Unit 3 Exam
1/68
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
69 Terms
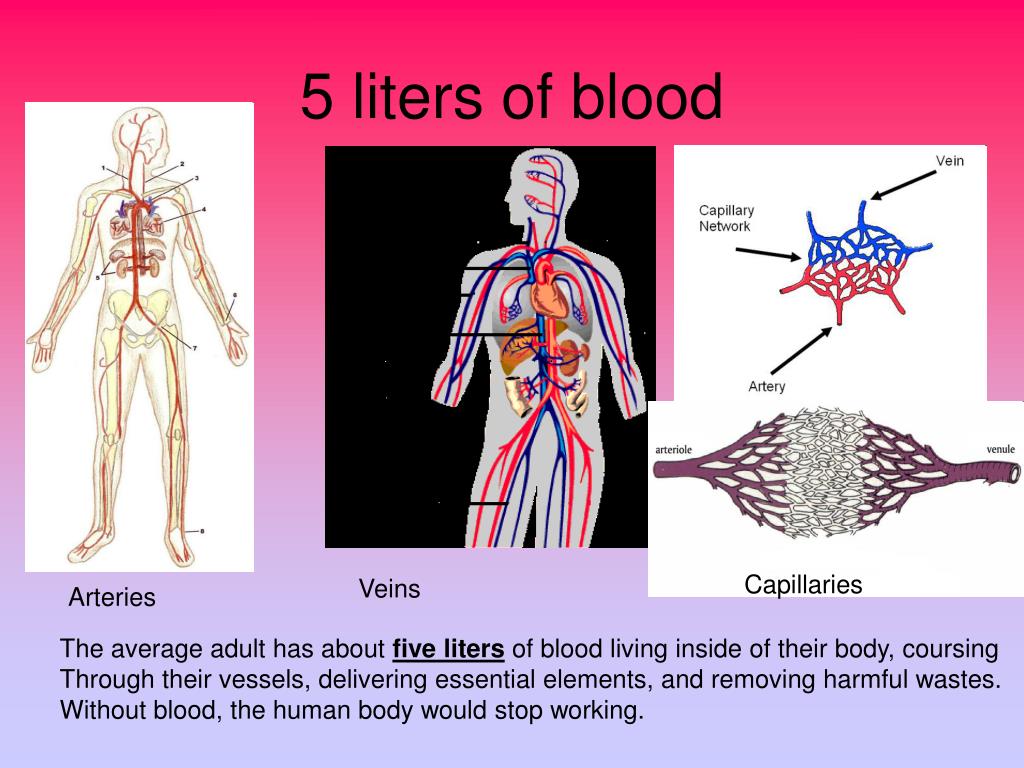
What is the amount of blood contained in the body?
5L
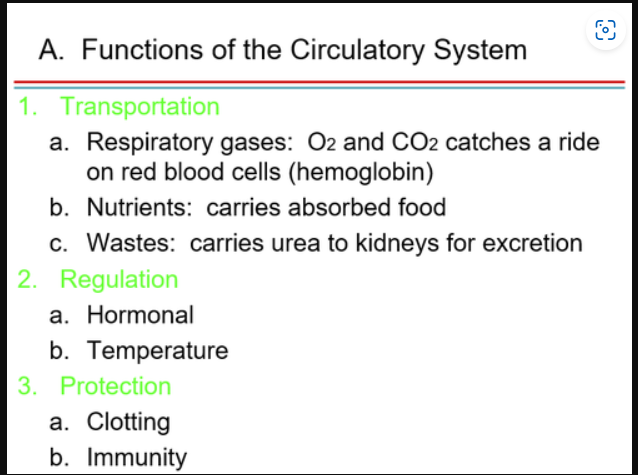
What is the function of the blood/circulatory system?
TRP
Transport - cellular metabolism are transported by the circulatory system
Regulation - blood carries hormones and other regulatory molecules
Protection - protects against injury & foreign microbes or toxins within the body
Clotting, mechanisms, leukocytes (immunity)
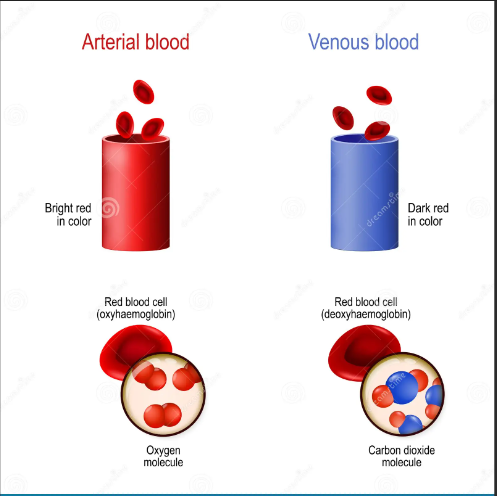
venous blood
deoxygenated
found in veins and pulmonary artery
oxygen-hemoglobin saturation approximately 75%
darker in color (blue)
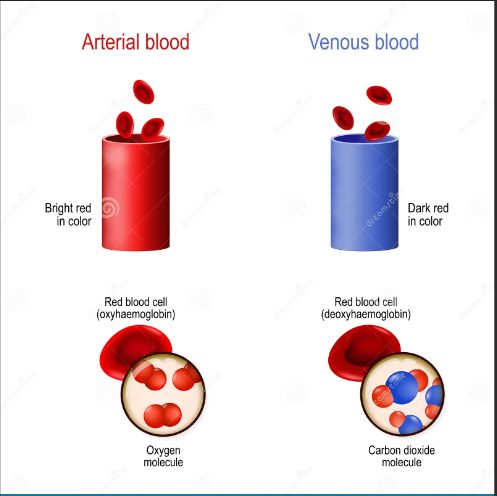
arterial blood
oxygenated, oxyhemoglobin
found in arteries and pulmonary vein
oxygen-hemoglobin saturation approximately 97-98%
bright (red)
Name the lowest plasma protein starting with an ‘F’ and it’s function?
Fibrinogen (4% of total plasma protein)
Assist thrombocytes in the formation of blood clots
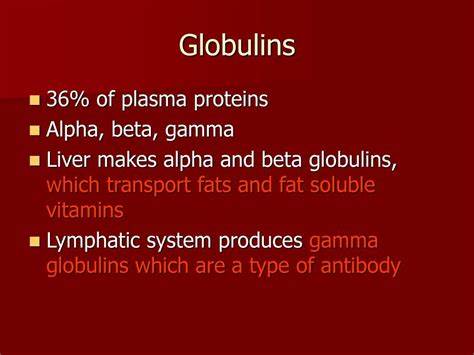
Name the second plasma protein with a ‘G’ and it’s function?
Globulins (36% of all plasma protein)
Alpha & beta - transport lipids & fat-soluble vitamins
Gamma - constitute anti-bodies of immunity
Name the third plasma protein with a ‘A’ and it’s function?
Albumin (60-80% of all plasma protein)
Functions to help maintain osmotic pressure of blood & carries certain molecules to the blood
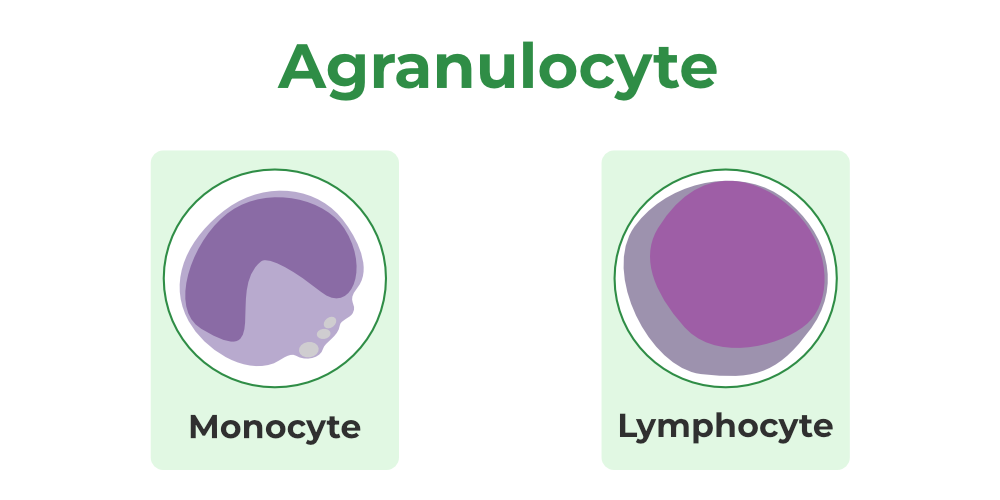
define agranulocytes & identify the purpose of each and prevalence in the body.
lack visibility in the cytoplasm
have spherical or kidney-shaped nuclei
lymphocytes - large purplish, circular nuclei with a thin rim of blue cytoplasm (25-45%)
mostly in lymphoid tissue, few circulate in the blood
crucial to immunity
monocytes - the largest leukocyte (3-8%)
abundant pale-blue cytoplasm
leave circulation, enter tissues, and differentiate into macrophages
actively phagocytic cells; crucial against viruses
activate lymphocytes to mount as immune response
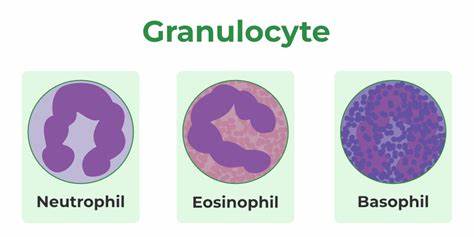
define granulocytes & identify the purpose of each and prevalence in the body
Neutrophils - bacterial infection; elevated neutrophil
most numerous WBCs
Give the cytoplasm a lilac color
Very phagocytic - “bacteria slayers”
Eosinophils - red-staining, bi-lobed nuclei
digest parasitic worms that are TOO large to be phagocytized
Basophils - antihistamines; blocking effects
Rarest WBCs
Large, purplish-black (basophilic) granules contain histamine
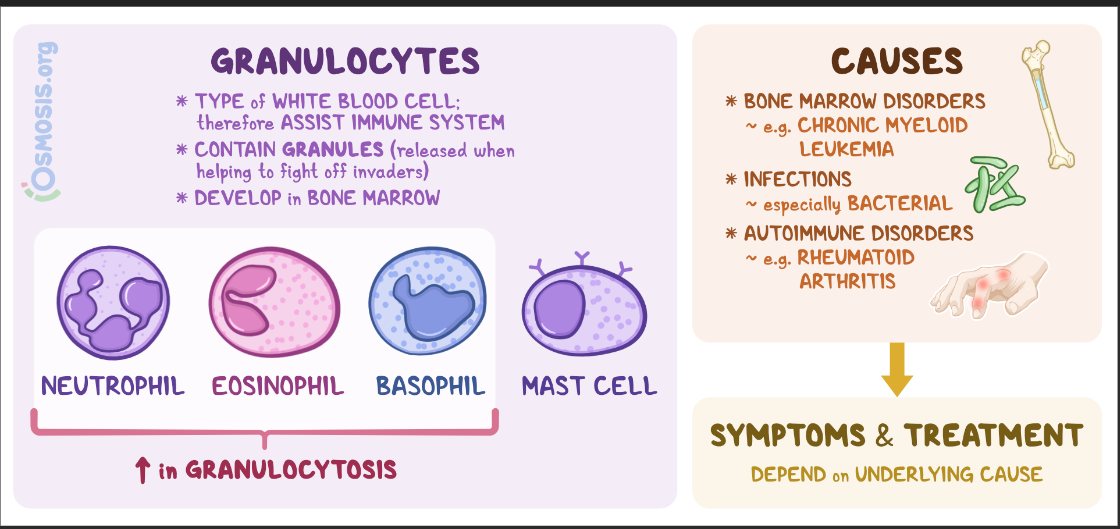
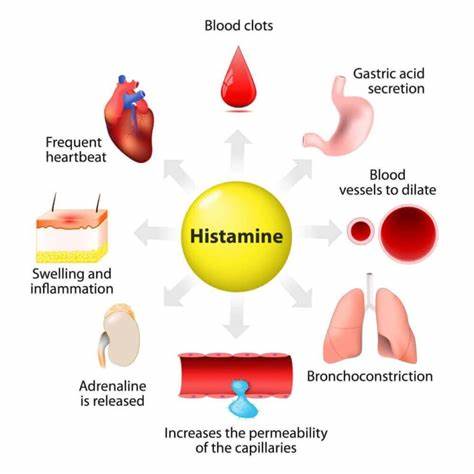
histamine
an inflammatory chemical that acts as a vasodilator and attracts other WBC to inflamed sites
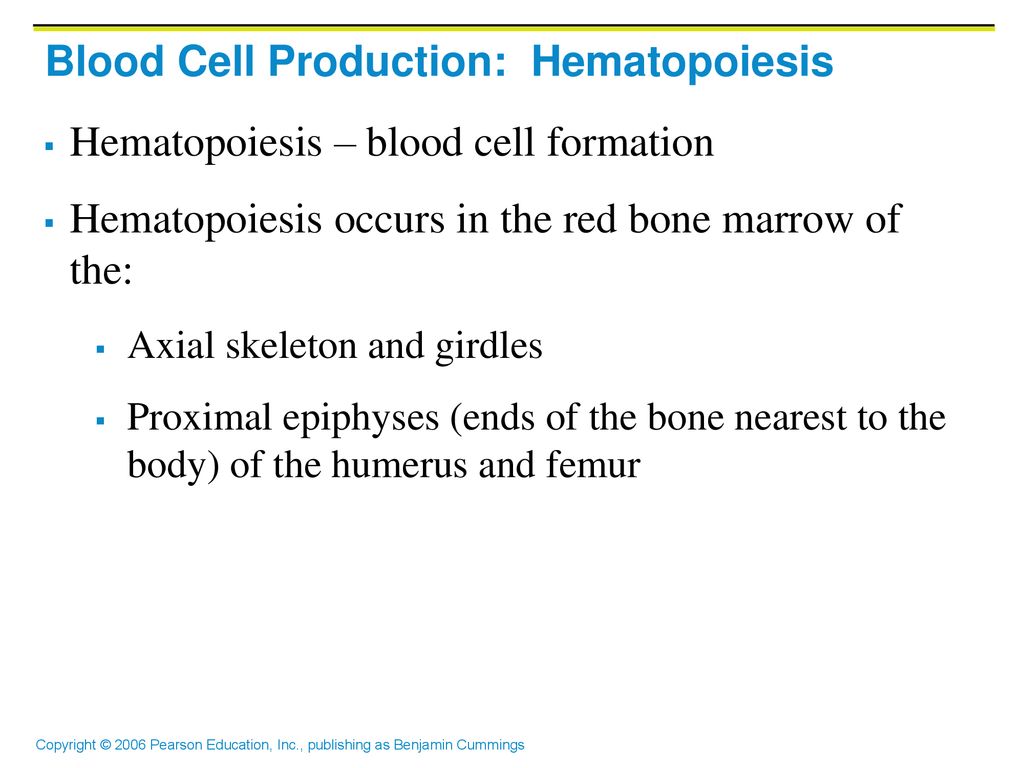
hemopoiesis
is the name of the process in which blood cells are formed
Starts with hemocytoblast (stem cell) → for all formed elements
ABO system
AB
Has both A and B antigens on the surface of red blood cells.
No anti-A or anti-B antibodies in the plasma.
universal recipient.
B
Has the B antigen on the surface of red blood cells
Anti-A antibody in the plasma.
Blood that can be received is B, O
A
Has the A antigen on the surface of red blood cells.
The anti-B antibody in the plasma.
Blood that can be received is A, O
O
Has no A or B antigens on the surface of red blood cells
Both anti-A and anti-B antibodies in the plasma.
It's the universal donor.
hemostasis
blood clotting is the mechanism in which injured vessels are repaired in order to control bleeding/blood loss
erythropoiesis
formation of erythrocytes (RBCs)
estimated that 2.5 million erythrocytes are produced every second in order to replace those destroyed
Myeloid Tissue - red bone marrow
Humeri
Femora
Ribs
Sternum
Vertebrae
Parts of the Skull
leuokpoiesis
leukopoiesis
formation of leukocytes (WBCs)
Lymphoid Tissue - lymphatic tissues
Lymph nodes
Tonsils
Spleen
Thymus
What are the three hemostatic mechanisms discussed?
Breakage of endothelial lining of a blood vessel exposes collagen proteins to the blood initiating…
Vascular Spasm - vasoconstriction of damaged blood vessel; reduced blood flow & minimize blood loss
Platelet Plug Formation
Positive feedback cycle
At site of blood vessel injury; platelets:
Stick to exposed collagen fibers with the help of plasma proteins
Coagulation
Blood is transformed from a liquid to a gel
Reinforces the platelet plug with fibrin
define blood
a vital fluid that circulates through your body, delivering essential substances like oxygen and nutrients to cells, and removing waste products.
connective tissue of plasma & formed elements
define formed elements
45 - 50% of blood volume
Erythrocytes (RBC) - most numerous blood cell
Leukocytes (WBC) - contain nucleus & mitochondria
Thrombocytes (platelets) - no nucleus
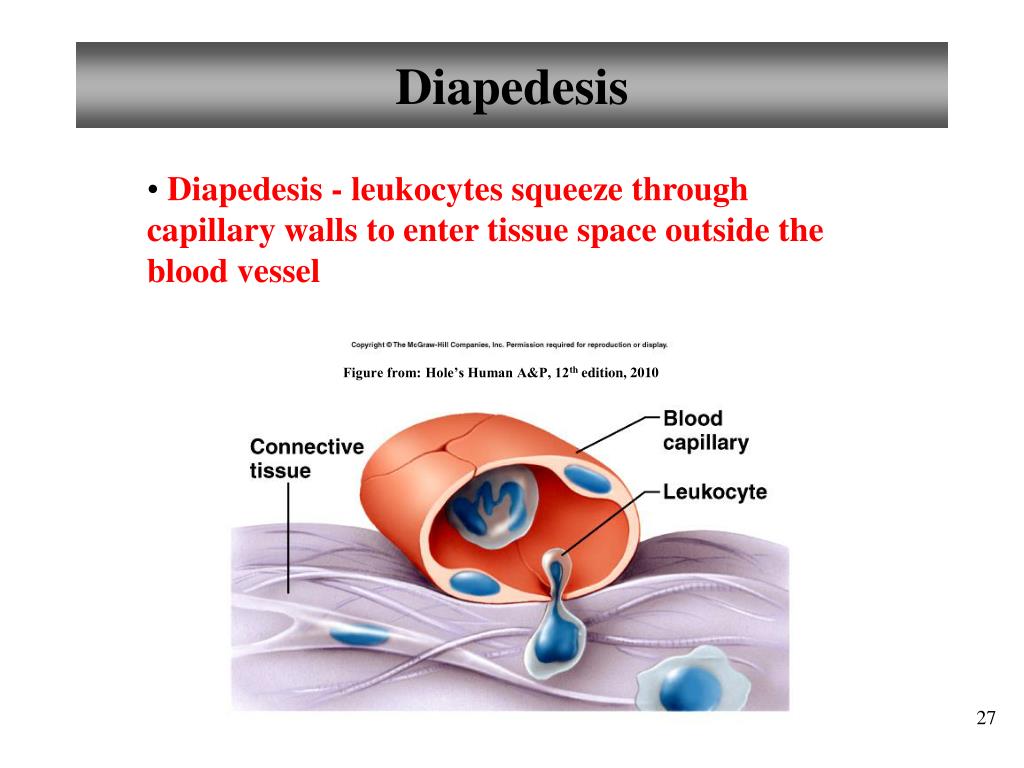
define diapedesis
leukocytes squeeze through capillary walls to enter tissue space outside the blood vessel
define plasma
50 to 55% of total blood volume
Straw colored liquid containing dissolved substances (liquid left after formed elements are removed)
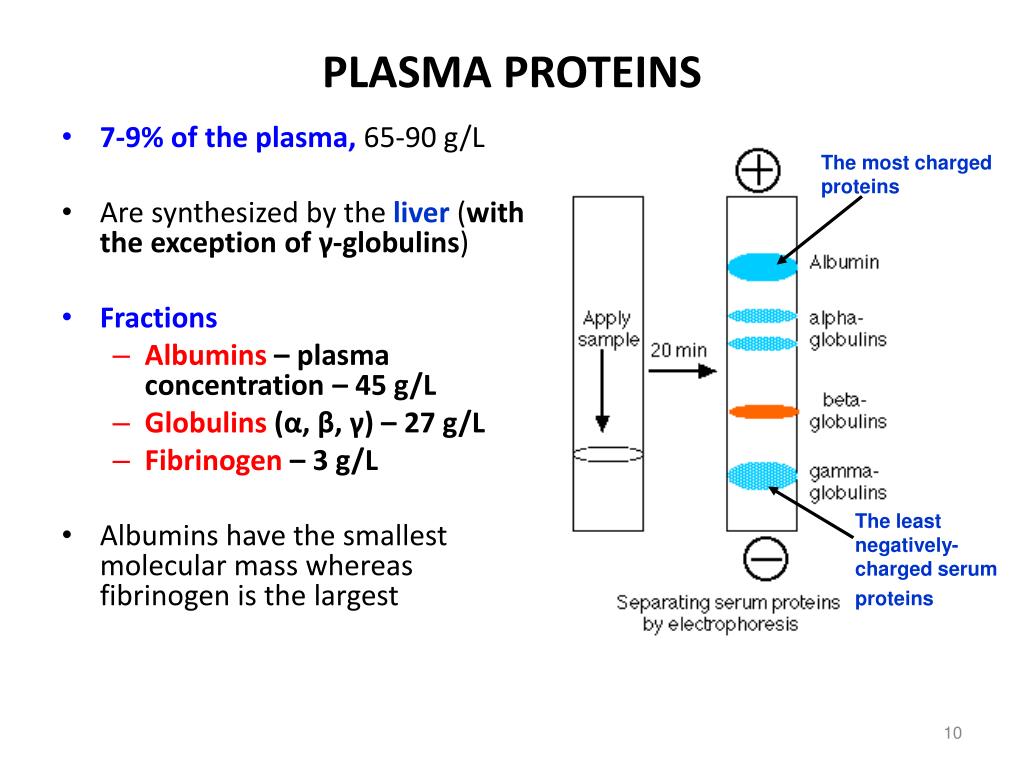
define plasma proteins
mostly produced by the liver found in (blood) plasma.
Function:
Including transport of lipids, hormones, vitamins, and minerals, as well as immune system activity.
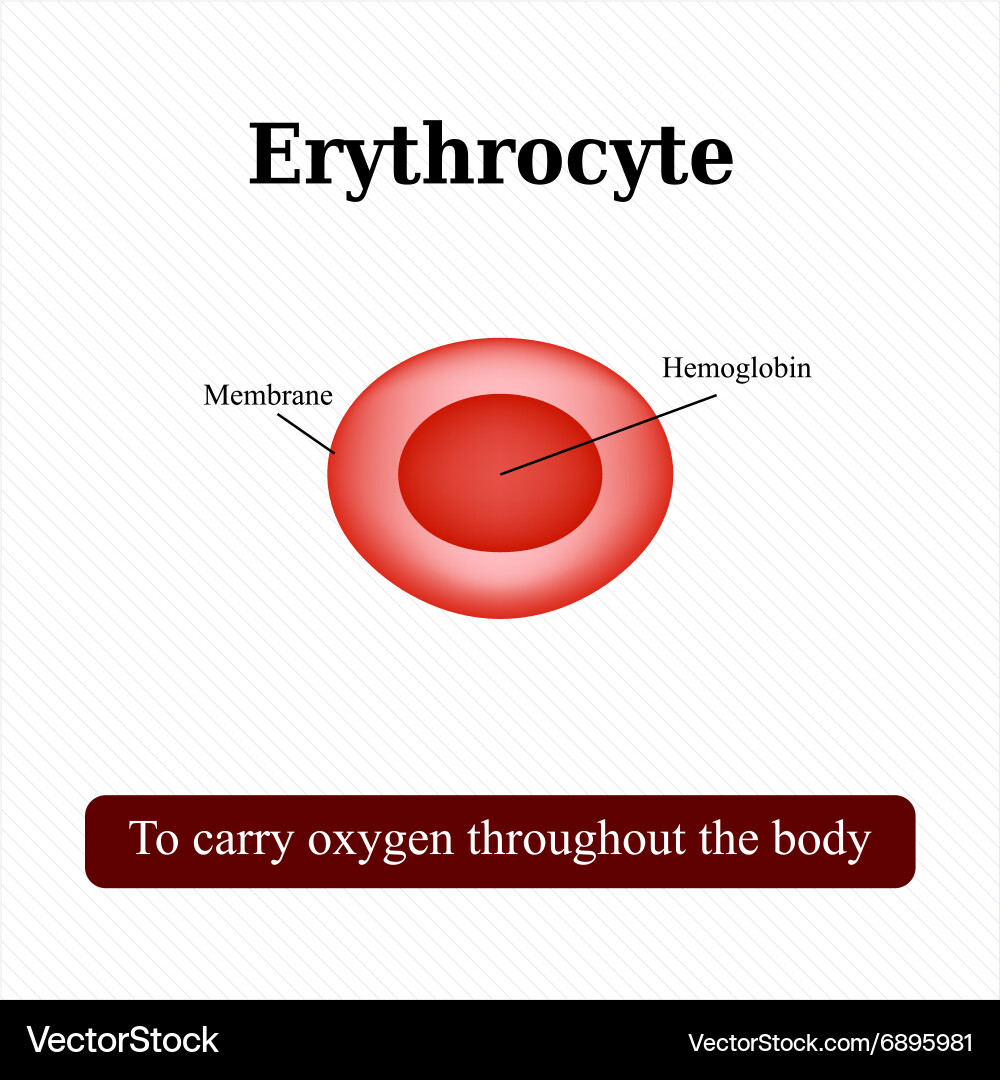
define erythrocytes
Biconcave (no nucleus); no organelles
Biconcave shapes increase surface area = increases gas exchange
No mitochondria: ATP production is anaerobic; no O2 is used in generation of ATP
Contains hemoglobin (Hb) which functions to transport oxygen & carbon dioxide within the blood
function of erythrocytes
Transport oxygen from the lungs to all body tissues.
Pick up carbon dioxide at the tissues and transport it to the lungs
definition of leukocytes
Contain nucleus & mitochondria
Can move in & out of the blood vessels. The name given to this movement
Only complete cells of the blood formed elements
function of leukocytes
to aid in defense against infections by micro-organisms
thrombocytes (platelets)
(cytoplasmic fragments) of large cells (megakaryocytes)
The phospholipid in their membrane serve to activate the clotting factors in the plasma
function of thrombocytes
to assist the blood clotting mechanisms
epicardium (1st part of heart wall)
visceral layer of the serous pericardium
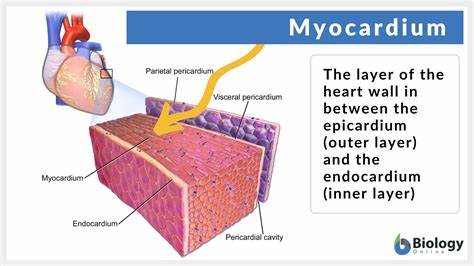
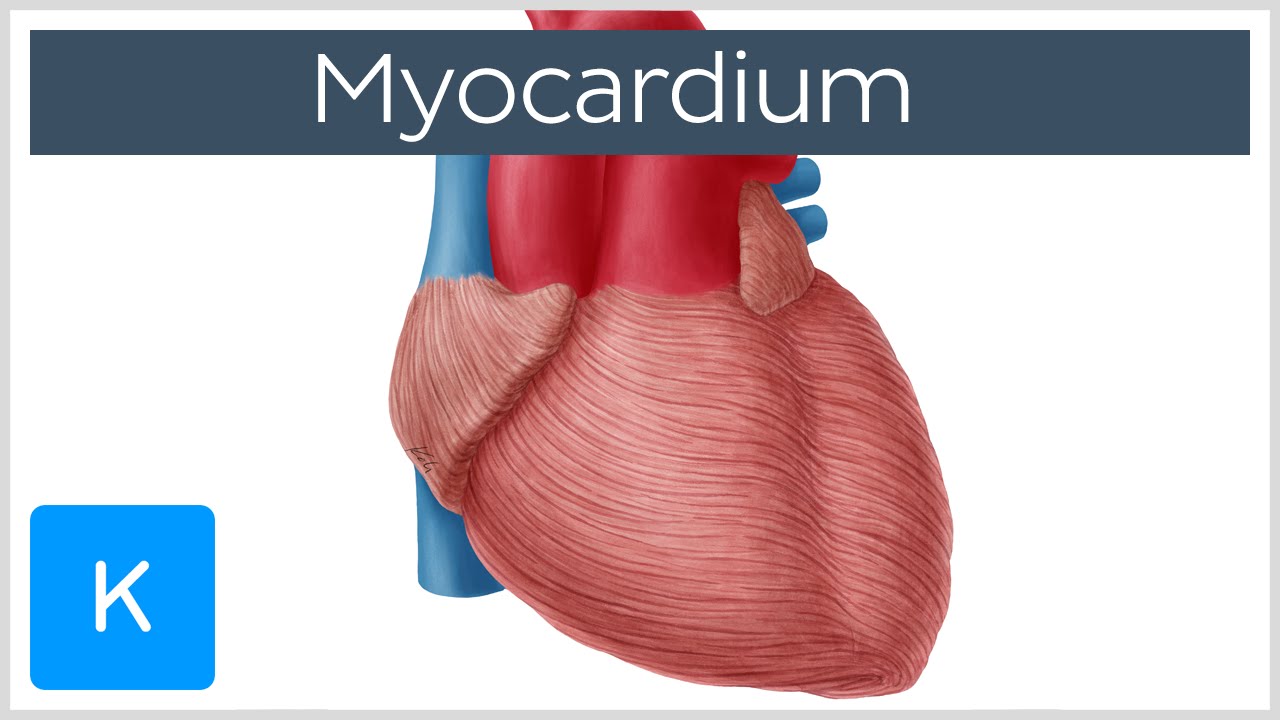
myocardium (2nd part of heart wall)
Spiral bundles of cardiac muscle cells
Fibrous skeleton of the heart: crisscrossing, interlacing layer of connective tissue
Anchors cardiac muscle fibers
Supports great vessels and valves
Limits spread of action potentials to specific paths
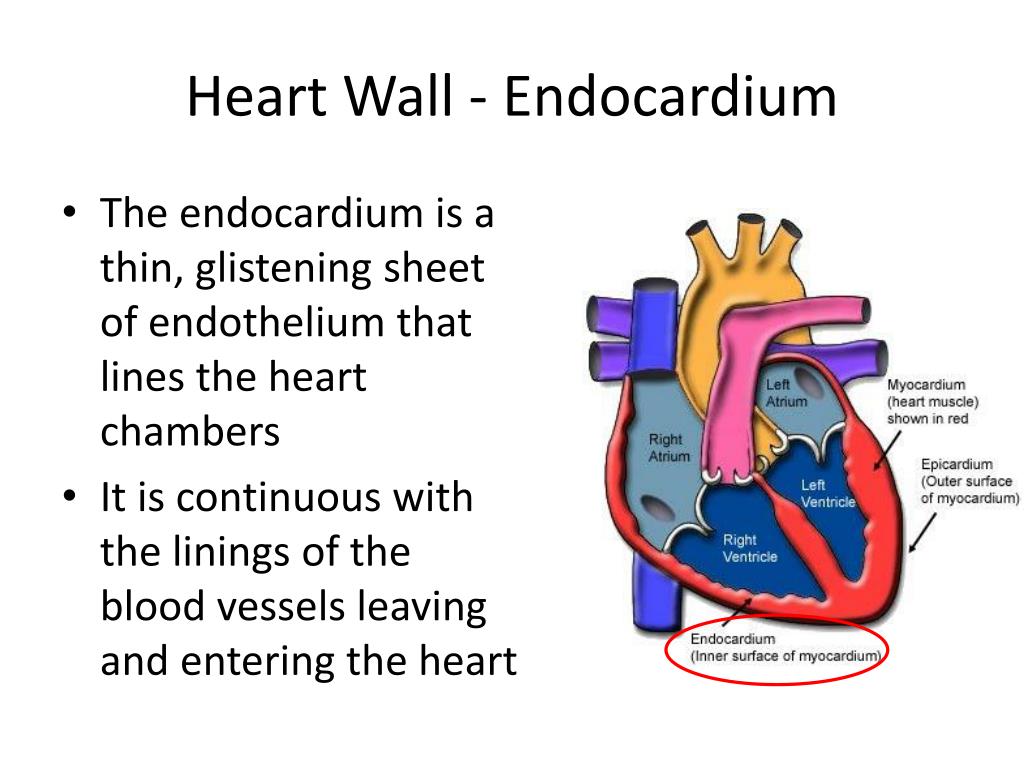
endocardium (3rd part of heart wall)
the continuous of linings blood vessels leaving and entering the heart
thin smooth membrane which lines the inside of the chambers of the heart and forms the surface of the valves
How does the myocardium differ between the R and L atria and the R and L ventricles?
Atria: The Receiving Chambers
R and L atria [need to contract only minimal blood for ‘downstairs’]
Blood drains back to the heart into the atria
Separated internally by the interatrial septum
Small, thin-walled structures
Ventricles: The Discharging Chambers
Two ventricles [massive walls]
Separated by the interventricular septum
Pumps blood into circulation [out from the heart into circuits
Walls are (irregular) ridged by trabeculae carneae
Papillary muscles project into the ventricular cavities
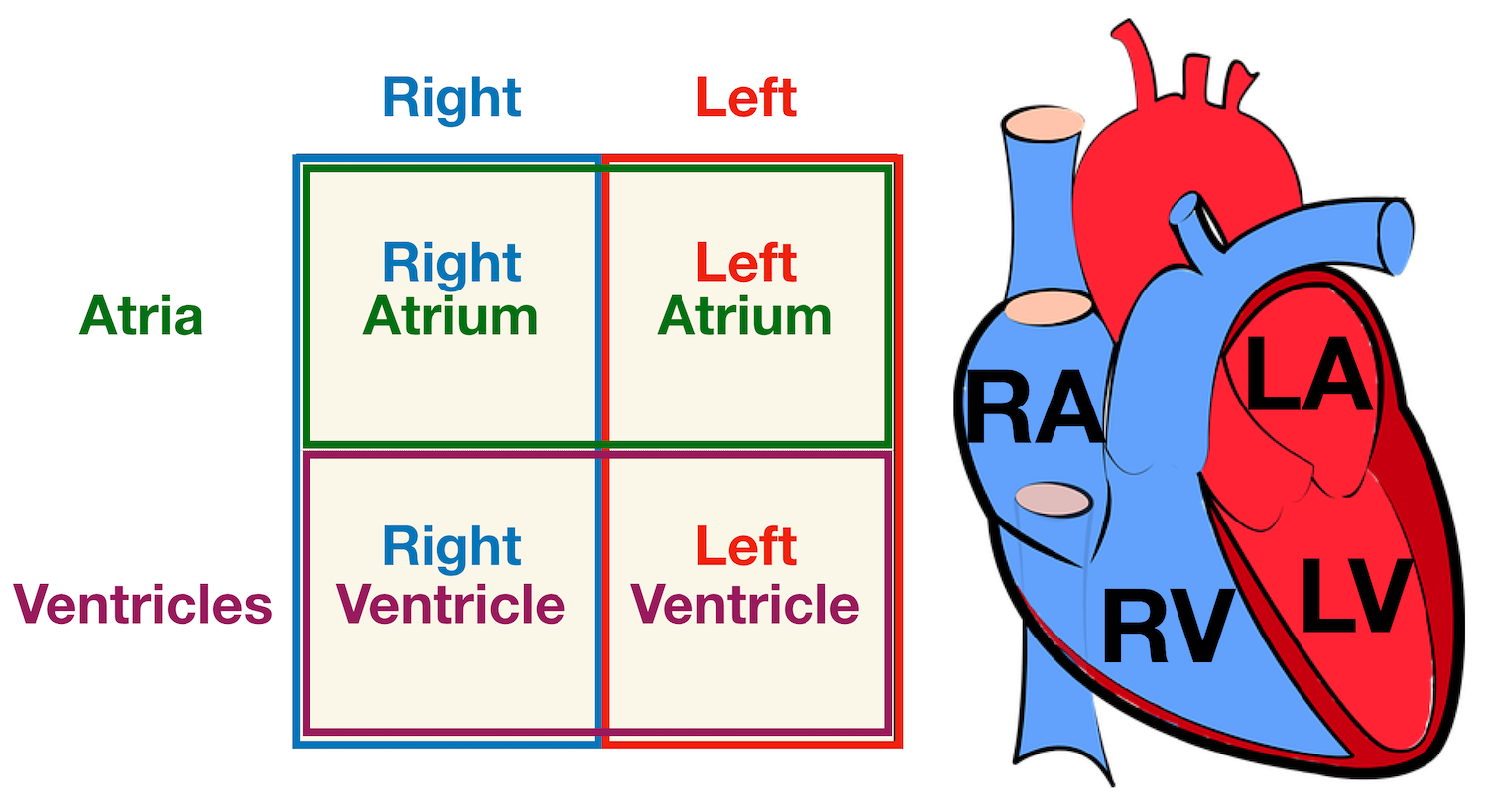
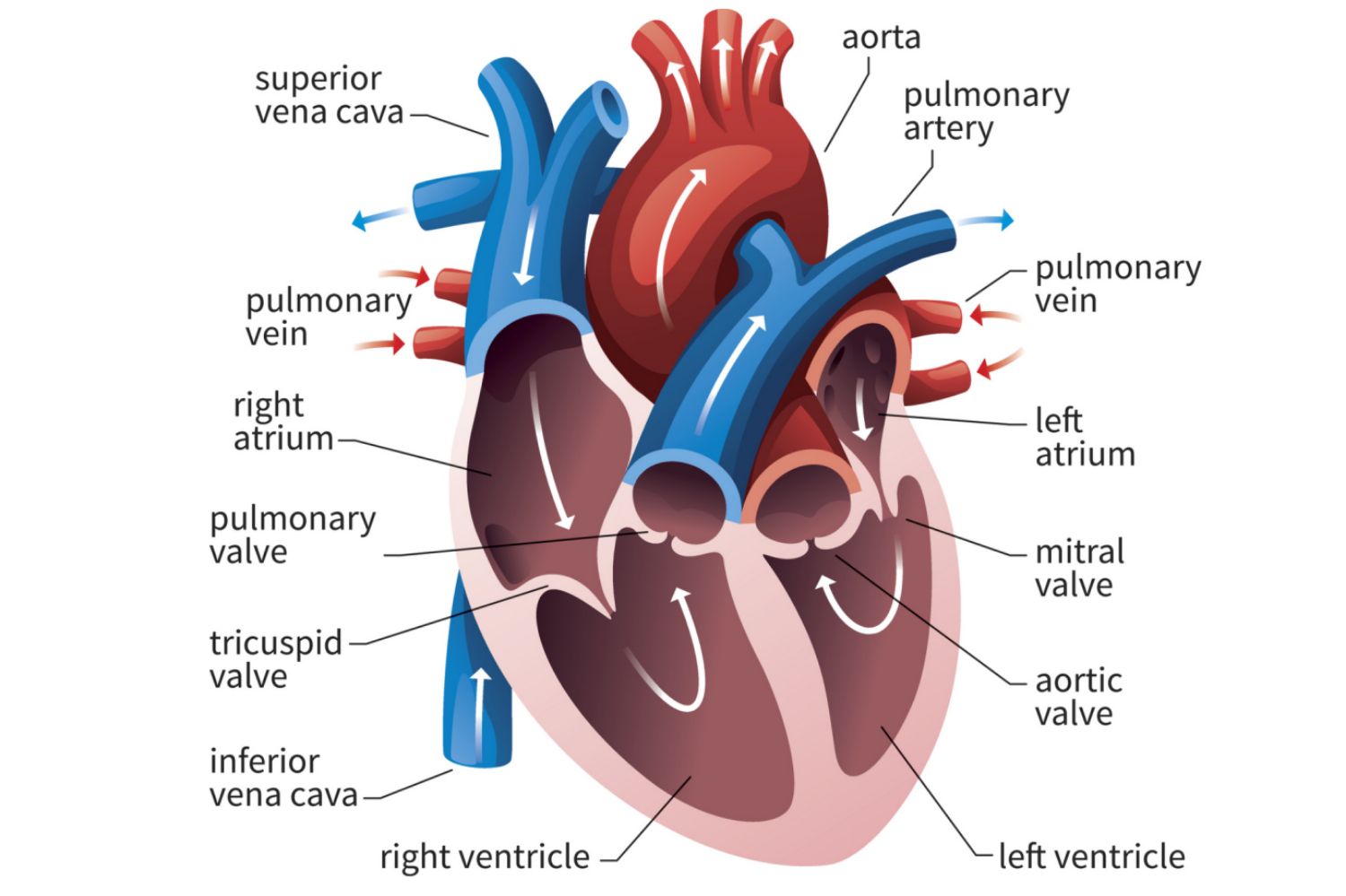
chambers of the heart and what it does?
4 chambers of the heart
Right Atrium: Receives deoxygenated blood from the body through the superior and inferior vena cavae.
Right Ventricle: Pumps deoxygenated blood to the lungs via the pulmonary arteries.
Left Atrium: Receives oxygenated blood from the lungs through the pulmonary veins.
Left Ventricle: Pumps oxygenated blood to the body through the aorta.
heart valves and what it does?
Atrioventricular Valves (AV) - prevents backflow of the blood, when ventricles contract
Tricuspid Valve (Right atrioventricular) - has three flexible flaps of endocardium reinforced by connective tissue cores
Bicuspid Valve (Mitral valve & left atrioventricular) - with two flaps
Semilunar Valves (SL) - guard the bases of the large arteries issuing from the ventricles
Pulmonary Semilunar Valve (Right Semilunar) - base of the pulmonary trunk
Aortic Semilunar Valve (Left Semilunar) -oxygenated blood leaves to the rest of the body
major vessels associated with each chamber and what it does
Right Pump Chamber
Superior & Inferior Vena Cava (vein)
Deoxygenated blood from body → heart (R atrium)
Pulmonary Artery (away from the heart)
Deoxygenated blood from heart (R ventricle → pulmonary trunk) → to the lungs
Left Pump Chamber
Pulmonary Vein (back to heart)
Oxygenated blood from lungs → heart (L atrium)
Aorta (from the heart to the artery)
Oxygenated blood from heart (L ventricle) to rest of the body
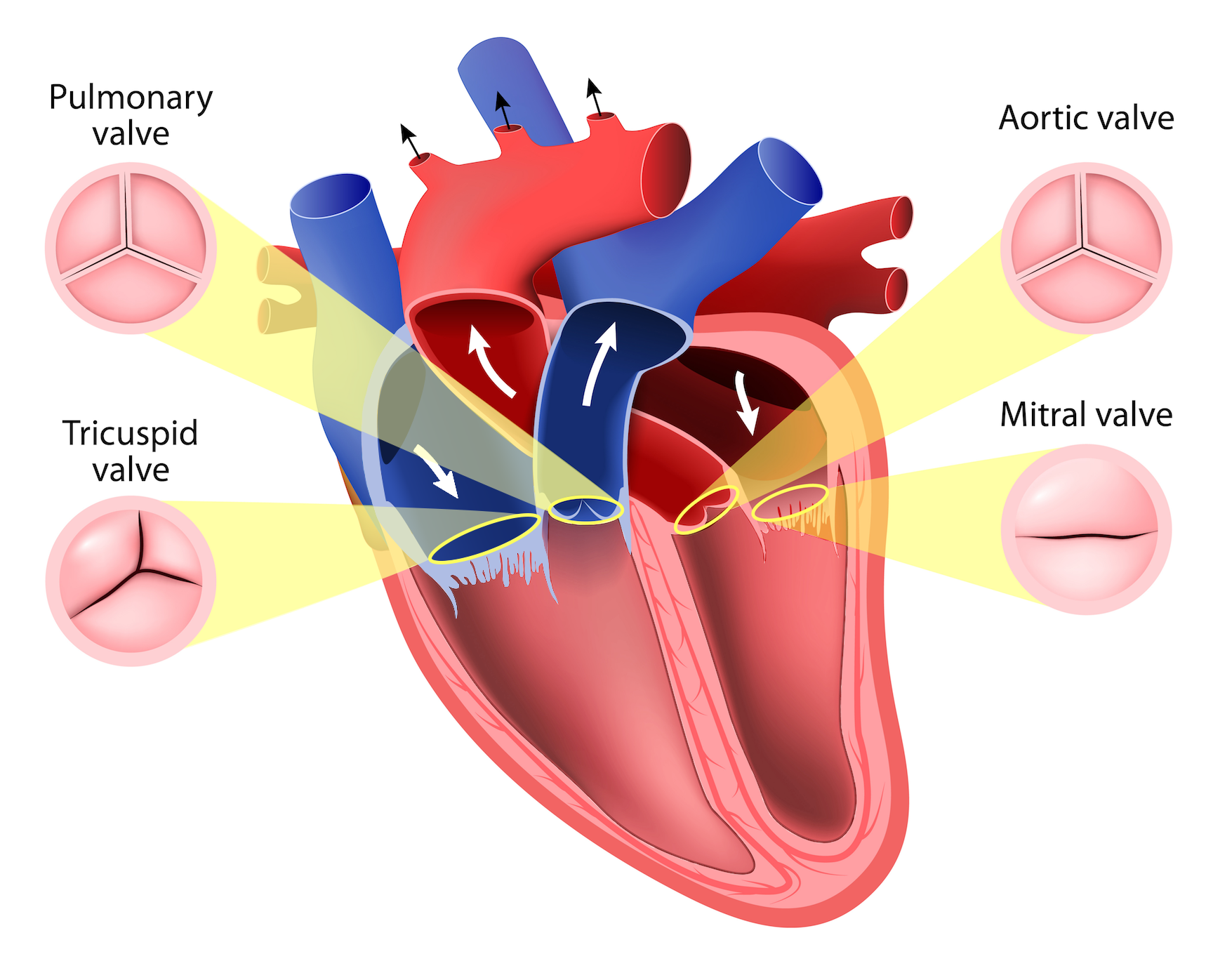
What is the purpose of the heart valves? Understand their precise role during the cardiac cycle.
blood flows in the correct direction through your heart, preventing any backflow and maintaining efficient circulation.
the opening and closing in response pressure differences that are generated from those mechanical events systole & diastole.
Basically ‘traffic controllers’ of the cardiovascular system
Identify the circulatory routes for blood flow throughout the body.
Right side is the pump for the pulmonary circuit (short, low pressure circulation)
Vessels that carry blood to & from the lungs
Left side is the pump for the systemic circuit & coronary circuit (blood encounters much resistance)
Vessels that carry blood to & from all body tissues
How is blood carried to and from the myocardium?
The coronary arteries branch off from the aorta and supply oxygen-rich blood to the myocardium.
irregular pulsating blood flow to the myocardium.
delivers blood when the heart is relaxed, but ineffective when ventricles are contracting
The coronary veins collect venous blood whose paths roughly follow those of the coronary arteries.
They join an enlarged vessel called the coronary sinus, which empties the blood into the right atrium.
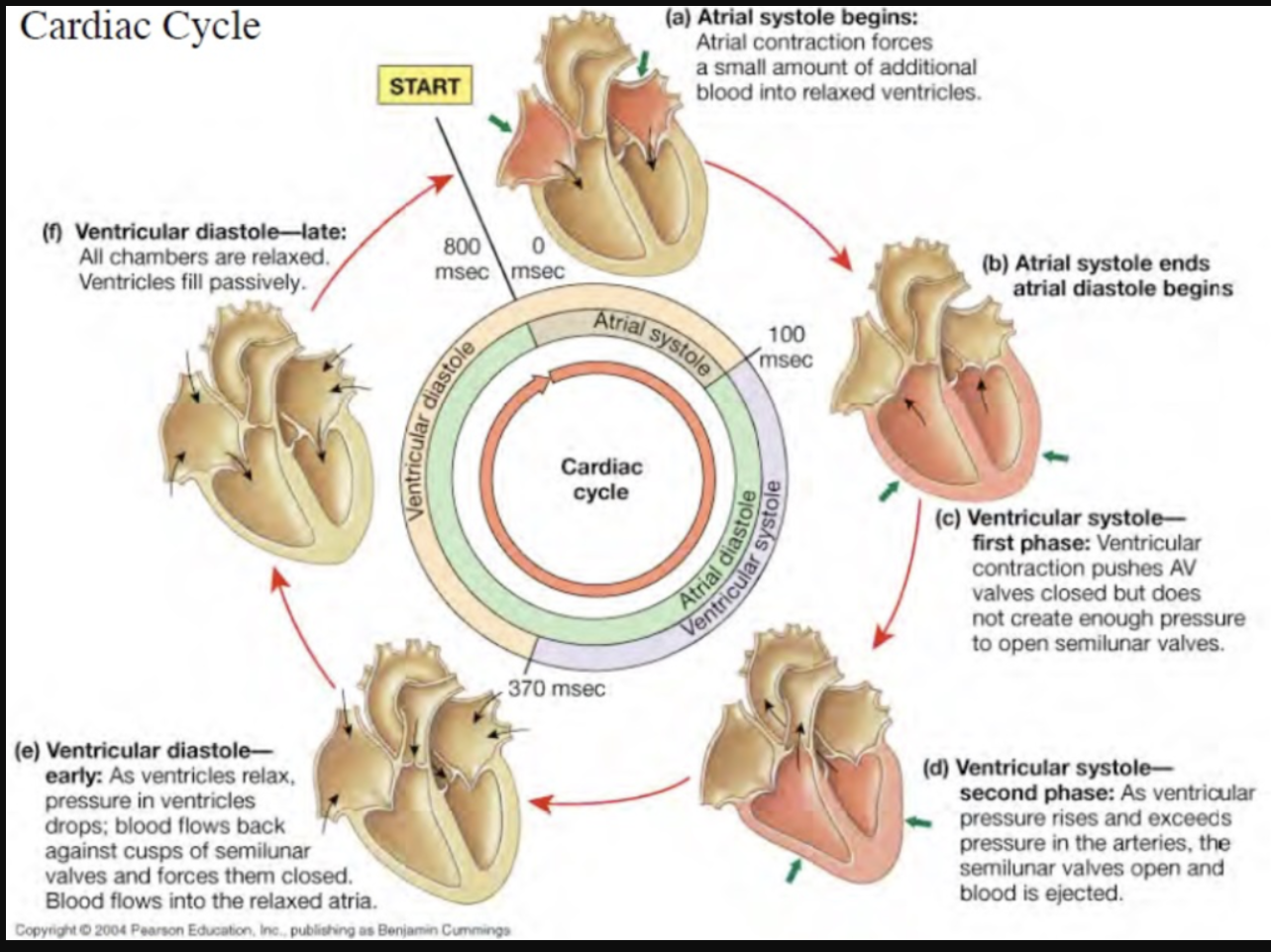
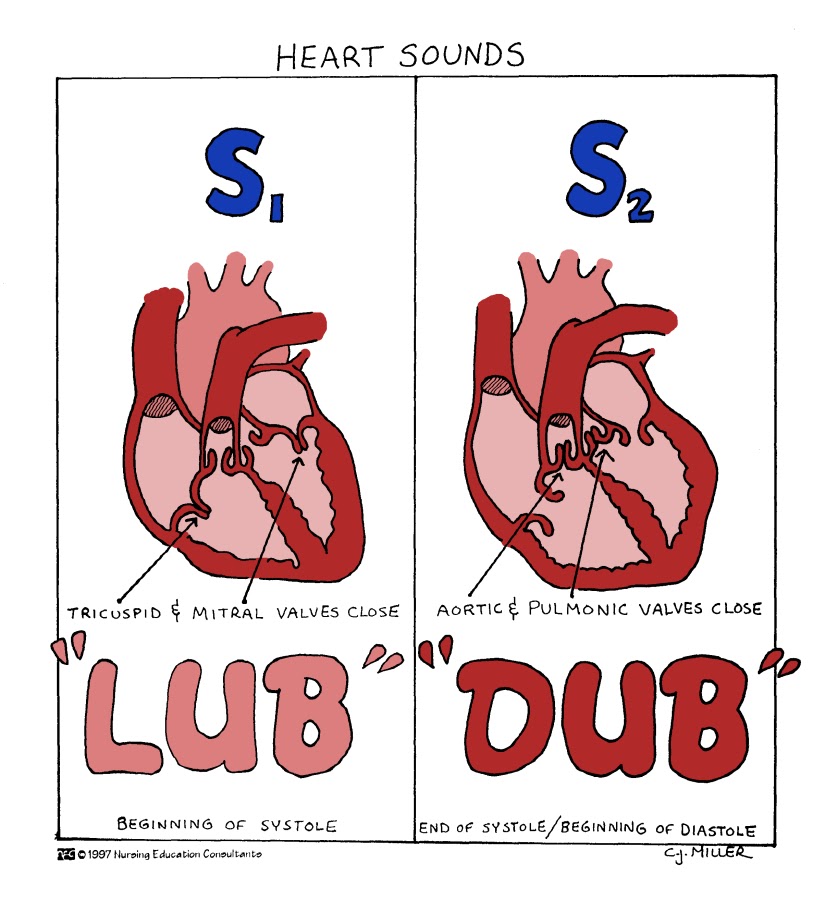
Understand the cardiac cycle: sequence of events encompassing one complete contraction and relaxation of the atria and ventricles of the heart.
Atrial Systole:
Atrial contraction forces a small amount of additional blood into relaxed ventricles.
Ventricular Systole:
Ventricles contract.
Blood is pushed out of the right ventricle into the pulmonary artery (to the lungs) and out of the left ventricle into the aorta (to the rest of the body).
The atrioventricular valves (tricuspid and mitral) close to prevent backflow into the atria.
Atrial Diastole:
Atria relax and fill with blood from the veins (vena cavae into the right atrium and pulmonary veins into the left atrium).
This phase coincides with ventricular systole.
Ventricular Diastole:
Ventricles relax after contraction.
Blood flows from the atria into the ventricles, filling them in preparation for the next cycle.
The semilunar valves (pulmonary and aortic) close to prevent backflow from the arteries.
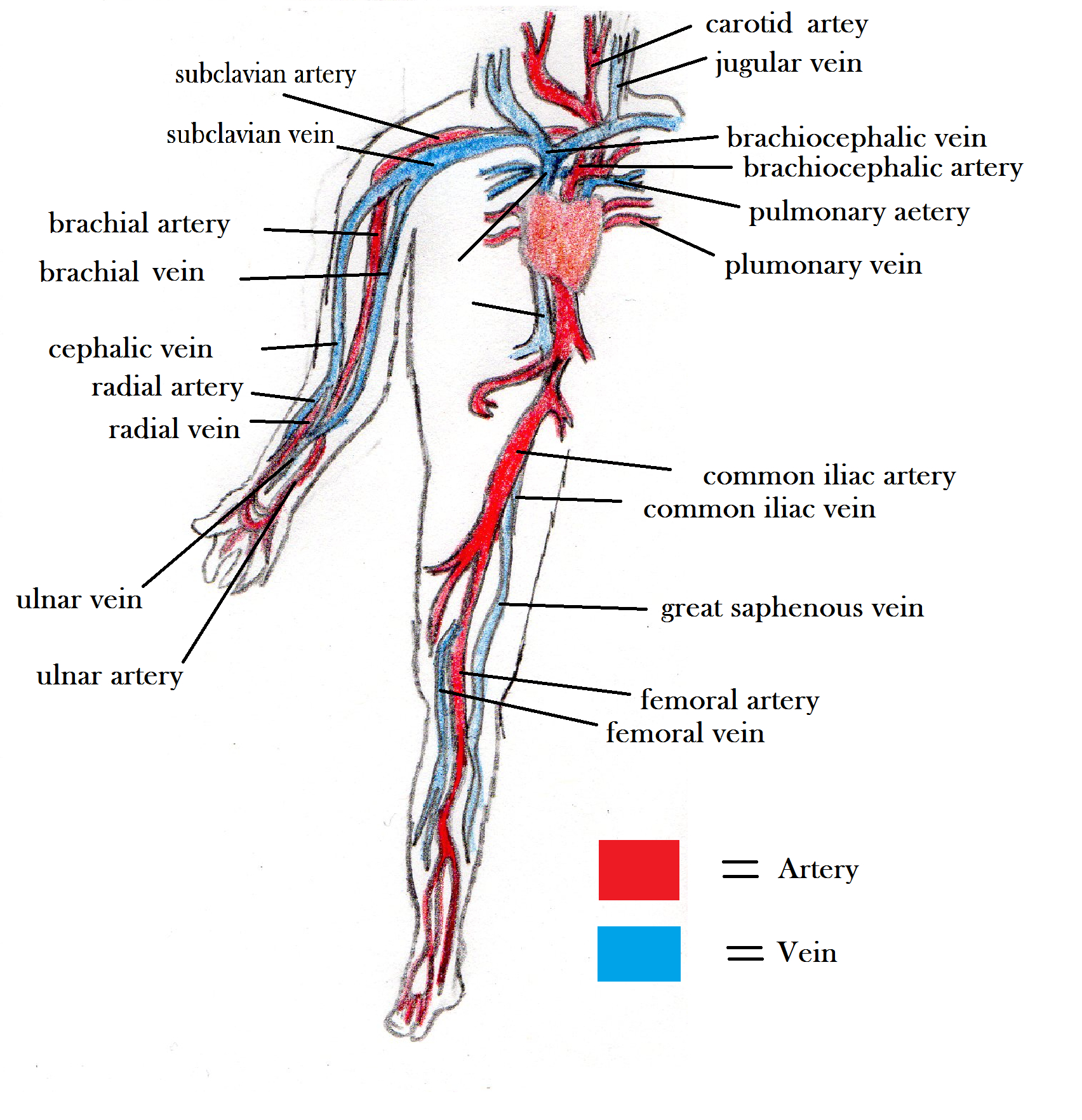
define arteries
Large thick-walled arteries with elastin in ALL three tunics.
Have thick tunica media with more smooth muscle
Carry blood under relatively high pressure
Expand & recoil as blood is ejected from the heart
resistance & distribution vessels
15% blood volume distribution
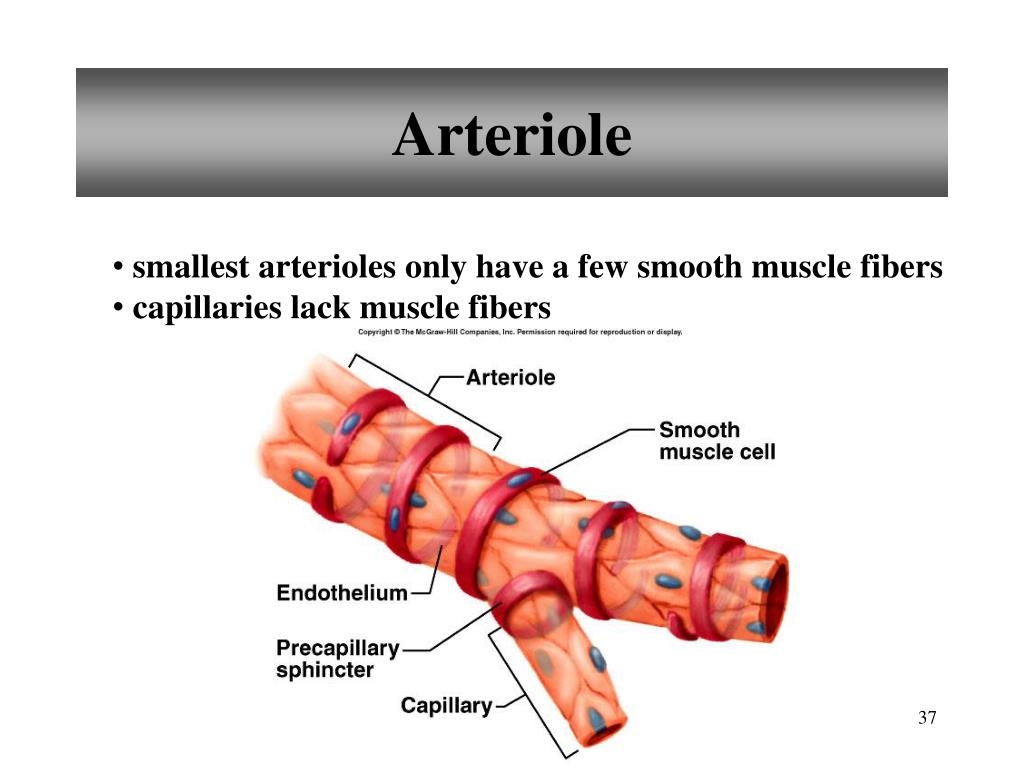
define arterioles
Smallest arteries
Lead to capillary beds
Control flow into capillary beds via vasodilation & vasoconstriction
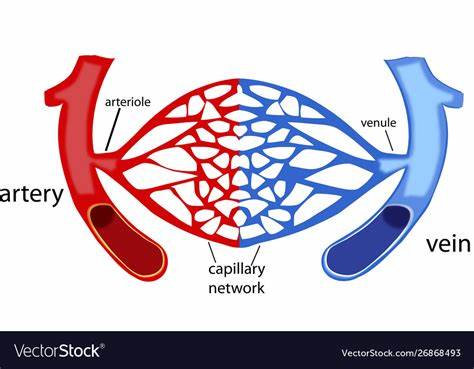
define capillaries
Microscopic blood vessels
Walls of thin intima, one cell thick
Size allows only a single RBC to pass at a time
5%
(35-15 mm Hg) low pressure
Exchange vessels
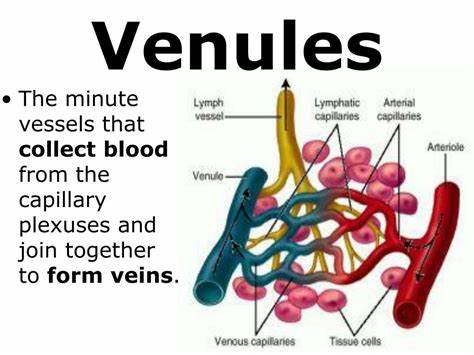
define venules
Formed when capillary beds unite with the veins.
Very porous; allow fluids & WBCs into tissues
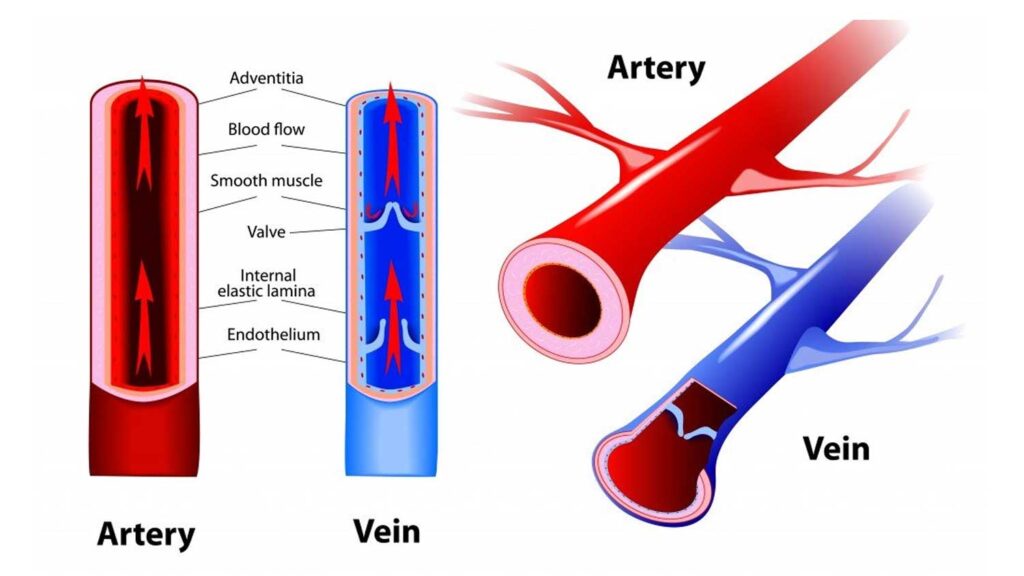
define veins
Thinner-walled than arteries, with larger lumens.
They contain valves to prevent backflow and rely on skeletal muscle contractions to help push blood back to the heart.
venous pumps
capacity vessels
64%
(15-0 mm Hg) ; low pressure
Why is the capillary conserved to be the “functional unit” of the circulatory system?
their thin walls allow for the exchange of oxygen, nutrients, and waste products between blood and tissues making it the functional unit.
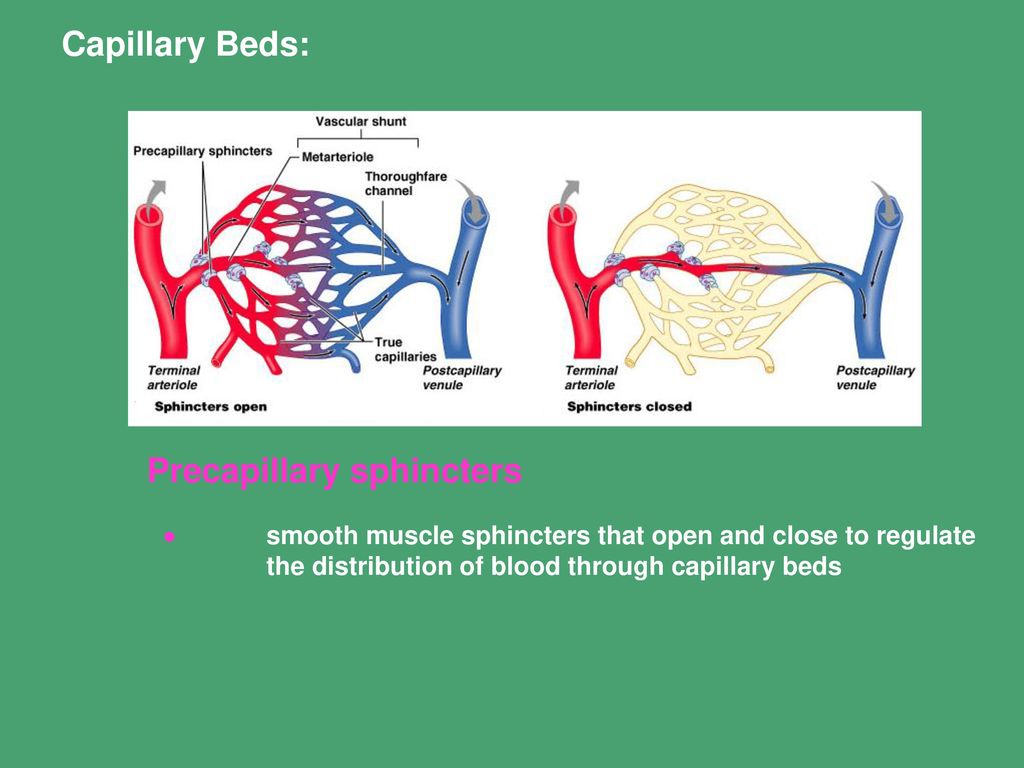
What is the function of the precapillary sphincter?
acts as a valve to regulate blood flow into the capillaries.
(not innervated) By constricting or relaxing, it controls the amount of blood that reaches the tissues, ensuring that blood is directed to the organs most needed.
Understand the factors that influence filtration and re-absorption between the capillaries and the surrounding tissues.
water & substances leave capillaries because of net outward pressure (arteriole end)
enter because of net inward pressure (venule end)
diffusion - lipid soluble substances pass directly through
filtration -
hydrostatic pressure pushes out
colloid osmotic pressure draws fluid back in
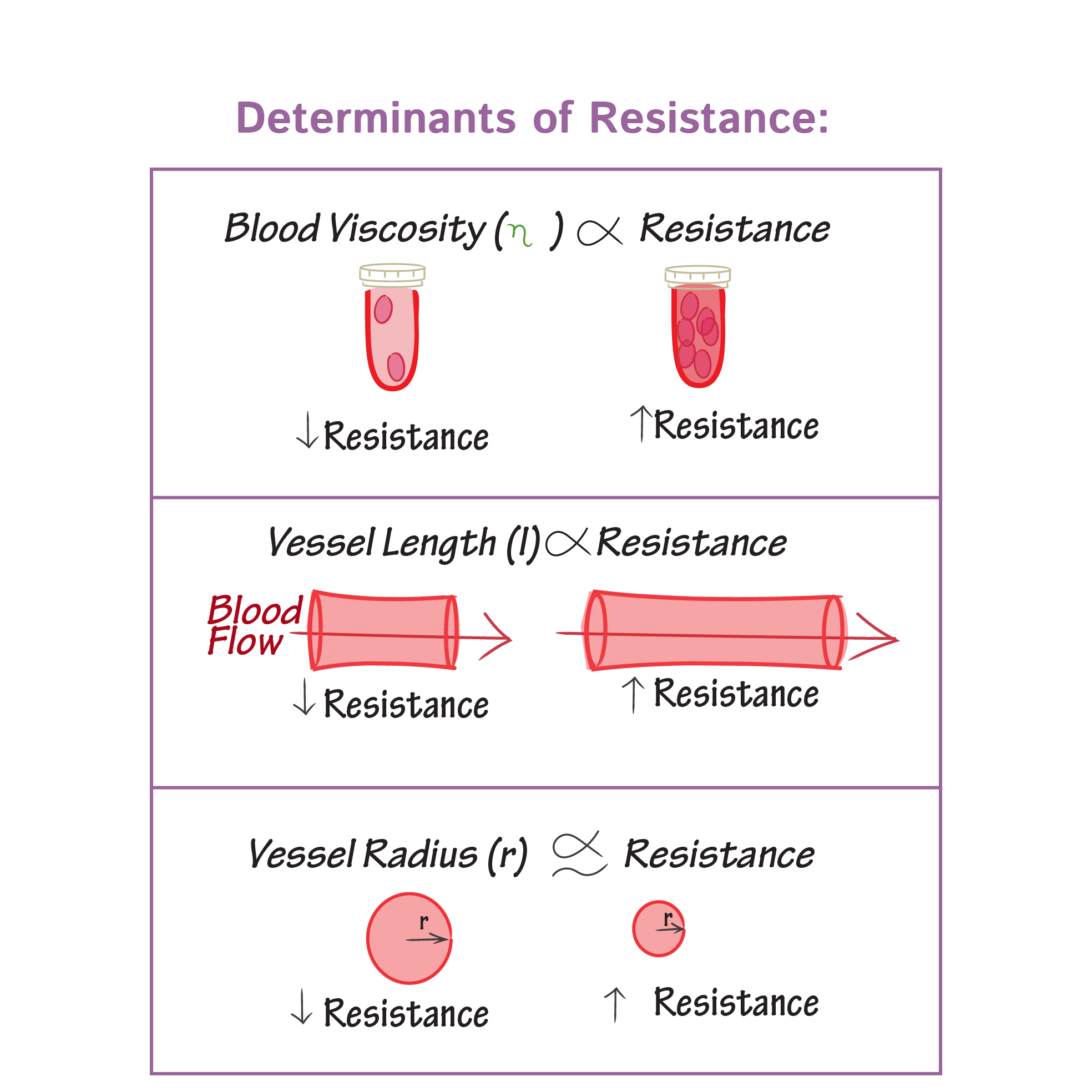
What factors influence peripheral (systemic) resistance?
Blood viscosity
Greater viscosity, the greater the resistance
Blood vessel length
Longer the vessel, the greater the resistance
Blood vessel diameter (size of the lumen)
Smaller the tube, greater the resistance
friction
(opposition to blood flow) b/w blood & vessel wall
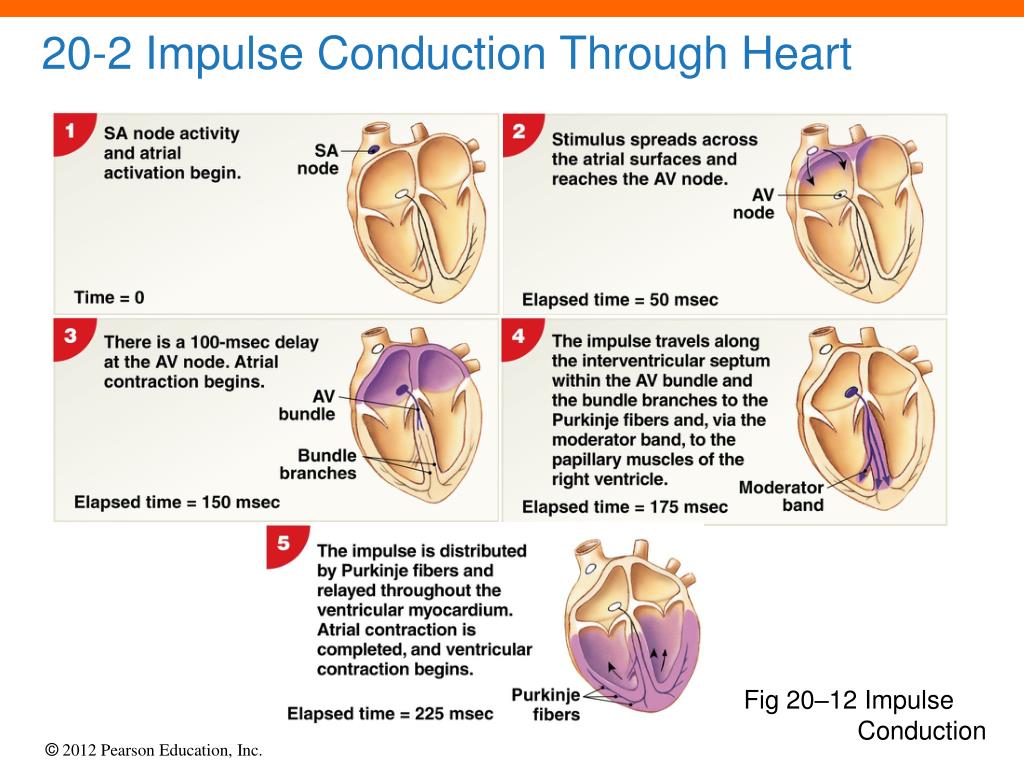
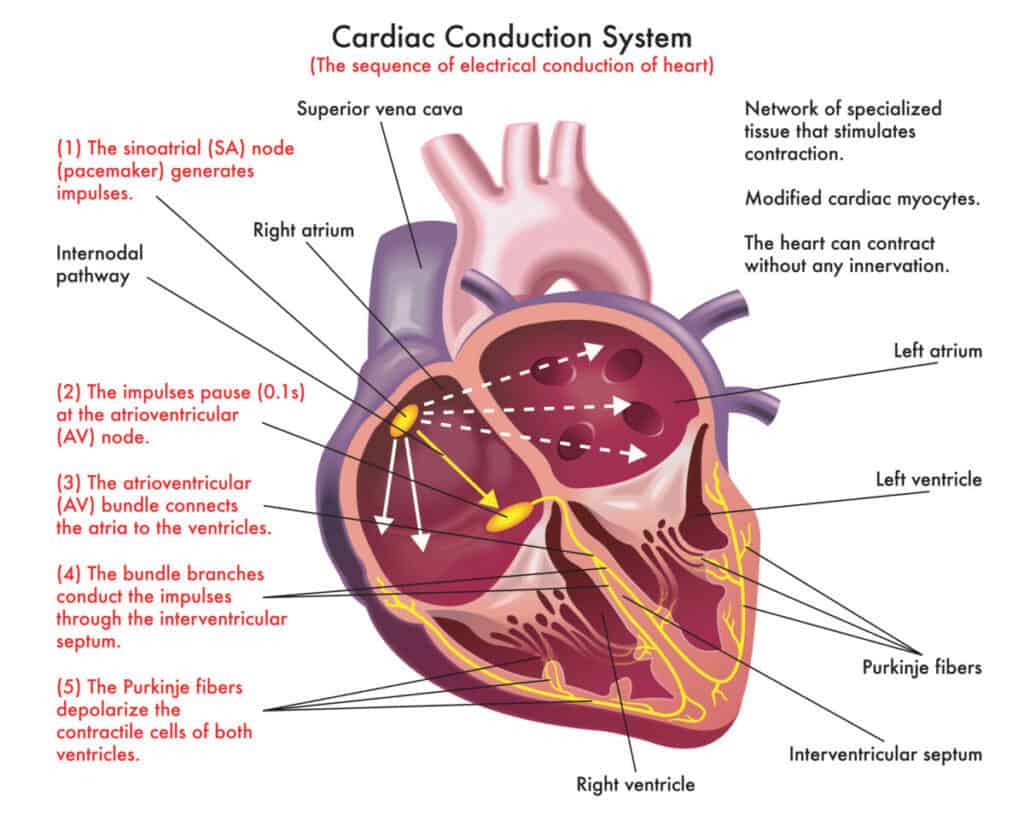
What is the order of transmission of the electrical impulses throughout the heart?
1) Sinoatrial (SA) Node: The pacemaker of the heart, located in the right atrium, generates an electrical impulse. (75 times/minute.)
depolarizes faster than the myocardium
intrinsic & extrinsic control (ANS)
2) Atrioventricular (AV) Node: The impulse reaches the AV node, where it is briefly delayed (0.1 second) to ensure the atria have fully contracted before the ventricles are stimulated. “electrical bridge”.
intrinsic & extrinsic control (ANS)
50 times/per minute
3) Atrioventricular (AV) bundle: Only electrical connection between the atria & ventricles
4) R & L bundle branches: two pathways in the interventricular septum that carry the impulses toward the apex of the heart
5) Purkinje fibers: complete the pathway into the apex & ventricular walls
AV bundle & Purkinje fibers depolarize only 30 times/minute in absence of AV
Ventricular myocardial contraction (systole)
sinus rhythm
determines heart rate
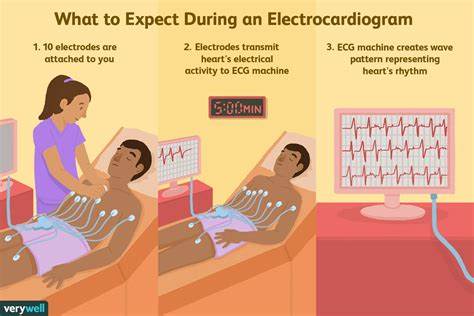
What does the electrocardiogram represent?
ECG or EKG is a composite of all the action potentials generated by nodal and contractile cells at a given time.
Monitors & amplifies
graphic record of heart activity
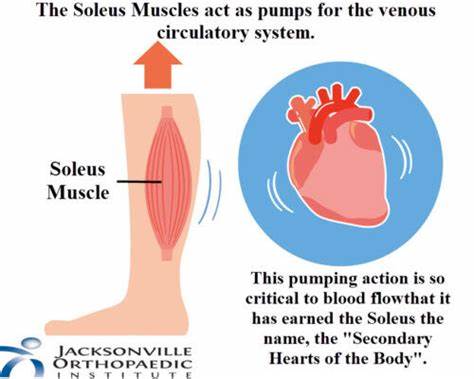
Understand the purpose of the venous valves and the skeletal muscle pump. What is the importance of this pump during exercise?
The purpose of the venous valves during exercise, is the contraction of the skeletal muscles compresses the veins, pushing blood towards the heart and increasing venous return; without it you’ll have a reduce in BP and CO.
The presence of one-way valves in veins prevents backflow of blood, ensuring that it moves efficiently towards the heart during the muscle pump action.
Understand the relationship between electrical activity, mechanical events, pressure changes, and blood flow in the heart.
depolarization causes systole (contraction), increase in pressure, increase in blood flow.
repolarization causes diastole (relaxation), decrease in pressure, decrease in blood flow.
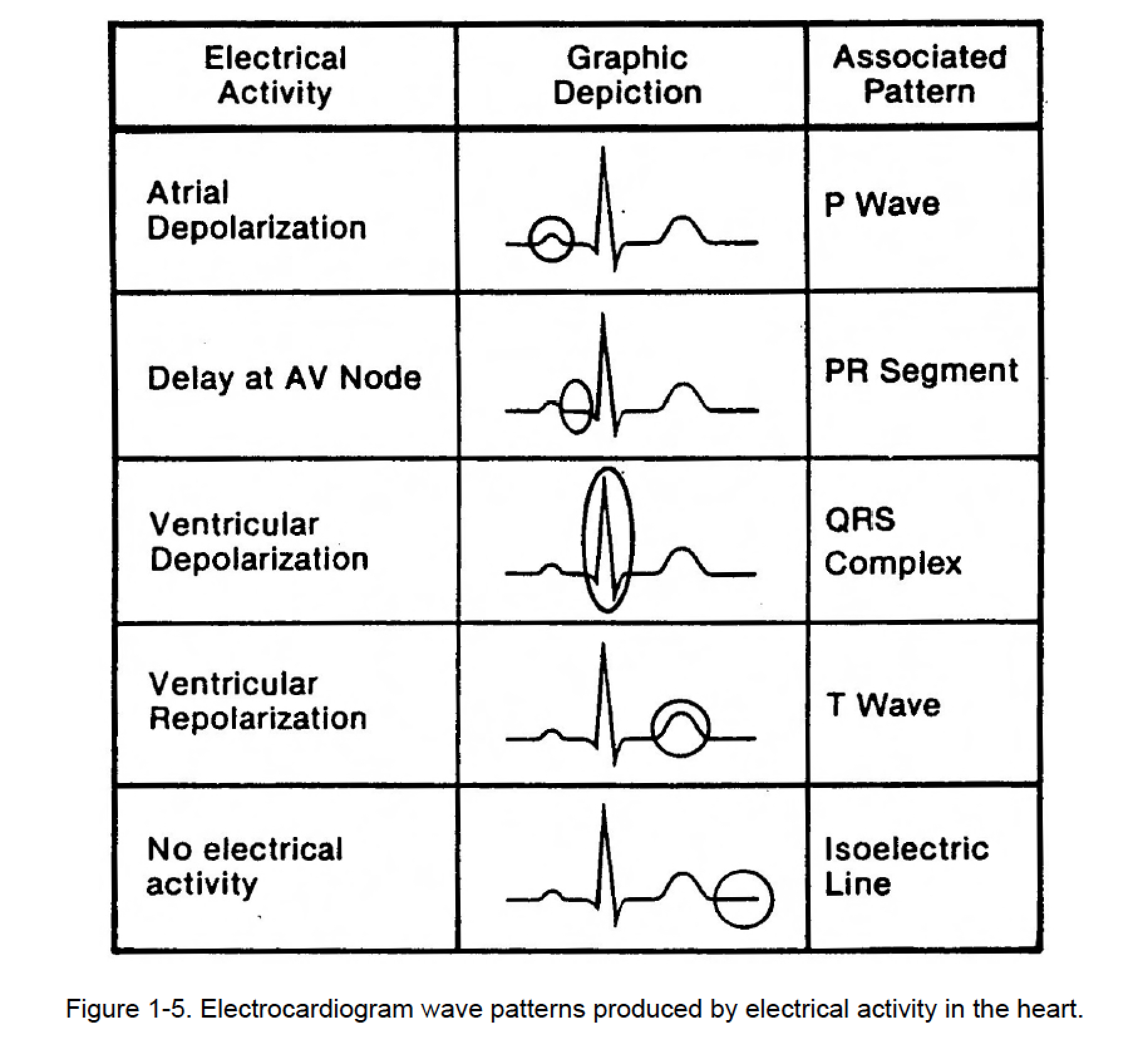
Identify the various components of waves of the ECG. Which are associated with atrial depolarization? Ventricular depolarization? Atrial repolarization? Ventricular repolarization?
P wave - Represents the contraction of the atria
Atrial depolarization, initiated by the SA node
QRS complex - Represents the contraction of ventricles.
Ventricular depolarization - beginning of systole; greater increase in ventricular pressure
isoventricular contraction - short phase; stays the same until ALL valves reopen
T wave - ventricular repolarization, passive filling, and isoventricular relaxation (relaxed) begins at the apex.
Relax to prepare for the next contraction.
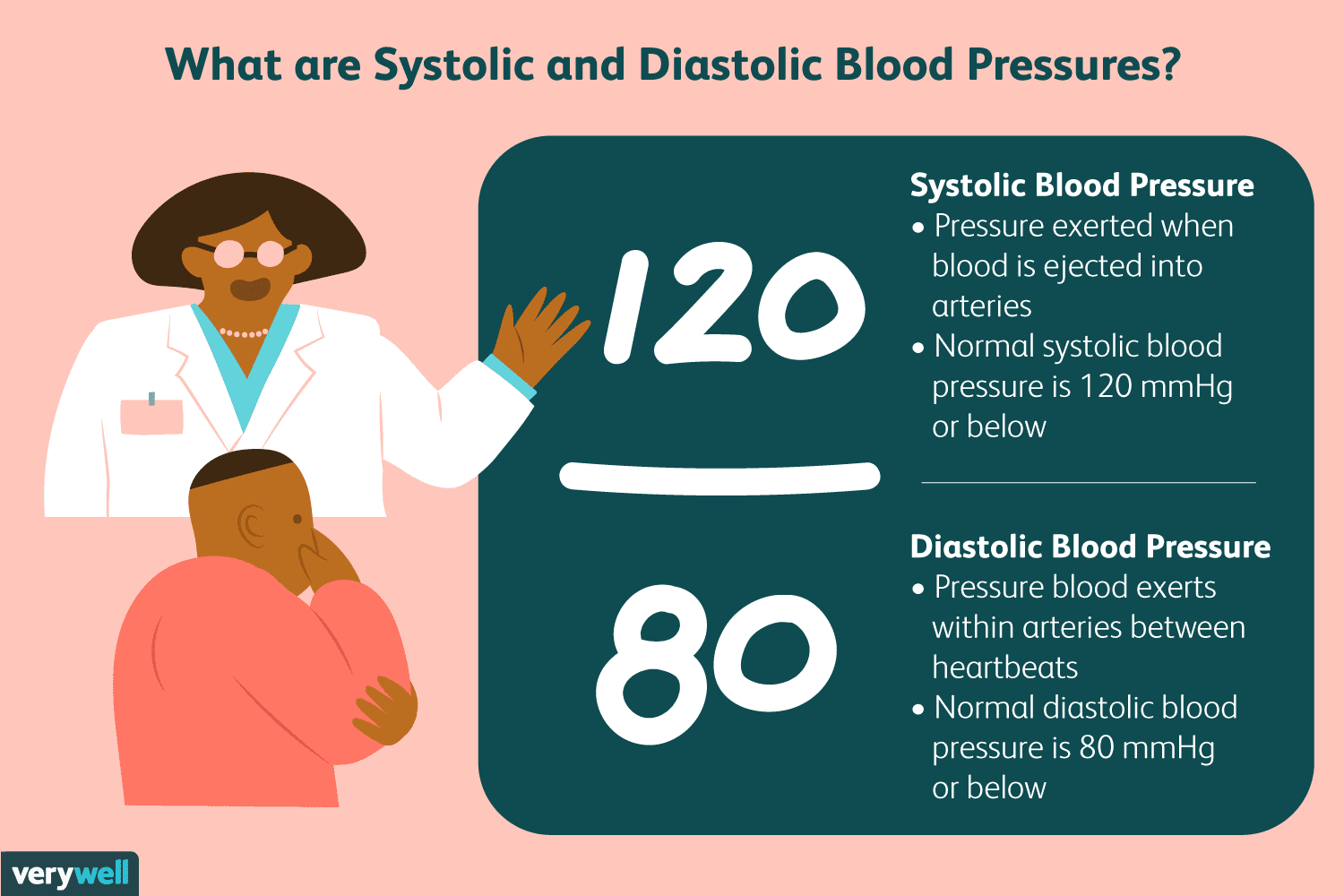
What is represented by systolic and diastolic blood pressure?
Systolic: This is the top number and represents the pressure in your arteries when your heart beats (contracts) and pumps blood. It’s like the peak pressure your heart generates.
Diastolic: This is the bottom number and represents the pressure in your arteries when your heart is resting between beats. It’s the lowest pressure your arteries experience.
What is hypertension?
also known as high blood pressure, is when the force of your blood against the walls of your arteries is consistently too high
How is venous pressure and venous blood flow maintained?
Veins can distend to hold a higher volume of blood, which helps maintain central venous pressure.
These valves ensure unidirectional blood flow, preventing backflow.
When muscles contract, they squeeze veins and help push blood back toward the heart.
This decreases venous compliance, increases central venous pressure, and promotes venous return by augmenting cardiac output.
How does walking or jogging after exercise aid circulation recovery?
it helps to enhance blood flow and helps with recovery
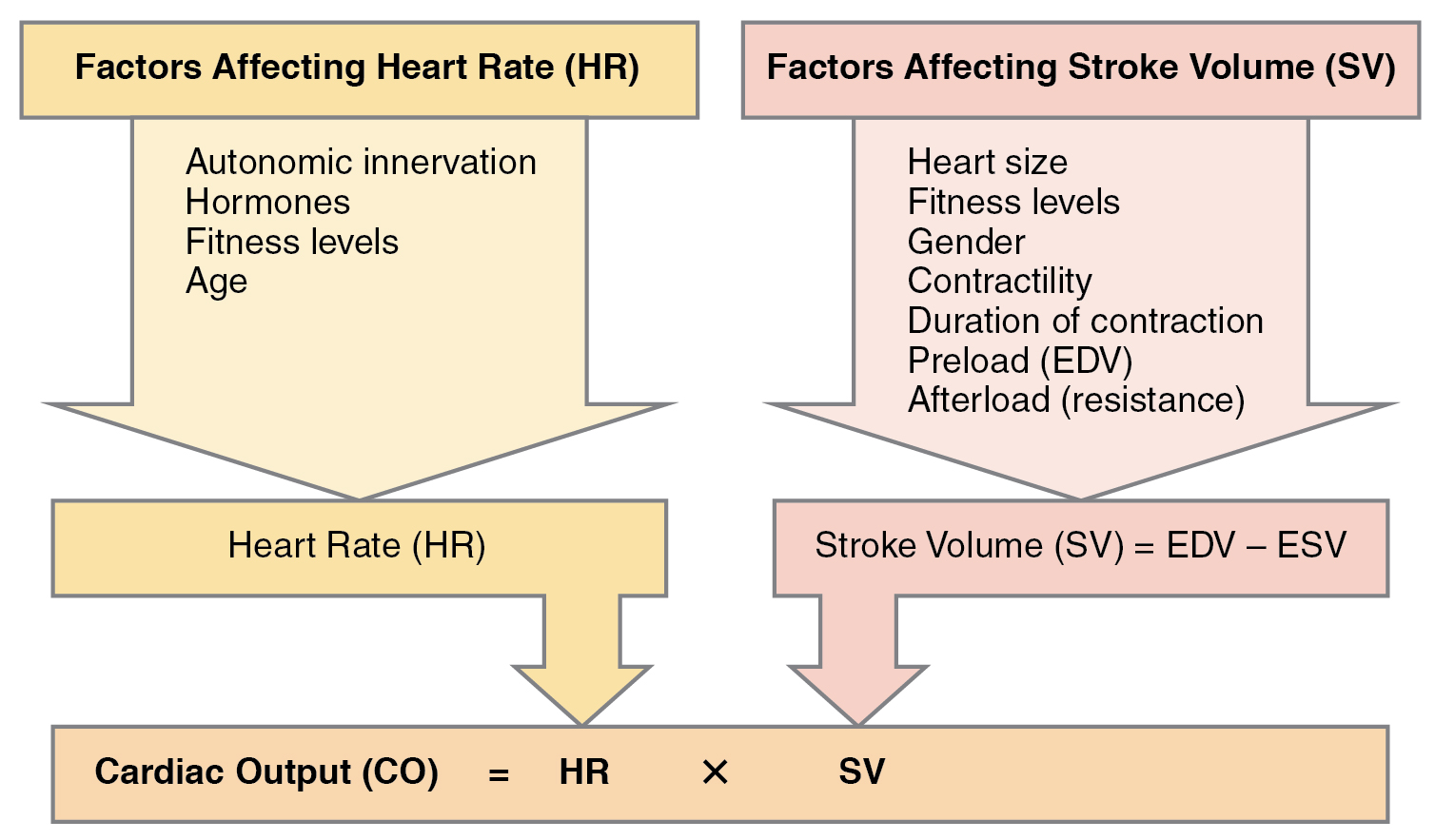
What is meant by cardiac output and what is its significance?
amount of blood pumped by each ventricle in one minute
CO = heart rate (HR) x Stroke volume (SV)
(L/min) or (ml/min) - (L/beat) or (ml/beat)
Essential for ensuring that tissues and organs receive enough oxygen and nutrients to meet the body's demands, especially during physical activity.
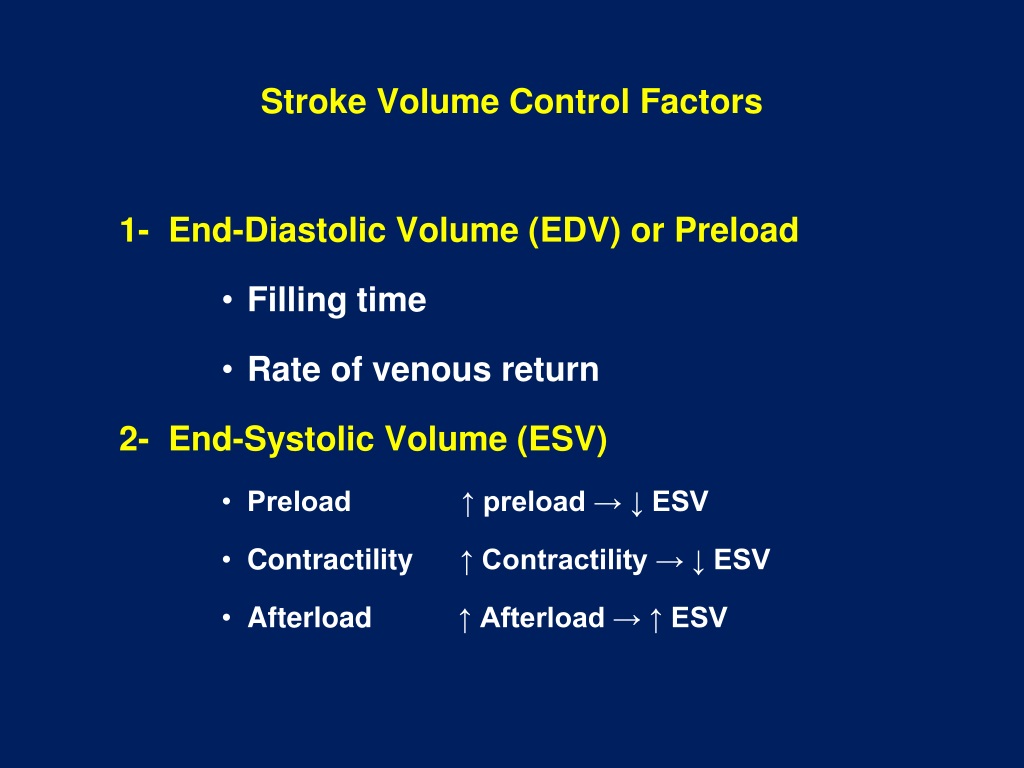
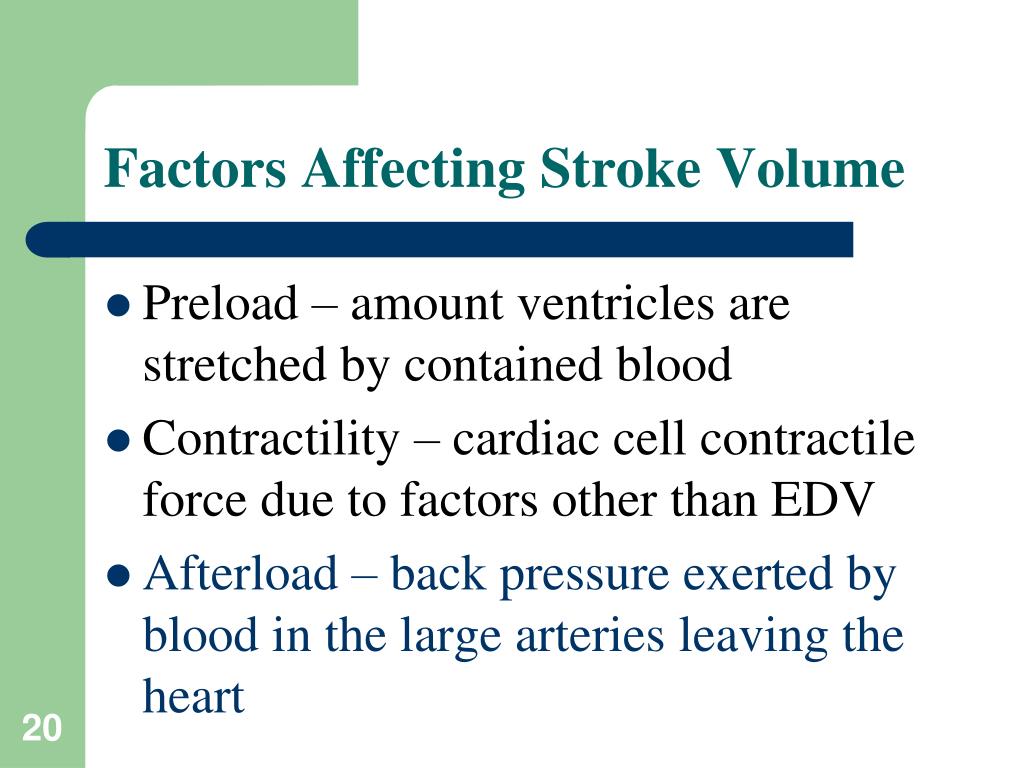
What are the factors that contribute to stroke volume?
Preload: degree of stretch of cardiac muscle cells before they contract (Frank-Starling law of the heart)
Increased venous return/volume = increased EDV = increased SV
decrease in ESV
Contractility: contractile strength at a given muscle length
Sympathetic stimulation increases contractility (ANS)
Independent of muscle stretch & EDV
Increased contractility = increased volume ejected = decrease ESV = increase SV
CONTRACTILITY affects ESV
Afterload: pressure that must be overcome for ventricles to eject blood
Hypertension increases afterload, resulting in increased ESV and reduced SV
Greater arterial pressure to overcome impacts amount of blood ejected
increased AFTERLOAD impacts increased ESV = decreased SV
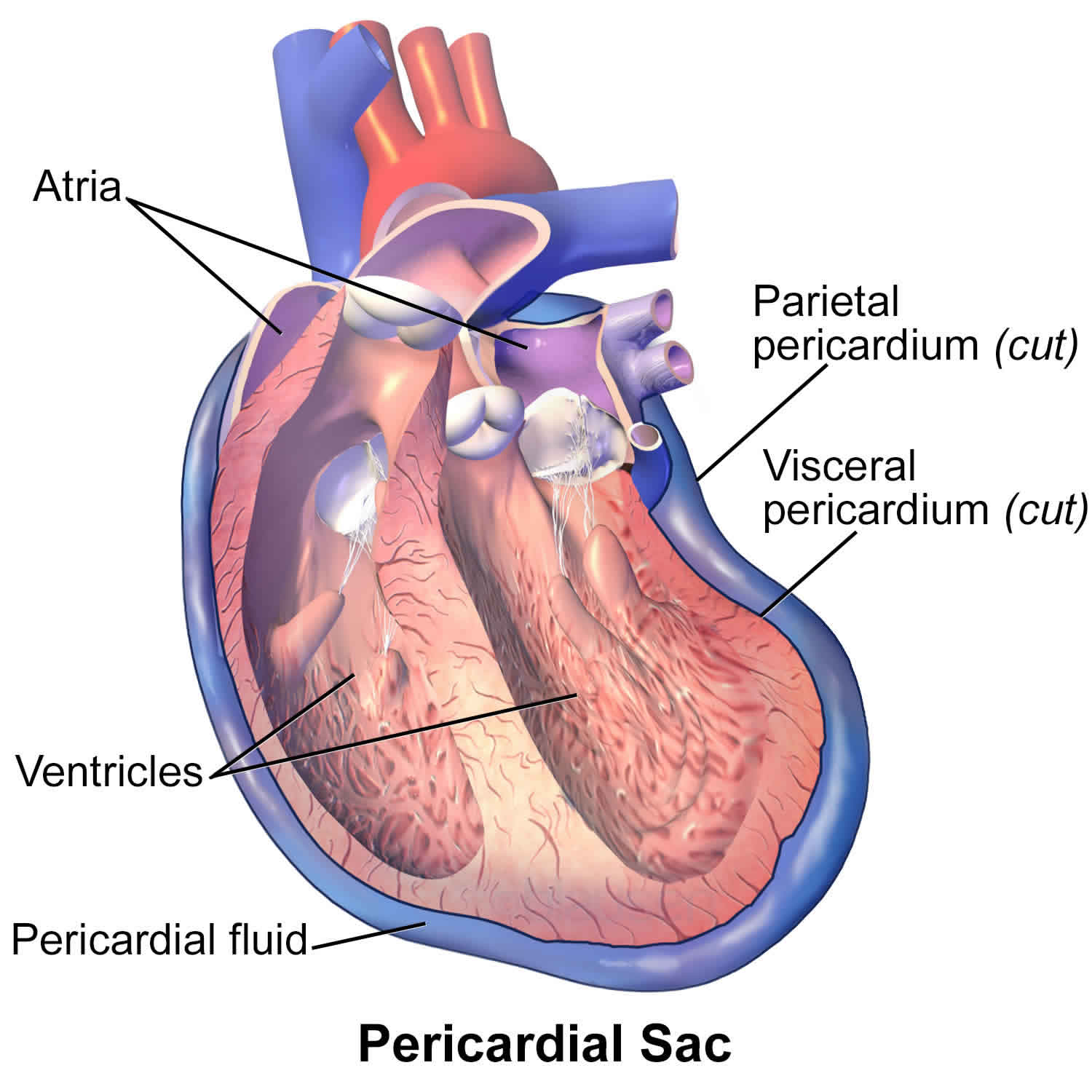
define parietal pericardium
is the outer layer of the pericardium, which is the sac that surrounds the heart.
It provides a protective layer and helps reduce friction between the heart and surrounding structures as the heart beats.
define heart wall
The heart wall, richly supplied with blood vessels, is composed of three layers: the epicardium, myocardium, and endocardium
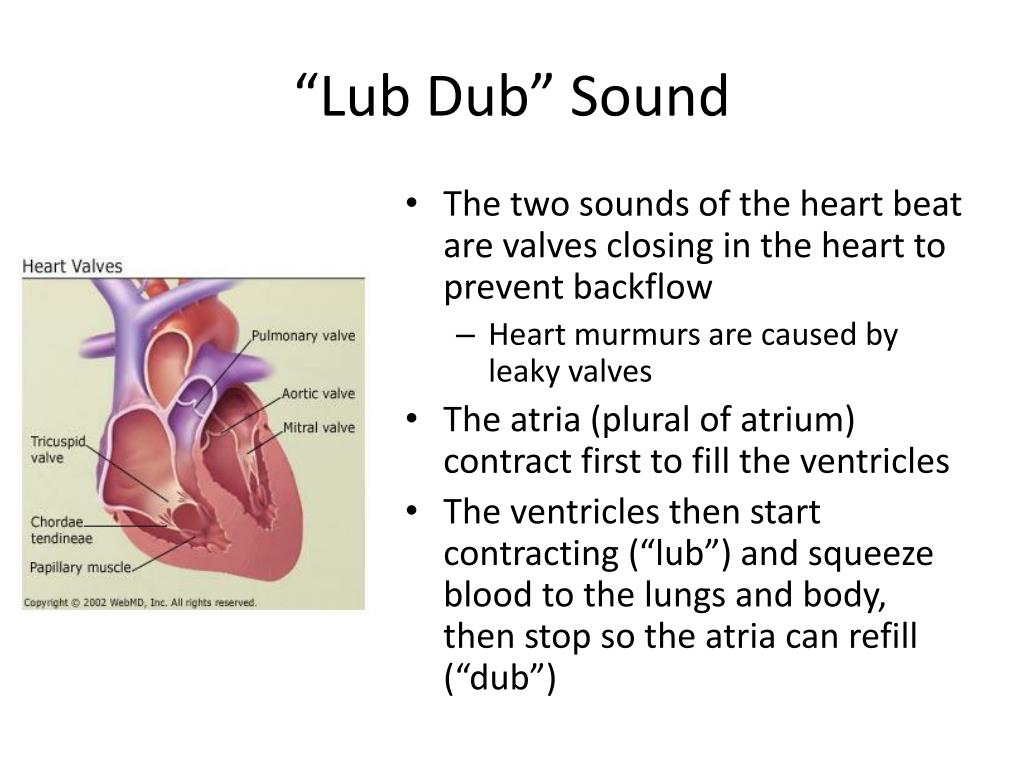
heart sounds lub-dup
sound is a classic “heartbeat”
AV (atrioventricular) and SL (semilunar) valves closing keeping everything in motion
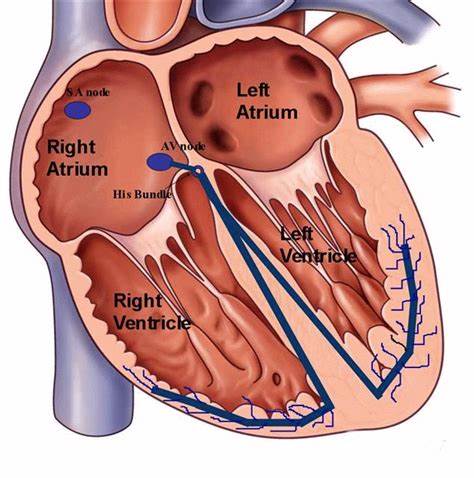
define sinoatrial node (SA)
The pacemaker of the heart, located in the right atrium, generates an electrical impulse. (75 times/minute.)
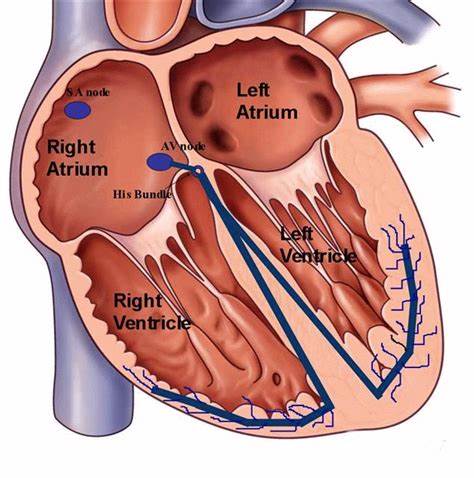
define atrioventricular node (AV)
The impulse reaches the AV node, where it is briefly delayed (0.1 second) to ensure the atria have fully contracted before the ventricles are stimulated. “electrical bridge”
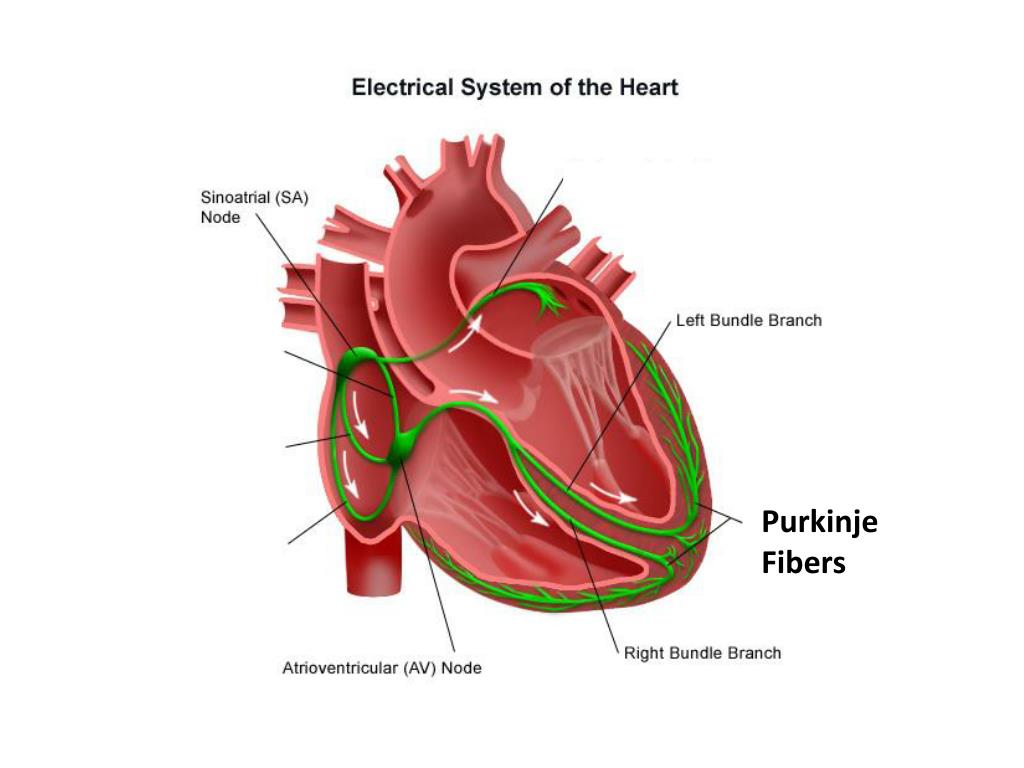
purkinje fibers
complete the pathway into the apex & ventricular walls
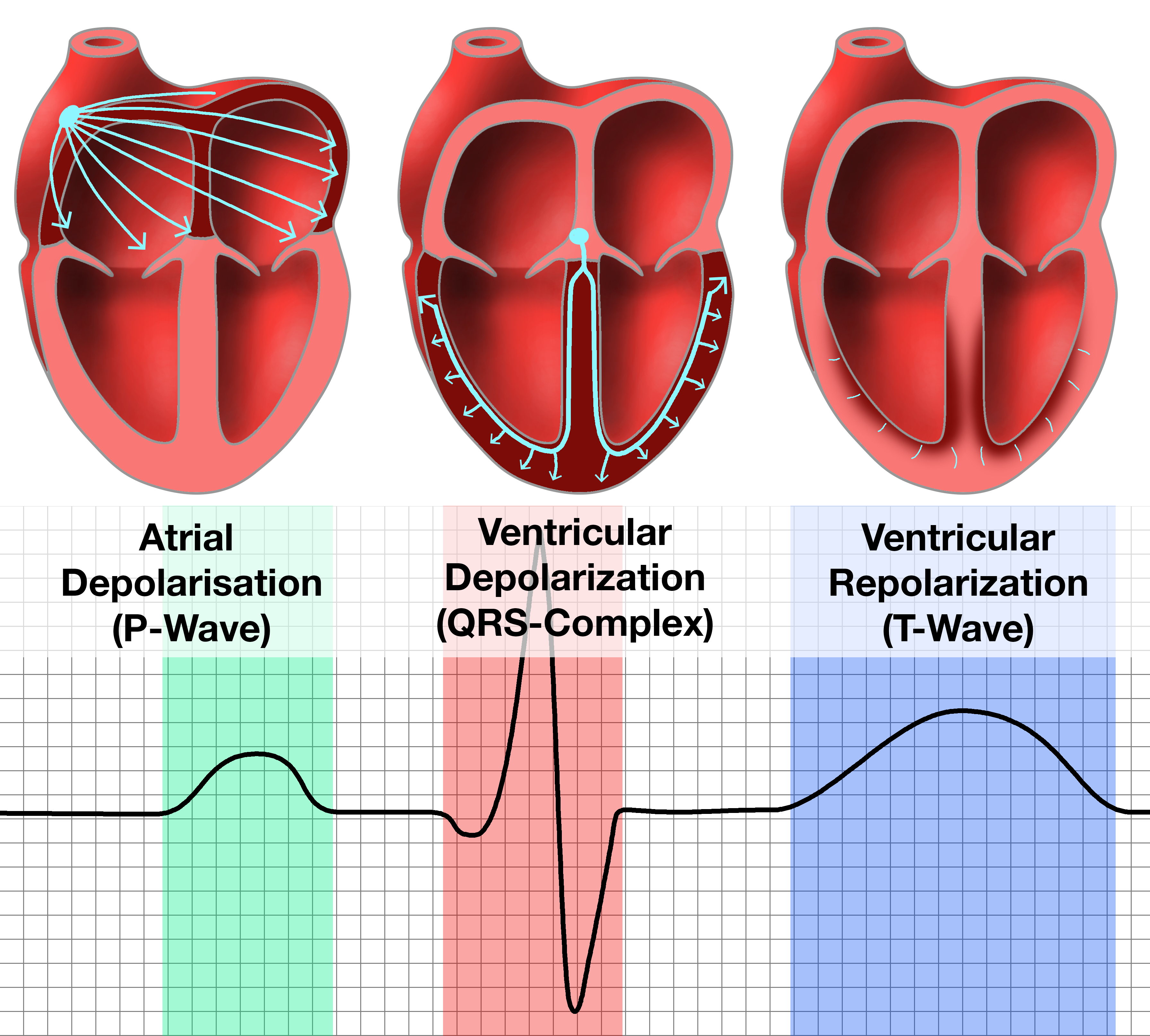
p wave
Time: 0.1 sec - 12.5%
Mechanical Activity: atrial depolarization (contracts), during ventricular relaxation (ventricular/active filling) initiates the SA node causing the P wave
Valve Position: AV valve (open), semilunar valve (closed)
Blood Flow: From the atria into the ventricles
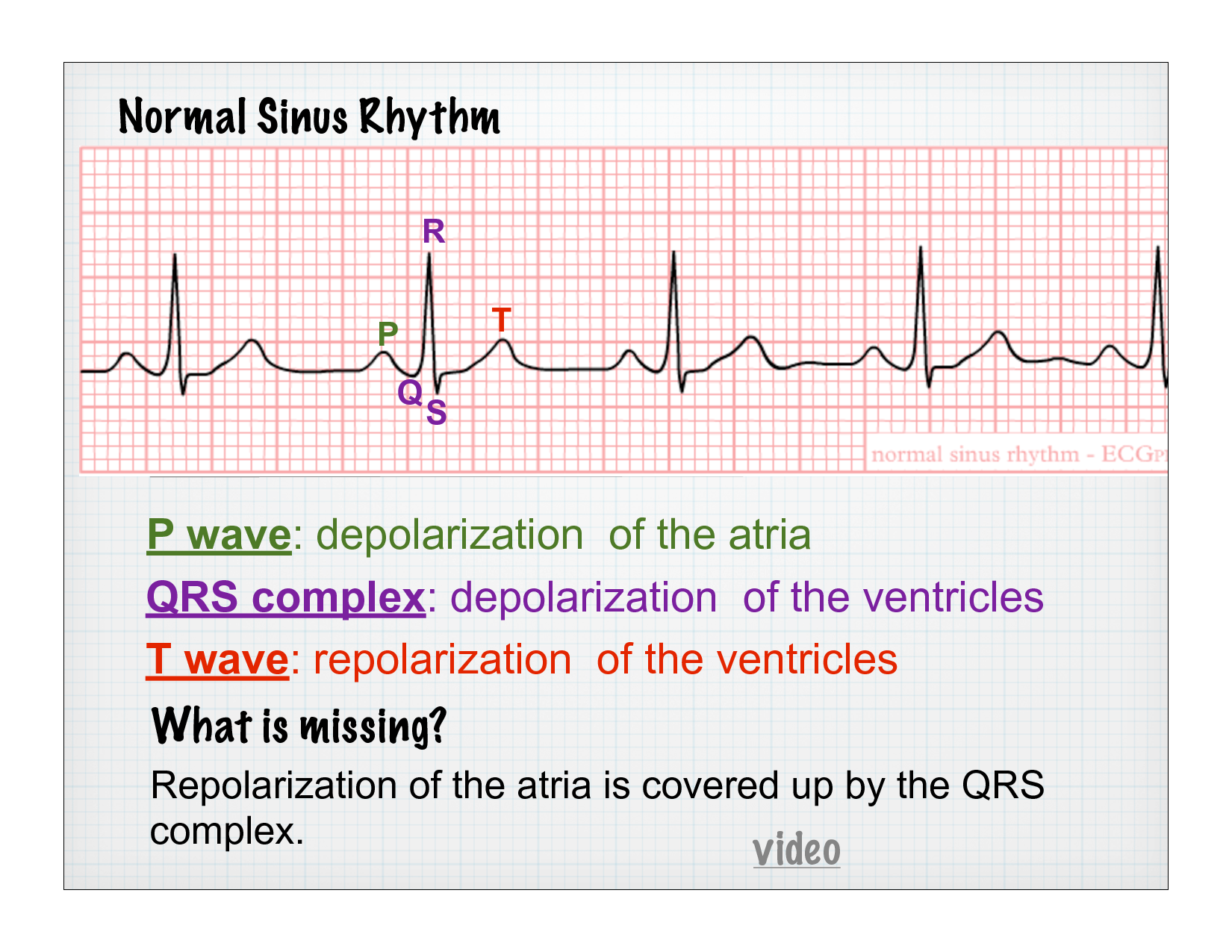
QRS complex
Time: 0.3 sec - 37.5%
Mechanical Activity: ventricles contract during atrial relaxation (ventricular ejection)
isovolumetric contraction
rapid ejection
reduced ejection
Valve Position: AV valve (closed), semilunar valve (open)
Blood Flow: From the ventricles into the arteries
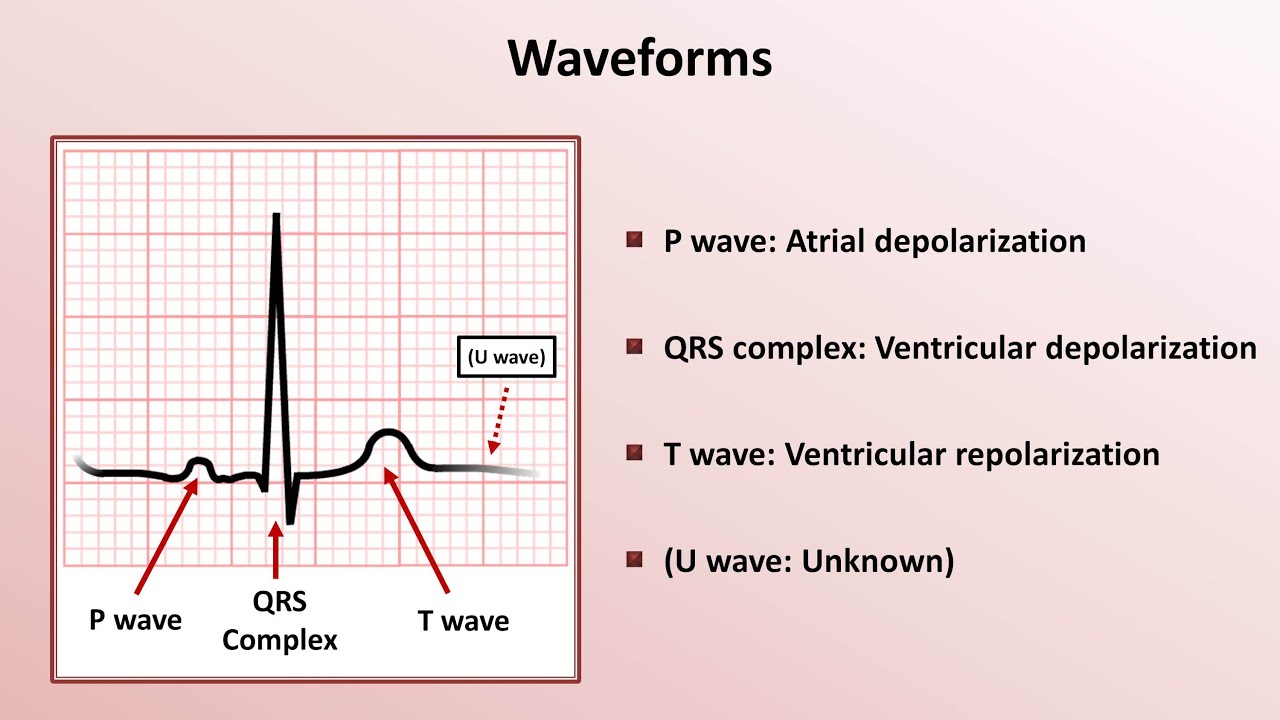
t wave
Time: 0.4 sec - 50%
Mechanical Activity: atrial & ventrical relaxation (ventricular filling)
isoventricular filling
isoventricular relaxation
passive filling
Valve Position: AV valve (open), semilunar valve (closed)
Blood Flow: from the veins → to the atria → ventricles