Ch 2: Reproduction (9%)
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
91 Terms
diploid, 2n, haploid, n
In animals, autosomal cells are said to be _________ (___), which means they contain two copies of each chromosome. Germ cells, on the other hand, are _________ (___), containing only one copy of each chromosomes.
G1, S, G2, M
name the 4 stages of the eukaryotic cell cycle for actively dividing cells
G1, S, G2
name the 3 stages of the eukaryotic cell cycle that are termed “interphase”
interphase, 90, G1, G0, division
___________ is the longest part of the cell cycle; even actively dividing cells spend about ___ percent of their time here. Cells that do not divide spend all of their time in an offshoot of the ___ stage, called the ___ stage. During this stage, the cell is simply living and carrying out its functions, without any preparation for _________.
G1 (Presynthetic Gap)
During this stage of the cell cycle, cells create organelles for energy G1and protein production while also increasing their size. In addition, passage into the next stage is governed by a restriction point. Certain criteria, such as containing the proper complement of DNA, must be met for the cell to pass the restriction point and enter the next stage.
G1, S
passage from ___ stage to ___ stage in the cell cycle is governed by the restriction point
S (Synthesis of DNA)
During this stage of the cell cycle, the cell replicates its genetic material so that each daughter cell will have identical copies. This means that cells leaving this stage have twice as much DNA as the cells did when they entered this stage (but the ploidy doesn’t change).
G2 (Postsynthetic Gap)
During this stage of the cell cycle, the cell passes through a second quality checkpoint. DNA has already been duplicated, and the cell checks to ensure that there are enough organelles and cytoplasm for two daughter cells. The cell also checks to make sure that DNA replication proceeded correctly to avoid passing on an error to daughter cells that may further pass on the error to their progeny.
M (Mitosis)
During this stage of the cell cycle, mitosis and cytokinesis occurs.
G1, S, G2, M, G1/S, restriction point, G2/M
The cell cycle is controlled by checkpoints, most notably between the ___ and ___ phase and the ___ and ___ phase. At the ___/___ checkpoint, the cell determines if the condition of the DNA is good enough for synthesis. This checkpoint is also known as the ___________ _______. At the ___/___ checkpoint, the cell is mainly concerned with ensuring that it has achieved adequate size and the organelles have been properly replicated to support two daughter cells.
cyclins, CDK (cyclin-dependent kinases)
the molecules responsible for the cell cycle (2)
mitosis
the process by which two identical daughter cells are created from a single cell
somatic cells
the type of cells that undergo mitosis
somatic cells
cells that are not involved in sexual reproduction
prophase, metaphase, anaphase, telophase
name the 4 phases of mitosis
prophase
During this phase of mitosis, the chromosomes condense, the nuclear membrane dissolves, nucleoli disappear, centrioles migrate to opposite sides of the cell, and the spindle apparatus begins to form
metaphase (equatorial plate is also known as the metaphase plate)
During this phase of mitosis, the chromosomes line up along the equatorial plate
anaphase
During this phase of mitosis, the sister chromatids are separated and pulled to opposite poles
telophase
During this phase of mitosis, the nuclear membrane reforms, spindle apparatus disappears, and the cytosol and organelles are split between two daughter cells through cytokinesis
gametocytes, germ cells, 4 nonidentical, gametes
Whereas mitosis occurs in somatic tissue and results in 2 identical daughter cells, meiosis occurs in _____________ (_____ _____) and results in up to ___ ____________ sex cells (________)
haploid daughter cells, reductional, sister chromatids, equational
In contrast to mitosis, meiosis consists of one round of replication followed by two rounds of division. Meiosis I results in homologous chromosomes being separated, generating _________ _____________ ______; this is known as ___________ division. Meiosis II is similar to mitosis in that it results in the separation of ________ __________ without a change in ploidy; this is known as ____________ division.
homologues
chromosomes that are given the same number but are of opposite parental origin; ex: maternal chromosome 15 & paternal chromosome 16
prophase I
During this phase of Meiosis, the events are the same in mitosis except that homologues come together and intertwine as a process called synapsis. The four chromatids are referred to as a tetrad and crossing over exchanges genetic material between one chromatid and material from a chromatid in the homologous chromosome.
crossing over
Which event, that occurs during Prophase I of meiosis, accounts for Mendel’s second law of independent assortment?
metaphase I
During this phase of Meiosis, homologous chromosomes line up on either sides of the equatorial plate.
anaphase I
During this phase of Meiosis, homologous chromosomes separate and are pulled to opposite poles of the cell in a process called disjunction.
disjunction
Which event, that occurs during Anaphase I of meiosis, accounts for Mendel’s first law of segregation?
telophase I
During this phase of Meiosis, each chromosome still consists of two sister chromatids joined at the centromere. The cells are now haploid; once homologous chromosomes separate, only n chromosomes are found in each daughter cell (23 in humans). The cell divides into two daughter cells by cytokinesis. The cell may then enter interkinesis.
Seminiferous Tubules, Interstitial Cells of Leydig
Male Reproductive Anatomy
The two functional components of the testes.
Seminiferous Tubules
Male Reproductive Anatomy
Highly coiled structures in the testes where the sperm are produced.
Sertoli Cells
Male Reproductive Anatomy
Cells near the seminiferous tubules that secrete nutrients for the sperm.
Interstitial Cells of Leydig
Male Reproductive Anatomy
Secrete testosterone and other male sex hormones.
Scrotum
Male Reproductive Anatomy
Holds the testicles outside of the body around 2-4 degrees C below the body's temperature.
Epididymis
Male Reproductive Anatomy
A long, coiled tube on the surface of the testes where the sperm gain their motility by the flagella developing and where they are stored until ejaculation.
Ejaculation
Male Reproductive Anatomy
When sperm travel through the vas deferens to the ejaculatory duct and out of the penis.
Ejaculatory Duct
Male Reproductive Anatomy
Located at the posterior edge of the prostate gland; two of them fuse to form the urethra, which carries sperm through the penis as they exit the body
Seminal Fluid
Male Reproductive Anatomy
Substance that nourishes sperm. It is made through combined effort of the seminal vesicles, prostate gland, and bulbourethral gland.
Semen
Male Reproductive Anatomy
The name for the combined sperm and seminal fluid.
Spermatogonia
Male Reproductive Anatomy
Diploid stem (germ) cells in males.
Diploid Primary Spermatocytes
Male Reproductive Anatomy
After the spermatogonia go through S phase where their genetic material is replicated, they develop into these.
Secondary Spermatocytes
Male Reproductive Anatomy
Haploid cells that result from the first meiotic division of the primary spermatocytes.
Spermatids
Male Reproductive Anatomy
Haploid cells that result from the secondary spermatocytes undergoing meiosis II.
Spermatozoa
Male Reproductive Anatomy
What the spermatids become after maturation
Sperm Head
Male Reproductive Anatomy
Part of the sperm that holds the genetic material of the sperm.
Spermatogenesis
Male Reproductive Anatomy
The formation of haploid sperm through meiosis
Acrosome
Male Reproductive Anatomy
Cap that covers the sperm head and is necessary for the sperm to enter the ovum. Develops from the Golgi apparatus.
3 million
The number of sperm produced per day once a male reaches sexual maturity.
Ovaries
Female Reproductive Anatomy
Female gonads which produce estrogen and progesterone. They also contain thousands of follicles and are located in the pelvic cavity.
Follicles
Female Reproductive Anatomy
Multilayered sacs that contain, nourish, and protect immature ova (eggs). The primary oocytes mature while they are inside these.
Diploid Zygote
Female Reproductive Anatomy
The ovum becomes this once the second polar body is released after meiosis II is complete, and the two pronuclei from fertilization unite. The ovum contributes nearly everything while the sperm only contributes ½ of the DNA.
Ovum (or Egg)
Female Reproductive Anatomy
This name is reserved ONLY for ovulated secondary oocytes that ARE fertilized. If it goes unfertilized, the gamete is menstruated as a secondary oocyte.
Fallopian Tubes
Female Reproductive Anatomy
Lined with cilia to move the egg forward; connected to the muscular uterus
Uterus
Female Reproductive Anatomy
Muscular organ that is connected to the fallopian tube and it is the site of fetal development.
Cervix
Female Reproductive Anatomy
Lower end of the uterus that connects to the vaginal canal where sperm are deposited during sex.
Vulva
Female Reproductive Anatomy
Collective term for the female external reproductive organs.
Oogenesis
Female Reproductive Anatomy
The production of female gametes (eggs).
Oogonia
Female Reproductive Anatomy
During fetal development, these cells give rise to primary oocytes. All of the oogonia that a female will ever have are formed during fetal development.
primary oocytes, prophase I, secondary oocyte, metaphase II, fertilized, ovum
Female Reproductive Anatomy
At birth, all oogonia have already undergone replication and are considered __________ __________. They are arrested in __________ ___ stage of meiosis. The ovulated egg each month is a ____________ ___________, which is arrested in ___________ ___. If the oocyte is __________, it will complete meiosis II to become a true _____.
Menarche
Female Reproductive Anatomy
A woman's first menstrual period at which point one primary oocyte will complete meiosis I to produce a secondary oocyte and a polar body.
Polar Body
Female Reproductive Anatomy
Cytokinesis is uneven in oogenesis. The cell receiving very little cytoplasm and organelles is called this
Zona Pellucida
Female Reproductive Anatomy
Oocytes are surrounded by this acellular mixture of glycoproteins that protects the oocyte and contains the compounds necessary for sperm binding
Corona Radiata
Female Reproductive Anatomy
Oocytes are surrounded by this layer of cells that adheres to the oocyte during ovulation and lies outside the zona pellucida
Corpus Luteum
Female Reproductive Anatomy
The remains of the ovarian follicle following ovulation. It produces progesterone, estradiol, and testosterone.
hypothalamus, hypothalamus, anterior pituitary gland, FSH, LH, sex
Sexual Development
Prior to puberty, the _____________ restricts the production of GnRH (gonadotropin-releasing hormone). At puberty, the _______________ stops restricting its release and it triggers the _________ _________ ______ to synthesize and release ____ and ___. These hormones trigger the production of other ____ hormones that develop and maintain the reproductive system.
androgens, differentiation, low, testosterone, sperm, FSH, LH
Male Sexual Development
During the fetal period, the presence of the Y chromosome leads to production of __________, resulting in male sexual _______________. For the duration of infancy and childhood, androgen production is ____. ____________, produced by the testes, increases dramatically during puberty, and ______ production begins. ____ stimulates the Sertoli cells and triggers sperm maturation, whereas ____ causes the interstitial cells to produce testosterone.
secondary sexual characteristics, high, declines, negative feedback
Male Sexual Development
Testosterone not only develops and maintains the male reproductive system, but also results in the development of _____________ __________ ________________. Testosterone production remains _____ into adulthood and then _________ with age. This hormone exerts __________ __________ on the hypothalamus and anterior pituitary so that production is kept within an appropriate range.
estrogens, FSH, secondary sexual characteristics, estrogens, reproductive tract, estrogens, uterus, endometrium, zygote
Female Sexual Development
__________ are secreted in response to ____ and result in the development and maintenance of the female reproductive system and female _____________ __________ ________________. In the embryo, ___________ stimulate development of the _______________ ______. In adults, ___________ lead to the thickening of the lining of the _______ (called the _____________) each month in preparation for the implantation of a ________.
progesterone, corpus luteum, LH, progesterone, endometrium, estrogen, endometrium, zygote, progesterone, placenta, corpus luteum
Female Sexual Development
________________ is secreted by the ________ ________ (the remains of the ovarian follicle following ovulation) in response to ____. ______________ is involved in the development and maintenance of the _______________, but not in the initial thickening of it → this is the role of __________. This means that both hormones are required for the generation, development, and maintenance of an _______________ capable of supporting a ________. By the end of the first trimester of a pregnancy, _______________ is supplied by the __________, while the ________ ________ atrophies and ceases to function.
Estrogens
Female Sexual Development
Hormones secreted in response to FSH. It does basically everything for female sexual development. In adults, it leads to the thickening of the lining of the uterus.
Endometrium
Female Sexual Development
The lining of the uterus.
Progesterone
Female Sexual Development
The hormone secreted by the corpus luteum that is involved in the maintenance and protection of the endometrium.
Placenta
Female Sexual Development
By the end of the first trimester this organ provides progesterone and the corpus luteum atrophies and ceases to function.
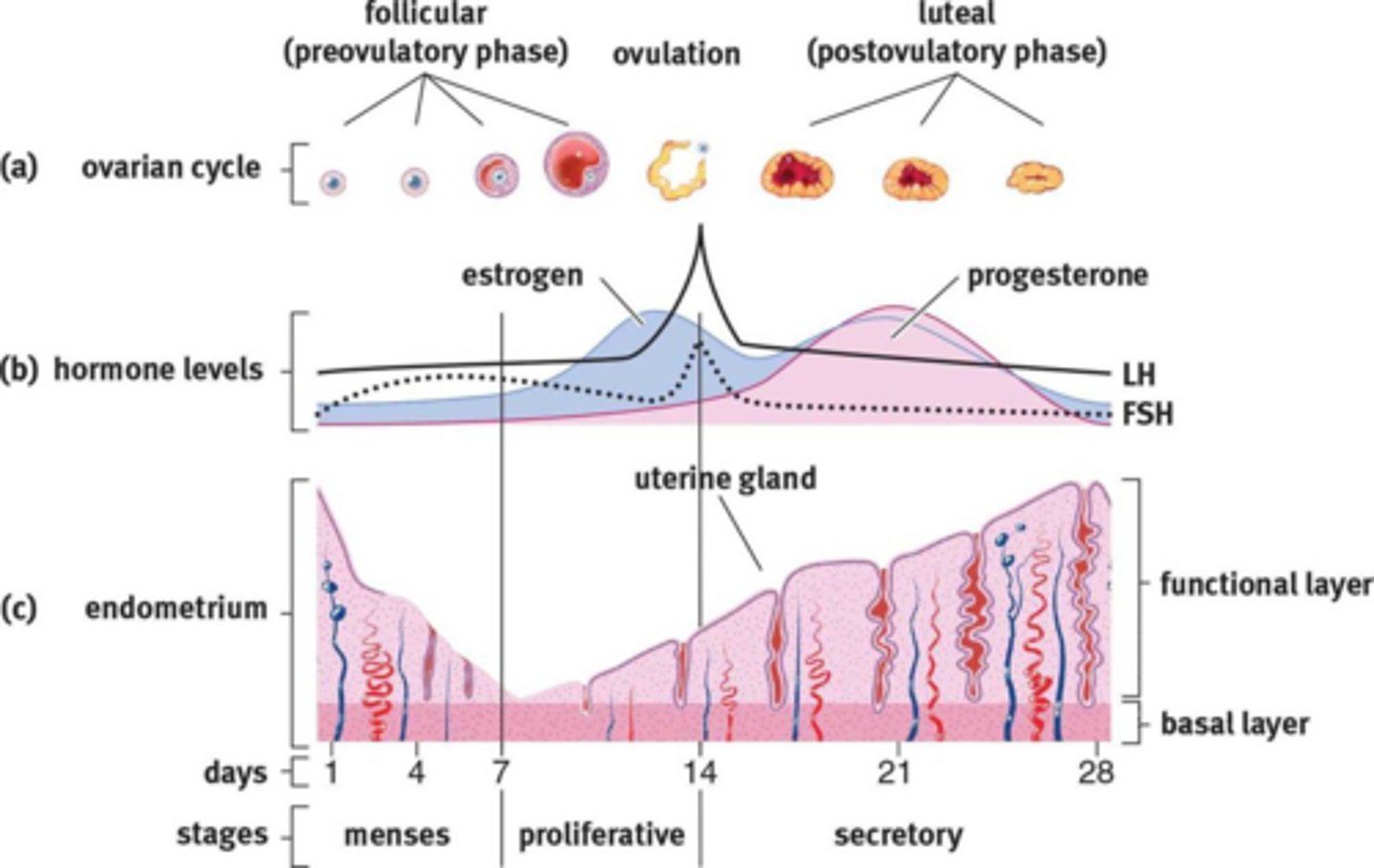
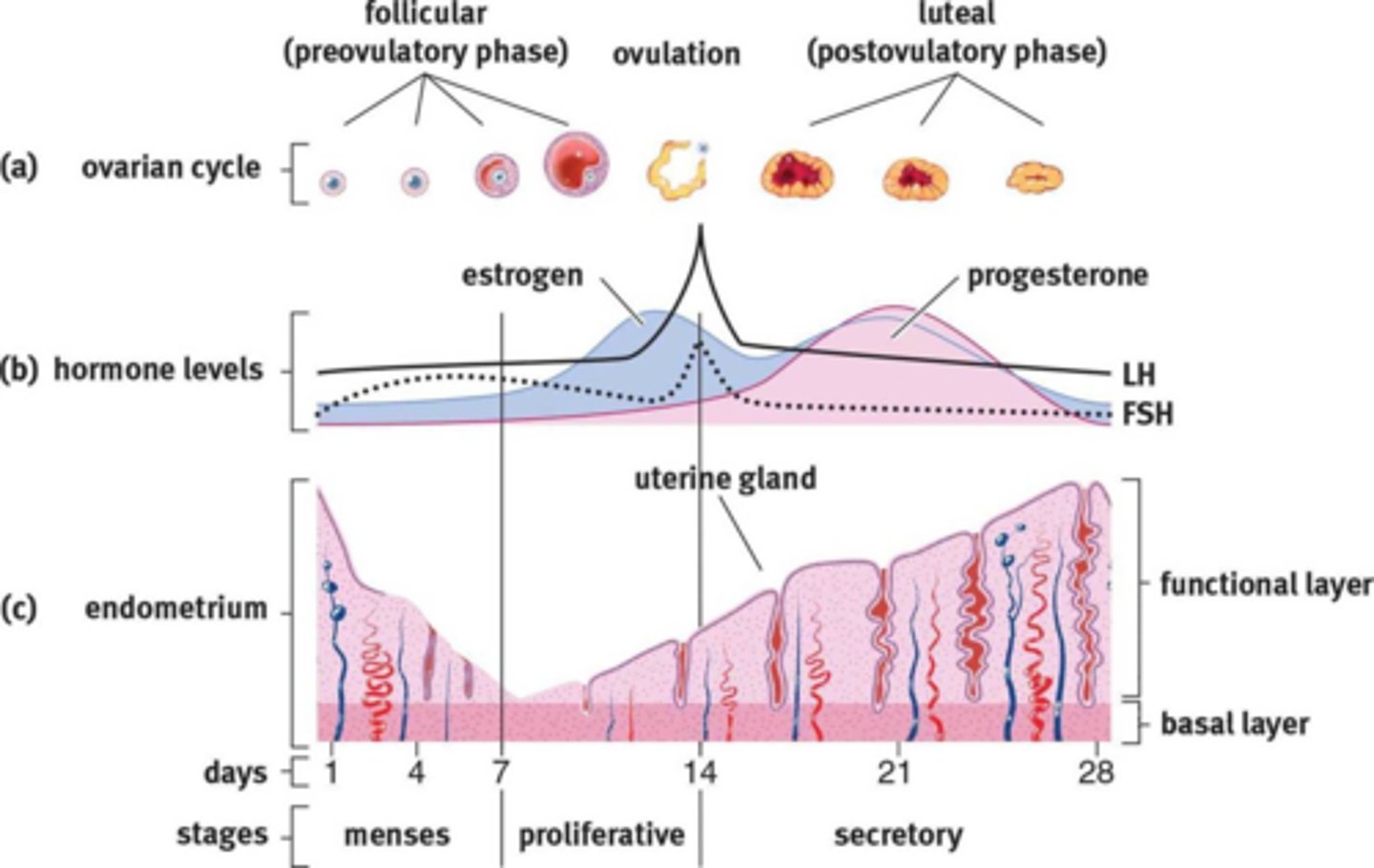
Follicular Phase, Ovulation, Luteal Phase, Menstruation
Menstrual Cycle
name the 4 stages of the menstrual cycle in order.
Follicular Phase
Menstrual Cycle
During this phase, GnRH secretion stimulates FSH and LH secretion, which promotes follicle development. Estrogen is released, stimulating vascularization and glandularization of the decidua.
Ovulation
Menstrual Cycle
This phase is stimulated by a sudden surge in LH. This surge is triggered when estrogen levels reach a threshold and switch from negative to positive feedback effects.
Luteal Phase
Menstrual Cycle
During this phase, LH causes the ruptured follicle to become the corpus luteum, which secretes progesterone that maintains the uterine lining. High estrogen and progesterone cause negative feedback on GnRH, LH, and FSH.
Menstruation
Menstrual Cycle
This phase occurs if there is no fertilization. As the estrogen and progesterone levels drop, the endometrial lining is sloughed off, and the block on GnRH production is removed.
menstrual flow, increases, decreased, fall off, higher, FSH, LH, follicles, follicles, estrogen, negative, level off, estrogen, decidua
Menstrual Cycle → Follicular Phase
The follicular phase begins when the ___________ ______, which sheds the uterine lining of the previous cycle, begins. GnRH secretion from the hypothalamus ___________ in response to the ___________ concentrations of estrogen and progesterone, which _____ _____ toward the end of each cycle. The _________ concentrations of GnRH cause increased secretions of both ____ and ____. These two hormones work in concert to develop several ovarian _________. The _________ begin to produce __________, which has _________ feedback effects and causes the GnRH, LH, and FSH concentrations to _______ _____. _________ stimulates regrowth of the endometrial lining, stimulating vascularization and glandularization of the ________.
Decidua
Menstrual Cycle
the modified mucosal lining of the uterus (that is, modified endometrium) that forms every month, in preparation for pregnanc
estrogen, estrogen, positive feedback, spike, LH, ovulation
Menstrual Cycle → Ovulation
Late in the follicular phase, the developing follicles secrete higher and higher concentrations of _________. Eventually, __________ concentrations reach a threshold that paradoxically results in __________ __________, and GnRH, LH, and FSH levels _______. The surge in ___ is important → it induces ___________.
LH, corpus luteum, progesterone, estrogen, progesterone, increase, high, high, negative, multiple eggs
Menstrual Cycle → Luteal Phase
After ovulation, ____ causes the ruptured follicle to form the ________ ________, which secretes ________________. Remember that ____________ helps regenerate the uterine lining, but __________________ maintains it for implantation. Progesterone levels begin to __________, while estrogen levels remain ______. The ______ levels of progesterone cause ___________ feedback on GnRH, FSH, and LH, preventing the ovulation of __________ ______.
implantation, corpus luteum, LH, decline, high, block
Menstrual Cycle → Menstruation
Assuming that _____________ does not occur, the ______ _______ loses its stimulation from ____, progesterone levels _________, and the uterine lining is sloughed off. The loss of ______ levels of estrogen and progesterone removes the ______ on GnRH so that the next cycle can begin.
High Levels of Progesterone
Menstrual Cycle
Primary characteristic of the luteal phase, in which the corpus luteum is secreting progesterone.
zygote, blastocyst, uterine lining, corpus luteum
Pregnancy
After the egg has been fertilized, the ________ will develop into a _____________ that will implant into the ________ _______ and secrete human chorionic gonadotropin (hCG), an analog of LH. This maintains the _________ _________.
corpus luteum, uterine lining, decrease, placenta
Pregnancy
hCG is critical during first trimester development because the estrogen and progesterone secreted by the _________ _________ keep the _________ _________ in place. By the second trimester, hCG levels _________ because the ___________ has grown to sufficient size to secrete enough progesterone and estrogen by itself.
Missed Period
Pregnancy
Sign of pregnancy, because the corpus luteum lives on producing hormones such as inhibin, which prevented another cycle from occurring.
hCG (Human Chorionic Gonadotropin)
Pregnancy
This hormone is an analogue of LH and can trigger the same receptors as LH. This causes the maintenance of the corpus luteum.
FSH, LH, atrophy, endometrium, atrophies, menstruation, negative, increase
Menopause
As a woman ages, her ovaries become less sensitive to _____ and ____, resulting in ovarian ________. As estrogen and progesterone levels drop, the _______________ also ________, and _______________ stops. ___________ feedback of FSH and LH is lost so the blood levels of these two hormones ___________. This causes many physiological changes.
Menses
Menstrual Cycle
Stage (not phase) characterized by the shedding of the previous cycle's endometrium during menstruation.
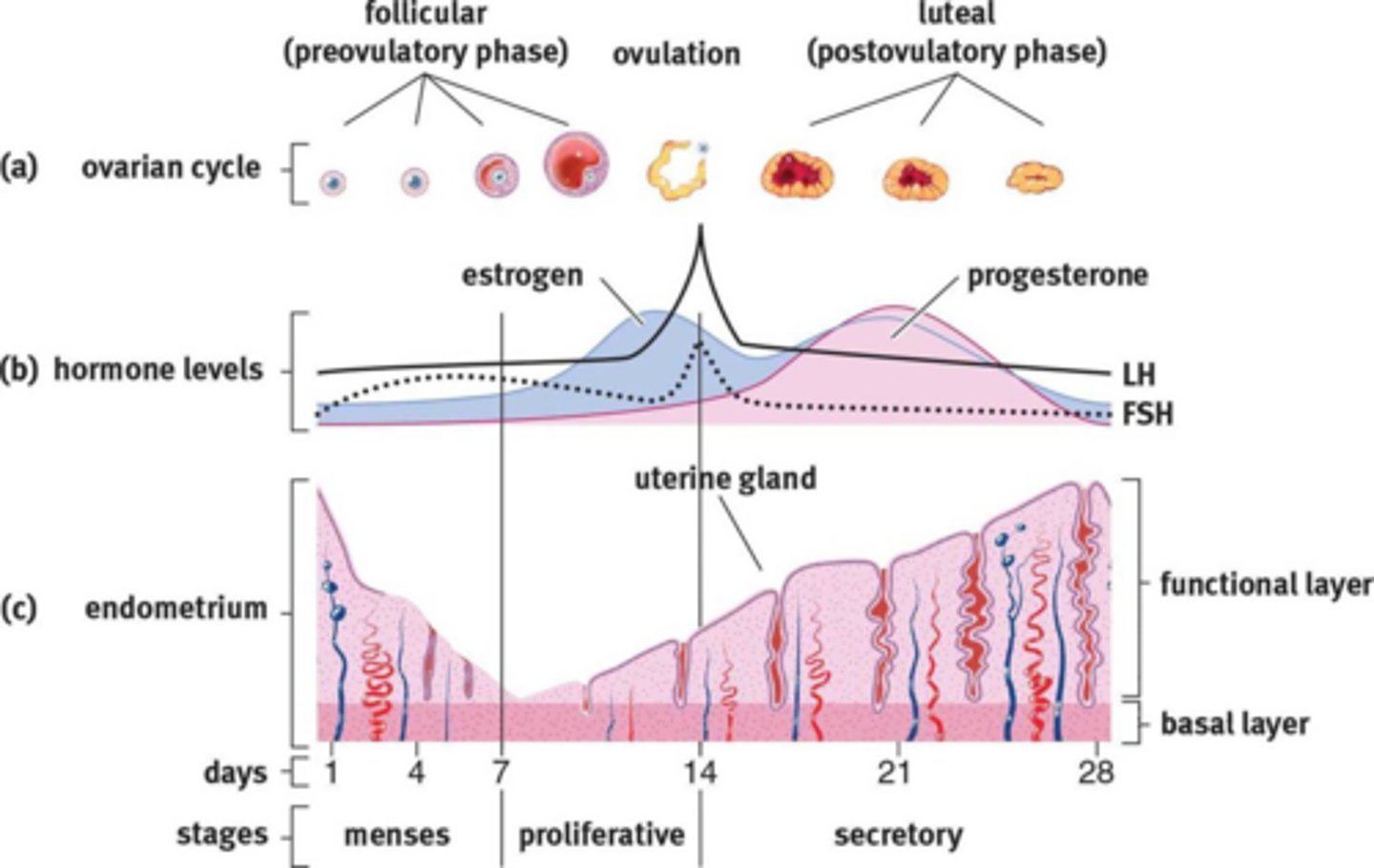
Proliferative
Menstrual Cycle
Stage (not phase) characterized by the increasing estrogen levels causing the endometrial lining to proliferate.
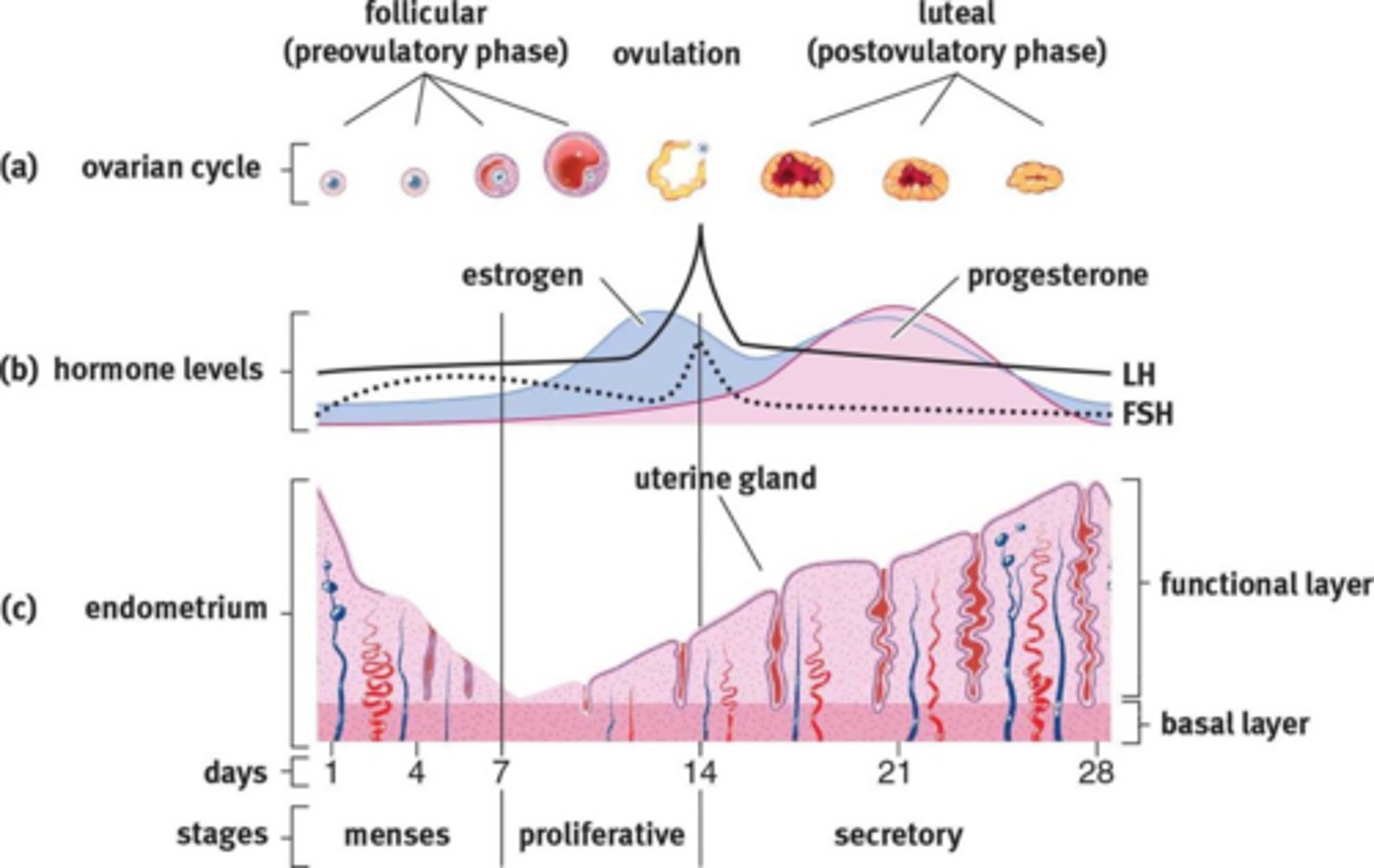
Secretory
Menstrual Cycle
Stage (not phase) in which progesterone stimulates the preparation of the endometrium in a few ways: It increases blood flow to the endometrium through spiral arteries; increases uterine secretions through glands in the endometrium; and it reduces contractility of the uterine muscles to prepare for expansion during gestation.