Monitoring in mechanical ventilation PPT (3/18)
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
PIP
Peak pressure represents highest pressure during an inspiration and can be affected by: Kinks/obstruction in vent, increased airway resistance, decreases in dynamic lung compliance.
Pplat
Plateau pressure reflects changes in overall lung compliance. Increased = worsening/decrease of lung compliance, making it not an easy fix as it would be based on pathology.
Causes: worsening ARDS/disease process, pneumonia, atelectasis, fluid in/around lung.
Solution: not an easy fix; however, adjusting VT can prevent further damage by either decreasing VT to keep Pplat <30cmH2O OR increasing RR to maintain VE.
Goal of PEEP
Avoid distention, keep alveoli open and prevent collapse during exhalation. It enhances tissue oxygenation, maintains PaO2, SpO2 and acceptable pH, recruits alveoli and maintains aeration and restores FRC.
Indications of PEEP
Bilateral infiltrates (CXR)
atelectasis w/ low FRC
reduced lung compliance
<60mmHg PaO2 @ >50% FiO2
PaO2/FiO2 @ <200mmHg for ARDS + <300mmHg for ALI
Refractory hypoxemia: PaO2 +<10mmHg w/ FiO2 +20%
Optimum PEEP evaluators
Pt. appearance
BP
BS
Vent parameters
Static compliance
Optimum PEEP study
Summary: a chart where as PEEP increases, data is affected. Mainly find where BP and QT DROP then back up a little. Keep an eye mainly on the PEEP, PaO2, BP and QT values.
PEEP increases = increased PIP and Pplat
Compromised cardiovascular
Thoracic pressure can affect intracranial pressure as it decreases QT. Artery has more muscle than a vein, so when the vena cava gets squeezed while they are naturally floppy (aka. reduced SA), blood will back up and increase intracranial pressure.
Summary: don’t want to affect other areas of the body!
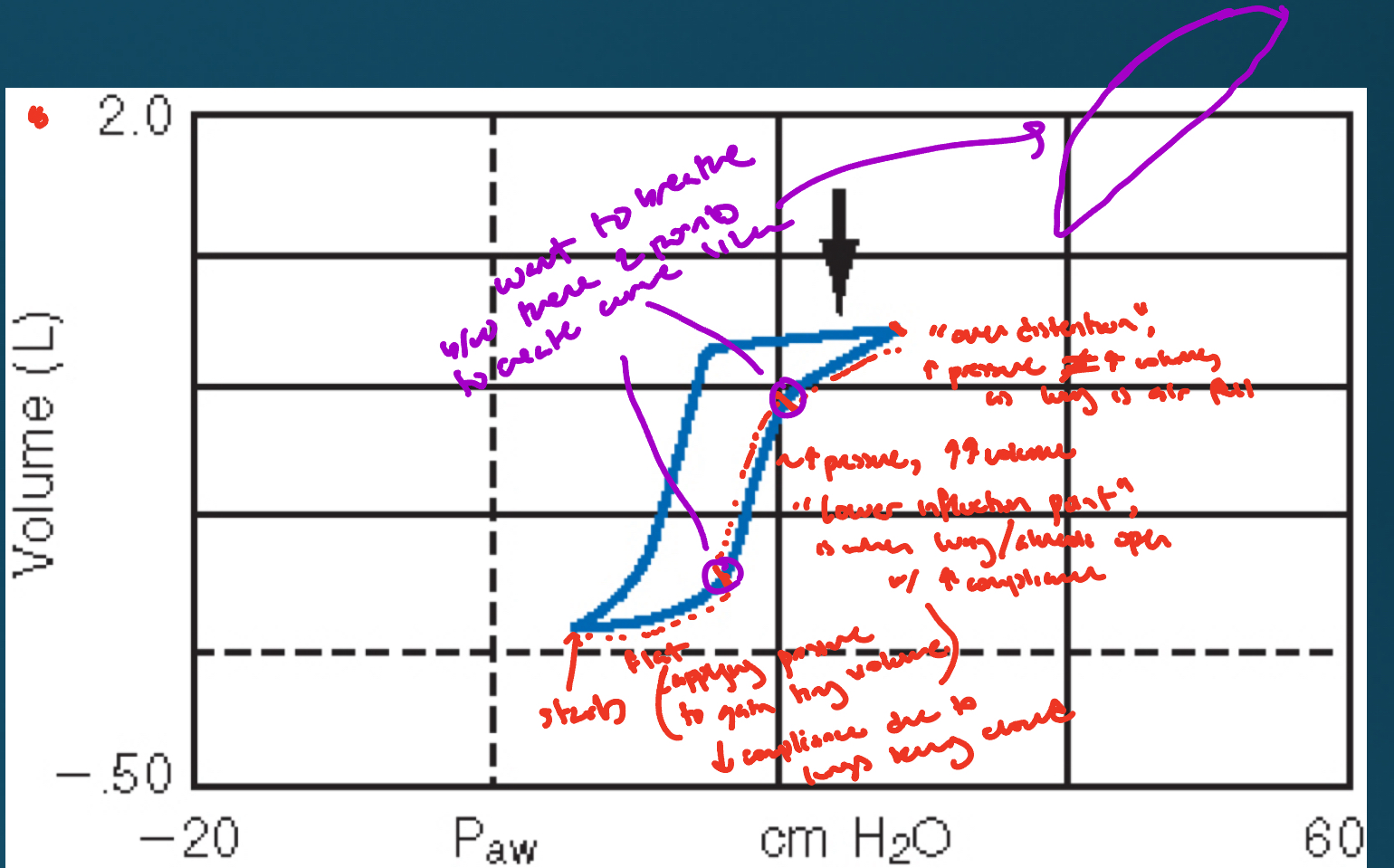
Pressure volume curve
Bottom circle: applying lots of pressure but to gain tiny volume. Due to decreased compliance due to lungs being closed.
Middle area: “Lower inflection point” where alveoli are open with increased compliance. This shows increased pressure producing lots of volume.
Top area: “Over distention” where increased pressure does not increase volume as lungs are full.
Summary: want to breathe in that middle area, as want to produce the shape drawn in the image.
PEEP w/ pulmonary vascular pressure monitoring
Requires a swans-ganz catheter or however u spell it. Refers to zones.
Contraindications of PEEP
hypovolemia (decreased circulation as decreased PEEP = decreased flow)
untreated pneumo or tension pneumo
intracranial pressure
preexisting hyperinflation
pulmonary effects of PEEP
transmission of airway pressure to pleural space
Indications of PEEP
CHF
Postop atelectasis and hypoxemia
Sleep apnea (NIV only)
CF
airway suctioning
PEEP weaning
>50% FiO2 = O2 injury = +PEEP
Criteria for weaning: acceptable PaO2 <40 FiO2, hemodynamically stable, non septic and improved lung condition
What increases MAP? What does MAP affect?
Increased I-time, PEEP = increased MAP
Increased MAP = increased oxygenation, as it doesn’t affect cardiovascular system due to it decreasing QT.
Improving oxygenation
hypoxemia (PaO2 <60mmHg requires Tx)
Increase FiO2
Add PEEP while hawking BP (use PEEP trial)
improve circulation
Hb (do we have enough box cars?)
CPAP / APRV / IRV / HFOV / ECMO / INO / IP
IRV = inverse ratio ventilation will cause them to airdrop on purpose by increasing I-time
what does intrapulmonary shunting affect?
atelectasis
pulmonary edema
pneumonia
pneumo
complete airway obstruction
PEEP/FiO2 ladder
tool that offers clinician way to adjust parameters that effect oxygenation on a vented patient mainly used on ARDS patients (but not limited to).
Flow and inspiratory time
Some vents give FLOW directly (60LPM is good for adults) or through I-TIME (1s is good start). Obstructive pt need longer E-time and hypoxemia patients need longer I-time.
Shorter I-time = longer E-time which leads to less air trapping but flow becomes more turbulent and peak pressure will increase
Longer I-time = shorter E-time which causes less turbulence, peak pressures to decrease, and MAP to increase, but could lead to air-trapping/auto PEEP
Flow INCREASES = I-time DECREASES
(inverse relationship, opposite works the same)