unit 1 cardiac
1/95
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
96 Terms
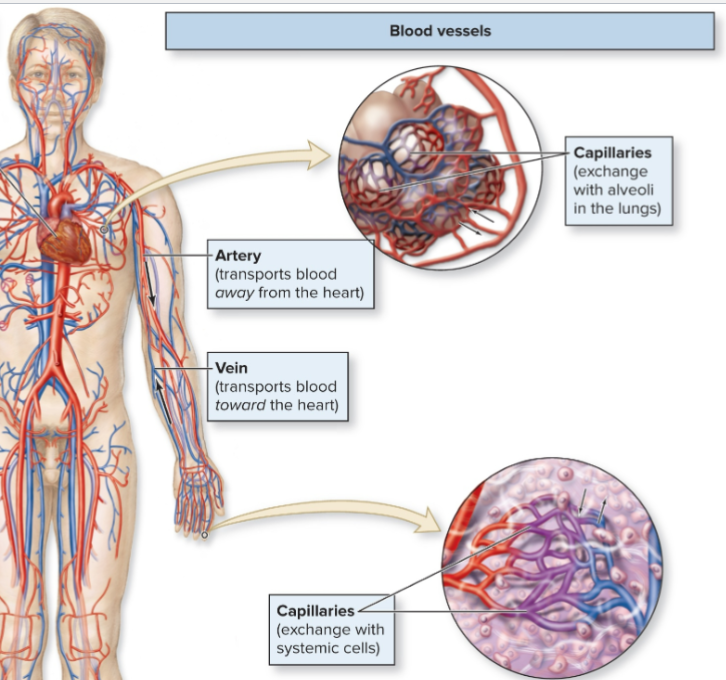
main function of cardiovascular (CV) system
transport blood thru body
deliver O2 (nutrients) and remove Co2 (waste)
3 basic components of CV system
1) heart - pump blood
2) blood vessels (BV) - carry blood to body and back to heart
3) blood - contains O2 and CO2
3 types of blood vessels
-artery = AWAY from heart to body. *usually oxygenated
-vein = TO heart from body. *usually deoxygenated
-capillary =tiny BV. exchange with cells such as alveoli (lung) or eye
Perfusion
amount of blood being delivered to tissue at one time.
Adequate perfusion: sufficient delivery to maintain cell health
→ Requires continual pumping of the heart and open, healthy
vessels
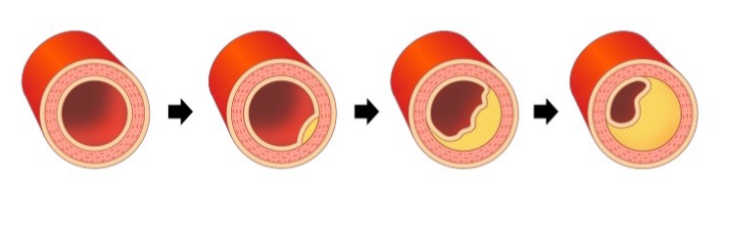
What can impact perfusion?
-occlusion = cholesterol buildup blocking BV
-can lead to heart attack, cardiac arrest
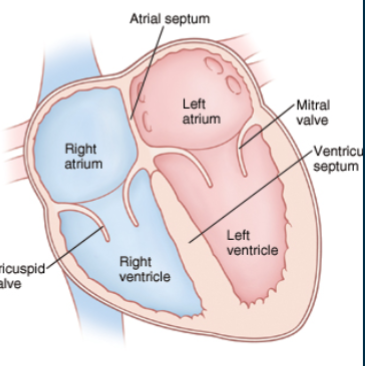
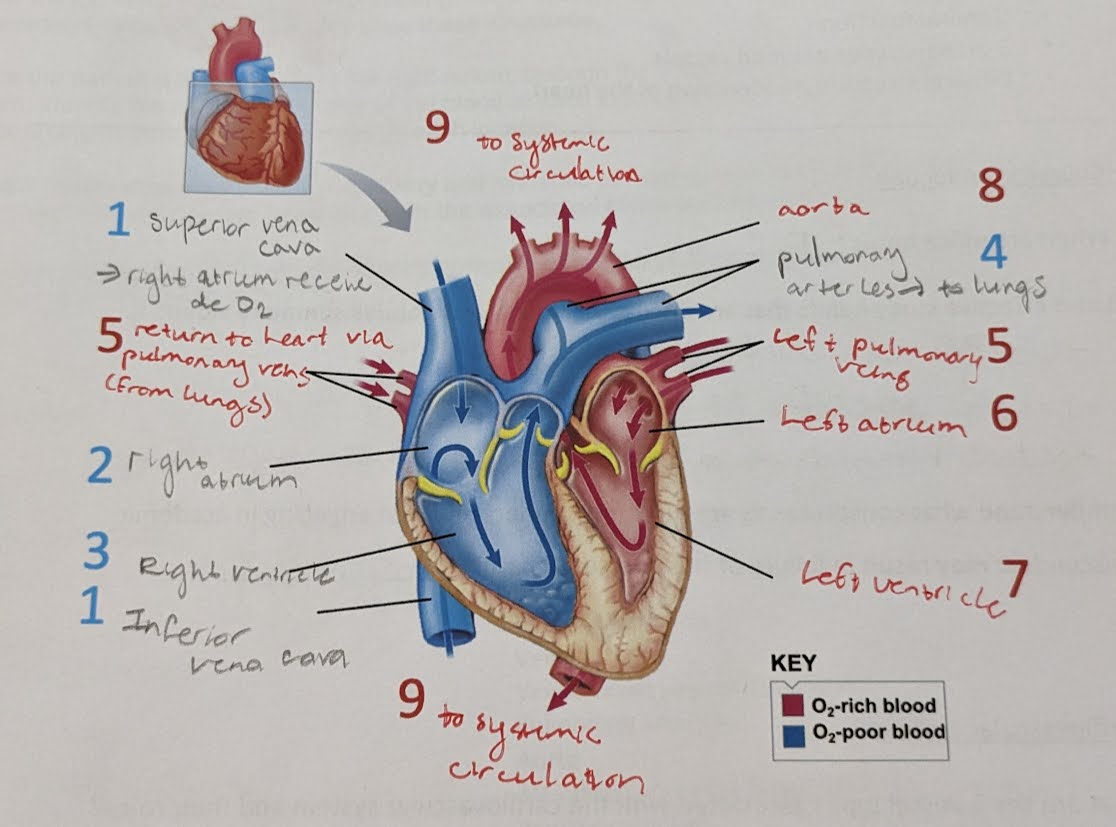
Atria vs Ventricles
-atria = upper 2 chambers. receive blood and transfer to lower chambers
-ventricles = lower 2 chambers. pump blood out from heart
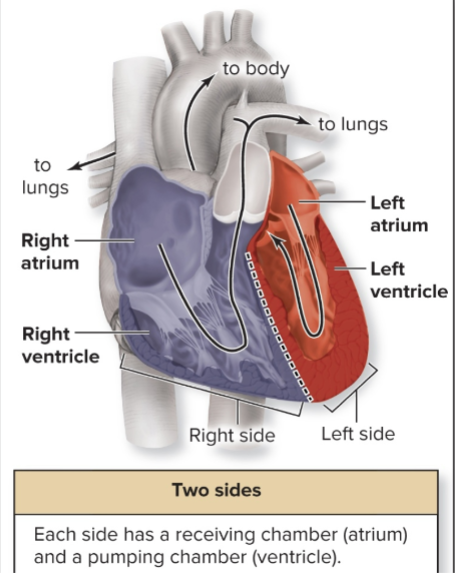
Dual pump - What do the 2 sides of the heart do? (R vs L)
2 sides of the heart function as 2 separate pumps
-Right side receive deoxygenated blood from body → pump to lungs
-Left side receive oxygenated blood from lungs → pump to body
-septum = tissue in the middle separates the 2 sides
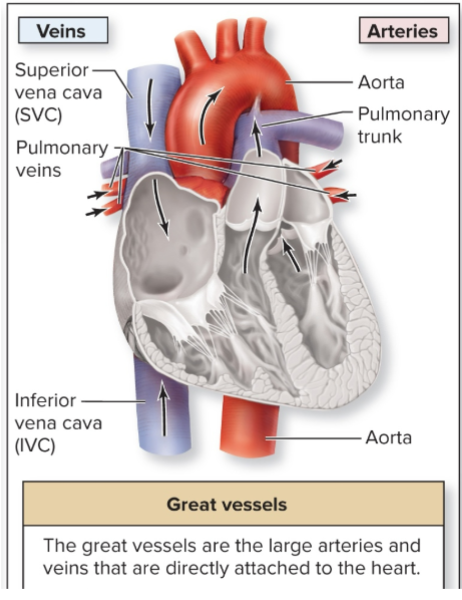
Great Vessels
transport blood to and from heart chambers
-remember, arteries AWAY from heart, veins TO heart
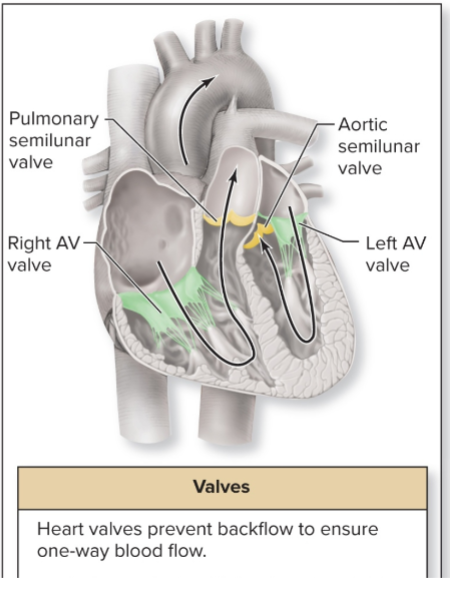
2 sets of heart valves
ensure one-way flow thru heart
-Atrioventricular (AV) valves = Sit between atrium and ventricle of each side
-Semilunar valves = Sit at boundary of ventricle and arterial trunk
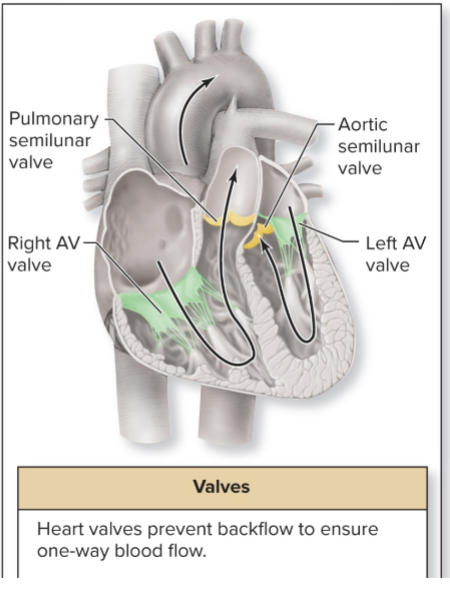
tricuspid & bicuspid valves. Which is R & L?
Tricuspid = Right AV valve
Bicuspid/Mitral = Left AV valve
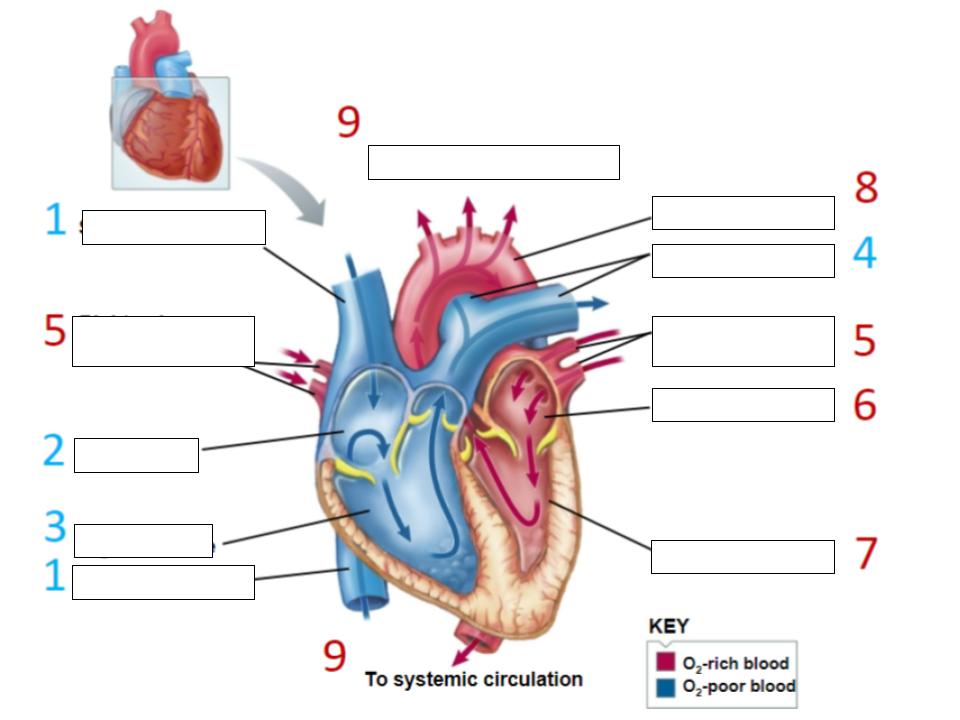
Trace the path blood takes thru the heart (image)
https://www.geoguessr.com/vgp/3805
Geoguessr quiz link for heart
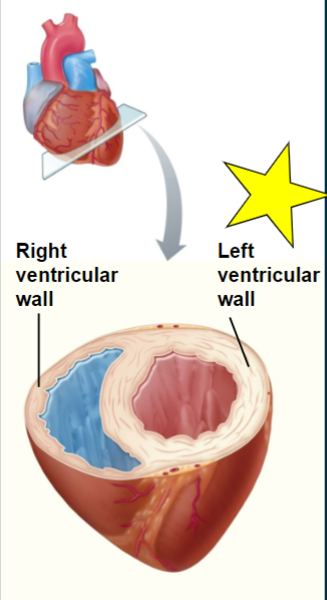
Which ventricle is thicker? Why?
LEFT ventricle.
→ it needs to pump to the whole body which requires more force than simply pumping to the lungs
*however, the amount of blood moved is the same as right side
Where in the body do R & L side of heart pump blood?
Both sides of heart pump same vol. of blood
• Right side- pumps to lungs
→ Low pressure
• Left side- pumps to systemic circulation
→ High pressure: blood pressure thru vessels (friction)
cardiac circulation vs systemic circulation
cardiac = circulation btwn heart and lungs
systemic circulation = blood circulation anywhere else in body
autorhythmicity
the heart can contract on its own without input from the brain
→ heart cells can spontaneously depolarize
autorhythmic cells
Do not contract
1% of cells in myocardium
• Do not contract
• Specialized for initiating and conducting action potentials that contract the working cells
autorhythmic (nodal) cell characteristics
-cells in SA node initiate heartbeat → spontaneously depolarize
-do not have a RMP = has many common membrane proteins
• Na/K pumps, Ca pumps, leak channels
-also has specific voltage gated channels
• slow Na VGC = FUNNY channels
• fast/slow Ca VGC
• K VGC
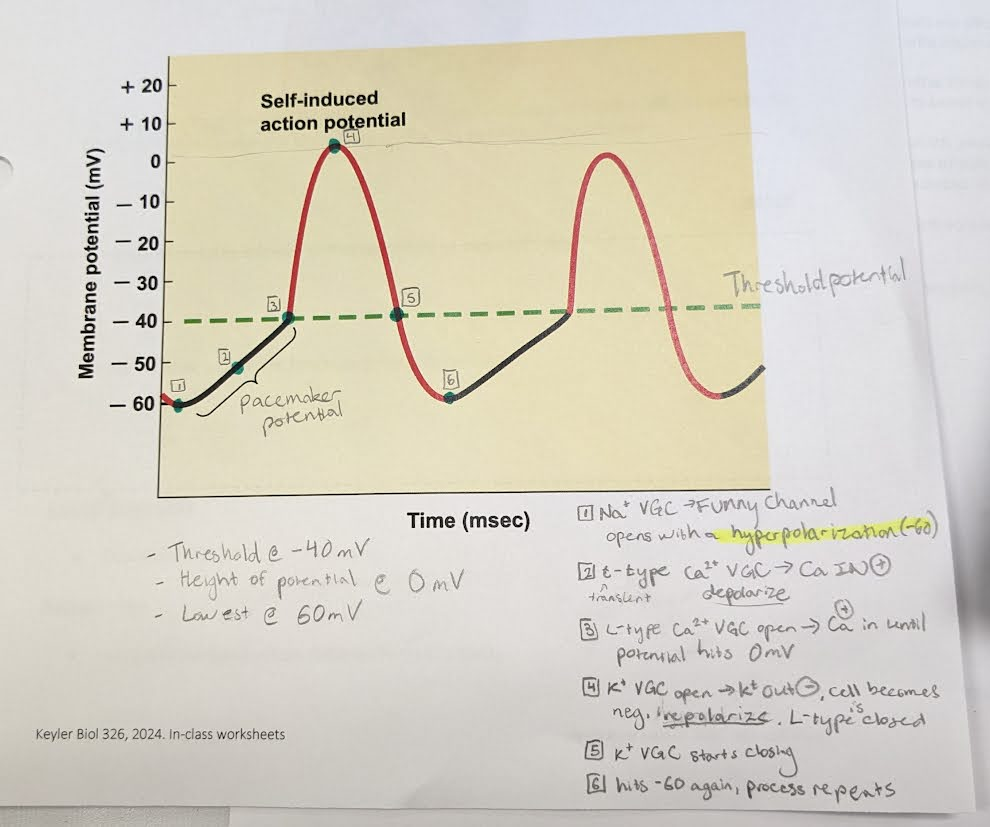
What is a funny cell?
slow Na+ voltage gated channel
-they are ‘funny’ because they are activated by a hyperpolarization, not a depolarization
-activated at -60 mV
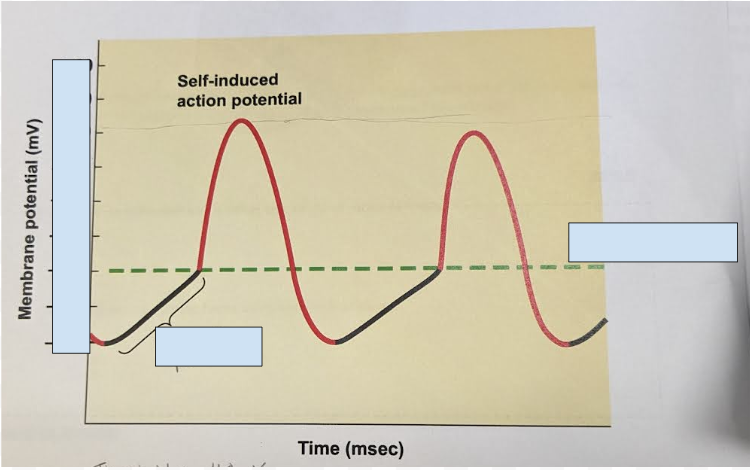
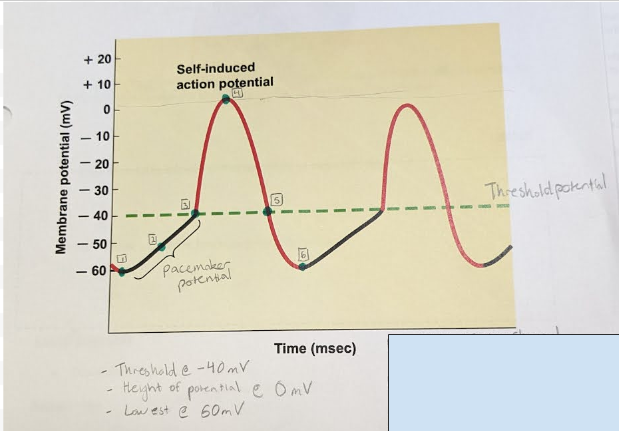
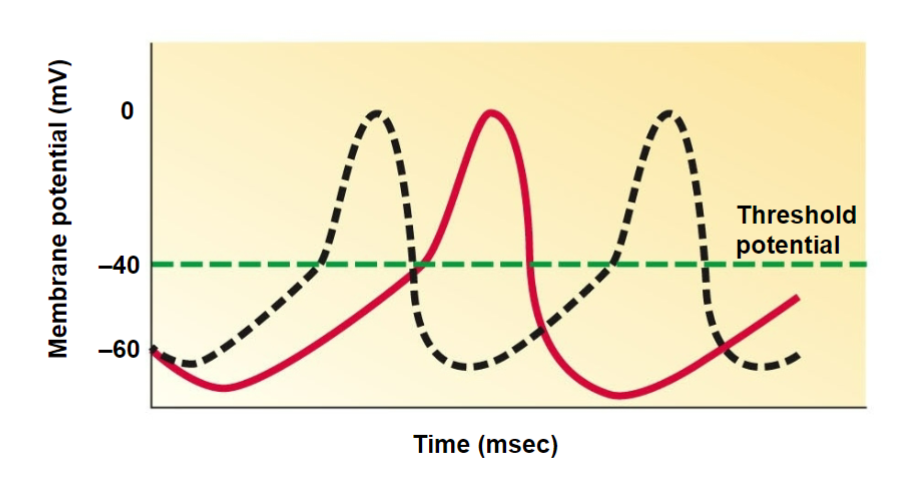
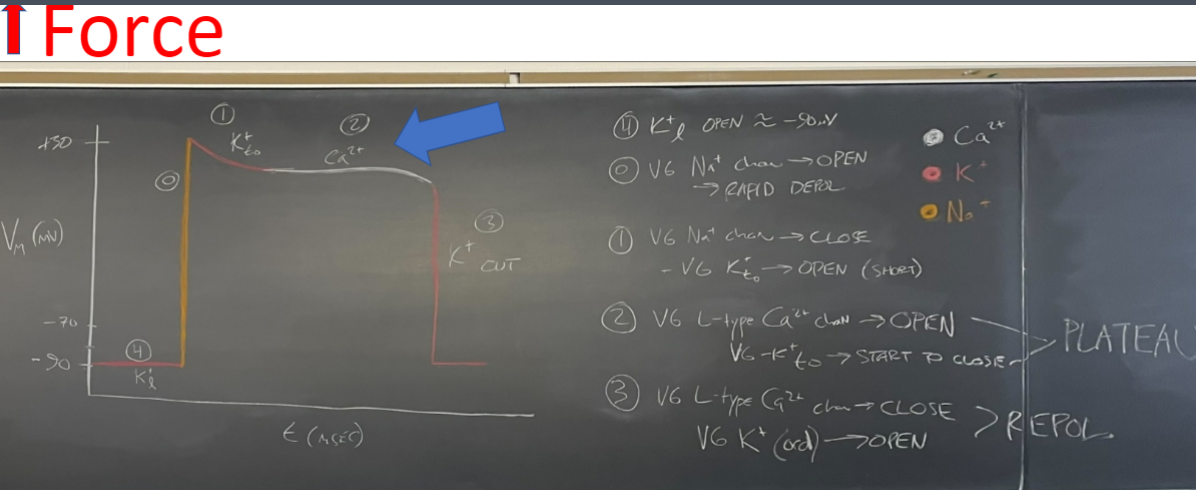
label the areas and state
-mV of threshold
-mV that activates Funny cells
-mV at potential peak
threshold = -40 mV
funny cell activation = -60 mV
peak potential = 0 mV
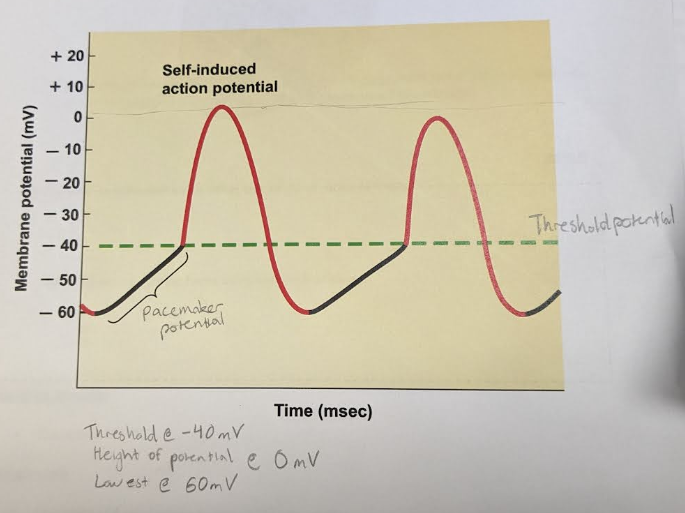
label the steps of contraction for an autorhythmic cell
*note - even tho funny channels open in a hyperpolarization, sodium will still rush in and depolarize the cell. only difference is gate opens when negative
-
khan academy video: https://www.khanacademy.org/science/health-and-medicine/circulatory-system/heart-depolarization/v/action-potentials-in-pacemaker-cells
2 main events of heart contraction (overview)
1) The conduction system propogates an AP→ moves from nodal cells to contractile cells via gap junctions
2) AP spreads to cardiac muscle cells, contraction of sarcomere
→ atria contracts first, then ventricles contract
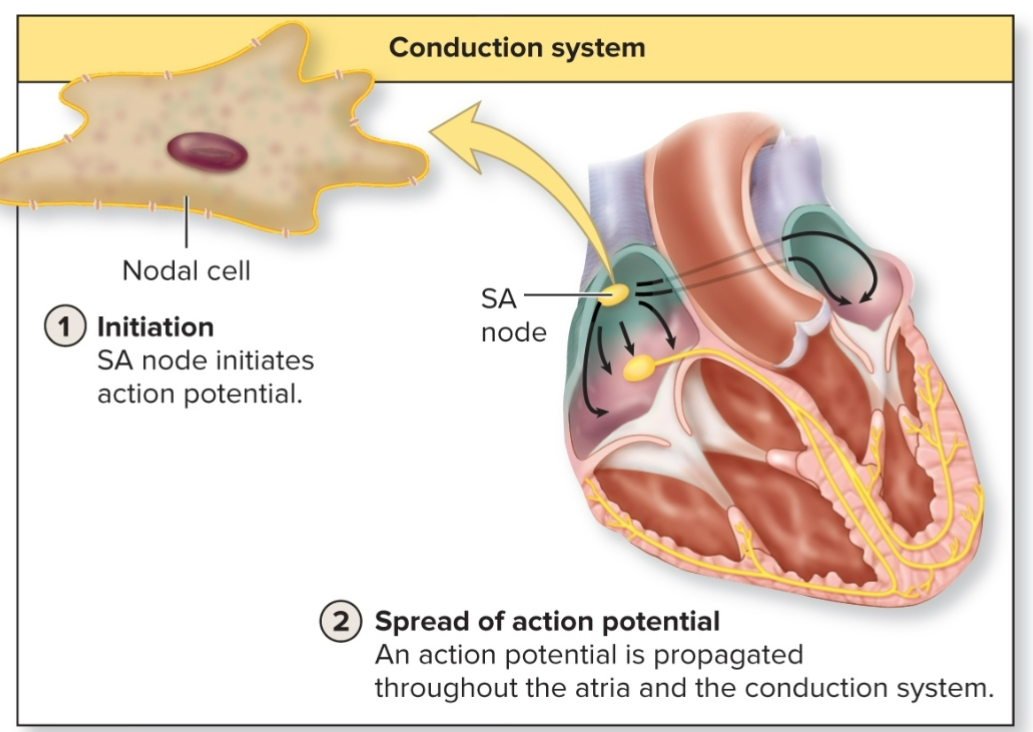
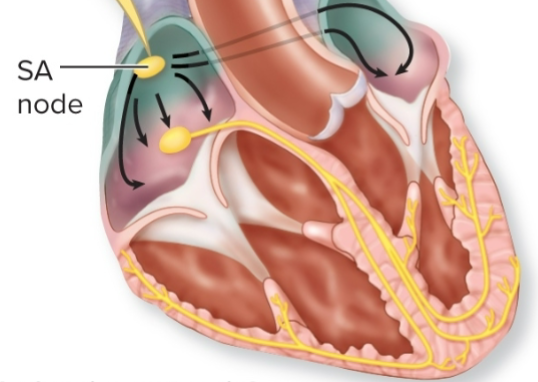
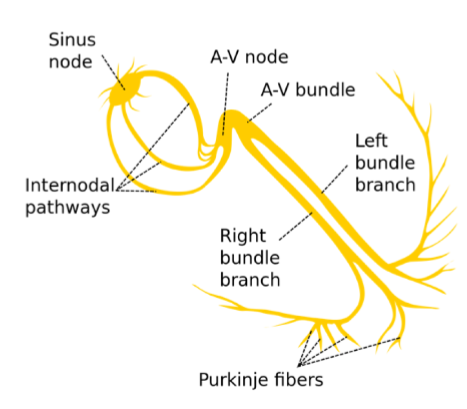
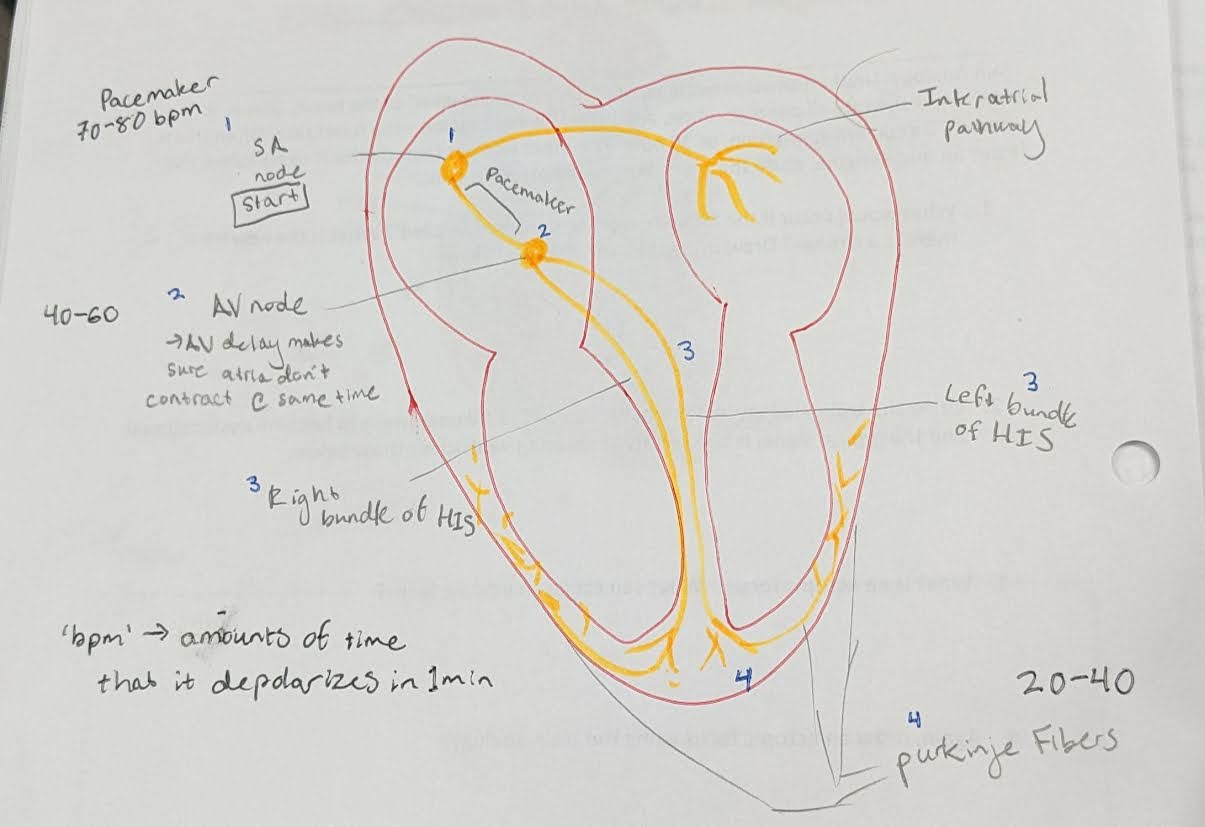
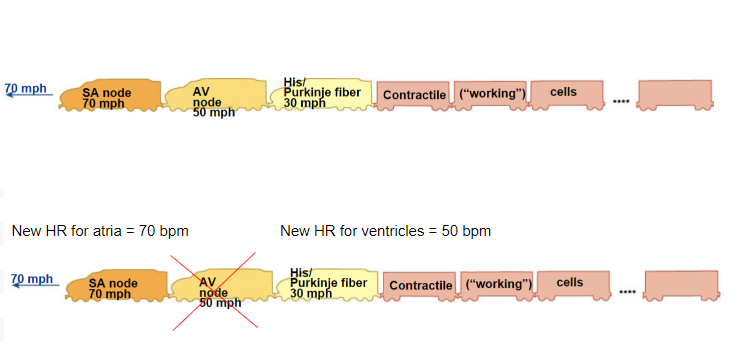
what is the conduction pathway? What order does it depolarize in?
pathway that AP travels inside the heart
SA node → AV node → Bundle of HIS → Purkinje fibers
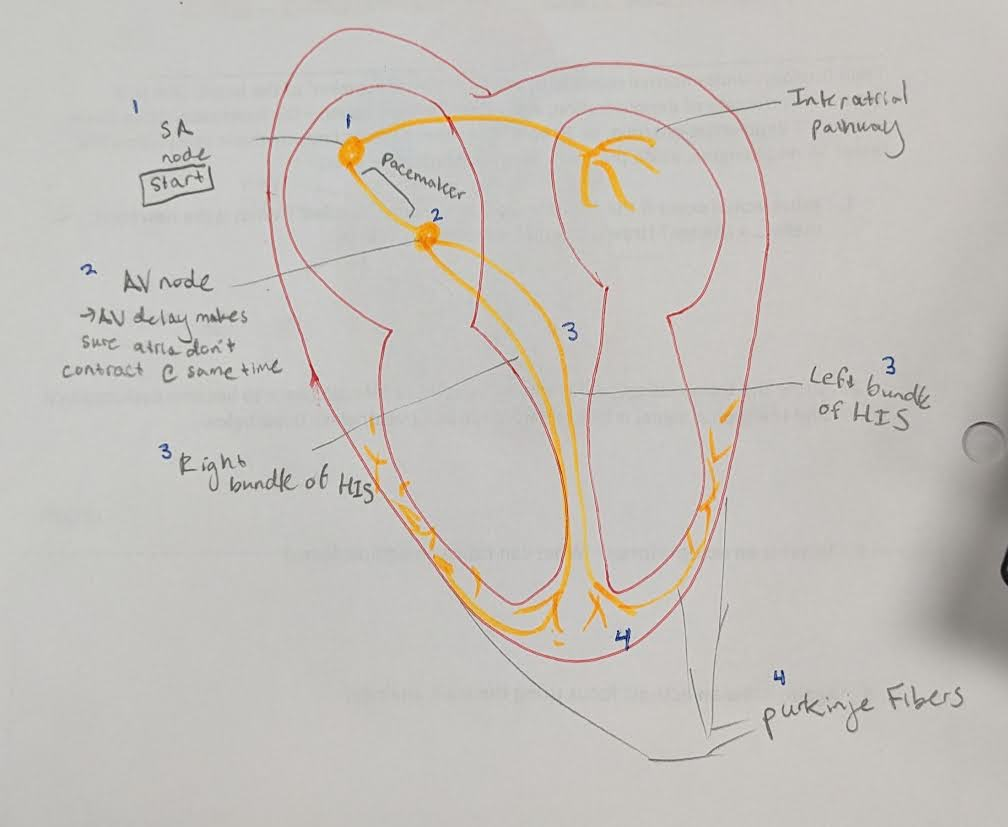
Name the different bpm of each area in the contractile pathway (SA, AV, HIS/Purkinje)
What rate does the heart go if each area is a diff bpm?
SA = 70 → pacemaker. whole (healthy) heart goes 70 since it’s the ‘start’ node.
AV = 50
HIS/Purkinje = 30
What happens if your SA node stops but the rest of the heart still works?
AV node goes 50. AV node takes over, new bpm is 50.
Heart still works but is slower
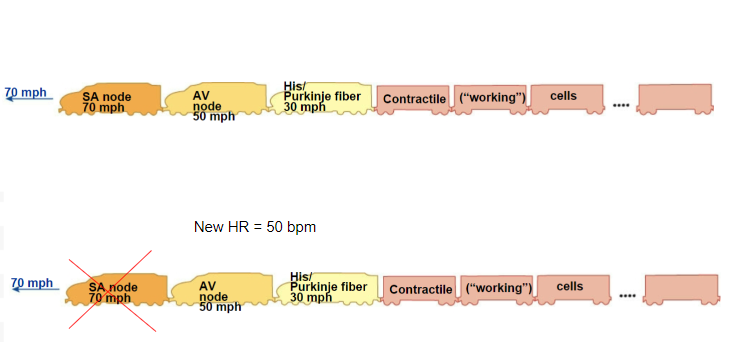
What happens if your AV node stops but the rest of the heart still works?
SA node is still going 70, but no communication to the other parts of the heart.
Other parts of heart (HIS & Purkinje) still working, but at 30. Atria going 70bpm, but ventricles going 30bpm.
Heart still works but is inefficient
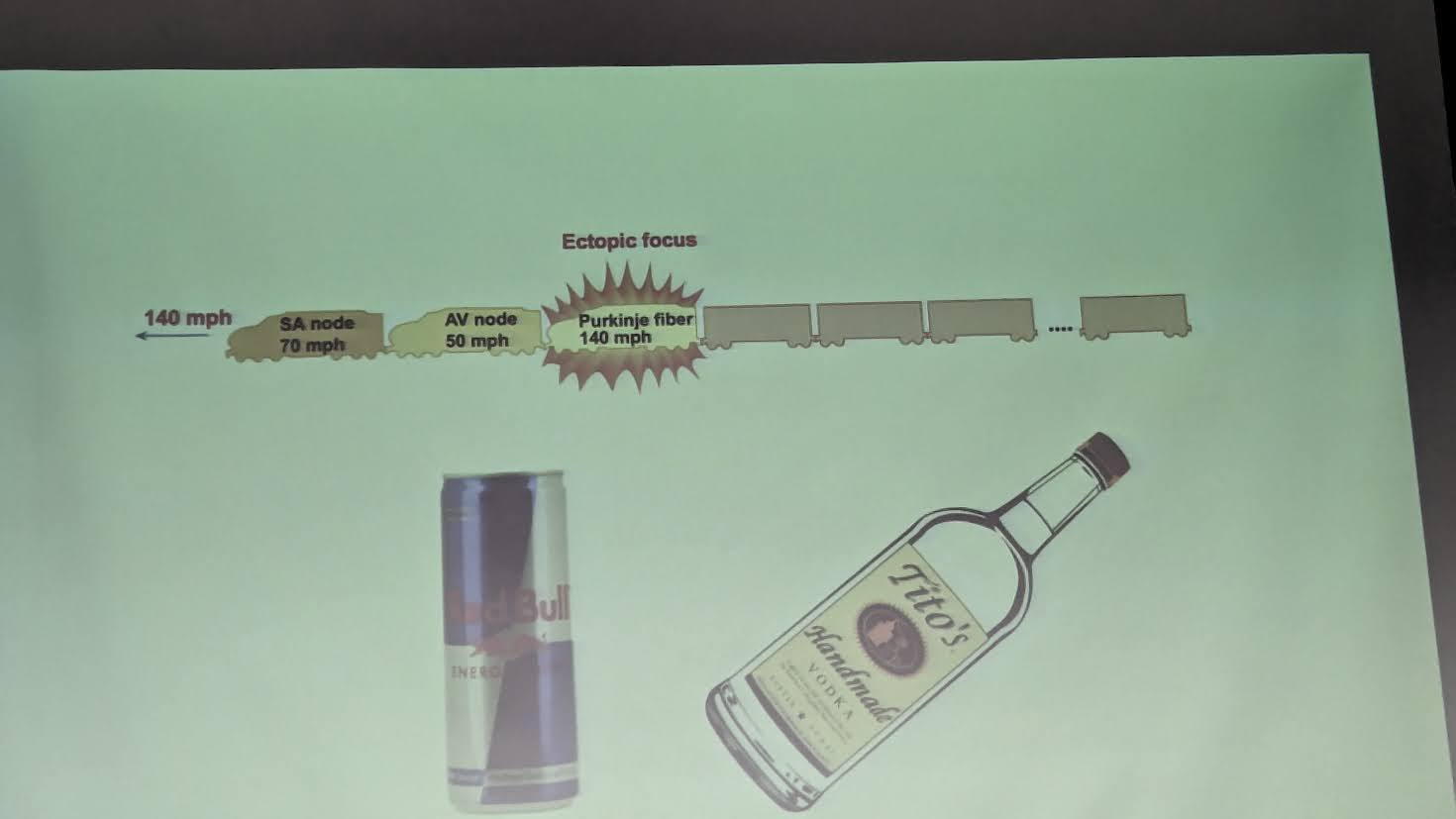
what is ectopic focus?
when HR goes to a very high rate, originating from anywhere other than the “start” point. (SA node)
-HR becomes out of wack
-can happen mixing caffeine with alcohol
contractile cells
99% of cardiac muscle cells
• Do mechanical work of pumping
• Normally do not initiate own action potentials
contractile cell characteristics
-highly vascularized → need O2 aerobic
-striated, has sarcomeres
-very small, big SA ratio for transport
-has a resting mV (-90)
-K+ leak channels, Na+ leak, Na/K pump
-branched, connected by intercalated disc
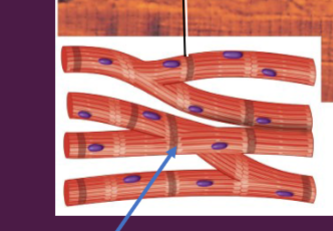
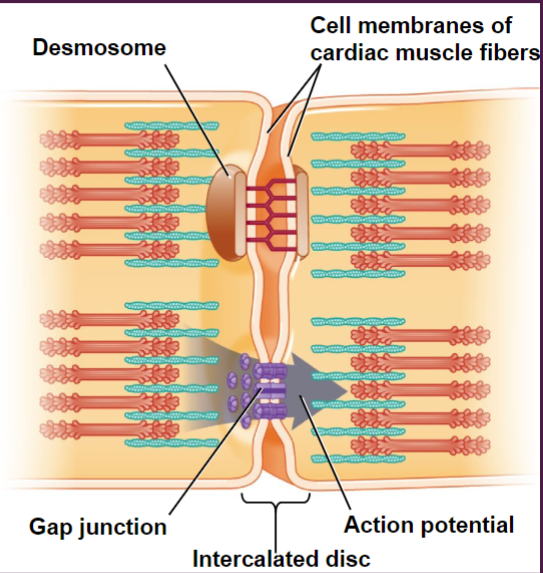
name the 2 junctions in an intercalated disc
1) desmosome
2) gap junction
together they form the functional syncitia → contract as single unit
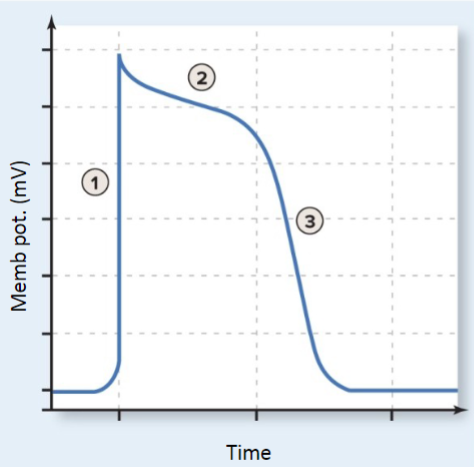
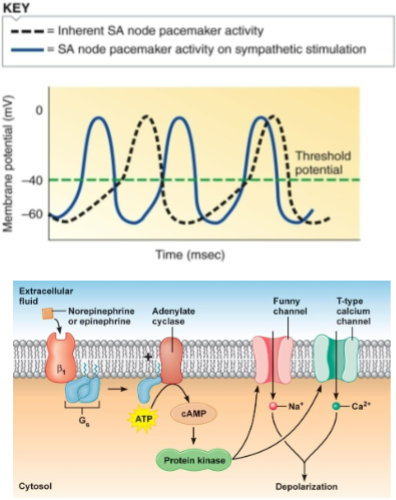
name the 3 steps of contractile cell
1) depolarization (charge comes from autorhyth. cell)
2) plateau
3) repolarization
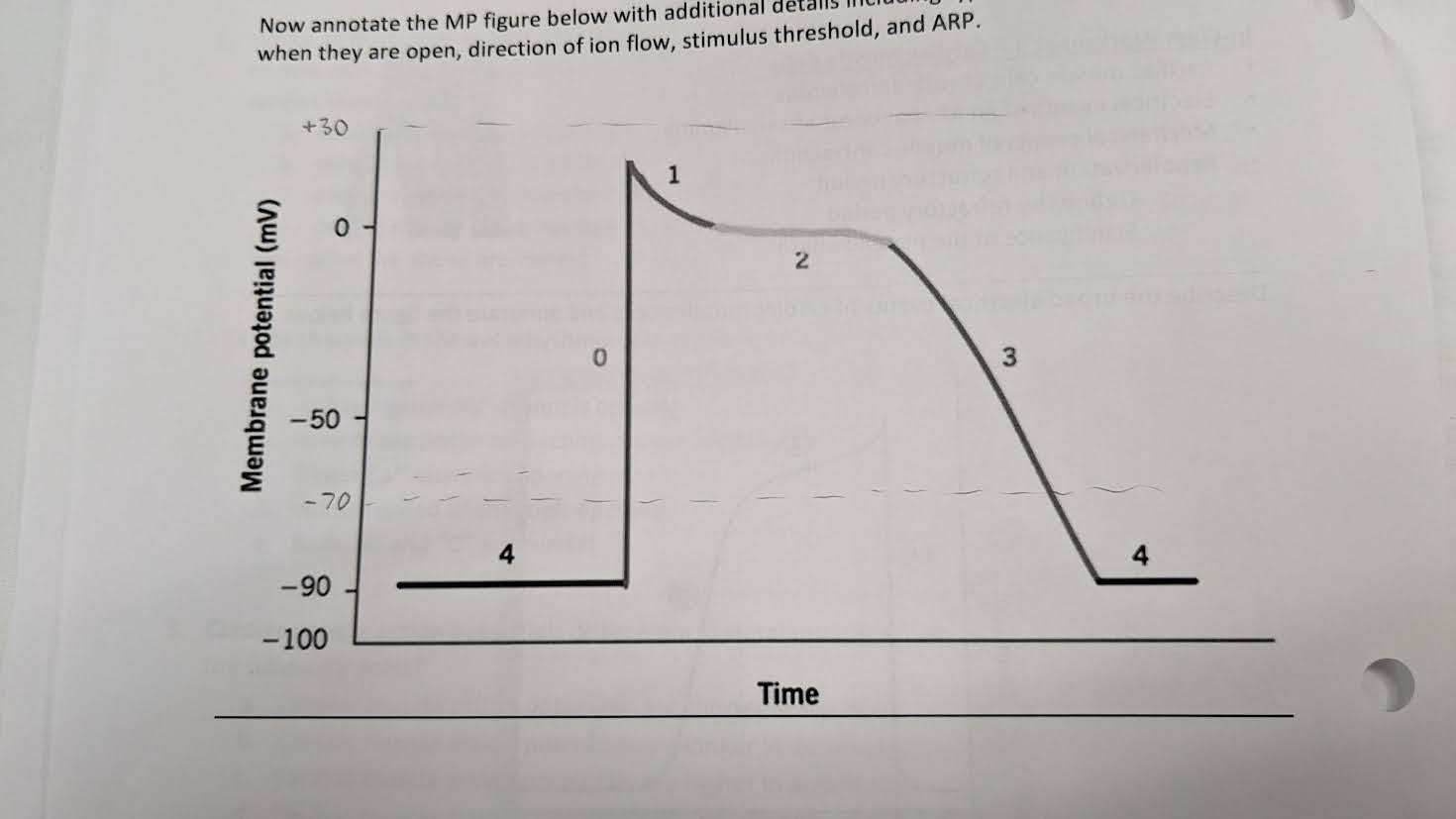
name the 4 steps of contractile cell AP. which ions are moving during each step?
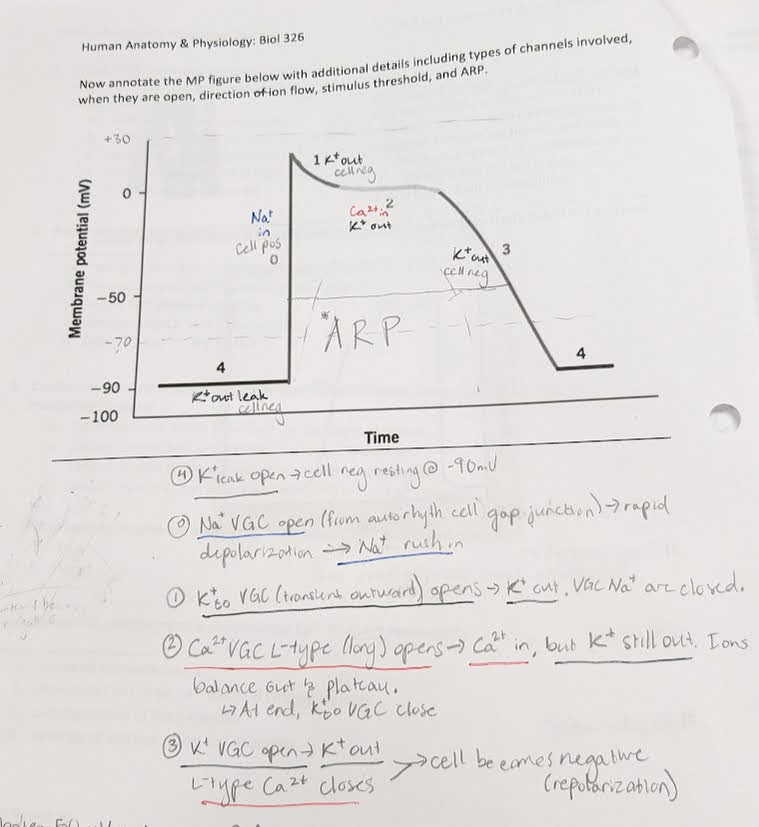
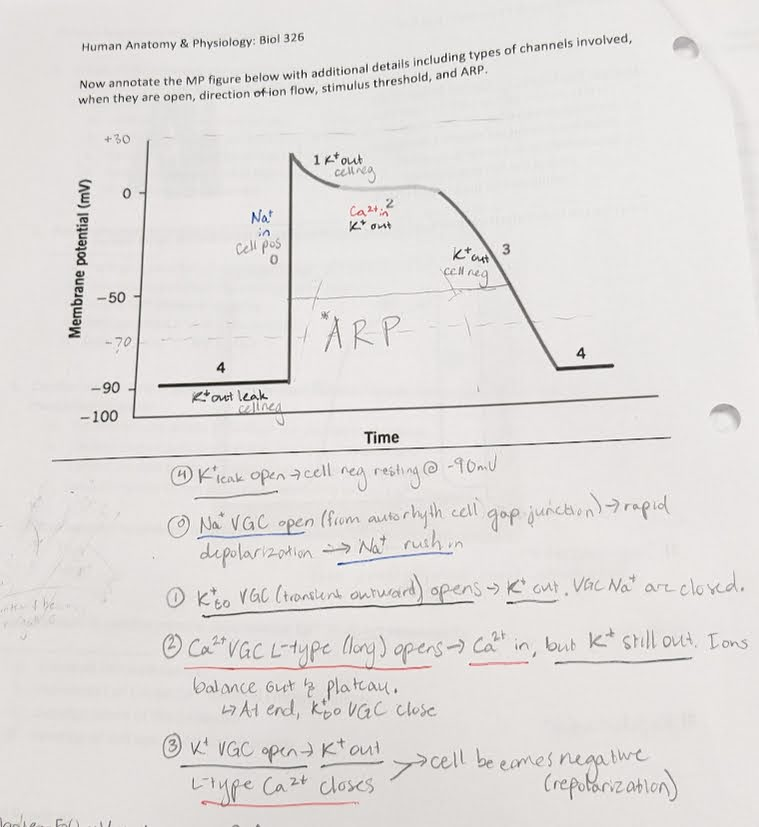
Why does a cardiac contractile cell have an absolute refractory period (ARP)? Why is this important?
-allows alternate period of contraction & relaxation
-prevents tetany so heart can beat → pump blood
define Calcium-induced calcium release (CICR)
Ion pumps located in the sarcolemma create a gradient and move Ca outside the cell. When an AP comes, L-type Ca VGC opens and Ca moves down gradient into cell. This powers the RyR receptor to release more Ca from the SR. Now the cell has Ca from 2 sources.
Afterward the SERCA pump moves Ca back into the SR (reset gradients)
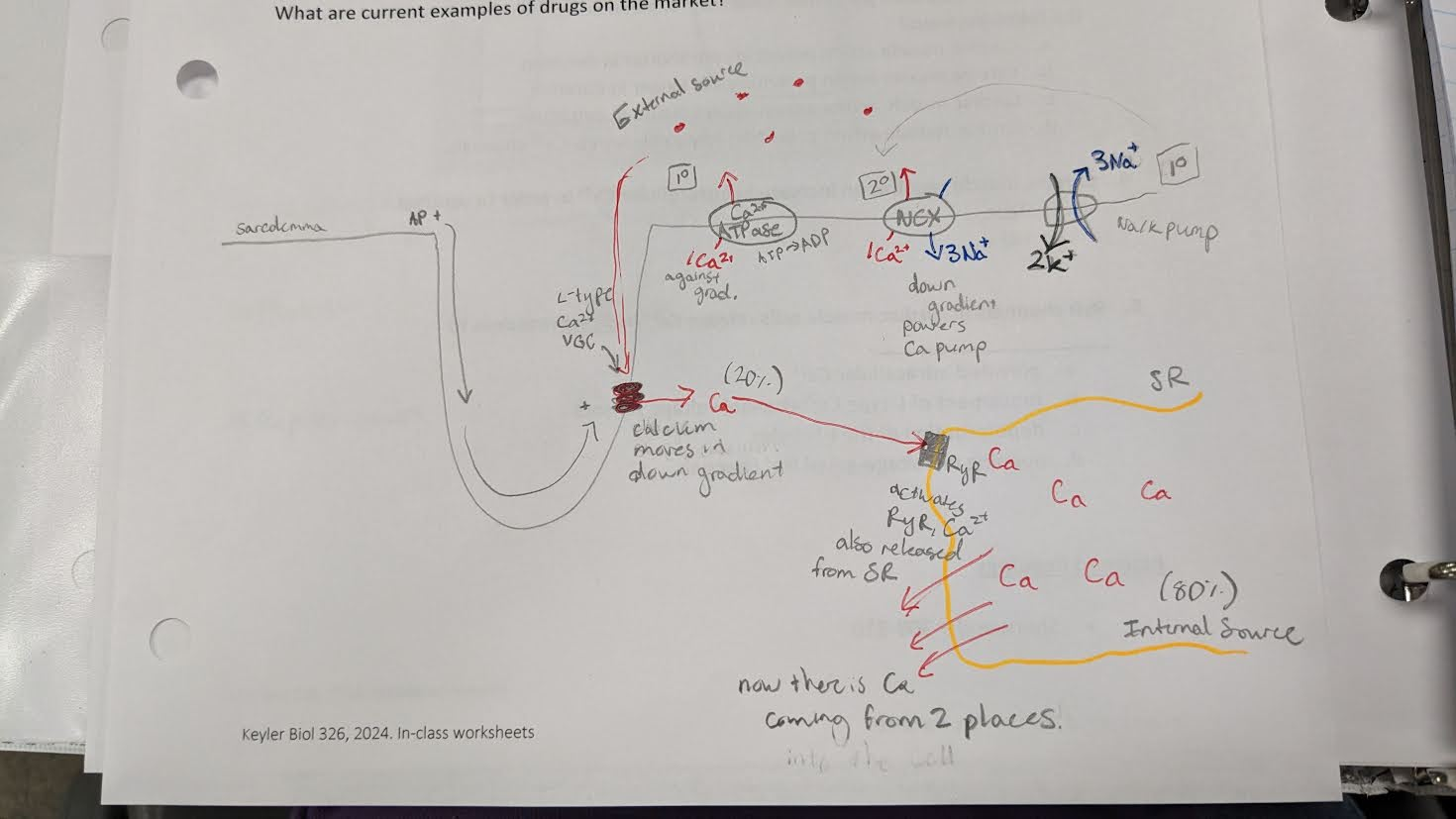
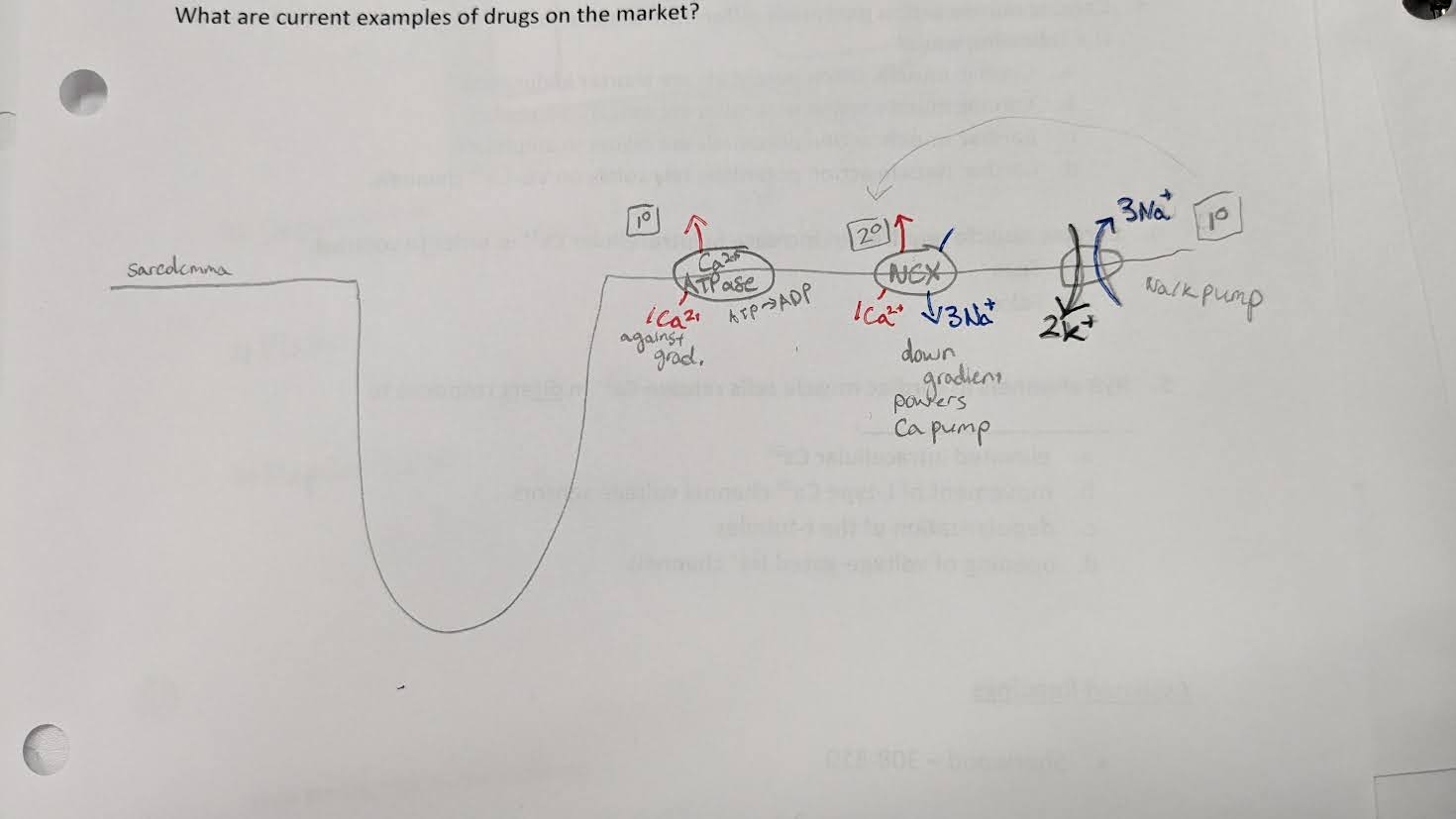
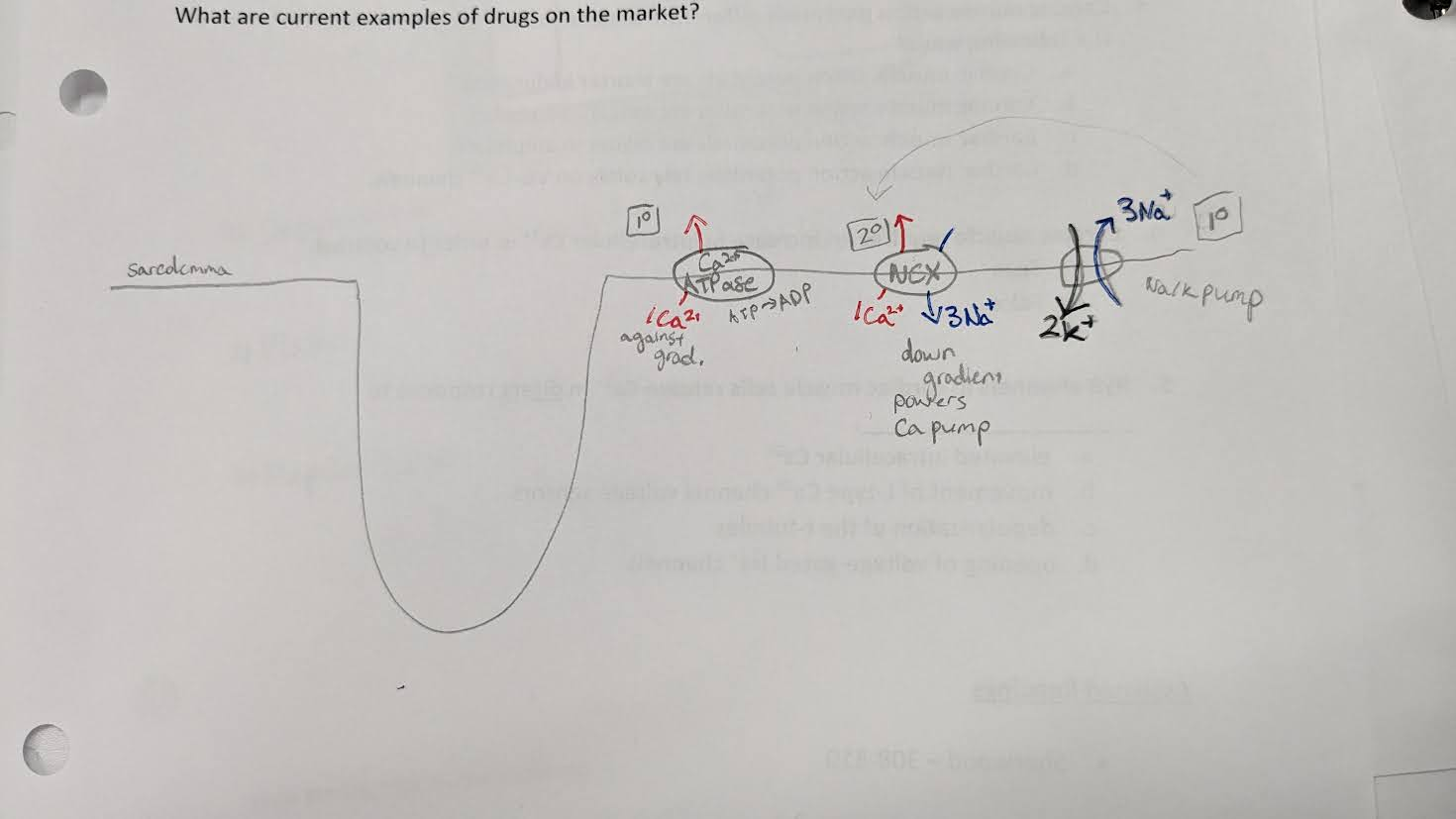
3 ion pumps that are used to create gradient in CICR
1) Na/K pump. 2K in, 3Na out. Primary
2) NCX pump (sodium calcium exchange). 3Na move down gradient to power 1 Ca moving out of cell up gradient. Secondary
3) Ca ATPase pump. ATP splitting used to move Ca out of cell up gradient. Primary
Calcium-induced calcium release (CICR) board drawing only
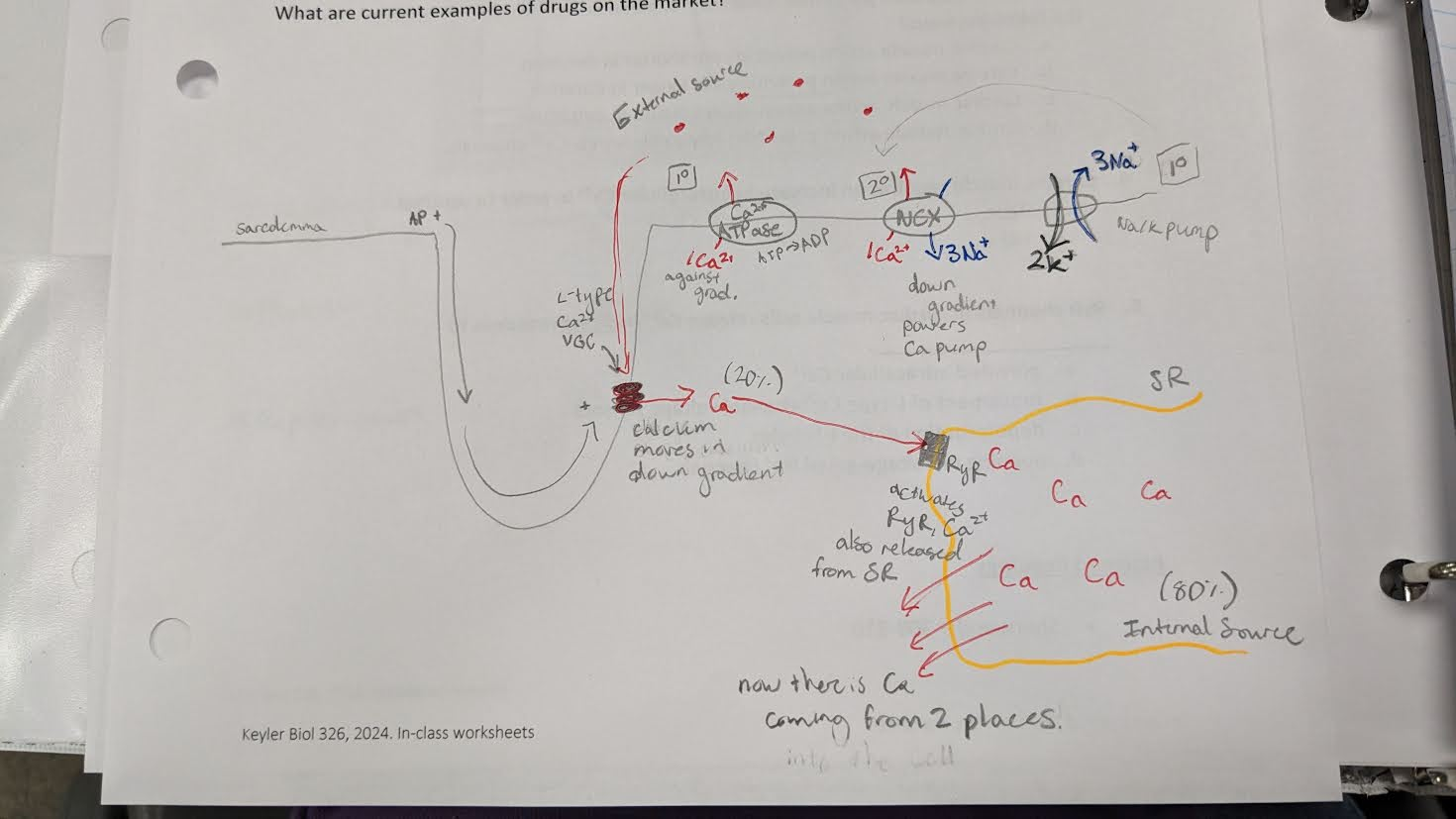
what percentages of calcium in CICR are from external vs internal?
20% is from external calcium
80% is from internal calcium (from SR)
→ most Ca in your cardiac cells come from inside, but you need the outside Ca to activate the SR release
Some people with heart conditions are given calcium channel blockers. How would CCB’s affect the heart? What condition would this drug be useful for?
Calcium channel blockers are medicines used to lower blood pressure. They stop calcium from entering the cells of the heart and arteries. Calcium causes the heart and arteries to squeeze more strongly. By blocking calcium, calcium channel blockers allow blood vessels to relax and open.
→ good for people with hypertension/high BP. dangerous for ppl with low BP
pulmonary circulation vs systemic circulation vs coronary circulation
pulmonary = BV that carry blood btwn heart and lungs
systemic = BV that carry blood btwn the heart and all other body stems
coronary =BV on top of the heart, carry blood to heart
in the coronary supply (outside heart BV) when does the heart receive its blood supply - in systole or diastole?
diastole
during systole, coronary vessels are compressed by the heart contracting. Diastole the heart is relaxed so blood can move thru the outside vessels
how does exercise affect blood flow to the heart?
blood supply to heart can increase up to 5x during exercise
→ heart contracts harder and faster
where does deoxygenated blood go when it exits the coronary blood supply?
goes into right atrium via great cardiac vein into coronary sinus
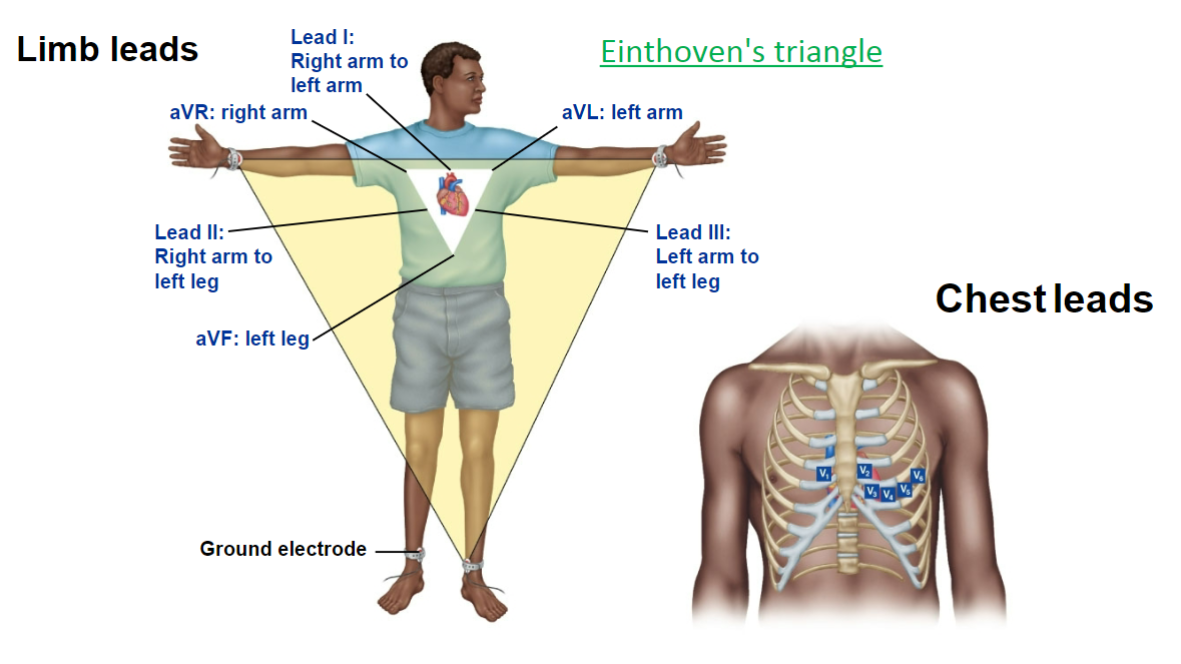
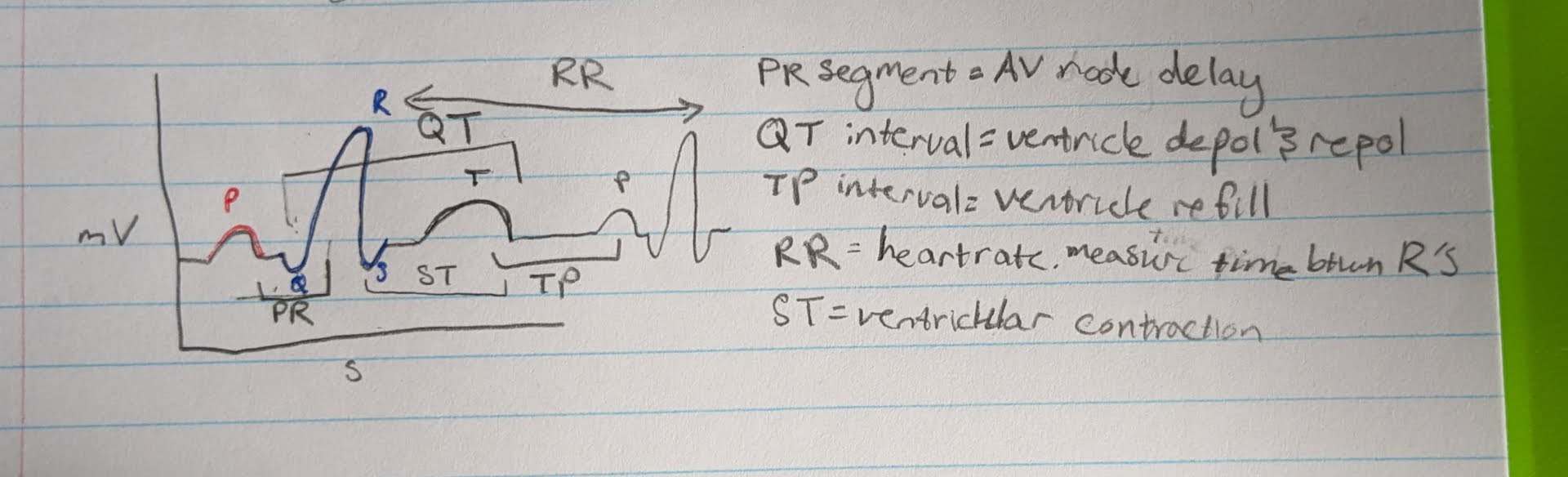
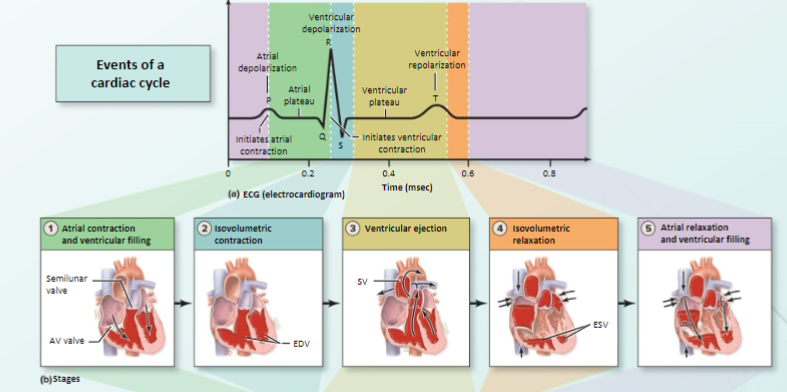
ECG/EKG
electrocardiogram
-look at overall spread of electrical activity of heart thru body (not just one AP)
-a recording of the body fluid current that reaches body surface → NOT a direct recording of actual electrical activity of heart
Einthoven’s triangle, limb leads and chest leads

identify all waves in an ECG
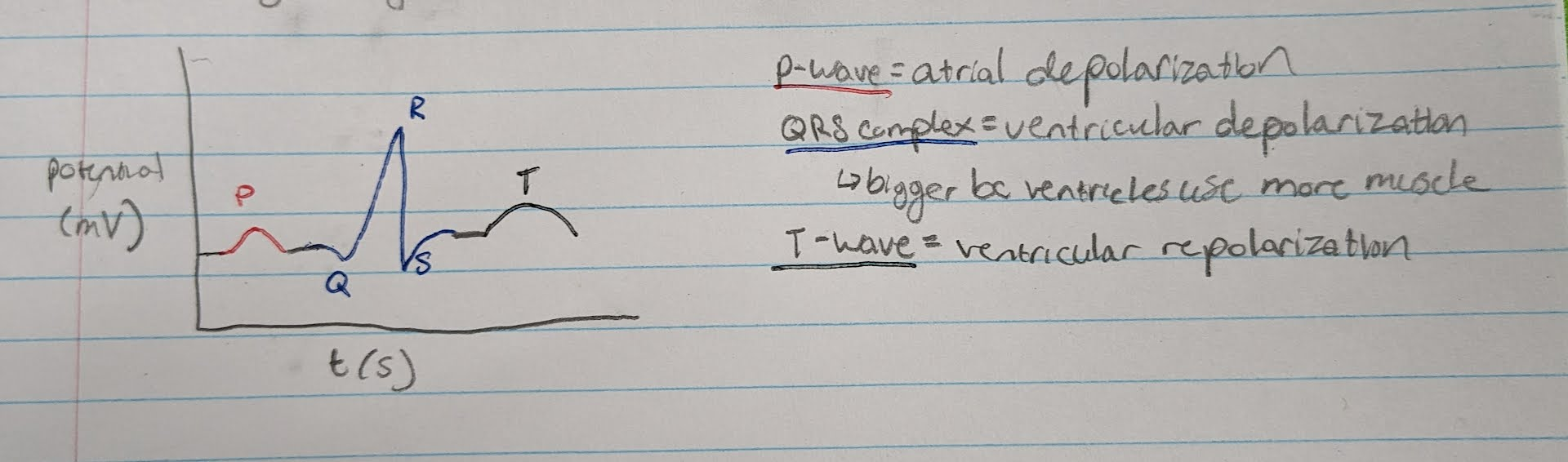
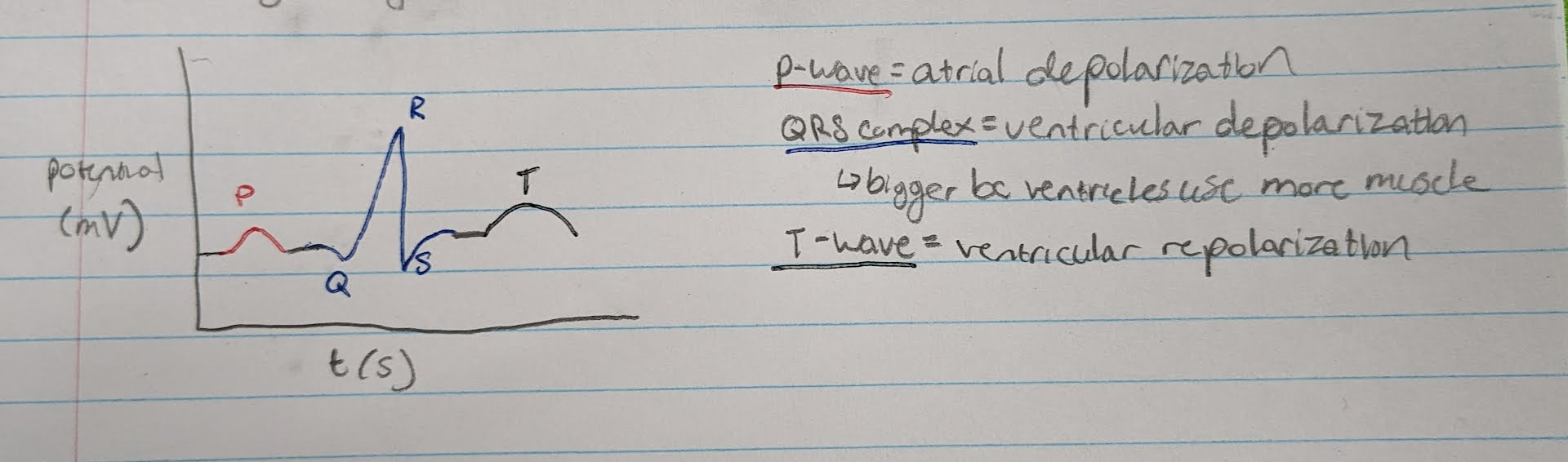
identify all segments in an ECG
differentiate the 2 sounds of the heartbeat
first sound (lub) = closure of AV valves
second sound (dub) = closure of semilunar valves
EDV
end diastolic volume
-ventricle total # blood when full
-@ end of diastole
-130 mL of blood
SV
stroke volume
-amt pumped during ventricle contraction
-70 mL
ESV
end systole volume
-blood left in ventricle at the end of systole
-not all blood leaves ventricle
-60 mL (EDV - SV)
ventricular balance
-both sides (L & R) are moving the same amounts of blood
-but the L side pumps farther, so L muscle must be stronger
-ejected blood vols must be the same or edema occurs
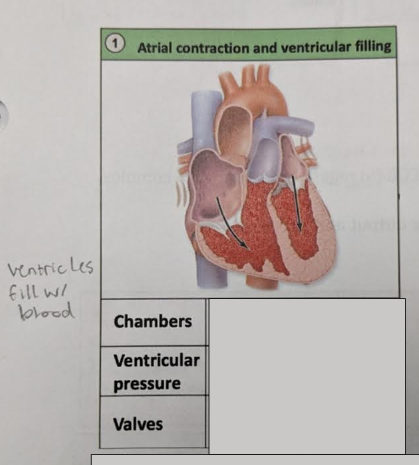
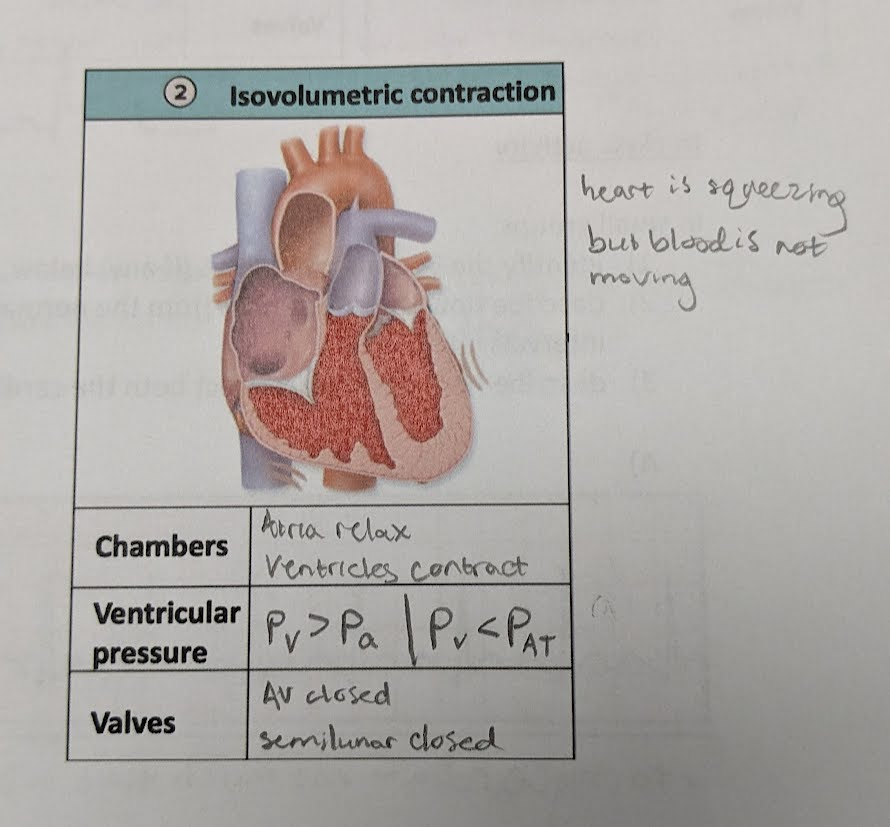
step 1
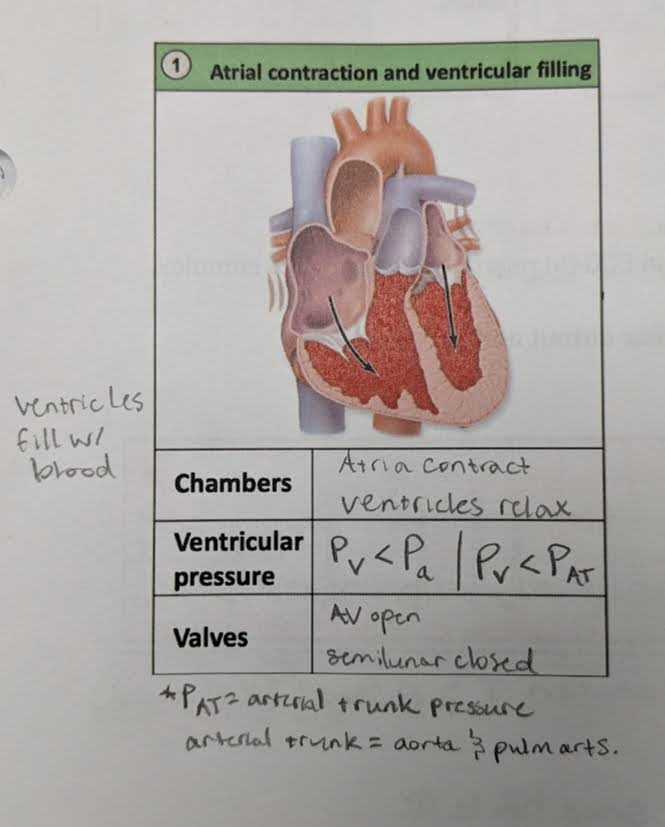
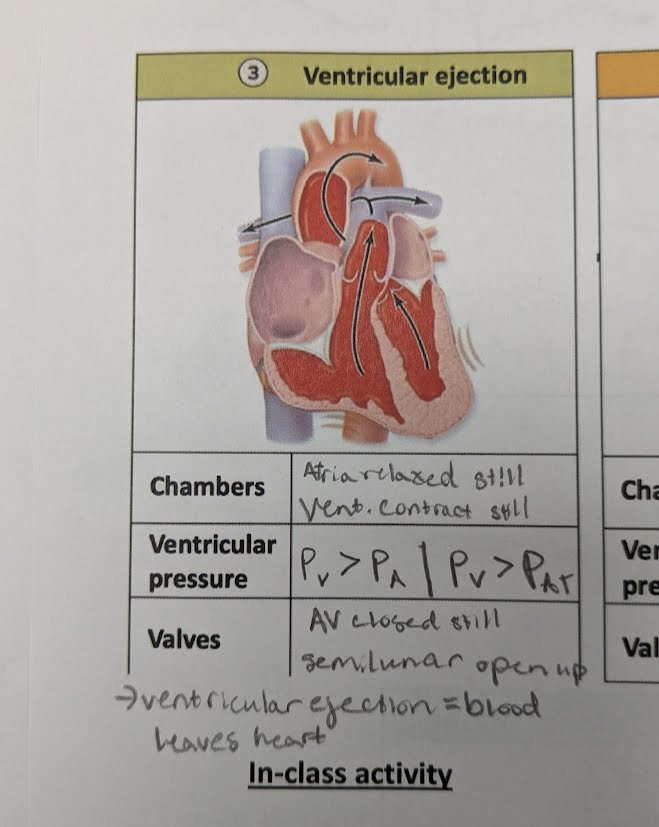
step 2
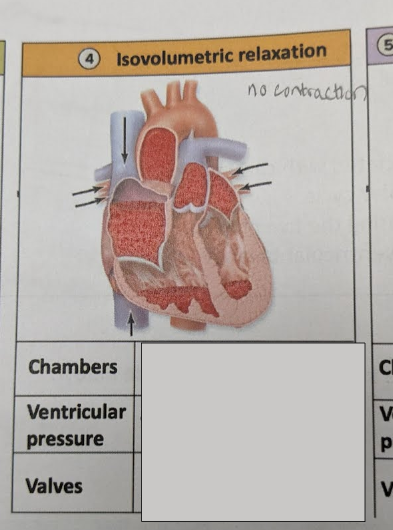
step 3
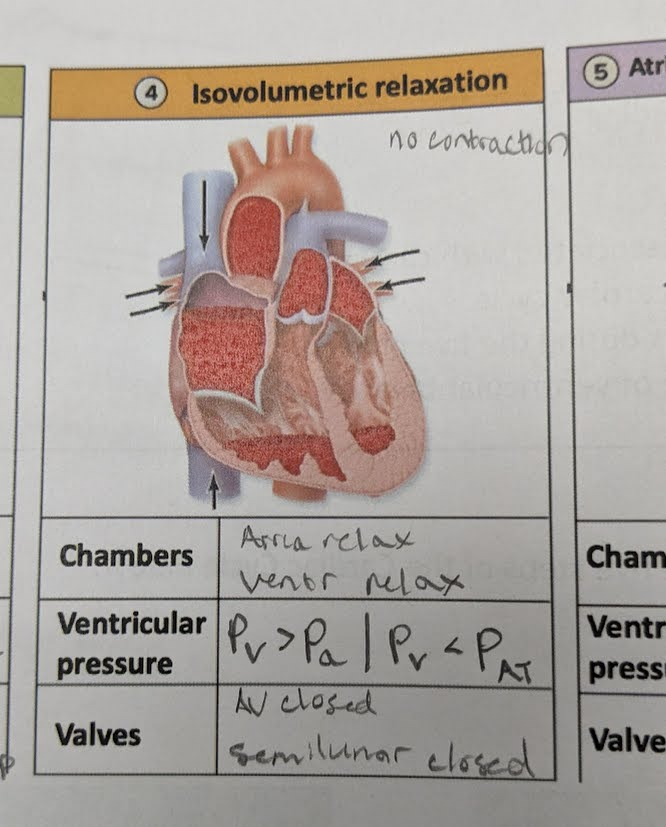
step 4
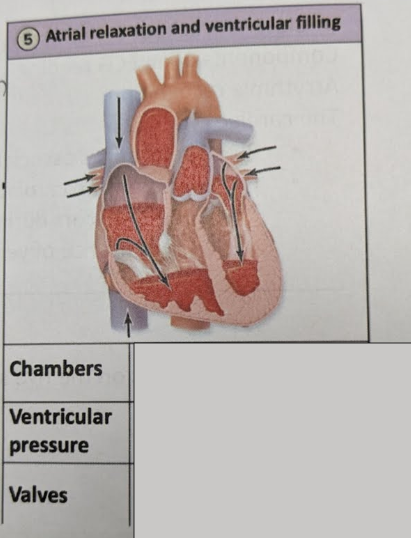
step 5
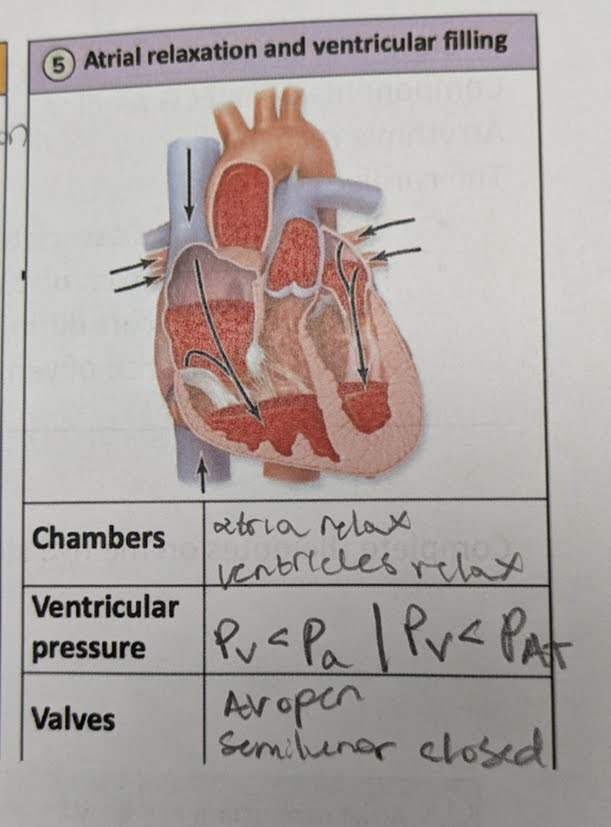
diagram the ECG phases with the 5 contraction phases
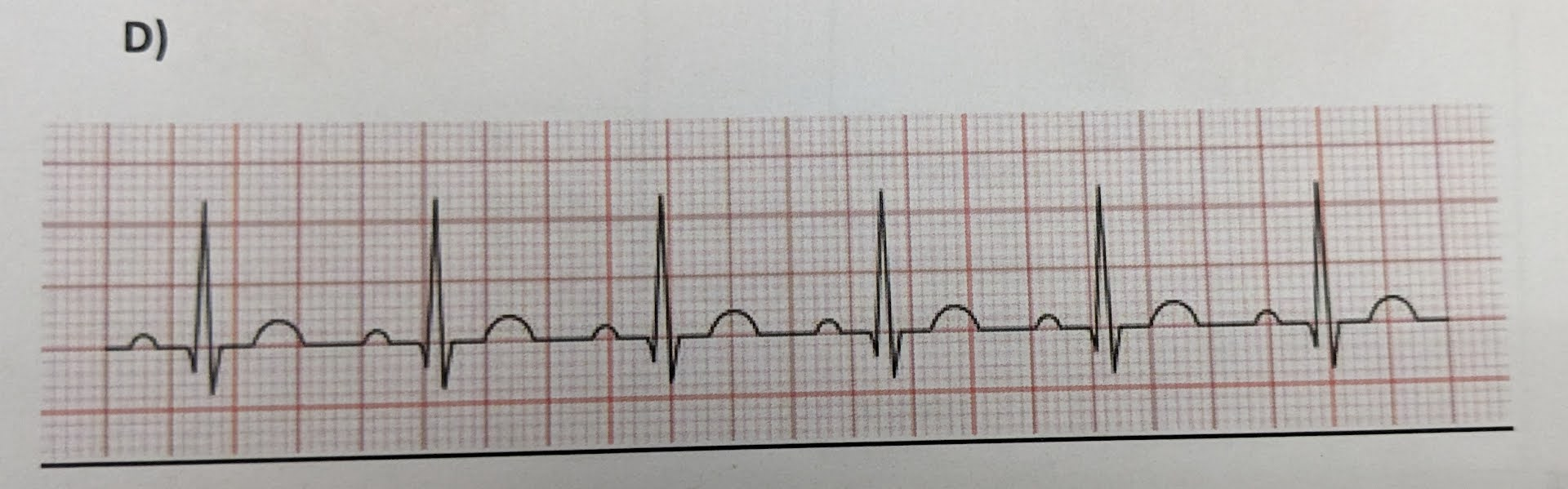
identify the ECG abnormalities (if any)
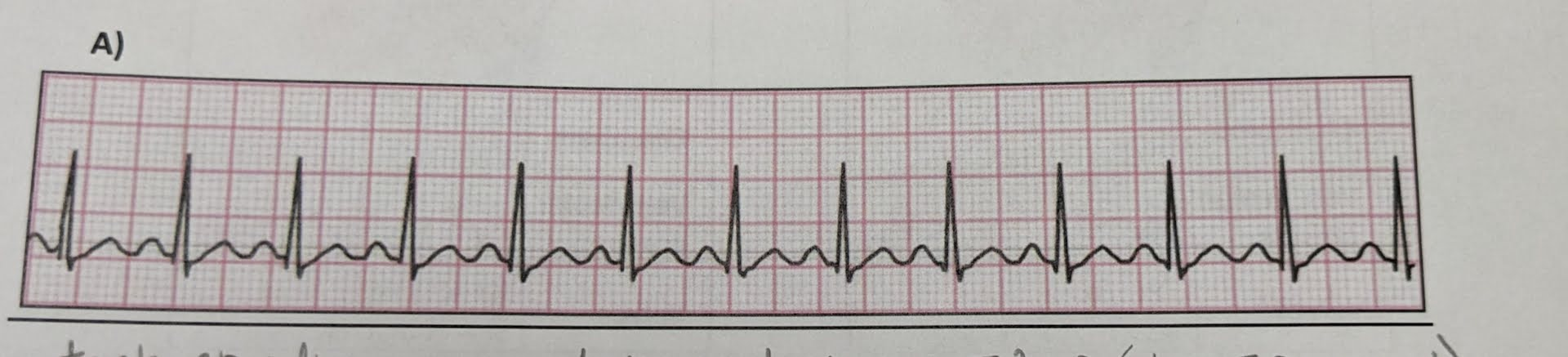
identify the ECG abnormalities (if any)
-tachycardia → fast HR
-noted by very little time in between T & P (short TP interval)
-rhythm is normal but rate is fast
-heart pumping more blood in a given time compared to normal
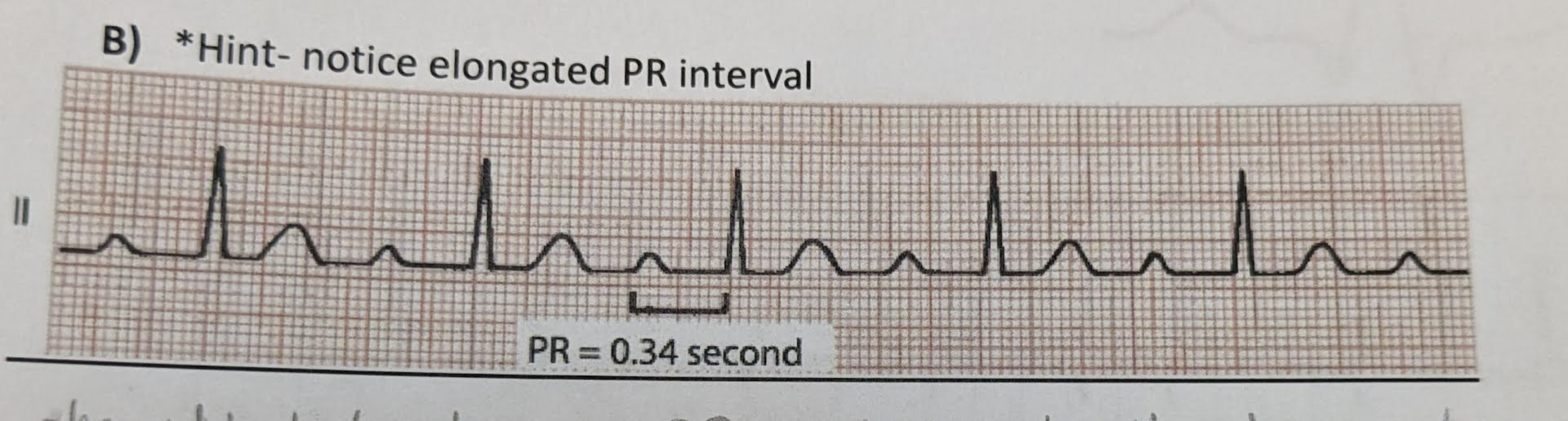
identify the ECG abnormalities (if any)
-1st degree heart block
-PR conduction length is longer than usual
-long AV node delay btwn P and R
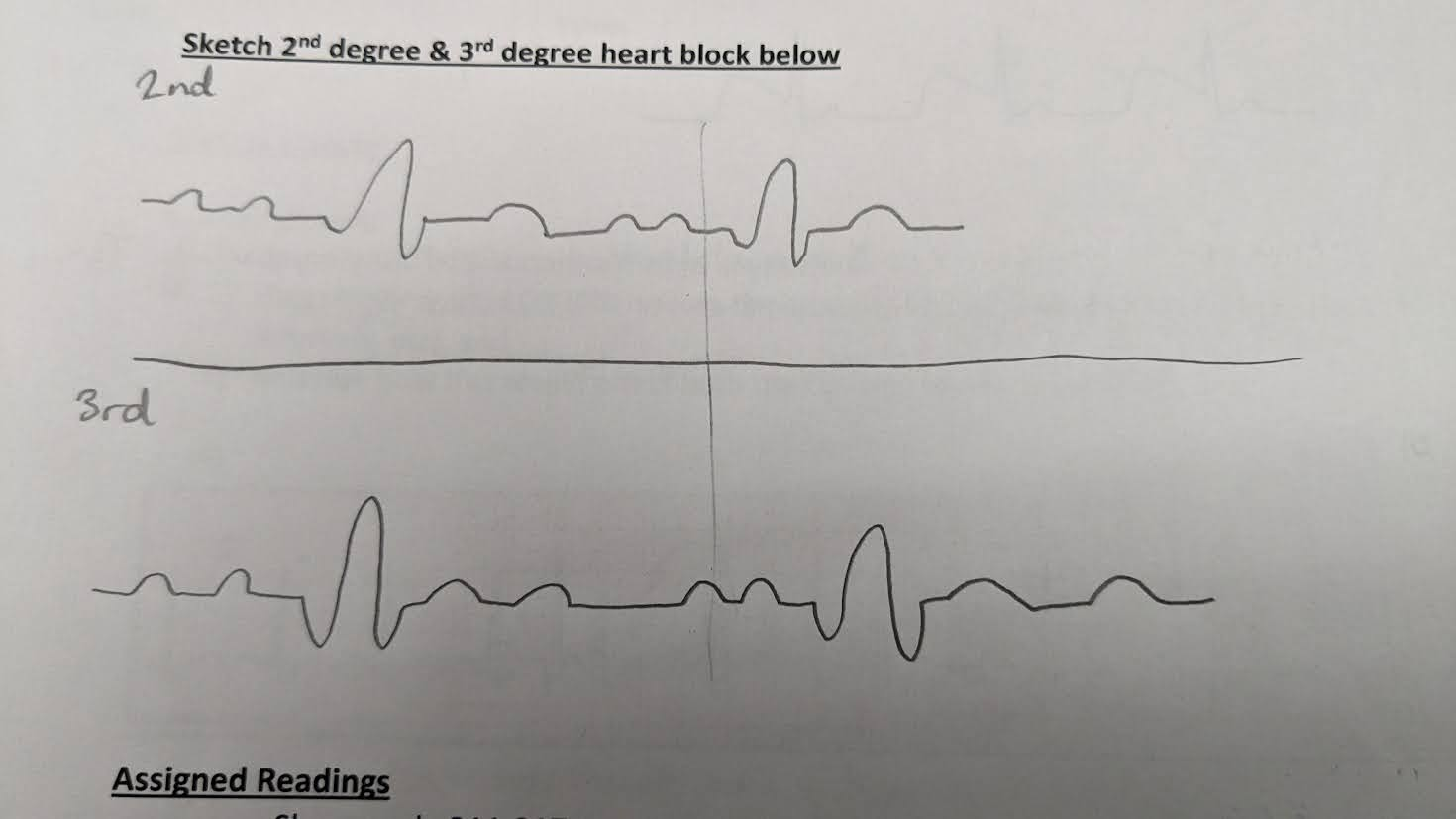
identify the ECG abnormalities of 2nd and 3rd degree heart blocks
2nd = more than 1 P wave
3rd = more than 1 P wave AND more than 1 T wave
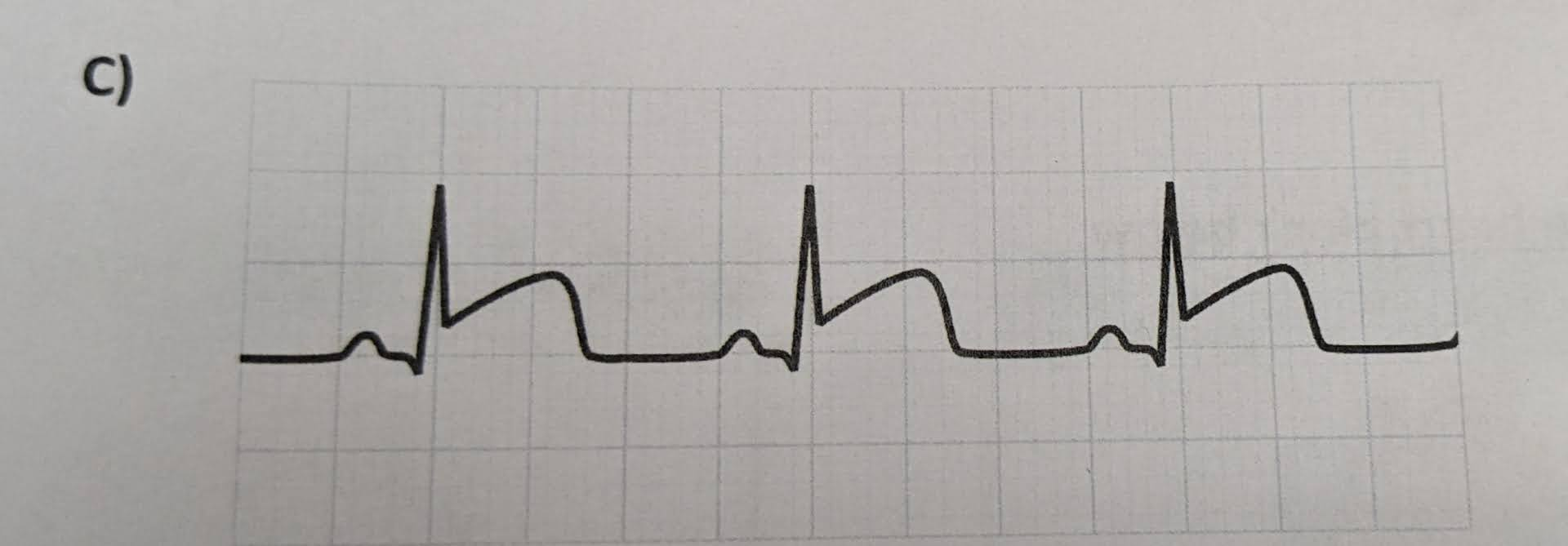
identify the ECG abnormalities (if any)
-myocardial infarction (heart attack)
-no S interval, leads directly to T. T wave is also very large
identify the ECG abnormalities (if any)
normal ECG
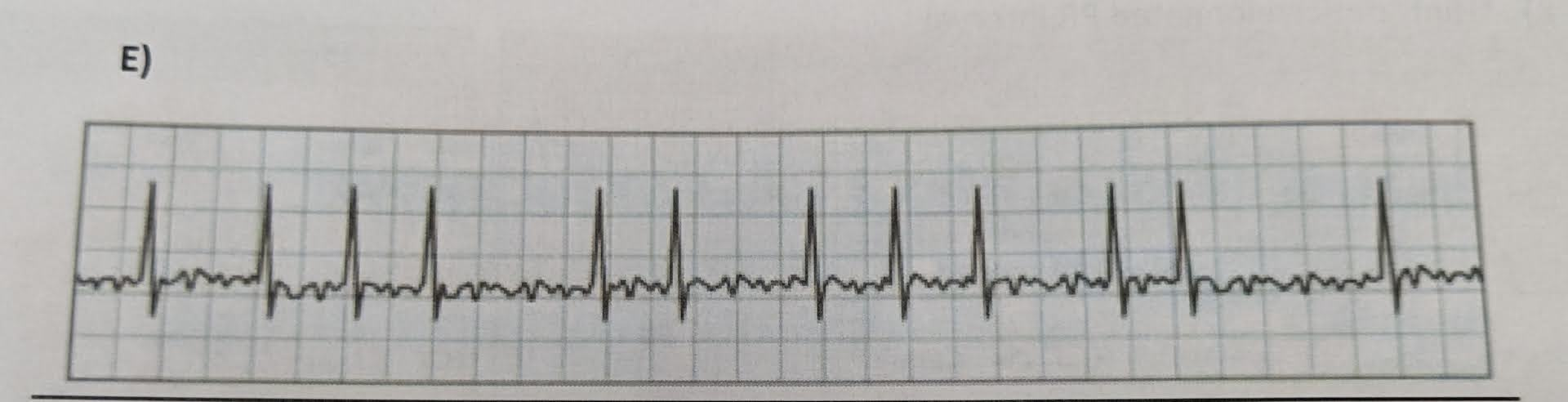
identify the ECG abnormalities (if any)
-arrythmia = A.fib (atrial fibrilation)
-no defined waves other than the R phase
-RR segment is also uneven, meaning an uneven HR
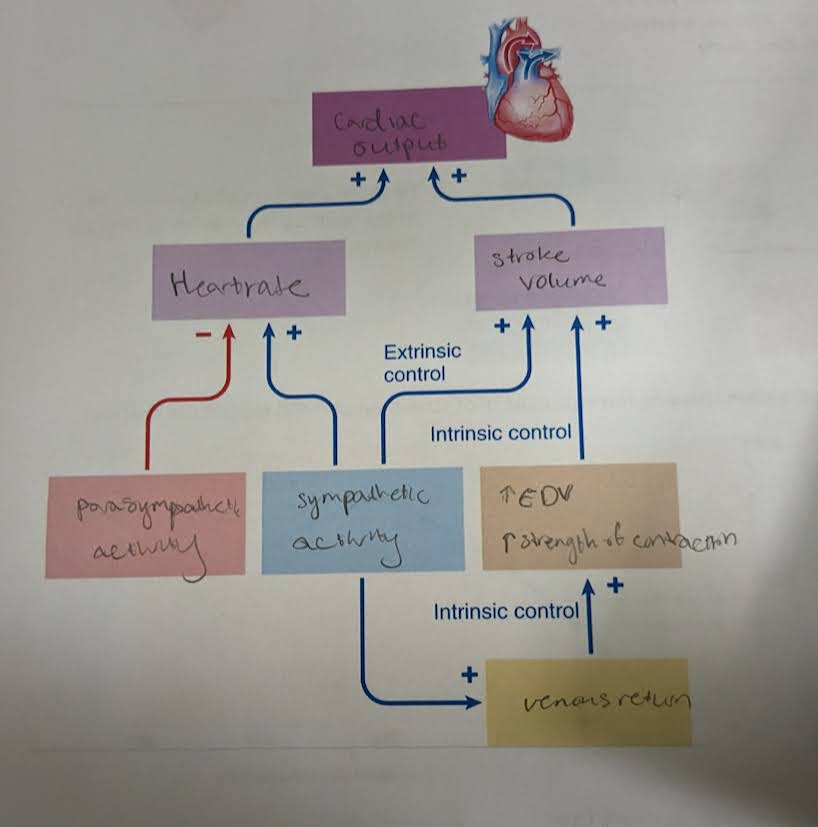
What is cardiac output? how to determine it?
amnt of blood pumped by each ventricle per unit per time
CO = HR x SV
CO = mL/min
HR = bpm
SV = mL/beat
cardiac reserve
the capacity to increase CO above rest level
-gives measure of lvl of exercise that someone can pursue
→ HR and SV increase during exercise
how does the autonomic NS affect heart?
-not needed for heart to beat, but can affect it (during exercise, fear, etc)
parasympathetic = decrease HR (via vagus nerve)
sympathetic = increase HR and SV (via cardiac nerve)
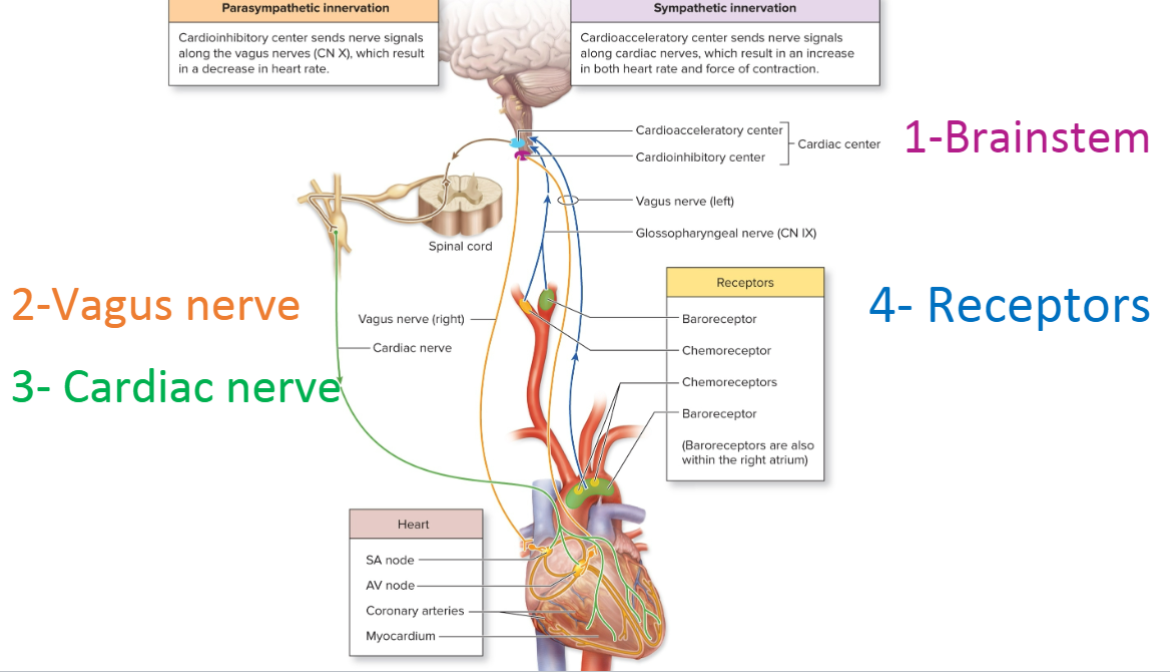
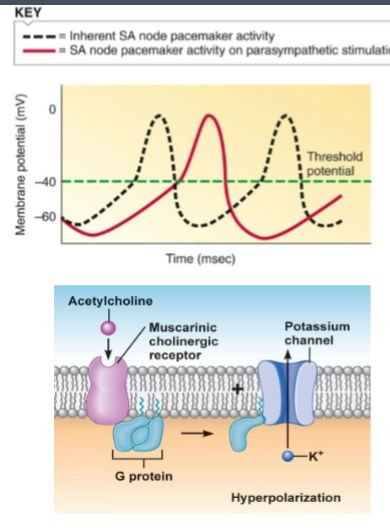
how does parasympathetic NS affect heart? (general)
-decrease HR (not SV, no change in contraction)
→ decrease SA node firing = prolong drift to threshold
→ increase delay at AV node
→ decrease pacemaker potential by making cell more negative
Mechanic that parasympathetic uses to decrease HR
-vagus nerve goes to heart, releases Ach on muscarinic receptors on autorhythmic cells
-binding activates GPCR, which opens a K+ VGC
-now K+ leaves cell, cell becomes more neg (hyperpolarize)
-cell is now further from threshold = harder to reach = reach less often = slower HR
How does sympathetic NS affect heart? (general)
-increase HR and SV
→ increase SA node firing = shorten drift to threshold
→ reduces delay at AV node
→ also enhances arterial & ventricular contraction = higher SV
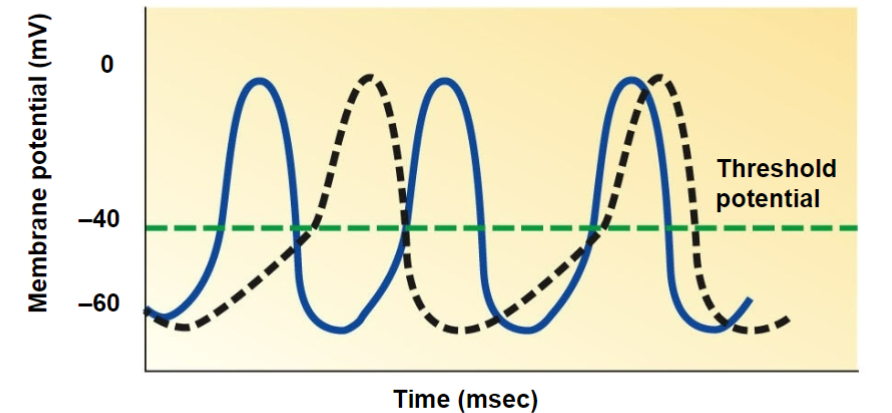
Mechanic that sympathetic uses to increase HR
-cardiac nerve goes to heart, release norepinephrine and epinephrine to autorhythmic cells
-binding activates GPCR, cAMP phosphorylates multiple VGC (Funny Na channels, and T-type Ca channel)
-Na and Ca enter cell, cell become more pos (depolarize)
-cell now closer to threshold = easier to reach = reach more often = faster HR
Mechanic that sympathetic uses to increase SV
-cardiac nerve goes to heart, release norepinephrine and epinephrine to contractile cells
-binding will open L-type Ca VGC
-more Ca enter cell → increase CICR effect
→ allows muscle to contract harder (by binding troponin) = increase SV
**this is a type of extrinsic control
chronotropic agents
Change HR
→ alter nodal cell (SA/AV node) activity
→ often work via autonomic NS or hormones
positive ChrA = increase HR (ex. EP and NEP)
negative ChrA = decrease HR (ex. Ach)
inotropic agents
Change SV
→ alter contractility (force of contraction), usually by altering Ca lvls
positive inoA = increase available Ca (ex. EP and NEP)
negative inoA = decrease available Ca (ex. BP drugs)
intrinsic vs extrinsic control
control SV
intrinsic = related to extent of venous return (heart regulate itself)
extrinsic = extent of sympathetic stimulation (change from outside influence)
venous return, Starling’s law
vol of blood that’s returned to the heart
→ determines amnt of ventricular blood prior to contraction (aka EDV)
-volume determines preload (pressure stretching heart wall)
-Starling’s law: as you increase venous return/EDV, heart stretches more, heart contracts more
**this is a type of intrinsic control
fill out the diagram
why do heart murmurs happen?
a valve is not opening or closing correctly
→ results in extra sound when listening to pulse
stenotic valve
-stiff, narrowed valve
-does not open completely → blood forced thru constricted opening at very high velocity
-murmur sounds like whistling
insufficient valve
-does not close completely
-valve edges are scarred, do not fit tgt properly
-blood flows backward thru the valve (regurgitation)
-murmur sounds like wooshing, gurgling
what are causes of heart murmurs?
-rheumatic fever = autoimmune disease triggered y strep infection
-atherosclerosis (plaque)
Which valve opens/closes at what heart sound?
lub = systolic. AV valve opens before, closes after
dub = diastolic. SL valve opens before, closes after
What kind of murmur is this?
Lub → whistle → dub
stenotic SL murmur
→ stenotic = whistle sound
→ SL = since stenotic means opening problem, it can’t be the AV since AV already opened before the “lub” sound. This means it has to be SL opening
What kind of murmur is this?
Lub → woosh → dub
inefficient AV valve
→ inefficient = woosh sound
→ AV = since inefficient means closing problem, cannot be the SL since the SL isn’t even open yet. This means it’s the AV valve closing
What kind of murmur is this?
Lub → Dub → whistle
Stenotic AV valve
→ stenotic = whistle
→ AV = since stenotic means opening problem, cannot be SL valve since it’s already closed. Must be AV valve since it opens before systole
What kind of murmur is this?
Lub → dub → gurgle
Insufficient SL valve
→ insufficient = gurgle
→ SL = since insufficient means closing problem, SL closes right after dub.
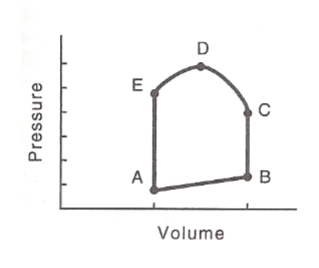
When are the ventricles closed, and contracting?
between B-C
→ isovolumetric contraction
When is ventricular filling?
A-B
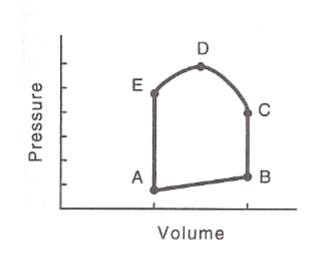
When does the left AV valve close?
B
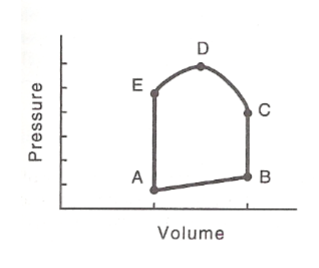
When does the left AV valve open?
A
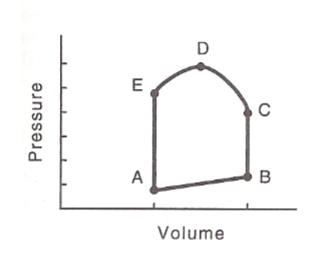
When does the aortic semilunar valve open?
C
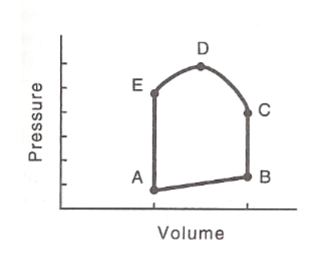
When does the aortic semilunar valve close?
E
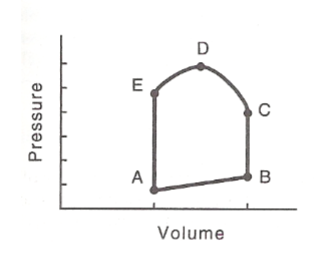
When does isovolumetric relaxation occur?
E-A
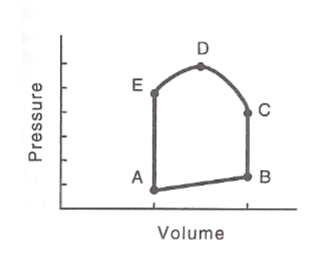
When is ejection of blood?
C-E
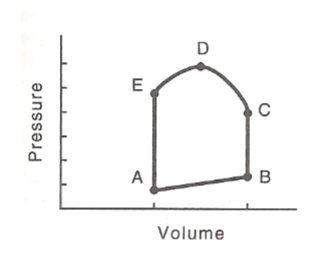
The QRS complex occurs prior to?
B-C
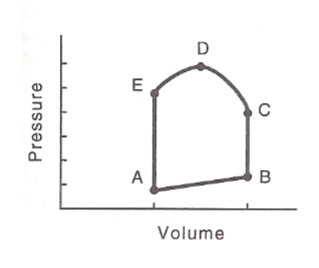
When is ESV?
A
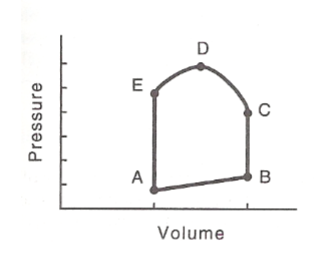
When is EDV?
B