Unit 2 - Diagnosis-Specific Considerations (Demyelinating and Basal Ganglia disorders)
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
MS Review
Chronic autoimmune disorder affecting CNS
Demyelination and axonal damage
Types: RRMS, SPMS, PPMS, PRMS
Common impairments: fatigue, weakness, spasticity, ataxia, balance/gait deficits
Types of MS
Relapsing-Remitting (RR)
marked by episodes of new or worsening symptoms followed by periods of partial or complete recovery
Types of MS
Secondary Progressive (SP)
often develops from RRMS and involves a steady progression of symptoms over time
Types of MS
Primary Progressive (PP)
characterized by gradual worsening without distinct relapses
Types of MS
Progressive Relapsing (PR)
the rarest form, showing steady progression with occasional acute relapses
Role of PT Across MS Disease Stages
Early Stage
Prevent deconditioning, educate, promote aerobic activity
Role of PT Across MS Disease Stages
Middle Stage
Manage fatigue, address gait and balance deficits
Role of PT Across MS Disease Stages
Late Stage
Prevent contractures, support transfers, maintain quality of life
MS
Fatigue Management Strategies
Pacing and energy conservation
Temperature regulation
cooling garments, air conditioning, and exercise timing to avoid overheating
Aerobic conditioning (submaximal, moderate intensity)
walking or stationary cycling
Activity diaries and fatigue scales (MFIS, FSS)
Modified Fatigue Impact Scale
Fatigue Severity Scale
MS
Strengthening and Functional Mobility
Avoid overwork weakness
Focus on multi-joint, functional exercises
Closed-chain > open-chain
provide joint stability, proprioceptive input, and often mimic the functional demands of upright activities
Task-specific training: sit-to-stand, stair climbing, transfers
improve strength, confidence, and independence
MS
Balance and Gait Training
Dual-task training
Static/dynamic balance (foam, perturbations)
Gait aids and orthotics (AFOs, FES)
Use of RAS (rhythmic auditory stimulation)
uses a metronome or music with a set tempo to improve gait, rhythm, and coordination
especially helpful for patients with ataxia or inconsistent stride patterns
MS
Spasticity and Tone Management
Stretching: slow, prolonged
30-60s
Positioning and splinting
help prevent contractures and minimize abnormal tone
Modalities: cryotherapy, TENS
Referral for medical management (baclofen, botox)
MS
Interdisciplinary Care and Patient Education
Education: pacing, exercise, stress management
Collaboration: OT, speech, neuropsych, neurology
Group therapy, support groups, telerehab options
Goal setting and self-efficacy
Overview of Guillain-Barré Syndrome
Acute, immune-mediated polyneuropathy
Rapid-onset muscle weakness, often ascending
Typically post-infectious (e.g., viral, bacterial)
Variants: AIDP (most common), Miller Fisher, AMAN/AMSAN
Types of GBS
Miller Fisher syndrome
typically presents with eye movement abnormalities and ataxia
Types of GBS
AMAN or AMSAN
involve axonal damage and often result in a more prolonged or incomplete recovery
Phases of GBS and PT Role
Acute (ICU)
Monitor vitals, positioning, respiratory support, PROM
Phases of GBS and PT Role
Plateau/Subacute
Begin gentle activity, prevent complications (DVT, contractures, skin breakdown), monitor fatigue
Phases of GBS and PT Role
Recovery
Progressive strengthening, mobility, function, community re-entry
GBS
Fatigue & Overwork Prevention
Monitor closely for overwork weakness
phenomenon where excessive or poorly dosed exercise during early recovery actually leads to a decline in strength rather than improvement, especially in partially denervated muscles
Low-rep, short-duration exercises initially
Prioritize rest and pacing
Use of fatigue scales and patient feedback
GBS
Functional Mobility & Strength Training
Task-specific retraining: transfers, gait, stairs
Use of ADs and orthoses (AFOs, walkers)
Progress resistance and reps slowly
Integrate balance and coordination as recovery allows
GBS
Interdisciplinary Collaboration & Patient Education
Work with OT, respiratory therapy, neurology, psychology
Teach energy conservation, joint protection
Support goal setting and long- term planning
Prepare for slow, nonlinear recovery trajectory
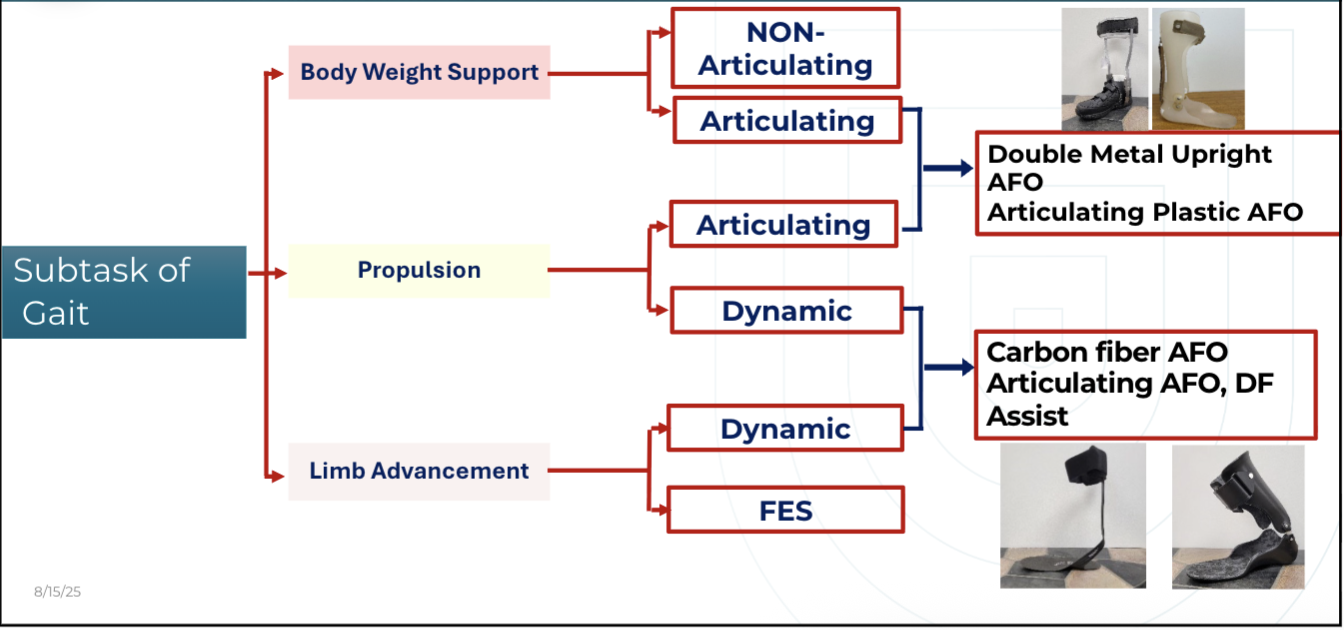
Orthotic Consideration
Body function/ structure
Patient activity
Environmental factors
Participation levels
KAFOs
<3+/5 MMT Quad strength
Met Participation criteria
If quads <2/5 MMT —> will need RGO
Met Completion criteria
KAFOs
Participation Criteria
No contractures
straight leg raised to 110 degrees
floor to wheelchair transfers are independent
ability to complete 50 dips in the parallel bars
VO2 max of greater than 20 milliliters
KAFOs
Completion Criteria
Ability to stand independently
ability to walk in the parallel bars
ability to walk 20 steps with supervision
AFOs
Weakness
Decreased Motor control
Can help improve foot drop
Can help improve knee hyperextension and knee flexion in stance phase
Solid Ankle AFOs
Foot clearance in swing phase
Medial and lateral support at the ankle
triplanar foot support
may prescribe for people with severe plantar flexor tone
Indirectly provides knee stability
can provide knee flexion in early stance phase
Articulated AFOs
Plantarflexion Stop (PS)
Allows ankle to be in more DF
Provide medial lateral support
Articulated AFOs
Dorsiflexion Stop (DS)
Prevent excessive DF in stance phase
Provide medial lateral support
Posterior Leaf Spring AFO
Provides foot clearance in swing phase
Does NOT provide any medial lateral support
less effective for people with severe tone or significant foot triplanar challenges
FES
Common fibular nerve is stimulated to improve dorsiflexion during swing phase
precautions
active cancer, osteomyelitis, epilepsy, pregnancy, skin tolerance, excessive subcutaneous tissue, or a history of implanted electrical devices
SO HOW DO WE CHOOSE TO USE AFOs or FES?
Level and pattern of motor recovery
Does the patient have volitional control of ankle dorsiflexors?
no active dorsiflexion, then the patient likely needs an AFO to maintain foot clearance during gait
some dorsiflexion, FES might be used to help activate and strengthen that movement
SO HOW DO WE CHOOSE TO USE AFOs or FES?
Spasticity & Tone
Moderate to severe spasticity → may favor AFO
Minimal tone issues → FES may be appropriate
SO HOW DO WE CHOOSE TO USE AFOs or FES?
Volitional Motor Control
Present but weak DF = FES can facilitate activation
Absent DF = AFO provides stability & safety
SO HOW DO WE CHOOSE TO USE AFOs or FES?
Fatigue and Endurance
If fatigue limits function → AFO can reduce energy cost
FES may be fatiguing for prolonged ambulation
SO HOW DO WE CHOOSE TO USE AFOs or FES?
Skin Integrity & Sensation
Impaired sensation or fragile skin → use caution with FES electrodes
SO HOW DO WE CHOOSE TO USE AFOs or FES?
Cognition & Compliance
FES requires more active participation, setup, and troubleshooting
AFO is more passive, easier to don/doff
Short Answer: AFO vs FES
When AFO’s and FES are directly compared one device is not superior to another in the ability to improve outcomes of QOL, gait speed, other mobility, dynamic balance, endurance, and little in gait kinematics.
No evidence was found to directly compared muscle activation
Long Answer: AFO vs FES
AFO
Inclusion of an AFO may demonstrate better immediate effects.
Increase an individual’s ability to participate at a higher level in the rehabilitation process.
AFO more effective in acute phase in individuals walking at slower gait speed or lower baseline mobility.
AFO may be most effective at improving balance confidence when compared to FES
FES
↑ User satisfaction and patient preference may be higher with FES
Greater therapeutic effects
Better choice for individuals walking at faster speeds or higher baseline mobility.
Expensive
Risk of Abandonment
AFO
Difficult to don and doff
Not clear on intent or benefits of device
Too much mobility restriction
Discomfort
Cosmesis
Skin irritation
Risk of Abandonment
FES
Intolerance to the sensation
Insufficient DF achieved (recommended ≥ stage 3)
Skin irritation
Challenges with electrode placement
AFO vs FES
Body Structure and Function Exam Considerations
Force Production
Amount of control needed to correct an abnormal movement pattern
Support needed to assist movement
Potential to improve active movement
AFO vs FES
Body Structure and Function Exam Considerations
Sensation/Integumentary
Crude touch/ Nociception: Can the individual perceive discomfort related to skin irritation or breakdown?
Swelling or edema present
AFO vs FES
Body Structure and Function Exam Considerations
ROM/Alignment
Does the individual have adequate ROM for the motions allowed by the device?
Does the individual require support to prevent contractures?
AFO vs FES
Body Structure and Function Exam Considerations
Cognition
Can the individuals and/or caregiver appropriately maintain and don/doff the device?
Quick Summary of AFO Decision Making Algorithm
PD
Gait Training
Physical therapists should implement gait training
Evidence Quality = HIGH // Recommendation Strength = STRONG
PD
Gait Training
Benefits
improvements in:
Reduced motor disease severity
Step length
Walking speed
Walking capacity
Functional mobility
Improved balance
PD
Gait Characteristics
Shuffling
Shortened step length, decreased foot clearance and flexed knees and hips
Rigid trunk and decreased/asymmetrical arm swing
Bradykinesia, worsens with dual tasking
PD
Gait Characteristics
Festination Anteropulsion
COM gets to far anterior, “run away train” (leads to falls)
TRIGGERS: wheeled walkers without hand breaks, forcing through a freeze, being pulled on during a freeze
PD
Gait Characteristics
Festination Retropulsion
COM gets too far posterior, Under scaled balance reaction, small steps to recover (leads to falls).
TRIGGERS: backing up, reaching overhead, opening door, carrying items too close to body
PD
Gait Characteristics
Freezing of gait (akinesia)
TRIGGERS: Tight/narrow spaces (doorways, elevators), cluttered areas, crowds, anxiety/stress/rushing, turning/pivoting, change in floor pattern
PD
External Cueing
Physical therapists should implement external cueing to reduce motor disease severity and freezing of gait, and improve gait outcomes
Evidence Quality = HIGH // Recommendation Strength = STRONG
Cueing including visual, auditory (rhythmic auditory stimuli), or somatosensory cueing superior in comparison to no cueing
No one mode of cueing is superior to another
PD
External Cueing
Benefits
improvements in:
Motor disease severity
Spatiotemporal parameters of gait (gait speed, stride length, cadence)
Functional gait outcomes (mobility, turning & distance walked)
Freezing of gait
PD
Visual Cueing
Most commonly used for gait training
Improve Step Length
150% longer than current
Target = 40% of patient height (24-28 inches)
Improve Turning
Improve Initiation of Gait
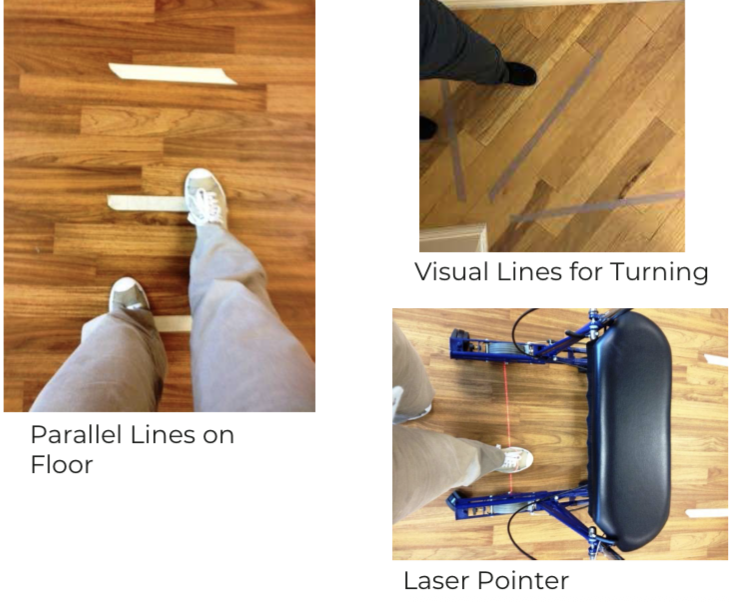
PD
External Accessories

PD
Auditory Cueing
Rhythmic cueing with use of metronome, music, clapping or snapping
Used with all exercises
PNF patterns – axial rotation
Stepping –
25% faster than baseline
100-125 bpm – for higher functioning patients
Resistance Exercise
Boxing
PD
Freezing of Gait
4 S’s
stop
stand tall
relax
correct posture
get COM over BOS
sway
step long/big
PD
FESTINATION of Gait
3 S’s
stop
stand tall
relax
correct posture
get COM over BOS
step long/big
Why Exercise and Movement Matter for Parkinsons Disease
Neuroplasticity: use it or lose it
Delays motor decline
Improves quality of life and ADLs
Encourages social connection and autonomy
PD
What is LSVT BIG?
Think Big, Move Big
= Lee Silverman Voice Treatment
Expanded from LSVT LOUD to movement-based therapy
4-week, 16-session protocol
PD
What is LSVT BIG?
The BIG Approach
Focus: amplitude (bigness) of movement
Intensive, repetitive, task-specific practice
Trains automaticity and recalibrates perception
PD
Evidence Behind LSVT BIG
Improved gait speed and stride length (decreased shuffling)
Better balance and reduced fall risk
Enhanced ADL participation
PD
What is PWR!?
Parkinson’s Wellness Recovery
Created by Dr. Becky Farley, LSVT BIG developer
Builds on BIG principles
need for a broader, more adaptable movement system, one that not only trained amplitude, but also incorporated flexibility, balance, and coordination
Includes 4 foundational “PWR! Moves”
PD
The 4 PWR! Moves: Foundation and Function
PWR! UP: postural extension
helping counteract the stooped posture by activating the extensor muscles
PWR! ROCK: weight shift
provides weight shifting, which is critical for improving balance, initiating movement, and reducing fall risk
PWR! TWIST: axial mobility
works on the axial mobility rotational movements through the spine and trunk that are essential for tasks like rolling in bed or turning while walking
PWR! STEP: transitional movement
emphasizes transitional movements, helping patients move confidently from one position or place to another, like sit to stand, stepping over obstacles, or navigating tight spaces
PD
What is Rock Steady Boxing? Rock Steady Boxing: Fight Back
Non-contact boxing program for PD
Combines agility, strength, balance, and coordination
Group-based, high-intensity
heavy bag punching, footwork drills, and core strengthening
PD
Rock Steady Boxing
Warm-up, drills, shadowboxing, mitt work
drills and shadowboxing to work on form, coordination, and motor planning
Mitt work allows for precision and reaction time
Voice activation and dual-tasking
helps with vocal strength and projection
Aerobic conditioning
boost cardiovascular health and overall endurance
PD
Rock Steady Boxing
Benefits
Improved balance and coordination
Increased strength and endurance
Reduces depression, apathy
PD
LSVT Review
focus: amplitude
format: 1:1, 4 weeks
intensity: high
use case: early-mid PD
PD
PWR! Review
focus: function, variety
format: 1:1, group
intensity: moderate-high
use case: lifelong integration
PD
Rock Steady Review
focus: conditioning
format: group
intensity: high
use case: community-based
PD
How to Choose and Apply Therapy
Consider stage, goals, and access
Start with 1:1, move toward group
Cross-train and re-evaluate quarterly