CH49: The Patient W Cleft Lip and/or Palate
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Learning objectives
After studying this chapter, you will be able to:
• Describe the types of cleft lip and palate that result from developmental disturbances
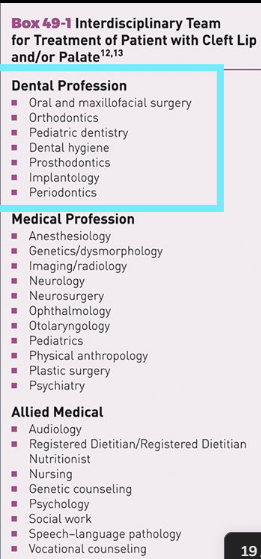
• Identify and describe the role of the professionals on the interdisciplinary team for the treatment of a patient with cleft lip and/or palate
• Recognize the oral characteristics a patient with cleft lip and/or palate may experience
• Explain how to adapt the dental hygiene appointment sequence for a patient with cleft lip and/or palate
Overview: Cleft Lip and Cleft Palate
Most common of the many types of congenital craniofacial anomalies
• May occur as isolated conditions, but frequently part of a syndrome with other birth defects
• Can significantly impact speech, hearing, adequate nutrition, oral health, mental and social development, and quality of life
• Global prevalence
• Prevalence varies by country and by ethnicity
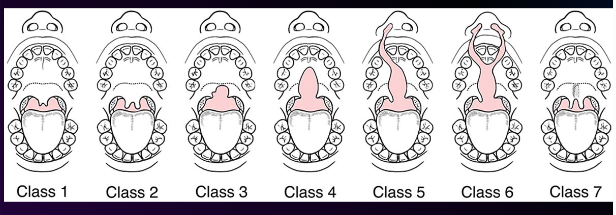
Classification of Clefts
• Based on disturbances in the embryologic formation of the lip and palate as they develop from the premaxillary region toward the uvula in a definite pattern
• Described based on structures involved, unilateral or bilateral, severity
• No universally agreed upon classification
1. Class 1: cleft of the tip of the uvula
2. Class 2: cleft of the uvula (bifiduvula)
3. Class 3: cleft of the soft palate
4. Class 4: cleft of the soft and hard palates
5. Class 5: cleft of the soft and hard palates that continues through the alveolar ridge on one side of the premaxilla, usually associated with cleft lip of the same side
6. Class 6: cleft of the soft and hard palates that continues through the alveolar ridge on both sides, leaving a free premaxilla, usually associated with bilateral cleft lip
7. Class 7: submucous cleft in which the muscle union is imperfect across the soft palate. The palate is short, the uvula is often bifid, a groove is situated at the midline of the soft palate, and the closure to the pharynx is incompetent.
Classification is based on disturbances in the embryologic formation of the lip and palate as they develop from the ______________ region.
a) maxillary
b) premaxillary
c) nasopalatal
d) all the above
b) premaxillary
Etiology
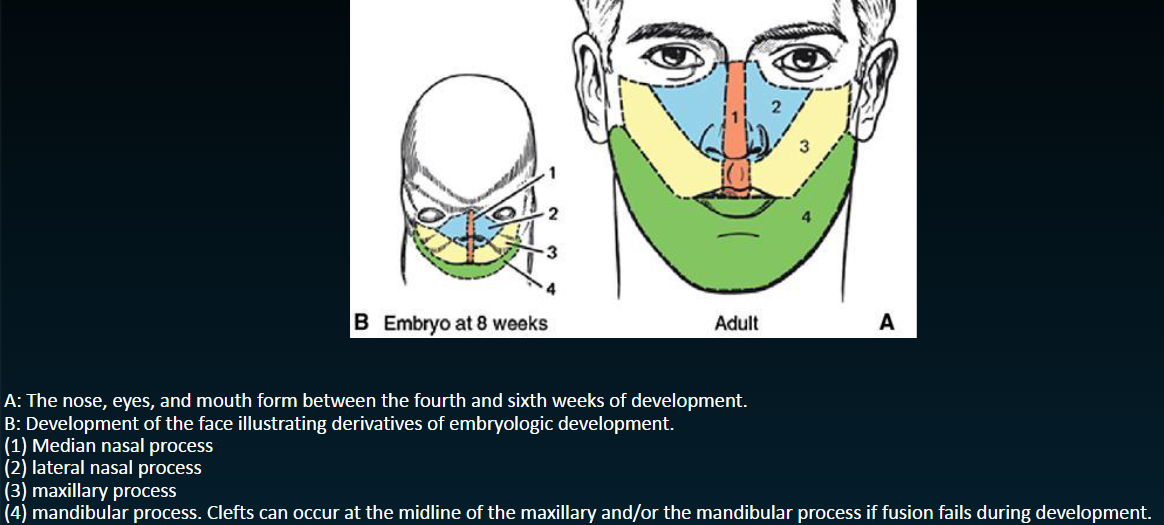
Embryology
• Cleft lip and palate represent a failure of normal fusion of embryonic processes during development in the first trimester of pregnancy
• Fusion begins in the premaxillary region and continues backward toward the uvula
• Formation of lip: 4th -8th weeks in utero, cleft apparent by end of second month
• Development of palate: 5th-12th weeks in utero, cleft apparent by end of third month
Risk Factors
Multifactorial genetic and environmental factors can be significant etiology of CL/P
• Nutritional
• Adequate folic acid (folate) may reduce risk by 40%
• Zinc deficiency=increased risk
• Drugs, both recreational and prescription
• Cocaine, tobacco smoking (10+ cigs/day), alcohol, anticonvulsants, corticosteroids
• Metabolic diseases
• Diabetes (including gestational), maternal weight and obesity
• Ionizing radiation
Risk factors for cleft lip and/or palate include genetics and environment. A single factor can be found as the specific cause of the cleft.
1st statement true, 2nd statement false
General physical characteristics
• Incidence of multiple congenital anomalies is high with cleft lip and/or palate
• At least 400 syndromes have been identified in which clefting is the primary feature
• Facial deformities include depression of the nostril on the side with the cleft lip, deficiency of upper lip (may be short or displaced backward), overprominent lower lip
Characteristic of CL/P
• Infections
• Predisposition to middle-ear infections is common
• Feeding Issues - Infants are unable to create the negative intraoral pressure to suck milk from a bottle or breastfeed, need a special feeding device
• Speech -Difficulty making certain sounds, children may experience language delays
• Hearing Loss - Increased incidence of mild-mod hearing loss, may be associated with delayed speech development
Tooth development
• Disturbances in normal development of tooth buds occur more frequently
• Higher incidence of missing teeth, supernumerary teeth, developmental enamel defects, and microdontia or peg-shaped anterior teeth
• Common missing teeth include maxillary lateral incisors, mandibular second premolars
• Usually correspond to the side of the mouth that has the cleft
Malocclusion
• Majority of children with cleft lip and palate require orthodontic care
• Ortho treatment may be required after each stage of surgical treatment for cleft palate
Open palate
• Before surgical correction an open palate provides direct communication with the nasal cavity
• Cleft palate may cause formula or breast milk to pass into the nasal cavity
• A prosthetic palatal obturator may be constructed to aid in drinking an eating
Muscle coordination
• Lack of coordinated movements of lips, tongue, cheeks, floor of mouth, and throat may exist
• Compensatory habits may be formed by the patient in the attempt to produce normal sounds while speaking
Periodontal tissues
• Dental biofilm accumulation is influenced by the irregularly positioned teeth, inability to keep lips closed, mouth breathing, and the difficulties in accomplishing adequate biofilm removal, especially around the cleft areas
• Patients with cleft palate and lip have increased plaque indices, pocket depths, and slightly greater attachment loss
Dental caries
Children with cleft lip and/or palate are at higher risk for dental caries
Risk factors include:
• Malpositioned teeth
• Problems with mastication
• Longer oral clearance time when eating
• Diet selection
• Difficulty with adequate removal of dental biofilm
Feeding difficulties of infants and toddlers also contribute to ECC
Cleft lip
Surgical repair is usually done at 2.5-6 months of age and before 12 months of age
General rule of 10s: when the child is approx. 10 weeks of age, weighs 10 pounds, and has achieved a serum hemoglobin of 10 mg/mL
• The infant’s general health is a determining factor regarding when it is safe to perform the surgery
Rationale for early treatment
• Aid in feeding
• Encourage development of the premaxilla
• Help partial closure of the palatal cleft
• Assist families in adjusting to the birth of a child with cleft lip and/or palate
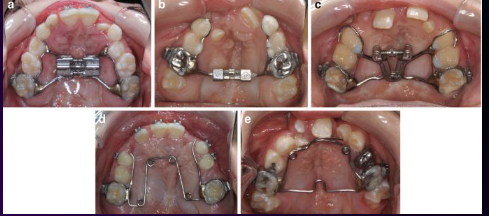
Orthodontics and dentofacial orthopedics
• In preparation for cleft closure, orthodontic, and orthopedic treatment may be needed to reduce the protrusion and stabilize the premaxilla
Cleft Palate: Surgery
Primary surgery to close the palate by 18 months of age or earlier when possible
Requires the combined efforts of many specialists
Goals for treatment:
• Produce anatomic closure, maximize maxillary growth and development, achieve normal function (particularly speech), relieve airway and breathing problems, establish good dental esthetics and functional occlusion
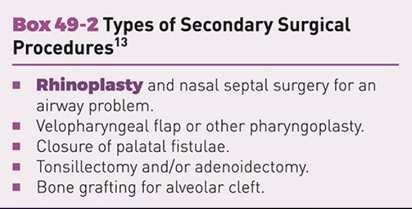
Secondary surgical care-see box
Use of bone grafting to repair residual alveolar and hard palate clefts
Alveolar graft: placed before eruption of max teeth at the cleft site, creates normal architecture teeth can erupt through, bone for implants if needed, support to teeth adjacent to cleft to minimize movement
• Hard palate graft: closure of oronasal fistulae, may be done simultaneously with alveolar graft, helps relieve compromised airway
• Sources for autogenous bone for graft: rib, iliac crest, skull, mandible, or bone morphogenetic proteins (BMPs)
• After bone grafting, implants can be used to replace individual teeth or provide support for a complete prosthesis
Other treatments
• Prosthodontics
• Orthodontics
• Speech-language therapy
• Restorative dentistry
• The dental hygienist is a member of the team with responsibilities to coordinate preventive dental and periodontal care
DH Role
• Preventive measures to preserve the teeth and supporting structures is essential to the success of the special care needed for the habilitation of the patient with cleft lip and/or palate
• Teeth are often poorly formed, lack enamel, and be at risk for loss due to decay
• Each phase of dental hygiene care and instruction takes on greater significance in light of magnified problems of cleft lip/palate
• Every attempt to avoid need to remove teeth, especially around cleft area (already weakened by lack of bone)
• Presence of teeth encourages optimum arch growth
DH Care
Parental counseling: anticipatory guidance
• Responsibility to refer for specialized care if not already initiated
• Primary concerns are daily dental biofilm removal and prevention of ECC
Objectives for appointment planning
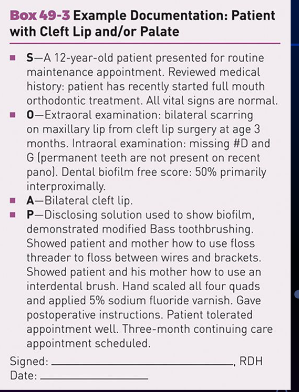
• Frequent appointments (every 3-4 mo) usually needed for maintenance
• Objectives include biofilm control, encouragement of good home care and cleanliness of removable prostheses
• Remove all calculus and biofilm as a supplement to patient’s self care
• Supervise caries prevention program for primary and permanent dentitions (fluoride and sealants)
Appointment considerations
Patient apprehension and self-esteem
• May be anxious due to multiple surgeries and medical visits
• Lower self-esteem, difficulties in social interaction, and bullying have been noted in patients with CL/P
Communication
• Speech may be difficult to understand
• Hearing loss may be a problem
Provide motivation
• MI can help patients and parents feel like active participants in decision making and goal setting
Patient education
Personal Oral Care Procedures
• Parents may be afraid of damaging the deformed areas or hurting the child when cleaning
• Be empathetic and provide continued instruction: personal daily care, fluoride
Diet
• Limit cariogenic foods and beverages
Smoking Cessation
• For patient or family members
• Emphasis on potential damage to the periodontal tissues
DH Care related to oral surgery
Presurgery
• Treatment objectives have particular significance because patients with cleft palate are more susceptible to upper respiratory and middle ear infections
Postsurgery Personal Oral Care
• After each feeding (liquid for several days, soft diet next week), the mouth is rinsed carefully
• Oral care needed but caution to avoid damage to healing suture lines
• Toothbrush with suction attachment may be useful
Documentation
• Description of location, classification, and extent of the cleft
• History and status of surgical interventions
• Missing teeth and related recommendations for self-care
• Description of prosthetic appliances and recommendations for daily care regimens
Quick points
• Provide parents with anticipatory guidance for management of risk factors for oral disease
• Individualized biofilm removal, especially for cleft areas
• Proper cleaning of tongue and removable appliances
• Necessity for regular dental hygiene appointments to prevent oral infection and caries
• Resources with addresses for team treatment clinics specializing in craniofacial development defects
(1) When communicating with a dental patient who has a cleft lip and/or palate, the dental hygienist should be aware that speech may be indiscernible. (2) If the patient has not been referred to a speech therapist, the dental hygienist should offer this recommendation.
Both are true
When is the primary surgery to close the palate usually performed?
A) prior to 1 week of age
B) prior to 1 month of age
C) prior to 6 months of age
D) prior to 12 months of age
E) prior to 18 months of age
E) prior to 18 months of age
Sarah is a 5-year-old who has just undergone secondary surgery related to her cleft palate. Her mother asks you the best way to clean her daughter’s oral cavity while she is recovering from the surgery. You explain that a useful adjunctive aid for cleaning the oral cavity after recent surgery is:
A.A fluoride mouthrinse
B.A disclosing solution
C.Gently rinsing with water
D.An interdental brush
C) Gently rinse with water
Brian is a 6-year-old patient with cleft palate and associated speech problems and hearing loss. A) Based on developmental milestones, Brian is old enough to assume sole responsibility for keeping his teeth cleaned. B) Parent involvement in his oral hygiene care should only be a supervisory role.
Both false
The development of the palate takes place during which weeks?
A.Weeks 3-4
B.Weeks 4-8
C.Weeks 12-14
D.Weeks 5-12
d) Weeks 5-12