NURS 344 (Health Assessment): Assessing Mental Status Including Risk for Substance Abuse
1/167
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
168 Terms
Mental Status
Refers to level of cognitive functioning (thinking, knowledge, problem solving) and emotional functioning (feelings, mood, behaviors, stability).
Mental Health
A state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community.
What components contribute to disorders?
Environmental, psychological, genetic, chemical, social, or other factors
Nurse's Role in Mental Health
Assess and screen for past and present mental health conditions
Involves observation, communication, administering questionnaires or assisting client to complete self-assessment questionnaires
Determine if need for referral to another health care professional
What factors affect mental health?
Economic and social factors
Unhealthy lifestyle choices
Exposure to violence
Personality factors
Spiritual factors
Cultural factors
Psychosocial developmental level and issues
Changes or impairments in the structure and function of the neurologic system
Substance Abuse
Excessive use or dependence on an addictive substance or drug that leads to social, physical, emotional, and job-related problems. It's also one of the most persistent conditions
How can mental health disorders be considered psychosomatic?
Psychological stress or emotional distress directly contributes to the development or worsening of physical symptoms in the body
EX: Panic attacks caused by anxiety that cause elevated HR and feeling of heart attack; stress causing the release of cortisol
Because THC overactivates certain brain cell receptors, what effects can it cause?
Altered senses
Changes in mood
Impaired body movement
Difficulty with thinking and problem solving
Impaired memory and learning
How is mental status assessed?
Assessment of mental status is accomplished by interviewing the client and observing their behaviors. Important verbal and behavioral clues about mental status can be assessed from the very outset and throughout the entire duration of your interaction with the client.
Mental Status Assessment (Subjective Data)
Biographical: Name, address, and telephone number; age, DOB, gender identity, martial status, educational level, employment
History of present health concern
Personal health history
Family history
Lifestyle and health practices
For a subjective mental status assessment, what are some things to ask about in regard to present health concerns?
What is your most urgent health concern at this time? Why are you seeking health care? Are you experiencing any other health problems?
Presence of headaches, trouble breathing, heart palpitations, insomnia, irritability or mood swings, suicidal thoughts, auditory or visual hallucinations
For a subjective mental status assessment, what are some things to ask about in regard to present health history?
Have you ever received medical treatment or hospitalization for a mental health problem or received any type of counseling services? Please explain.
Have you ever had any type of head injury, meningitis, encephalitis, or stroke?
What changes did you notice as a result of these?
Have you ever served on active duty in the armed forces? Explain.
Have you ever had any type of head injury, meningitis, encephalitis, or stroke? What changes did you notice as a result of these?
For a subjective mental status assessment, what are some things to ask about in regard to family history?
Is there a history of mental health problems (anxiety, depression, bipolar disorder, and schizophrenia) or Alzheimer disease in your family? How were they treated? Was the treatment effective?
For a subjective mental status assessment, what are some things to ask about in regard to lifestyle and health practices?
Describe a typical day. Does your present health concern affect your ADLs? Describe your energy level.
Sleep patterns, eating habits, daily bowel elimination, drinking caffeinated beverages, any medications, use of opioids, alcohol and drug use, medical marijuana use, stressors, family relationships
What are some psychiatric disorders that have a genetic or familial connection?
Anxiety, depression, bipolar disorder and/or schizophrenia, or Alzheimer disease.
Why is it important to inquire about a patient's past medical treatment for mental health problems?
Some clients may have had a positive or a negative past experience with mental health care services or counseling that may influence their decision to seek help in this area again.
A past hospitalization for mental health may indicate a more serious problem than if the client received outpatient services. Some mental health disorders may recur or symptoms may intensify. Clients who have experienced depression are at greater risk for dementia later in life
How does a patient providing biological data help assess their mental status? Examples of biological data are name, address, birthdate, etc.
Their answers provide baseline data about the client's level of consciousness, memory, speech patterns, articulation, or speech defects. Inability to answer these questions may indicate a cognitive/neurologic defect.
Information about age and DOB helps determine a reference point with which the client's psychosocial developmental level and appearance can be compared. Women tend to have a higher incidence of depression and anxiety, whereas men tend to have a higher incidence of substance abuse and psychosocial disorders.
What conditions occur more in men, and what conditions occur more in women?
Women have a higher incidence of depression and anxiety, whereas men tend to have a higher incidence of substance abuse and psychosocial disorders.
Why is it important to collect subjective information about a patient's educational level and employment status when doing a mental assessment?
Clients from higher socioeconomic levels tend to participate in more healthy lifestyles. They are less likely to smoke and more likely to exercise and eat healthfully. Healthy lifestyles may influence one's ability to more effectively cope with mental disorders.
SBIRT (Screening, Brief Intervention, and Referral to Treatment)
Tool to identify, reduce, and prevent problematic use, abuse, and dependence on alcohol and illicit drugs. This is the most current recommended tool to use when substance abuse is suspected.
The tool is designed for use by physicians, other health workers, and mental health professionals and can be used with clients 12 years of age and older.
CAGE Self-Assessment Tool
Tool to detect alcohol dependence in trauma center populations.
C: Have you ever tried to cut back on your use?
A: Have you ever been annoyed/angered when questioned about your use?
G: Have you ever felt guilt about your use?
E: Have you ever had an eye‐opener to get started in the morning?
What is an essential assessment areas for mental health
Appearance
General behavior
Cognitive function
Memory
Thought processes
Use appropriate questionnaires or tests
What equipment is used for mental status objective assessment?
Pencil and paper
Glasgow Coma Scale
PHQ-2
PHQ-9
Depression Questionnaire
Self-Report Depression Questionnaire
Columbia Suicide Severity Rating Scale (C-SSRS)
PTSD Screen for DSM-5 (PC-PTSD-5)
St. Louis University Mental Status (SLUMS) Assessment Tool
CAGE questionnaire
The Alcohol Use Disorders Identification Test
Clinical Institute Withdrawal Assessment Scale
Patient Health Questionnaire-2 (PHQ-2)
A brief, two-item screening tool used to assess for depression and anhedonia symptoms. It is based on the first two questions of the Patient Health Questionnaire-9 (PHQ-9), a more comprehensive measure of depression.
Over the past two weeks, how often have you felt little interest or pleasure in doing things? (0 = not at all, 3 = nearly every day)
Over the past two weeks, how often have you felt down, depressed, or hopeless? (0 = not at all, 3 = nearly every day)
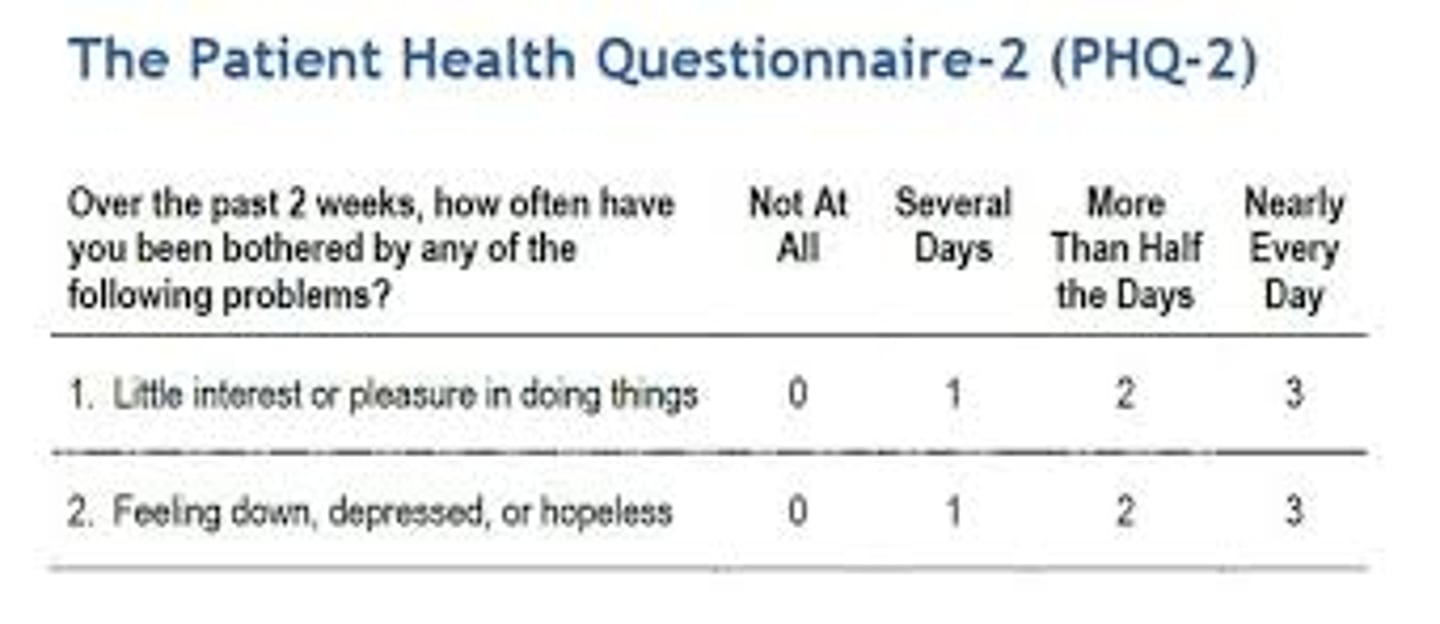
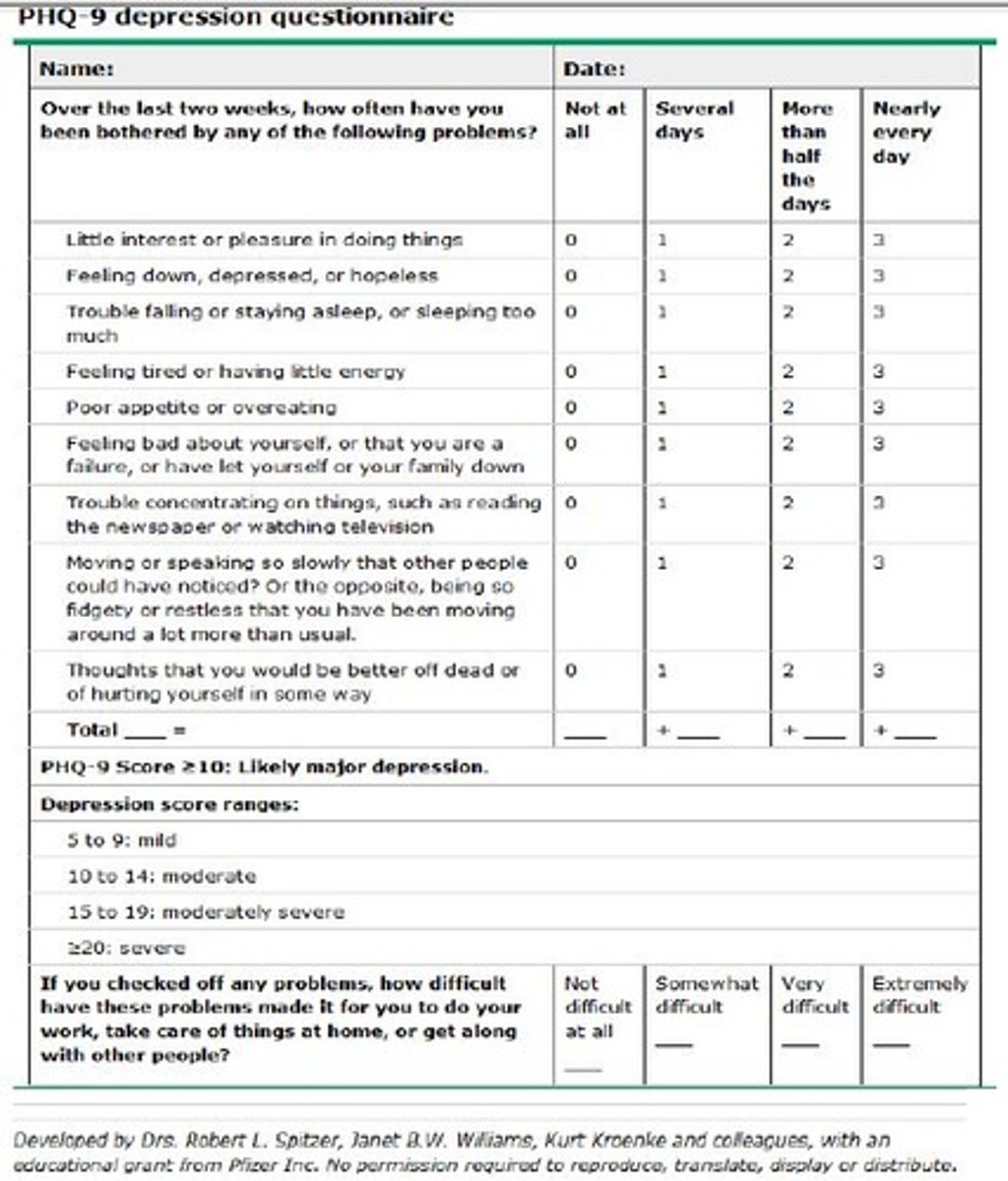
What score indicates abnormal and positive results for the PHQ-2 and PHQ-9?
Using a PHQ-2 threshold score of 2 or higher rather than 3 or higher resulted in more depressed clients being correctly identified.
A PHQ-9 score of 10 or higher appears to detect more depressed clients than the originally described PHQ-9 scoring for major depression
Patient Health Questionnaire (PHQ-9)
A brief 9-item self-report questionnaire used as a screening tool to assess severity of depression; widely used by health care providers, in validity is well established, particularly for identifying severe depression.
Glasgow Coma Scale
A neurological assessment tool used to evaluate a person's level of consciousness after a brain injury. It assesses three key areas: eye opening, verbal response, and motor response.
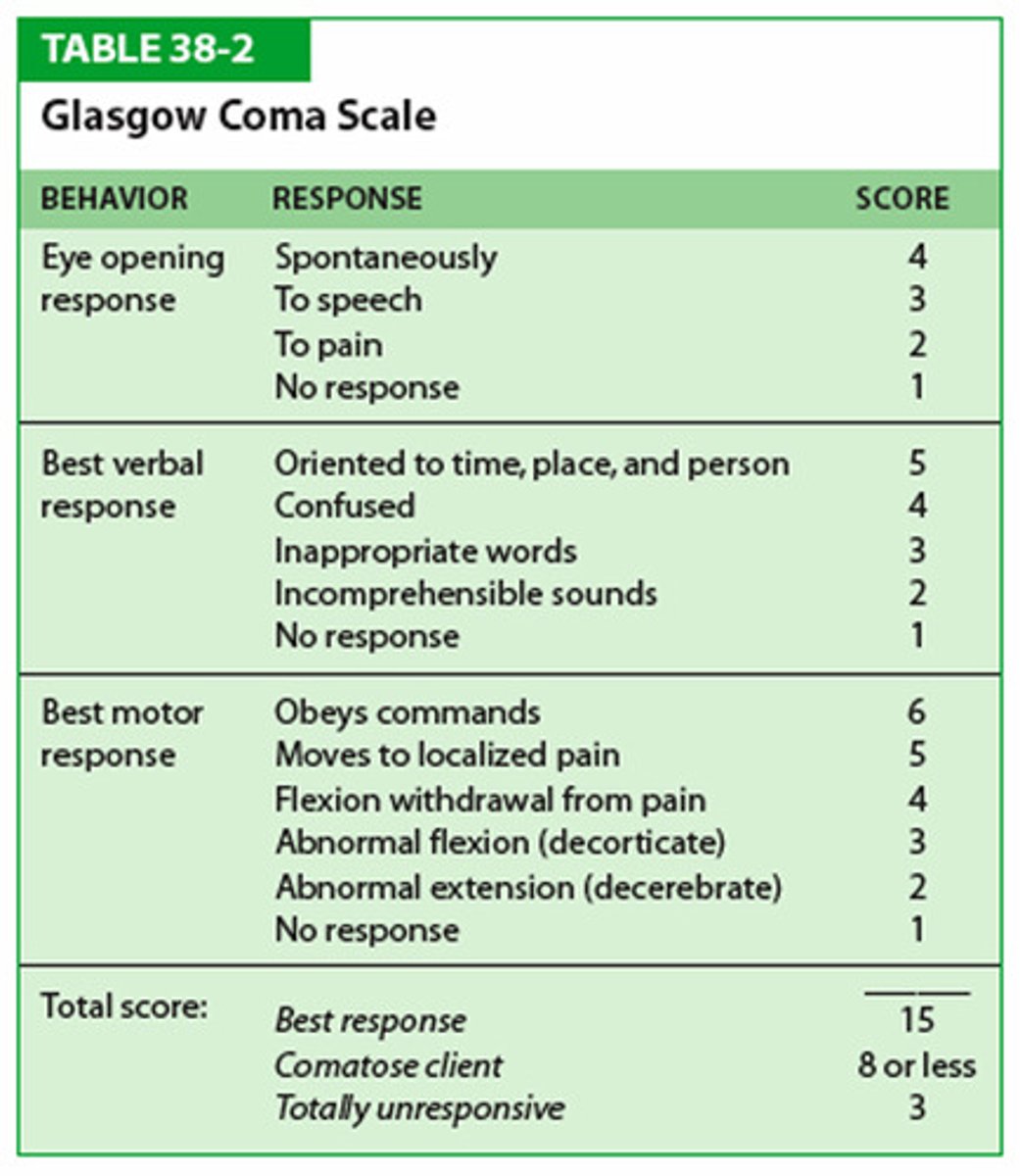
What three areas are assessed by the Glasgow Coma Scale?
Eye opening response
Most appropriate verbal response
Most integral motor response (arm)
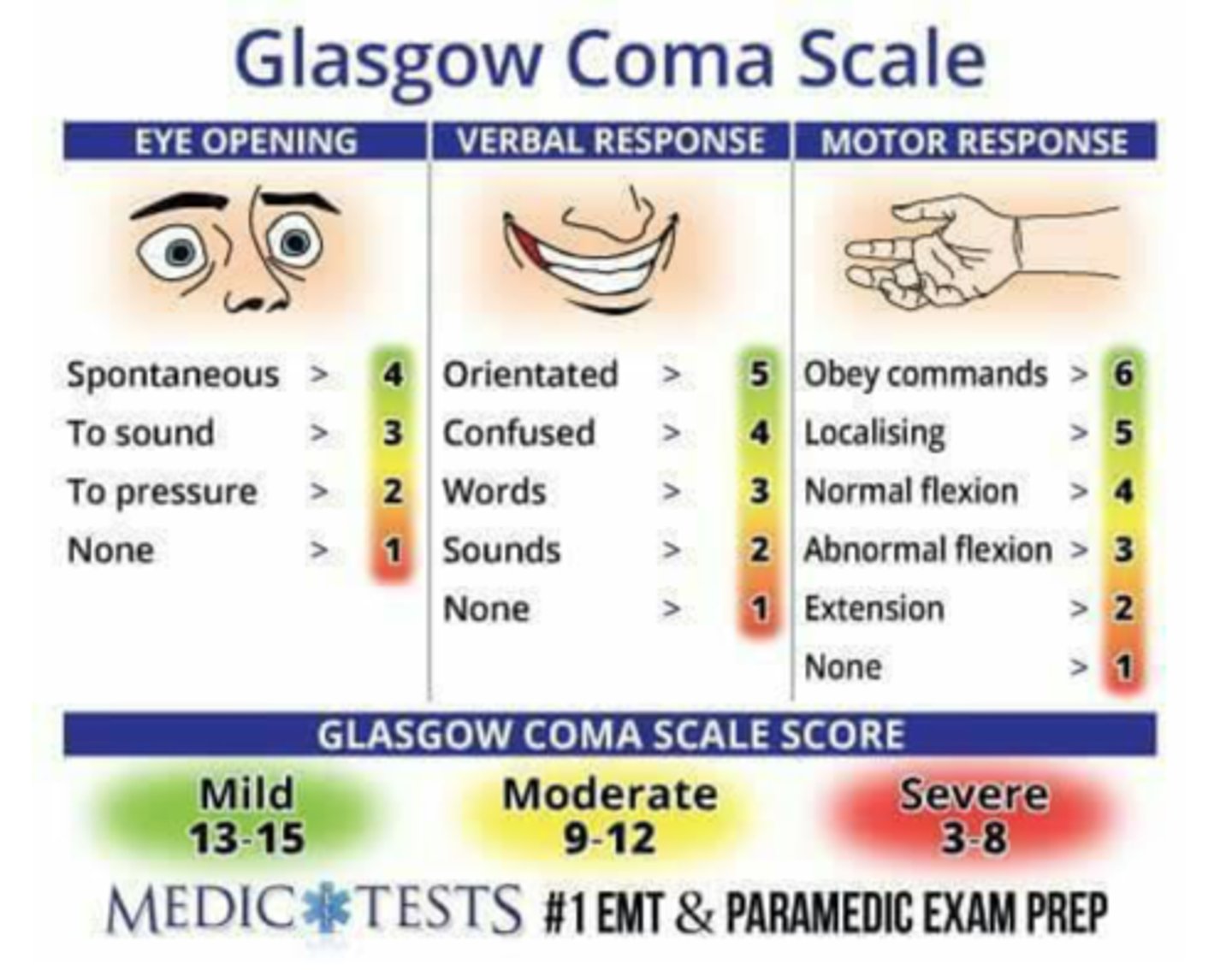
How does scaling work for Glasgow Coma Scale?
The Glasgow Coma Scale is useful for rating one's response to stimuli. The client who scores 10 or lower needs emergency attention. The client with a score of 7 or lower is generally considered to be in a coma.
Glasgow Coma Scale Ratings (3-15)G
High score (13-15): Mild brain injury, no impairment
Moderate score (9-12): Moderate brain injury, significant impairment
Low score (3-8): Severe brain injury, deep coma
Glasgow Score of 3-8 (SEVERE)
Patient is at high risk for respiratory failure due to the patient's inability to maintain their own airway. The priority action of the nurse is to alert the rapid response team so they can intubate the patient. The nurse would also call the health care provider and continue to monitor the client but would not do either of these first because it would delay necessary action.
A nurse performs a Glasgow Coma Scale (GCS) on a hospitalized client. The nurse records a score of 8. What is the priority action of the nurse?
The priority action is to call the rapid response team to intubate patient because they're at high risk for respiratory failure due to the patient's inability to maintain their own airway.
Glasgow Score of 9-12 (MODERATE)
Frequent neurological assessments, monitoring for changes in consciousness, pain management, and consideration for further imaging studies.
Glasgow Score of 13-15 (MILD)
Chapter 6: Assessing Mental Status Including Risk for Substance Abuse - Page 88
Observation for neurological symptoms, cognitive assessment, and management of any associated injuries.
A GCS of 8 places the client at high risk for respiratory failure due to the client's inability to maintain their own airway. The priority action of the nurse is to alert the rapid response team so they can intubate the client. The nurse would also call the health care provider and continue to monitor the client but would not do either of these first because it would delay necessary action. The client needs to be intubated and ventilated, and a mask will not improve the client's condition.
Levels of Consciousness (5)
Alert: Fully awake, responsive to stimuli, normal conversation.
Lethargic: Drowsy, can be easily awakened with verbal stimuli, may fall back asleep quickly.
Obtunded: Moderately decreased alertness, requires repeated stimulation to stay awake.
Stupor: Deeply asleep, only awakens to strong painful stimuli, immediately falls back asleep when stimulation stops.
Coma: Remaining unresponsive to all stimuli; eyes stay closed and no purposeful response to stimuli
Abnormal Levels of Consciousness
lethargy, obtunded, stupor, coma
Alert
Fully awake, responsive to stimuli, normal conversation.
Obtunded
Moderately decreased alertness; Opening eyes to loud voice, responding slowly with confusion, seeming unaware of environment.
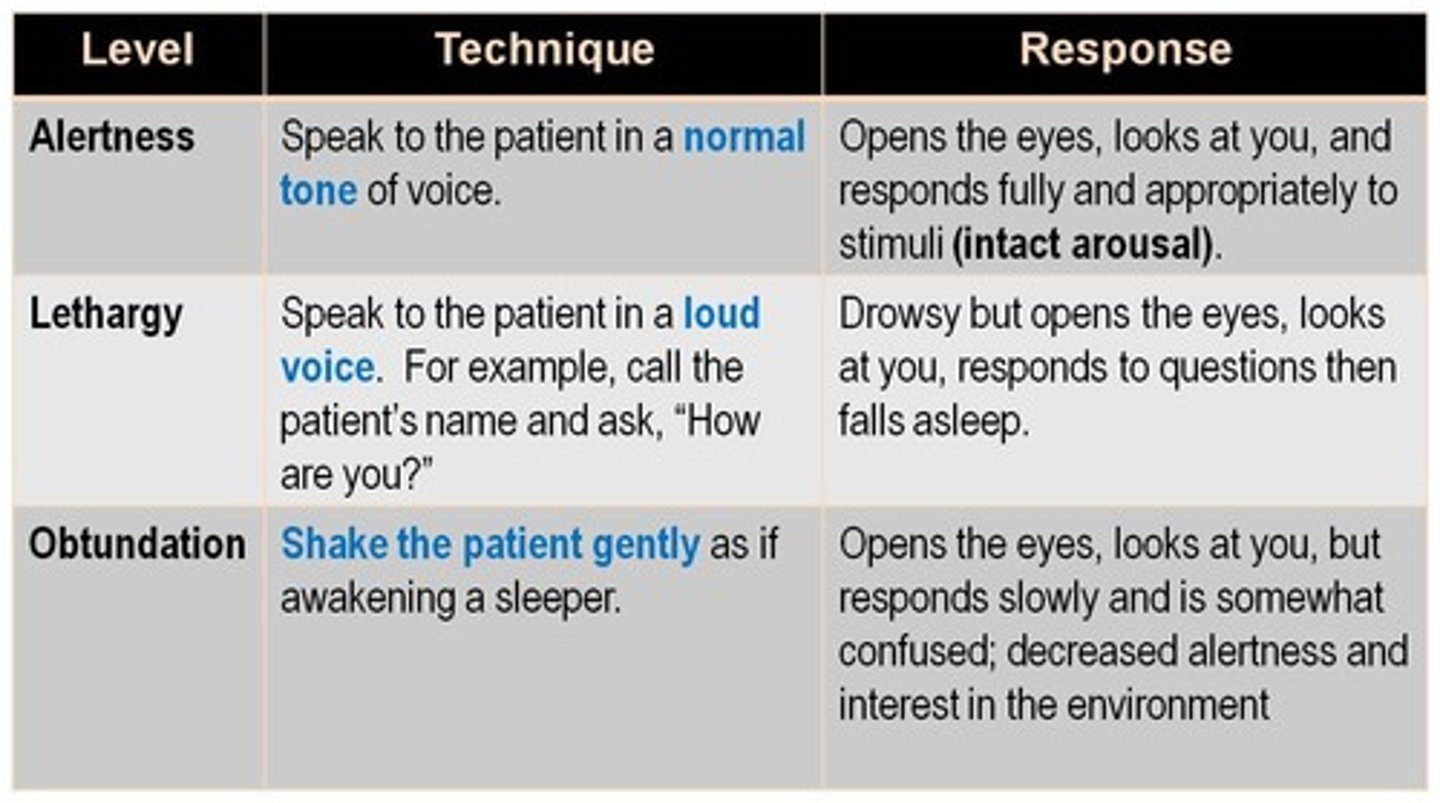
Stuporous
Deeply asleep and difficult to arouse; awakens to vigorous shake or painful stimulus but returns to unresponsive sleep

Lethargy
Can be easily awakened with verbal stimuli; opening eyes, answering questions, and falling back to sleep quickly
Coma
Remaining unresponsive to all stimuli; eyes stay closed and no purposeful response to stimuli
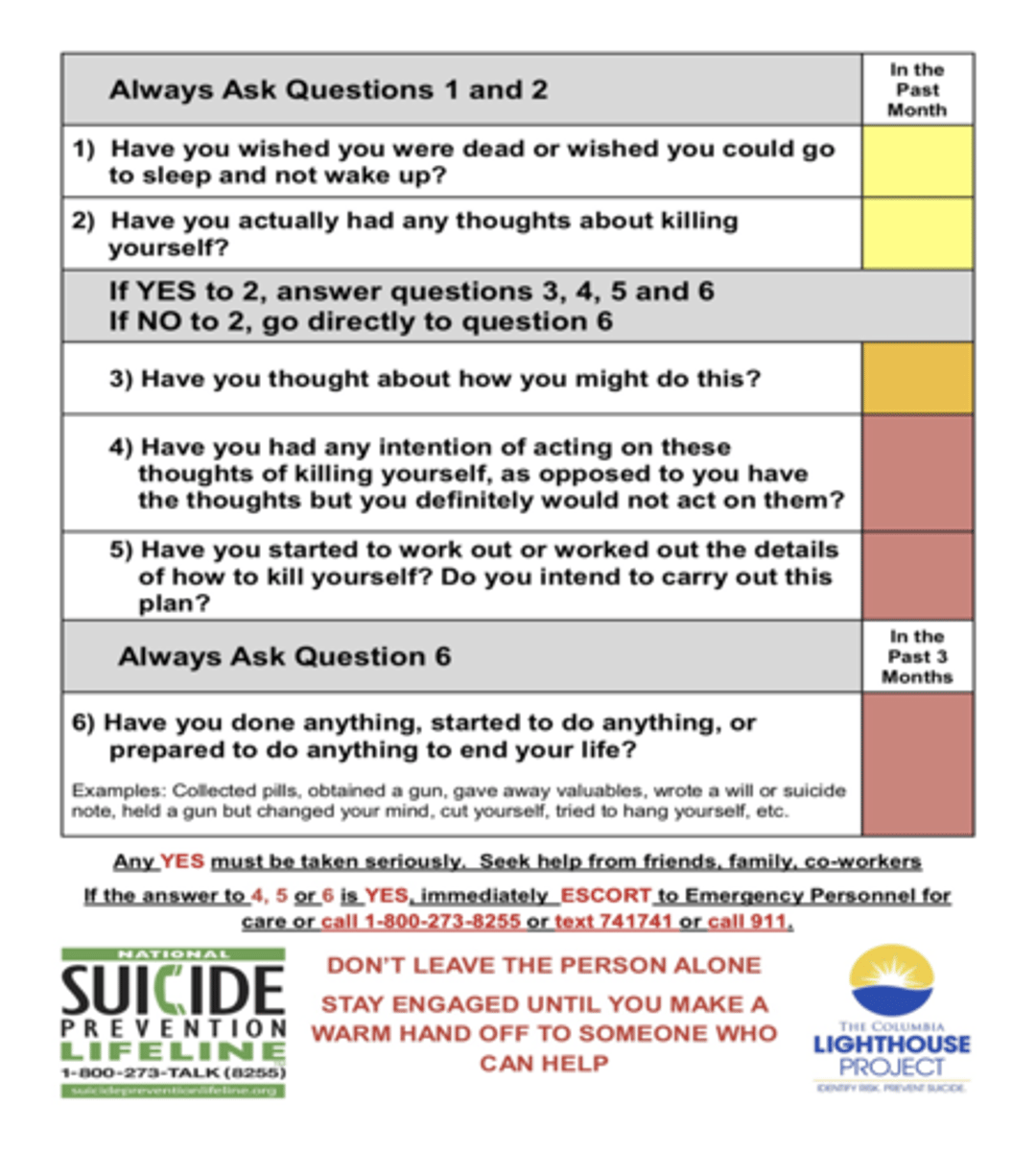
Columbia Suicide Severity Rating Scale (C-SSRS)
Used to screen patients for both suicidal behavior and ideation
SAD PERSONS Suicide Risk Assessment Tool
Sex
Age
Depression
Previous attempt
Ethanol abuse
Rational thinking loss
Social supports lacking
Organized plan
No spouse
Sickness
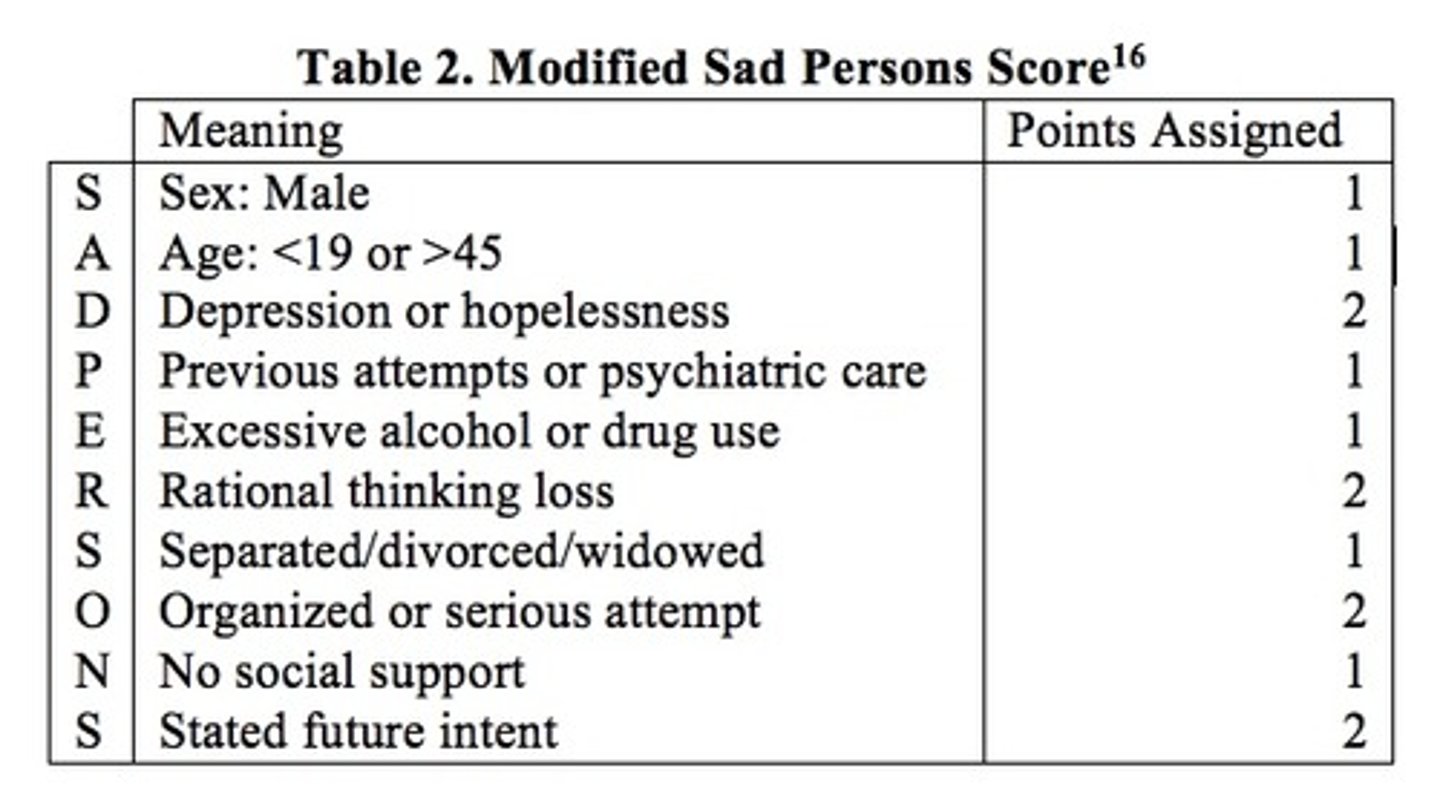
SAD PERSONS Scoring
Ranges from 0 to 10, with 10 being the highest risk for suicide (0-2 send home with follow-up; 3-4 close follow-up, consider hospitalization; 5-6 strongly consider hospitalization; 7-10 hospitalize or commit).
A nurse working in an emergency department (ED) uses the SAD PERSONS tool to assess a client's suicide risk. The nurse records client score as 8. What action should the nurse take?
A) Initiate involuntary commitment.
B) Continue to monitor the client.
C) Notify the health care provider.
D) Discharge the client home.
With a score of 8, the client is at high risk for suicide, so the health care provider needs to be notified immediately of findings so action can be taken to ensure client safety. The nurse should initiate one-on-one supervision until the client is transferred to a mental health unit. The client cannot be discharged home. The nurse cannot initiate the involuntary commitment; the health care provider will initiate this.
The nurse is precepting a new nurse to the mental health unit. The nurse intervenes when which of the following is observed during a focused mental health assessment in a locked unit?
A) Documenting physical appearance of the client in the chart
B) Using the SLUMS examination tool to assess cognitive function
C) Testing remote memory by asking questions related to client's childhood
D) Assessing the client's deep tendon reflexes with a reflex hammer
D) Assessing the client's deep tendon reflexes with a reflex hammer
Assessing deep tendon reflexes is not part of a focused mental health assessment; it is performed in a neurological assessment. Documenting the physical appearance of the client in the chart, using the SLUMS examination tool, and testing remote memory are included in a mental health assessment. Essential assessment areas for mental status include appearance, general behavior, cognitive function and memory, and thought processes.
Signs and Symptoms of Alzheimer's (10)
Memory loss that disrupts daily life
Challenges in planning or solving problems
Difficulty completing familiar tasks at home, at work, or at leisure
Confusion with time or place
Trouble understanding visual images or spatial relationships
New problems with words in speaking or writing
Misplacing things and losing the ability to retrace steps
Decreased or poor judgment
Withdrawal from work or social activities
Changes in mood or personality
Risk Factors of Alzheimer's
Increasing age, especially 65 years or older Genetic predisposition and family history
Mild cognitive impairment
Latino or African American descent due to higher vascular disease rates
Heart-head connection (diseases that predispose a client to vascular complications, such as diabetes, high blood pressure, and high cholesterol)
Head trauma (traumatic brain injury)
Alcohol Use Disorders Identification Test (AUDIT)
A 10-question instrument used to get information on the amount of the patient's drinking, the symptoms of dependence, and alcohol's harmful effects on their life
Scores range from 0-40; a score of 8+ indicates likelihood of harmful alcohol consumption
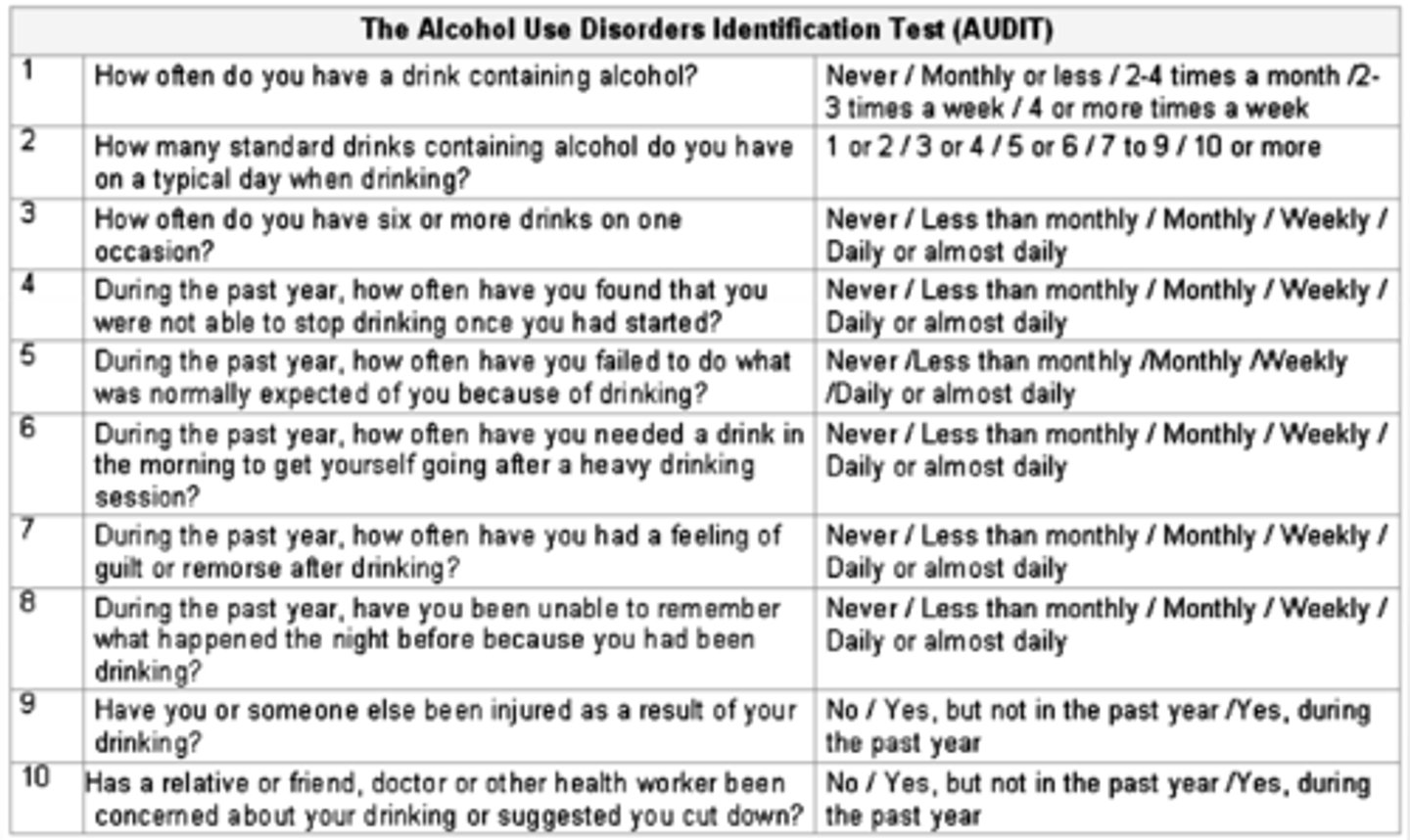
Alcohol Use Disorders Identification Test (AUDIT): Questions Part 1
How often do you have a drink containing alcohol?
How many drinks containing alcohol do you have on a typical day when you are drinking?
How often do you have six or more drinks on one occasion?
How often during the past year have you found that you were not able to stop drinking once you had started?
How often during the past year have you failed to do what was normally expected from you because of drinking?
How often during the past year have you needed a first drink in the morning to get yourself going after a heavy drinking session?
Alcohol Use Disorders Identification Test (AUDIT): Questions Part 2
How often during the past year have you had a feeling of guilt or remorse after drinking?
How often during the past year have you been unable to remember what happened the night before because you had been drinking?
Have you or someone else been injured as a result of your drinking?
Has a relative or friend or a doctor or another health worker been concerned about your drinking or suggested you cut down?
What are scores for GCS?
GCS score of 15 indicates an optimal level of consciousness.
GCS score of <15 indicates some impairment in the level of consciousness. A score of 3, the lowest possible score, indicates deep coma.
With regards to a mental assessment, what are normal and abnormal findings of posture, gait, and body movements?
NORMAL: The client is relaxed, with shoulders and back erect when standing or sitting. Gait is rhythmic and coordinated, with arms swinging at sides.
ABNORMAL: Slumped posture may reflect feelings of powerlessness or hopelessness characteristic of depression or organic brain disease. Bizarre body movements and behavior may be noted in schizophrenia or may be a side effect of drug therapy or other activity. Tense or anxious clients may elevate their shoulders toward their ears and hold the entire body stiffly
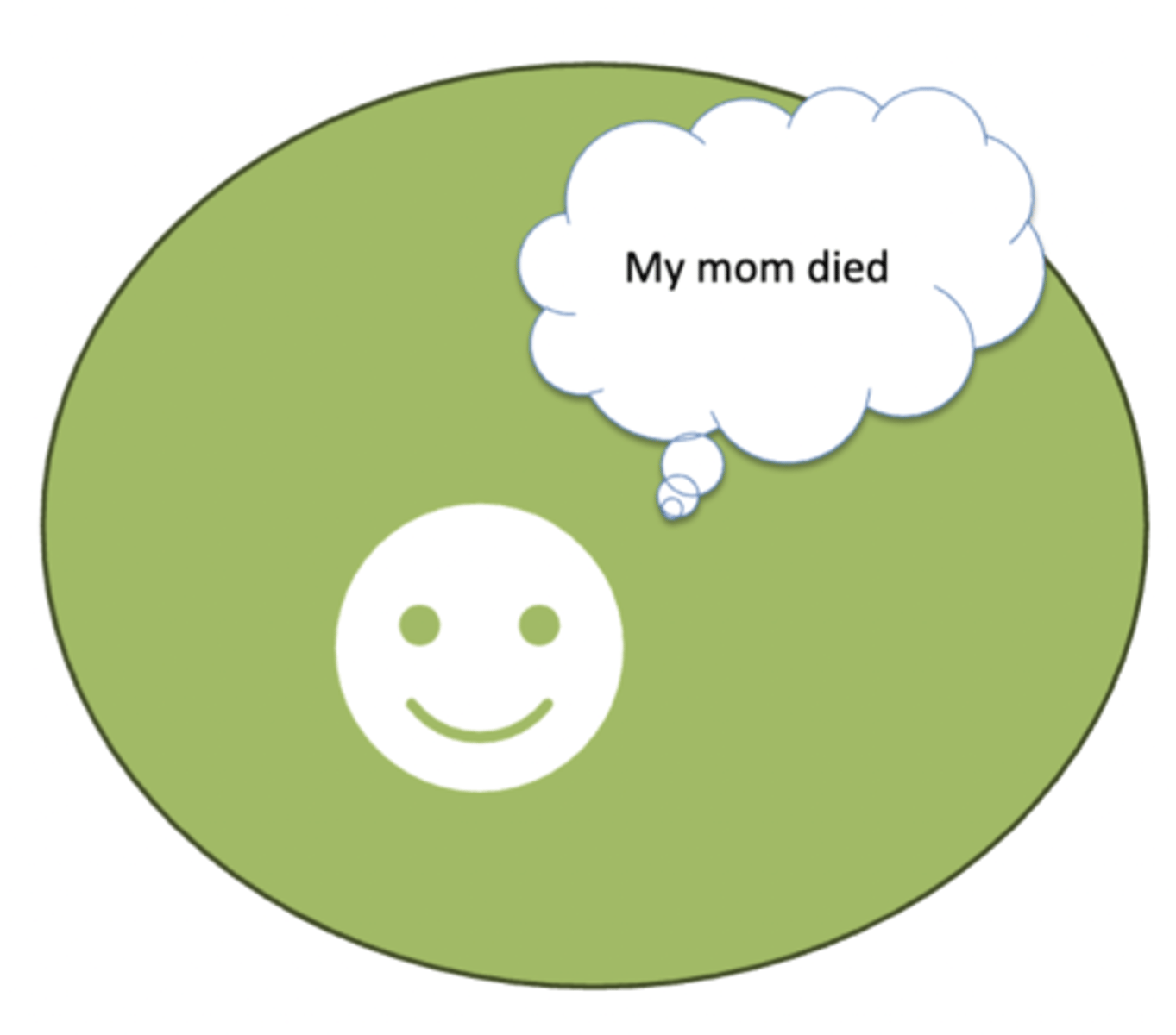
Mood vs. Affect
Mood is the patient's self-report of their prevailing emotions. Ask things like "how are you feeling" and have them rate it from 0-10.
Affect is how they appear to you- happy, sad, excited, etc. Their "emotional tone". Assess the range of their affect, the duration and intensity of their affect, whether their affect is appropriate to the context and matches their stated mood.
With regards to a mental assessment, what are normal findings of behavior and affect?
Client is cooperative and purposeful in their interactions with others. Affect is appropriate for the client's situation.
Mild-to-moderate anxiety may be seen in a client who is apprehensive about having a health assessment performed.
With regards to a mental assessment, what are abnormal findings of behavior and affect?
Uncooperative, bizarre behavior may be seen in the angry, mentally ill, or violent client. Anxious clients are often fidgety and restless. Some degree of anxiety is often seen in ill clients.
Apathy or crying may be seen with depression. Incongruent behavior may be seen in clients who are in denial of problems or illness. Prolonged, euphoric laughing is typical of mania.
In regards to behavior and affect, how may people with anxiety present?
Anxious clients are often fidgety and restless. Some degree of anxiety is often seen in ill clients.
In regards to behavior and affect, how may people with depression present?
Apathy or crying may be seen with depression.
In regards to behavior and affect, how may people with mania or those in denial present?
Incongruent behavior may be seen in clients who are in denial of problems or illness.
Prolonged, euphoric laughing is typical of mania.
How do you observe and assess grooming and dress?
Keep the examination setting and the reason for the assessment in mind as you note the client's degree of cleanliness and attire.
For example, if the client arrives directly from home, they may be neater than if they come to the assessment from the workplace.
With regards to a mental assessment, what are normal findings for grooming and dress?
Dress is appropriate for occasion and weather. Dress varies considerably from person to person, depending on individual preference. There may be several normal dress variations depending on the client's developmental level, age, socioeconomic level, and culture or subculture.
In regards to dress and grooming, how may people with OCD present?
Unusually meticulous grooming and finicky mannerisms may be seen in obsessive-compulsive disorder.
If client is extremely anxious and agitated with sweats, tremors, nausea and vomiting, or tactile disturbances, what else needs to be ruled out?
It may be necessary to rule out withdrawal from alcohol because it presents with the same symptoms
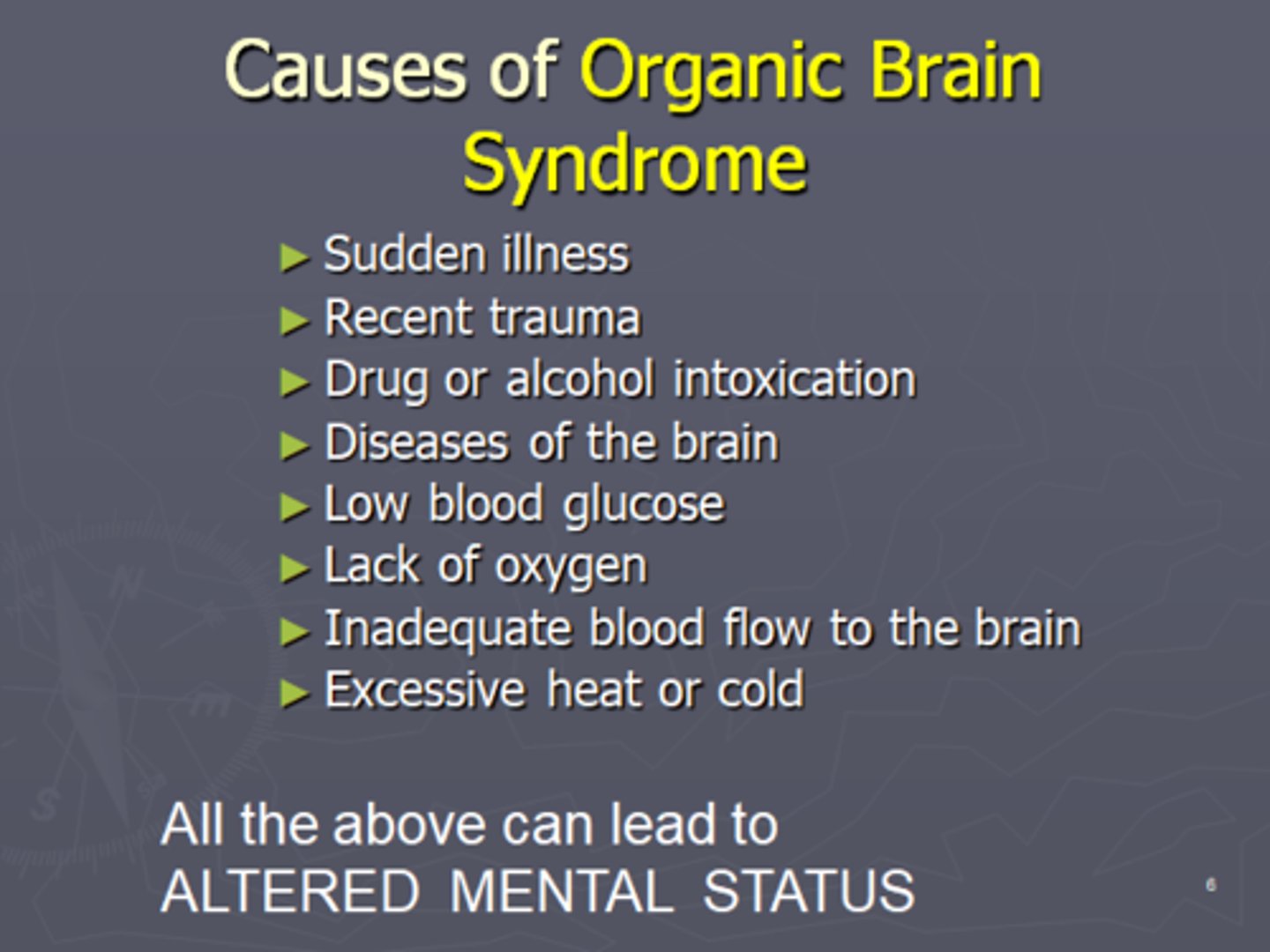
Organic Brain Syndrome
Temporary or permanent dysfunction of the brain, caused by a disturbance in the physical or physiologic functioning of brain tissue.
In regards to dress and grooming, how may people with organic brain syndrome present?
Poor hygiene and inappropriate dress may be seen with organic brain syndrome.
In regards to dress and grooming, how may people with mania or schizophrenia present?
Bizarre dress and exaggerated makeup/cosmetics may be seen in schizophrenia or manic disorders.
In regards to dress and grooming, what condition can cause extreme unilateral neglect?
Extreme unilateral neglect may result from a lesion due to a cerebral vascular accident.
In regards to dress and grooming, how may mentally ill, grieving, depressed, or poor patients present?
Uncoordinated clothing, extremely light clothing, or extremely warm clothing for the weather conditions may be seen on mentally ill, grieving, depressed, or poor clients. This may also be noted in clients with heat or cold intolerances.
In regards to dress and grooming, what can soiled clothing indicate?
Soiled clothing may indicate homelessness, vision deficits in older adults, or mental illness
With regards to a mental assessment, what are abnormal findings for hygiene?
A dirty, unshaven, and unkempt appearance with a foul body odor may reflect depression, drug abuse, or low socioeconomic level (i.e., homeless client).
Poor hygiene may be seen in dementia or other conditions and may indicate a self-care deficit. If others care for the client, poor hygiene may reflect neglect by caregiver or caregiver role strain. Breath odors from smoking or from drinking alcoholic beverages may be noted
How do you observe and assess hygiene?
Observe hygiene. Consider normal level of hygiene for the client's developmental level, socioeconomic status, and ethnic/cultural background.
With regards to a mental assessment, what are abnormal findings for facial expressions?
Reduced eye contact is seen in depression or apathy. Extreme facial expressions of happiness, anger, or fright may be seen in anxious clients. Clients with Parkinson disease may have a mask-like, expressionless face.
Staring watchfulness appears in metabolic disorders and anxiety. Inappropriate facial expressions (e.g., smiling when expressing sad thoughts) may indicate mental illness. Drooping or gross asymmetry occurs with neurologic disorder or injury (e.g., Bell palsy or stroke).
What conditions can cause drooping or gross asymmetry?
Drooping or gross asymmetry occurs with neurologic disorder or injury (e.g., Bell palsy or stroke).
With regards to a mental assessment, what facial expressions may be present in anxious patients?
Extreme facial expressions of happiness, anger, or fright may be seen in anxious clients.
How do you assess speech for a mental assessment?
Note tone, clarity, and pace of speech.
With regards to a mental assessment, what are abnormal findings for speech?
Slow, repetitive speech is characteristic of depression or Parkinson disease. Loud, rapid speech may occur in manic phases of bipolar disorder. Disorganized speech, consistent (nonstop) speech, or long periods of silence may indicate mental illness or a neurologic disorder (e.g., dysarthria, dysphasia, speech defect, or garbled speech).
If a person has depression or Parkinson disease, how can their speech present as?
Slow, repetitive speech is characteristic of depression or Parkinson disease.
If a person has bipolar, how can their speech present as during manic phases?
Loud, rapid speech may occur in manic phases of bipolar disorder.
What can disorganized or nonstop speech during a mental assessment be indicative of?
Disorganized speech, consistent (nonstop) speech, or long periods of silence may indicate mental illness or a neurologic disorder (e.g., dysarthria, dysphasia, speech defect, or garbled speech).
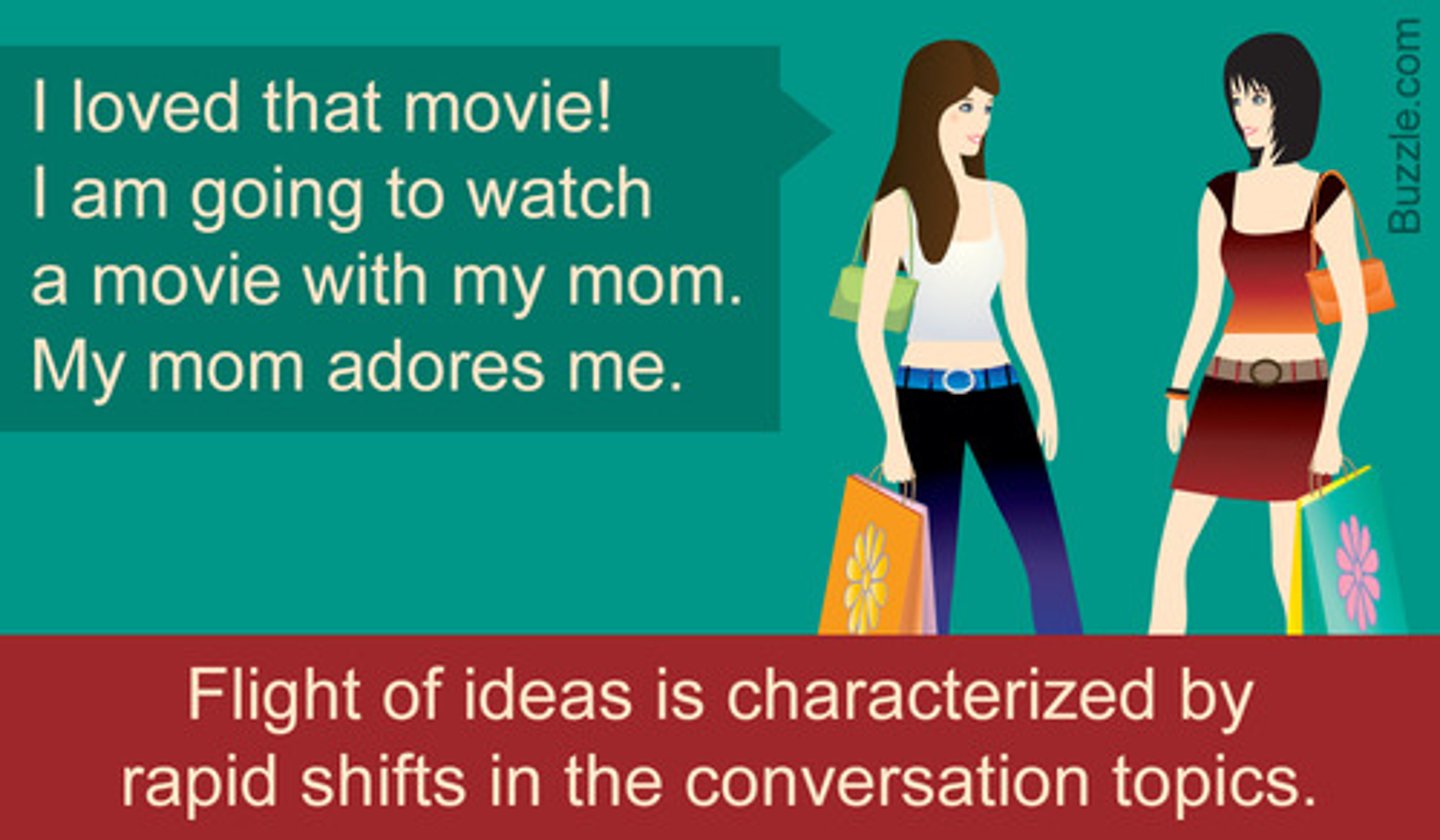
Flight of Ideas
Symptom of mania that involves an abruptly switching in conversation from one topic to another
If the client has difficulty with speech, what additional tests should be performed?
Ask the client to name objects in the room.
Ask the client to write a sentence.
Ask the client to read from printed material appropriate for their educational level.
With regards to a mental assessment, what are normal findings for mood, feelings, and expressions?
Cooperative or friendly, expresses feelings appropriate to situation, verbalizes positive feelings regarding others and the future, expresses positive coping mechanisms (support groups, exercise, sports, hobbies, and counseling).
With regards to a mental assessment, what are abnormal findings for mood, feelings, and expressions?
Flat affect, euphoria, elation, ecstasy, anxiety, fear, ambivalence, irritability, depression, depersonalization, quick mood change, depression, and/or rage are all examples of altered mood expressions. Depression, anxiety, and somatization are common mental disorders seen in at least 5%-10% of clients
Expression of prolonged negative, gloomy, despairing feelings is noted in depression. Expression of elation and grandiosity, high energy level, and engagement in high-risk but pleasurable activities are seen in manic phases. Excessive worry may be seen in anxiety or obsessive-compulsive disorders. Eccentric moods not appropriate to the situation are seen in schizophrenia.
What are examples of altered mood expressions?
Flat affect, euphoria, elation, ecstasy, anxiety, fear, ambivalence, irritability, depression, depersonalization, quick mood change, depression, and/or rage are all examples of altered mood expressions.
Types of Affects (6)
Blunted - pt show little or no facial expression
Euthymic- Normal, steady, tranquil mental state
Flat - no facial expression at all
Inappropriate - facial expression that is not appropriate
Restricted - only one type of expression (anger)
Full range/broad - a person is able to change their expression in response to the situation.
Euthymic Affect
Normal, steady, tranquil mental state; non-depressed, reasonably positive mood
What disorders can euthymic affect be seen with?
May be a tranquil, steady state or a temporary steady state between the up- and downswings of affect seen in bipolar disorder
Flat Affect
A severely reduced emotional expressiveness (commonly seen with schizophrenia and depression)
A person shows very little to no outward display of emotions through facial expressions, body language, or tone of voice, appearing emotionally "flat" regardless of the situation

What conditions are flat affect seen with?
Often seen in depression or schizophrenia
Constricted Affect
A mildly diminished range or intensity of emotional expression that is less severe than that of blunted affect.

Blunted Affect
Markedly diminished emotional expression
Reduced affect (constricted, blunted) is often associated with autism, schizophrenia, depression, PTSD, brain injury (tumor, head trauma, dementia, brain damage, or side effects from medications)

What conditions can blunted and constricted affect be seen with?
Reduced affect (constricted, blunted) is often associated with autism, schizophrenia, depression, PTSD, brain injury (tumor, head trauma, dementia, brain damage, or side effects from medications)
Labile Affect
Irregular and severe mood swings
Associated with bipolar disorder, borderline personality disorder, or from overstimulation, stress, or anxiety
What conditions are labile affects associated with?
Associated with bipolar disorder, borderline personality disorder, or from overstimulation, stress, or anxiety
Inappropriate Affect
Emotional responses that are not in keeping with the situation or are incompatible with expressed thoughts or wishes, such as smiling when told about the death of a friend
What conditions are inappropriate affect associated with?
Often seen in disorganized schizophrenia or with brain injury (tumor, head trauma, dementia)
Elation
A feeling of extreme joy, optimism, and excitement. It can be a symptom of a number of disorders, including mania, schizophrenia, and psychosis.
Depersonalization
A dissociative disorder characterized by persistent or recurrent feelings of detachment from one's mental processes or body
What mood, feelings, and expressions are seen with manic episodes?
Expression of elation and grandiosity, high energy level, and engagement in high-risk but pleasurable activities are seen in manic phases