PATH 3610 - Midterm 1
1/409
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
410 Terms
Number 1. Which of the following microscopic features is the best indicator of necrosis?
a. cytoplasmic swelling
b. blurring and/or loss of cellular outlines
c. nuclear pyknosis, karyorrhexis or karyolysis
c

Number 2. Which of the following is not a post-mortem change?
a. hemorrhage
b. rigor mortis
c. settling of blood in dependent parts, termed "lividity"
a
Number 3. Local death of a cell or cells due to injury is known as:
a. ischemia
b. necrosis
c. Infarction
b
Number 4. Which of the following is not true of jaundice?
a. yellow discolouration of connective tissues occurs
b. it is a disease of the liver
c. it can occur secondary to widespread hemolysis of red blood cells
b
Number 5. The switch of cells from aerobic to anaerobic metabolism can cause:
a. stabilization of organelle membranes
b. damage to lysosomal membranes, potentially worsening cell injury
c. acetic acid production
b
Number 6. Which of the following is not a cause of impaired cell energy production?
a. hyperglycemia
b. respiratory obstruction or disease
c. uncoupling of oxidative phosphorylation
a
Number 7. Apoptosis refers to:
a. shrunken nuclei seen in necrosis
b. programmed cell death to remove "old" cells
c. lysis of cells caused by membrane injury
b
Number 8. Swelling of mitochondria caused by impaired cell energy production can cause:
a. cloudy or vacuolar cytoplasmic changes
b. increased oxidative phosphorylation
c. acceleration of ATP synthesis
a
Number 9. Free radicals generated within cells are unstable and can lead to:
a. stabilization of lipid membranes
b. breaking down of protein cross-links
c. degradation of nucleic acids
c
Number 10. Alcohol comsumption can lead to fatty liver changes by:
a. decreasing hepatic oxidation of triglycerides
b. decreasing mobilization of adipose tissue due to increased caloric (alcohol) intake
c. induction of enzymes to increase fatty acid conversion into triglycerides
c
The release of cytoplasmic enzymes from necrotic cells may be useful diagnostically. T/F
T
Bilirubin is:
a. lipid soluble when conjugated
b. water soluble when conjugated
c. conjugated in the kidney for excretion in the urine
b
Agents such as radiation, mutagenic drugs and viruses can lead to acquired DNA abnormalities.
Damage to cells such as blood cell precursors in the bone marrow is the result of:
a. failed synthesis of structural proteins
b. failure of growth regulating proteins
c. interference with mitosis
Starvation can lead to a fatty liver. T/F
T
Free radicals can impair cell membrane function by causing:
lesions in DNA
lipid peroxidation
protein cross-linking
b
Apoptosis refers to:
the internalization of material by a cell
disintegration of tissues which occurs after death
programmed cell death
c
The colour changes in a bruise are related to:
necrosis of tissue
synthesis of hemoglobin
breakdown of hemoglobin
c
Elevated conjugated serum bilirubin levels are most likely caused by:
acute hypoxic hepatic injury
obstruction of the biliary tract
intravascular hemolysis
b
Dystrophic calcification refers to abnormal deposition of calcium salts:
in dead or dying tissues
in tissues due to high serum calcium levels
associated with inherited calcium metabolic disorders
a
Bilirubin is:
lipid soluble when conjugated
water soluble when conjugated
conjugated in the kidney for excretion in the urine
b
Hypoxia, leading to impaired energy production by the cell, may be caused by:
anemia
low blood glucose levels
inhibition of respiratory enzymes
a
A myocardial infarct is seen as a dry, well demarcated area of pale tissue. This would be described as:
coagulation necrosis
caseation necrosis
an abscess
a
What is an infarct?
A small area of dead tissue resulting from failure of blood supply
Chronic over-consumption of alcohol can lead to fatty liver due to:
decreased oxidation of triglycerides
increased activity of hepatic enzyme systems, leading to increased conversion of fatty acids to triglycerides
decreased mobilization of adipose tissue due to increased alcoholic caloric consumption
b
Cellular injury can result when bilirubin accumulates in:
parenchymal cells (such as the liver or brain)
connective tissue
skin
a
Cloudy swelling is the result of:
intracellular accumulation of fluid and electrolytes
decreased intracellular pH
triglyceride accumulation
a
Anemia will lead to impaired energy production by the cell because there is:
insufficient oxygen
low glucose levels
enzyme inhibition
a
Death of cells in a living organism is termed:
gangrene
necrosis
ischemia
b
The primary change in hemolytic jaundice is:
inadequate bilirubin excretion
increased production of bilirubin
serum accumulation of conjugated bilirubin
b
The release of cytoplasmic enzymes from necrotic cells may be useful diagnostically.
true
false
T
Agents such as radiation, mutagenic drugs and viruses can lead to acquired DNA abnormalities. Damage to cells such as blood cell precursors in the bone marrow is the result of:
failed synthesis of structural proteins
failure of growth regulating proteins
interference with mitosis
c
Triglyceride accumulation in the cytoplasm of parenchymal cells (such as the liver) is termed:
cytoplasmic vacuolation
hyperglycemia
fatty degeneration
c
Epithelial tissue
covers surfaces, skin, and inner linings, houses secretory glands
Connective Tissue
also called stroma, supports structures of body, organs
Hermolymphatic Tissues
comprises the immune system, including blood and inflammatory response
When the ________________ of a cell is exceeded, cell injury and death occur
adaptive response
Why is the light microscope not the best method of detecting cell death?
Severe biochemical damage may be undetectable under light microscope
What is Etiology?
The actual cause of the disease
What is Pathogenesis?
The development of the disease
Is immunological abnormality etiology or pathogenesis?
etiology
Is genetic abnormality etiology or pathogenesis?
etiology
Is nutritional imbalance etiology or pathogenesis?
etiology
Is infection etiology or pathogenesis?
etiology
Is trauma etiology or pathogenesis?
etiology
Are toxins etiology or pathogenesis?
etiology
Is biochemical change etiology or pathogenesis?
pathogenesis
Is structural change etiology or pathogenesis?
pathogenesis
Reversible Cell Injury: explain cellular swelling
increased cell permeability
Reversible Cell Injury: explain fatty change
lipid vacuoles containing triglycerides in the cytoplasm
Reversible Cell Injury: explain compensation state
a state where an un-optimal function is sufficient enough for the cell to continue functional at a sub-efficient level
What are the 3 things that occur during Reversible Cell Injury
Cellular swelling, fatty change and compensation state
What are the 3 things that occur during the Transition point of "reversible" to "irreversible"
- inability to restore mitochondrial function
- loss of function of cell membranes
- loss of DNA and chromatin integrity
Somatic death
death of the whole body
What is eosinophilia
Higher than normal levels of white blood cells
In necrosis, what are the two types of cytoplasmic evidence?
cytoplasm become homogenous, and deeply staining : denaturing of cytoplasmic proteins and loss if ribosomes
cytoplasm becomes vacuolated/bubbly : impaired energy production. Leads to failure of cell membrane pumps, and can cause mitochondria to swell up
In necrosis, what are the 3 types of nuclear evidence?
Pyknosis means that the nucleus shrinks and increased basophilia.
Karyorrhexis: next, the nuclear fragmentation occurs.
Karyolysis: basophilia fades after the DNase (deoxyribonuclease) digests the DNA due to lysosomal enzymes.
Which is better evidence of necrosis - cytoplasmic or nuclear?
nuclear
Explain cause and brief description of following necrosis type:
coagulative
caused by ischemia (loss in blood supply)
underlying tissue architecture is preserved for days because of decreased blood flow and because the injury denatures proteins and enzymes
What is microscopic evidence of coagulative necrosis?
cell outline is present, but nuclei is lost
Injection sites and
infarcts are examples of ___________ necrosis
coagulative
Proteins are denatured in which type of necrosis?
coagulative
Explain cause and brief description of following necrosis type:
liquefactive
caused by bacterial infection
there are many inflammatory cells, and where enzymes of white blood cells liquefy the tissue. materials is sometimes yellow and creamy - pus
Fungal inflections & Focal bacteria are examples of ____________ necrosis
liquefactive
Explain cause and brief description of following necrosis type:
Gangrenous
loss of blood supply, often to entire limb - type of coagulative necrosis
death of multiple layers of tissue
Explain cause and brief description of following necrosis type:
caseous
seen in foci of tuberculous infection
collection of fragmented and lysed cells
What type of necrosis happens in foci of tuberculous infection?
caseous
What is a unique microscopic property of caseous necrosis
obliterated cell oulines
What necrosis looks cheese-like
& yellow-white color?
caseous
Explain cause and brief description of following necrosis type:
Fat necrosis
caused by pancreatic lipases that are released into peritoneal cavity and substance of pancreas
liquefies fat cell membranes
What type of necrosis produces chalky white areas?
fat necrosis
What type of necrosis happens during - release of pancreatic lipases into the pancreas and peritoneal cavity
- acute pancreatitis
fat necrosis
Explain cause and brief description of following necrosis type:
Fibrinoid necrosis
Caused by immune response where antigens and antibodies are deposited on the walls of blood vessels.
What type of necrosis causes wall of damaged blood vessels to produce pink, amorphous appearance on H&E preparation (Fibrinoid)
fibrinoid
What type of necrosis happens during - severe hypertension
- immunologically mediated diseases (polyarthritis nodosa)
fibrinoid
What are the 2 types of fat necrosis and explain each?
Enzymic fat necrosis: Occurs in pancreatic injuries and acute pancreatitis
Release of pancreatic enzymes (especially lipase) into adjacent tissue
There is considerable adipose tissue in abdominal mesentery and omentum.
Pancreatic lipase breaks down triglycerides in fat cells into glycerol and fatty acid
Creates Ca 2+ soaps which give white chalky appearance
Nonenzymic fat necrosis:
Occurs in breasts and or subcutaneous (under the skin) tissue following trauma
Induces inflammatory response - granulomatous
dystrophic calcification
- abnormal deposition in DEAD tissue
- Calcification of fatty plaques (atheroma) or atherosclerosis
Explain how loss of tissue occurs during tissue necrosis?
decreased vascular flow
typically in farthest reaches of body
Explain how secondary infection occurs during tissue necrosis?
- necrotic tissue minimizes blood flow, and reduces inflammatory response and delays repair
- great place for infection because it is outside the reaches of the immune system
Explain how systemic effect occurs during tissue necrosis?
- Fever and increased white cell blood count (due to inflammatory response)
- Occurs due to release of pyrogens (fever inducing agents) from necrotic cells
Explain how local effect occurs during tissue necrosis?
blood vessel rupture, pain, gastric ulcers and blood in stool
Explain how release of enzymes from necrotic cells occurs during tissue necrosis?
cytoplasmic enzymes of necrotic cells can be released by necrotic tissue, and can be examined for diagnosis via serum sample
Which type of cell death exhibits inflammation? apoptosis or necrotic
necrosis
What is physiological apoptosis?
unwanted cells are destroyed and replaced
What is apoptosis by pathological condition?
elimination of cells that are beyond repair
Apoptosis is regulated by biochemical pathways that cause the activation of ________.
caspases
What are caspases?
protease enzyme that plays a major role in cell death and inflammatory response - activates "executioner caspases" to degrade DNA and cell proteins
What are the names of the 2 pathways that apoptosis can occur?
Intrinsic and Extrinsic
Briefly explain the intrinsic pathway of apoptosis?
Mitochondria becomes permeable
cytochrome c leaks into cytoplasm
activates caspase-9
cell death
Briefly explain the extrinsic pathway?
FasL receptor on the T-lymphocyte binds to TNF receptor on the host
the receptor binds with receptor proteins in cytoplasmic side of membrane
activates caspase-8
cell death
In which pathway is caspase-8 activated?
extrinsic (involving T-lymphocyte)
In which pathway is caspase-9 activated?
intrinsic (involving mitochondrial death)
What is Necroptosis?
This is triggered when TNF receptors are activated, along with other triggers.
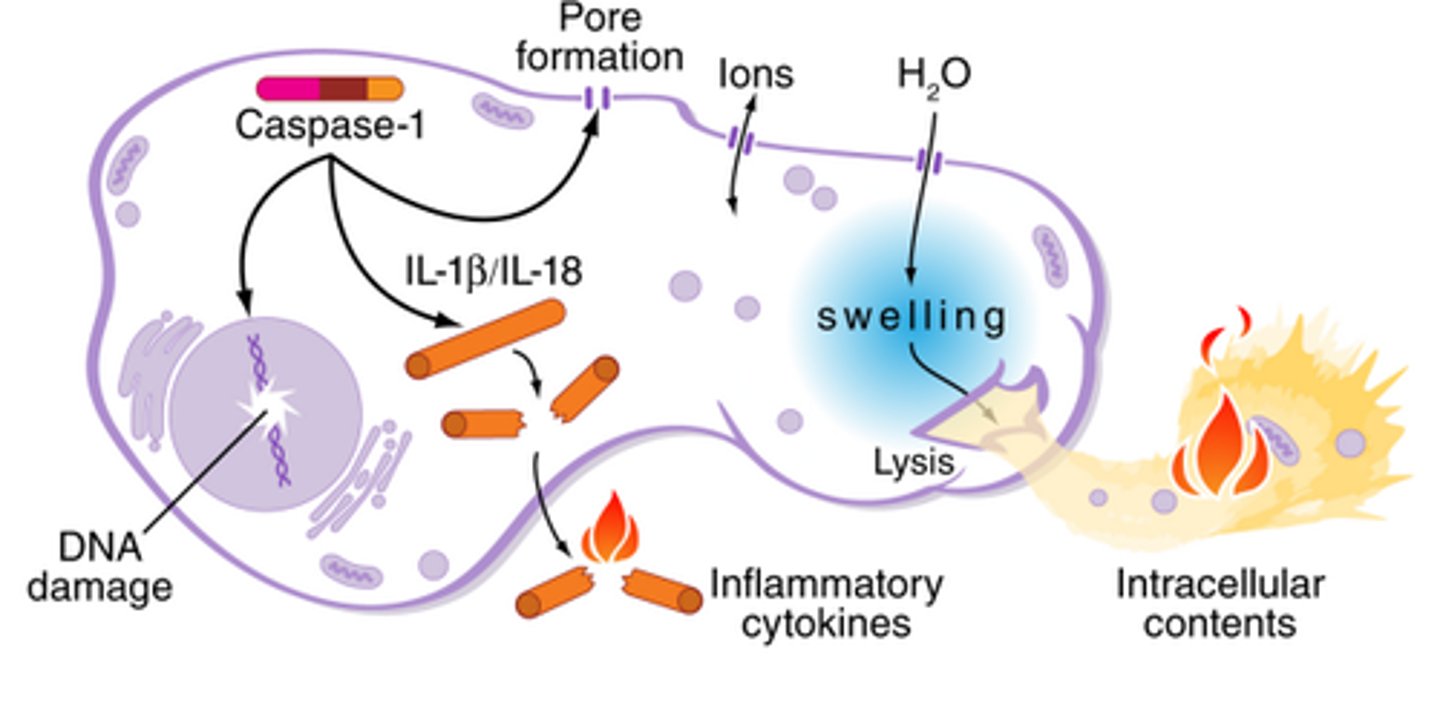
Pyroptosis
activation of cytosolic protein complex called inflammasome which activates caspases causing cell death.
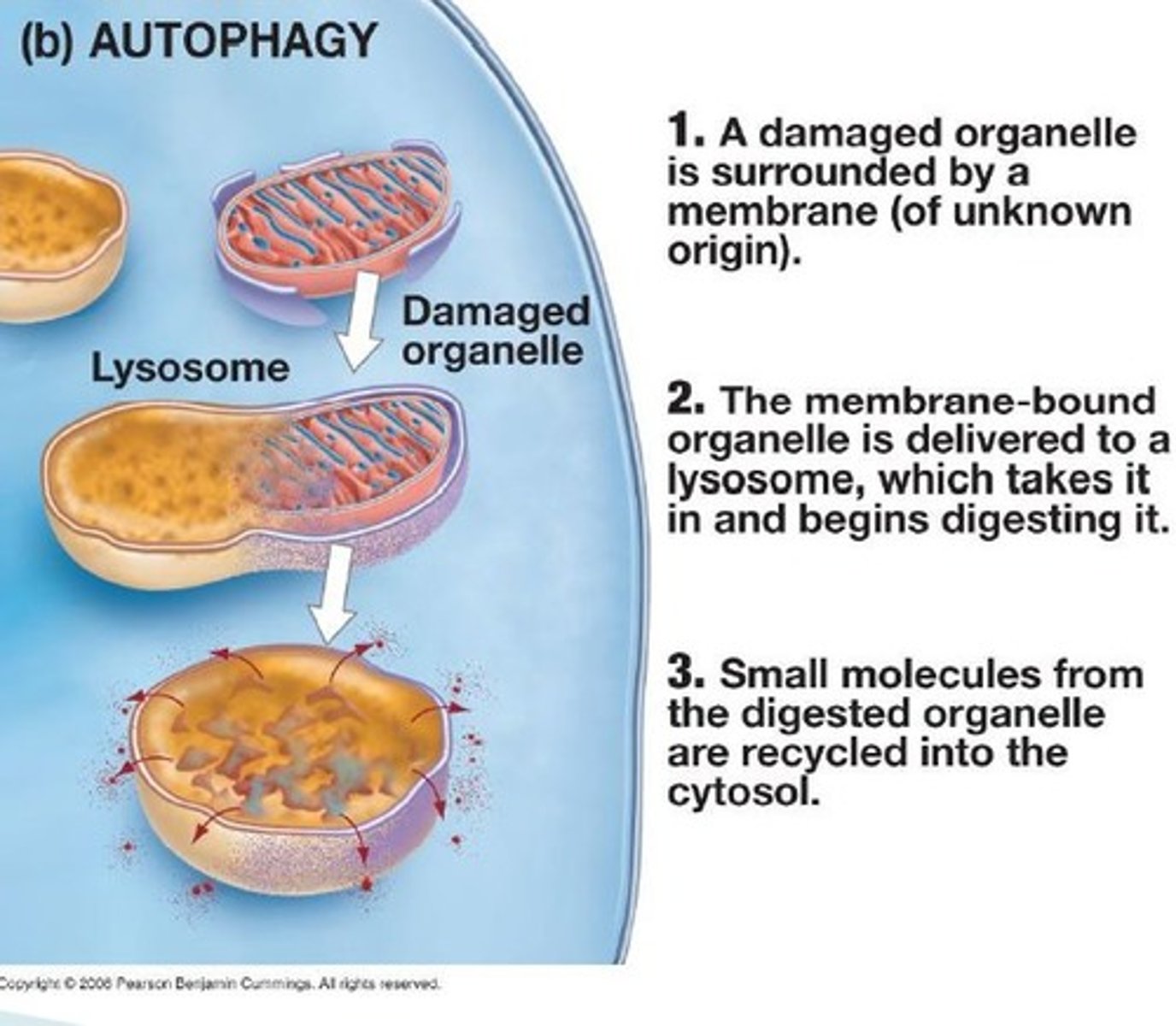
Autophagy
self-eating
cell eats organelles through lysosomal enzymes & digestion
How does lysosomal enzyme release happen?
occurs due to lack of oxygen to utilize anaerobic metabolism - causes production of lactic acid
which lowers cell pH
causes damage to lysosomal membranes
enzymes are released
Rigid Mortis:
stiffening of body due to reduction of ATP in muscle
Post mortem lividity:
gravitational settling of blood in low parts - breakdown of hemoglobin causes green tone in the skin
Post mortem blood clotting:
large clots in chambers of the heart
Putrefaction:
fermentation caused by saprophytic (organism that lives off of dead material) bacteria, gas accumulation may rupture stomach and foamy liver
Autolysis:
disintegration of tissue due to action of own enzymes