Non-Neoplastic salivary gland disease
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
What are the different types of salivary glands?
Major - parotid, submandibular, sublingual
Minor - found all around the mouth
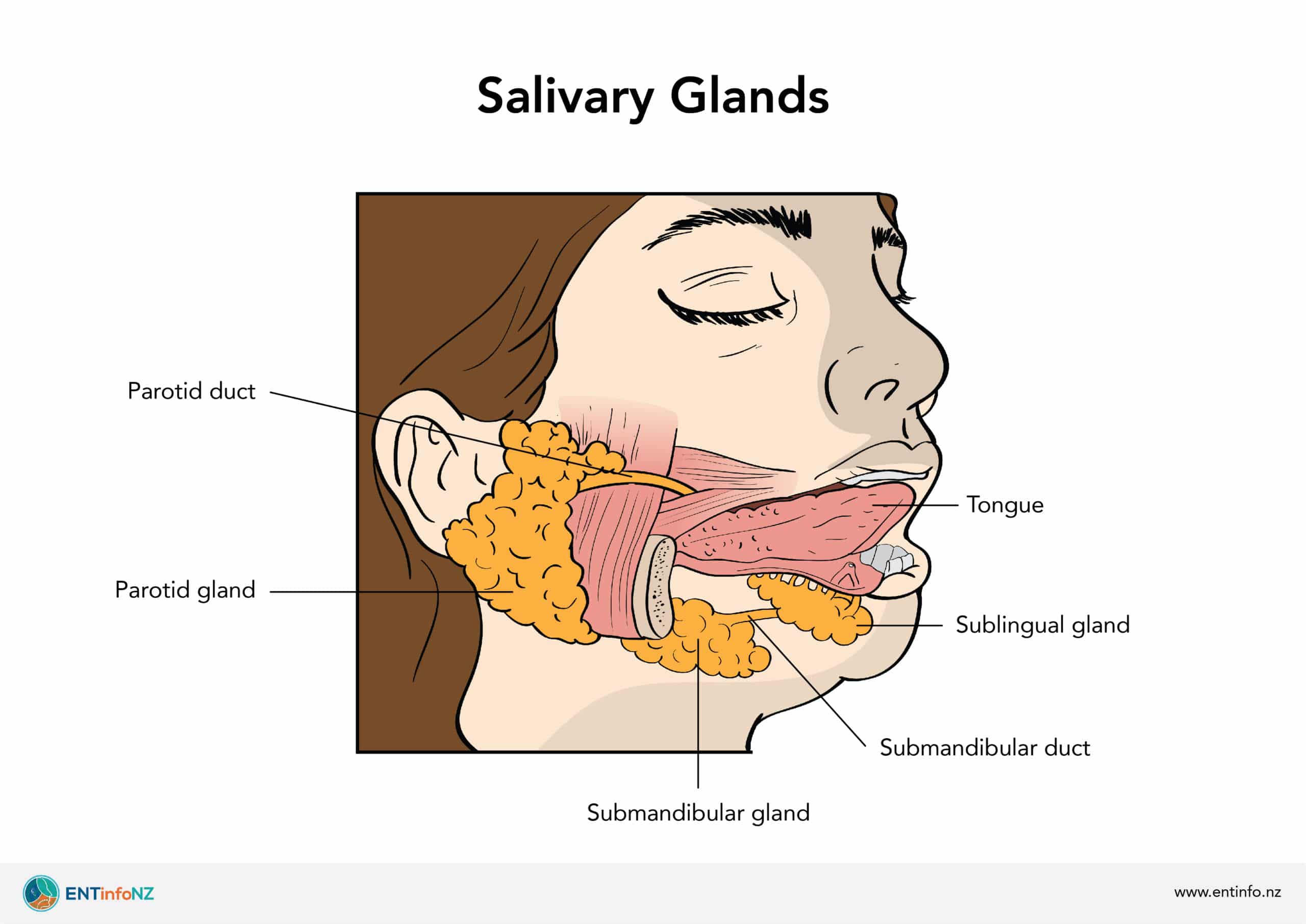
Where is the parotid gland? Does it produce serous or mucous secretion and how much % does it contribute to saliva?
Pre-auricular region (infront of ear)
Serous
20-40% saliva
Largest in size
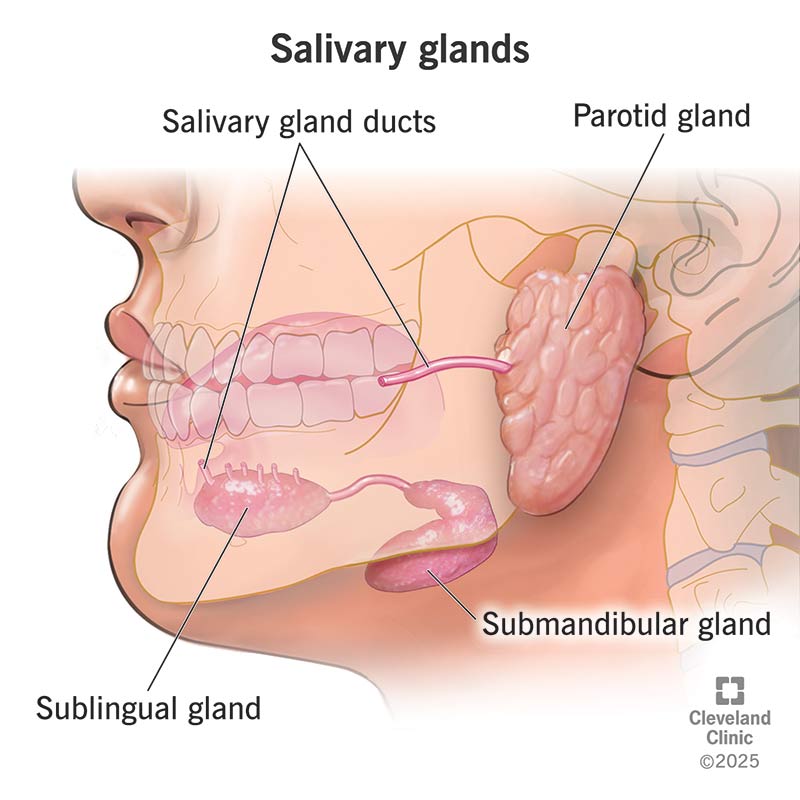
Where is the submandibular gland? Does it produce serous or mucous secretion and how much % does it contribute to saliva?
Just below mandible
Mixed - serous and mucous
60-70%
Where is the sublingual gland? Does it produce serous or mucous secretion and how much % does it contribute to saliva?
On FOM under tongue
Mucous
10% saliva
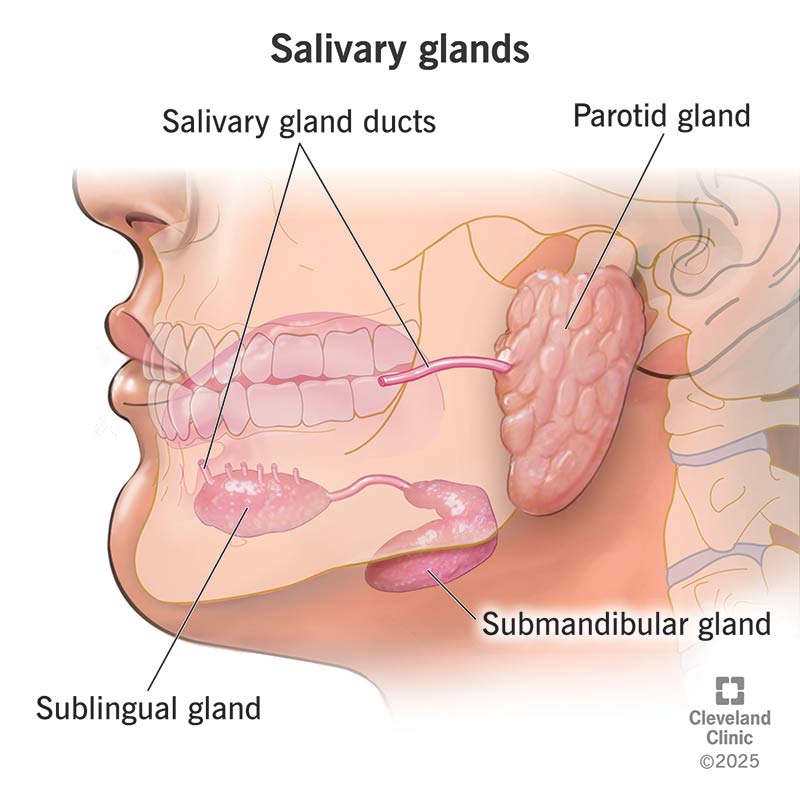
Where are the minor glands? Do they produce serous or mucous secretion and how much % do they contribute to saliva?
Lips, palate, cheeks, tongue (800+)
Mucous
5-10%
What are the categories of Non-Neoplastic Lesions of Salivary Glands?
Developmental Abnormalities
Inflammatory- Sialadenitis
Obstruction and Trauma
What Developmental Abnormalities are there of salivary glands?
Aplasia - complete absence of salivary tissue (associated with other syndromes)
Stafnes bone cavity AKA heterotopic (occurring in abnormal location) salivary tissue
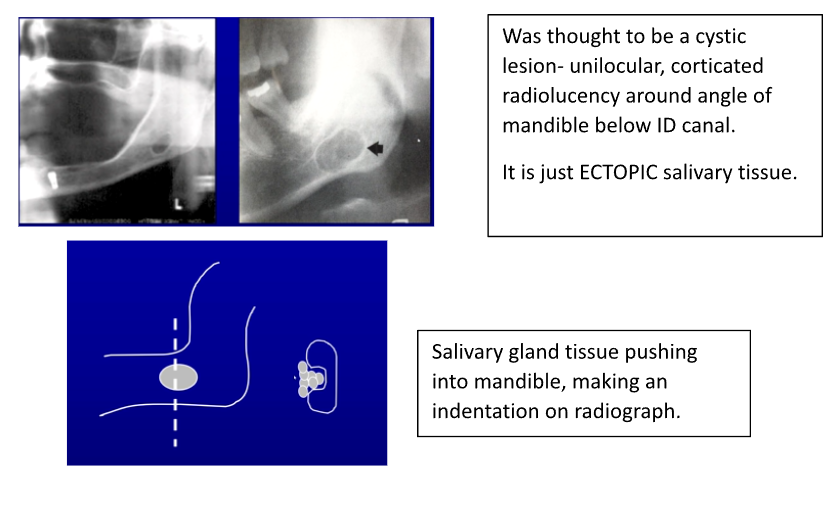
How does stafnes bone cavity appear on xray and what causes it to appear that way on xray?
Unilocular
Corticated
Around angle of mandible
BELOW ID canal
Its ectopic salivary gland tissue → pushes into mandible - causes indentation on radiograph
What forms can Sialodentitis occur in and what are they usually caused by?
Acute - bacterial or viral
Chronic - bacterial, post irradiation, sjogren’s syndrome
What is acute parotitis, what causes it, what are the symptoms and what is it secondary do?
Infection from mouth to parotid duct → then to gland
S.aureus causes it
Pain, swelling, pus in duct
Secondary to dry mouth → which is caused by radiotherapy, Sjogren, drug induced xerostomia
What is the cause of recurrent parotitis in adults?
Recurrent infection secondary to dry mouth → radiation, meds, sjogrens
40-60 yr olds
Unilateral
What is recurrent parotitis of childhood, what causes it?
repeated episodes of inflammation and swelling of the parotid gland in children,
No obvious cause or predisposing factors
May be evidence of infection - pain redness, fever
How does recurrent parotitis in children appear on sialogram and histology?
Punctate sialectasis → blotchy deposits (like Sjogren’s - loss of branching architecture)
Gradual destruction of acinar elements and reduced flow
Histology:
Dilation of salivary ducts with fibrosis around duct (salivary tissue replaced
Reduced salivary ducts where acini damaged
Inflammation (;lymphocytes) extending into ducts

What does mumps cause( Paramyxovirus), what are the features of it?
Viral sailodentitis (epidemic parotitis)
Incubation period 2-3 weeks
Direct or droplet spread
Features
Bilateral parotid swelling
Painful, malaise, fever
May spread to other glands or organs
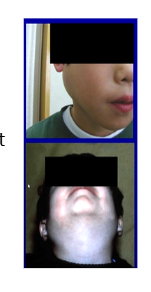
What are the complications of mumps in viral sialodentitis?
Orchitis (up to 30%)- inflammation of testes.
Meningitis (10%).
Oophoritis (5%)- inflammation of ovaries.
Pancreatitis (5%).
Cranial nerve palsies.
VIII nerve (Vestibulocochlear) deafness.
What are salivary calculi?
An accumulation of calcium and phosphate salts which deposit in the salivary ducts or gland.
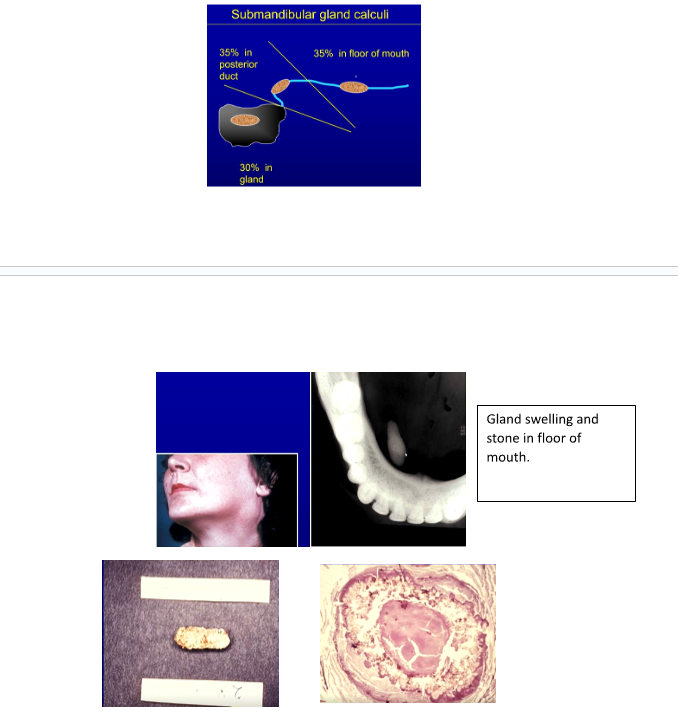
Which glands do salivary calculi commonly affect and why?
Submandibular gland ~80% of the time.
Parotid 20%.
Minor Glands 1-15%.
More in submandibular as its only gland pushing saliva against gravity → saliva pools. duct has bends in it
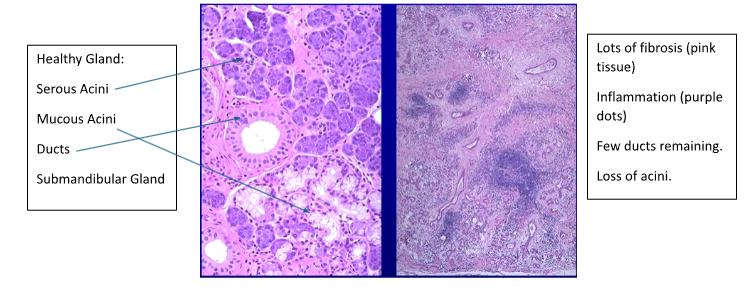
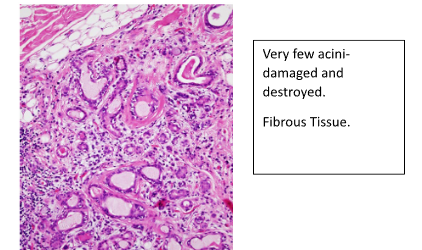
How do calculi cause disease?
Obstruction of duct → saliva retention and inflammation of gland
Swelling and fibrosis of gland → damage acini → reduce saliva production
Fibrosis → leads to irreversible loss of function
In radiation sialodentitis which acini are most sensitive?
Serous
Inflammation and fibrosis of glands → loss of function
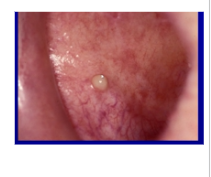
What are the 2 types of mucoceles?
Mucous extravasation cyst. (85%) → ruptured duct
Mucous retention cyst. (15%) → without rupture
Who do mucous extravasation cysts usually affect, where is it commonly affect and how do they occur?
Who→ younger age groups
Where → lower lip
Due to ruptured duct:
Blockage or trauma → rupture from build up of pressure → gland spills out into connective tissue forming cyst like lesion - lined by granulation tissue
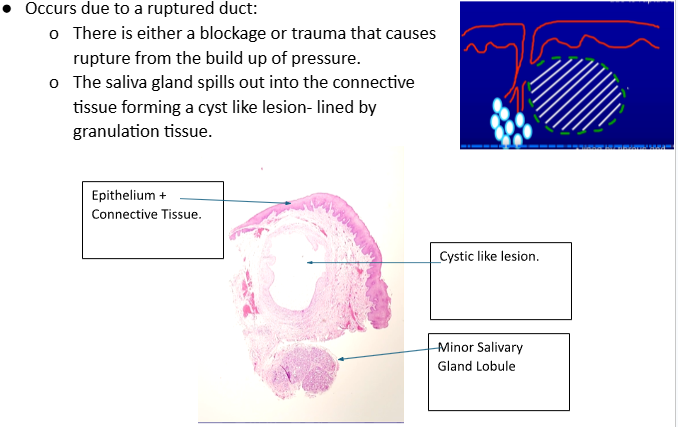
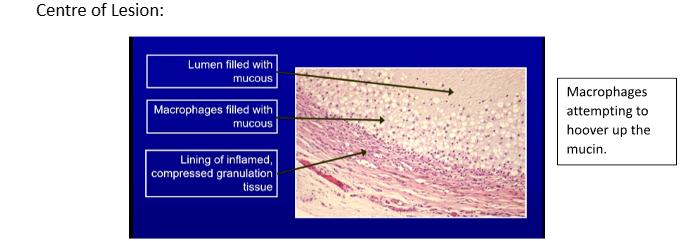
What does mucous extravasation cyst appear like in histology?
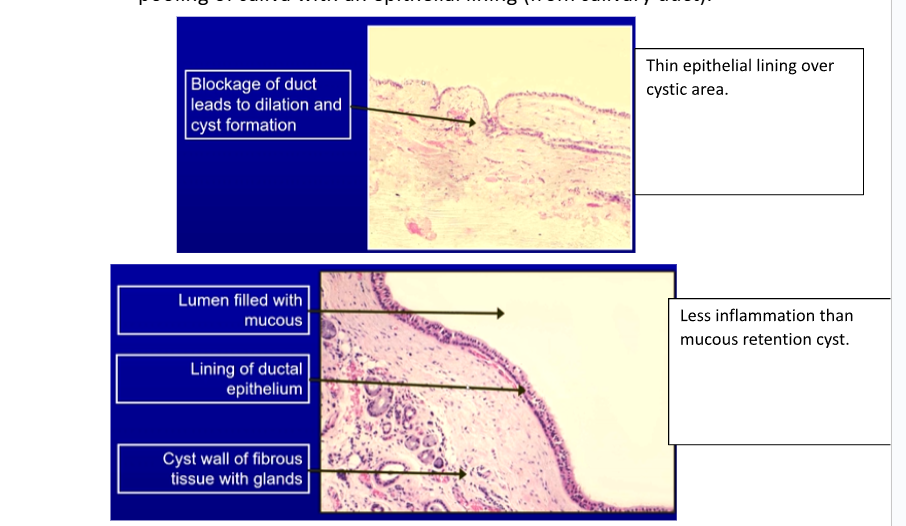
Who do mucous retention cysts usually affect, where is it commonly affect and how do they occur?
Who → older age groups 40+
Where → FOM, buccal mucosa
Blocked duct → no rupture → saliva produced → duct expands → pooling of saliva with epithelial lining from duct
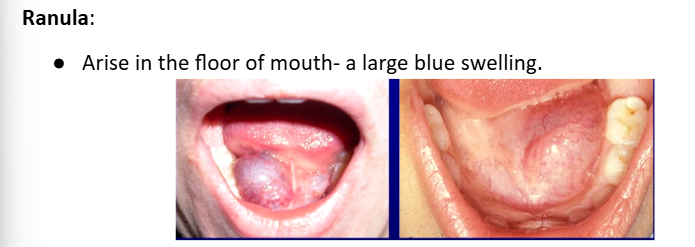
What is a ranula?
large blue painless swelling FOM usually in kids → may affect swallowing or airway concerns
usually extravasation cysts
from sublingual gland
2-3cm
rupture and recur
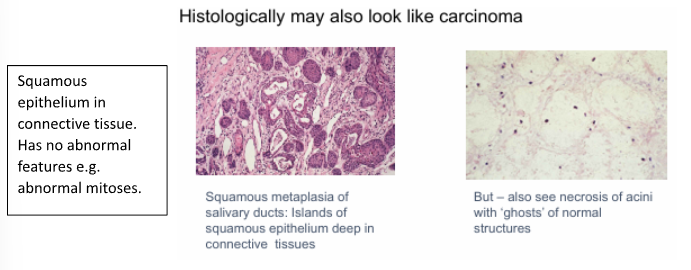
What is necrotising sialometaplasia?
Indurated (hard) and ulcerated swelling
Usually on palate
Benign inflammatory disease
Heals after 4-8 weeks
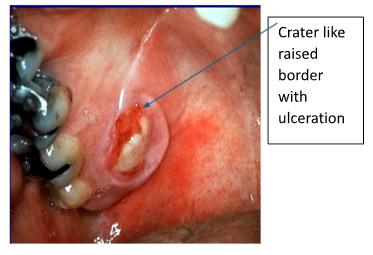
How does necrotising sialometaplasia appear?
Looks like carcinoma histologically
Islands of Squamous epithelium in connective tissue → no abnormal features e.g abnormal mitoses