Pathology Nervous system I Responses of the nervous system to injury, cerebro- vascular disease, brain ischemia and infarction, hemorrhage
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
what type of cell are the principal functional unit of CNS?
neurons
t/f: mature neurons are incapable of cell division
true
what type of cells are responsible for repair and scar formation?
astrocytes (gliosis)
what type of cells produce myelin?
oligodendrocytes
what type of cells are the phagocytes of the CNS?
microglial cells
what type of cells line the ventricular system and the central canal of the spinal cord?
ependymal cells
what type of cells are responsible for the secretion of CSF?
choroid plexus (in continuity with the ependyma)
what is phagocytosis?
Removal of dead tissues by engulfment via microglial cells and recruited monocytes
what is the most important histopathologic marker of CNS injury?
gliosis
what happens during gliosis?
hypertrophy and hyperplasia of astrocytes
activated astrocytes proliferate
scar and repair formation
protects neurons
largely damaged areas of the brain can be partyl gliotic with _______
cystic components
what is cerebral edema (brain parenchymal edema)?
accumulation of excess fluid within the brain
what are the 2 types of cerebral edema?
vasogenic edema (increase in extracellular fluid)
cytotoxic edema (increase in intracellular fluid)
what is vasogenic edema caused by? cytotoxic edema?
Vasogenic edema: Increase in extracellular fluid
Caused by:
Blood brain barrier disruption
Increased vascular permeability
Cytotoxic edema: Increase in intracellular fluid
Caused by:
Neuronal, glial, or endothelial membrane injury
t/f: In practice, conditions associated with generalized edema often have elements of both vasogenic and cytotoxic edema
true
what is hydrocephalus? what is it caused by?
Accumulation of excessive CSF within the ventricular system
Caused by:
Impaired flow of CSF
Decreased resorption of CSF
what is herniation? what are the 3 different types?
The displacement of brain tissue from one compartment to another in response to increased cranial pressure
1. Subfalcine (cingulate) herniation
2. Transtentorial (uncinate) herniation
3. Tonsillar herniation
what are some different brain responses to injury?
herniation
hydrocephalus
cerebral edema
phagocytosis
gliosis
what is subfaicine (cingulate) herniation?
• Compression of anterior cerebral artery
• Unilateral/asymmetric expansion displacing cingulate gyrus under edge of falx cerebri
what is transtenrotial (uncinate) herniation?
• Temporal lobe compressed
• 3rd CN compromised-pupil dilation & impaired eye movement
• Posterior cerebral artery may be compressed
what is tonsillar herniation?
• Displacement of cerebellar tonsils through foramen magnum
• Compresses brain stem-life threatening
what is thrombus?
clot forming in a vessel (fibrin and blood cells)
what is Embolus?
any foreign substance that moves in your bloodstream until it blocks a vessel (a dislodged thrombus can become an embolus)
what is Ischemia?
inadequate supply of blood
what is Aneurysm?
ballooning in the wall of a vessel due to weakening of the wall
what is Infarction?
obstruction of the blood supply to an organ or region of tissue causing local death of the tissue
Cerebrovascular diseases are brain disorders caused by pathologic processes involving …?
blood vessels
t/f: the clinical designation of cerebrovascular disease is stroke and it is one of the leading causes of death in the US.
true
Cerebrovascular disease occurs via 3 pathologic mechanisms. What are these mechanisms?
thrombolic occlusion
embolic occlusion
vascular rupture (HTN, aneurysm, malformation)
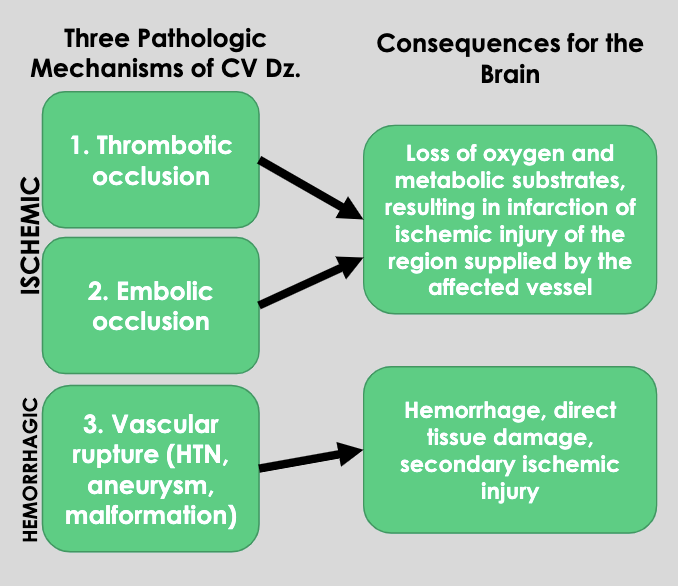
what are the consequence for the brain thrombotic occlusion and embolic occlusion (ischemic)?
Loss of oxygen and metabolic substrates, resulting in infarction of ischemic injury of the region supplied by the affected vessel
what are the consequence for the brain of vascular rupture (hemorrhagic)?
Hemorrhage, direct tissue damage, secondary ischemic injury
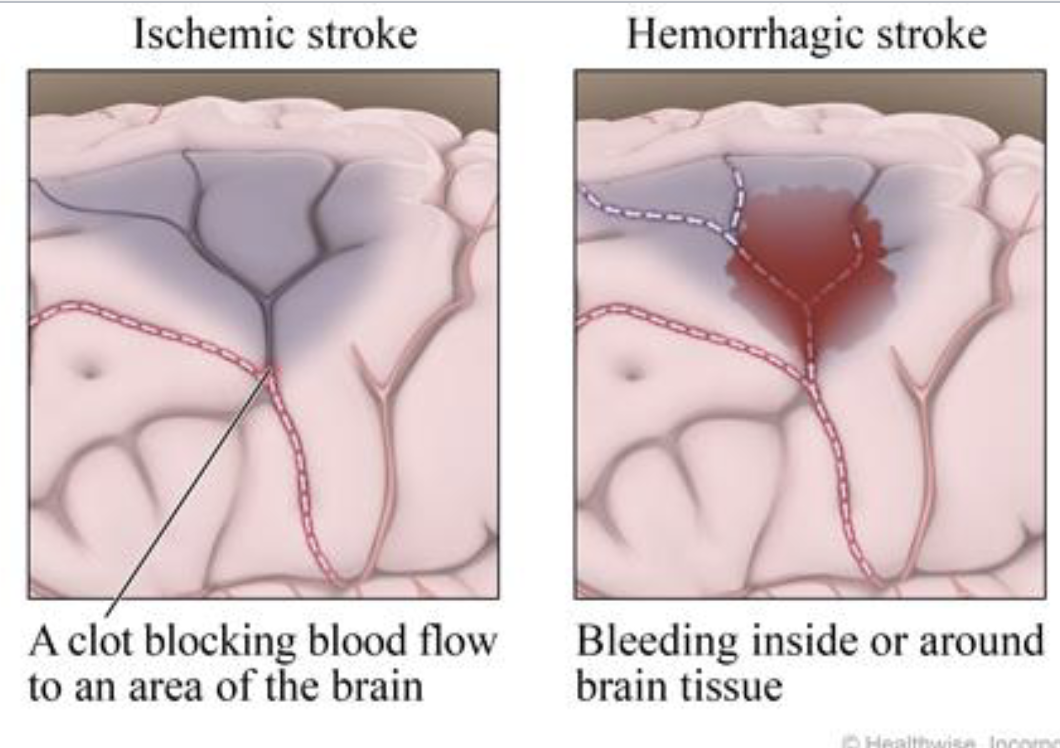
what is the difference between an ischemic stroke and a hemorrhagic stroke?
characteristics of spontaneous intracranial hemorrhage (non-traumatic)?
• Mid to late adult life
• Most due to rupture of a small intracranial vessel (can lead to death if large enough)
• Can extend into ventricular system
• May be clinically silent if small enough
what is the leading cause of spontaneous intracranial hemorrhage (non-traumatic)?
Hypertension
what happens if a patient survives a spontaneous intracranial hemorrhage (non-traumatic)?
If patient survives, gradual removal of hematoma ensues via macrophages (Astrocytic gliosis at periphery)
what is a subarachnoid hemorrhage?
Layer of blood over brain surface into the subarachnoid space
what are common causes of subarachnoid hemorrhage?
trauma (most common overall)
spontaneous subaracnoid hemorrahge = rupture of saccular aneurysm in cerebral artery
Non-traumatic subarachnoid hemorrhage may also result from:
• Rupture of a primary intracerebral hemorrhage into the ventricular system
• Vascular malformation
• Hematologic disturbances
• Tumors
Overall % of aneurysms bleed each year
~1.3
what is the most frequent cause of clinically significant nontraumatic subarachnoid hemorrhage?
saccular (berry) aneurysm
what is the most common type of intracranial aneurysm?
saccular (berry) aneurysm
the incidence of saccular (berry) aneurysms is % of population. however, increased incidence can be observed in pts with what coniditons…?
2%
AD polycystic kidney disease, Ehlers-Danlos syndrome, NF1, and Marfan syndrome
t/f: Injury of several cubic centimeters of brain parenchyma may be clinically silent, severely disabling, or fatal
true
The physical forces associated with head injury may result in:
• Skull fractures
• Parenchymal injury (Concussion (mild) and Contusions and lacerations (severe))
• Vascular injury
• All 3 of these may coexist
The magnitude and distribution of a traumatic brain injury depends on:
• The shape of the object causing the trauma
• The force of the impact
• Whether the head is in motion at the time of injury
what is a concussion?
Clinical syndrome of altered consciousness secondary to head injury
Typically brought about by change in the momentum of the head
what are signs/symptoms of concussion?
• Transient neurologic dysfunction (including loss of consciousness)
• Temporary respiratory arrest
• Loss of reflexes
what is a cerebral contusion?
A blow to the surface of the brain, transmitted through the skull, leading to rapid tissue displacement, disruption of vascular channels, and subsequent hemorrhage, tissue injury, and edema
what are the most common locations of a cerebral contusion?
Frontal and temporal lobes (Crests of gyri are most susceptible)
cerebral contusion may develop at the point of contact (a coup injury) or on the brain surface diametrically opposed to it (contrecoup injury). What situations would result in each kind of injury?
• If the head is immobile at time of trauma only a coup injury is found
• If the head is mobile both a coup and contrecoup lesion may be found
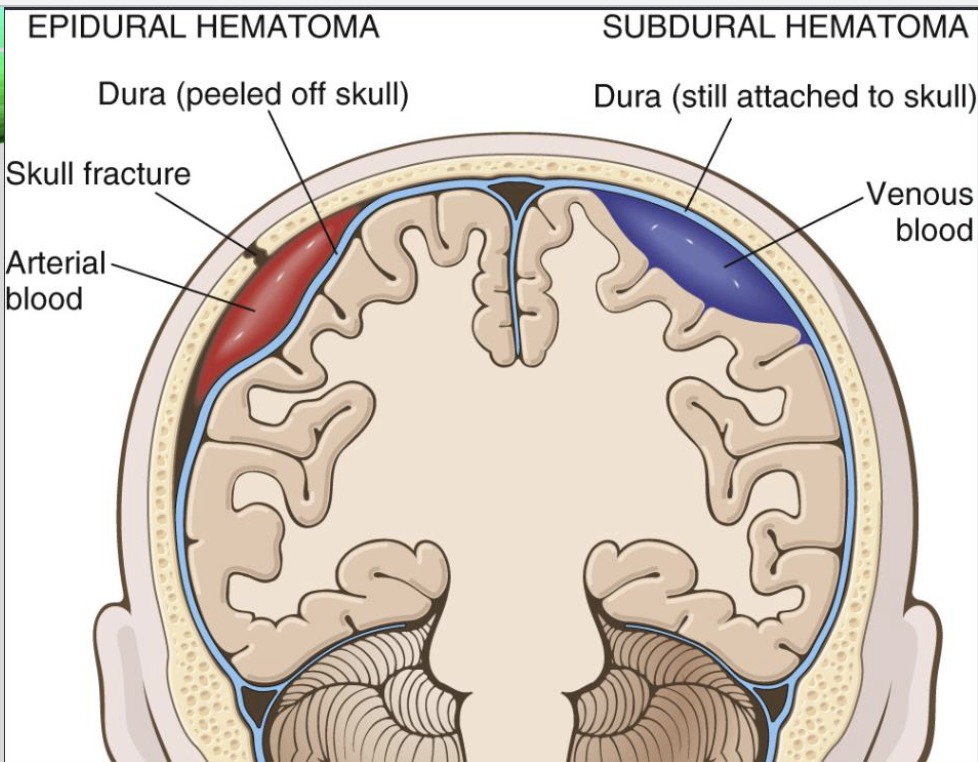
what is a subdural hematoma?
Hemorrhage in space between the two layers of the dura
inner cell layer of dura is thin and close to arachnoid layer
blood appears to be between the dura and arachnoid
underlying brain is flattened by clotted blood
subdural hematoma is caused by…?
traumatic tearing of veins that traverse the subdural space (“bridging veins”)
what pts are at higher risk of subdural hematomas?
pts with brain atrophy
bridging veins stretched out and brain has additional space within which to move accounting for higher rate of subdural hematomas in older adults
Infants
bridging veins are thin walled
what are epidural hematomas?
Blood accumulates between the skull and dura mater
pressure from blood accumulation dissects dura away from inner skull surface
epidural hematomas are almost wlays caused by…./
skull fracture
what are clinical characteristics of epidural hematomas to be aware of?
Patients can be lucid for several hours after event before neurologic signs appear (slow blood accumulation)
Without prompt diagnosis and drainage, it is fatal within a few hours
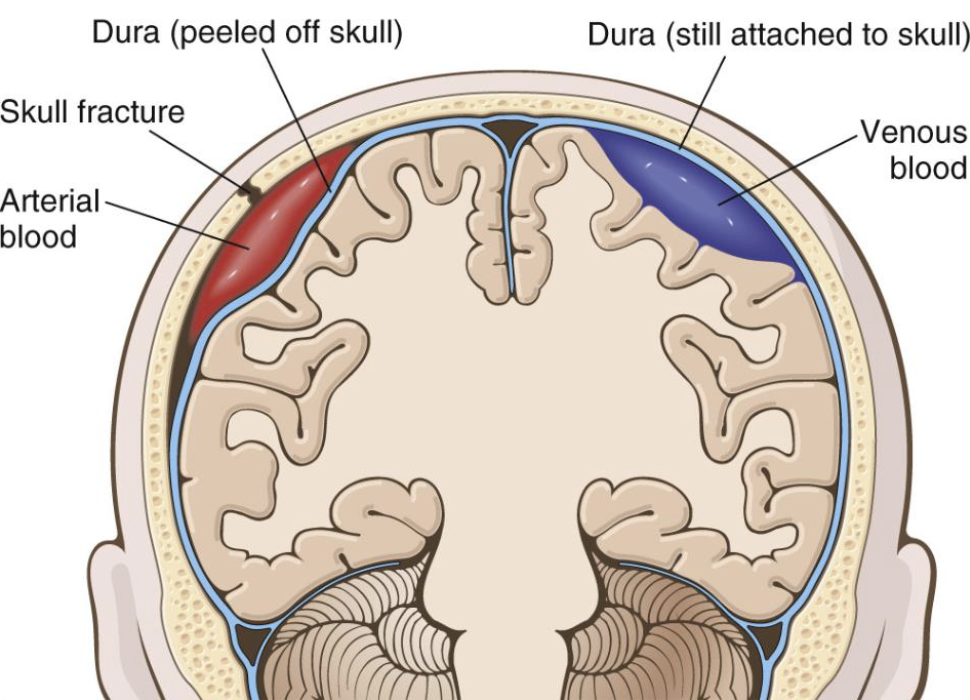
what type of hematoma is portrayed in red? purple?
what are the 4 principal routes by which microbes enter the nervous system?
Hematogenous (most common)
Direct implantation
often traumatic, but can occur from a congenital malformation
Local extension
can originate from infected adjacent structures like sinuses, teeth, skull, or vertebrae
Peripheral nerves
infection of the CNS via peripheral nerves can be seen with what type of viruses?
rabies and herpes zoster virus
what is the inflammatory process of the leptomeninges and CSF within the subarachnoid space, usually caused by an infection?
meningitis
what is Meningoencephalitis?
inflammation of the meninges and brain
meningitis is classified based on etiology and clinical evolution. what are the classifications?
o Acute pyogenic- usually bacterial
o Aseptic- usually viral
o Chronic- TB and other organisms
Symptoms of Acute pyogenic (Bacterial) Meningitis include …?
headache, neck stiffness, photophobia
what type of organisms are found in Acute pyogenic (Bacterial) ?
• E. coli and Group B strep. in neonates
• Neisseria in young adults
• Strep. pneumoniae in adults
when a thick layer of suppurative exudate covers the brain surface and thickens the leptomeninges, this is called…?
Pyogenic meningitis
what is the term used for an absence of organisms by bacterial culture in a patient with manifestations of meningitis?
aseptic meningitis
symptoms of aseptic meningitis
irritation, fever, alterations in consciousness
characteristics of aseptic meningitis
usually viral but can be bacterial, rickettsial, or autoimmune
self-limiting and usually treated symptomatically
what type of viral disease of CNS can be caused by herpes simplex virus?
• Type 1-Necrotizing encephalitis in children and young adults
• Type 2-Meningitis and neuronal necrotizing encephalitis in adults
what type of viral disease of CNS can be caused by herpes zoster (shingles) virus?
• Peripheral nerve dermatomes from latent CNS infection
• Postherpetic neuralgia, granulomatous arteritis (rare)
what type of viral disease of CNS can be caused by cytomegalovirus (HHV-5) virus?
• Encephalitis in immunosuppressed (immunocompromised)
what type of viral disease of CNS can be caused by HIV/AIDS virus?
HIV encephalitis and myelopathy
what type of viral disease of CNS can be caused by rubeola (measles) virus?
• Subacute sclerosing panencephalitis in childhood
• Neuronal death and gliosis
what type of viral disease of CNS can be caused by rubella (German measles) and Zika virus?
In utero infection leads to microcephaly
what type of viral disease of CNS can be caused by rhabdovirus?
• Rabies by animal bite (incubation period 1-3 months)
• Travel to peripheral nerves to CNS → Severe meningoencephalitis
• Death usually from respiratory failure
fungal infections of the CNS primarily occur in what pt populations?
immunocompromised individuals
Three main forms of injury in the CNS from fungal infection are…?
• Chronic meningitis
• Vasculitis
• Parenchymal invasion- usually in the form of granulomas or abscesses
what are the most frequent fungi that cause infections of the CNS?
• Candida albicans- occasional vasculitis, multiple microabscesses with or w/o granuloma formation
• Mucor species- vasculitis, direct extension of vascular invasion
• Aspergillosis fumigatus- vasculitis, hemorrhagic infarctions due to marked predilection for vessel walls
• Cryptococcus neoformans- common opportunistic infection in the setting of AIDS
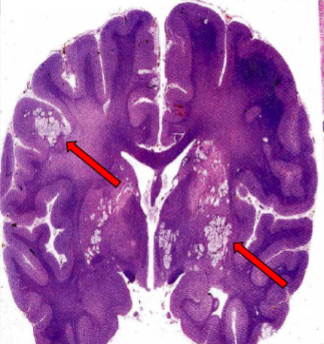
CRYPTOCOCCI IN CEREBRAL HEMISPHERES (ARROWS)
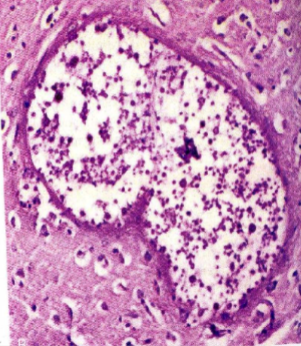
HIGHER MAGNIFICATION OF MULTIPLE CRYPTOCOCCI