HRM - Lecture 10: Renal regulation of volume
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
Via the RAAS:
decreased stretch in afferent arteriole -> increased renin release -> increased angiotensin and aldosterone -> Decreased GFR and increased sodium reabsorption -> higher serum osmolarity -> ADH stimulation -> water reabsorption
How do the kidneys detect hypovolaemia?
- If sodium is high, osmolarity increases.
- If osmolarity increases, ADH increases
- If ADH increases water reabsorption increases and volume goes up
Explain how serum sodium levels and ECF volume levels linked, with the example of high sodium levels
1. seconds to minutes: Baroreceptors and chemoreceptors measure changes in osmolarity and pressure and trigger increases in contractility and cardiac output and venous and distal arteriolar vasoconstriction to shift blood to arteries
2. minutes to hours: Stress relaxation and capillary fluid shift. Stress relaxation is a slow increase in stretching of vessel walls due to high pressure. In a low BP situation, this would reverse and vessels narrow. Capillary fluid shift drains more fluid from interstitium due to falling hydrostatic capillary pressure
3. long-term control: RAAS system and renal volume-pressure control. In a low BP situation, decreased afferent arteriolar stretch will increase renin secretion
Briefly describe the levels of blood pressure regulation, given a low BP disturbance. (level numbers are arbitrary)
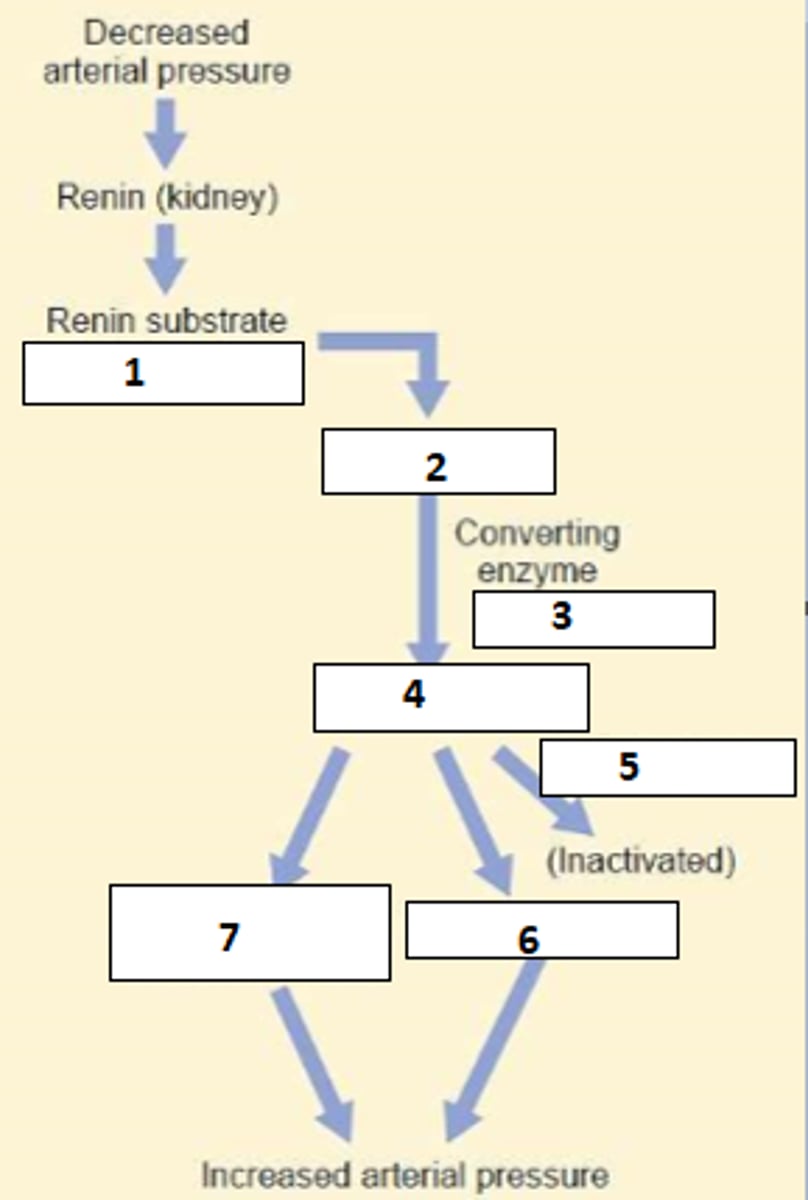
1. angiotensinogen (from liver)
2. angiotensin I
3. Angiotensin converting enzyme (ACE) (Lung)
4. Angiotensin II
5. Angiotensinase inhibited
6+7 Vasoconstriction and Renal salt and water retention via:
- vasoconstriction induced GFR drop
- direct effect of ATII on NHE transporter increase in PCT
- stimulation of aldosterone -> sodium reabsorption
- stimulation of ADH -> H2O reabsorption
Fill the blanks (include flow-on effects in 6+7)
These are in the atria and function the same as the others. They are "low pressure" due to location
What are the low pressure baroreceptors?
Located in carotid bodies, aortic arch and juxtaglomerular apparatus
What are the high pressure baroreceptors?
This is the volume of blood found in the arterial system, which is responsible for tissue perfusion. ~700ml
What is effective circulating volume?
This is an intrarenal mechanism where higher pressure means higher GFR, which allows less time for reabsorption and increases excretion of Na+
What is pressure natriuresis?
- decreased nephrons for filtration limits ability to clear fluid
- damage to glomeruli inhibits filtration
- increased preglomerular vessel resistance
- abnormal RAAS activity
How is renal disease linked to hypertension?
This is an intrarenal mechanism where higher pressure means higher GFR, which allows less time for reabsorption and increases excretion of H2O
What is pressure diuresis?
- Bladder gradually accumulates urine
- detrusor muscle stretches
- bladder stretch reaches upper limit of ability to stretch normally
- first an autonomic nervous reflex triggers the start of micturition by opening the internal urethral sphincter
- stretching of the neck of the bladder and the bladder itself sends a powerful signal to the cortex which triggers a desire to urinate
- the cerebral cortex inhibits the opening of the skeletal muscle external sphincter until time of choosing
- cortical inhibition stops when desired or overwhelmed by autonomic reflex and the external sphincter opens, allowing emptying of the bladder
Describe the process from an empty bladder to micturition
Segment Ia: Up to 100ml there is a gradual increase in pressure.
Segment Ib: Between 100-300ml the bladder stretches well and pressure barely increases.
Segment II: Above 300ml pressure rises sharply and the micturition reflex is triggered
Describe the volume-pressure relationship of the bladder as it fills
1. pudendal nerve (S2,3,4): Controls the external urethral sphincter and voluntary control of urination
2. Hypogastric nerve (L1,2,3): Bladder wall relaxation and internal urethral sphincter contractions
3. Pelvic nerves (S2,3,4): Detrusor contraction, internal sphincter relaxation
Give the nerve, roots and activity achieved by the different segments of the nervous system in bladder control
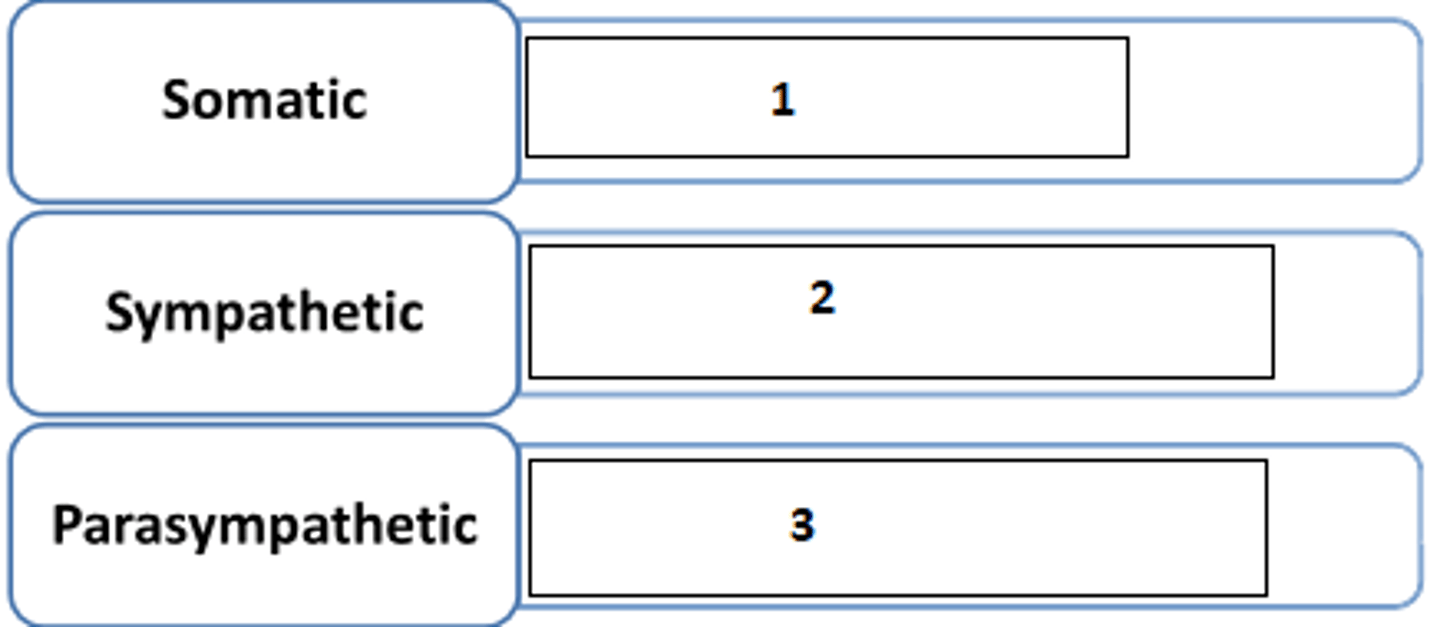
- beta3
- alpha1
What kind of sympathetic receptor is present at the detrusor and internal sphincter respectively?
1. Stretch receptors in the bladder wall and highly sensitive receptors in posterior urethra
2. afferent pathway via pelvic nerves
3. center: spinal cord, pons, medulla, hypothalamus, cortex
4. efferent nerves via pelvic nerves
5. detrusor muscle, internal and external sphincters
Name the 5 components of the micturition reflex arc
150ml and 400ml
At what volumes is the first urge to void the bladder and a high urgency felt respectively?
facilitate: pons and posterior hypothalamus
inhibit: Cerebral cortex and midbrain
Which areas of the brain facilitate and inhibit micturition respectively?
Cortical centre facilitates sacral micturition centres to help initiate a micturition reflex and at the same time inhibit the external sphincter
What happens when an individual decides to urinate in terms of control centres, pathways and effectors
- PNS activity is inhibited
- SNS activity increases
- Somatic motor nerve activity increases (forced contraction of external sphincter)
What are the effects on parasympathetic, sympathetic and somatic control of the bladder when the cortical centre decides to inhibit micturition (ie does activity go up or down)?
- afferent nerve
- efferent nerve
- facilitatory or inhibitory pathways from the brain
Usually the detrusor cannot contract sufficiently and some urine remains in the bladder
In which areas can neural lesions occur that will cause micturition abnormality? What is the result?
- Absent afferent pathway due to damage, which may be due to trauma, tumors, etc.
- Loss of bladder control despite efferent pathway
- Bladder becomes distended and thin walled
- Bladder keeps on filling and overflows continually a small amount at a time: overflow incontinenence
Describe atonic bladder. Include cause, mechanism and consequence
- Transection/damage to spinal cord in suprasacral region
- Loss of higher centre communication and preservation of sacral centre
- Suppression of micturition reflex due to spinal cord shock and absence of facilitatory input from higher centres
- Overflow incontinence
- After spinal shock resolves filling and emptying becomes automatic but happens at lower volumes
Describe automatic bladder. Include cause, mechanism and consequence
- Muscle becomes active and shows contractions
- muscle becomes hypertrophied
- bladder size shrinks
What gradual changes might you expect in a denervated/decentralised bladder?
- cauda equina
- filum terminale
Tumors in which region cause decentralisation of the bladder?
The volume of plasma completely cleared of a substance per unit of time
In simplest terms, what is renal clearance?
Cl = ([U] x V) / [P]
Cl=clearance
[U] = concentration of substance in urine
V = volume of urine formed in a given time (rate of urine formation)
[P] = concentration of substance in plasma
Give the formula for renal clearance and explain what each variable means
- glucose (totally reabsorbed)
- albumin (not filtered)
Name 2 substances which have 0 clearance
Inulin: is freely filtered, but neither reabsorbed nor secreted
Name a substance which is a good indicator for GFR and give a reason
organic acids (eg: para-aminohippuric acid PAH) and organic bases (eg: morphine). These are filtered and secreted
What kind of substances have the highest clearance rate?
GFR markers
What are substances such as inulin which are freely filtered but neither reabsorbed nor secreted nor change the GFR called?
- administered intravenously
- measure amount in plasma
- measure amount in urine
How is insulin used to measure GFR?
Cl = (125mg/ml x 1ml/min) / 1mg/ml = 125ml/min
Given an administration of enough inulin to achieve 1mg/ml [P], [U] of 125mg/ml, and V of 1ml/min - what is the Cl?
Cl = (125mg/ml x 1ml/min) / 5mg/ml = 25ml/min
Given an administration of enough of a substance to achieve 5mg/ml [P], [U] of 125mg/ml, and V of 1ml/min - what is the Cl?
Pro: endogenous substance does not require administration -> convenient
Con: some creatinine secreted -> overestimation of GFR
What are the pros and cons of creatinine as a GFR marker?
No other perfect markers known aside from inulin
Name any other perfect biomarkers which meet all criteria:
- freely filtered at glomerulus
- biologically inert
- does not bind to plasma protein
- non-toxic
- neither synthesised nor metabolised in the kidney
- neither absorbed nor secreted
- no effect on renal function
- can be accurately quantified
10%
By how much is GFR approximately overestimated using creatinine as a marker?
- estimated GFR uses plasma creatinine concentration without measuring urine
- patients age, height, weight and sex taken into account to estimate expected creatinine output which depends on muscle mass
How can eGFR be used to estimate creatinine clearance?
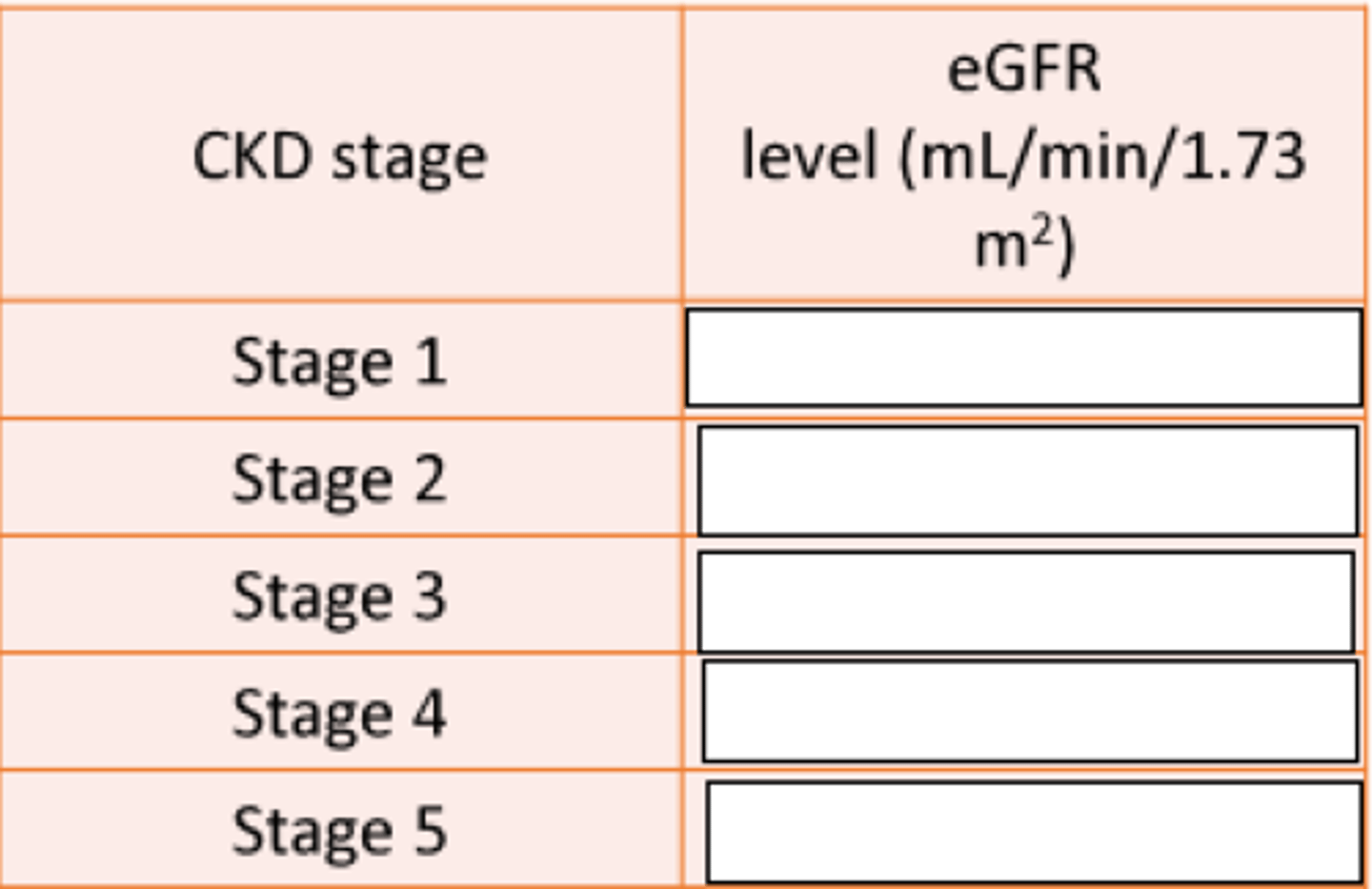
≥ 90
60-89
30-59
15-29
<15
Fill the blanks
~25% - remaining nephrons compensate
How much is GFR reduced if 50% of nephrons are lost?
plasma creatinine(PCr)/eGFR
What is the most common clinically assessed parameter for kidney function?
inverse proportion (significant drop in GFR required to increase creatinine by measurable amounts)
What is the relationship of plasma creatinine and GFR?
PCr will quadruple
If GFR falls to a quarter, what happens to PCr?
PAH (para-aminohippuric acid). It is ideal because:
- almost all PAH which reaches the glomerulus is filtered
- PAH is neither metabolised nor produced by the kidney
- PAH does not alter kideny function
- Most PAH is removed by filtration and secretion
- as a result of the above almost all PAH which reaches the kidney will end up in urine
Which substance is ideal for measuring RPF and why?
Effective renal plasma flow is eqaul to the clearance of PAH.
What is Effective RPF?
10% bigger true RPF compared to effective because not absolutely all PAH is filtered
What is the difference between effective and true RPF and what causes this?
RPF / (1-Hematocrit). Renal plasma flow/fraction of blood which is made up of plasma
How is renal blood flow measured?
RBF = 650ml/min/(1-0.45) = 1182ml/min
For a hematocrit of 0.45 and a renal plasma flow of 650 - what is the RBF?