First Aid USMLE Step 1: Cardiovascular
1/389
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
390 Terms
Defect in left-right dynein (involved in L/R asymmetry) can lead to___________, as seen in Kartagener syndrome (primary ciliary dyskinesia).
Dextrocardia
Patent foramen ovale is caused by a failure of __________ and ___________ to fuse after birth. What can this lead to?
-Caused by failure of septum primum and septum secundum to fuse after birth; most are left untreated.
-Can lead to paradoxical emboli (venous thromboemboli that enter systemic arterial circulation), similar to those resulting from an ASD.
What is the most common congenital cardinal anomaly?
VSD
Outflow tract formation
Truncus arteriosus rotates; neural crest and endocardial cell migrations cause truncal and bulbar ridges that spiral and fuse to form aorticopulmonary septum to form ascending aorta and pulmonary trunk.
Fetal circulation diagram
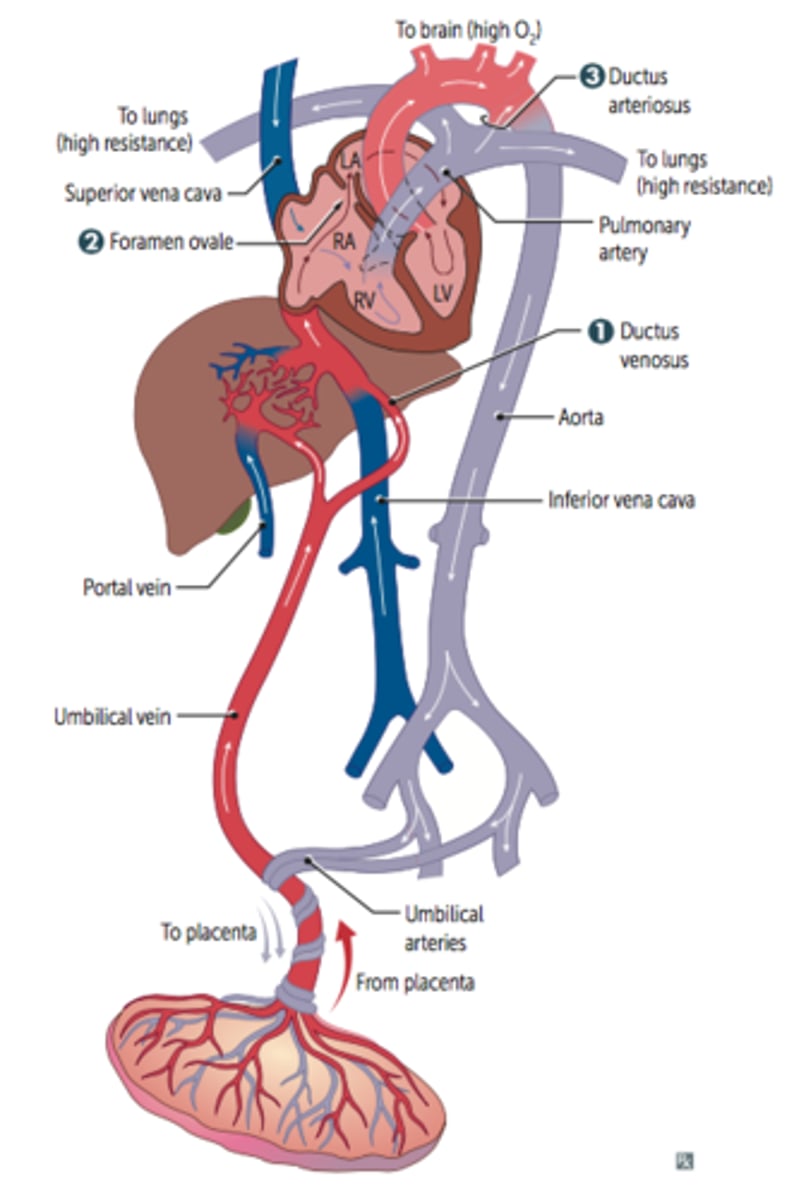
Ductus venosus
Blood entering fetus via placenta through the umbilical vein is conducted via the ductus venosus into the IVC, bypassing hepatic circulation.
Foramen ovale
Most of the highly oxygenated blood reaching the heart via the IVC is directed through the foramen ovale and pumped into the aorta to supply the head and body.
Ductus arteriosus
Deoxygenated blood from the SVC passes through the RA -> RV -> main pulmonary artery through patent ductus arterioles -> patent descending aorta; shunt is due to high fetal pulmonary artery resistance (due partly to low O2 tension).
Closure of foramen ovale
At birth, infant takes a breath; decreased resistance
in pulmonary vasculature (d/t a decrease in intra-thoracic pressure from the baby taking a breath) -> increased left atrial pressure vs. right atrial pressure (d/t increase in blood entering the pulmonary artery & more blood returning to the LA); foramen ovale closes (now called fossa ovalis);
Closure of ductus arteriosus
Increase in O2 (from respiration) and decreaese in prostaglandins (from placental separation) causes closure of ductus arteriosus.
________ helps close a PDA
Indomethacin
__________ keeps the PDA open.
PGE1 and PGE2
**Prostaglandins dilate vessels
"E1 & E2 kEEp PDA open"
What becomes of the allaNtois-> urachus
MediaN umbilical ligament
What is the adult remnant of the ductus arteriosus?
Ligamentum arteriosum
Tunica adventitia
-Outer layer of blood vessel wall
-A layer of c.t. containing collagen and elastic fibers
-In large and medium veins it contains longitudinal smooth muscle fibers
-Small blood vessels called vasa vasorum may be present
Internal elastic lamina
-A layer of elastic tissue that forms the outermost part of the tunica intima of blood vessels. It separates tunica intima from tunica media
External elastic lamina
A layer of elastic connective tissue lying immediately outside the smooth muscle of the tunica media of an artery
SA and AV nodes are usually supplied by _____.
RCA
Infarct of blood supply to SA and AV nodes may cause _____________.
Nodal dysfunction (bradycardia or heart block).
The left circumflex artery (LCX) supplies what?
Lateral and posterior walls of left ventricle, anterolateral papillary muscle
The left anterior descending artery (LAD) supplies what?
The anterior 2/3 of the interventricular septum, anterolateral papillary muscle, and anterior surface of the left ventricle
"Widow-Maker"
Branches of the Right Coronary Artery (RCA)?
Right (acute) marginal artery and the posterior descending/interventricular artery (PDA)
What does the right (acute) marginal artery supply?
Right ventricle
What does the posterior descending/interventricular (PDA) artery supply?
The posterior 1/3 of the IV septum, posterior walls of the ventricles, and the posteromedial papillary muscle
What is right-dominant circulation?
PDA arises from RCA (occurs 85% of the time)
"most people are right-handed"
What is left-dominant circulation?
PDA arises from LCX (occurs 8% of the time)
What is co-dominant circulation?
PDA arises from both RCA & LCX (occurs 7% of the time)
Coronary artery occlusion most commonly occurs in the ____.
LAD
Coronary blood flow peaks in ________.
Early diastole
What is the most posterior part of the heart?
Left atrium
Enlargement of the left atrium can cause?
Dysphagia due to compression of the esophagus and/or hoarseness due to compression of the left recurrent laryngeal nerve (a branch of the vagus)
Cardiac output (CO) =
stroke volume (SV) × heart rate (HR).
Definition of SV?
Amount of blood pumped out of heart w/ each heart beat
Mean arterial pressure (MAP) =
1) CO x total peripheral resistance (TPR) AKA (P=Q*R)
2) 2/3 diastolic Pressure + 1/3 systolic Pressure
"MAP is mainly used to find Diamonds"
Pulse pressure =
systolic - diastolic pressure
Pulse pressure is proportional to ____, inversely to __________.
SV, compliance of aorta
**If the aorta becomes rigid (decreased compliance) in conditions such as arteriosclerosis or atherosclerosis, the pulse pressure would be very high
What stage of the cardiac cycle is altered most with increased HR? Why is this?
Diastole
Less filling time -> decreased CO (i.e. ventricular tachycardia & A-fib)
Conditions that cause an increased Pulse Pressure
hyperthyroidism, aortic regurgitation, aortic stiffening (isolated systolic HTN in elderly), obstructive sleep apnea (increases sympathetic tone), exercise (transient)
Conditions causing decreased pulse pressure
Aortic stenosis, cardiogenic shock, cardiac tamponade, advanced heart failure (HF)
What causes an increase SV?
-Increased contractility (e.g., anxiety, exercise)
-Increased preload (i.e. early pregnancy, exercise-> d/t muscle contraction pushing more blood up to the heart, increased blood volume)
-Decreased afterload
"SV CAP"-> Stroke Volume affected by Contractility, Afterload & Preload
What decreases both preload and afterload?
ACE inhibitors and ARBs
Normal ejection fraction is ____.
greater than or equal to 55%
EF is ____ in systolic HF.
Decreased
EF= ventricular contractility (as EF increases, your contractility has improved)
EF is ____ in diastolic HF.
Normal
Viscosity increased in?
Hyperproteinemic states (e.g., multiple myeloma), polycythemia, Hereditary Speherocytosis
_______ provide most of the blood storage capacity.
Veins
What is inotropy?
contractility
What is chronotropy?
HR
What are some ⊕ inotropic agents?
Catecholamines, digoxin, exercise
What are some ⊝ inotropic agents?
Uncompensated HF, narcotic overdose, increased afterload
What are some ⊕ venous return agents?
Fluid infusion, sympathetic activity
What decreases TPR?
Exercise, AV shunt
Exercise ______ inotropy and _________TPR to maximize CO.
increase, decrease
HF _______ inotropy & causes __________ to ________ to maintain CO.
decreases, fluid retention, increase preload
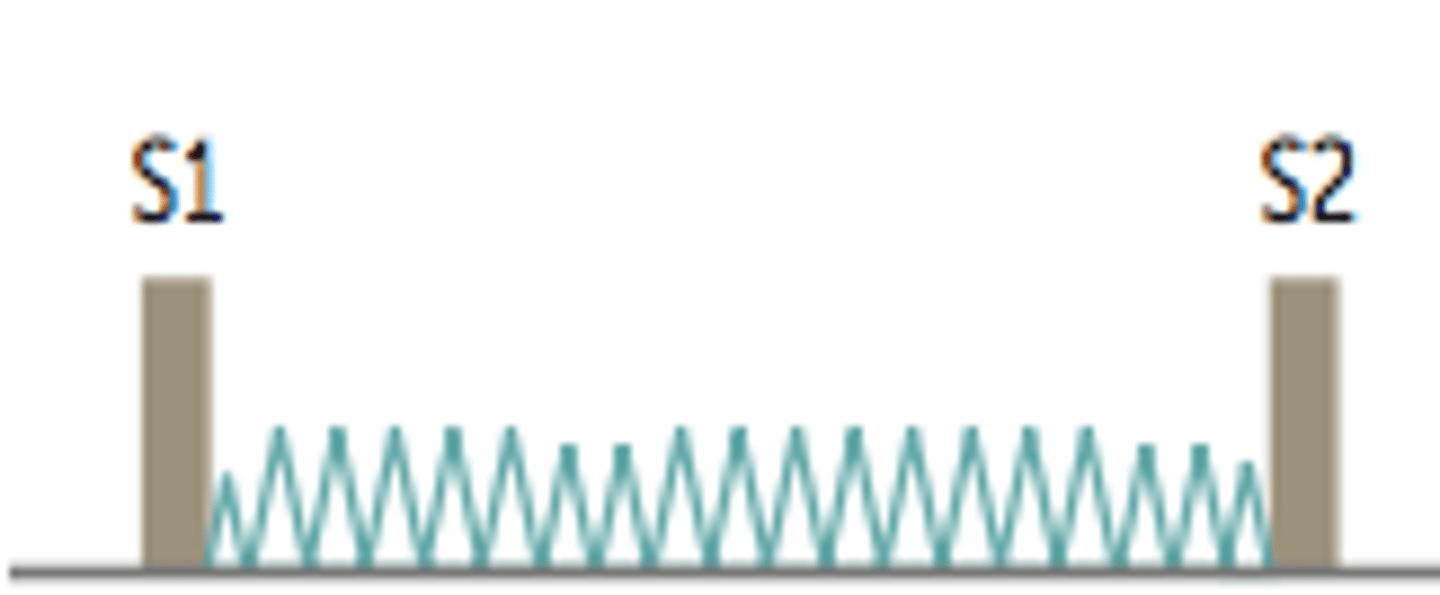
Cardiac cycle
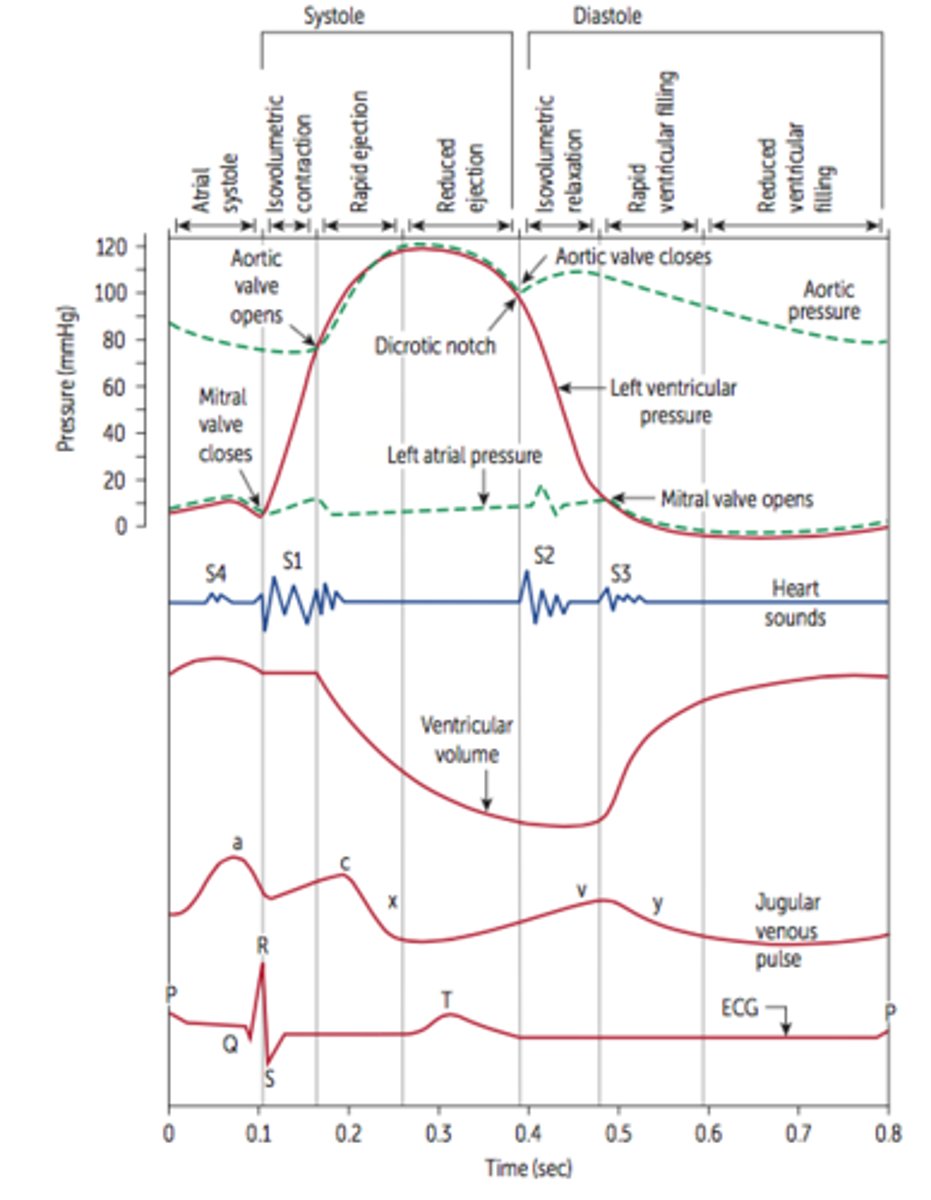
What is a heart sound caused by?
turbulence of blood as valve closes
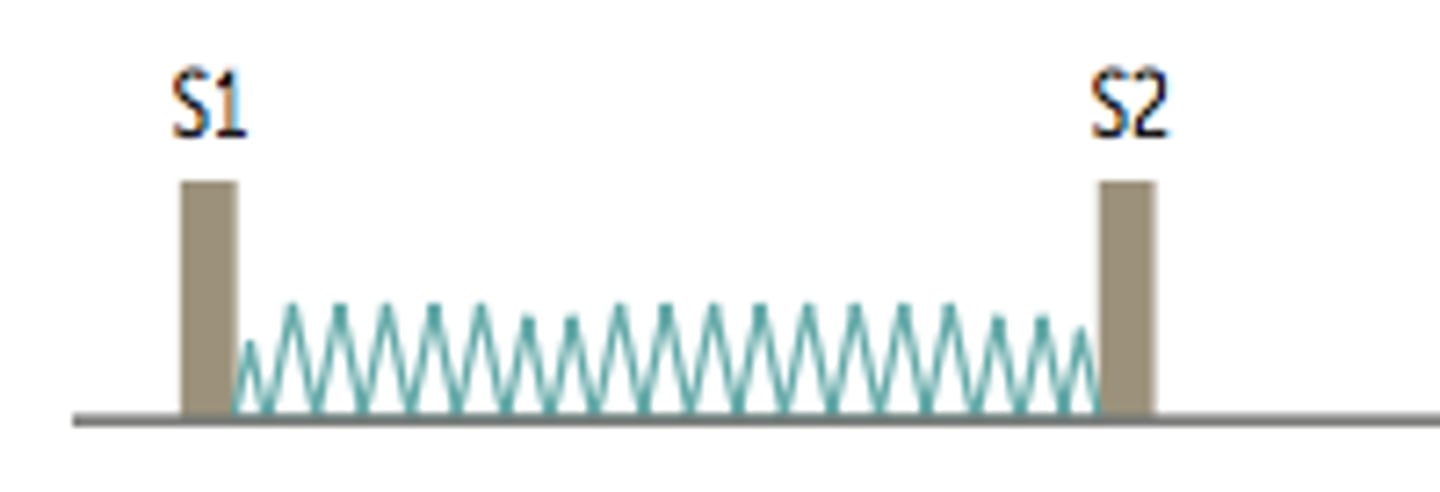
S1 heart sound
S1—mitral and tricuspid valve closure.
Loudest at mitral area.
S2 heart sound
S2—aortic and pulmonary valve closure.
Loudest at left upper sternal border.
S3 heart sound
S3—in early diastole during rapid ventricular
filling phase. Associated with increased filling pressures (e.g. mitral regurgitation, HF) and more common in dilated ventricles (but normal in children and pregnant women).
S4 heart sound
S4—in late diastole ("atrial kick"). Best heard
at apex with patient in left lateral decubitus position. High atrial pressure. Associated with ventricular hypertrophy. Left atrium must push against stiff LV wall.
**considered abnormal, regardless of patient age
What causes a splitting of S2?
caused when the aortic & pulmonary valve closer is not synchronized
Normal splitting
**Aortic valve closing a little before the pulmonary valve on normal inspiration
Inspiration -> drop in intrathoracic pressure increasing venous return-> increased RV ejection time-> delayed closure of pulmonic valve.
Decreased pulmonary impedance (increased capacity of the pulmonary circulation) also occurs during inspiration, which contributes to delayed closure of pulmonic valve.
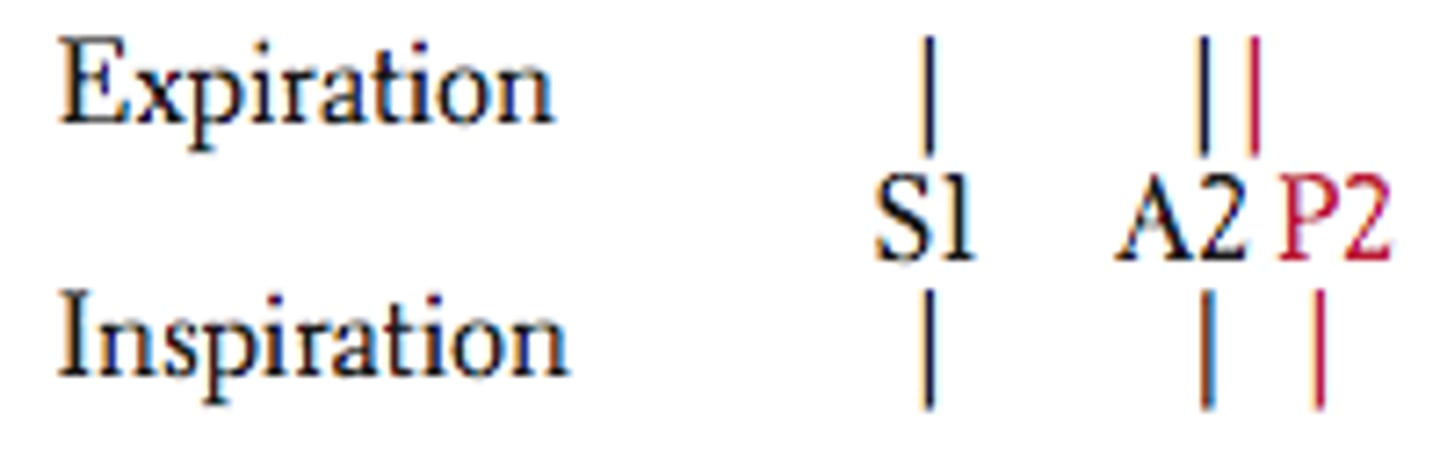
Wide splitting
Seen in conditions that delay RV emptying (e.g., pulmonic stenosis, right bundle branch block). Delay in RV emptying causes delayed pulmonic sound (especially on inspiration). An exaggeration of normal splitting.

Fixed splitting
Seen in ASD.
ASD causes left-to-right shunt -> increased RA and RV volumes -> increased flow through pulmonic valve such that, regardless of breath, pulmonic closure is greatly delayed.
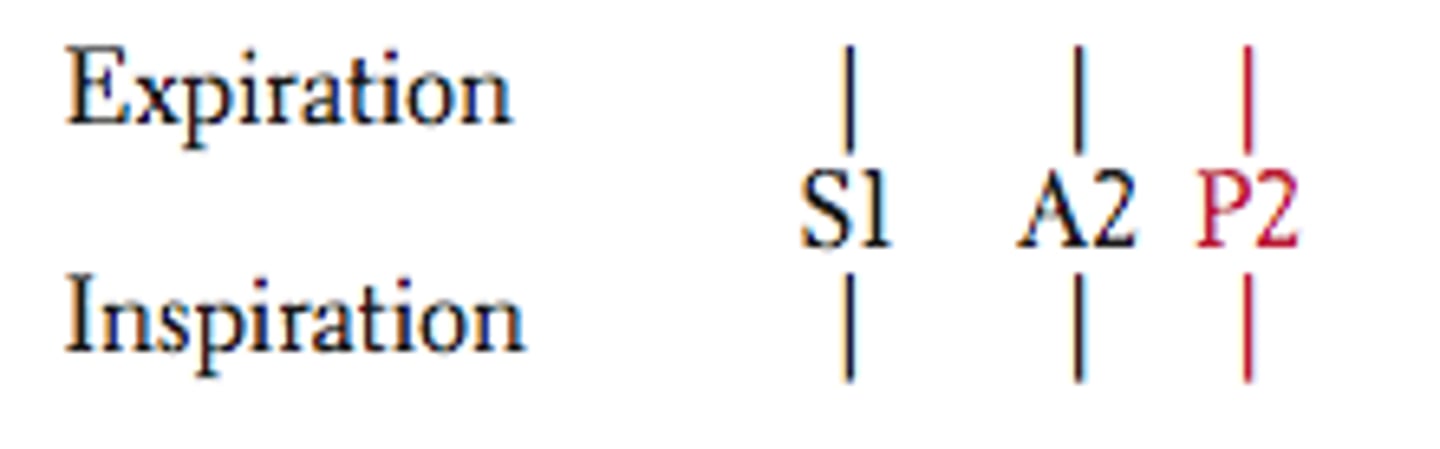
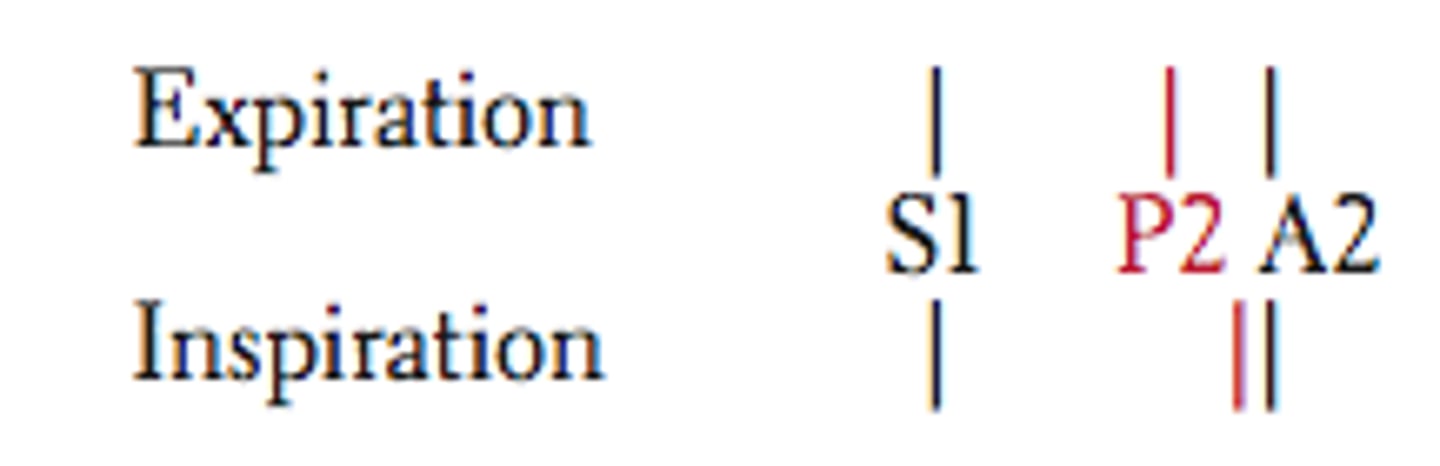
Paradoxical splitting
Seen in conditions that delay aortic valve closure AKA "delay LV emptying" (e.g., aortic stenosis, left bundle branch block).
Normal order of valve closure is reversed so that P2 sound occurs before delayed A2 sound.
Therefore on inspiration, P2 closes later and moves closer to A2, thereby "paradoxically" eliminating the split. (usually heard in expiration)
**delayed emptying of the left side of the heart
Auscultation of the heart
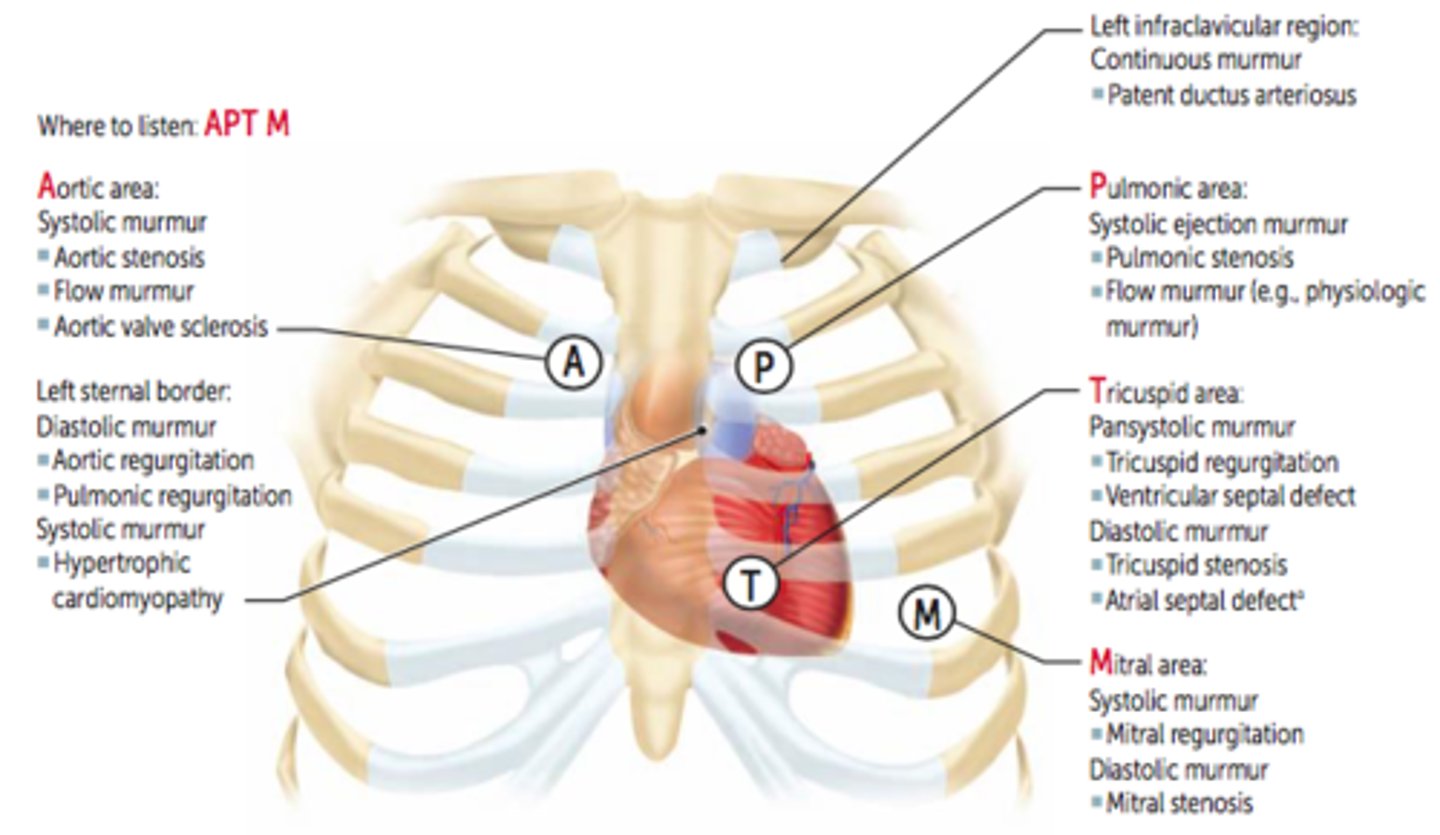
Sounds best heard at the left sternal border
-Diastolic murmur: aortic regurgitation, pulmonic regurgitation
-Systolic murmur: hypertrophic cardiomyopathy
Sounds best heard at the pulmonic area
Systolic ejection murmur: pulmonic stenosis, flow murmur
Sounds best heard at tricuspid area
-Pansystolic murmur: tricuspid regurgitation, VSD
-Diastolic murmur: tricuspid stenosis, ASD
Sounds best heard at mitral area
-panystolic murmur: mitral regurgitation
-Late systolic murmur: MVP
-Diastolic murmur: mitral stenosis
What does inspiration cause in regards to blood flow to heart?
increase venous return to RA d/t the negative intra-thoracic pressure created, which pulls blood from vena cava-> RA
Effect of inspiration of heart?
increased intensity of right heart sounds
bc the amount BV is increased
decreased intensity of LEFT sided murmurs
Hand grip (↑ afterload d/t muscle tension increasing SVR)
⬆️ intensity of MR, AR, VSD murmurs
⬇️hypertrophic cardiomyopathy murmurs
Later onset of click/murmur in MVP
Valsalva (phase II), standing up (⬇️preload)
**Valsalva creates a positive intra-thoracic pressure, which decreases blood to RA & decreases BP
⬆️ intensity of hypertrophic cardiomyopathy murmurs
Earlier onset of click/murmur in MVP (also gets louder?)
⬇ intensity of most murmurs
Rapid squatting (⬆️venous return, ⬆️preload, increased afterload)
⬆Most murmurs ( flow through stenotic or regurgitant valve)
⬇️intensity of hypertrophic cardiomyopathy murmurs
Later onset of click/murmur in MVP
What are the Systolic heart sounds?
aortic/pulmonic stenosis
mitral/tricuspid regurgitation
VSD
MVP
What are the Diastolic heart sounds?
aortic/pulmonic regurgitation
mitral/tricuspid stenosis
What is heart murmur caused by?
turbulent blood flow against valve
MR is often due to _____________.
Ischemic heart disease (post-MI), MVP, LV dilatation.
rheumatic fever
infective endocarditis
TR commonly caused by ___________.
RV dilatation
infective endocarditis
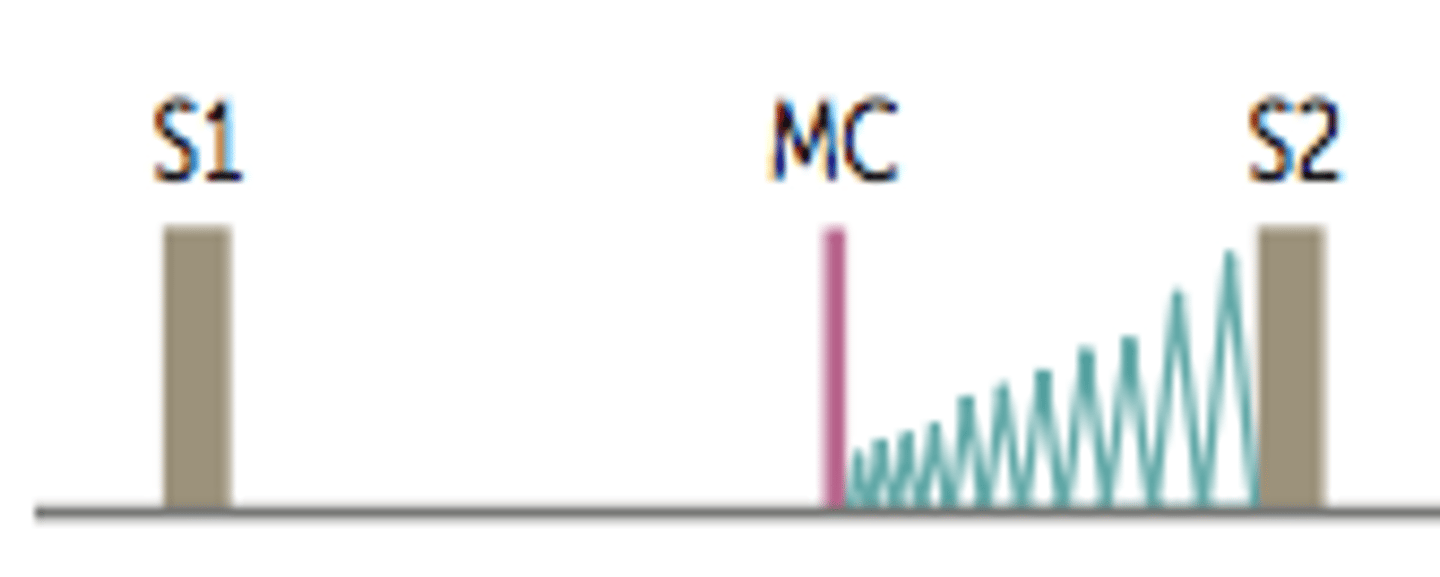
Mitral valve prolapse (MVP)
-Late systolic crescendo murmur with midsystolic click (MC; due to sudden tensing of chordae tendineae). Most frequent valvular lesion.
-Best heard over apex. Loudest just before S2.
-Usually benign. Can predispose to infective endocarditis.
-Can be caused by myxomatous degeneration (1° or 2° to connective tissue disease such as Marfan or Ehlers-Danlos syndrome), rheumatic fever, chordae rupture.
**leaflets bulge upward or back into LA during contraction
VSD
-Holosystolic, harsh sounding murmur
-Loudest at tricuspid area
**seen in newborns
PDA
cause
what does it sound like
-Continuous machine-like murmur.
-Loudest at S2. Often due to congenital rubella or prematurity. Best heard at left infraclavicular area.
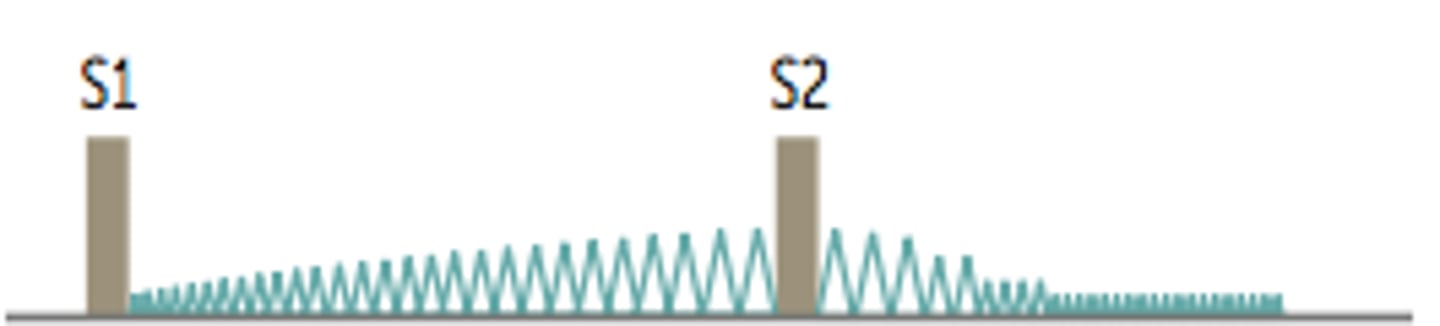
Aortic stenosis (AS)
-Crescendo-decrescendo systolic ejection murmur (ejection click may be present). LV >> aortic pressure during systole.
-Loudest at heart base; radiates to CAROTIDS.
"Pulsus parvus et tardus"—pulses are weak with a delayed peak. Can lead to Syncope, Angina, and Dyspnea on exertion (SAD).
-Often due to age-related calcification in older patients (over 60) or early-onset calcification of bicuspid aortic valve.
"Pulsus parvus et tardus"
-Pulses are weak with a delayed peak. Can lead to Syncope, Angina, and Dyspnea on exertion (SAD).
-Aortic stenosis
Mitral/tricuspid regurgitation
(MR/TR)
-Holosystolic (AKA "pan" throughout systole), high-pitched "blowing murmur."
-Mitral—loudest at APEX and radiates toward AXILLA. MR is often due to ischemic heart
disease (post-MI), MVP, LV dilatation.
-Tricuspid—loudest at TRICUSPID area and radiates to right STERNAL border. TR commonly caused by RV dilatation.
-Rheumatic fever and infective endocarditis can cause either MR or TR.
**seen in IVDU
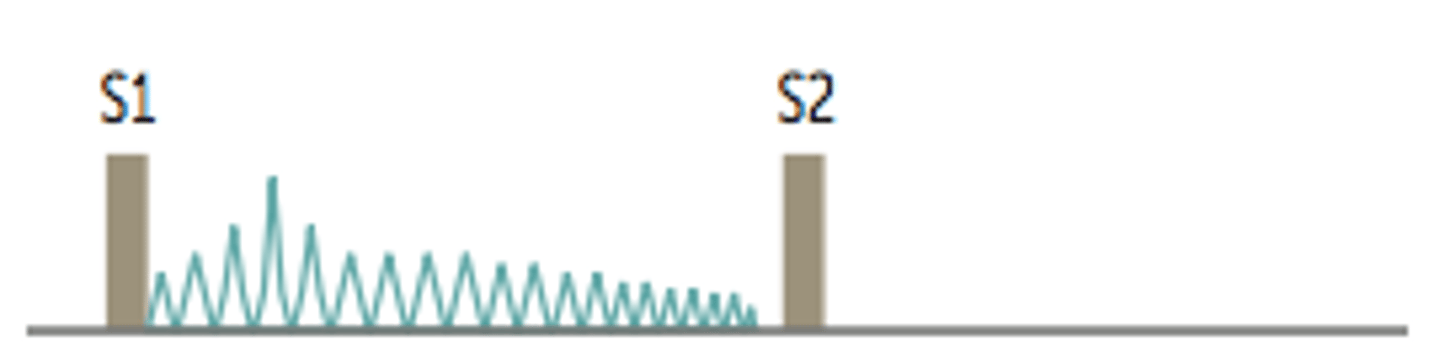
Aortic regurgitation (AR)
-High-pitched "blowing" early diastolic decrescendo murmur.
-Long diastolic murmur and signs of hyper dynamic pulse, & head bobbing when severe and chronic.
-wide pulse pressure (b/c blood flows back into LV & pressure in aorta decreases)
-Often due to aortic root dilation (marfans or syphilis), bicuspid aortic valve, endocarditis, rheumatic fever
-Progresses to left HF.
**heard at the left side of the sternum because blood is shooting back into the LV, peripheral pulses are strong & bounding
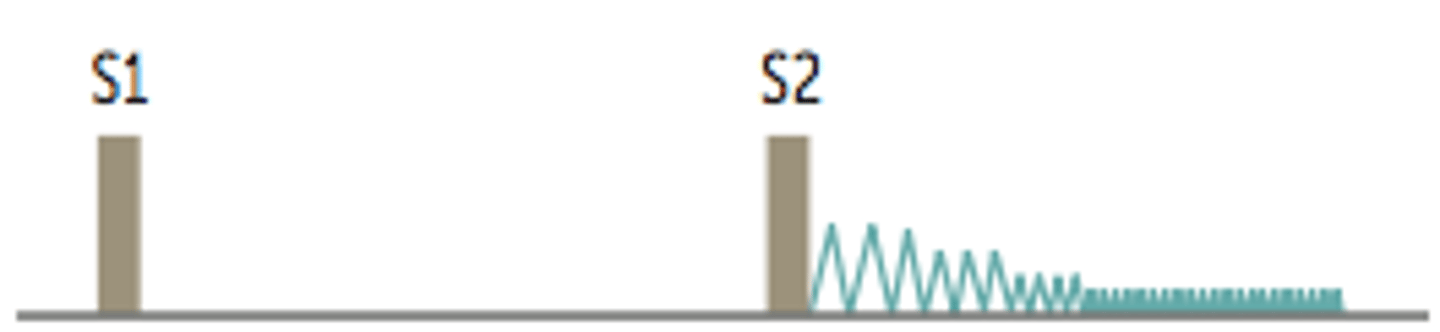
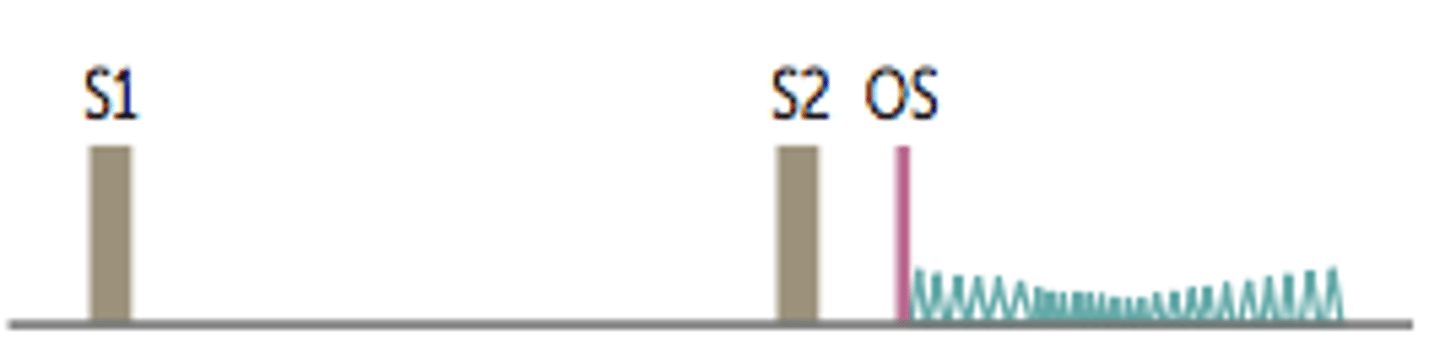
Mitral stenosis (MS)
-Follows opening snap (OS; b/c leaflets are stenosis).
-Delayed rumbling late diastolic murmur (interval between S2 and OS correlates withseverity).
-LA >> LV pressure during diastole.
-Often occurs 2° to rheumatic fever.
-Chronic MS can result in LA dilatation.
**increase with expiration b/c you are filling up LA more "lEft= Expiration"
Trick for Mitral/Tricuspid/Aortic regurgitation murmurs**
All have high-pitched blowing murmurs
"When a girl gives head, she has to regurgitate the c-m!"
Trick for MVP & Mitral stenosis**
Both begin in the middle of diastole & systole; respectively
.
MVP bw 1 and 2
MS bw 2 and 1
What is the conduction pathway?
SA node ("pacemaker" that creates the AP)-> atria-> AV node-> bundle of His (only electrical connection between atria & ventricles)-> right & left bundle branches-> Purkinje fibers-> ventricles
What happens if the bundle of His/Purkinje/ventricles are in control?
wide QRS
Torsades de pointes
-Polymorphic ventricular tachycardia, characterized by shifting sinusoidal waveforms on ECG; can progress to ventricular fibrillation.
-LONG QT interval predisposes to torsades de pointes.
-Caused by drugs,K+, Mg2+, other abnormalities
-Treatment includes magnesium sulfate.
**"Twisting of the points" d/t various QRS amplitudes
Drugs that induce Long QT (Torsades)
"ABCDE"
-Class 1A, III antiArrhythmics
-AntiBiotics (e.g. macrolides)
-Anti"C"ychotics (e.g. haloperidol)
-AntiDepressants (e.g. TCAs)
-AntiEmetics (e.g. ondansetron)
Congenital long QT syndrome
Inherited disorder of myocardial repolarization, typically due to ion channel defects; ⬆️ risk of sudden cardiac death (SCD) due to torsades de pointes.
Romano-Ward syndrome
-Congenital long QT syndrome
-Autosomal dominant, pure cardiac phenotype (no deafness).
Jervell and Lange-Nielsen syndrome
-Congenital long QT syndrome
-Autosomal recessive, sensorineural deafness
Brugada syndrome
-Autosomal dominant disorder most common in Asian males.
-ECG pattern of pseudo-right bundle branch block and ST elevations in V1-V3.
-⬆️risk of ventricular tachyarrhythmias and SCD. Prevent SCD with implantable cardioverter-defibrillator (ICD).
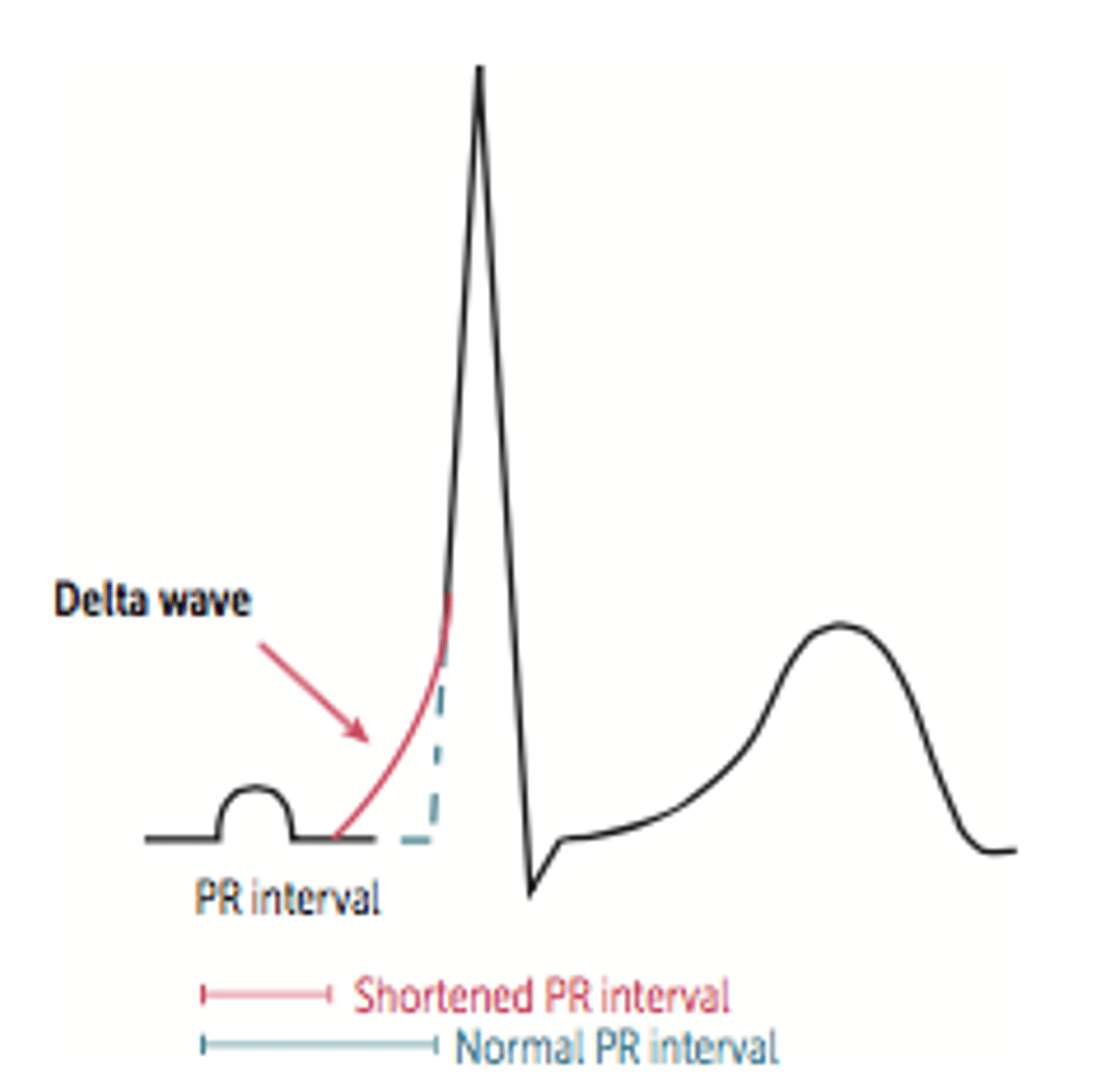
Wolff-Parkinsion-White syndrome (WPW)
-Most common type of ventricular pre- excitation syndrome. Abnormal fast accessory conduction pathway from atria to ventricle (bundle of Kent= accessory pathway) bypasses the rate-slowing AV node ➡️ ventricles begin to partially depolarize earlier ➡️ characteristic delta wave with widened QRS complex and shortened PR interval on ECG. May result in reentry circuit ➡️ supraventricular tachycardia.
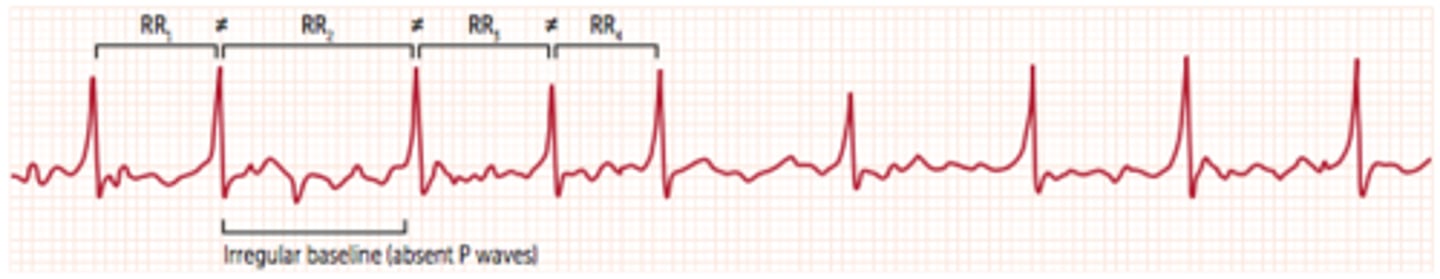
Atrial fibrillation
Chaotic and erratic baseline with no discrete P waves in between irregularly spaced QRS complexes. IRREGULARLY IRREGULAR heart beat.
**RR intervals are not =