Fielding Chapter 24: Colloids
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
What are the two types of colloid solutions?
Natural
Synthetic
Natural Colloids
Plasma
Whole Blood
Albumin
Synthetic Colloids
Hydroxyethyl starch solutions (hetastarch, Hextend, Voluven, VetStarch, pentastarch)
Dextran
Gelatin
Polymerized hemoglobin
What are the three attributes of hydroxyethylstarch that determine its pharmacokinetics?
Molecular weight
Degree of substitution
C2/C6 Ratio
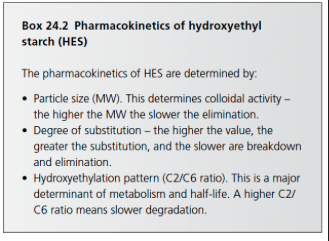
Attributes Determined by Molecular Weight of HES
Lower molecular weight solutions exert a greater oncotic pressure (greater number of particles) but have a lower half-life in the circulation as they are more rapidly degraded and eliminated
Degree of Substitution of HES
Indicates the average number of hydroxyethyl groups per glucose unit
A-amylase can only degrade unsubstituted glucose units
By changing the degree of substitution it is possible to influence the degree of enzymatic breakdown and control the extent and duration of the volume effect
A higher degree of substitution results in slower breakdown and elimination of the molecule
C2/C6 Ratio of HES
HES hydroxyethylation can occur at carbon positions C2, C3, C6 of the glucose molecules
This higher the C2/C6 ratio (i.e. the greater the number of glucose molecules hydroxyethylated at the C2 atom compared to the C6 atom), the slower the starch is metabolized
Hydroxyethyl residues bound at the C2 position of glucose inhibit plasma amylase, increasing the intravascular half life of HES
Renal function has been shown to decrease after administration of HES with a degree of substitution of more than 0.62 in humans undergoing surgery as well as with the administration of 10% solution
What are the two main mechanisms by which HES is removed from circulation?
Renal excretion
Redistribution
Renal Excretion of HES
2 phases
Elimination, by glomerular filtration, of polymers with a MW of less than 50kDa
Occurs almost immediately after administration
Glomerular filtration as the HES molecules are metabolized by hydrolysis by a amylase
Once the product of a-amylase digestion is smaller than 72kDa it can be renally excreted
Some are also excreted in the bile but this is a much less important elimination route
What % of HES molecules does renal excretion remove?
70-80%
What % of HES molecules does redistribution remove?
20-30%
Redistribution of HES
Consists of uptake and temporary storage of HES in the tissues
Extravasated molecules are stored in phagocytic cells of the liver, lymph nodes, and spleen and degradation by lysosomal enzymes occurs over time
Distribution of HES After 24 Hours
After 24 hours, only 38% of the initial dose remains in the intravascular space, 39% is excreted in urine, and 23% is sequestered in tissues
Effect of a-amylase on COP
A-amylase due to intravascular hydrolysis of large polymers of HES, yields a greater number of osmotically active molecules and serves to sustain the increases in plasma colloid osmotic pressure (COP) associated with hetastarch administration
What are the three HES products available in the US?
Hetastarch
Pentastarch
Tetrastarch
Hetastarch
0.7 degree substitution
MW 450 kDa
Advantage is its relatively prolonged volume effect because of the larger MW colloid particles and the high degree of substitution
Associated with dose dependent coagulation abnormalities
Pentastarch
0.5 degree substitution
Available for leukapheresis in humans but not for fluid therapy
MW 264 kDa
Tetrastarch
0.4 degree substitution
MW 130 kDa
Low molar substitution is the main reason for the benefits on pharmacokinetics, intravascular volume expansion, and hemodilution
C2/C6 ratio is 9:1, which increases the half life
Recommended dose for small animals is 20 ml/kg/day
Contraindications include fluid overload, renal failure with oliguria or anuria, and severe hypernatremia
Elimination is faster than pentastarch with lower persistence in tissue
May be associated with fewer renal side effects
Hemoblobin-Based Oxygen-Carrying Solutions (HBOCs)
Alternative to whole blood transfusions
One commercial product, Oxyglobin
Oxygen, carrying properties, excellent colloids, and decrease blood viscosity
Purified hemoglobin is used in horses principally for the treatment of acute life-threatening anemia
Due to cost, used primarily in newborn foals with NI
No adverse effects and a good clinical response for the treatment of anemia
Beneficial Effects of HES Resuscitation
Increases colloidal osmotic pressure (COP)
Plugging of leaky vessels
Blunting of endothelial-neutrophil interaction
Beneficial Effects of HES Resuscitation - Plugging of Leaky Vessels
Hydroxyethyl starch may have the ability to seal endothelial "pores" or gaps that develop in microvessels after different forms of endothelial injury, including sepsis and endotoxemia
HES may prevent leakage of plasma proteins (especially albumin) from the intravascular space, preventing secondary fluid extravasation
Medium MW particles between 100 and 300 kDa, may act as plugs at these endothelial "pores"
Beneficial Effects of HES Resuscitation - Blunting of Endothelial - Neutrophil Interaction
Evidence suggests that HES has the ability to modulate the endothelial inflammatory response and attenuate the permeability increase associated with sepsis
May reduce the expression of adhesion molecules which reduces leukocyte adhesion
What is the recommended dose of HES in horses?
5-10 ml/kg
Adverse Effects of HES - Plasma Viscosity
Plasma viscosity is determined by the number and physical properties of macromolecules in plasma
Plasma viscosity is an important contributor to the microcirculatory disturbances that characterize shock
Highly substituted HES is less desirable in this regard because it increases plasma viscosity
Medium MW HES with low C2/6 ratios and low MW starches decrease plasma viscosity and have better rheological properties
Adverse Effects of HES - Effects on Hemostasis
Major effects of HES on coagulation are dilution of plasma clotting factors, an additional decrease in factor VIII, and accelerated fibrin clot formation in the last stages of clotting
In addition, platelet dysfunction associated with coating of their surface occurs
What % of the blood volume is plasma in horses?
55-65%
Functions of Albumin
Maintains COP
Transports endogenous and exogenous substances
Mediates coagulation
Inhibits oxidative damage
Maintains the integrity, function, and repair of the GI tract
What synthesizes albumin?
Hepatocytes
What degrades albumin?
Reticuloendothelial system
What is the one of strongest stimuli for albumin release?
Plasma COP at the hepatic interstitial space is one of the strongest stimuli for albumin synthesis
Supranormal administration of colloids suppresses albumin synthesis
What % of COP does albumin account for?
70-80%
What % of total albumin does interstitial space contain?
60-70%
What are the forces opposing fluid escape from the vasculature?
Colloid osmotic pressure regulates transvascular fluid flow - is one of the forces opposing fluid escape from the vasculature
Gibbs-Donnan effect also contributes to water's attraction to colloids - negative charges of albumin molecules attract sodium cations which causes water to follow across the semipermeable endothelial membrane
What does a plasma transfusion contain?
Plasma transfusions are the only source of equine specific albumin replacement
Plasma also contains immunoglobulins used for foals with FPT as well as macroglobulins, coagulation protein s9II, VII, IX, and X), antithrombin III, elastase, and proteinase inhibitors
How much plasma is needed to raise the plasma albumin of a horse by 0.1 g/dL?
10-15 ml/kg