Immunology - Lecture 14 - Organization of the immune organs
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
What are the two types of lymphoid organs?
Primary lymphoid organs and secondary lymphoid organs.
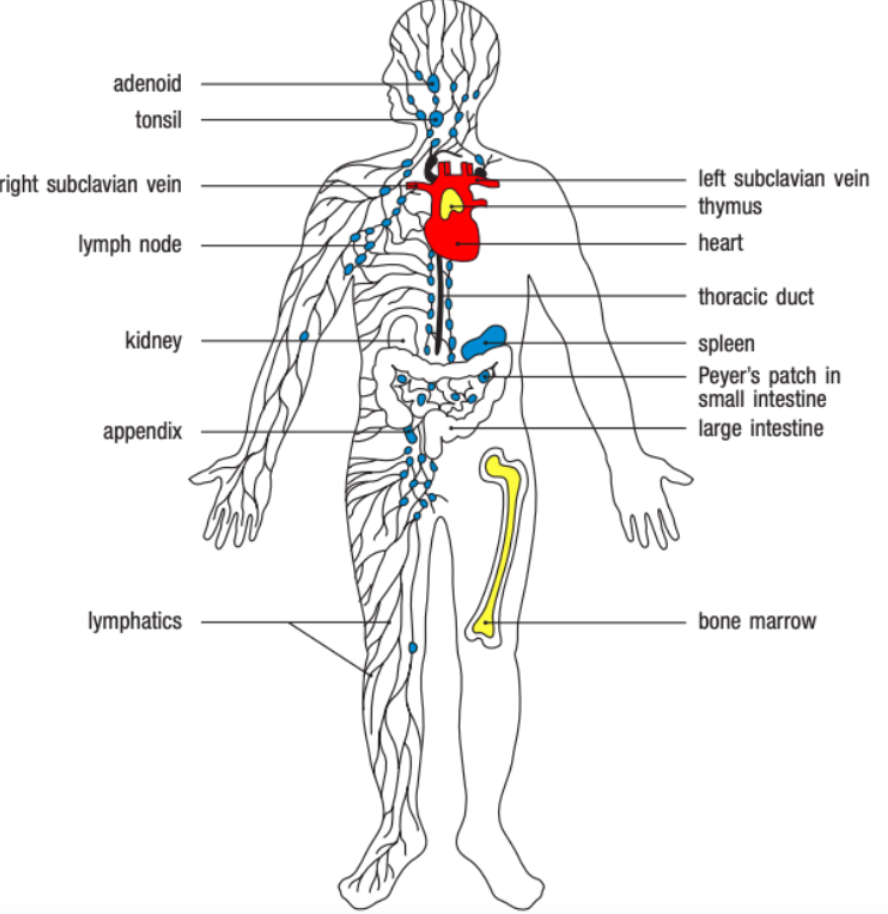
What is the role of primary lymphoid organs?
Primary lymphoid organs are where immune cells develop. Examples include the bone marrow and thymus.
What is the role of secondary lymphoid organs?
Secondary lymphoid organs facilitate immune responses by housing immune cells.
Spleen
Skin and mucosal tissue draininglymph nodes
Peyer Patches
Why is it important to separate primary and secondary lymphoid organs?
Separation ensures continuous production of new immune cells.
Prevents interference from active immune responses.
Maintains balance between immune cell development and immune defense.
What is the function of the spleen in the immune system?
Filters blood-borne pathogens, purifying blood and initiating immune responses against blood infections.
What role do skin and mucosal tissue draining lymph nodes play?
Filter interstitial fluids similar to the spleen’s filtration of blood.
Capture antigens from the skin or mucosal surfaces and facilitate a local immune response.
What is the difference between peripheral lymph nodes and mucosal lymph nodes?
Peripheral lymph nodes are associated with skin drainage
While mucosal lymph nodes are located near mucosal areas, such as the intestines, genital tract, and airways.
What are Peyer patches, and where are they located?
Are small lymphoid structures in the intestine responsible for generating antibody responses to manage commensal microbes.
Which organs contain organized immune cell populations besides the spleen and lymph nodes?
The peritoneal cavity and the liver also contain organized immune cell populations that contribute to immune responses.
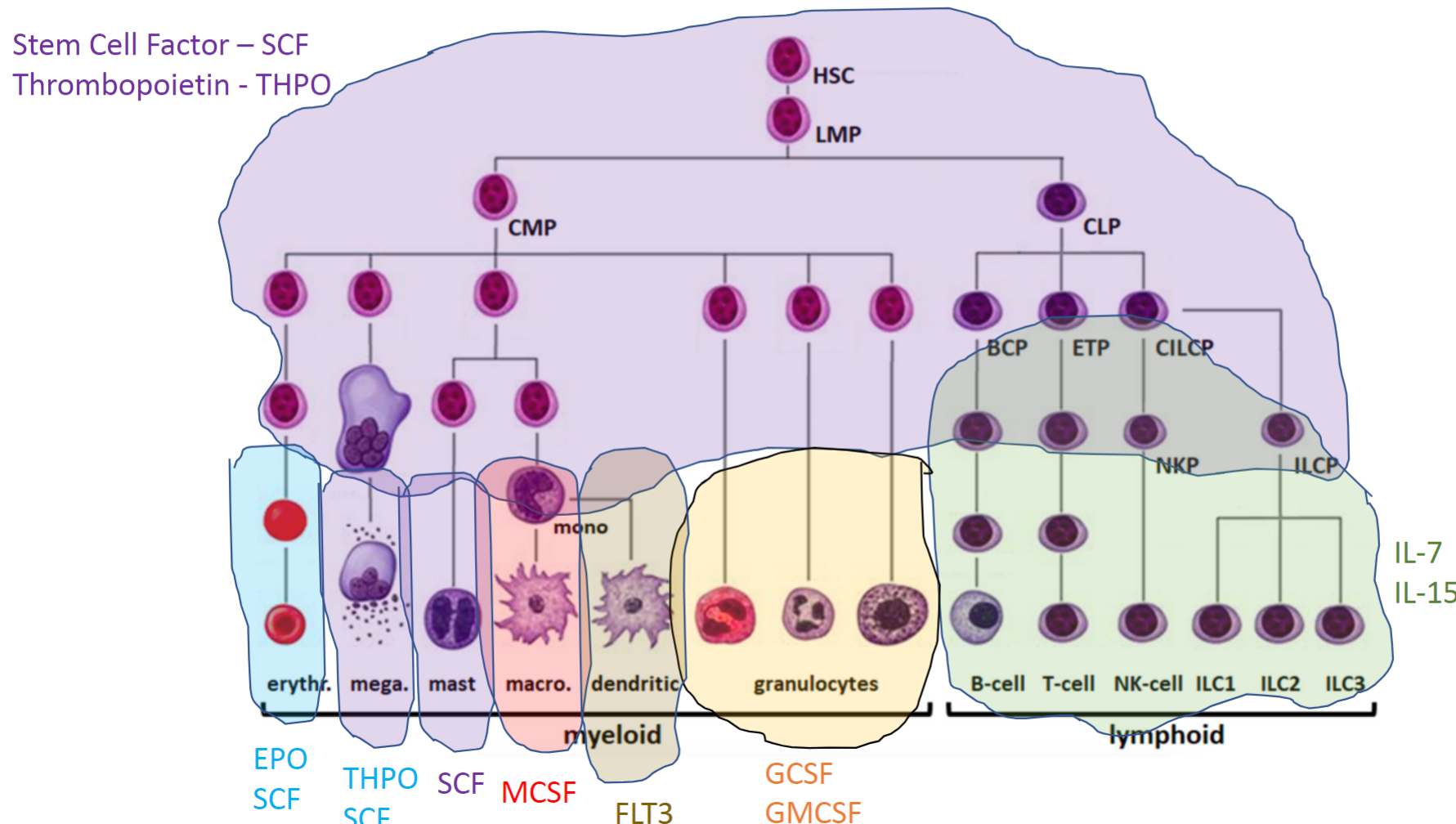
Describe the lineage and properties of hematopoietic stem cells (HSC) and their differentiation in the bone marrow.
HSCs in bone marrow give rise to immune cells, red blood cells, and megakaryocytes (for platelets).
T cells mature in the thymus, but all other immune cells start from HSCs.
HSCs are unique for their ability to self-renew and differentiate into various blood cell types.
Mostly quiescent, HSCs slowly divide to form progenitors with specific differentiation potential.
HSCs sit at the top of the differentiation hierarchy, leading to specialized cells in both myeloid and lymphoid lineages.
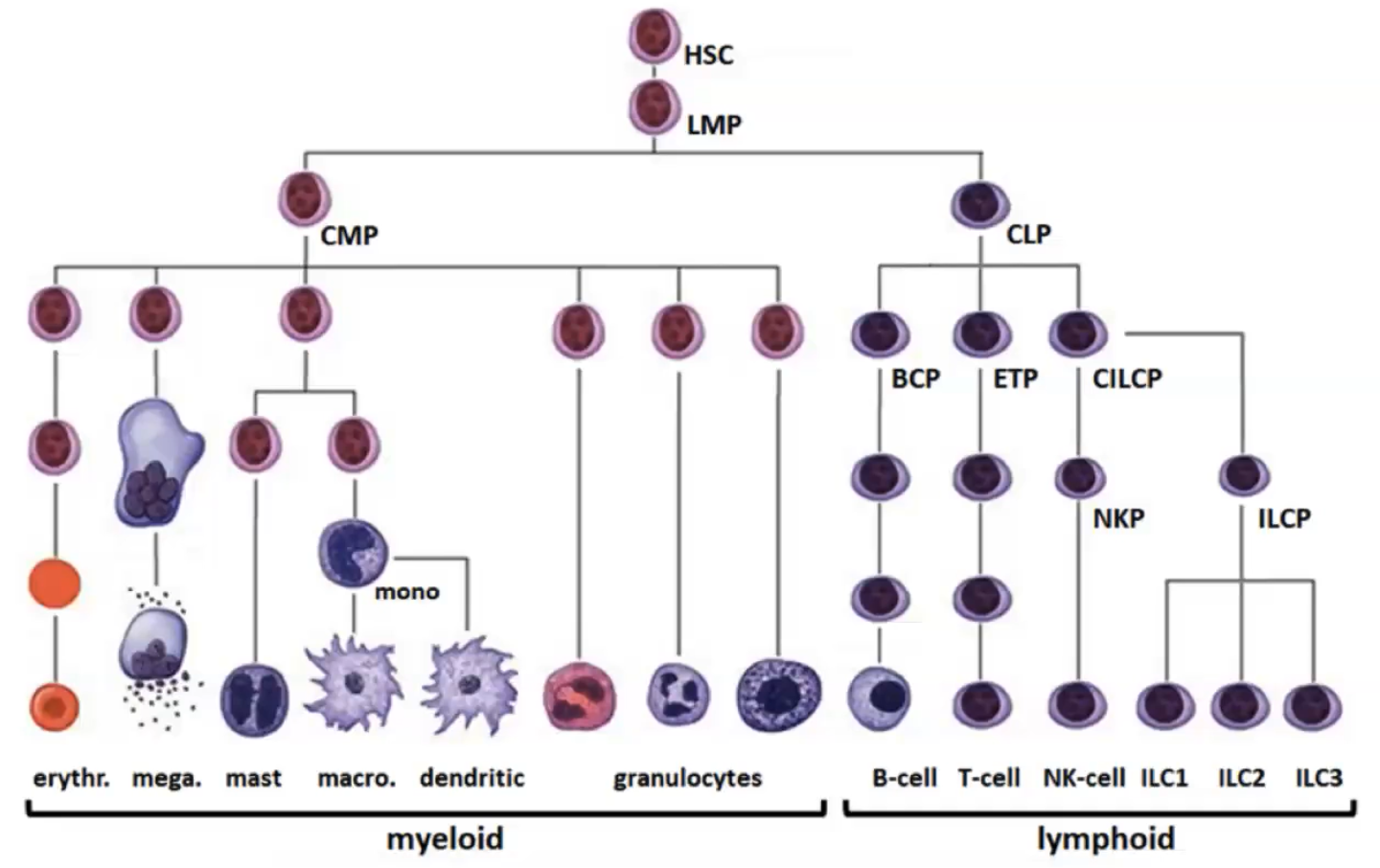
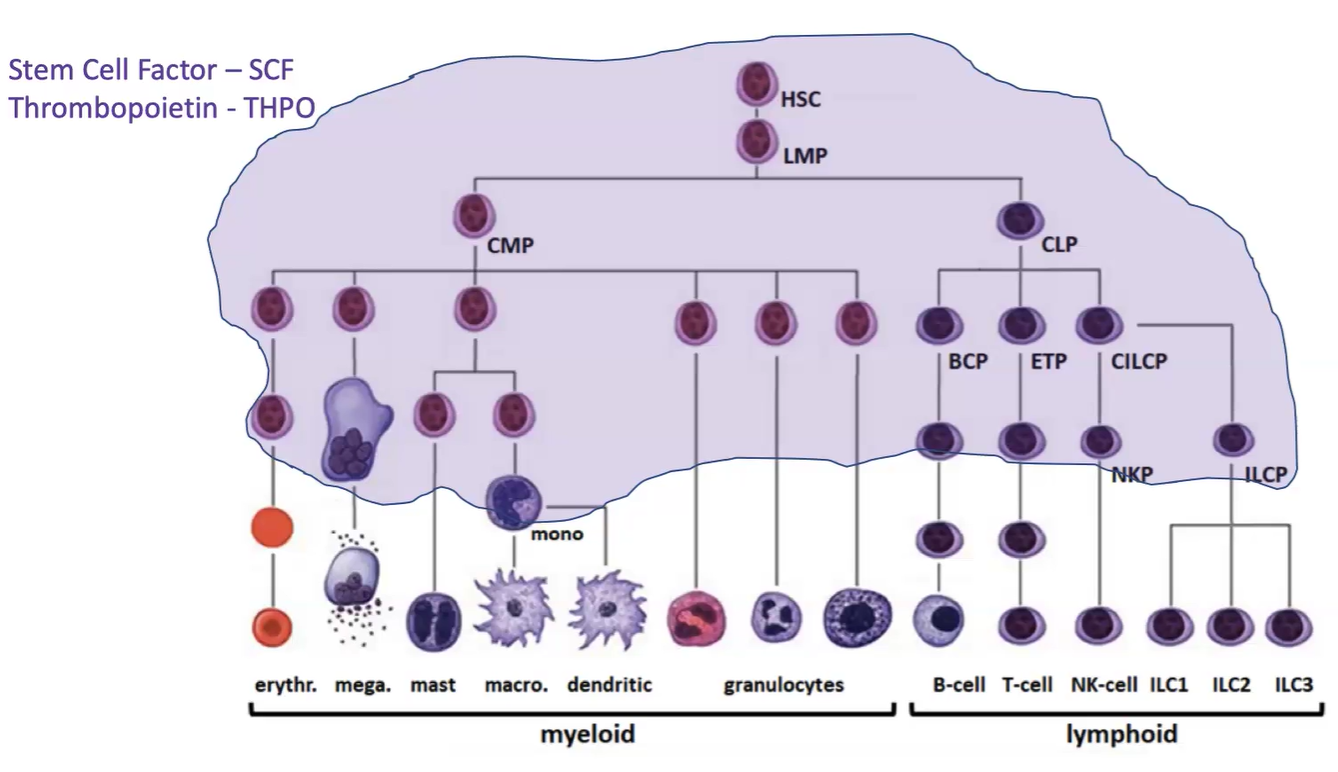
How does a cell decide which lineage to differentiate into within the hematopoietic tree?
Differentiation relies on cytokines and growth factors.
Key factors SCF and THPO support survival and proliferation of HSCs and early progenitors.
Further down the differentiation path, specialized cytokines drive myeloid or lymphoid lineage development.
For lymphocytes, what key cytokine is needed for their development, and their function?
IL-7; Function: Adaptive immunity, recognizing specific antigens.
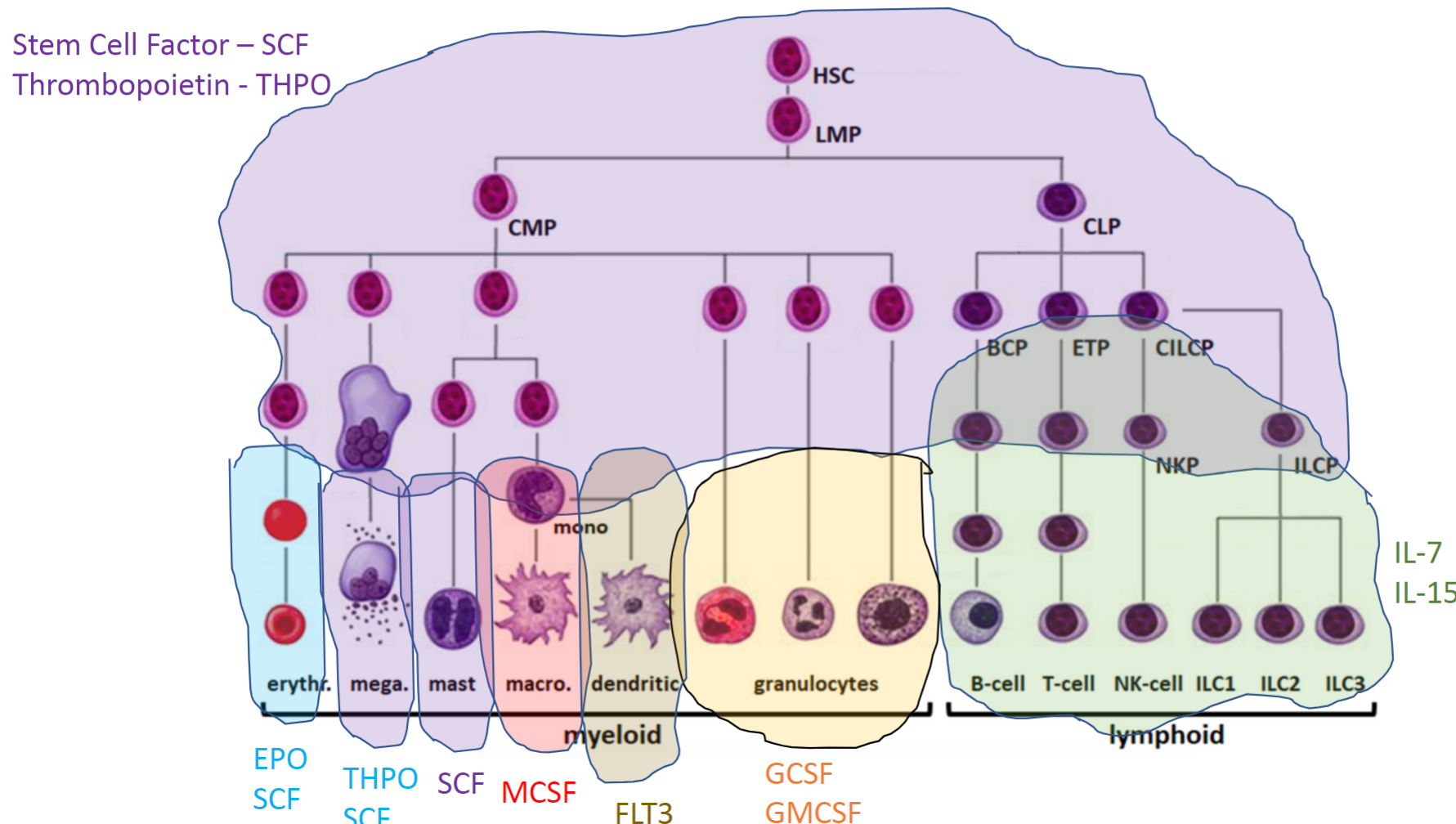
For NK cells, what key cytokine is needed for their development, and their function?
IL-15; Function: Innate immunity, targeting virus-infected and cancer cells.
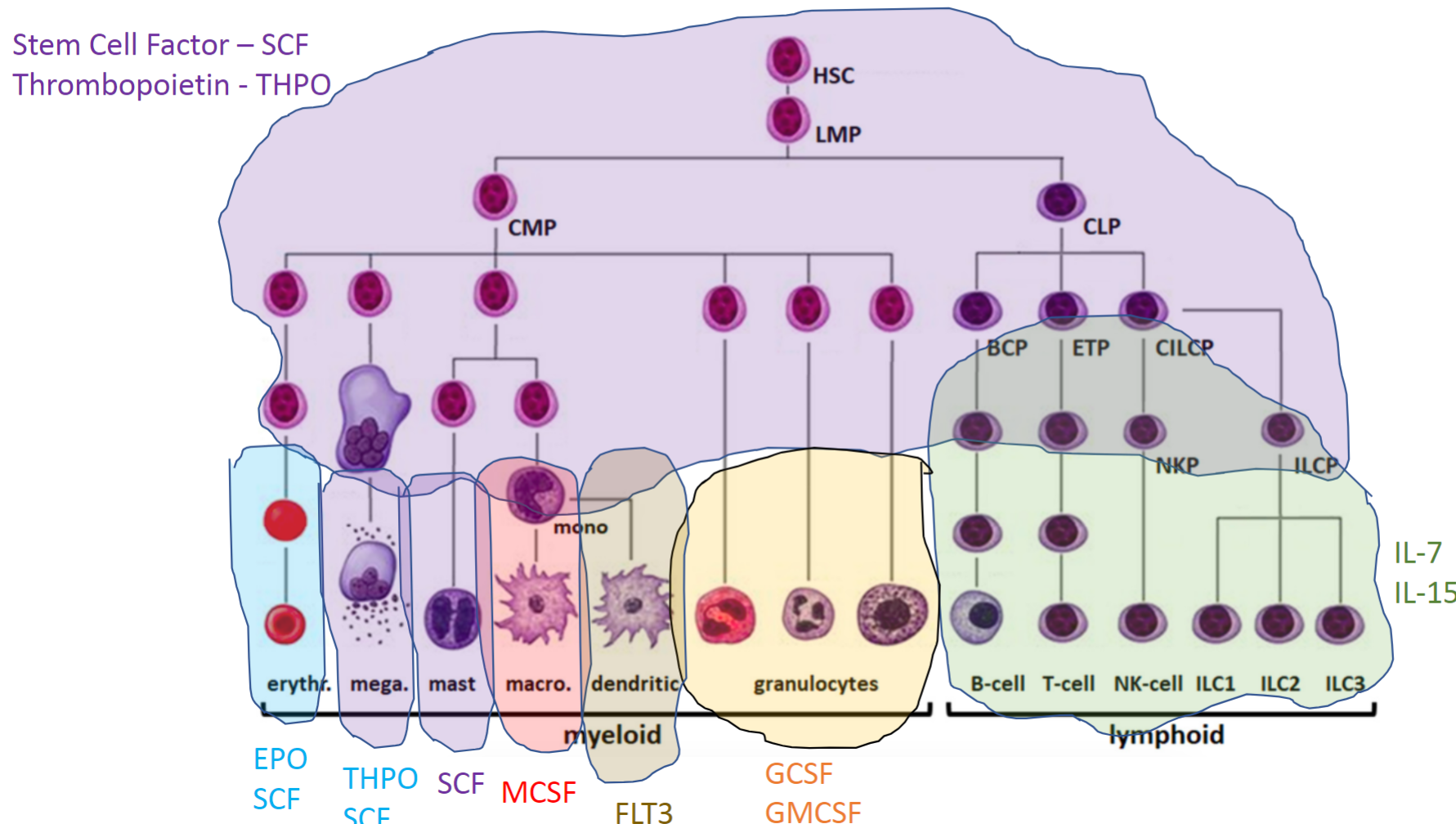
For granulocytes, what key cytokines are needed for their development, and their function?
GCSF and GMCSF; Function: Innate immunity, responding to infections and inflammation.
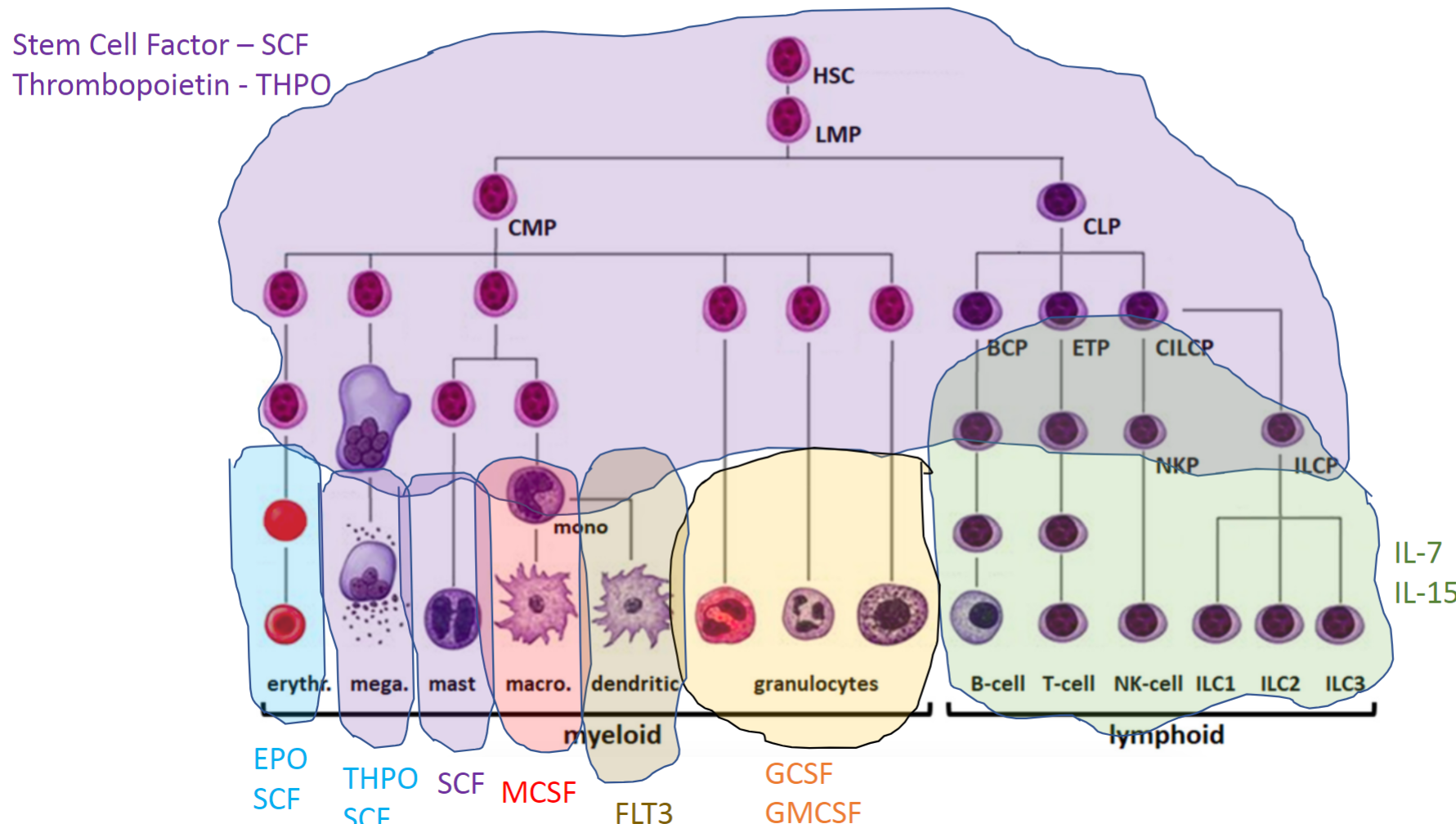
For dendritic cells, what key cytokine is needed for their development, and their function?
FLT3; Function: Antigen presentation, initiating immune responses by activating T cells.
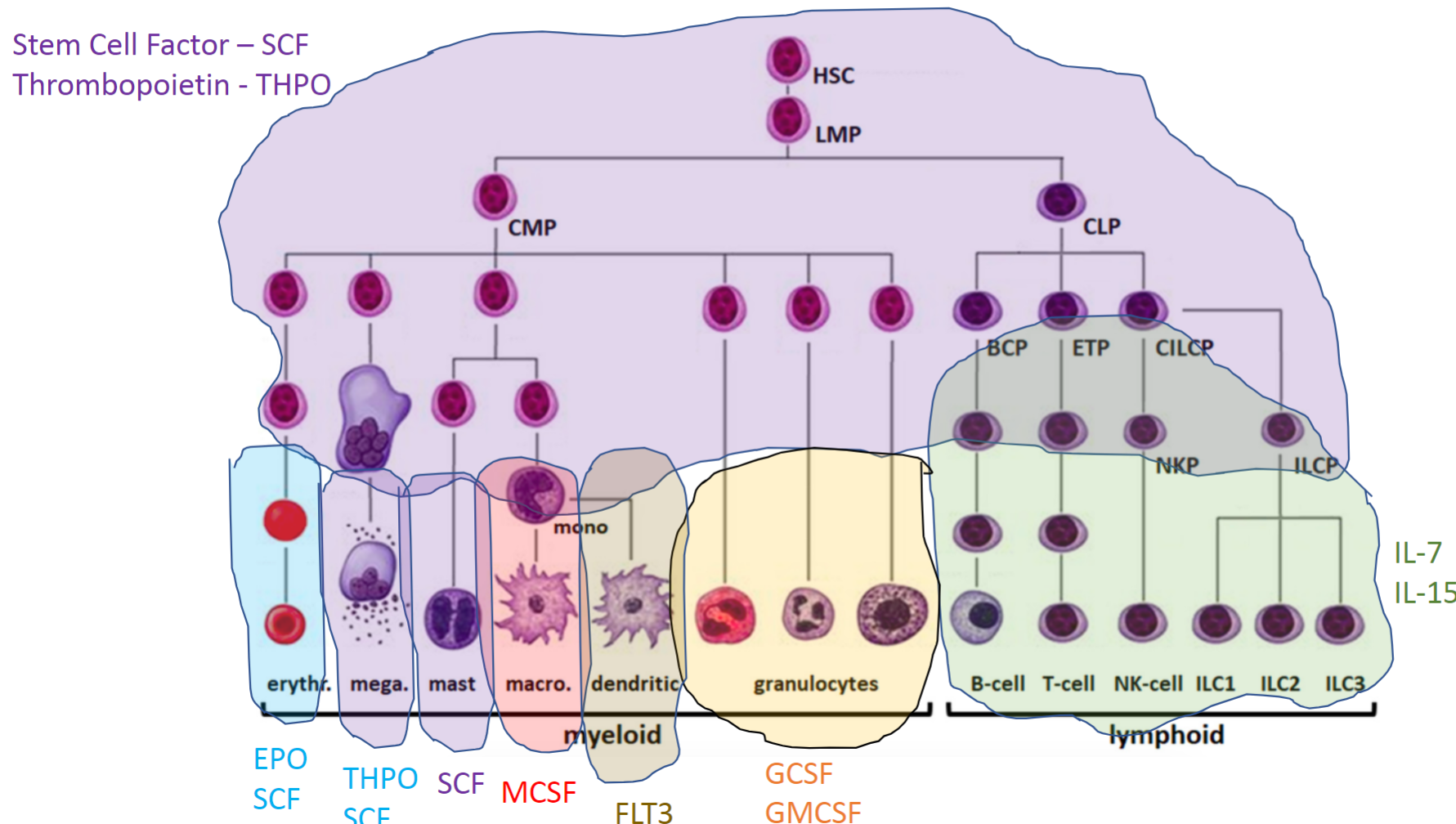
For monocytes and macrophages, what key cytokine is needed for their development, and their function?
MCSF; Function: Phagocytosis, tissue repair, and immune modulation.
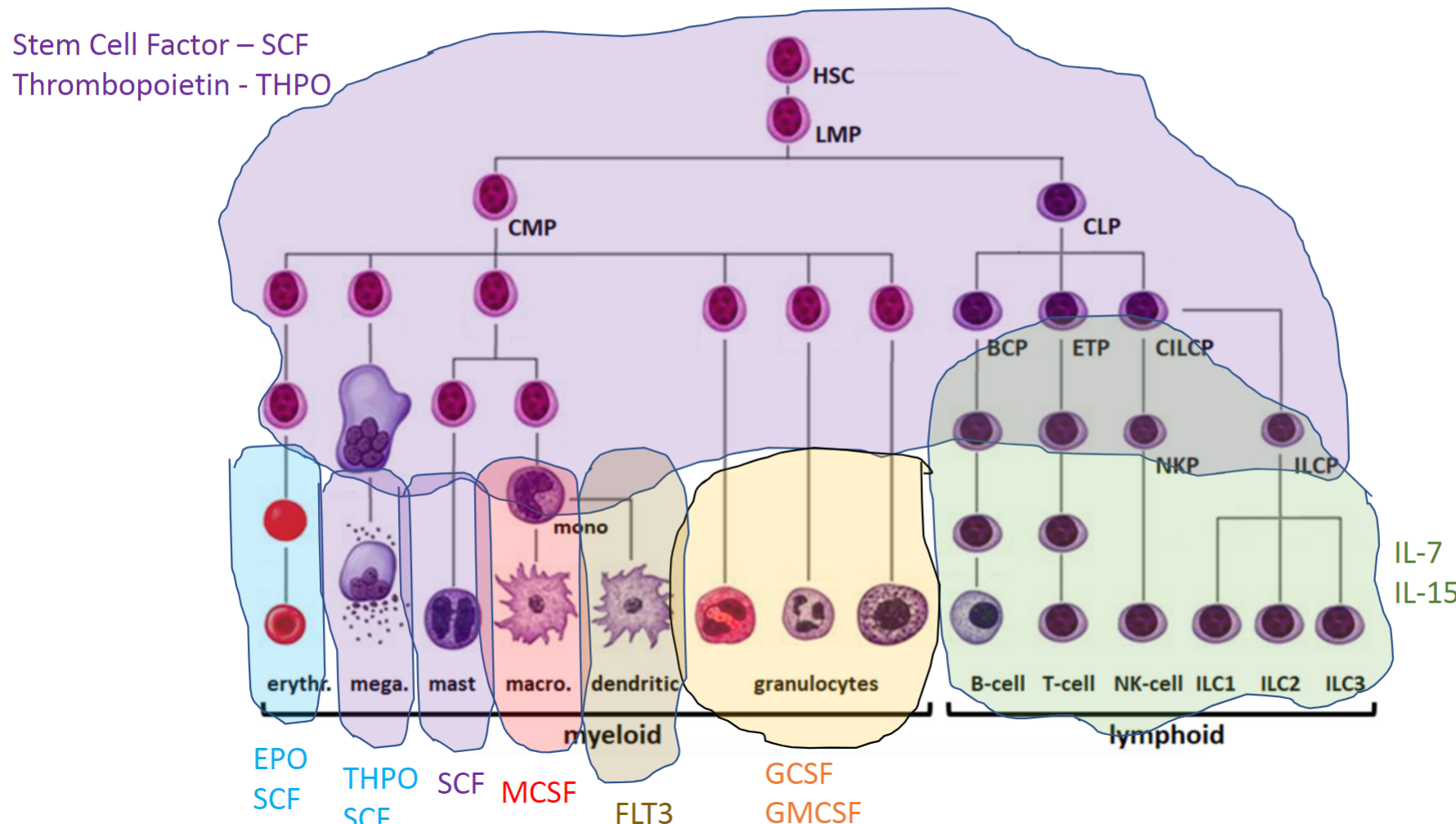
For mast cells, what key cytokine is needed for their development, and their function?
SCF; Function: Release of histamine and other mediators in response to allergens.
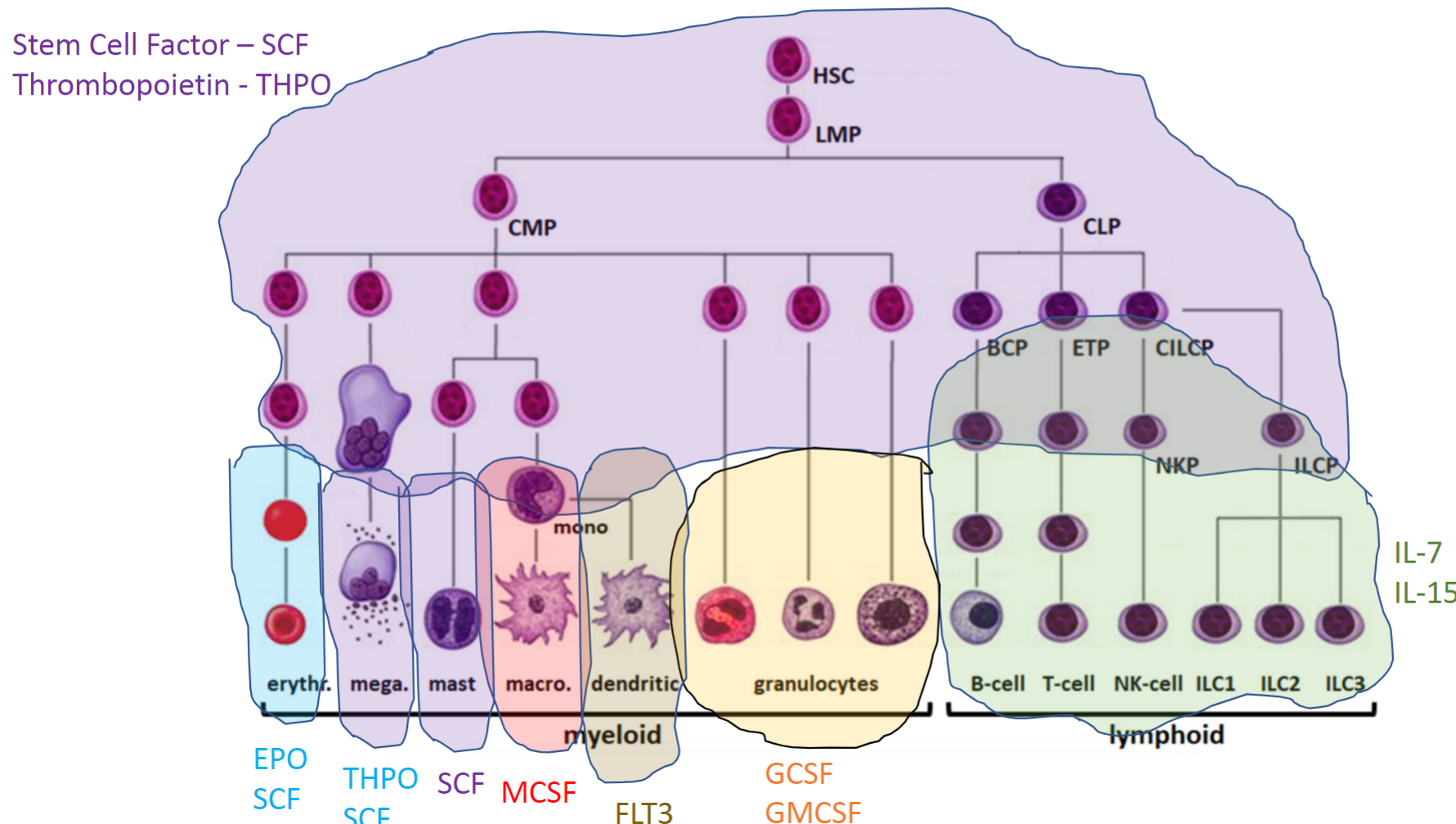
For megakaryocytes, what key cytokines are needed for their development, and their function?
THPO and SCF; Function: Platelet production for blood clotting.
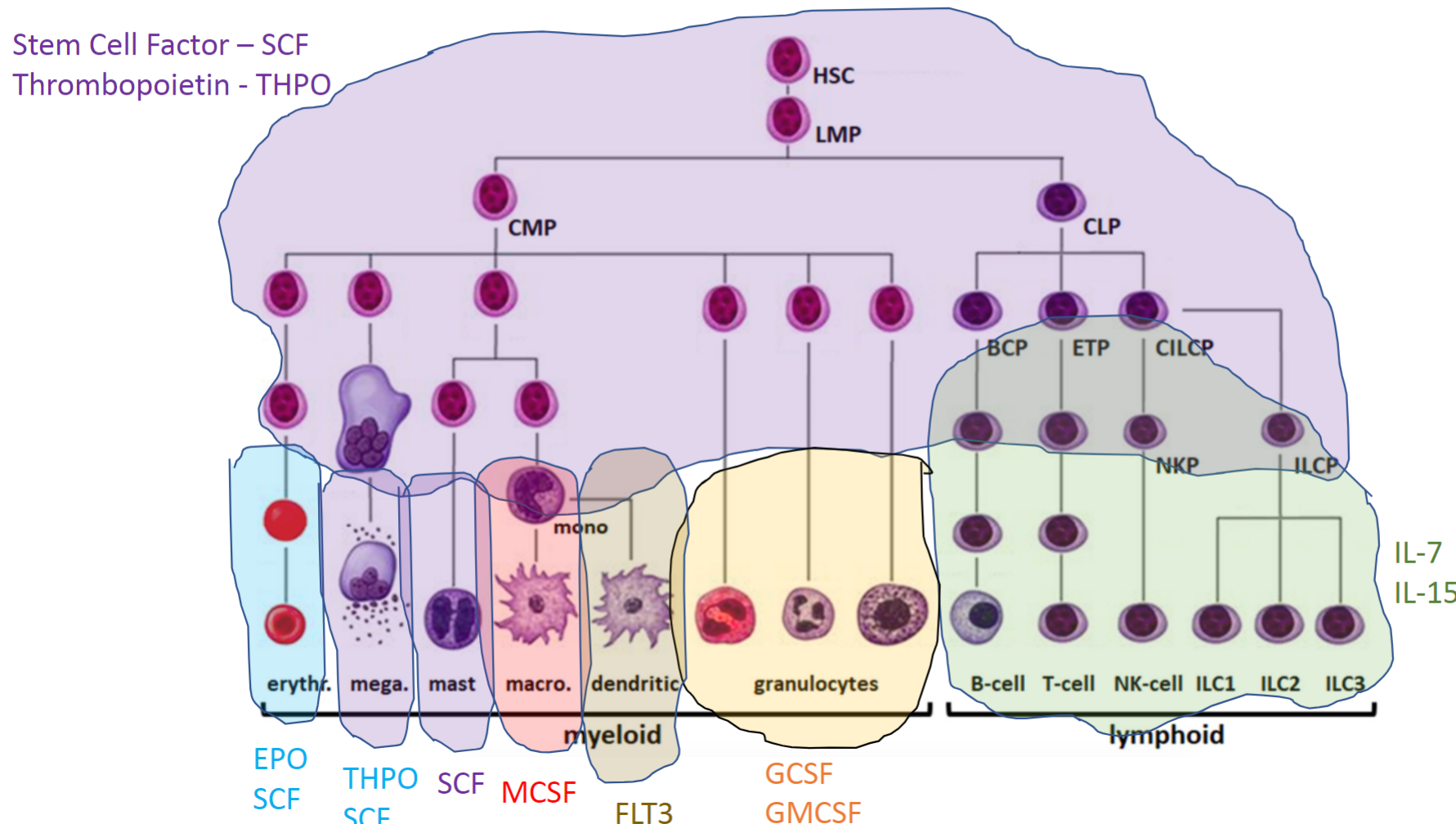
For erythrocytes, what key cytokines are needed for their development, and their function?
EPO and SCF; Function: Oxygen transport in the blood.
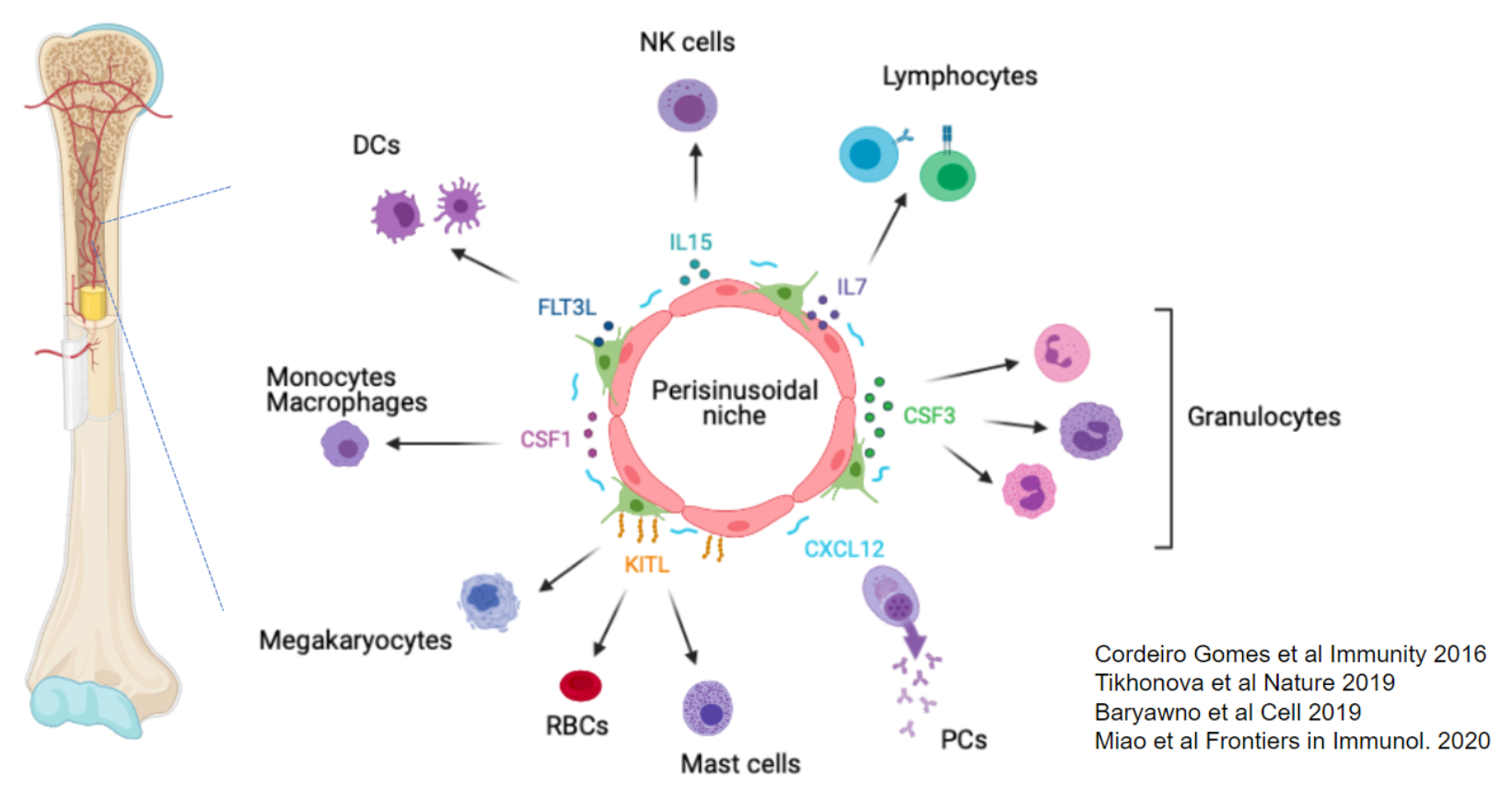
What types of cells and structures support hematopoiesis in the bone marrow, and what are their roles?
In the bone marrow, hematopoiesis is supported by a variety of cells and structures:
Mesenchymal Stem Cells (MSCs): Give rise to osteoblasts, fibroblasts, and cartilage; fundamental source for stem cell factor.
Osteoblasts: Bone-producing cells that help maintain the bone structure.
Adipocytes: Found abundantly in human bone marrow (but not in mice), providing structural and metabolic support.
Chondrocytes: Cartilage cells that contribute to the bone marrow environment.
Vascularization: The bone marrow is highly vascularized, allowing for the transport of nutrients and cells.
All hematopoietic cells, except T cells, develop in this niche.
What is a key function of mesenchymal stem cells (MSCs) in the bone marrow?
MSCs produce key cytokines, especially SCF, which supports HSC survival and proliferation in the bone marrow.
How does CXCL12 function as a "ZIP code" for SCF in the bone marrow?
CXCL12, produced alongside SCF in the bone marrow, attracts immune cells via GPCRs.
This co-expression directs immune cells to SCF-rich regions, promoting development and migration.
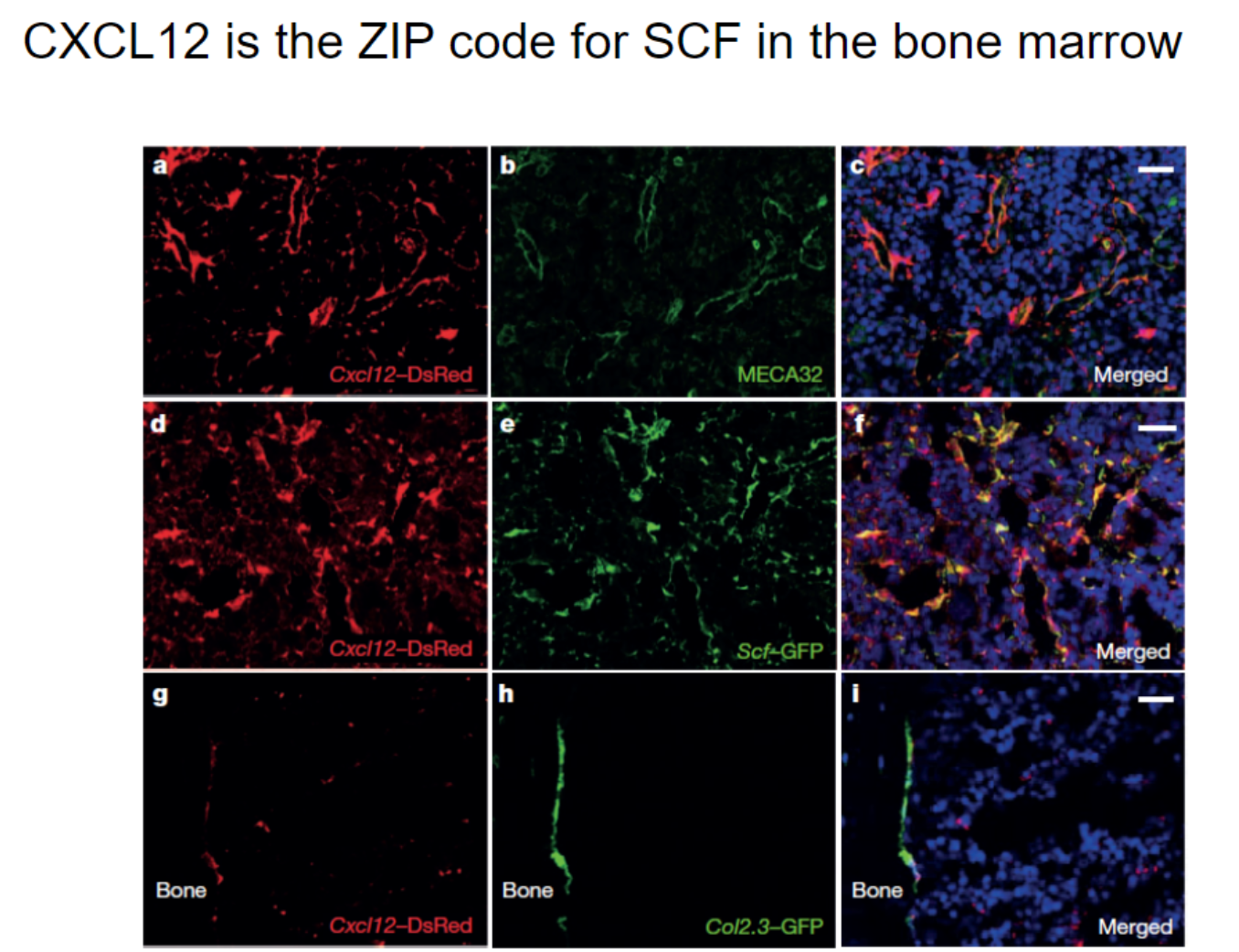
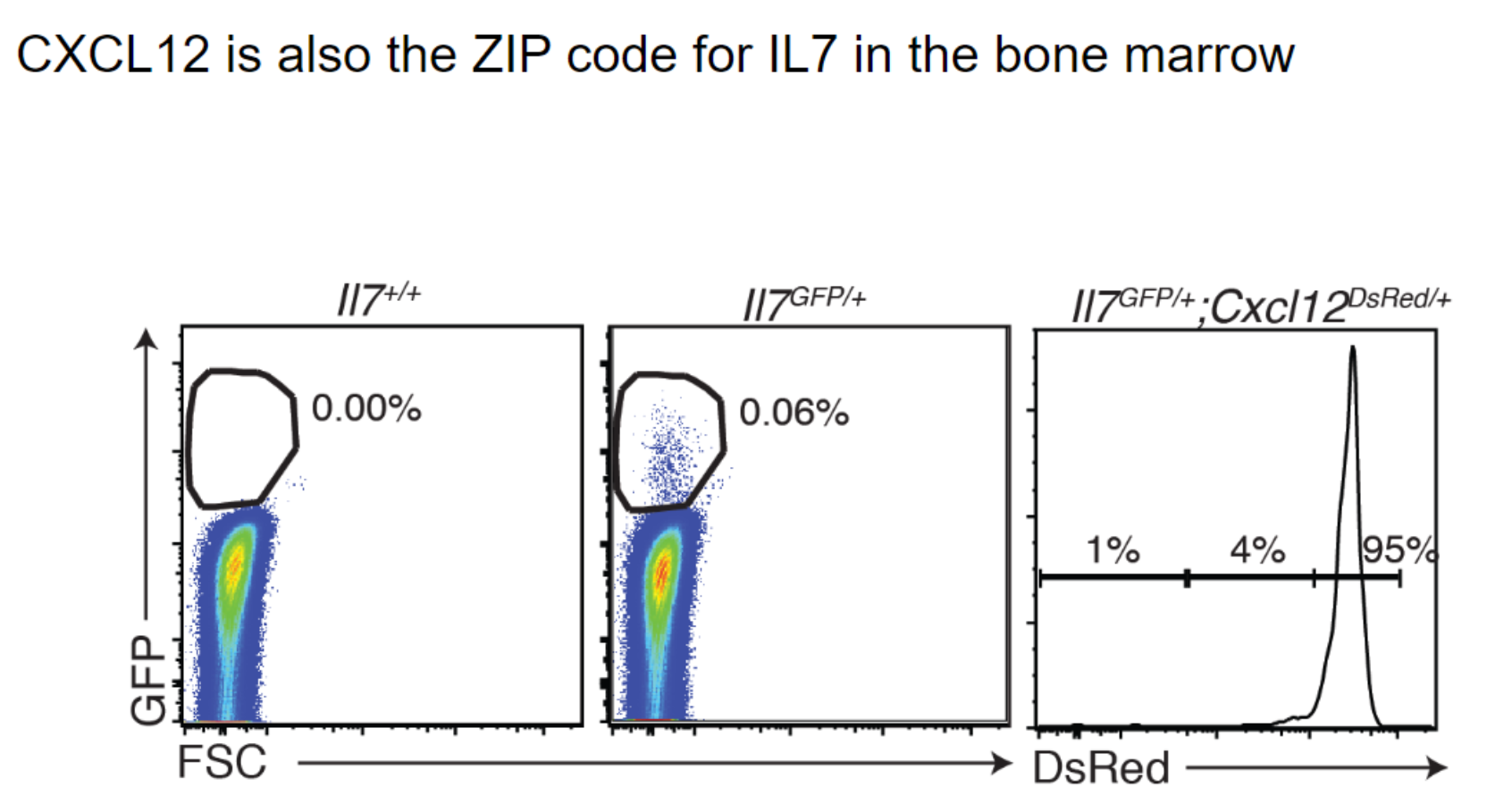
What is the relationship between CXCL12 and IL-7 production in the bone marrow?
Cells producing CXCL12 also produce IL-7, essential for immune cell development.
Mesenchymal stem cells (MSCs) in the bone marrow are key sources of both SCF and IL-7.
This dual production underscores MSCs' crucial role in supporting immune cell development.
How does the bone marrow niche support hematopoiesis, and what is the role of CXCL12?
Bone Marrow Niche: Supported by MSCs and endothelial cells, providing essential cytokines for immune cell generation.
Central Cytokine Location: Ensures HSCs and progenitors encounter necessary signals in one spot, forming “islands” of hematopoiesis.
CXCL12 Role: Produced locally to retain HSCs in the bone marrow through its receptor, CXCR4.
CXCR4 Inhibition: Mobilizes HSCs into the bloodstream for easier collection, aiding bone marrow transplants without extraction.
What is the function of CXCR4 inhibitors in hematopoietic stem cell (HSC) collection?
CXCR4 Inhibitors: Prevent HSCs from staying in bone marrow, mobilizing them into the bloodstream.
New Collection Method: Oral CXCR4 inhibitors release HSCs into blood, replacing needle-based bone marrow extraction.
Blood Collection: HSCs can now be collected via a blood draw, then purified for bone marrow transplants.
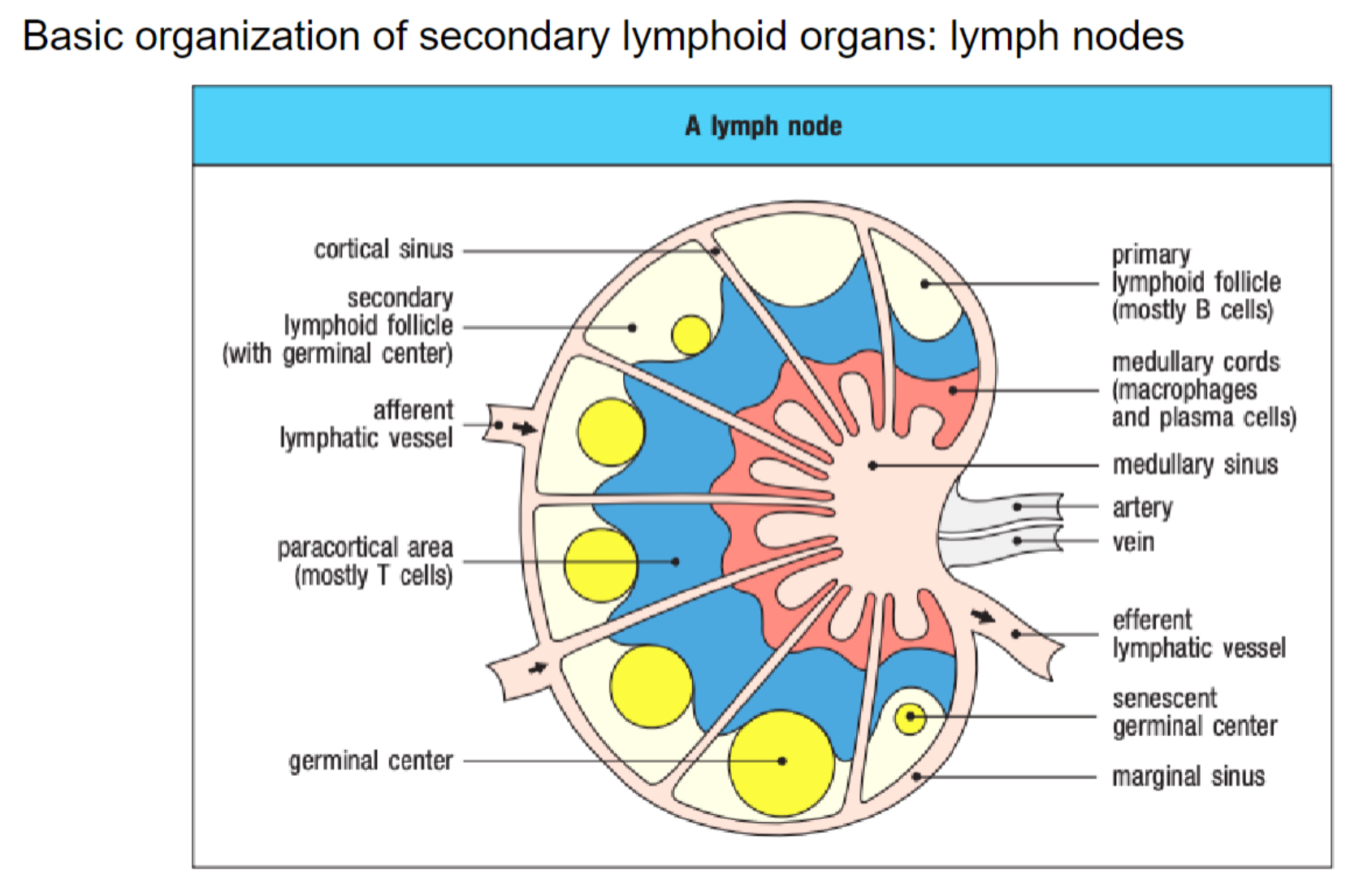
What is the basic structure of a lymph node and its role in immune response?
Lymph Nodes: Filter interstitial fluid from lymphatic system, brought in through afferent lymphatic vessels.
Antigen Encounter Zones: Channels direct fluid to areas for immune cell-antigen interaction.
B Cells: Found in outer follicles; form germinal centers upon antigen recognition.
T Cells: Localize in the paracortical area, separated from B cells.
Antigen Capture: Trapped in lymph nodes for immune cell recognition; macrophages near the efferent vessel capture any remaining antigens before fluid exits.
Immune Cell Entry: T and B cells enter lymph nodes via blood circulation.
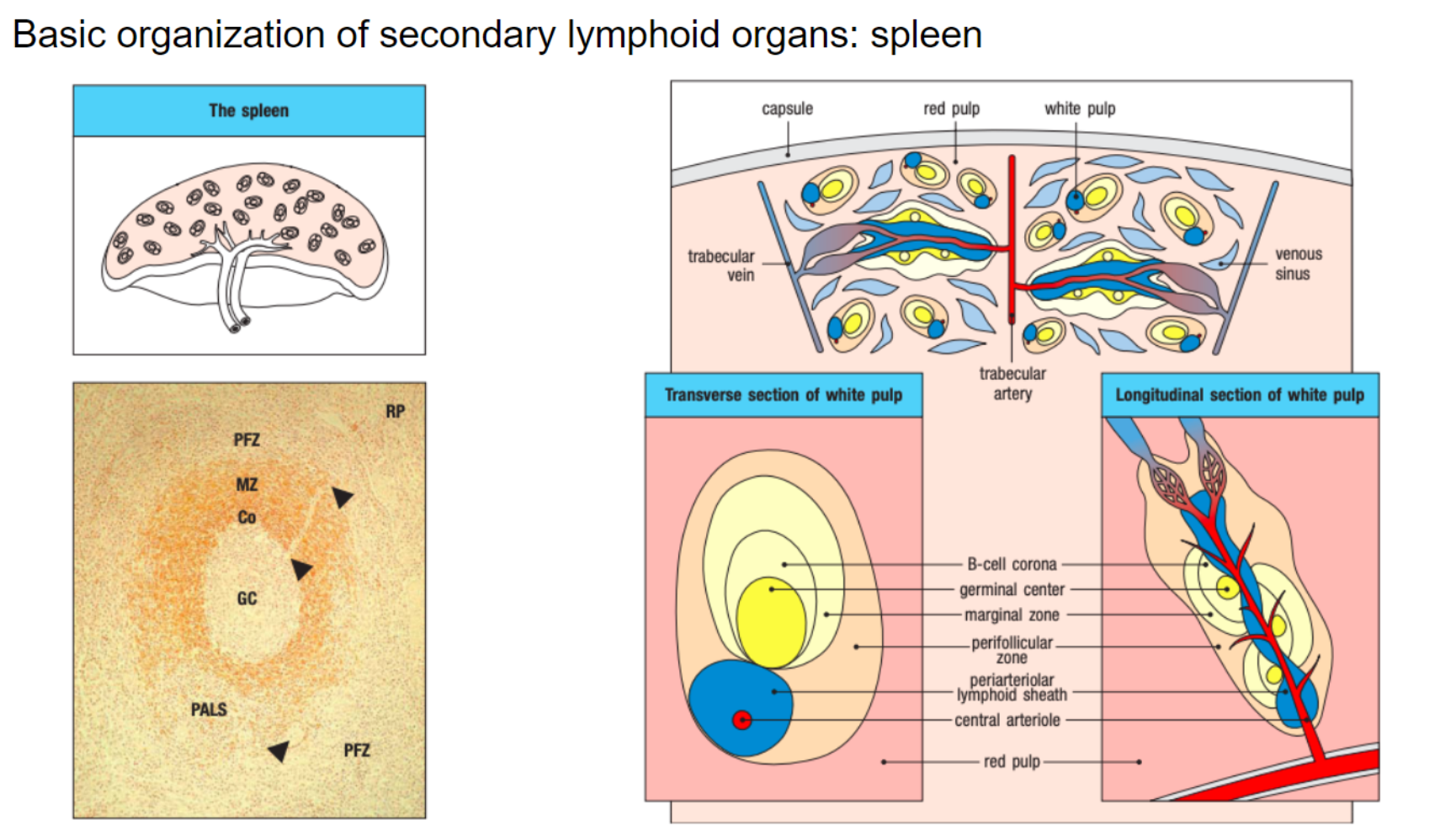
What is the structure of the spleen and its primary function?
Spleen Structure: Divided into red pulp (rich in red blood cells) and white pulp (houses B and T cells).
Function: Filters blood entering through the splenic artery.
Blood Vessel Structure: Open-ended vessels increase risk of internal bleeding if ruptured.
Antigen Sampling: Macrophages in red pulp sample antigens and act as a barrier to the white pulp.
B Cell Concentration: B cells in follicles of the white pulp capture remaining antigens.
What are the key functions and learning goals for understanding immune system organs?
The immune system develops in primary lymphoid organs (bone marrow and thymus) from hematopoietic stem cells through hematopoiesis.
Specific cytokines and growth factors in bone marrow niches support lymphoid and myeloid cell development.
Peripheral lymph nodes filter fluids from skin and muscle, while mucosal lymph nodes filter fluids from mucosal sites (e.g., intestine, airways).
The spleen filters antigens in the blood.
Secondary lymphoid organs have distinct immune cell zones for efficient antigen capture and immune responses.