Pathophysiology and Pharmacology of asthma
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
What is asthma?
Recurrent and reversible short-term obstruction of the airways
Triggered by substances or stimuli that:
Are not necessarily noxious
Normally do not affect non-asthmatic individuals
What are common triggers of asthma attacks?
Allergens (in atopic individuals)
Exercise (especially in cold, dry air)
Respiratory infections (e.g., viral)
Smoke, dust, environmental pollutants
What happens in acute asthma at the airway level?
Acute airway obstruction from smooth muscle contraction
Mucus hypersecretion and thickening/plugging
Airway inflammation
What are the common symptoms of acute asthma?
Dyspnoea (especially on expiration)
Wheezing
Coughing
What type of hypersensitivity reaction is asthma?
Type I (immediate) hypersensitivity reaction
what happens during Sensitisation (first exposure – no symptoms yet)?
step 1 : exposure to allergen, which is inhaled into the airway
step 2: Dendritic cells capture the allergen. Allergen is presented to naïve CD4⁺ T cells.
step 3: Naïve T cells differentiate into TH2 helper T cells.
what are the other steps of sensitisation to asthma?
step 4: Activated TH2 cells release cytokines:
IL4, IL13,IL5
What is the role of IL-4 in asthma sensitisation?
Stimulates IgE production by B cells
Activates mast cells
What is the role of IL-13 in asthma sensitisation?
Promotes mucus production from bronchial epithelial and submucosal glands
Supports IgE class-switching in B cells
Enhances mast-cell–related responses
What is the role of IL-5 in asthma sensitisation?
Activates locally recruited eosinophils
Contributes to airway inflammation
what happens in the second exposure to allgern mechansim?
Second exposure to allergen causes IgE cross-linking on sensitised mast cells
Mast cell degranulation releases histamine, leukotrienes, and prostaglandins
Leads to bronchoconstriction, mucus secretion, airway oedema,
What are the immediate and late-phase reactions in an asthma attack?
Immediate phase: mainly bronchospasm
Late phase: inflammatory reaction contributing to airway swelling and hyperreactivity
What happens during the early phase of an asthma attack?
Bronchoconstriction
Increased mucus production
Vasodilation / increased vascular permeability
Release of inflammatory mediators
What happens during the late phase of an asthma attack?
Recruitment of leukocytes and T cells by cytokines/chemokines from mast cells and epithelial cells
Further release of inflammatory mediators
Contributes to sustained airway inflammation
What happens in the immediate response when an asthmatic is re-exposed to an antigen? (Stepwise)
Step 1: Antigen binds to IgE-IgE receptor complex on mast cells
Step 2: Cross-links IgE receptors → calcium entry into mast cells
Step 3: Mast cells release secretory granules containing histamine
Step 4: Production & release of other mediators (e.g., leukotrienes LTC4, LTD4) → airway smooth muscle contraction
Step 5: Release of chemotaxins (e.g., LTB4) → attract inflammatory cells (eosinophils) to the area
What are the effects of mast cell mediators (histamine and leukotrienes) in the immediate phase of an asthma attack?
Bronchospasm
Increased vascular permeability & vasodilation
Mucus production
Recruitment of additional mediator-releasing cells from the blood
What happens during the late phase of an asthma attack?
Arrival of recruited cells: basophils, eosinophils, neutrophils, TH2 lymphocytes
Release of pro-inflammatory mediators
Eosinophils: release major basic protein → epithelial damage & more airway constriction
Cytokines: amplify inflammation
What happens during the early phase of allergic asthma?
Antigen binds to IgE on mast cell receptors
IgE receptors cross-linked → Ca²⁺ entry into mast cells
Release of mast cell granules containing:
Histamine
Leukotrienes (LTC4, LTD4) → smooth muscle contraction / bronchoconstriction
Release of chemotaxins (e.g., LTB4) → recruit inflammatory cells
What happens during the delayed (late) phase of allergic asthma?
Recruited cells arrive: eosinophils, basophils, neutrophils, TH2 lymphocytes
Pro-inflammatory mediators released →
Epithelial damage
Amplification of inflammation
Leads to sustained airway obstruction and hyperreactivity
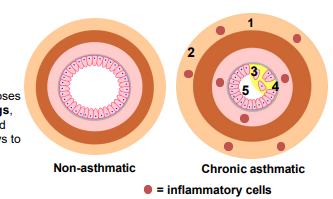
What structural changes occur in chronic asthma (steps 1–3)?
Step 1: Increased mass of smooth muscle → contributes to airway narrowing
Step 2: Accumulation of interstitial fluid (oedema) → thickens airway walls
Step 3: Increased secretion of mucus → further obstructs airflow
What are the functional consequences of airway remodelling in chronic asthma (steps 4–5)?
Step 4: Epithelial damage exposes sensory nerve endings → increases airway sensitivity
Step 5: Airway narrowing by inflammation and bronchoconstriction →
Increased airway resistance
Decreased FEV₁ and Peak Expiratory Flow (PEFR)
Bronchial hyperresponsiveness → airways overreact to triggers
How is asthma diagnosed?
Demonstration of airflow obstruction:
Spirometry
Peak-flow test
Clinical signs: difficulty with exhalation, wheezing on prolonged expiration
Blood tests: eosinophil count
Allergy tests: skin prick test, specific IgE blood test
How does parasympathetic innervation regulate the airways?
Innervates bronchial & vascular smooth muscle, and glands
Step 1: Acetylcholine (ACh) binds to M3 muscarinic receptors
Step 2 : The Gq protein activates PLC
step 3 : PLC converts (PIP₂) into IP₃ and DAG
Step 4: IP₃ diffuses through the cytoplasm to the endoplasmic reticulum.
step 5 : IP₃ binds to IP₃ receptors on the ER, causing Ca²⁺ to be released into the cytoplasm.
step 6 : Stimulation causes:
Bronchoconstriction
Increased mucus secretion
How does sympathetic innervation regulate the airways? step 1
step 1 : Adrenergic stimulation: Adrenal medulla releases adrenaline (epinephrine) into the blood.
Adrenaline binds to β₂-adrenergic receptors on bronchial smooth muscle.
How does sympathetic innervation regulate the airways? step 2-5?
B2 receptor is coupled to Gs protein
Step 2: Gs protein activates adenylyl cyclase
Step 3: Adenylyl cyclase converts ATP → cAMP
Step 4: cAMP activates protein kinase A (PKA)
causes : broncholidation
the second sympathetic innervation: noradrengic
Step 1: Neuronal noradrenaline is released from sympathetic nerve endings.
Step 2: Noradrenaline binds to β₂-adrenergic receptors on airway gland cells.
Step 3: β₂ receptors are Gs-coupled, activating adenylyl cyclase → ↑cAMP → PKA.
Step 4:this casues decreased mucus production.