Injury & Repair of the Nervous System
1/65
Earn XP
Description and Tags
These flashcards summarize key concepts, facts, and processes related to injury and repair of the nervous system as discussed in the lecture notes.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
What are the changes that occur after sensory nerve injury in the dorsal root ganglion?
Changes in cell somas include chromatolysis, swelling, and migration of the nucleus.
What two roots make the spinal nerves
The dorsal and ventral roots
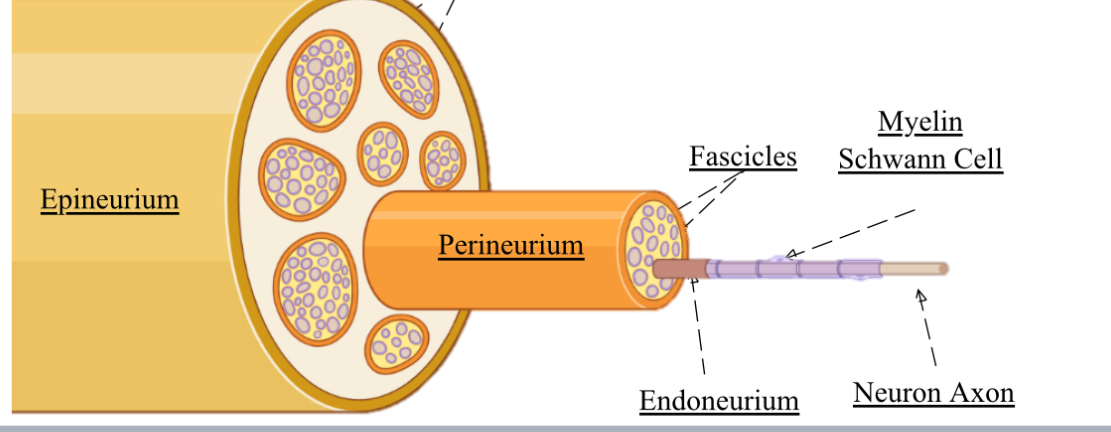
3 layers of connective tissue in the spinal nerve
Epineurium
Perineurium - wraps fascicles
Endoneurium - wraps a single axon
What are the 3 types of nerve damage
neuropraxia - mild
Axonotmesis - mid
Neurotmesis - severe
What is Neuropraxia?
A mild nerve injury , so temporary disruption of nerve function due to compression or stretch.
where the myelin is intact , no anatomical injury.
Reversible
Outline axonotmesis
Nerve stretch or crush due to trauma.
The Axon / myelin is damaged, so nerve conduction is reduced.
Full recovery takes time and needs regeneration of axons.
Epineurium and endoneurium stays intact.
Outline nerotemesis
Both axons and the myelin sheath are disrupted , due to cutting of the nerve.
The endoneurium ruptures and demyelination reduces nerve conduction.
Not reversible on its own , so immediate surgery is needed.
What distinguishes Axonotmesis from Neuropraxia?
In Axonotmesis, both myelin and axon are not intact, leading to potential sensory and motor loss.
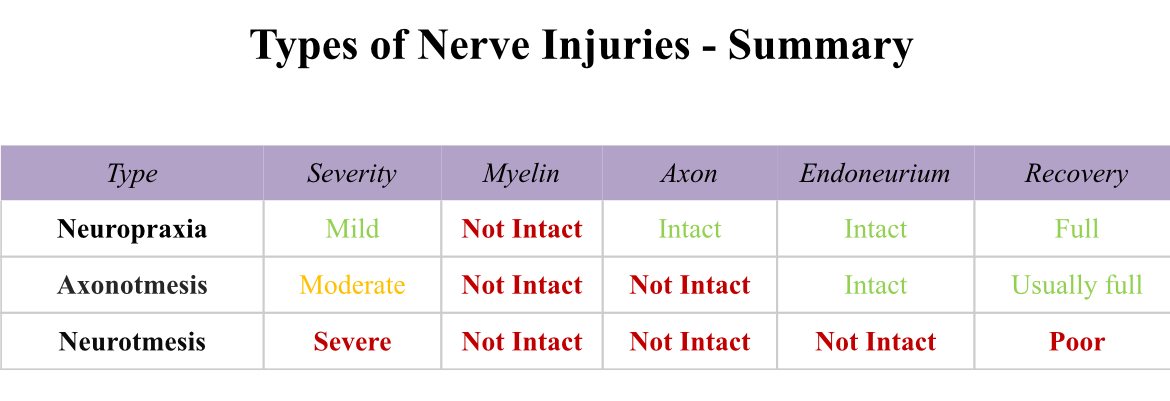
What is the prognosis for recovery in Neurotmesis?
Recovery is poor, and full motor and sensory recovery is rare; typically requires surgical intervention.
What happens during Wallerian Degeneration?
Degeneration occurs distal to the site of injury, leading to myelin and axon breakdown.
What is the growth rate for axon regeneration?
Approximately 1-1.5 mm per day.
What factors influence the success of nerve repair?
The severity of the initial injury and extent of secondary damage from inflammation and ischemia.
What role do Schwann cells play after nerve injury?
They help in the repair process by detaching from axons, proliferating, and remyelinating the new axon.
What are the 2 places cellular change happens in the nerve, after axonotemesis ?
proximal retrograde - chromatolysis (reactive changes in the cell body or soma) , so cell body swells, nucleus migrates.
Distal anterograde - which is degeneration down the axon first.
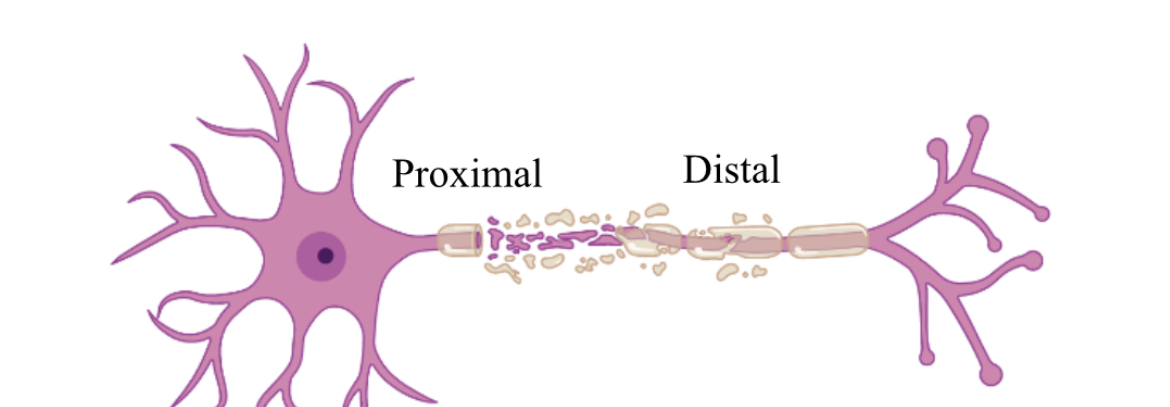
Go over steps in distal anterograde.
Schwaan cells detach from axons and differentiate to repair the cells.
Distal axons degenerate, and anterograde from site of injury down axon- called wallerian degeneration.
The debris left is cleaned by activated resident macrophages. They release histamines to attract more macrophages.
Then nerve fibres start sprouting from the proximal end , to create a growth cone.
Repaired Schwaan cells repair and release growth factors to guide growth cone to axonal tip.
Schwaan cells remyelinate the axon and chromolysis ends.
What are 3 ways the site on injury in nerves spread ?
Anterograde degeneration
Retrograde degeneration- axons ‘die-back’.
To cell body
all by transneuronal damage.
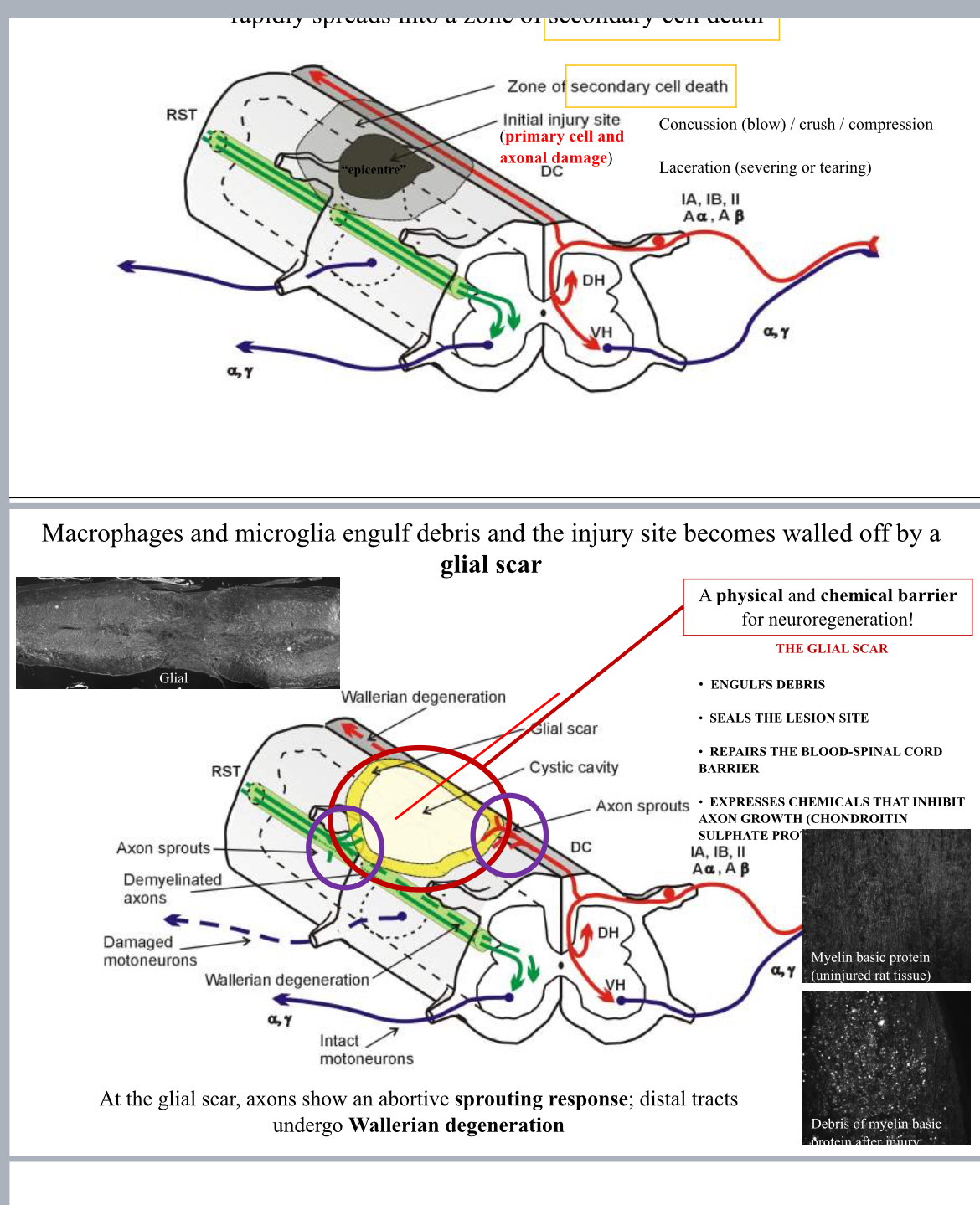
How do astrocytes contribute to the challenges of CNS repair?
They form a glial scar that acts as a physical and chemical barrier, inhibiting axonal growth.
What are CSPGs and their function in CNS injury?
Chondroitin sulfate proteoglycans are secreted by activated astrocytes and inhibit axon regeneration.
What is the effect of prolonged muscle denervation?
It leads to muscle atrophy, fibrosis, and a significant decrease in regenerating axons.
What is the relationship between injury proximity to the cell body and regeneration?
Closer injuries to the cell body result in a longer recovery process.
Difference between primary and secondary damage ?
Primary is immediate damage to nerves from trauma …
Secondary is after , so things like inflammation and harmful chemicals .
What defines the epicenter in spinal cord injury?
The site of primary cell death that rapidly spreads into a zone of secondary cell death.
What is the typical recovery timeline for sensory recovery after nerve injury?
By 100 days at the wrist, by 1 year at fingertips, and by 2 years for pain discrimination.
What are the key players in PNS repair compared to CNS repair?
Swann cells and macrophages in PNS vs. oligodendrocytes and astrocytes/ microbial in CNS.
What challenges do macrophages face in CNS repair?
They are less efficient in debris clearance compared to macrophages in the PNS.
What happens to the axon and myelin after axonotmesis?
They undergo degeneration with debris left behind, prompting Schwann cell repair mechanisms.
What could improve axonal regeneration after injury?
Neuroprotection to minimize early trauma effects, and promoting axonal regeneration through trophic support.
In repair of the CNS what are 3 things that make it more difficult ? And why
Reduced debris clearance - microglia/ atrocities are not as good as macrophages. So debris obstructs the growth cone.
Glial scar formation- resident astrocytes are activated and proliferate. The scar seals debris and inflammation around the lesion. Again physically inhibits growth cone.
Axon regeneration inhibition.
What are the chemical barriers to CNS Repair ?
activated astrocytes in the glial scar secrete CSPGs or chondroitin sulphate proteoglycans
degenerating oligodendrocytes release myelin associated inhibitors or MIA
What are the two types of degeneration after a nerve injury?
Retrograde (proximal) and anterograde (distal) degeneration.
What are myelin-associated inhibitory proteins?
They are proteins like Nogo and MAG that inhibit axonal growth in the CNS.
Where does spinal cord trauma spread? From the epicentre or area of primary cell death ?
To the zone of secondary cell death.
What is the definition of axonotmesis?
A moderate nerve injury where the myelin is not intact, and both axon and endoneurium may be affected.
What happens to the nerve at the site of neurotmesis?
Both the axons and nerve sheath are disrupted, leading to a need for surgical intervention.
What effect does time have on nerve repair outcomes?
The longer the time post-injury, the less favorable the outcome tends to be.
How fast can nerve growth speed vary?
From 0.5 mm to 9 mm per day, but typically around 1 mm per day.
Why is immediate surgical intervention recommended for neurotmesis?
To ensure a higher chance of recovery due to the complete nerve severance.
What is a significant limitation of CNS regeneration?
The presence of glial scars and inhibitory proteins impedes axonal regrowth.
How do injuries to the spinal cord impact overall function?
They can lead to conditions such as tetraplegia and paraplegia due to disrupted neural pathways.
What is the significance of the research mentioned for CNS injuries?
Research is ongoing to find ways to facilitate and improve recovery mechanisms in the CNS.
What is the role of microglia following CNS injury?
Microglia are activated to clear debris but are less efficient than macrophages in the PNS.
What is the importance of promoting axonal growth after CNS injury?
To re-establish appropriate connectivity and restore function.
What are neurotrophins?
Growth factors that support neuron survival and growth during regeneration.
What factor significantly reduces the chances of recovery after prolonged axotomy?
The number of motoneurons that can regenerate decreases significantly.
What can physical barriers do in the nervous system repair process?
They can prevent the growth cone from moving distally, inhibiting successful regeneration.
How does the CNS compare to the PNS in terms of repair success?
CNS regeneration is generally less successful due to more complex barriers and a hostile environment.
What is the outcome for motor and sensory recovery in Clint Hallam's case after 2 years?
Sensory and some motor functions showed significant improvement, though not completely normalized.
What defines a 'glial scar'?
A cellular barrier formed by astrocytes that restricts axonal regrowth after CNS injury.
How do resident astrocytes contribute post-injury?
They proliferate rapidly to form a glial scar which hinders axonal growth.
What is the relationship between inflammation and nerve injury recovery?
Inflammation can contribute to secondary damage, worsening outcomes for nerve repair.
What is an example of an irreversible nerve injury?
Neurotmesis, where surgical intervention is often necessary for any chance of recovery.
What happens to sensory and motor functions immediately following an injury?
They can temporarily decline, depending on the severity and type of nerve injury.
What is the effect of secondary damage on nerve injuries?
It can lead to further complications and hinder the recovery process.
How does injury classification (mild, moderate, severe) impact recovery?
Severity affects the recovery potential and complexity of treatment needed.
Why is debris clearance important in nerve repair?
To prevent physical barriers and facilitate the regeneration of axons.
What is a critical factor in the timeline of nerve regeneration?
The location of the injury influences how quickly recovery can occur.
What happens to resident macrophages after a nerve injury?
They are activated to aid in debris clearance and support repair mechanisms.
What role does the environment play in neural repair?
The injury environment can support or inhibit axonal growth and regeneration.
What is a 'composite tissue allograft'?
A graft that includes multiple tissue types, requiring axons to regrow to restore function.
How does axonal regeneration differ in the PNS compared to the CNS?
PNS repair is generally more successful due to supportive microenvironments.
What is one outcome of delayed nerve repair?
It can lead to permanent loss of function due to prolonged atrophy or degeneration.
What is the significance of chemical barriers in the CNS?
They inhibit growth cones and axonal regrowth after injury, complicating recovery.
What happens during axon regeneration in the PNS?
A growth cone forms at the proximal end and attempts to reconnect with distal targets.
What therapeutic strategy could aid CNS recovery?
Combination therapies that address multiple barriers to axon regeneration.
What is the main goal of research into the central nervous system injuries?
To find effective treatments that enhance regeneration and restore function.
What does the process of nerve regeneration include?
Clearance of debris, axonal sprouting, and remyelination by Schwann cells.