Tietze Chapter 1
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Clinical pharmacy
The term — historically described patientoriented rather than product-oriented pharmacy practice.
Clinical Pharmacist
The term — was used to describe a pharmacist whose primary job was to interact with the health care team, interview and assess patients, make patientspecific therapeutic recommendations, monitor patient response to drug therapy, and provide drug information
Pharmacist
the term — implies the integration of patient- and product-oriented pharmacy practice.
Pharmaceutical care
The term — is used to describe the broad-based, patient-focused responsibilities of pharmacists
Helper and Strand
Who define pharmaceutical care as the “responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life.
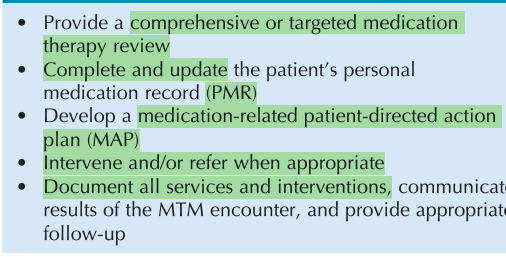
Medication Therapy Management
It is defined as “a distinct service or group of services that optimize therapeutic outcomes for individual patients”. The goals of its services include improved medication understanding, adherence and detection of medication-related problems, including adverse drug reactions.
American Council on Pharmaceutical Education (ACPE)
To be eligible for licensure, pharmacists must be graduates of a college of pharmacy accredited by the —
Foreign Pharmacy Graduate Examination Committee (FPGEC)
Pharmacists who graduated from foreign pharmacy schools are eligible for licensure if they have earned the — certification or follow other statespecific requirementS.
Califonia
All states except — require successful completion of the North American Pharmacist Licensure Examination (NAPLEX).
1500 hours
All states require that licensure candidates complete a specified number of internship hours, typically around — , prior to seeking licensure.
Continuing education units (CEUs)
Most licensing boards require that pharmacists earn — for relicensure. These are earned by successful participation in ACPE-accredited programs
True
True or false
Licensure for authorization to administer injectable medications (e.g., immunizations) is a separate but parallel licensing process.
Postlicensure credentialing
It is voluntary and is available at the specialist or disease level. It indicates that the pharmacist has additional expertise above and beyond what is required for licensure
Council on Credentialing in Pharmacy (CCP)
— defines certification as “a voluntary process through which a nongovernmental agency or an association grants recognition to an individual who has met certain predetermined qualifications specified by that organization. This formal recognition is granted to designate to the public that this individual has attained the requisite level of knowledge, skill, and/or experience in a well-defined, often specialized, area of the total discipline.”
Specialist credentialing
Board certification (official recognition of specific knowledge and skills) is achieved in addition to state and federal professional licensure. WHat is this called?
Board of Pharmacy Specialties (BPS)
—, created in 1976 by the American Pharmacists Association (APhA), is responsible for setting standards for certification and recertification and for administering the certification and recertification processes.
BCNP (1972)
BCPS (1988)
BCNSP (1988)
BCPP (1992)
BCOP (1996)
Five specialty practice areas are recognized by BPS:
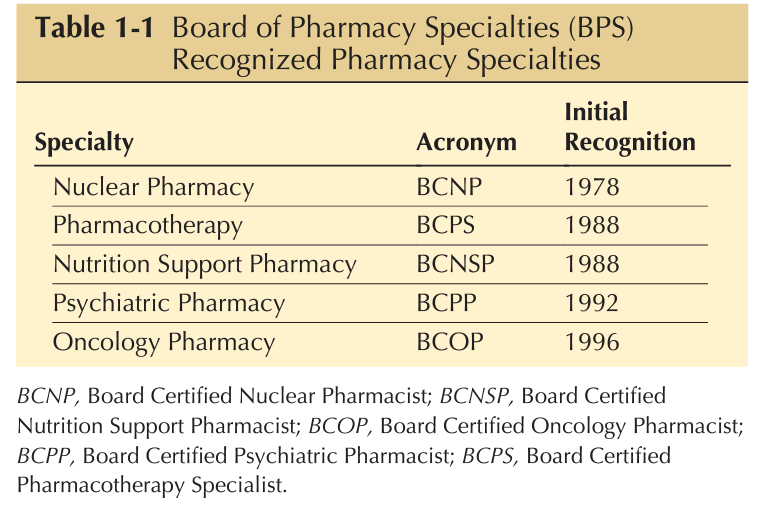
7 years
For specialist, recertification is required every —
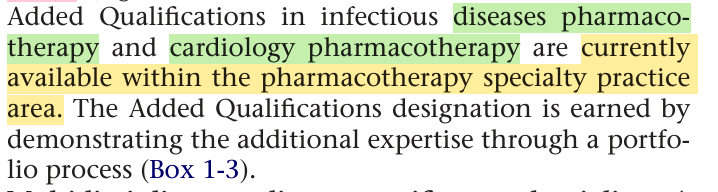
AQ (Added Qualification)
The BPS also recognizes additional expertise within a subspecialty area by the designation —
Pharmacy based immunization delivery
Pharmaceutical care for patients with diabetes
Pharmacy based lipd management
OTC Advisor
These are voluntary and do not require any additional training or experience beyond that required for pharmacy licensure. What are some certificate programs?
Residency
It is defined as an “organized, directed, postgraduate training program in a defined area of pharmacy practice”8 . It provides pharmacists with 1 to 2 years of supervised experience in practice and management activities.
Generalists
Specialty patient care area
Post graduate year 1 (PGY1) residency programs train —; postgraduate year 2 (PGY-2) residency programs train pharmacists in a —.
Fellowship
It is a highly individualized program designed to prepare the pharmacist to become an independent researcher. As of 2009, 17 programs of this are recognized
Clinical environment
Answer clinical environment
Fee for service FFS
Patients may select any doctor, hospital, or laboratory without permission of primary care physician (PCP). Patients pay up front then submit the bill for reimbursement.
Health maintenance organization HMO
Patients must choose a PCP and are restricted to in-network doctors. Referrals are made through the PCP.
Point of service POS
Similar to HMO but with fewer restrictions.
Preferred provider organization pPO
Permission is not required to see in-network specialists; some coverage for out-of-network care.
Medical home
Defined by the Association of American Medical Colleges as “a concept or model of care delivery that includes an ongoing relationship between a provider and patient, around-the-clock access to medical consultation, respect for a patient’s cultural and religious beliefs, and a comprehensive approach to care and coordination of care through providers and community services,”
Clinics
These establishments serve general unrestricted patient populations or very specific patient groups (e.g., hypertension clinic, diabetes clinic, anticoagulation clinic, medication refill clinic). They may share the same physical space; in this situation the schedule is set to allow each clinic to have a unique weekly or daily schedule
Public hospital
These are publicly funded and provide heath care services to all patients, regardless of the patient’s type of insurance or ability to pay for the health care services. Some cities and states pay for this hospital services from tax revenues
Private hospitals
These are privately funded institutions whose services are generally not available, except for emergency care, to patients who are not part of the private group
Veterans Administration hospital system
The federal government funds federal hospitals. The — is an extensive nationwide system of hospitals, clinics, and nursing homes funded by the federal government to provide health care services to American armed forces veterans.
Teaching hospitals
Hospitals, regardless of the funding source, may be affiliated with medical schools. These hospitals, known as —, provide training sites for physicians and other health care professionals.
Community hospitals
Community-based, nonteaching hospitals are sometimes called —
Tertiary hospitalis
Some hospitals, recognized for their highly specialized services (e.g., pediatrics, oncology, cardiology) and large referral patient populations, are known as
Paramedicals
Allied health care professionals, also known as —, provide health care services and perform tasks under the direction of physicians
Allopathic physician
Osteopathic physician
Physicians, doctors who have medical or osteopathic degrees, are generally considered the health care team leaders.
What physicians rely on standard treatment
What physicians use techniques of spine and joint manipulation
American Board of Medical Specialties (ABMS)
There are 26 approved medical board specialties. The —, a group of 24 member boards, certifies more than 145 physician specialties and subspecialties
Nurses
They care for the physical and psychosocial needs of patients and carry out physician-directed orders regarding patient care.
Nurse practitioners
“licensed independent practitioners who practice in ambulatory, acute and long term care as primary and/or specialty care providers.”
Physician assistants
health care professionals licensed, or in the case of those employed by the federal government they are credentialed, to practice medicine with physician supervision.
Health care team
It consists of all health care professionals who have responsibility for patient care plus the patient
Teaching hospitals
These are the primary training sites for most health care professionals. Health care services in these hospitals are structured around medical teaching teams composed of physicians, medical students, and, depending on the hospital, other health care professionals
Medical team
—, organized to provide a structured training environment, are responsible for the care of patients located in assigned areas of the hospital (e.g., the cardiology unit) or patients located throughout the hospital
Medical team
The — functions as a unit, with the division of labor and the responsibility of each member determined according to the status of each individual.
Attending physician
— is the senior physician on the medical team. They assume responsibility for all patients assigned to the team and provides guidance and direction to team members.
True
True or false
Patient presentations may take place in a conference room, in the hallway outside of the patient’s room, or in the patient’s room.
Medical fellows
These are physicians who have completed residency training and have elected to continue their training in a research-oriented fellowship program
Medical fellows
They work closely with the attending physician and have fewer direct patient care responsibilities than residents. They teach the more junior members of the team
Medical Residents
They are physicians who have graduated from medical school and are in structured and supervised residency training programs.
First year residents
They are known as interns. Internal medicine internships of at least 1 year often are required before the resident moves on to more specialized training in areas such as surgery or psychiatry
First year residents
They have an intensive year of training, with frequent night call duty and direct responsibility for the care of a variety of inpatients and outpatients.
Second year internal medicine residents
They are also are known as junior admitting residents (JARs)
Third year medical residents
—, also known as senior admitting residents (SARs), are in the final year of 3-year internal medicine residency programs. The senior medical resident sets the daily team rounding schedule, prioritizes the work schedule, coordinates the team’s work, supervises the interns, supervises and works closely with the medical students on the team, and consults with the attending physician
Chief medical resident
— is a senior medical resident who, in addition to the usual resident responsibilities, has administrative responsibility for various aspects of the residency program, such as scheduling rotations and vacations and organizing and overseeing seminars and other education program
True
True or false
The chief medical resident position is competitive; typically one or two residents per year are selected for this position.
Third
Although medical students get some experience examining and interviewing patients in the first or second year of medical school, clinical clerkships usually start in the - year of medical school.
Third year medical students/Junior medical students
They spend part of the year in the patient care environment in month-long rotations such as internal medicine, surgery, obstetrics and gynecology, and pediatric services. Their patient workloads are limited to a small number of patients, and medical school faculty and more experienced team members closely supervise them.
Senior medical students/externs
They are in the last year of medical school. Depending on the medical school curriculum, senior medical students may spend all or part of the last year of medical school in a variety of selective or elective rotations. They have more patient care responsibilities than do junior medical students but less than interns or other residents.
Admitting physician
The — evaluates the patient and orders laboratory tests, procedures, diets, and medications. They may consult with specialty physicians and other health care professionals, including pharmacists.
Head nurse
Each floor, unit, or ward has a — with administrative responsibility for nursing services. Some hospitals assign each patient to a primary NP who determines the nursing care plan for the patient and coordinates patient care.
Morning
Medical team rounds usually occur in the —.
Work rounds
These rounds, led by the medical resident, usually take place early in the morning. It allows all members of the team to catch up on the status of each patient and plan for the day’s tests, consultations, and other patient care activities.
Attending rounds
These rounds, led by the attending physician, generally occur after work rounds and are held in conference rooms rather than at the patient’s bedside. Although some teaching takes place during work rounds, most in-depth teaching discussions take place during these rounds.
Sign out rounds
At the end of the day the team gathers for — rounds, during which the physician responsible for providing medical coverage in the evening and overnight is briefed about each patient on the service.
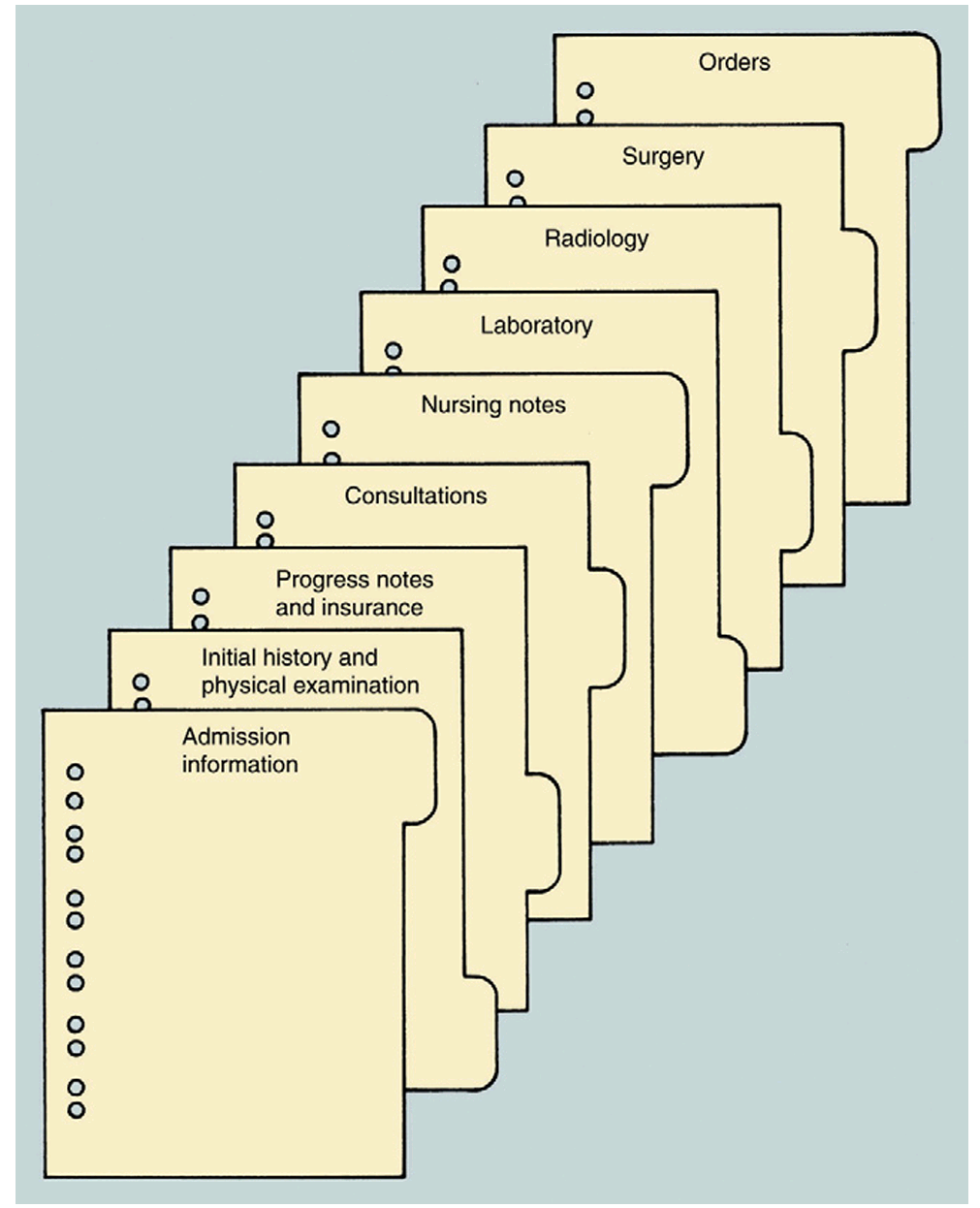
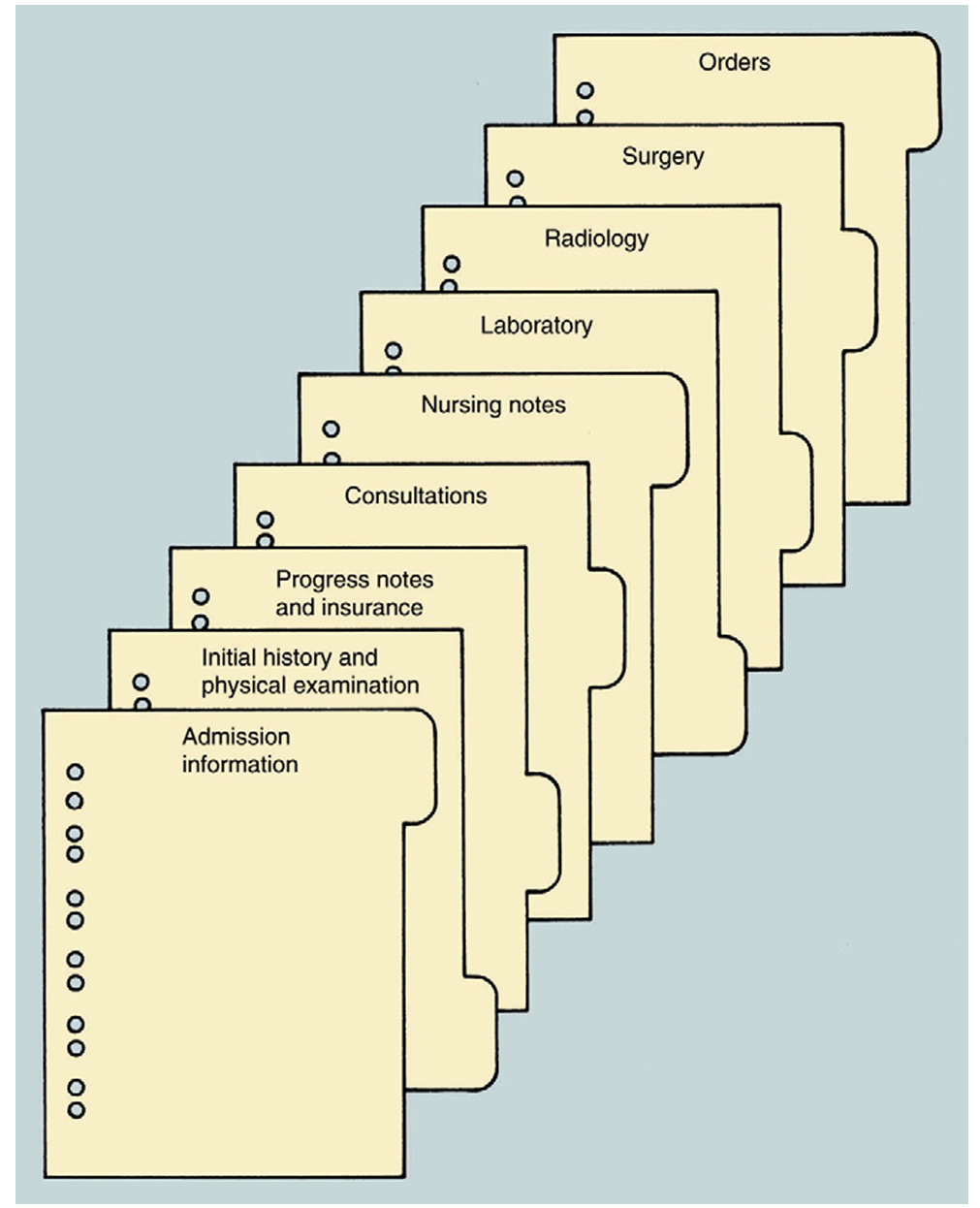
Inpatient medical record / CHART
It is a legal document that includes sections for hospitalspecific admission and insurance information, initial history and physical examination, daily progress notes written by every health care professional who interacts with the patient, consultations, nursing notes, laboratory results, and radiology and surgery reports
True
True or false
-Access to patient charts is restricted to authorized health care professionals.
Hospital admission number
Upon patient discharge, the medical record is stored in the medical records department and is retrievable by referencing the patient’s —
Ward secretary/Ward clerk
A — coordinates the processing of paperwork on a hospital unit or part of a hospital unit. Some large units have two or more of them
Problem-oriented medical record POMR
Many institutions and practices chart in a specified format known as a —. It is structured around a prioritized patient problem list. Progress notes and discharge summaries address each patient problem as itemized on the patient problem list.
Outpatient
The — medical record or chart contains the same type of information as the inpatient chart with the exception of the admitting data, physician orders, admission history and physical examination, and medication administration sections.
False
True or false
Inpatient charts are used more to document patient-specific encounters and data than to communicate with other health care professionals.
Medicare Part D
It provides for prescription drug benefits for medicare beneficiaries including pharmacist provided MTM