Peds Exam 2
1/115
Earn XP
Description and Tags
Musculoskeletal, Integumentary, and Respiratory
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
116 Terms
Bacterial Skin Infections
Cellulitis, impetigo, acne
Viral skin infections
HPV and molluscum contagiosum
fungal skin infections
candida and tinea corporis
cellulitis
bacterial infection caused by streptococcus or staphylococcus; presents with inflammation, intense erythema and edema (causes pain) most likely on face and extremities; infections on face, genitals, or joints are most likely to lead to sepsis, implanted hardware is at increased risk of osteomyelitis or sepsis; treated with antibiotics and supportive care (warm or cold compresses)
impetigo
very contagious bacterial infection caused by staphylococcus aureus often around mouth, nose, or on face; starts a pruritic erythematic edematous lesion then vesicle (fluid filled) with surrounding erythema that bursts into a honey-colored crust; treated with topical antibiotic like Mupirocin for 7-10 days; prevent with hand washing and keeping child home for first 24 hr on antibiotic treatment
acne treatment
wash twice a day, topical benzoyl peroxide or antibiotic, then Tretinoin (Rentin-A) or Isotretinoin (Accutane)- cause birth defects so 2 forms of birth control and pregnancy testing is required for Accutane
molluscum contagiosum
papules caused by Poxvirus, small (2-6mm) raised flesh-like pink with small central depression occasionally with exudate; common on trunk, axillae, face, and groin in groups (not on palms or soles of feet); lasts 6-18 months; spread with scratching and especially contagious when wet; disinfect tub and towels; resolve on own but may need removal in severe cases
human papillomavirus (HPV)
common warts (rough, cauliflower, raised or flat, flesh colored with black dot, alone or in cluster), plantar warts (soles of feet, black dot in center, painful when big), flat warts: on face or legs, flesh-colored and smooth, no pain or pruritus); treat with OTC meds, laser or curettage or blister beetle juice
tinea corporis
“ringworm” caused by trichophyton that is spread with skin-to-skin contact or with contaminated bed linens/uniforms or pets; causes pruritic erythematous lesions with a raised border, central clearing and well defined border, takes about a month to resolve with antifungal (azoles); treat animals and owners to prevent recurrence
candidiasis
fungal infection caused by Candida albicans in chronically moist areas; oral thrush (steroid inhaler) causes white exudate and lesions that cannot be removed; on skin (diaper rash) it is inflamed areas of erythema, raised papules with scalloped border (satellite lesions, peeling, easy bleeding, pruritus on border); treated with oral or topical nystatin and keeping diaper area and bottles clean and dry
atopic dermatitis
eczema; inflammation of skin usually associated with allergies and asthma; pruritus, red to brownish-gray patches and papules, occasional vesicles, lesions disappear when scratching stops (“the itch that rashes”); secondary lesions (lichenification-thickened skin); not in diaper region but face, elbows, and knees; treatment to reduce pruritus hydrate skin and anti-inflammation (oatmeal baths in warm water)
atopic triad
eczema, allergic rhinitis, and asthma
contact “irritant” dermatitis
when allergen or skin irritant (poison oak/ivy) causes irritated, inflamed pruritic rash within 48 hr with vesicles that may weep; could be hives if allergic; treated with topical anesthetics, drying agents for weeping, hydrocortisone or steroids or calamine lotion for pruritus
diaper dermatitis
erythema/scaling of skin due to prolonged contact with urine and or feces (frequently seen in easy babies); can lead to secondary infection (candida) if longer than 3 days; barrier ointment without total occlusion
pediculosis capitis
lice; pruritis of scalp with identification of nits (eggs in any part of hair) and louse (adults live at nap of neck of behind ears); kill adults and remove eggs, wash bedding and towels in hot water and dry at hottest setting, vacuum, non washables go in sealed plastic bag for 2 weeks, topicals such as permethrin shampoo
scabies
burrow into skin to lay eggs in warm places like skin folds; highly transferable through close contact; s/sx: pruritic especially at night, fine linear red/pink/gray rash commonly between fingers, waist, axillae, wrists, groin and butt; wash and boil everything; permethrin (left on skin overnight if older than 2) or ivermectin (oral if topical isn’t working)
lyme disease
tick-borne illness caused by the bacteria spirochete borrelia which enters skin through saliva and feces of deer ticks; early s/sx: fever, chills, fatigue, muscle and joint aches, bullseye rash; late s/sx: severe headaches and neck stiffness, paresthesia, memory problems, palpitations and chest pain
ointments/oils vs creams/lotions
oils prevent evaporation of moisture and hold meds on skin for longer (atopic dermatitis) while creams are absorbed by skin quickly and are non-greasy
topical corticosteroids
applied directly to lesion, more is not always more effective, use for 5-7 days or less due to risk of resistance and thinning of skin and SubQ
burn injuries
affect children more because they have a greater central body surface area, great fluid volume, and are less effective at responding to fluid shifts; skin is thinner so they burn at lower temps and with shorter exposure; scarring is more severe; test adequacy of fluid resuscitation with capillary refill
diaphysis
long part (shaft) of bone
epiphysis
proximal and distal end of bone adjacent to joints, contains growth plate (physis), increased risk of problems with future growth
fracture definition and healing
partial or complete break in bone; body causes inflammation and bleeding at site, hematoma around fracture site to stabilize bone, osteoblasts scaffold new bone to create callus, remodeling process up to 1 year, quicker in kids due to thick periosteum and generous blood supply
comminuted fracture
splintered into pieces, rare in peds
displaced vs nondisplaced
displaced: bone ends not aligned
nondisplaced: bone ends aligned
spiral fracture
twisting stress (ski/snowboarding with foot stuck in boot, soccer-run into players, football and wrestling, or jerking limb)
salter-harris system fracture
classification to describe fractures at growth plate
purpose of traction
provide rest to extremity, prevent contracture deformity, treat dislocation, correct position and alignment, immobilization, reduce muscle spasms; keep weights off floor and pin sites clean, CMS checks, provide developmental distraction that won’t affect traction
5 P’s of compartment syndrome
Pain, Paresthesia (pins and needles) are early then Pulselessness, Pallor, and Paralysis are late signs
soft splints
allow for more give to make room for swelling to prevent compartment syndrome before casting
developmental dysplasia of the hip (DDH)
hip socket (acetabulum) is too shallow to cover head of thighbone (femoral head), can be congenital or happen in childhood; s/sx: shortened limb on affected side, unequal gluteal folds or knee height, limited abduction, positive Barlow or Ortalani tests (clunk heard from dislocation when hip is rotated); greater risk in breeched infants and females
spica cast
hip and leg casts for developmental dysplasia of the hip (DDH), risk for infection (diaper area), impaired mobility (muscle weakness), pain, impaired circulation (compartment syndrome)
CMS testing
cap refill, temp (cool is bad), pulse, sensation and movement
soft tissue injuries
unusual in young kids because their growth plate is weaker than ligament so it breaks first but is common in adolescents (growth plate is solid), RICE
scoliosis
curvature and rotation of the spine greater than 10 degrees; can be idiopathic (alone) or with other neuromuscular conditions; screened at 10-12 with girls and 13-14 with boys; Adams test (forward bend) to look for shoulder blade or hip asymmetry; curve can cause difficulty breathing
scoliosis treatment
bracing is not curative but will slow or prevent progress, brace is worn under clothes for 23 hrs a day (remove for physical activity and bathing) without any lotion or powders under, may just watch and wait or need surgery in severe cases. needs log rolling after surgery to prevent bend or twist of spine during healing
osgood-schlatter disease
overuse condition or injury of knee causing a painful lump and swelling on the shinbone along the patellar tendon under knee, common during growth spurts and resolves on own when bones are done growing
slipped capital femoral epiphysis (SCFE) definition and demographics
upper femoral epiphysis (growth plate) gradually (not from injury) slips (like ice cream on cone) posteriorly from its functional position; most common in early adolescent obese males with endocrine anomalies
slipped capital femoral epiphysis (SCFE) symptoms and treatments
s/sx: acute onset of painful thigh/knee/groin limiting activity, limping, increased pain with internal hip rotation, leg length discrepancy; emergent non weight bearing and no ROM to prevent it from fully separating (bedrest with traction before surgery), surgical pinning needed
legg-calve perthes disease (LCPD)
idiopathic (no cause, not infection) epiphysis disnegration from lack of blood flow more common in preschool/early school boys; s/sx: hip or knee pain that increases after activity, limp, quadriceps atrophy, limited ROM; may resolve with limiting running and jumping hard which can restore blood flow after 18-24 months, monitor for several years to ensure revascularization and bone growth
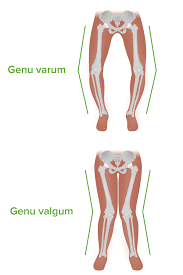
normal knee joint findings in kids
genu varum: knees curving outward is normal in infancy through 3 years
genu valgum: knees curving inward is normal and expected at ages 3-7/8 years
juvenile idiopathic arthritis (JIA)
chronic autoimmune disorder causing inflammation of joints and other tissue with unknown cause; diagnosis with xray for joint pain, ESR and CRP (inflammatory markers) will be elevated, CBC, and slit-lamp eye exam; can cause uveitis (inflammation in anterior chamber of eye) that leads to vision loss so needs regular eye exam
treatments for JIA
NSAIDS (first-line, reduce inflammation and pain, not long term because of GI bleeding/upset and rebound headaches, not aspirin), corticosteroids (oral pills or joint injections with many long and short term effect), disease-modifying antirheumatic drugs (DMARDs) (slows joint damage and reduces swelling), biologics (subQ injection/infusions that target specific inflammatory cell reactions)
DMARDs and biologics side effects
DMARDs: GI upset
Biologics: body aches, fatigue
Both: hepatotoxicity and leukocytopenia (cancer), immunosuppressant (infection risk)
corticosteroids short-term effects
hyperglycemia (increase hunger and weight), increase infection due to decreased immune response, thrush, GI upset, hypertension
corticosteroids long-term effects
osteoporosis and stunted growth (Ca is not absorbed and is excreted in urine), increased intraocular pressure, hypertension, adrenal insufficiency
nursing care for JIA
PT and OT (kids limit movement because it hurts but moving helps stiffness), exercises like simple isometric or tensing exercises), heat (no ice)
muscular dystrophy
group of genetic disorders where there is a gradual degeneration of muscle fibers which leads to progressive weakness and wasting of symmetric groups of skeletal muscles
Duchenne muscular dystrophy (DMD)
most severe and common MD, x-linked (mostly boys) recessive (30% are new mutations)
s/sx: learning difficulties, decrease heart muscle (HF) and diaphragm (vent in teens, pneumonia), loss of muscle mass, fibrosis, brittle/weak bones, Gower’s sign (using hands to walk up body to stand)
goals: maintain optimal function of all muscle for as long as possible (respiratory and cardiac function) and prevent contractures
clubfoot definition
bi or unilateral ankle and foot deformity with forefoot adduction (inward), midfoot supination, heel points down, and ankle equinus; more common in boys may be alone or with other condition like spina bifida
clubfoot treatment
phase 1: ponseti serial casting does correction by placing a new cast every 7-10 days for 8-12 weeks (achilles tendon is cut before last cast)
phase 2: bracing with splint to maintain correction, worn for 23 hr for 2 months then 12 hr (when sleeping) until kindergarten
osteomyelitis
acute or chronic infection on bone
s:sx 2-7 days of pain and warmth of affected area with decreased ROM and fever or malaise, seen on MRI or CT
treatment: IV antibiotics via PICC for at least 3-4 weeks
dura mater
tough outer layer of meninges providing the most protection
arachnoid
middle meninges that contains CSF
pia mater
inner meninge that adheres to surface of the brain
epidural hematoma
between dura and skull, rapid bleed from artery
subdural hematoma
blood that accumulates between the dura mater (the outermost layer of the brain's protective membranes) and the arachnoid mater (the middle layer)
subarachnoid hemorrhage
acute or chronic bleeding between the arachnoid and the pia mater layers
intracerebral hemorrhage
bleeding in brain- stroke
intracranial pressure (ICP)
pressure in cerebrum plus pressure in blood plus pressure in CSF
monro-kellie doctrine
compensatory mechanism between brain, CSF, and intracranial blood; when one changes the other change to stabilize ICP
cerebral perfusion pressure (CPP)
pressure needed to maintain blood flow to the brain, MAP-ICP, raising MAP raises CPP and raising ICP lowers CPP
early and late signs of increased ICP
early: slight changes in consciousness, headaches, N/V, diplopia, seizures, increased head circumference in infants, bulging fontanelle
late: significant decrease in LOC, bradycardia, decreased motor and sensory responses, changes in pupil size and reactivity, abnormal posturing, Cheyne-Stokes respirations (alternating periods of rapid, deep breathing followed by pauses in breathing), coma
glasgow coma scale
tests eye opening, verbal and motor response, 3-8 is severe problem
Cushing’s triad
less blood flow to brain causes hypertension with widening pulse pressure (systolic-diastolic, larger means heart is more stressed)(to increase CPP), irregular and shallow respirations (from non functioning brainstem), and bradycardia (short time tachy then slow)
primary vs secondary head injuries
primary (time of injuries): skull fracture, intracranial hematomas, diffuse axonal injury (shearing of small blood vessels off the brain), coup
secondary (complications of primary injury): increased ICP, hypoxic brain damage, cerebral edema, herniation (through brain stem), contrecoup
assume spine injury (c collar) unless ruled out with imaging
peak of cerebral edema
swelling peaks around 72 hours (could come in walking and talking then go unconscious) so first 5 days are critical in severe TBI, need to manage ICP to continue getting the brain enough blood, look for drainage from nose/ears (CSF: positive for glucose or halo ring test)
nursing management of ICP
diuretics (manatiol) and steroids (decrease inflammation), HOB: 30-45 degrees, decrease stimuli (lights, noise, screens), avoid valsalva maneuver (coughing/bearing down, limit suctioning to PRN), wake PT overnight for neurochecks and vitals, LOC is first to change
neurological assessment
LOC with GCS, orientation, mood, behavior, motor skills, balance, coordination, ROM for all joints, deep tendon reflexes, sensory and symmetry
look for racoon (bruising around eye) or battle (bruising behind ear) sign, no NG without imaging
brain healing
brains heal slower in kids while bones heal faster than in adults
signs of concussion
feeling mentally slow, repeats questions, memory problems, headache, N/V, sensitivity to light and noise, dizziness/balance problems, sleeping more or less than usual, different emotions, numbness/tingling
return to activity only depends on child’s symptom improvement (more rest if symptoms worsen)
hydrocephalus
abnormal accumulation of CSF in brain (CSF is continuously made even if ICP increases) because of overproduction (rare) or blocked or lack of absorption of CSF; most are congenital (genetic or in prenatal events) but may be acquired after bleeding, inflammation, or infection
signs of hydrocephalus
infants: may not have signs due to fontanel compensation, irritability, V, major head circum growth, poor head control from heavy head, eye crossing, split sutures of skull, bradycardia, apnea, delayed milestones, sunsetting sign (eyes trend downward)
older kids: headache, N/V, irritability, lethargy, vision changes, neck pain, gait changes, learning problems, papilledema (swelling of optic disc/nerve)-blindness may be permanent if not treated
hydrocephalus treatment
temporary ways to decrease ICP until ventriculoperitoneal (VP) shunt can be places to pump fluid out, afterwards monitor for vomiting/headaches and returning symptoms and prevent scratching at site to prevent infection
spina bifida
neural tube (formed at 3-4 weeks) defect when the vertebrae doesn’t fuse anywhere along the spine which leads to progressive loss of strength and mobility; due to hyperthermia, folic acid deficiency, seizure meds
nursing care of meningeal
keep in prone position, assess for infection, cover with sterile non-adherent gauze and moisten with normal saline every 24 hr, no diaper
complications of spina bifida
hydrocephalus is very common, altered sensation and motor ability below defect, progressive scoliosis (resp. issues), central sleep apnea, neurogenic bladder, bowel program to prevent constipation, executive functioning challenges (intellectual disability), skin breakdown, latex allergy
meningitis
infection of meninges surrounding the brain and spinal cord; sx: headache, fever, stiff neck (unable to put chin to chest due to pain), tight leg muscles/muscle spasms, blue to blotchy skin or lips, labored breathing, hard to awake; droplet transmission; most causes are viral so supportive care is treatment,
positional signs of meningitis
kernig sign: can’t straighten leg with hip flexed
Brudzinski sign: flex at knees when neck is flexed
generalized seizure
sudden, uncontrolled electrical disturbance in the both sides of the brain
absence seizure
brief (5-20 sec) episodes of altered consciousness, no muscle activity, blank facial expression, can be up to 100s in a day, generalized seizure
tonic-clonic seizure
generalized grand mal seizure, abrupt arrest of activity with impaired consciousness
tonic phase: sustained muscle stiffening
clonic phase: symmetric and rhythmic muscular contraction and relaxation
status epilepticus
seizure lasting more than 5 min or more that 1 in 5 min period without returning to normal consciousness between is a medical emergency needing rescue med and 911
atonic seizure
abrupt loss of postural tone, impairment of consciousness, confusion, lethargy, sleep, may fall down from losing consciousness for a few sec then get back up as if nothing happened
myoclonic seizure
brief random, contractions of a muscle group followed by loss of muscle tone and falling forward
focal seizures
affect one area of the brain which leads to specific features exhibited during seizure but may have awareness or impaired awareness
febrile seizure
convulsions caused by quick increase in temp to fever, mostly under 5 years
seizure rescue meds
given for seizures over 5 min, benzodiazepines in nostril or rectal gel (midazolam, diazepam, lorazepam)
adverse effects of antiepileptic drugs (calm the brain)
common: sedation/lethargy, cognitive defects, N/V, headaches, dizziness, behavior outburst/irritability
less common: leukopenia, aplastic anemia, liver failure/drug toxicity so routine CBC and liver enzyme tests
nursing care for seizures
remove obstacles or dangers, turn child on side, do not insert anything in mouth; watch for affected areas/behaviors (which side, lip smacking, incontinence), time seizure
cerebral palsy
nonprogressive disorder of movement, muscle tone, or posture due to abnormal brain development or damage
symptoms of cerebral palsy
exaggerated reflexes, floppy or rigid limbs, involuntary (spasms) movement, hypo- or hypertonic
cerebral palsy care
treat symptoms; botox for spasticity and drooling; baclofen (oral or pump) to relax skeletal muscles; diazepam (benzo) for sedation, anticonvulsant and anxiety, and relax muscles, various anti-epileptic drugs (AED)
Reye’s syndrome
rare but severe swelling in liver and brain, linked to aspirin use with viral infection (most commonly flu or chickenpox), needs quiet atmosphere
differences in child vs adult airway
obligate nose breathers until 6 months, tongue fills mouth more, shorter and narrower trachea and bronchi, epiglottis is floppy, more can get trapped at bifurcation of bronchus, decreased alveolar surface area, increased O2 needs, more force needed for ventilation, increased friction and resistance, higher risk of rapid decompensation
signs of respiratory distress in child
rapid resp rate and HR, nasal flaring (normal when eating), retractions, grunting, sounds (wheezing, stridor, coarse), sweating, head bobbing, change in color and alertness, head tipped backwards or tripod positioning, symptoms may lessen during resp failure (shouldn’t get quite or better too fast-run out of energy)
upper resp infection (URI)
viral infection in nose and throat; common cold, sx: nasal congestion, fever, fatigue, sore throat, sneezing or coughing; supportive care with warm compresses, cool liquids/popsicles to stay hydrated, suction congestion
otitis externa (OE)
swimmers ears; inflammation of external auditory canal from viral, bacterial, or fungal (if wet) infections; sx: itching, pain, feeling of pressure or fullness, sounds like they are under water (hearing loss), manage pain and teach to keep canal dry
acute otitis media (AOM)
inflammation and infection of middle ear due to fluid accumulation behind tympanic membrane that can’t drain through a narrowed eustachian tube; viral or bacterial; sx:acute ear pain, irritability, fever, poor eating, pulling on ear, bulging tympanic membrane
prevention and treatment for acute otitis media (AOM)
prevented by: no secondhand smoking, eliminate environmental allergens, breastfeeding for 6 months and avoid pacifiers
treat: pain (Tylenol under 6 mon, ibuprofen over 6 mon), warm pack under and behind ear, ear tubes to drain if recurrent, watchful wait (come back in 48 hr if it doesn’t improve even if its bacterial)