhesus blood group system
. based on antigens that occur on surface of RBCs
. Rh antigens are proteins
. With Rh antigens = Rh+, without = Rh-
—> without is able to produce an anti-Rh antibody that reacts against those antigens
—> Rh+ cannot produce an anti-Rh antibody
Blood transfusion
. the transfer of blood, or one of the components of blood, from one person to another
—> avoid bringing together corresponding antigen and antibody since agglutination will occur
—> however in reality, incompatible antibodies in transfusion are diluted by recipient’s plasma, so this can be safe
When is a blood transfusion given and what does this involve?
. given to a person suffering from: excessive blood loss, anaemia, leukaemia, haemophilia
. involves: blood or a blood product, from a donor being injected directly into patient’s bloodstream
Different types of blood transfusions (6)
Whole blood: blood as it is taken from the donor but with a chemical added to prevent clotting.
Red cell concentrates: produced by spinning blood at very high speed in a centrifuge. The heavier cells sink to the bottom, leaving the lighter plasma on top. The concentrate may or may not have platelets and white blood cells (leucocytes) removed. Transfusions of red cell concentrates are used for patients suffering from heart disease or severe anaemia
Platelet concentrates: given to patients who have abnormal platelets or a reduced number of platelets
Cryoprecipitate: obtained by freezing the plasma and thawing it slowly. When the plasma is thawed, the cryoprecipitate remains solid. It contains many of the substances necessary for blood clotting. Cryoprecipitate may be used to treat some forms of haemophilia, but it is most often used for severe bleeding.
Immunoglobulins: group of proteins that act as antibodies. They are extracted from the blood and used for patients who are deficient in antibodies. e.g tetanus immunoglobulin may be used to treat tetanus.
Autologous transfusion: when the patient’s own blood is used. The blood is collected from the patient prior to an operation that may require a transfusion. Autologous transfusions eliminate the risk of transmission of disease and most possible side effects of the usual transfusions.
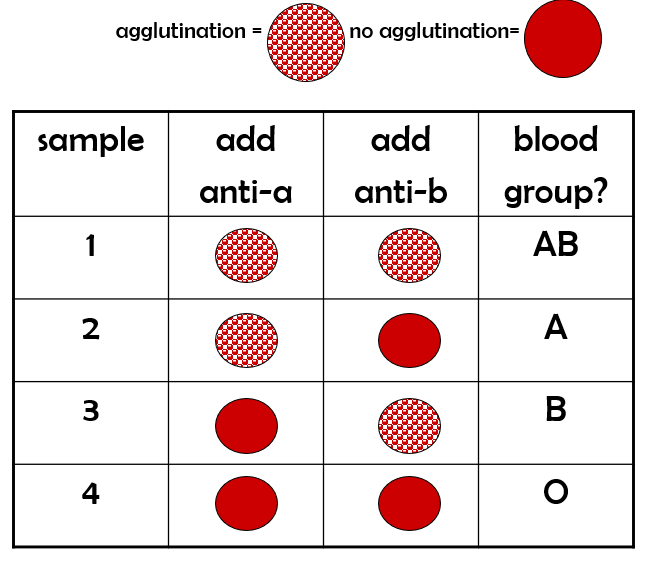
How does blood group typing work
. before any transfusion, patient’s blood group needs to be determined
—> done by: adding pure anti-a and anti-b antibodies to small spots of patient’s blood
How is lymph fluid formed
fluid leaks out of the arterial end of a capillary due to high pressure
Some of this fluid returns to capillary at venous end but excess fluid surrounding tissues is returned to blood via lymphatic system
What’s the lymphatic system and lymph
. a one-way drainage system that carries lymph from body tissues back to general circulation
Lymph = a clear yellow liquid that carries WBCs (especially lymphocytes)
What is the blood
. a liquid connective tissue
Functions of blood (3)
Transport: nutrients, O2, water, hormones, heat TO tissues + removes waste: CO2, urea, creatinine, uric acid
Regulation: pH levels + body temp
Protection: prevents blood loss if blood vessels are damaged + protects body against pathogens + toxins
Blood volume components
Plasma: liquid
Cells: formed elements - RBCs (erythrocytes), WBCs (leukocytes), platelets (thrombocytes)