Anatomy Lecture Exam 2 Ledogar
1/120
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
121 Terms
Ribs
How many and how do they differ?
>>True = 1-7 and they have their own costal cartilage that reaches the sternum.
>>False = 8-12 and they either have a costal cartilage that joins the cartilage of rib 7 or their cartilage doesn't reach the sternum at all in the case of the last two.
>>We can call the ones that don't reach the sternum floating ribs (ribs 11-2)
transversus thoracis function and innervation
Function: depresses ribs
Innervated at the intercostal nerves
Describe articulations between ribs and vertebrae + ribs and sternum.
A rib tubercle articulates with a costal facet of a transverse process, while the rib head articulates with the costal demifacets of two adjacent vertebrae. These are both synovial. Between the ribs and sternum we also mainly have synovial joints.
Diaphragm
Function: Upon inhalation, the diaphragm contracts and flattens and the chest cavity enlarges. This contraction creates a vacuum, which pulls air into the lungs. Upon exhalation, the diaphragm relaxes and returns to its domelike shape, and air is forced out of the lungs.
Innervated by the phrenic nerve
Lungs difference, function, and innervation
What are involved with lungs?
-There are 10 segments per lung (names aren't important)
Differences of the lungs: 3 lobes on right lung (Horizontal AND oblique fissures); Left lung is slightly smaller with two lobes to accommodate the heart. ("Cardiac notch")
Function: When you inhale (breathe in), air enters your lungs, and oxygen from that air moves to your blood. At the same time, carbon dioxide, a waste gas, moves from your blood to the lungs and is exhaled (breathed out).
Innervation: phrenic nerve
Conducting portion: Bronchi, Bronchioles, Terminal bronchioles.
Respiratory portion: Respiratory bronchioles and Alveoli
Trachea and Bronchioles
Trachea contains hyaline cartilage
5in pipe anterior to esophagus
C-shaped rings of cartilage
Gapped by membrane and trachealis muscle (smooth)o Lined with ciliated epithelium and goblet cells
Carries air larynx→lungs
Bronchioles is made of only smooth muscle and can constrict/dilate in response to ANS.
Homeostasis of Blood pH
Homeostasis of Blood pH Respiratory system helps regulate blood pH
A pH of 7 is preferred
Acid-base balance
Two components: Respiratory (lungs) and Metabolic (kidneys)
Per lung, how many lobes, primary bronchi, secondary bronchi, tertiary bronchi
>>Right lung: 3 lobes, 1 primary, 3 secondary, 10 tertiary
>>Left lung: 2 lobes, 1 primary, 2 secondary, 10 tertiary
Which vessel(s) carries oxy-blood?
SVC, pulm trunk, pulm vein, pulm artery
>> Only the pulmonary veins
Inspiration..... which muscles contract, how do thoracic volume & intrapulmonary pressure change?
>>Diaphragm (innervated by phrenic nerve) and external intercostals (innervated by intercostal nerves) both contract. This increases thoracic volume and lowers the intrapulmonary pressure.
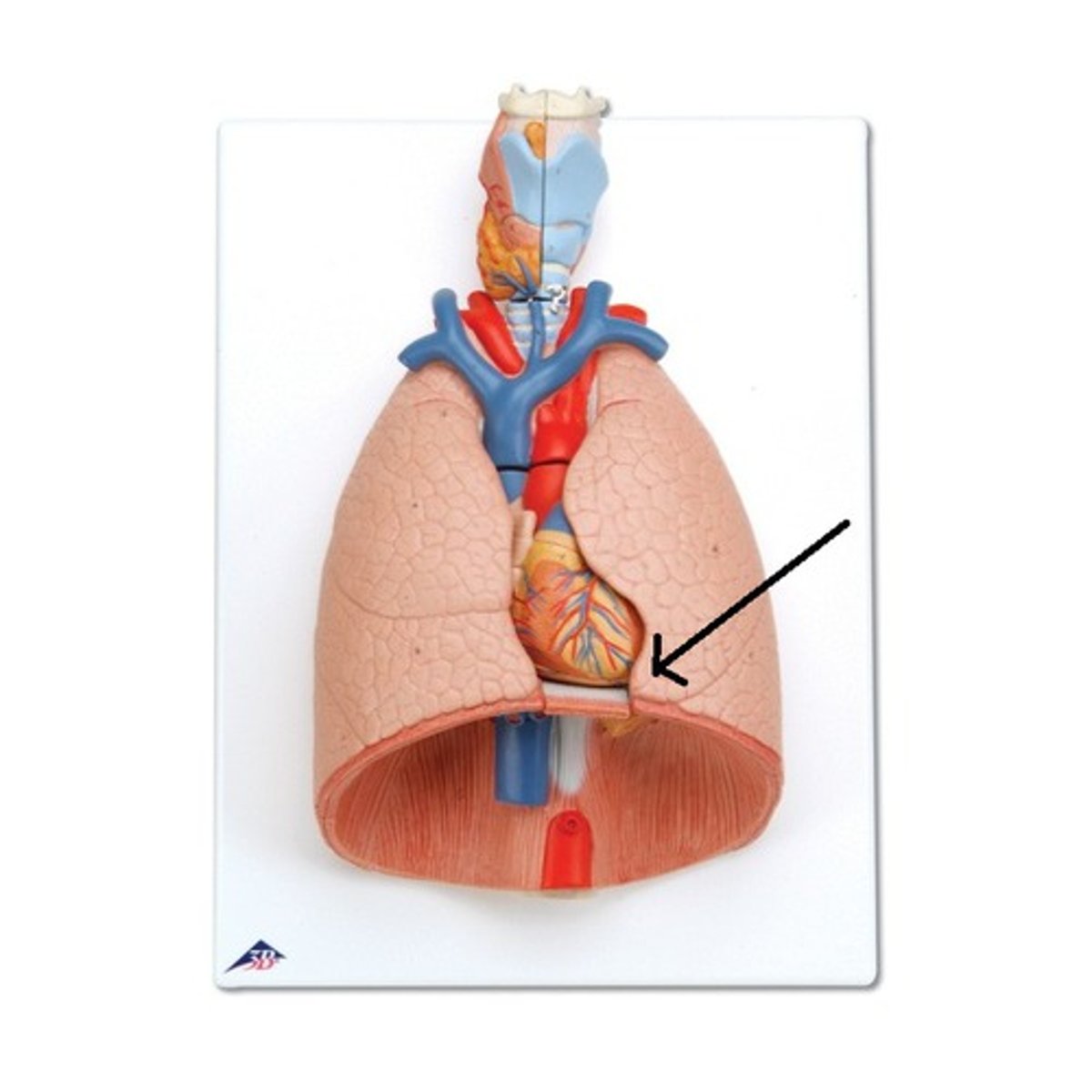
ID structure
Lingula (left lung)
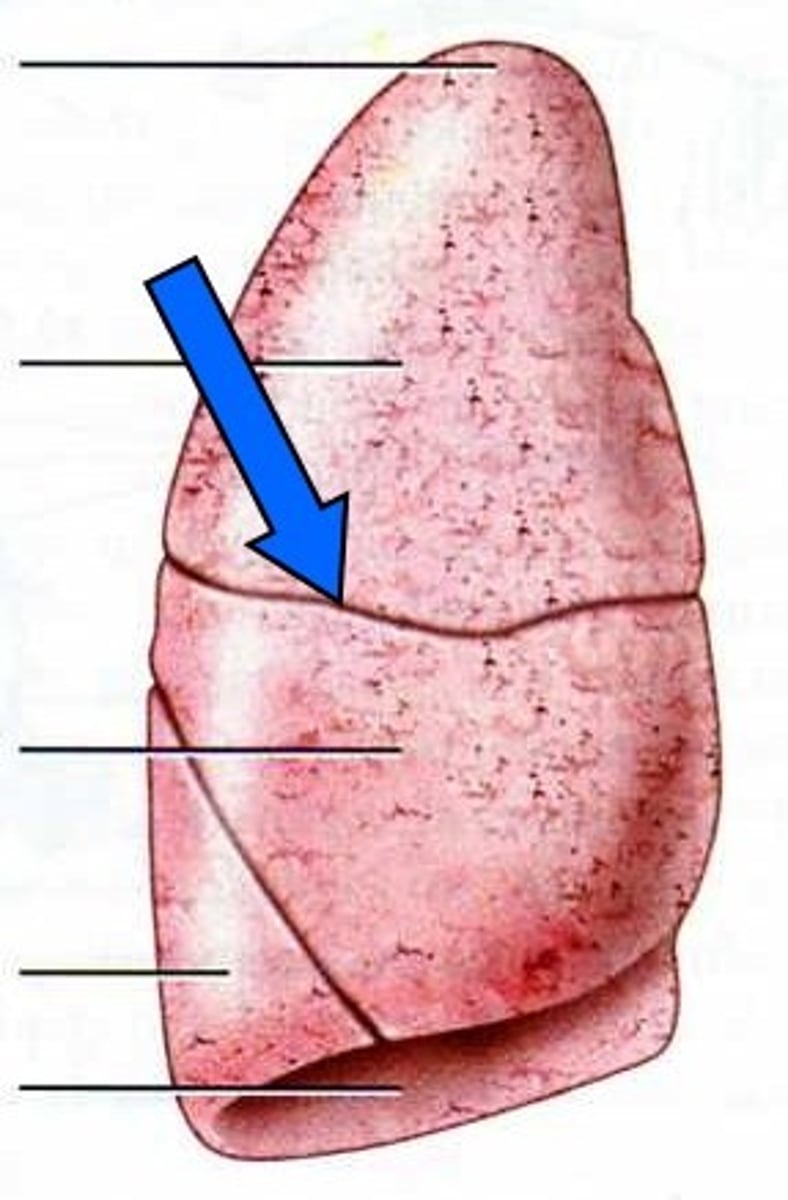
ID structure
Horizontal fissure (right lung)
Describe the structure of the rectus sheath above and below the arcuate
Above the Arcuate Line:
The rectus sheath above the arcuate line is formed by the aponeuroses of all three abdominal muscles: external oblique, internal oblique, and transversus abdominis.
The aponeuroses of the external oblique and the anterior lamina of the internal oblique muscle pass anteriorly to the rectus abdominis muscle and fuse together in the midline, forming the anterior layer of the rectus sheath.
-The aponeuroses of the posterior lamina of the internal oblique muscle and the transversus abdominis muscle pass posteriorly to the rectus abdominis and fuse together in the midline, forming the posterior layer of the rectus sheath.
-Therefore, above the arcuate line, the rectus sheath is composed of both anterior and posterior layers formed by the fusion of all three aponeuroses.
Below the Arcuate Line:
-Below the arcuate line, the rectus sheath undergoes a change in its structure. The aponeurosis of the external oblique muscle does not contribute to the rectus sheath below this line.
The rectus sheath below the arcuate line is formed by the aponeuroses of the internal oblique and transversus abdominis muscles only.
-The anterior layer of the rectus sheath is formed by the fusion of the anterior lamina of the internal oblique and the aponeurosis of the transversus abdominis muscles.
-The posterior layer of the rectus sheath is formed by the fusion of the posterior lamina of the internal oblique and the aponeurosis of the transversus abdominis muscles.
In summary, above the arcuate line, the rectus sheath consists of both anterior and posterior layers formed by the aponeuroses of all three lateral abdominal muscles. Below the arcuate line, the rectus sheath lacks the contribution of the aponeurosis of the external oblique muscle and is formed by the aponeuroses of the internal oblique and transversus abdominis muscles.
What are the superior, inferior, posterior, and anterolateral boundaries of the abdominal cavity?
Superior is formed by the diaphragm, separating the thoracic and abdominal cavities.
Posterior includes the lumbar vertebrae, erector spinae, and the psoas major and minor.
Inferior includes the bony pelvis, pelvic bones and structures such as the sacrum and coccyx.
Anterolateral is external and internal obliques, traversus abdominis, rectus abdominis, and linea alba.
Describe the actions and innervations of the skeletal muscles of the abdomen. Focus on diaphragm, quadratus lumborum, rectus abdominis, external oblique, internal oblique, and transversus abdominis.
1. Diaphragm:
- Action: The diaphragm is the primary muscle of respiration. It contracts and flattens during inhalation, increasing the volume of the thoracic cavity and causing air to be drawn into the lungs. During exhalation, it relaxes and returns to its dome-shaped resting position.
- Innervation: The diaphragm is innervated by the phrenic nerve, which arises from the spinal nerves C3, C4, and C5.
2. Quadratus Lumborum:
- Action: The quadratus lumborum muscle has multiple actions depending on the contraction of its different parts. It can laterally flex the trunk, extend the lumbar spine, and assist in elevating the hip.
- Innervation: The quadratus lumborum muscle is innervated by the branches of the lumbar spinal nerves, specifically from the ventral rami of T12-L4.
3. Rectus Abdominis:
- Action: The rectus abdominis muscle is responsible for flexing the trunk, as in performing a sit-up or crunch. It also contributes to compressing the abdominal contents during forced exhalation and stabilization of the trunk.
- Innervation: The rectus abdominis muscle is innervated by the lower intercostal nerves (T7-T12) and the first lumbar nerve (L1).
4. External Oblique:
- Action: The external oblique muscles on both sides, when contracting together, help flex the trunk forward and rotate it to the opposite side. When contracting individually, they assist in lateral flexion of the trunk.
- Innervation: The external oblique muscles are innervated by the lower intercostal nerves (T7-T12) and the iliohypogastric and ilioinguinal nerves (L1).
5. Internal Oblique:
- Action: The internal oblique muscles on both sides, when contracting together, assist in flexing the trunk forward and rotating it to the same side. When contracting individually, they aid in lateral flexion of the trunk.
The free edge of which abdominal muscle's aponeurosis forms the inguinal ligament?
the external oblique
Which layers of the abdominal wall contains the deep and superficial inguinal rings? What passes through these rings?
Deep: located in the transversalis ring
Super: Opening in the aponeurosis of the external oblique muscle
Spermatic cord [in males] and the round ligament of the uterus [in females]
The aponeurosis of which abdominal muscle forms the linea alba?
External oblique, internal oblique, and the transverse abdominis
Describe the primary functions of digestive system organs in the abdomen. Which components are involved in propulsion, chemical digestion, mechanical digestion, and absorption?
Propulsion: Swallowing [oropharynx], peristalsis[esophagus, stomach, small and large intestine]
Chemical digestion: Chemical breakdown of materials via acid and enzymes [stomach]
Mechanical: Chewing [mouth], churning [stomach], and segmentation [small intestines]
Absorption: Nutrients and water to blood vessels and lymph vessels [small intestine], water to blood vessels [large intestines]
Which components of the digestive system make up the gastrointestinal tract? Which make up the alimentary canal? Which are considered accessory digestive organs?
G.I: Esophagus, stomach, small and large intestines
-Stomach, Small and large intestines make the "gut"
Alimentary canal[digestive tract]: mouth ---) anus
Accessory organs: teeth, tongue, salivary glands, liver, pancreas, and gallbladder.
Which components of the GI tract contain skeletal/striated muscle and which contain smooth muscle?
Mouth and Pharynx: The muscles involved in chewing (mastication) and swallowing (deglutition) in the mouth and pharynx include both skeletal/striated muscles and smooth muscles. The voluntary muscles used in chewing are skeletal muscles, while the muscles involved in swallowing are a combination of skeletal and smooth muscles.
Esophagus: The esophagus is a muscular tube that connects the pharynx to the stomach. It contains a combination of skeletal and smooth muscles. The upper third of the esophagus has skeletal muscles, the middle third has a mix of skeletal and smooth muscles, and the lower third has predominantly smooth muscles.
Stomach: The stomach is primarily composed of smooth muscle. The smooth muscle layers in the stomach allow for mixing and churning of food, aiding in digestion.
Small Intestine: The small intestine includes the duodenum, jejunum, and ileum. The muscular layers of the small intestine contain smooth muscles. These muscles help to propel food through the digestive tract and assist in the absorption of nutrients.
Large Intestine (Colon): The colon, which includes the ascending, transverse, descending, and sigmoid colon, primarily consists of smooth muscle. However, it also contains some portions of skeletal muscle, particularly in the external anal sphincter, which allows for voluntary control over defecation.
Rectum and Anus: The rectum contains a combination of smooth and skeletal muscles. The inner circular smooth muscle layer helps with rectal continence, while the external anal sphincter is composed of skeletal muscles and allows for voluntary control over defecation.
Describe the 4 concentric layers of the GI tract. What function(s) does each serve? Which organs has 3 layers of muscularis externa rather than two?
>>Mucosa (innermost layer) = Epithelial lining that is responsible for secretion and absorption, has some lymphatics and a thin smooth muscle layer that forms rugae
>>Submucosa = Supports the mucosa via vessels and lymphatics
>>Muscularis externa = Thicker smooth muscle layer. All GI tract has longitudinal and circular fibers. The stomach has a third oblique layer.
>>Serosa (outermost layer) = Connective tissue & visceral peritoneum
Which abdominal organs are intraperitoneal and which are retroperitoneal?
Intraperitoneal (grows into sac): liver, spleen, most of the small intestines, transverse colon, sigmoid colon, ovaries, uterus [mostly].
Retroperitoneal (behind the sac): aorta, IVC, kidneys, ascending and descending colon, and part of rectum.
Describe the mesentries of intraperitoneal organs
Helps hold organs in place and allow passage of vessels and nerves.
Name three layers of heart wall and describe. Outermost has two names.
>>epicardium [visceral serous pericardium] = outer layer of adherent visceral serous pericardium
>>myocardium = cardiac muscle tissue
>>endocardium = inner layer of epithelial tissue that is continuous with the endothelium of great vessels
Trace blood entering the heart from vena cavae to the ascending aorta (name valves & major vessels along way)
vena cavae > R atrium > tricuspid valve > R ventricle > pulmonary semilunar valve > pulmonary trunk > pulmonary arteries > lungs > pulmonary veins > L atrium > bicuspid valve > L ventricle > aortic semilunar valve > aorta
Describe two structures that allow the fetal circulation to bypass the pulmonary circuit + name what they are called after they obliterate.
Foramen ovale allows blood to move from R atrium to L atrium (becomes fossa ovalis)
Ductus arteriosus allows blood to move from pulmonary trunk to aortic arch (becomes ligamentum arteriosum)
Trace path of an action potential from the heart's pacemaker to the ventricular walls. Name all the conducting tissues along the way.
SA node > atria (via junctional fibers) > AV node > AV bundle (of His) > R&L bundle branches > Purkinje fibers > ventricular walls
What is the structure and function of the pericardium?
The pericardium is a double-layered sac that surrounds and protects the heart. It consists of two main layers:
1. Fibrous Pericardium: The outer layer is called the fibrous pericardium, which is a tough, dense, and fibrous connective tissue layer. It is composed of collagen fibers and serves to anchor and protect the heart within the thoracic cavity. The fibrous pericardium is continuous with the central tendon of the diaphragm and the adventitia of the great vessels that enter and exit the heart.
2. Serous Pericardium: The inner layer of the pericardium is the serous pericardium, which consists of two sublayers:
a. Parietal Layer: The parietal layer lines the internal surface of the fibrous pericardium. It is a serous membrane composed of simple squamous epithelium and connective tissue. The parietal layer helps to hold the heart in place and provides a smooth surface for the movement of the heart within the pericardial cavity.
b. Visceral Layer (Epicardium): The visceral layer, also known as the epicardium, is the innermost layer of the serous pericardium. It is closely adhered to the surface of the heart, covering the external surface of the myocardium (the heart muscle). The visceral layer is also a serous membrane and is continuous with the parietal layer.
Between the parietal and visceral layers of the serous pericardium, there is a potential space called the pericardial cavity. This cavity contains a small amount of serous fluid, which acts as a lubricant, reducing friction between the layers as the heart beats and moves.
Functionally, the pericardium serves several important roles:
1. Protection: The fibrous pericardium provides structural support and protects the heart from external trauma and infection.
2. Anchorage: The fibrous pericardium anchors the heart within the thoracic cavity and limits its excessive movements.
3. Lubrication: The serous pericardium and the pericardial fluid reduce friction between the layers, allowing for smooth and frictionless movement of the heart during contractions.
4. Prevention of Overfilling: The pericardium helps prevent overdistension of the heart by limiting its expansion, thereby contributing to the regulation of cardiac output.
In summary, the pericardi
What is the path of the blood through the systemic circulation beginning at the left ventricle? [Be able to trace the general path of blood from the heart and back]
blood is pumped from the left ventricle into the aorta, which distributes oxygenated blood to the arteries. The arteries branch out into arterioles, which lead to capillary networks for the exchange of substances with tissues. Deoxygenated blood is collected by venules, which merge to form veins. The veins then return the blood to the heart, specifically the right atrium. From there, the blood is pumped to the lungs via the pulmonary artery, where it undergoes oxygenation. Oxygenated blood returns from the lungs via the pulmonary veins and enters the left atrium, before being pumped out of the heart again by the left ventricle.
How does the fetal circulation bypass [for the most part] the pulmonary circuit?
In fetal circulation, the developing fetus has a specialized circulatory system that allows it to bypass the pulmonary circuit for the most part since the lungs are not yet fully functional. The two main adaptations that enable this bypass are the presence of the ductus arteriosus and the foramen ovale.
1. Oxygenation in the Placenta: In fetal circulation, oxygen and nutrients are exchanged between the mother and fetus in the placenta. The placenta acts as the organ of gas exchange, supplying oxygen-rich blood to the fetus.
2. Oxygenated Blood from the Placenta: Oxygenated blood from the placenta enters the fetus through the umbilical vein.
3. Bypassing the Liver: The blood from the umbilical vein partially bypasses the liver through a vessel called the ductus venosus. This allows oxygenated blood to reach the fetal heart more directly.
4. Entering the Right Atrium: Oxygenated blood enters the right atrium of the heart through the inferior vena cava, which carries blood from the lower body.
5. Foramen Ovale: Within the right atrium, there is a small opening called the foramen ovale. The foramen ovale allows blood to pass directly from the right atrium to the left atrium, bypassing the right ventricle. This is possible due to the higher pressure in the right atrium compared to the left atrium.
6. Entering the Left Ventricle: From the left atrium, oxygenated blood flows into the left ventricle.
7. Pumping to the Body: The left ventricle then contracts, pumping oxygenated blood into the aorta, the main artery of the systemic circulation. Oxygenated blood is distributed to the body, supplying oxygen and nutrients to the developing tissues and organs.
8. Bypassing the Lungs: To bypass the lungs, a fetal blood vessel called the ductus arteriosus connects the pulmonary artery (which carries blood to the lungs) with the aorta (which carries blood to the body). This allows a significant portion of the oxygenated blood to flow directly from the right ventricle to the aorta, bypassing the lungs.
9. Deoxygenated Blood Return: Deoxygenated blood, which has given up its oxygen to the fetal tissues, returns to the placenta through the umbilical arteries for reoxygenation.
After birth, the fetal circulation undergoes signi
Trace the path of depolarization stimulus from the SA node to the left and right ventricle
the depolarization stimulus originates at the SA node, passes through the AV node, bundle of His, bundle branches, and Purkinje fibers, leading to the contraction of the ventricles and the subsequent ejection of blood.
When do the AV and semilunar valves shut? What causes the first and second heart sounds?
The AV (atrioventricular) valves shut during systole, specifically during ventricular contraction, to prevent the backflow of blood into the atria. The semilunar valves shut during diastole, specifically during ventricular relaxation, to prevent the backflow of blood from the arteries into the ventricles.
First Heart Sound (S1): The first heart sound is caused by the closure of the AV valves (tricuspid and mitral valves) during ventricular contraction. This sound is often described as "lub" and marks the beginning of systole.
Second Heart Sound (S2): The second heart sound is caused by the closure of the semilunar valves (pulmonary and aortic valves) during ventricular relaxation. This sound is often described as "dub" and marks the beginning of diastole.
In summary, the AV valves shut during ventricular contraction, causing the first heart sound (S1), while the semilunar valves shut during ventricular relaxation, causing the second heart sound (S2). These sounds help in assessing the normal functioning of the heart and provide important diagnostic information.
How do cardiac muscles differ from skeletal muscle cells?
Cardiac muscles differ from skeletal muscle cells in several ways:
1. Structure: Cardiac muscles are striated, like skeletal muscles, but they have smaller and branched cells connected through intercalated discs. These discs allow for coordinated contraction and electrical signaling between adjacent cardiac muscle cells. Skeletal muscle cells, on the other hand, are long and cylindrical with multiple nuclei.
2. Control: Cardiac muscles are under involuntary control, regulated by the autonomic nervous system. The heart's contraction is primarily controlled by the specialized cells of the conduction system, with the SA node acting as the natural pacemaker. In contrast, skeletal muscles are under voluntary control, allowing conscious movement.
3. Contraction Pattern: Cardiac muscles exhibit a rhythmic and continuous contraction pattern, allowing the heart to pump blood efficiently. Skeletal muscles, in contrast, contract in a more discrete and voluntary manner, providing movement and stability to the body.
4. Fatigue Resistance: Cardiac muscles have high fatigue resistance due to their continuous activity and reliance on aerobic metabolism. They are designed to contract continuously without tiring. Skeletal muscles, while capable of sustained activity, can experience fatigue over time due to their reliance on anaerobic metabolism and the buildup of metabolic byproducts.
5. Regeneration Capacity: Cardiac muscle cells have limited regenerative capacity. When damaged, they are typically replaced by scar tissue rather than new functional muscle cells. Skeletal muscle cells, on the other hand, have a greater ability to regenerate and repair themselves after injury.
How is the heart innervated by sympathetic and parasympathetic? What are the specific ANS effects?
The heart is innervated by both the sympathetic and parasympathetic divisions of the autonomic nervous system (ANS). Here's a summary of how these divisions innervate the heart and their specific effects:
1. Sympathetic Innervation: Sympathetic fibers originate from the thoracic region of the spinal cord (specifically, the sympathetic chain ganglia) and form a network of nerves that innervate the heart. Sympathetic stimulation increases heart rate and contractility.
- Sympathetic nerve endings release norepinephrine (noradrenaline) onto beta-1 adrenergic receptors in the heart.
- Activation of beta-1 adrenergic receptors leads to an increase in heart rate (positive chronotropic effect) and an increase in the force of contraction (positive inotropic effect).
- Sympathetic stimulation also causes coronary vasodilation, increasing blood flow to the heart muscle.
2. Parasympathetic Innervation: Parasympathetic fibers arise from the vagus nerve, specifically the nucleus ambiguus in the medulla oblongata. Parasympathetic stimulation decreases heart rate and has minimal effects on contractility.
- Parasympathetic nerve endings release acetylcholine onto muscarinic receptors in the heart, specifically M2 receptors.
- Activation of M2 receptors slows down the heart rate (negative chronotropic effect) by reducing the firing rate of the SA (sinoatrial) node, which serves as the natural pacemaker of the heart.
- Parasympathetic stimulation does not significantly affect contractility or coronary blood flow.
In summary, sympathetic innervation of the heart increases heart rate, contractility, and coronary blood flow through the release of norepinephrine onto beta-1 adrenergic receptors. Parasympathetic innervation, mediated by acetylcholine acting on M2 receptors, decreases heart rate by reducing the firing rate of the SA node. The balance between sympathetic and parasympathetic influences helps regulate heart rate and maintain cardiovascular homeostasis.
What are the primary functions of the lungs?
Transport Oxygen into blood supply and remove Carbon dioxide from body.
What are the components of the upper and lower respiratory tracts (airways)?
Upper airway
-Nasal cavity
-Oral cavity
-Pharynx
-Larynx
Lower airway
-Trachea
-Lungs
*Bronchi
*Bronchioles
*Alveoli
What are the components of the conduction portion and respiratory portion of the lungs?
Conducting portion
-Bronchi
-Bronchioles
-Terminal Bronchioles
Respiratory portion
-Respiratory Bronchioles
-Alveoli
How many bronchopulmonary segments per lung?
10 bronchopulmonary segments in the right lung (3 in superior lobe, 2 in middle lobe, 5 in inferior lobe)
9 segments on the left (4 in upper lobe, 5 in lower lobe).
Which components of the lungs contain hyaline cartilage?
Trachea and bronchi contain rings that allow them to move and flex when breathing.
Starting at the right atrium, what is the path of blood flow through the pulmonary circuit?
the path of blood flow through the pulmonary circuit involves the right atrium, tricuspid valve, right ventricle, pulmonary valve, pulmonary artery, pulmonary capillaries, pulmonary veins, and left atrium. This circuit allows for the oxygenation of blood in the lungs before it is returned to the heart for distribution to the rest of the body.
With respect to gas exchange, what occurs at the lung alveoli?
-Alveoli also work to remove viruses and irritants from respiratory system by sneezing, mucus, and coughing. "dust cells"
Simple squamous epithelium
Walls of capillaries &alveoli each 1 cell thick
Gas Exchange at the alveoli
-Oxygen ---) alveoli to blood
-Carbon dioxide ---) blood to alveoli
How is the pressure within the pleural cavity involved in respiration/ventilation?
The pleural cavity is a potential space that only contains serous fluid.
There is intrapleural pressure kept below atmospheric and intrapulmonary pressure in the pleural cavity.
Negative pressure and serous fluid helps keep the lungs adhered to thoracic wall [vital for normal ventilation]
Which skeletal muscles are involved in inspiration? Which are involved in expiration?
---Inspiration--
-Diaphragm and external intercostals contract [Thoracic volume increases]
-Lung volume increases, intrapulmonary pressure decreases [air in]
---Expiration---
-Internal and Innermost intercostal + transversus thoracis
-Muscle relaxation and elastic recoil of lungs [Thoracic volume decreases]
-Lung volume decreases, intrapulmonary pressure increases [air out]
How is the abdominal diaphragm innervated and what are the spinal levels?
The phrenic nerve originates at the C3 through C5 nerve roots, which exits the spinal canal at the neck root and descends caudally, parallel to the pericardial sac to provide the motor innervation to the diaphragm.
How are changes in intrapulmonary pressure involved in respiration/ventilation?
Pressure differences drive air flow in and out of the lungs.
Air will move from high to low pressure
Air enters the lungs when intrapulmonary pressure is less than atmospheric pressure
Air leaves the lungs when intrapulmonary pressure is greater than atmospheric pressure.
What is Boyle's law?
P1V1=P2V2
pressure and volume are inversely related
A change in lung volume --) changes in intrapulmonary pressure
What is a pneumothorax?
air in the pleural space
What factors contribute to the compliance of the lungs?
-The elasticity of the lung tissue
-The surface tension of alveoli
*Helps to collapse alveoli
How are the lungs innervated by sympathetics & parasympathetics? What are the specific ANS effects?
--------The Visceral efferent--------
-The Vagus nerve ( CN X) of the parasympathetic system innervates the lungs.
*Constricts bronchioles
-The parasympathetic system slows your breathing rate. It causes your bronchial tubes to narrow and the pulmonary blood vessels to widen.
-The sympathetic trunk innervates the lungs
*Dilates bronchioles
-The sympathetic system increases your breathing rate. It makes your bronchial tubes widen and the pulmonary blood vessels narrow.
-------The Visceral afferent [GVA]--------
-Info from receptors in lungs (e.g stretch)
How do ribs 1 & 2 differ from "typical" ribs?
Ribs 1 and 2, also known as the first and second ribs, differ from the rest of the ribs in several ways:
1. Shape and Size: Ribs 1 and 2 are shorter, flatter, and broader compared to the other ribs. They have a more curved shape and are wider at their attachment points to the vertebrae and sternum.
2. Articulation: Rib 1 has a unique articulation with the sternum. It attaches to the sternum at the sternoclavicular joint, forming the sternocostal joint. This joint allows for limited movement, providing stability to the thoracic cage.
3. Mobility: Ribs 1 and 2 have limited mobility compared to the other ribs. Their flatter shape and attachment to the sternum restrict their movement, which is important to protect and support vital structures in the thoracic cavity, such as the heart and lungs.
4. Muscle Attachment: Ribs 1 and 2 have specific muscle attachments that are not present in the other ribs. These muscles include the scalene muscles and the serratus anterior muscle. The scalene muscles are involved in neck movement and assist in elevating the first and second ribs during deep inhalation. The serratus anterior muscle helps stabilize and move the scapula (shoulder blade).
5. Function: Ribs 1 and 2 provide protection for essential structures in the thoracic cavity, including the heart, major blood vessels, and portions of the lungs. They also serve as attachment sites for muscles involved in respiration and upper limb movement.
Overall, the unique characteristics of ribs 1 and 2 allow them to provide stability, protection, and limited movement while supporting vital structures and facilitating respiration and upper limb function.
How do ribs and thoracic vertebrae articulate and what are the major structures involved? What type of joints are these and how do they facilitate respiratory movements of the thoracic skeleton?
Ribs and thoracic vertebrae articulate through a combination of joints, including the costovertebral joints and costotransverse joints. These joints play a crucial role in the movement and stability of the thoracic skeleton.
Costovertebral Joints:
Structure: The costovertebral joints are formed between the heads of the ribs and the corresponding vertebral bodies and intervertebral discs.
Joint Type: These joints are classified as synovial joints and specifically categorized as gliding joints.
Major Structures Involved: The articulating surfaces of the rib heads and the vertebral bodies are covered with hyaline cartilage. The joint cavity is lined with a synovial membrane, which secretes synovial fluid to lubricate the joint.
Function: The costovertebral joints allow for gliding and sliding movements, providing flexibility and stability between the ribs and the thoracic vertebrae. During respiratory movements, these joints facilitate the elevation and depression of the ribs, contributing to chest expansion during inhalation and contraction during exhalation.
Costotransverse Joints:
Structure: The costotransverse joints are formed between the tubercles of the ribs and the transverse processes of the corresponding thoracic vertebrae.
Joint Type: These joints are also classified as synovial joints, specifically categorized as plane joints.
Major Structures Involved: The articulating surfaces of the rib tubercles and the transverse processes are covered with hyaline cartilage, and a synovial membrane lines the joint cavity.
Function: The costotransverse joints allow for gliding movements between the ribs and the transverse processes of the vertebrae. These movements contribute to the biomechanics of the thoracic cage during respiratory activities, enabling the ribs to rotate and pivot, aiding in chest expansion and contraction.
Together, the costovertebral joints and costotransverse joints provide stability and flexibility to the thoracic skeleton. During respiration, these joints allow for the coordinated movement of the ribs, facilitating thoracic cage expansion during inhalation and contraction during exhalation.
What type of joints do we find between ribs and vertebrae? How do these facilitate respiratory movements of the thoracic skeleton?
-Sternocostal and Manubriosternal.[Synovial]
-The gliding movements facilitated by the costovertebral joints allow the ribs to articulate with the vertebrae, providing stability while still permitting the necessary range of motion for respiratory movements. The articulation between the ribs and vertebrae is crucial for the coordinated expansion and contraction of the thoracic cavity during breathing.
In summary, the costovertebral joints between the ribs and vertebrae are gliding joints that play a vital role in respiratory movements. They enable the ribs to elevate and expand during inhalation and lower during exhalation, contributing to the rhythmic expansion and contraction of the thoracic cavity needed for breathing.
What type of joint do we find between the different parts of the sternum?
Manubriosternal joint [symphysis]
What type of joint do we mostly find between the ribs and sternum?
Sternocostal joint [cartilage between first rib and sternum but the rest are synovial]
External intercostal
Internal intercostal
Innermost intercostal
Transversus thoracis
How do the these muscles function in respiration? How are they innervated?
During inhalation, the external intercostal muscles contract. These muscles are located on the outermost layer of the intercostal muscles, and their contraction helps elevate the ribcage. This action expands the thoracic cavity, creating a negative pressure that allows air to enter the lungs.
During forced exhalation, the internal intercostal and innermost intercostal muscles contract. These muscles are located on the inner layers of the intercostal muscles. Their contraction helps depress the ribcage, reducing the volume of the thoracic cavity and aiding in the expulsion of air from the lungs.
The transversus thoracis muscle, located on the inner surface of the anterior thoracic wall, also contributes to exhalation. Its contraction assists in depressing the ribs during forced exhalation, further reducing the volume of the thoracic cavity.
In terms of innervation, the intercostal muscles, including the external, internal, and innermost intercostal muscles, are innervated by the intercostal nerves. These nerves originate from the thoracic spinal nerves and run along the intercostal spaces, supplying motor signals to the intercostal muscles.
-The transversus thoracis muscle is innervated by branches of the anterior rami of the intercostal nerves.
Overall, these muscles function in respiration by coordinating the movements of the ribs, allowing for the expansion and contraction of the thoracic cavity during inhalation and exhalation. Their innervation by the intercostal nerves enables the transmission of motor signals to control their contraction and relaxation.
What vein do the hemiazygos and accessory hemiazygos veins drain into? Where does the azygos vein drain to?
The hemiazygos and accessory hemiazygos veins drain into the azygos vein, which in turn drains into the superior vena cava.
---Thoracic duct---
What portions of the body are drained by the thoracic duct?
What vessel does the thoracic duct drain into?
-The thoracic duct drains the lower extremities, pelvis, abdomen, left side of the thorax, left upper extremity, and left side of the head and neck.
-In most people, the thoracic duct drains into the subclavian vein on the left side.
What portions of the body are drained by the right lymphatic duct?
-The right lymphatic duct drains most of the right upper quadrant of the body, including the right upper trunk, right upper extremity, and right head and neck
Parietal pleura and visceral pleura
How does this bilayer form with lung development?
-Simple squamous epithelium
Parietal-layer lining body cavity wall
Visceral-layer adhered to organ
-Parietal and visceral pleura of the lungs form from somatopleuric and splanchnopleuric layers of mesoderm respectively during weeks 5 to 7
phrenic nerve
C3,4,5 (keeps the diaphragm alive)
---Thymus---
What happens here?
What are immunocompetence and thymic involution?
T cell education- Immature T cells mature into immunocompetent T cells
- Immunocompetence: ability to recognize foreign antigens Thymic Involution: Shrinking of thymus with age
What types of secretions are produced by the stomach?
Cephalic Phase: Vagus stimulation in response to sight, smell, and thought of food. Stomach secretes HCl and pepsinogen.
Gastric Phase: Stimulation by distension, change in pH, protein[increase in HCl which is mediated by a decrease in pH]
Intestinal Phase: Chyme enters small intestines, inhibits stomach, and simulates synthesis and release of pancreatic juice and bile.
Trace the path of food material from the esophagus to the anus. Include all major valves/sphincters.
[In order]
Esophagus
Lower Esophageal Sphincter
Stomach
Pyloric Sphincter
Small intestines
Ileocecal Valve
Large intestines [colon]
Rectum
Anal Sphincter
Anus
What kinds of secretions are received by the duodenum through the major duodenal papilla?
Pancreatic juice and bile
-Pancreatic juice [produced by pancreas] contains enzymes that aid in the digestion of carbohydrates, proteins, and fats.
-Bile [produced by the liver] and stored in the gallbladder, helps in the emulsification and absorption of fats. The combination of secretions play a crucial role in the digestion and absorption of nutrients in the duodenum.
Describe the functions of the plicae circularis, villi, and microvilli. How do they increase the surface area of the small intestine?
-Plicae circularis: increases the surface area by creating a larger inner surface for nutrient absorption and slow down the movement of chyme, allowing more time for absorption.
-Villi: amplify the absorptive surface area and facilitate the absorption of nutrients, such as carbohydrates, proteins, fats, and vitamins into the bloodstream.
-Microvilli: increase the surface area by providing additional microscopic projections and contain numerous enzyme and transport protein that facilitate final digestion.
How do the duodenum, jejunum, and ileum differ in their anatomy and function?
-Duodenum: The duodenum is the first and shortest part of the small intestine, located immediately after the stomach. It receives secretions from the liver (bile) and pancreas (pancreatic enzymes) through the major duodenal papilla. The primary function of the duodenum is to continue the digestion process by mixing chyme with digestive enzymes and absorbing nutrients.
-Jejunum: The jejunum is the middle section of the small intestine, following the duodenum. It is characterized by a thicker wall, larger and more numerous villi, and a rich blood supply. The jejunum is primarily responsible for the absorption of nutrients, including carbohydrates, proteins, and fats, into the bloodstream.
-Ileum: The ileum is the final and longest part of the small intestine, connecting to the large intestine. It has fewer and less prominent villi compared to the jejunum. The ileum plays a vital role in the absorption of bile salts, vitamin B12, and remaining nutrients, as well as the reabsorption of water and electrolytes.
Describe the function of peristalsis and segmentation. Which muscles are involved?
-Peristalsis: Peristalsis is a coordinated muscular contraction and relaxation that propels food along the gastrointestinal tract. Circular muscles contract behind the food bolus, while longitudinal muscles contract ahead of it, creating a wave-like motion. This movement helps move food forward, from one digestive organ to another, allowing for the sequential digestion and absorption of nutrients. Smooth muscles, primarily found in the walls of the esophagus, stomach, small intestine, and large intestine, are responsible for generating peristaltic contractions.
-Segmentation: Segmentation involves localized contractions and relaxations of the circular muscles in the digestive tract. It occurs primarily in the small intestine and serves to mix and churn the food, allowing for thorough mixing with digestive enzymes and optimal absorption of nutrients. Unlike peristalsis, segmentation does not propel the food in a specific direction but rather helps break it down and expose it to the absorptive surfaces. Smooth muscles, particularly circular muscles, contribute to segmentation movements.
How does the large intestine differ from the small intestine in its anatomy and smooth muscle structure?
The large intestine differs from the small intestines in anatomy by being wider in diameter and having a relatively shorter length, and in terms of smooth muscle structure, the large intestine has a thicker layer of smooth muscle in its muscular wall, which contributes to its characteristic haustral contractions and facilitates the movement and elimination of fecal matter.
What are the supposed functions of the appendix?
-The concentration of lymphoid tissue suggests an immune function.
-may be a "safe house" for gut microflora. An example being if a person is about to have diarrhea, gut microflora may move to the appendix to protect themselves.
-the appendix is not a vital organ
-What nerves supply abdominal viscera with sympathetic and parasympathetic innervation?
-What are the sympathetic and parasympathetic effects on abdominal viscera?
-Where do preganglionic sympathetic fibers synapse with postganglionic fibers?
- Abdominal viscera receive sympathetic innervation from the splanchnic nerves, which originate from sympathetic ganglia located along the vertebral column.
- Parasympathetic innervation to the abdominal viscera is supplied by the vagus nerves (cranial nerve X) and the pelvic splanchnic nerves (S2-S4).
- Sympathetic stimulation generally leads to vasoconstriction, reduced motility, and decreased secretions in the abdominal viscera, while parasympathetic stimulation promotes vasodilation, increased motility, and enhanced secretions.
- Preganglionic sympathetic fibers synapse with postganglionic fibers in sympathetic ganglia, which are located in the sympathetic chain near the vertebral column or in prevertebral ganglia situated anterior to the vertebral column.
What are the major unpaired arterial branches of the abdominal aorta that supply the foregut, midgut, and hindgut with oxygen-rich blood?
The major unpaired arterial branches of the abdominal aorta that supply the foregut, midgut, and hindgut with oxygen-rich blood are the celiac trunk (supplying the foregut), the superior mesenteric artery (supplying the midgut), and the inferior mesenteric artery (supplying the hindgut).
Describe rectus sheath above & below arcuate line
>> Above EAO aponeurosis in front of rectus, IAO splits around it, TA goes behind
>>Below All aponeuroses to the front
Which layers of abdominal wall have superficial & deep inguinal ring?
>>Transversalis fascia has deep ring
>>EAO aponeurosis had superficial ring
What are the primary functions of the liver?
-Main digestive function = production and secretion of bile
Also:
-Detoxify blood from gut
-Regulate blood glucose
-Lipid metabolism and elimination of cholesterol
-Synthesize plasma proteins
-Eliminates RBCs [along with spleen]
What structures pass through the porta hepatis and what do they carry?
-The hepatic artery proper
*Supplies liver with oxygen-rich blood
-The portal vein
*Drains blood from the gastrointestinal tract into the liver
-The common hepatic duct
*Drains bile form the liver
Trace blood entering the liver from the portal vein and hepatic artery proper to the IVC. What happens as blood flows through hepatic sinusoids?
=Portal Triad=
-Branches of Portal vein, hepatic artery proper, and *hepatic duct
-Blood from vein and artery mix ==) drains via the central vein ==) to *IVC
-Bile from hepatocytes drained via caniculli flows opposite direction to hepatic ducts.
===============================================================
-Blood enters the liver through the portal vein and hepatic artery proper. Inside the liver, it flows through specialized capillaries called hepatic sinusoids. As it passes through the sinusoids, the liver filters and processes the blood, extracting nutrients, detoxifying harmful substances, and removing debris. The sinusoids also allow for the exchange of substances between the blood and liver cells. After passing through the sinusoids, the blood is collected by central veins, which merge to form hepatic veins that drain into the inferior vena cava, returning the blood to the heart.
What is the structure that delivers oxygenated blood to the fetal liver and what do we call it after it has become obliterated in adult?
The structure that shunts oxygenated blood from the fetal circulation directly to the inferior vena cava (IVC), bypassing the liver, is called the ductus venosus. It is a short, vascular connection between the umbilical vein and the IVC. After birth, when the ductus venosus becomes obliterated, it is referred to as the ligamentum venosum. The ligamentum venosum is a fibrous remnant of the ductus venosus and is one of the landmarks used to identify the internal structures of the liver in adults.
What types of secretions are produced by the liver and pancreas and delivered to the duodenum through the major duodenal papilla?
The liver produces bile, which is a yellowish-green fluid that contains bile salts, bilirubin, cholesterol, and other substances. Bile helps in the emulsification and digestion of fats. The pancreas, on the other hand, produces pancreatic juice, which contains enzymes such as amylase, lipase, and proteases that aid in the digestion of carbohydrates, fats, and proteins respectively. Both bile and pancreatic juice are delivered to the duodenum through the major duodenal papilla, a small opening in the duodenal wall through which these secretions enter the digestive tract.
What is bilirubin and how is it formed? How does the body get rid of bilirubin?
Bile Salts [from cholesterol]
-Bile salts synthesized from cholesterol by liver
-From emulsion droplets that increase surface area for pancreatic lipase
Bile pigment
-It's a waste product of heme catabolism [from spleen and liver]
-Synthesized by hepatocytes and stored in gallbladder until released into duodenum.
-Enterohepatic circulation
*Recycling of bile salts
*Bile salts secreted in bile, reabsorbed by ileum, shunted back to liver and reused.
What are the major components of bile? What does bile do?
===Major Components===
-Cholesterol, phospholipids
-Ions [ex. bicarbonate]
-Water
===What it does===
-It breaks down fats into fatty acids, which can be taken into the body by the digestive tract.
How are the liver & pancreas involved in regulating blood glucose?
-The liver plays a central role in this process by balancing the uptake and storage of glucose via glycogenesis and the release of glucose via glycogenolysis and *gluconeogenesis.
-The pancreas secretes endocrine hormones into the blood that helps regulate blood glucose levels. These hormones are synthesized by pancreatic islets ( or *Langerhans)
What are the major functions of the spleen?
-Intraperitoneal
-Rids the body of
*Antibody-tagged bacteria
*Antibody-tagged blood cells
*Eliminates old RBCs [does so with liver]
*Recycles iron
*Heme converted to bilirubin by liver
-Stores RBCs
What structures do we find in the retroperitoneal space?
-The kidneys
-Adrenal glands
-Pancreas
-Nerve roots
-Lymph nodes
-Abdominal aorta
-Inferior vena cava.
What are the major unpaired and paired branches of the abdominal aorta?
===Unpaired Median Branches===
-Celiac Trunk [Foregut]
-Superior Mesenteric artery [Midgut]
-Inferior Mesenteric artery [Hindgut]
===Paired Lateral Branches===
-Inferior phrenic arteries [Diaphragm and adrenal glands]
-Middle suprarenal arteries [Adrenal glands]
-Renal arteries [Kidneys and adrenal glands]
-Gonadal arteries [Gonads]
Blood detoxification in liver
-Stellate macrophages aka "Kupffer cells"
-Chemical alteration of toxins formed by hepatocytes
*Ammonia becomes urea
*Drugs become less active forms that are more water soluble
-Excretion in bile
*Heme becomes bilirubin
Clinical Applications
===Cirrhosis===
-Liver damage due to chronic inflammation and scar tissue [fibrosis]
-Caused by hepatitis, alcoholism, drugs, etc
===Gallstones===
-Supersaturated cholesterol and/or pigment [bilirubin] that become crystalized in gallbladder
-can obstruct ducts
-treated through oral bile acids, shockwaves, or removal of gallbladder
===Jaundice===
-Excess bilirubin in blood
-Caused by impaired liver function [hepatitis, cirrhosis] or blockage of bile duct
What is the billiary tree?
What is their function?
Tubes that carry bile connect the liver to the gallbladder, and connect the liver and gallbladder to the duodenum.
===The tubes===
-The left hepatic duct and right hepatic duct drain bile from the left and right sides of the liver. These ducts unite to form the *common heptatic duct. It exits the liver through the porta hepatis.
-The *common hepatic duct is joined by the cystic duct from the gallbladder. The cystic duct allows bile to flow into and be stored by the gallbladder.
-The union of the cystic duct and common hepatic duct forms the bile duct. The bile duct runs inferiorly and joins the *main pancreatic duct from the pancreas.
-The union of these ducts forms the hepatopancreatic ampulla ( of Vater) shortly before draining into the duodenum via a common opening called the major duodenal papilla, which is guarded by the sphincter of Oddi.
Major Intraperitoneal and Retroperitoneal structures
===Intraperitoneal===
-Liver
-Stomach
-Transverse colon
-Small intestine
===Retroperitoneal===
-Ascending colon
-Descending colon
-Kidneys
-Aorta + IVC
Briefly describe the primary kidney functions.
-Removes waste products from blood and produces urine
===Bone Structure===
-Calcium Balance
-Vitamin D Activation
===Removal of Urea, Creatinie etc===
-Metabolic End Products
===Water Balance and Sodium Removal===
-Blood pressure regulation/ Production of urine is in correlation of water absorption and blood pressure.
Low BP= Less urine leaving body
High BP= More urine excreted
===Potassium Balance===
-Cardiac Activity
===Erythropoeitin Synthesis===
-Blood Formation
Briefly describe the primary adrenal gland functions.
-Secretion of corticosteroids and weak androgens by cortex and norepinephrine and epinephrine by medulla
-Adrenal glands produce hormones that help regulate your metabolism, immune system, blood pressure, response to stress and other essential functions.
Name and describe the three tissue layers supporting the kidneys
-Renal Parenchyma: Functional portion. Where urine formation takes place
-Renal Cortex: Outermost layer, dense connective tissue. Anchors the Kidney and separates it from other organs
-Renal Sinus: Drains urine from kidney and allows passage of blood vessels
-Renal Capsule: Dense connective tissue, protects from distension in every direction within kidney
-Renal Cortex and Renal Medulla make up the Renal Parenchyma
Describe the position of the kidneys, adrenal glands, ureters, and bladder in relation to the peritoneum
The kidneys, adrenal glands, ureters, and bladder are all located retroperitoneally, which means they lie behind the peritoneum. The kidneys are positioned on either side of the vertebral column, with the right kidney typically slightly lower than the left. The adrenal glands sit on top of each kidney. The ureters, which are tubes that carry urine from the kidneys to the bladder, run retroperitoneally from the kidneys to the pelvic region. The bladder, where urine is stored, is located in the pelvic cavity, also retroperitoneally, and is anterior to the rectum in males and anterior to the uterus and vagina in females.
Trace the path of plasma filtrate (and urine) from a renal corpuscle to a ureter.
The path of plasma filtrate (and urine) from a renal corpuscle to a ureter involves several structures within the kidney. After filtration at the renal corpuscle, the filtrate enters the proximal convoluted tubule (PCT), where reabsorption of nutrients and water occurs. From the PCT, the filtrate continues into the loop of Henle, where further reabsorption of water and electrolytes takes place. The filtrate then enters the distal convoluted tubule (DCT), where fine-tuning of electrolyte balance occurs. Finally, the filtrate passes into collecting ducts, which merge together to form larger papillary ducts. These papillary ducts empty urine into the renal pelvis, which connects to the ureter. The ureter carries the urine from the kidney to the urinary bladder for storage and eventual elimination from the body.
Describe the three functions of the nephron: filtration, reabsorption, & secretion
===Filtration===
-Filtration occurs at the renal corpuscle, where blood is filtered under pressure, separating small molecules such as water, ions, glucose, and waste products from larger molecules like proteins and blood cells. This creates a fluid called the filtrate.
===Reabsorption===
-Reabsorption takes place primarily in the renal tubules. It involves the selective reabsorption of valuable substances, such as glucose, amino acids, and water, from the filtrate back into the bloodstream. This process helps maintain the body's fluid and electrolyte balance.
===Secretion===
-Secretion occurs in the renal tubules, where certain substances, such as hydrogen ions, potassium ions, and drugs, are actively transported from the bloodstream into the tubules. This helps eliminate waste products and maintain proper pH and electrolyte levels in the body.
What types of capillaries make up the glomerulus? What kinds of substances does the glomerulus allow to be filtered and enter the filtrate? What kinds of substances does the glomerulus not allow to enter the filtrate? What are the other two filtration barriers called and how do they function?
-The glomerulus is composed of specialized capillaries called fenestrated capillaries. These capillaries have small pores or fenestrations in their walls, allowing for the filtration of fluid and solutes.
-The glomerulus allows smaller substances such as water, ions (sodium, potassium, etc.), glucose, amino acids, urea, and small proteins to be filtered and enter the filtrate. On the other hand, larger substances like blood cells and large proteins are not allowed to enter the filtrate.
-The other two filtration barriers in the glomerulus are the basement membrane and the podocyte filtration slits. The basement membrane is a thin layer of specialized extracellular matrix that acts as a physical barrier, preventing the passage of larger molecules. The podocytes, which are specialized cells that wrap around the glomerular capillaries, have foot-like extensions called pedicels that form filtration slits. These slits also act as a selective barrier, further preventing the passage of larger particles.
-Together, the fenestrated capillaries, basement membrane, and podocyte filtration slits form a filtration barrier known as the glomerular filtration barrier, which selectively filters substances based on their size, charge, and other properties, allowing for the formation of the filtrate while retaining larger molecules in the bloodstream.
Where along the nephron tubule system does salt and water reabsorption occur? Which of these is constant in its proportion of reabsorption and which one is dependent on an individual's hydration level?
-Salt and water reabsorption occur at different segments of the nephron tubule system.
-Salt reabsorption primarily occurs in the thick ascending limb of the loop of Henle and the early distal convoluted tubule (DCT). In these segments, sodium (salt) is actively reabsorbed, creating an osmotic gradient for water reabsorption.
Water reabsorption occurs predominantly in the proximal convoluted tubule (PCT) and the descending limb of the loop of Henle. These segments are responsible for the reabsorption of water passively following the osmotic gradient created by salt reabsorption.
-The reabsorption of salt is relatively constant and independent of an individual's hydration level. On the other hand, water reabsorption is dependent on an individual's hydration status. When well-hydrated, the body conserves water by reducing its reabsorption in the nephron tubules, resulting in the production of dilute urine. When dehydrated, the body increases water reabsorption to minimize water loss, leading to the production of concentrated urine.
Describe the process of salt and water reabsorption at the proximal tubule
The proximal convoluted tubule (PCT) is responsible for the reabsorption of the majority of filtered salt and water in the nephron. The process begins with the active reabsorption of sodium (Na+) ions from the tubular fluid into the epithelial cells lining the PCT. This creates a concentration gradient that drives the passive reabsorption of water through osmosis. As water moves out of the tubular lumen, solutes such as glucose, amino acids, and ions are carried along, undergoing paracellular or transcellular reabsorption. This combined process of salt and water reabsorption in the PCT helps maintain the body's fluid balance and reabsorb valuable substances before the remaining fluid continues through the nephron.
Describe the countercurrent multiplier system and the process of salt and water reabsorption at the nephron loop (of Henle). Does it vary with individual hydration levels? Which limb actively pumps salt into the renal tissue space? Which limb is permeable to water?
-The countercurrent multiplier system in the nephron loop (of Henle) is a mechanism that creates and maintains an osmotic gradient in the renal medulla. This gradient enables the reabsorption of water and further concentration of urine.
-In the descending limb of the loop, water is passively reabsorbed through aquaporin channels, driven by the increasing osmolarity of the medullary interstitium. This causes the tubular fluid to become more concentrated as it descends.
In the ascending limb, there is active reabsorption of sodium (Na+) and chloride (Cl-) ions, but water permeability is low. This segment pumps Na+ and Cl- out of the tubular fluid into the renal tissue space, creating a high osmolarity in the medullary interstitium.
-The countercurrent flow of fluid in opposite directions in the descending and ascending limbs establishes a concentration gradient that allows for the reabsorption of water in the collecting ducts, concentrating the urine. This process is critical for water conservation in the body.
-The rate of salt and water reabsorption at the nephron loop does not directly vary with an individual's hydration levels.
-However, the overall reabsorption and concentration of urine can be influenced by hormonal regulation, such as antidiuretic hormone (ADH), which adjusts the permeability of the collecting ducts to water based on hydration status.
Describe countercurrent exchange and the function of the vasa recta and peritubular capillaries.
-Countercurrent exchange is a mechanism that allows for the efficient exchange of substances, such as oxygen and solutes, between two adjacent flowing fluids that move in opposite directions. This process is particularly important in the vasa recta and peritubular capillaries in the kidney.
-The vasa recta are specialized capillaries that run parallel to the nephron loop (of Henle). They function to maintain the concentration gradient in the medullary interstitium by allowing for the exchange of water and solutes between the blood and the interstitium. This helps prevent the dissipation of the osmotic gradient created by the nephron loop.
-Peritubular capillaries are tiny blood vessels that surround the renal tubules throughout the kidney. They play a crucial role in reabsorption and secretion processes by carrying away reabsorbed substances from the renal tubules and supplying necessary nutrients and oxygen to the renal tissue.
-Both the vasa recta and peritubular capillaries contribute to the efficient exchange of substances, ensuring the proper functioning of the nephron and the maintenance of the osmotic gradient in the kidney.