Module 5 - Communication, Homeostasis & Energy
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
82 Terms
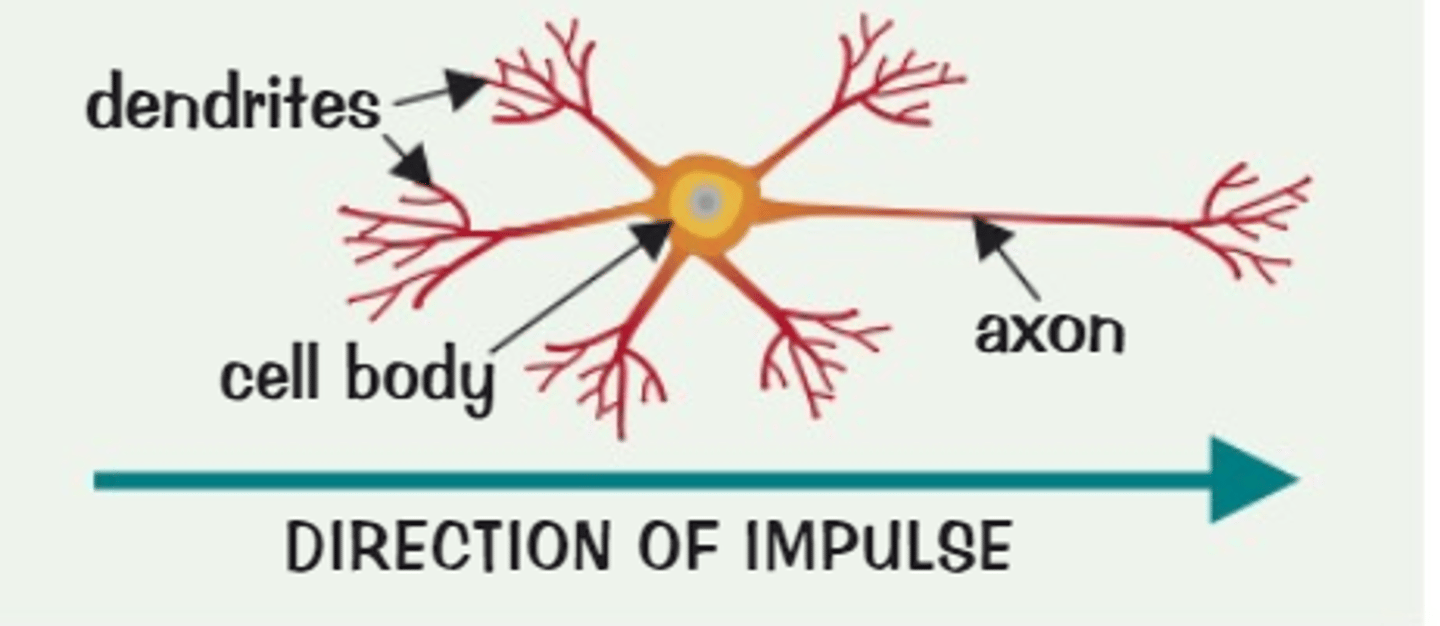
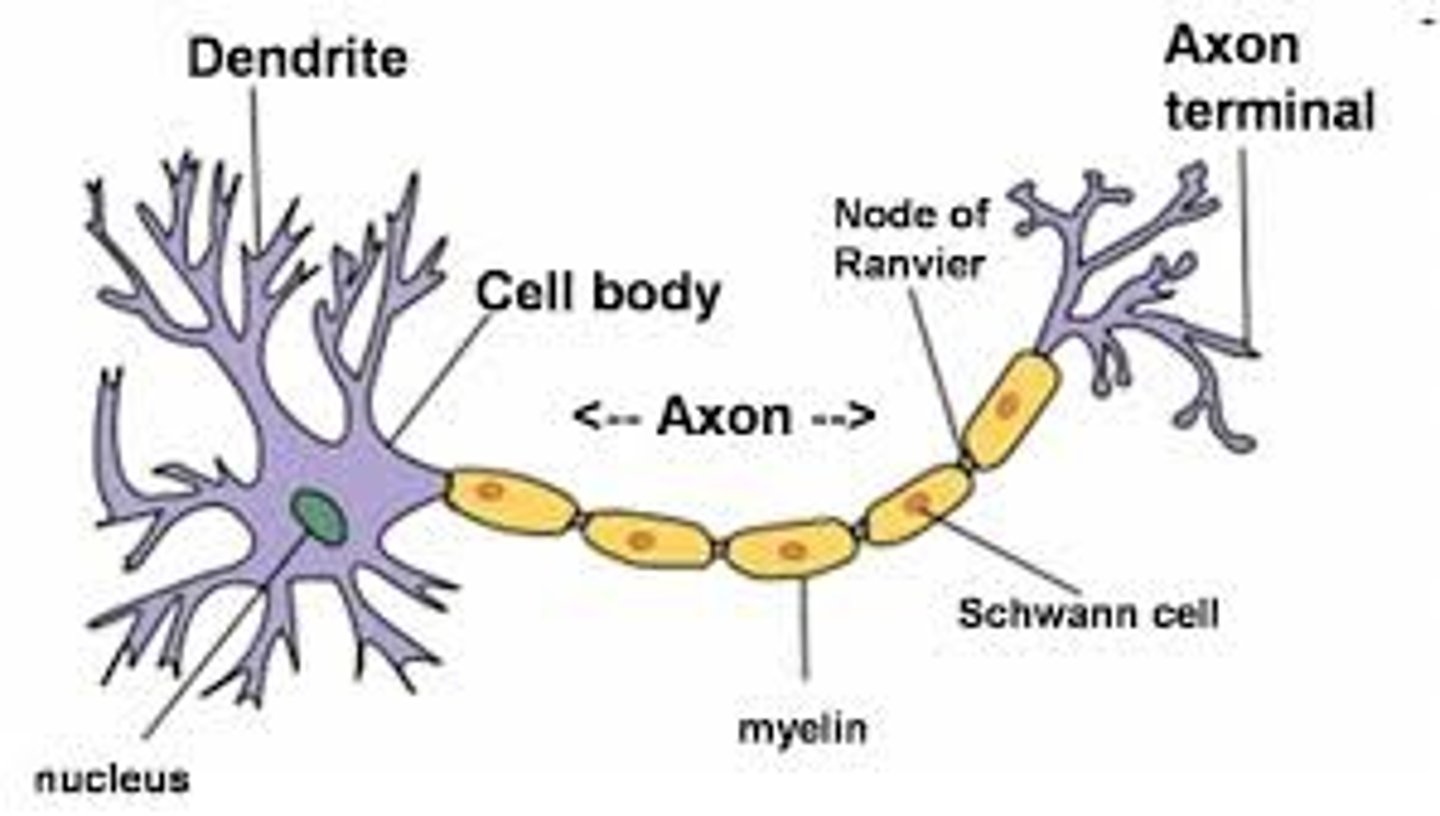
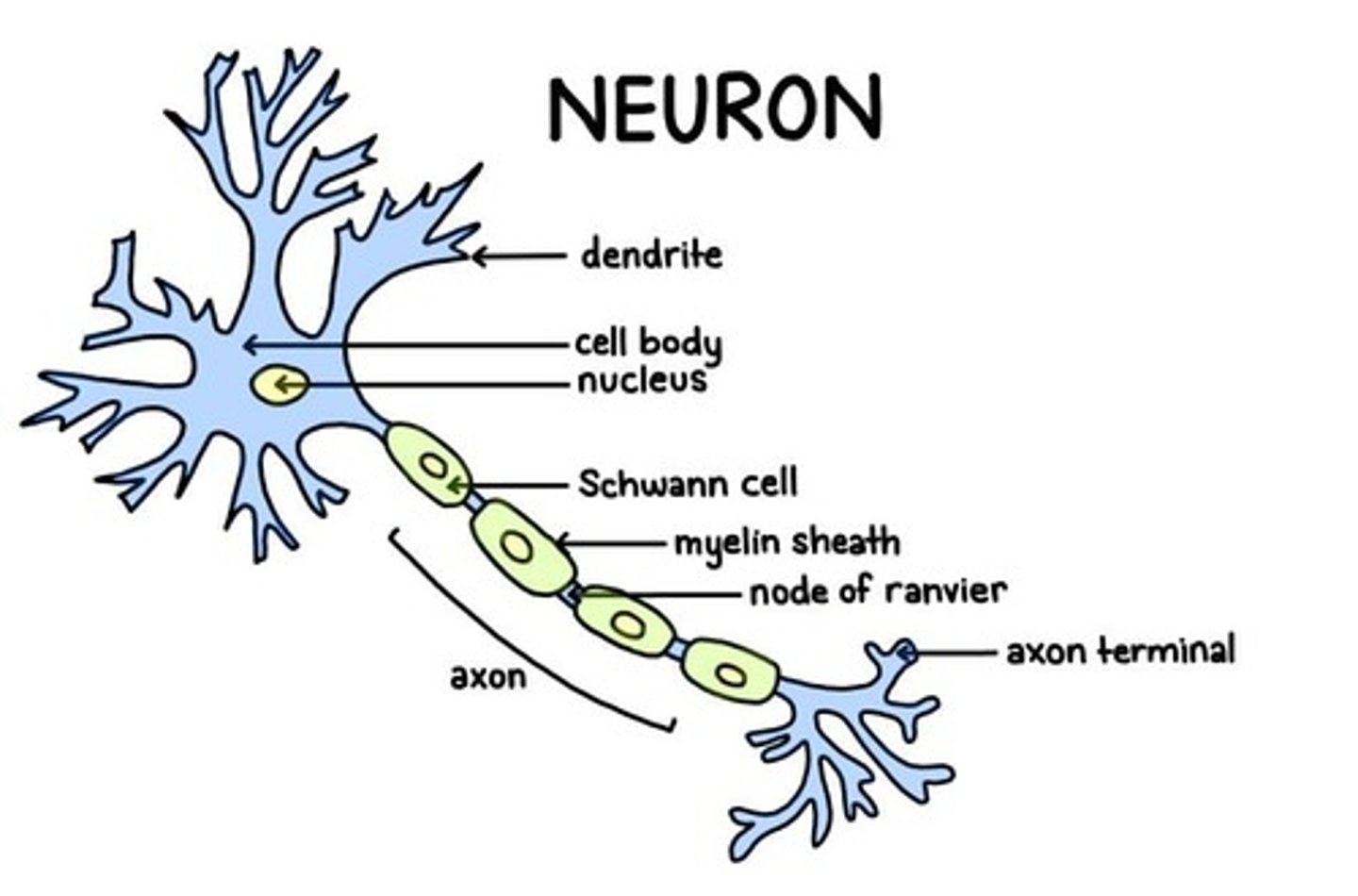
What are neurones?
Nerve cells that transmit electrical impulses quickly through body
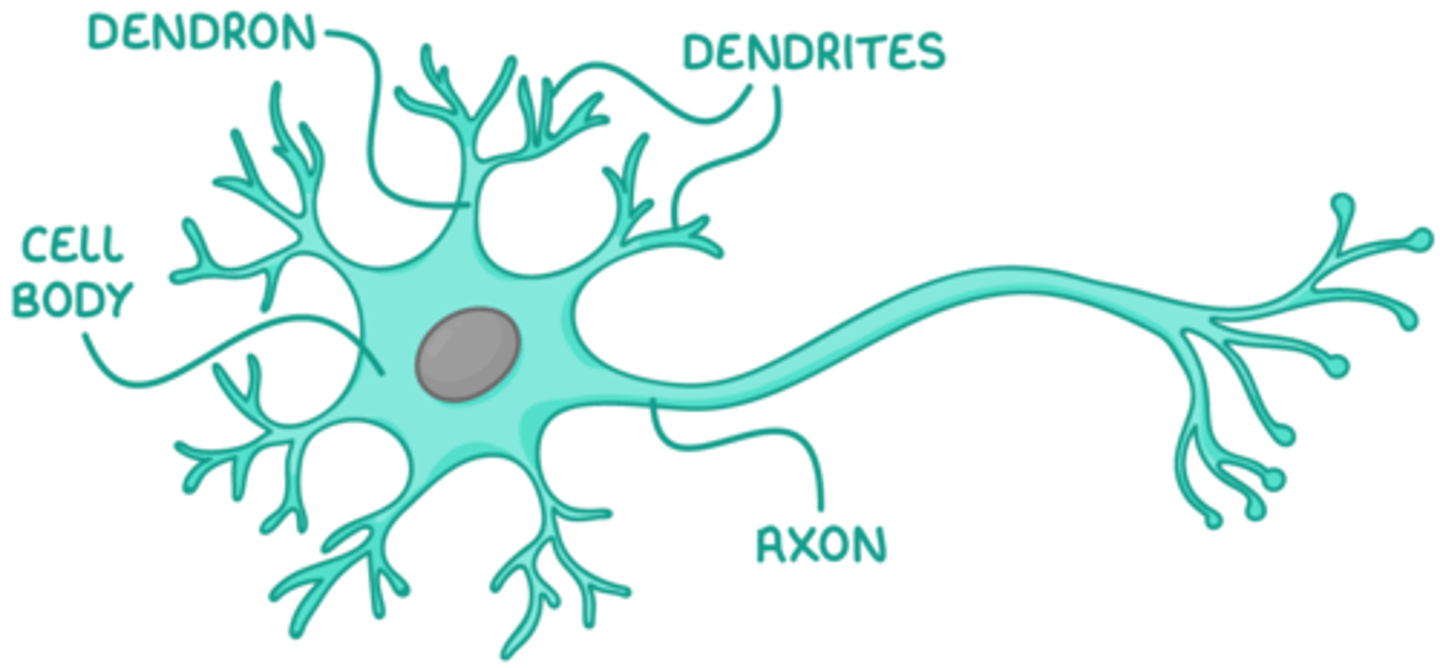
What are the key parts of a neurone? + their function
- Cell body = produces neurotransmitters
- Dendrons = carries impulses toward cell body
- Axon = carries impulses away from cell body
Structures in cell body
Nucleus, cytoplasm, lots of endoplasmic reticulum, mitochondria
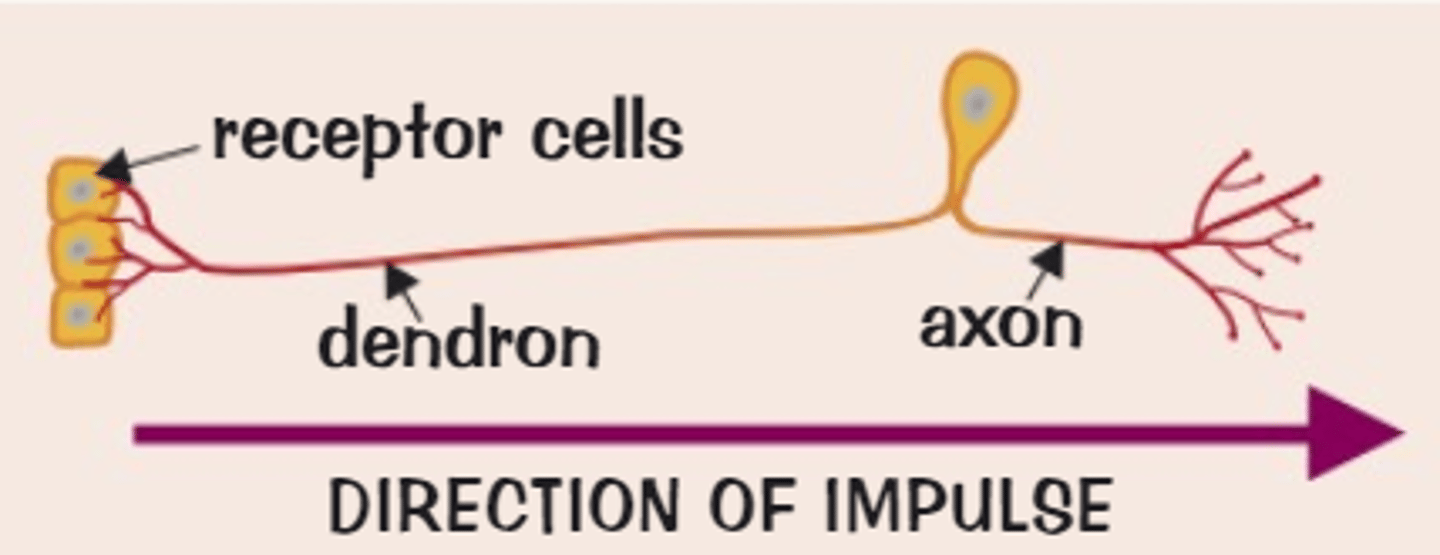
Sensory neurone: Structure + Function
- Carries impulses from sensory receptors to the CNS
- Has an axon and dendron which lead into smaller dendrites
Relay neurone: Structure + Function
- Carries impulses through CNS
- Connects sensory and motor neurones
- Many short axons and dendrites
Motor neurone: Structure + Function
- Carries impulses from CNS to effectors
- Long axon (longer than sensory neurone)
- No dendrons but has dendrites
- Cell body in CNS at end of neurone
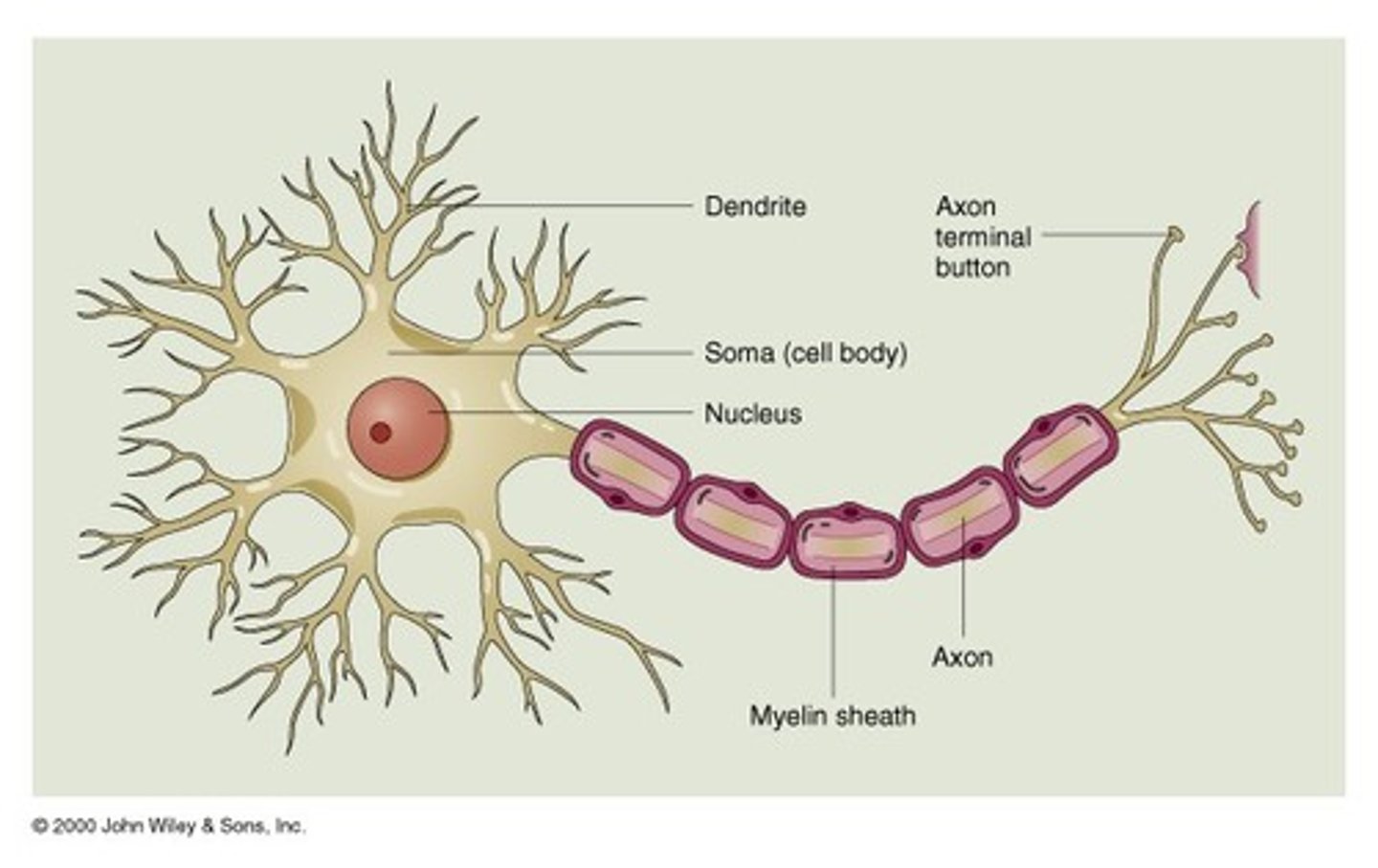
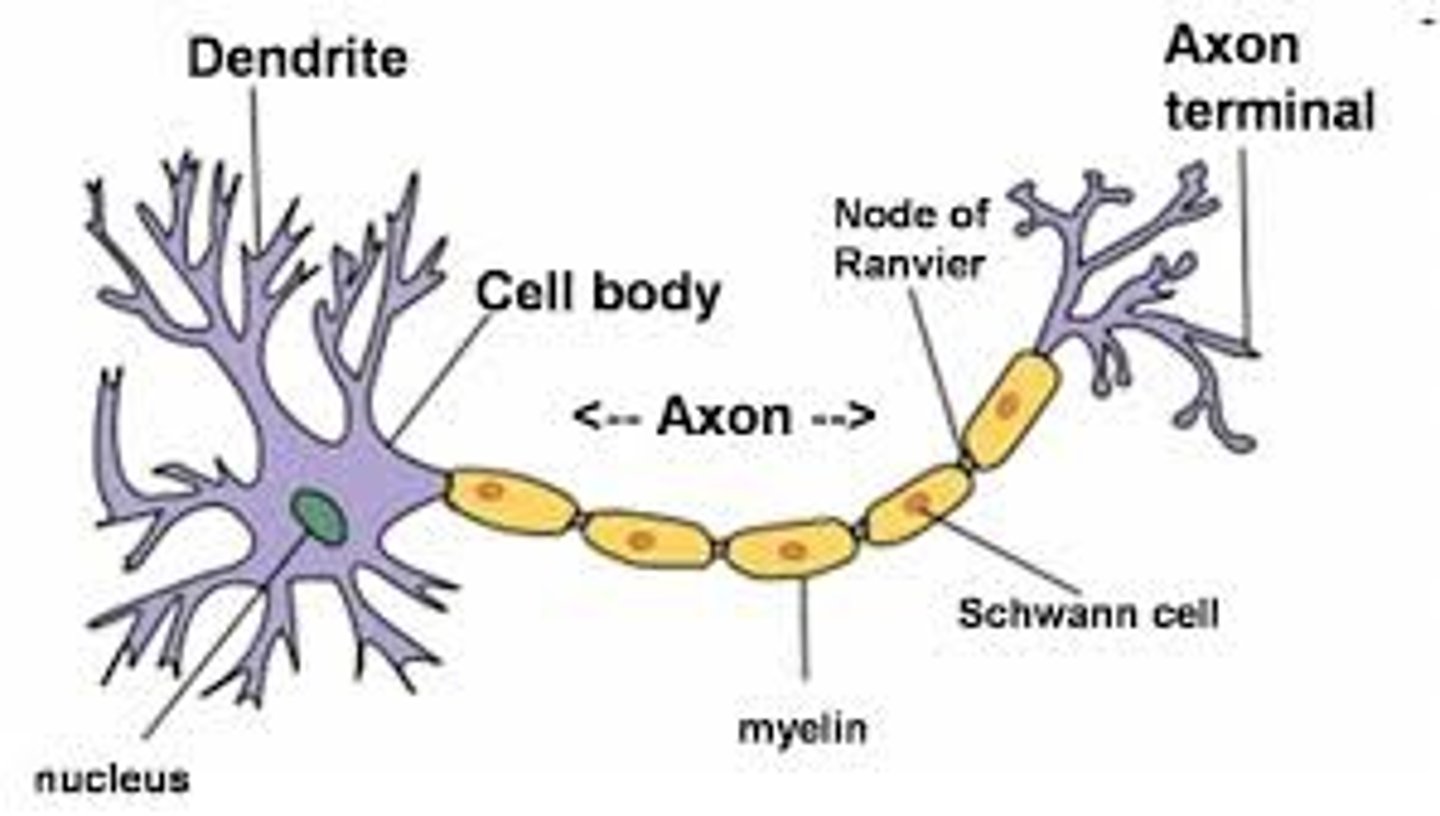
Myelinated neurones
Neurones that have axons covered in myelin sheaths
What makes up the myelin sheath?
- Schwann cells which grow around the axon, forming layers of membrane
- Sheath acts as insulator that prevents movement of ions
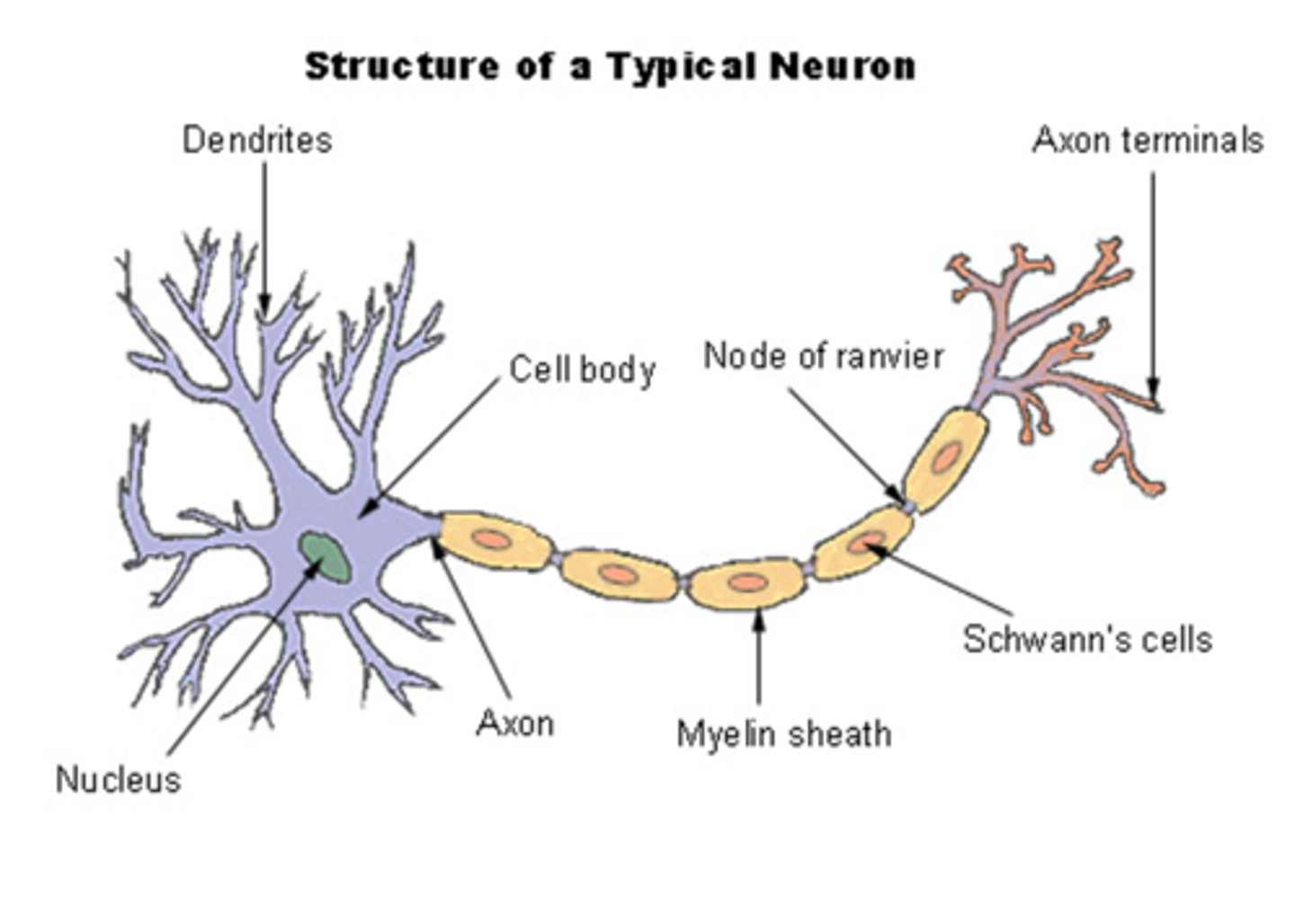
What are the nodes of ranvier?
Gaps in the myelin sheath
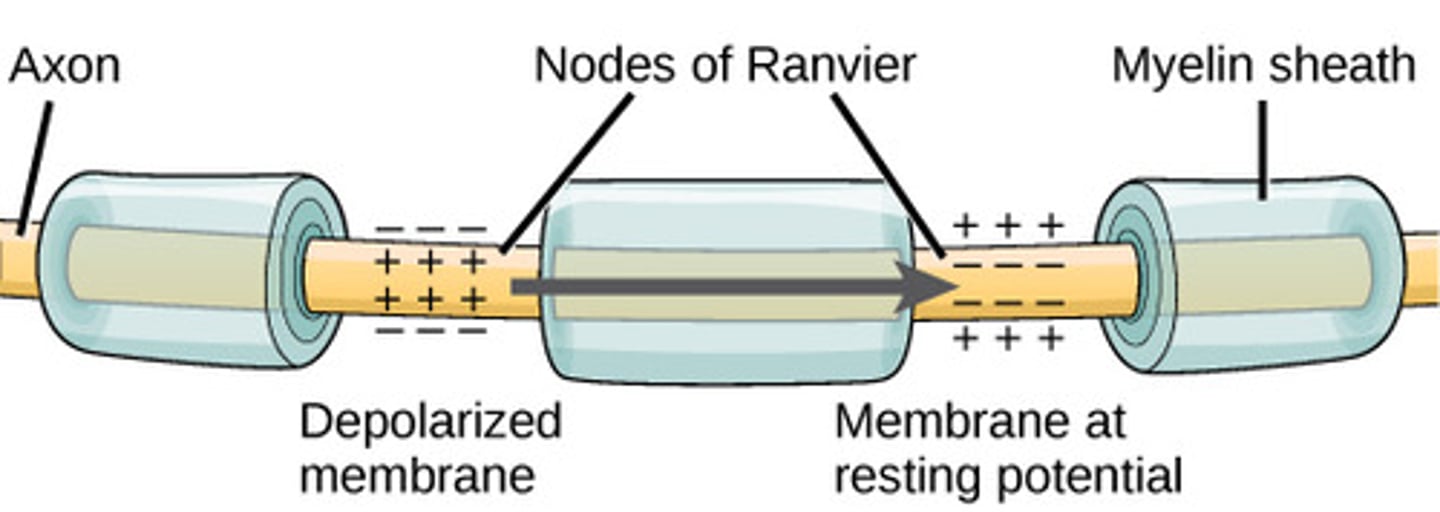
How do myelinated neurones conduct impulses?
Saltatory conduction
- Membrane can only be depolarised at the nodes of Ranvier
- This creates a longer localised circuit
- increasing rate of transmission
Sensory receptors
Specialised cells that detect stimuli from the environment
Types of receptor cells
- Mechanoreceptors (pressure/movement)
- Thermoreceptors (temperature)
- Chemoreceptors (chemicals)
- Photoreceptors (light)
What is a transducer?
Convert energy from one form to another
Eg; receptors convert stimulus energy into electrical impulse

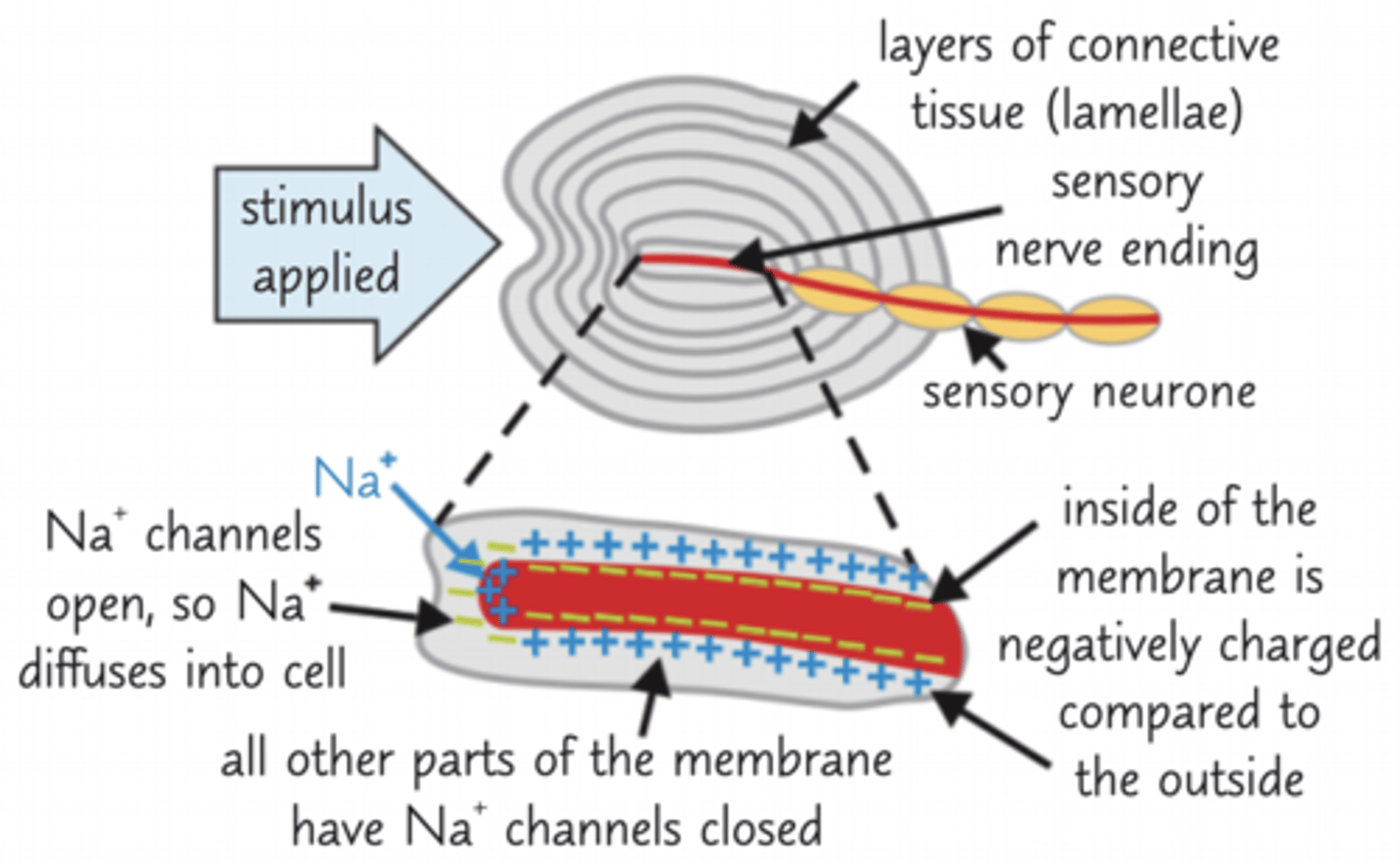
What is a Pacinian Corpuscle?
Nerve endings in the skin (pressure receptors)
How does a Pacinian Corpuscle work?
- Pressure (stimulus) stretches membrane
- This creates gaps between phospholipids
- Stretch-mediated Na+ channels open
- Na+ diffuses into sensory neurone along electrochemical gradient
- This generates an action potential
Why is the rate of transmission slower in non-myelinated neurones?
No nodes of Ranvier so impulses can't jump, making transmission much slower
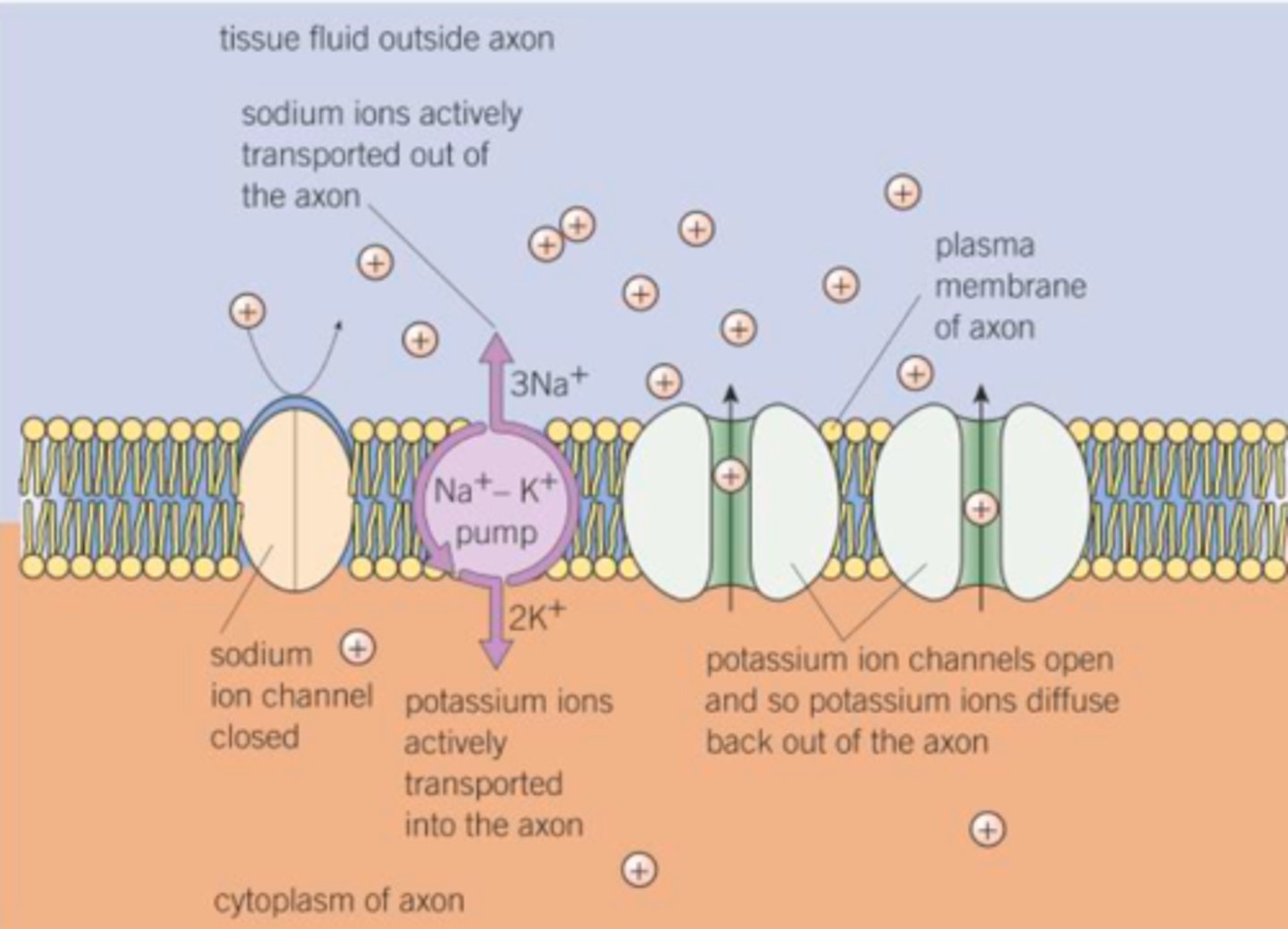
Resting potential
Potential difference across a neurone's membrane (-70mV)
How is resting potential established?
- 3 Na+ ions actively transported out of axon
- 2K+ ions are actively transported into axon
- Via Na-K pump
- Some K+ diffuses out down the electrochemical gradient (membrane is more permeable to K+)
- Na+ channel is closed
Action potential
nerve impulse
How is an action potential established?
- Membrane is at resting potential
- Voltage-gated Na+ channels open, so more Na+ flows into the axon making the inside less negative
- Depolarisation - if threshold potential (-55 mV) is reached, more Na+ channels open causing an influx of Na+
- Repolarisation - At +30 mV, Na+ channels close and K+ channels open, so K+ flows out of the axon
- Hyperpolarisation - excess of K+ leaves the axon, dropping the potential below the -70 mV resting level
- Refractory period - Na/K pump restores the membrane back to the resting potential.
What is the all or nothing principle?
Reaching the threshold potential always triggers a uniform action potential
What affects frequency of action potential?
A stronger stimulus
Why is refractory period useful?
- Ensures action potentials don't overlap
- Limits frequency that impulses are transmitted
- Guarantees impulses travel in only 1 direction
How does refractory period work?
Na+ channels remain closed during repolarisation, preventing depolarisation.
Why do multicellular organisms need communication systems?
- To respond to changes in internal/external environment
- To co-ordinate organ functions
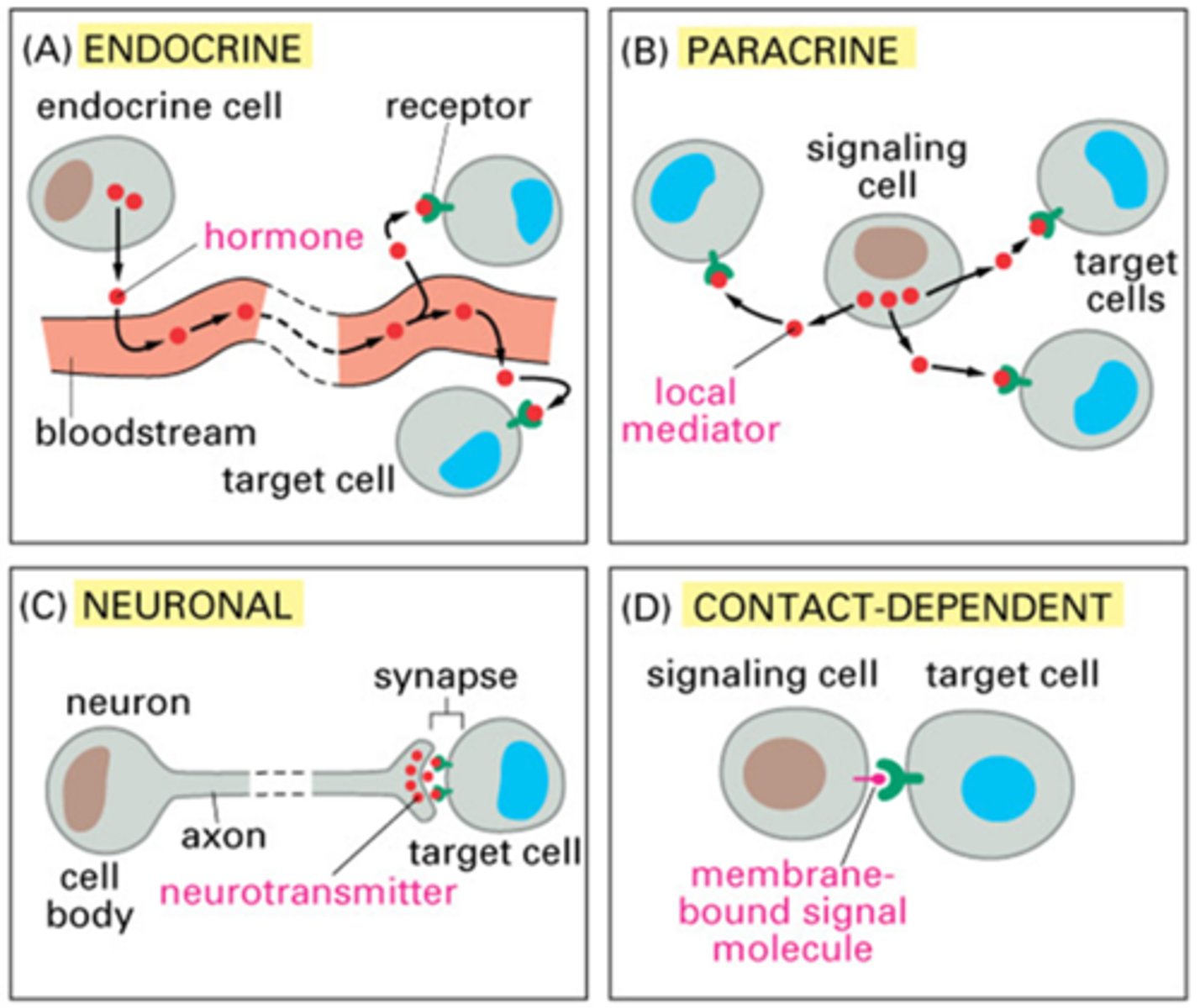
What is cell signalling?
Communication between cells
* Can be hormones (distant cells) or neurones (adjacent cells)
Homeostasis
Maintaining a constant internal environment within set limits of organism
Why is homeostasis important?
- Keeps internal environment constant for metabolism
- Ensures cells function and avoid damage
- Helps organisms adapt to external changes
Role of receptors and effectors (Homeostasis)
* Receptors - detect stimuli and send signals to the brain about changes in the internal environment
* Effectors - muscles/glands that act on signals and cause responses
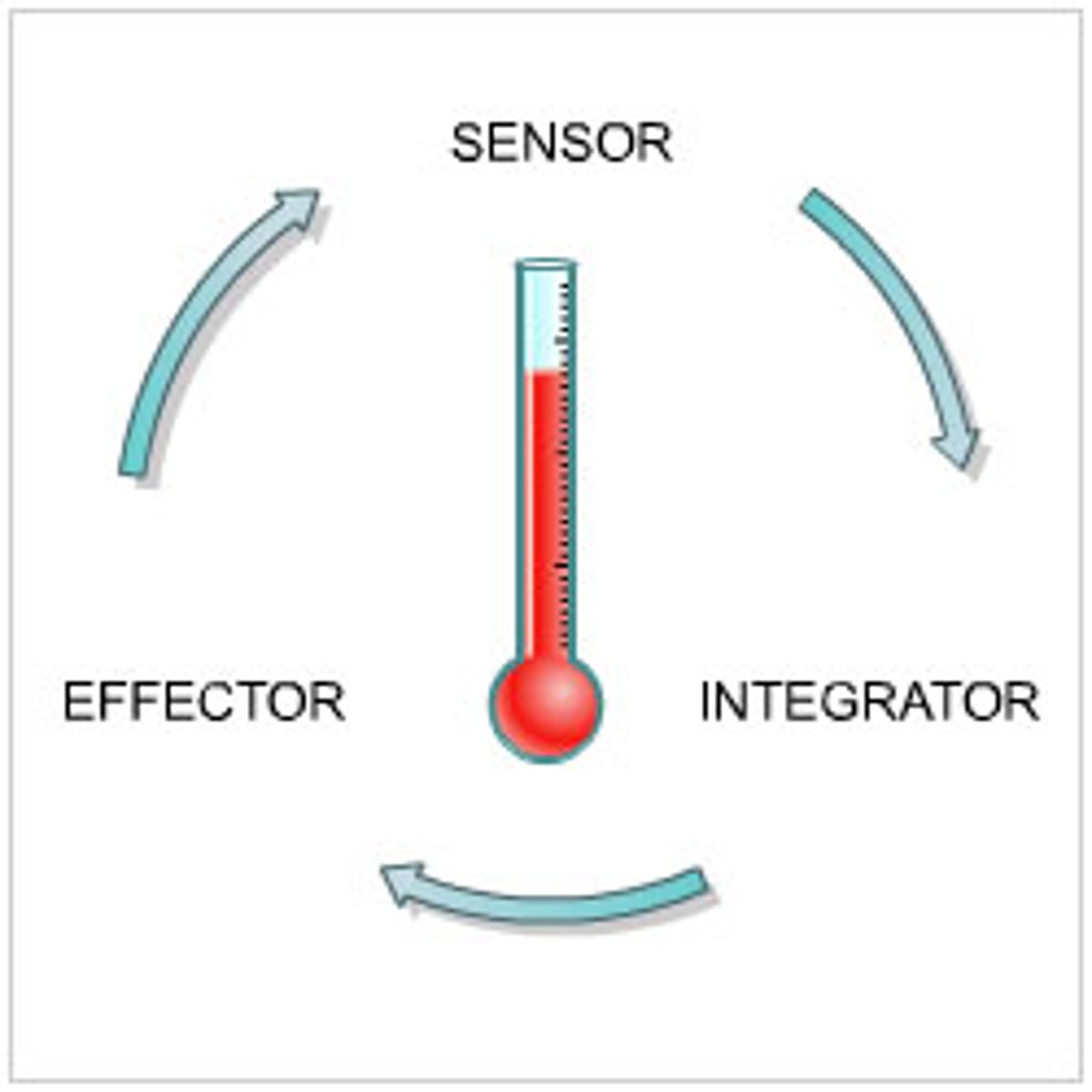
Negative feedback
Process that counteracts change
*Ensures optimum internal conditions are maintained
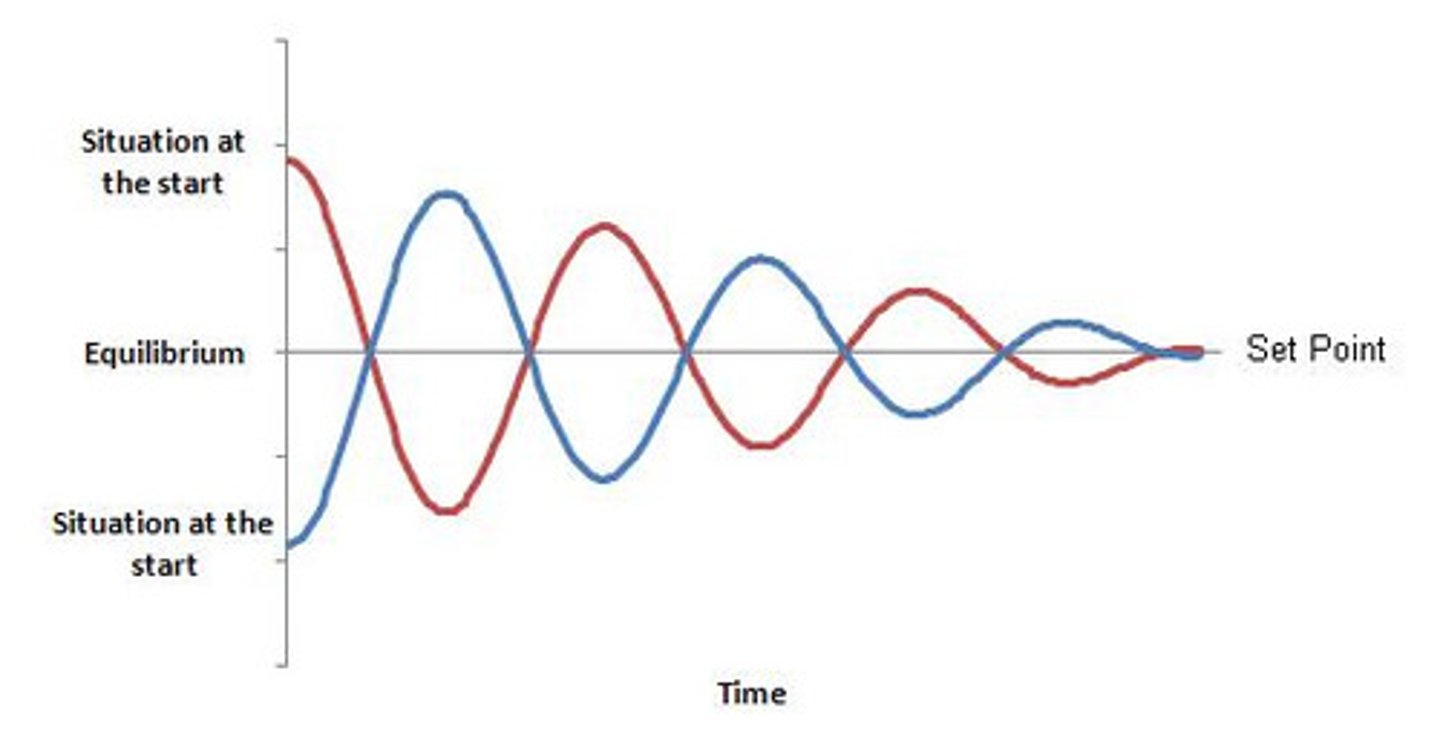
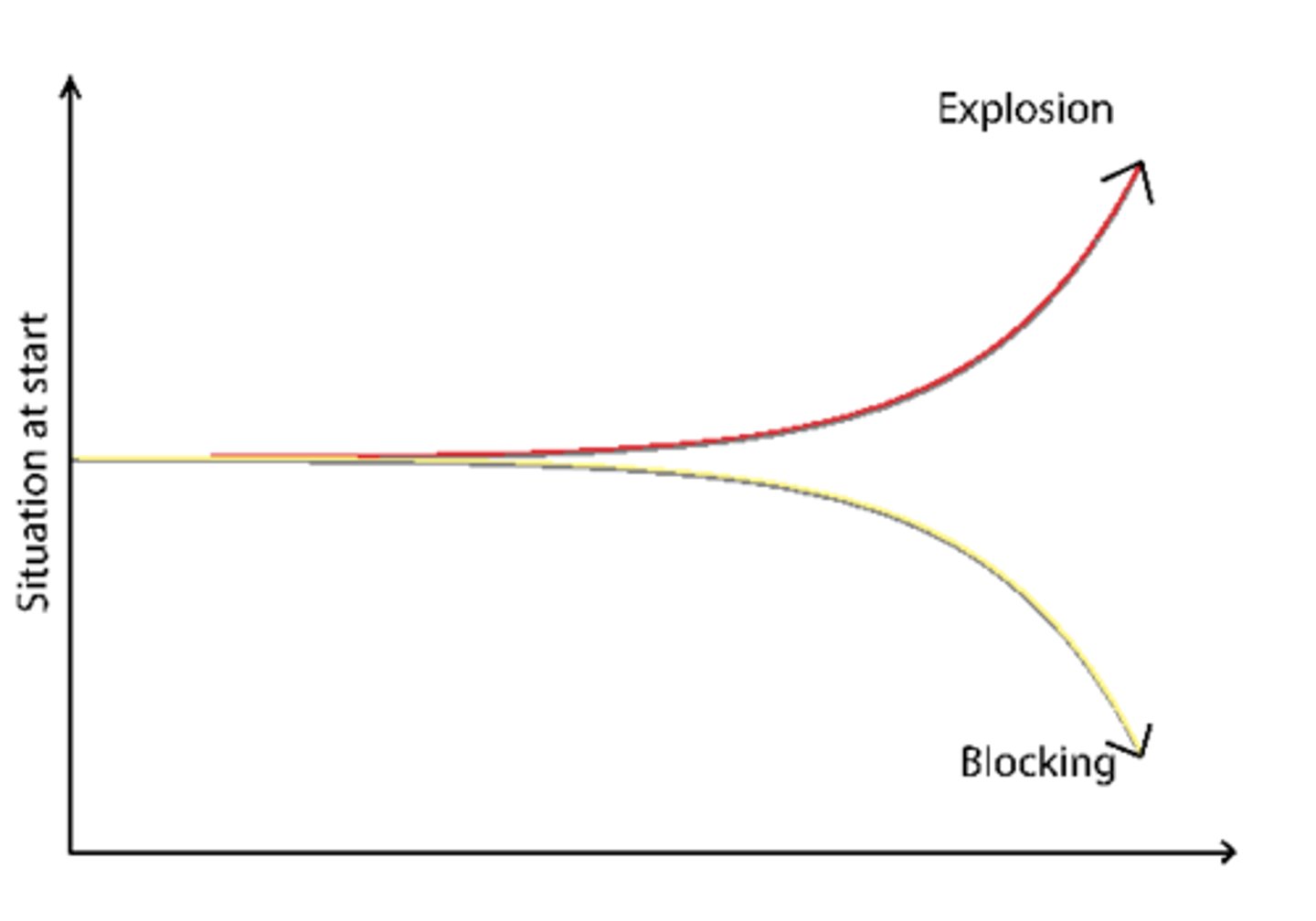
Positive feedback
Process where change is magnifed
- Not used in homeostasis bc doesn't keep environment constant
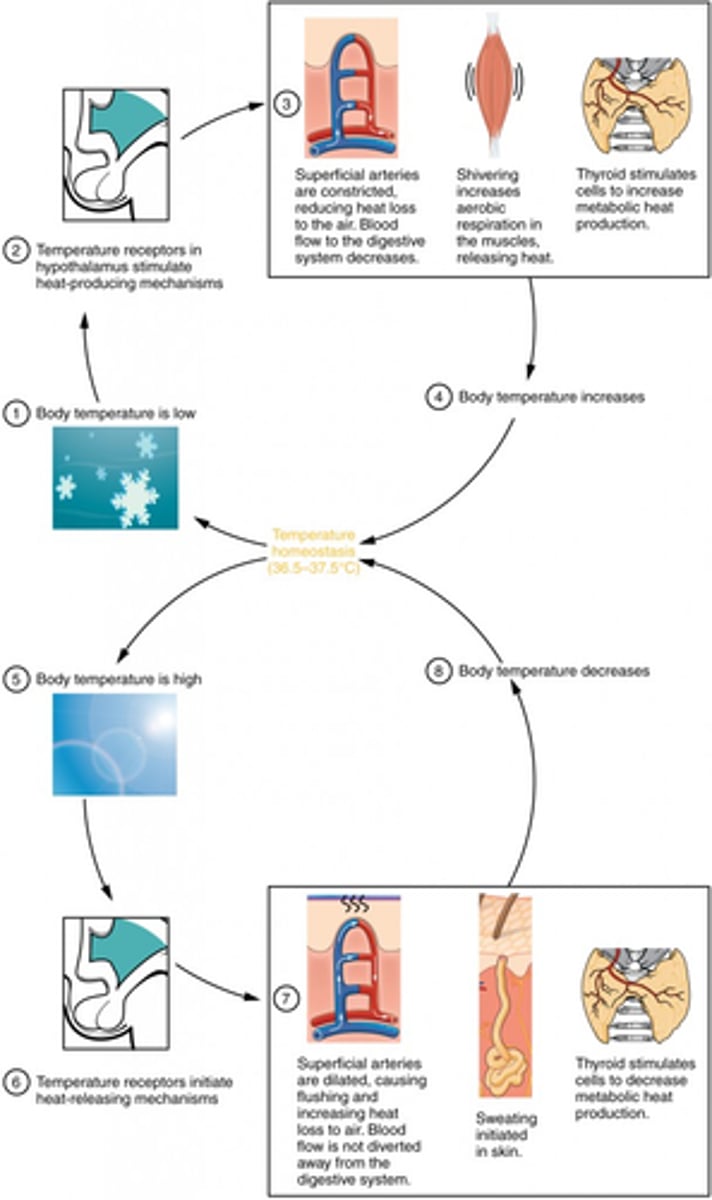
Thermoregulation
Maintaining constant core body temperature

Ectotherm
Animal that can't control its own body temperature (cold blooded)
- Their activity and internal temp depends on the external temperature
- Eg; reptiles, fish

Endotherm
Animal which controls its own body temperature (warm blooded)
- Their activity and internal temp is independent of external temperature
- Eg; mammals, birds

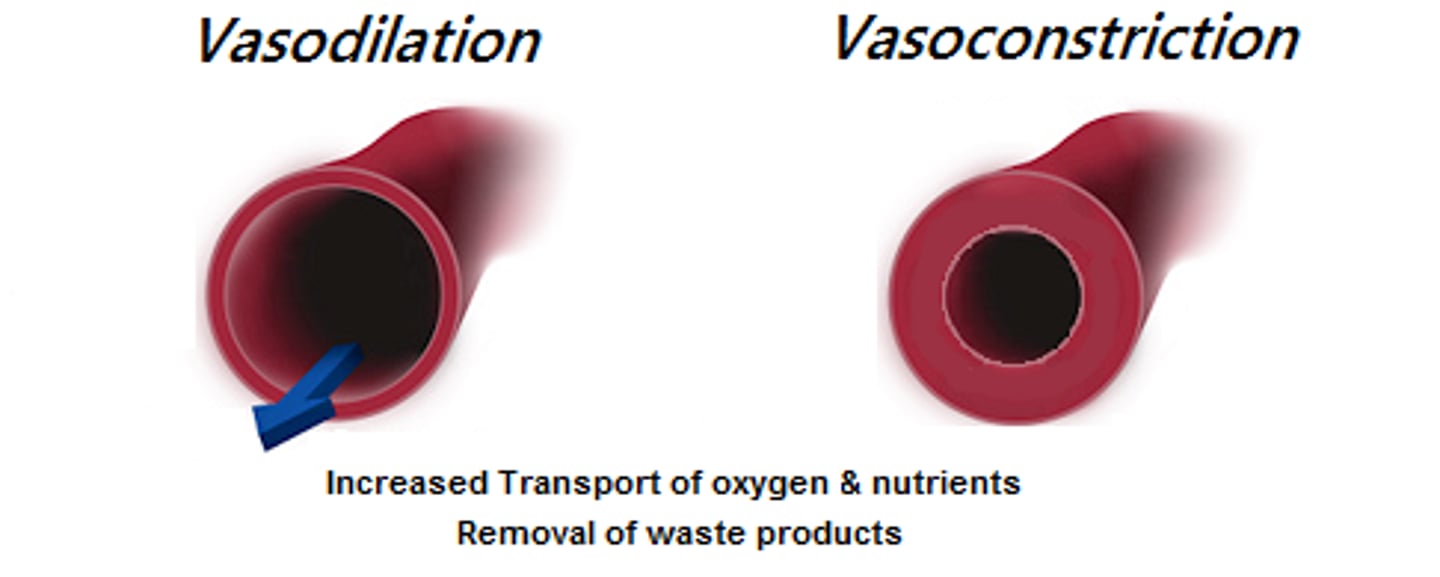
How do mammals increase their body temperature?
- Shivering - skeletal muscles contract
- Hairs stand up - pili muscles contract (traps layer of warm air)
- Vasoconstriction - arterioles constrict
- Releasing adrenaline and thyroxine - speeds up metabolism
How do mammals reduce their body temperature?
- Sweating - sweat evaporates and cools
- Vasodilation - arterioles dilate
- Hairs lie flat - pili muscles relax (less warm air trapped)
Advantages and disadvantages of Ectotherms
A: Need less food (less respiration)
A: More energy used for growth
D: Activity depends on external temperature
D: Can't live in wide range of climates

Advantages and disadvantages of Endotherms
A: Constant temp (maintains enzyme activity)
A: Can live in colder environments
D: Lots of energy used to maintain body temp
D: More food required

Role of the Hypothalamus (thermoregulation)
- Hypothalamus receives info about body temperature from thermoreceptors
- Hypothalamus receptors = detects internal temp
- Skin receptors = detects external temp
- Hypothalamus sends signals to effectors
- Effectors respond to restore optimum temp
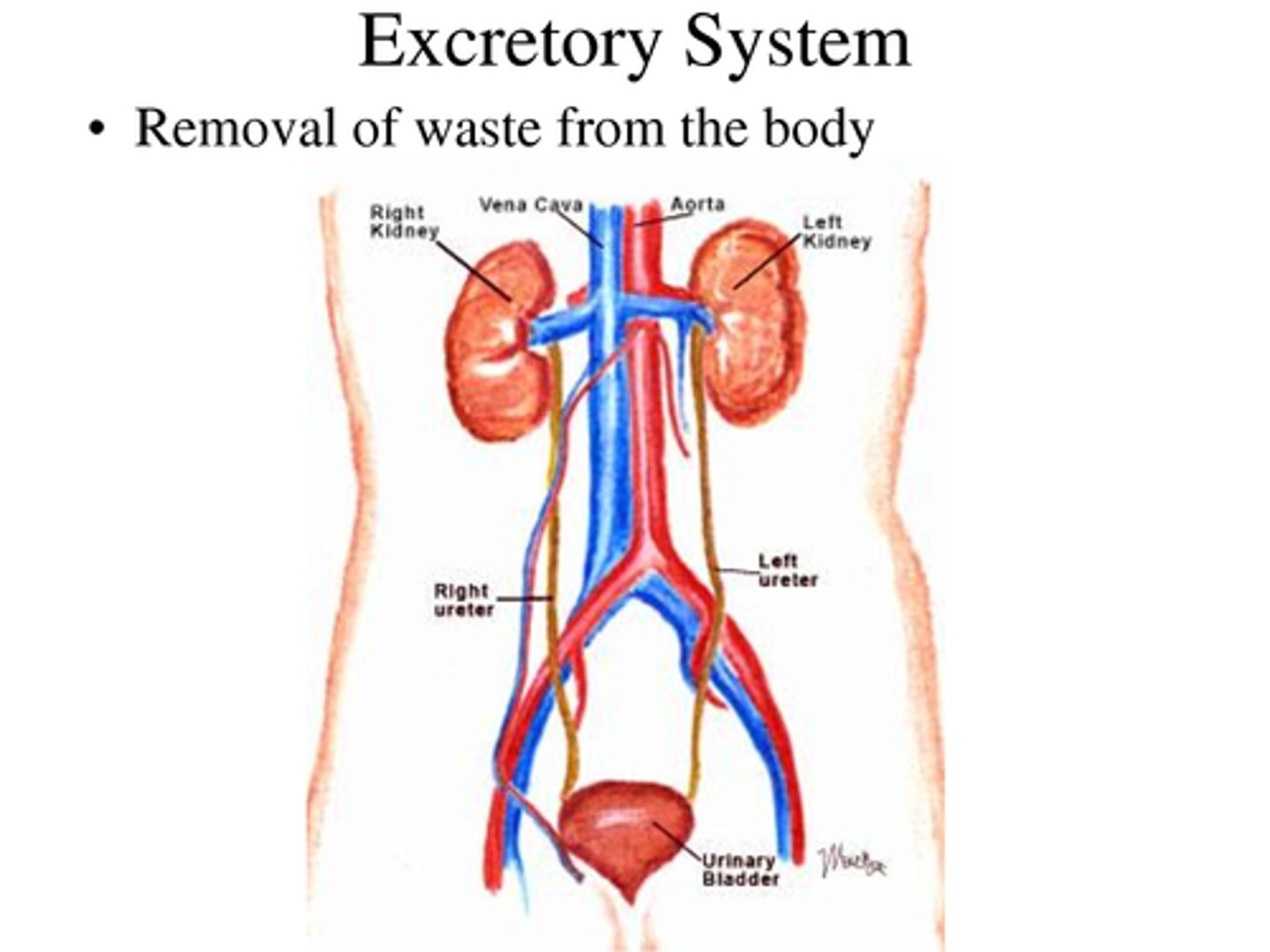
Excretion
Removing metabolic waste from cells
How does the liver break down amino acids?
1) Deamination: amine groups are removed (producing toxic ammonia and organic acids)
2) Organic acids are used to produce ATP or stored as glycogen
3) Ammonia reacts with CO₂ to form urea via the ornithine cycle
4) Urea is excreted from liver + enters the blood
5) Urea is filtered out the body via the kidneys in urine
What other substances does the liver detoxify?
* Alcohol - alcohol dehydrogenase converts ethanol to ethanal
* Hydrogen peroxide - catalase breaks it into O₂ and H₂O
* Paracetamol - broken down to prevent toxicity
* Insulin - metabolised to regulate blood glucose concentration
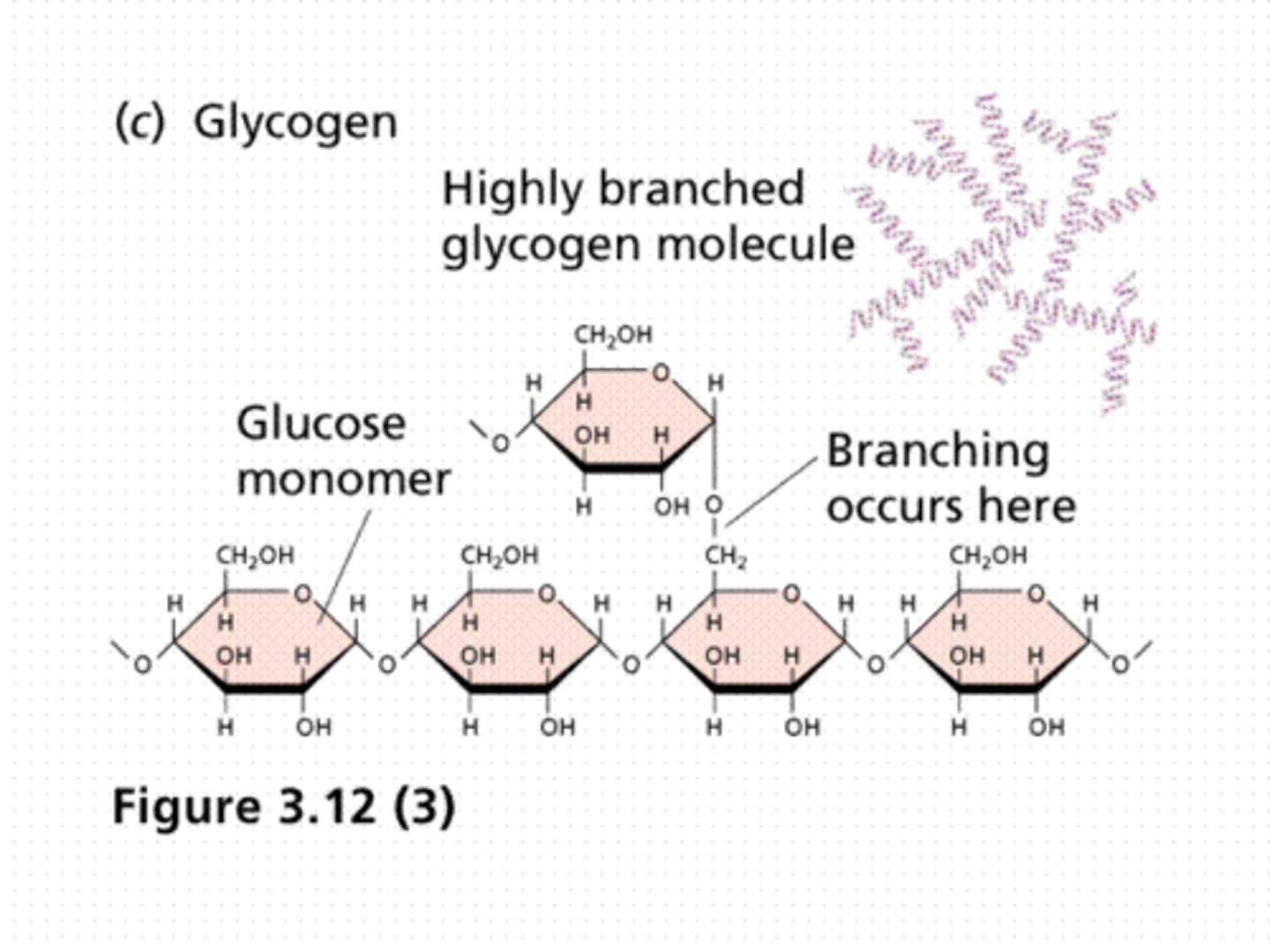
How does the liver help regulate blood glucose levels?
- Converts excess glucose into glycogen - for storage (when levels are high)
- Releases glucose into the bloodstream by breaking down glycogen (when levels are low)
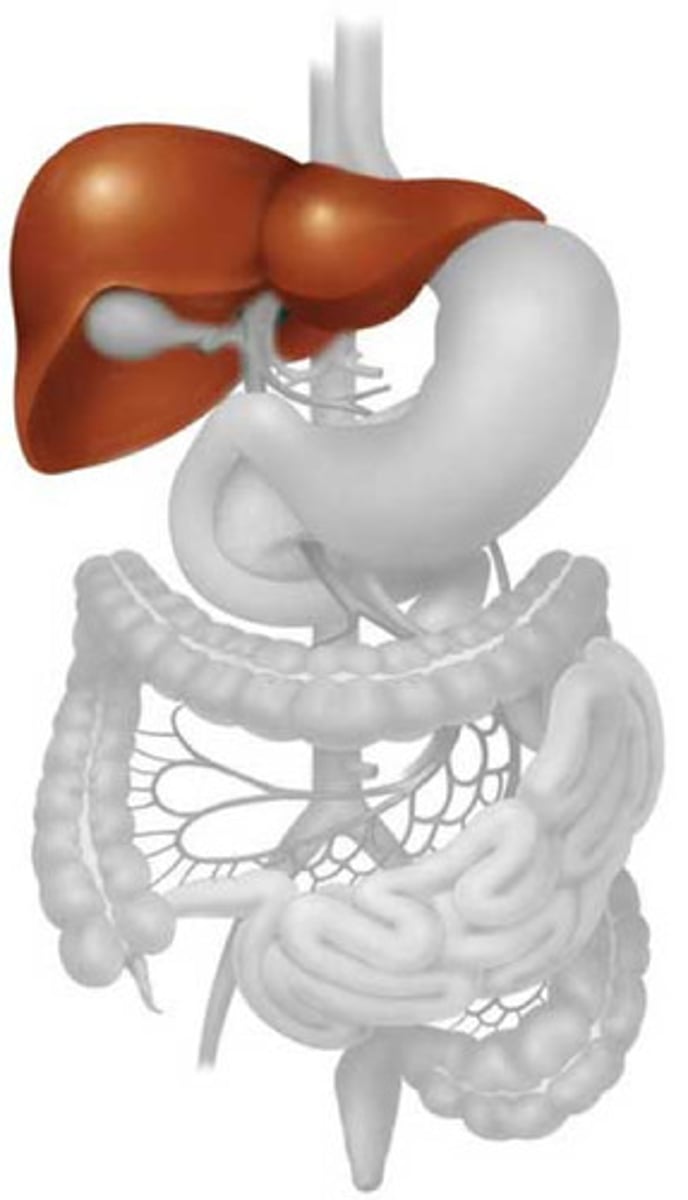
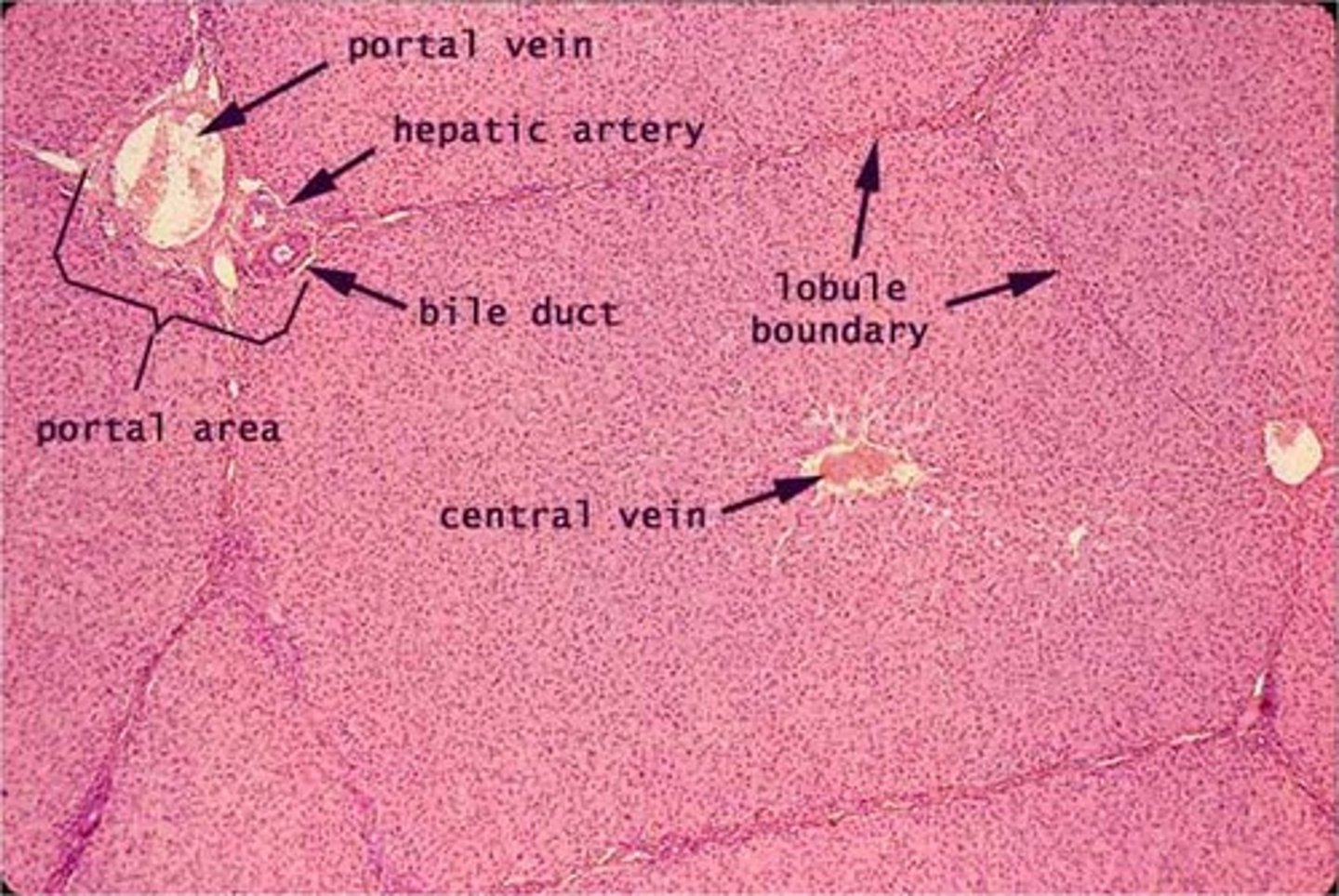
Gross structure of the liver (veins, arteries etc.)
Liver lobules are connected to:
Hepatic artery (supplies oxygenated blood)
Hepatic vein (carries away deoxygenated blood)
Hepatic portal vein (brings nutrient-rich blood from the intestines)
Bile duct (transports bile to gallbladder)
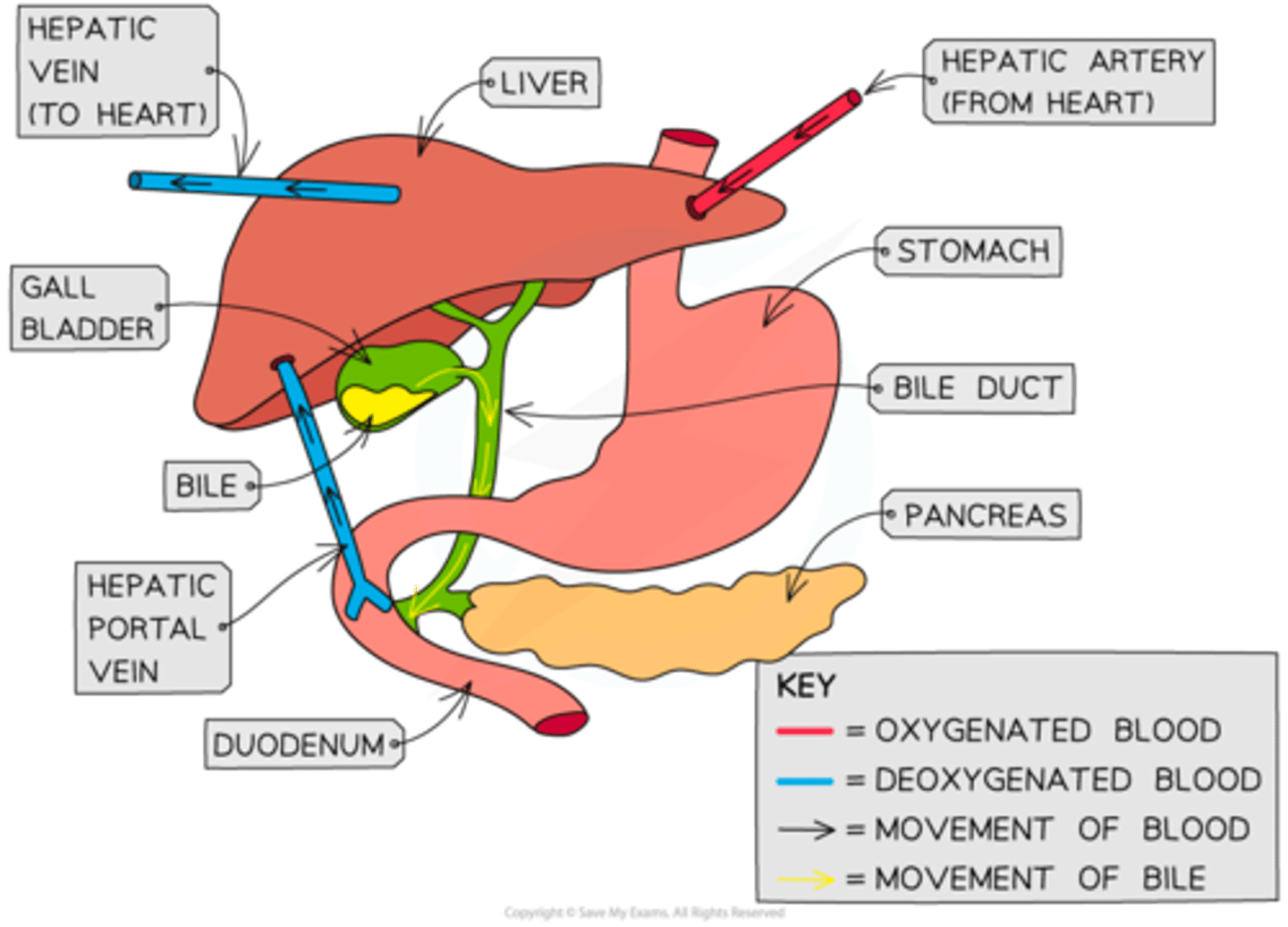
Microscope view of liver
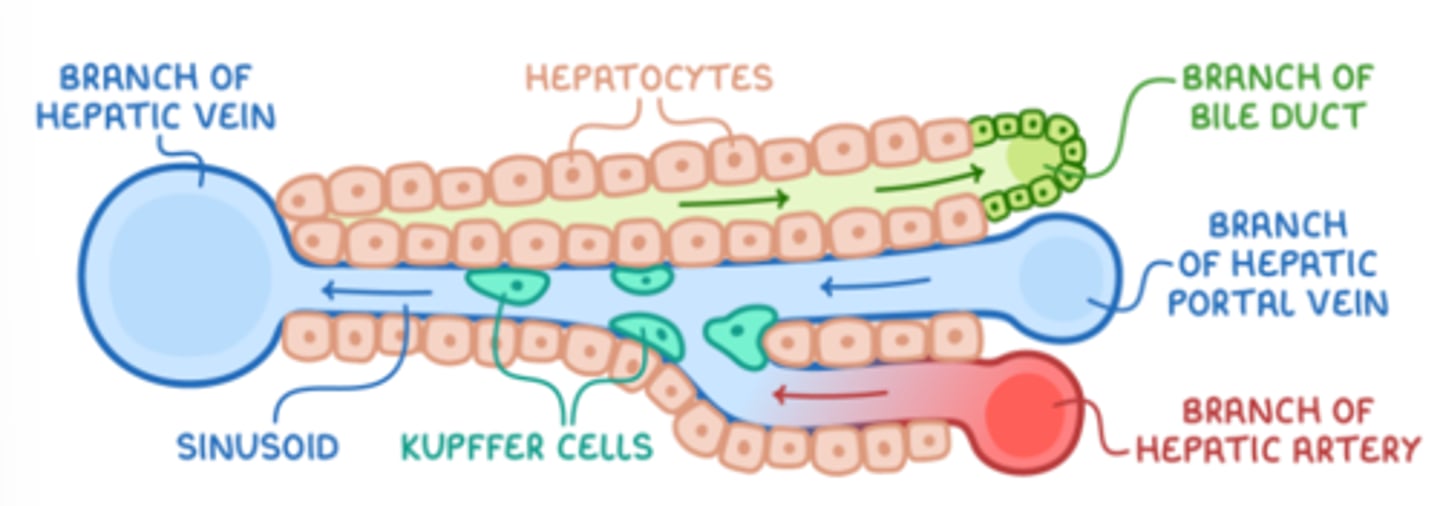
Structure of liver lobules
- Made of hepatocytes
- Has central vein attached to the hepatic vein (to remove deoxygenated blood)
- Sinusoids act as capillaries
- Kupffer cells ingest pathogens (protect against disease)
- Bile canaliculus connects bile duct to central vein
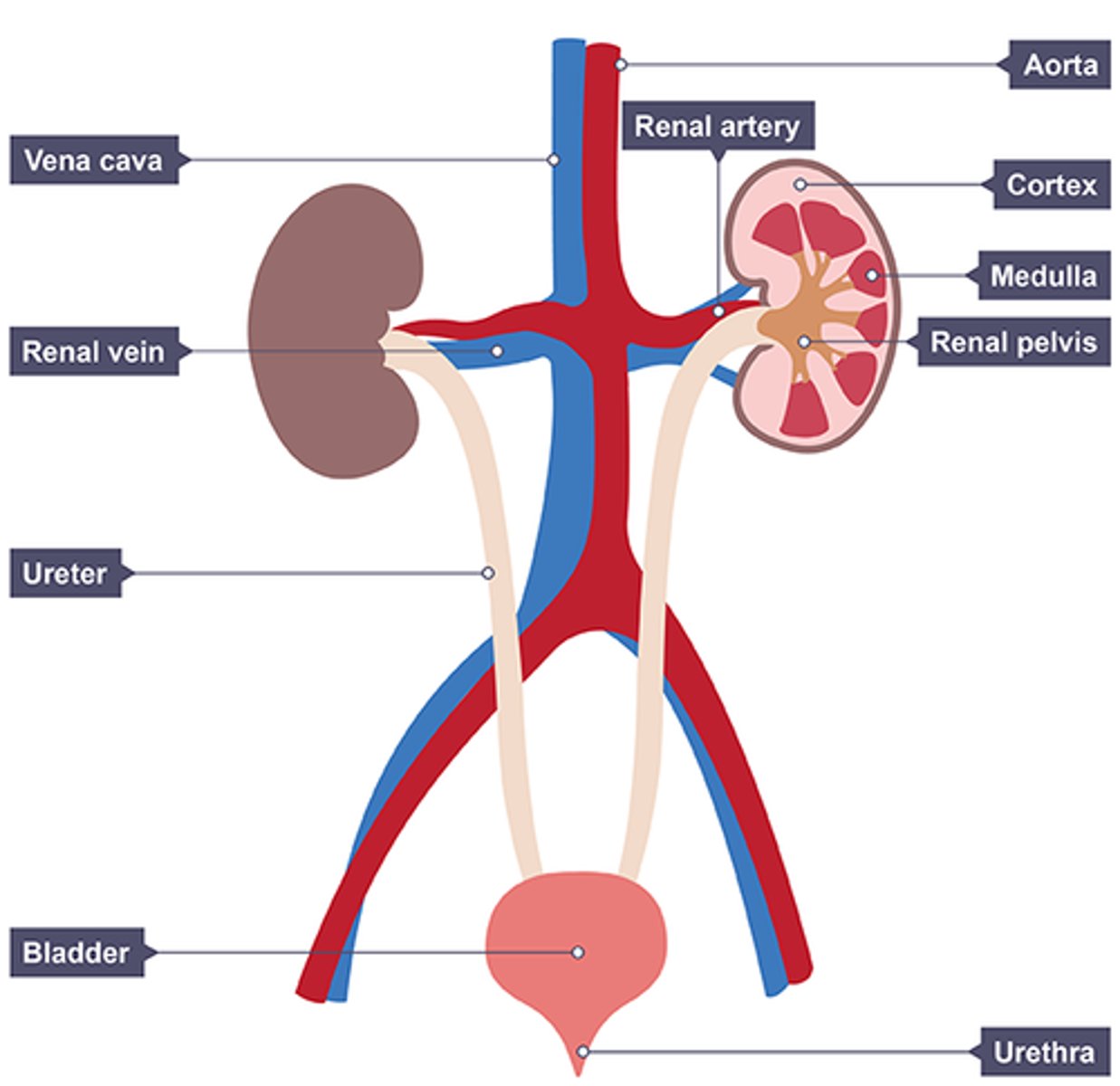
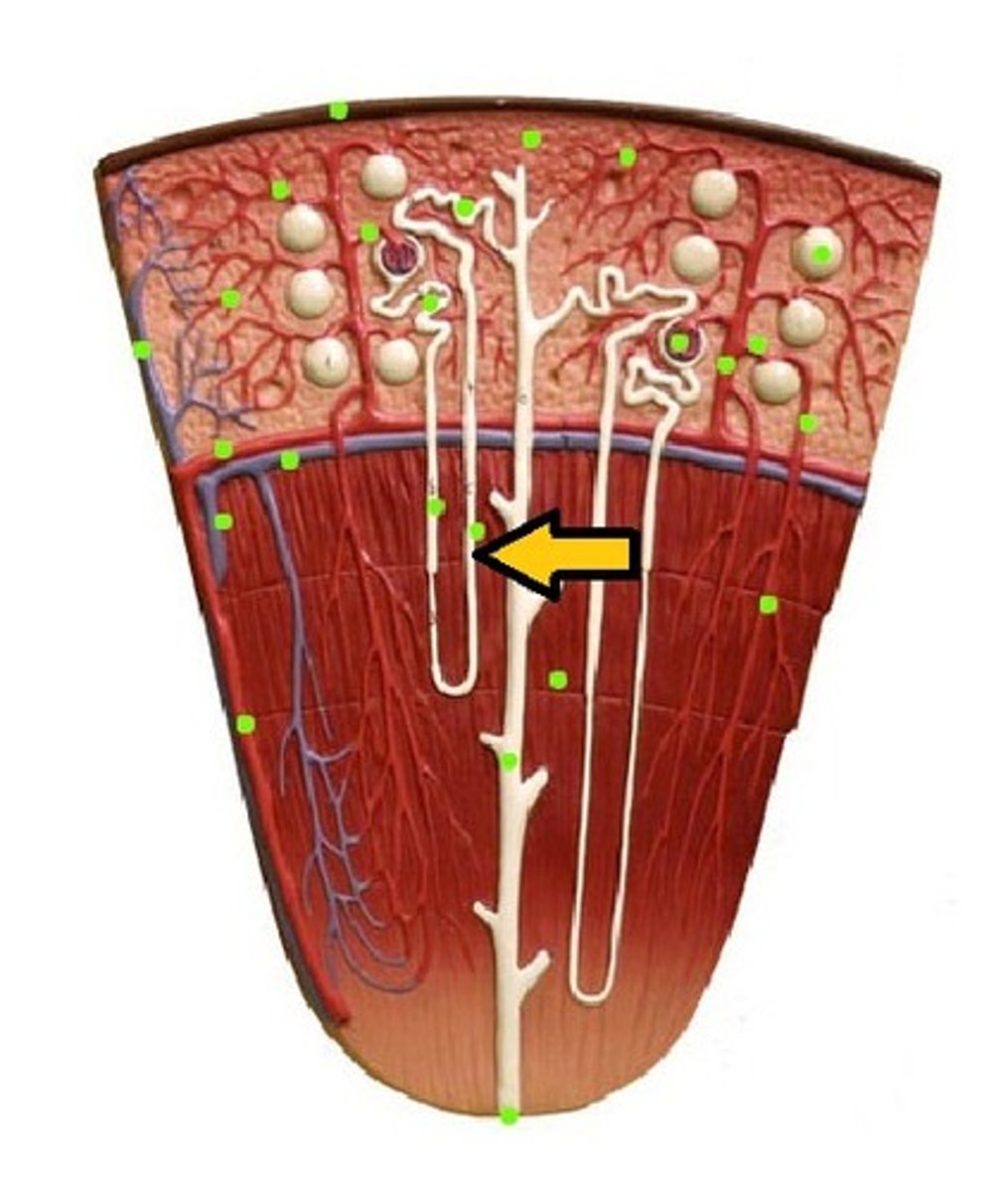
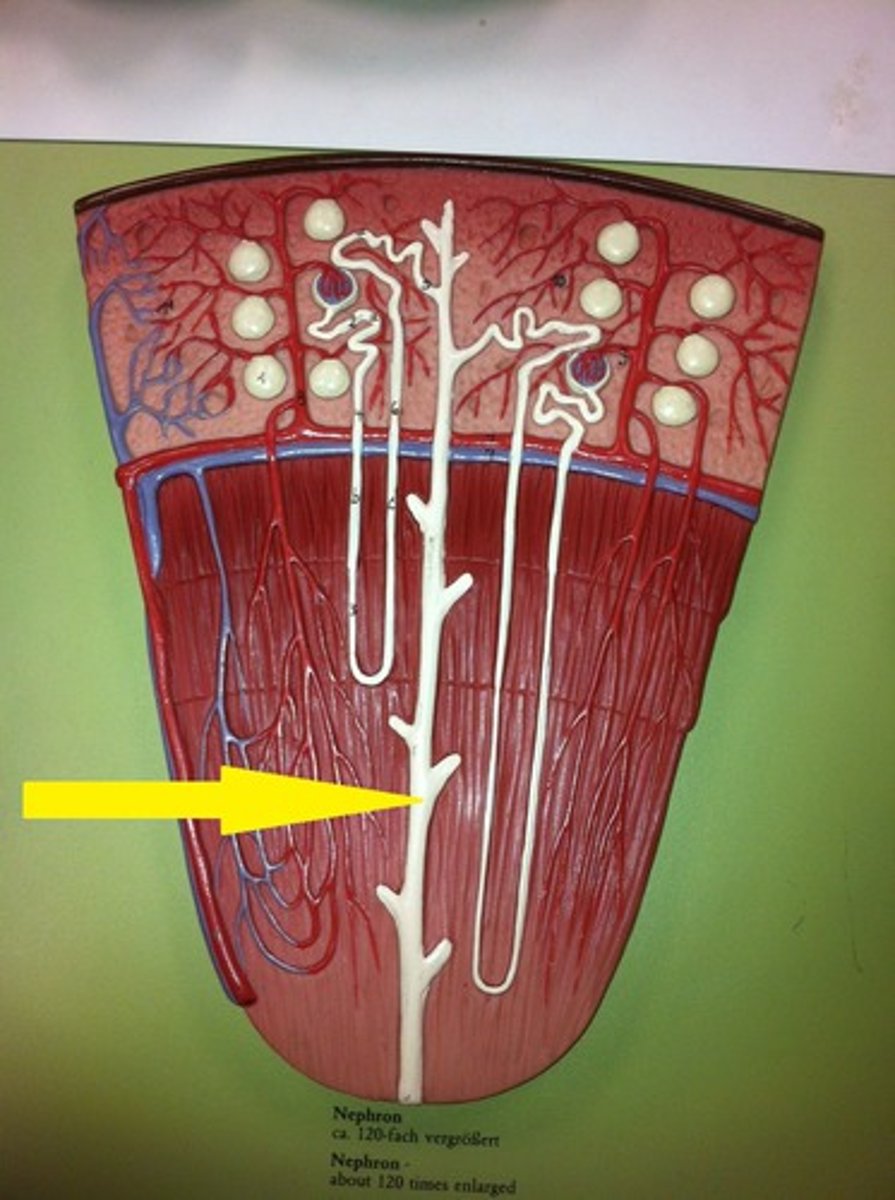
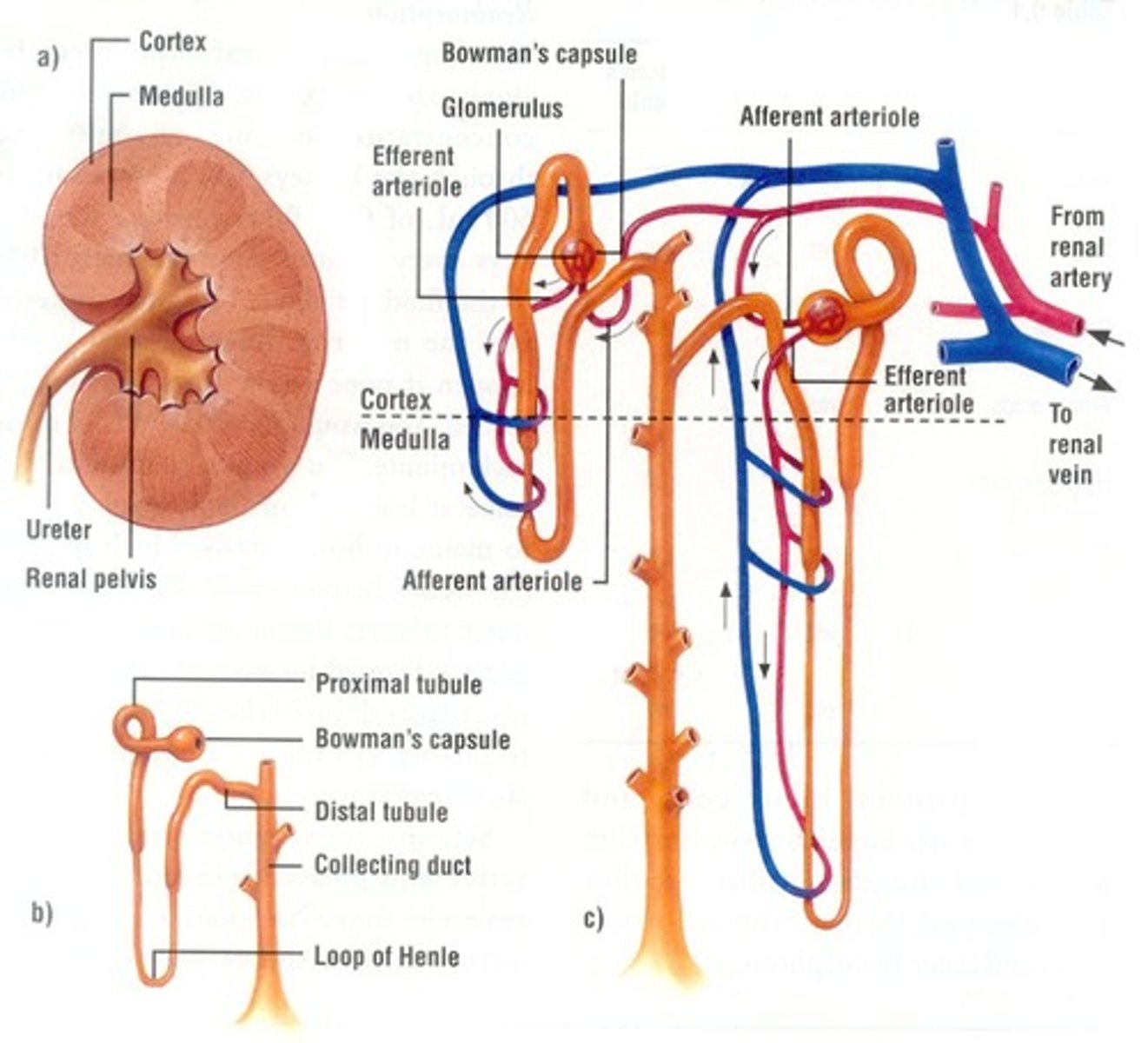
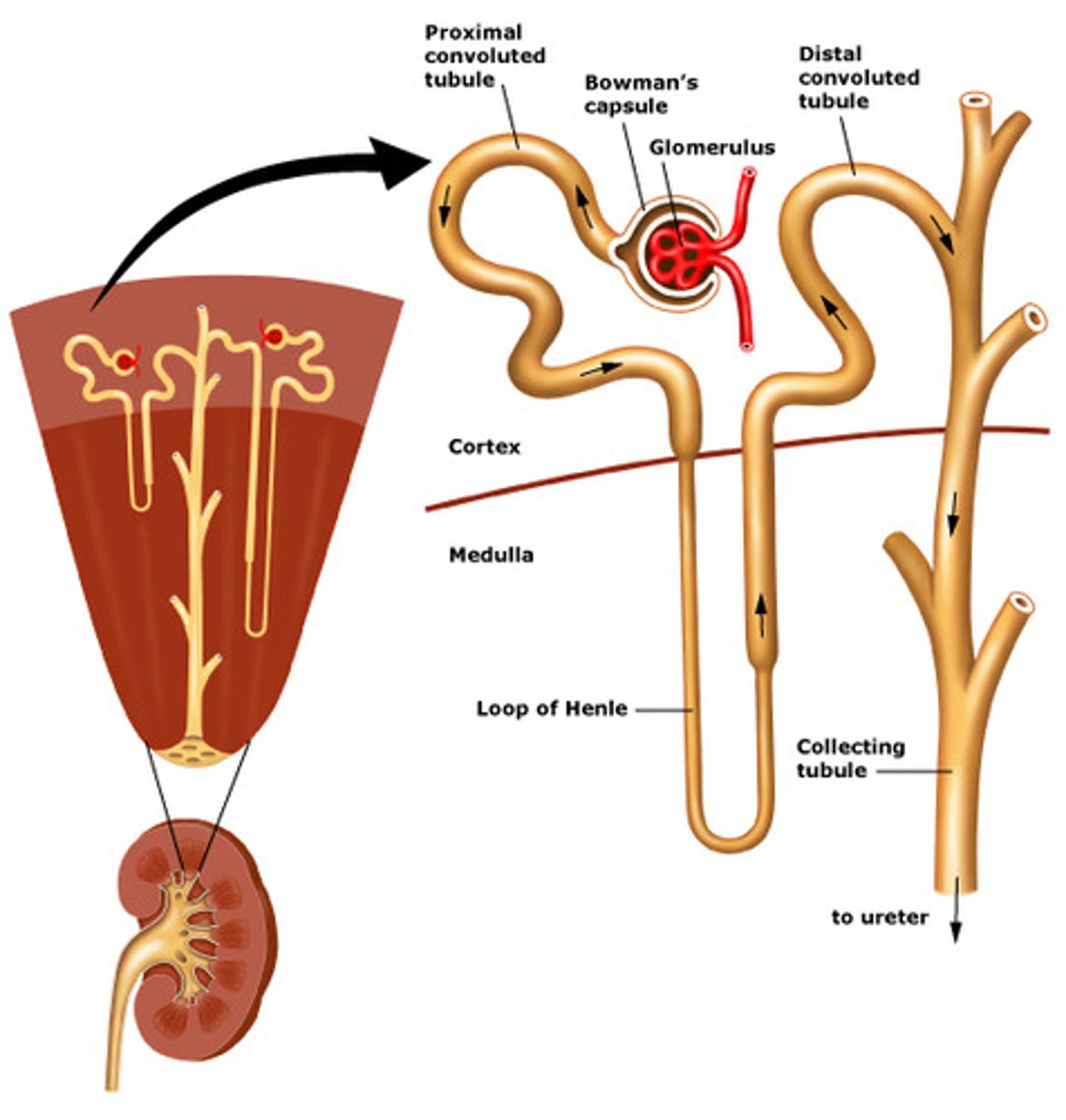
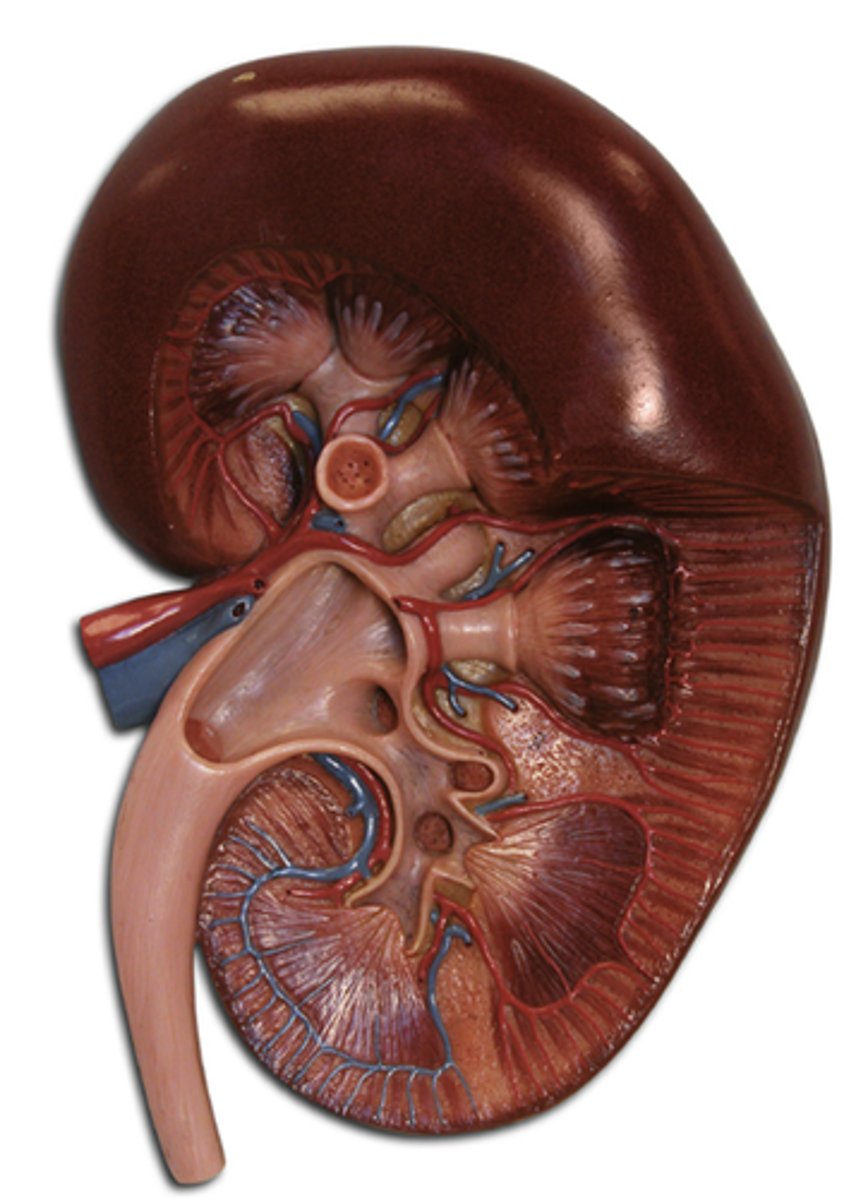
Structure of kidneys
* Fibrous capsule - outer membrane that surrounds and protects kidney
* Renal cortex - outer region containing Bowman's capsules, convoluted tubules, and blood vessels
* Renal medulla - inner region containing loops of Henle, collecting ducts, and blood vessels
* Renal pelvis - cavity that collects urine into ureters
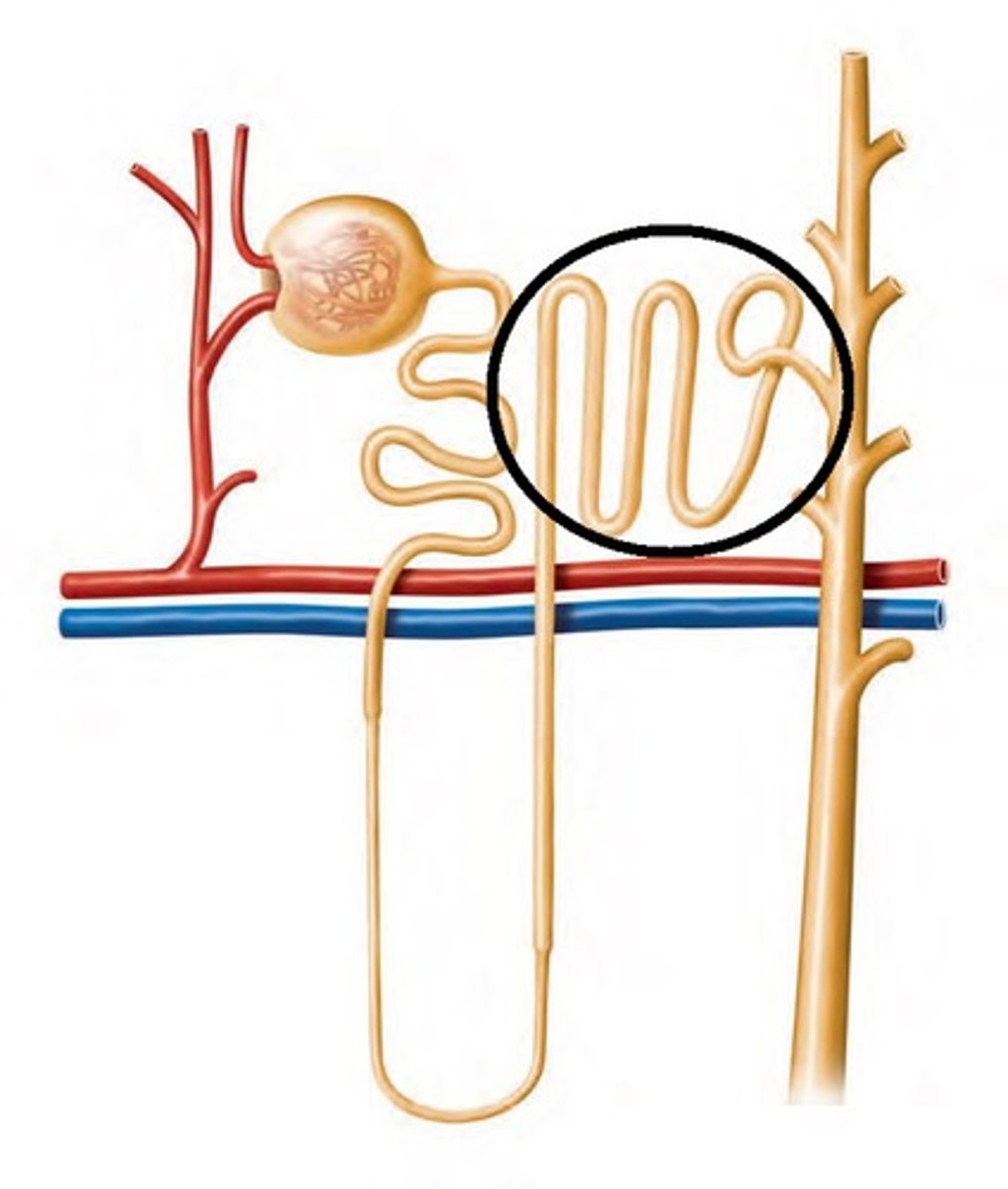
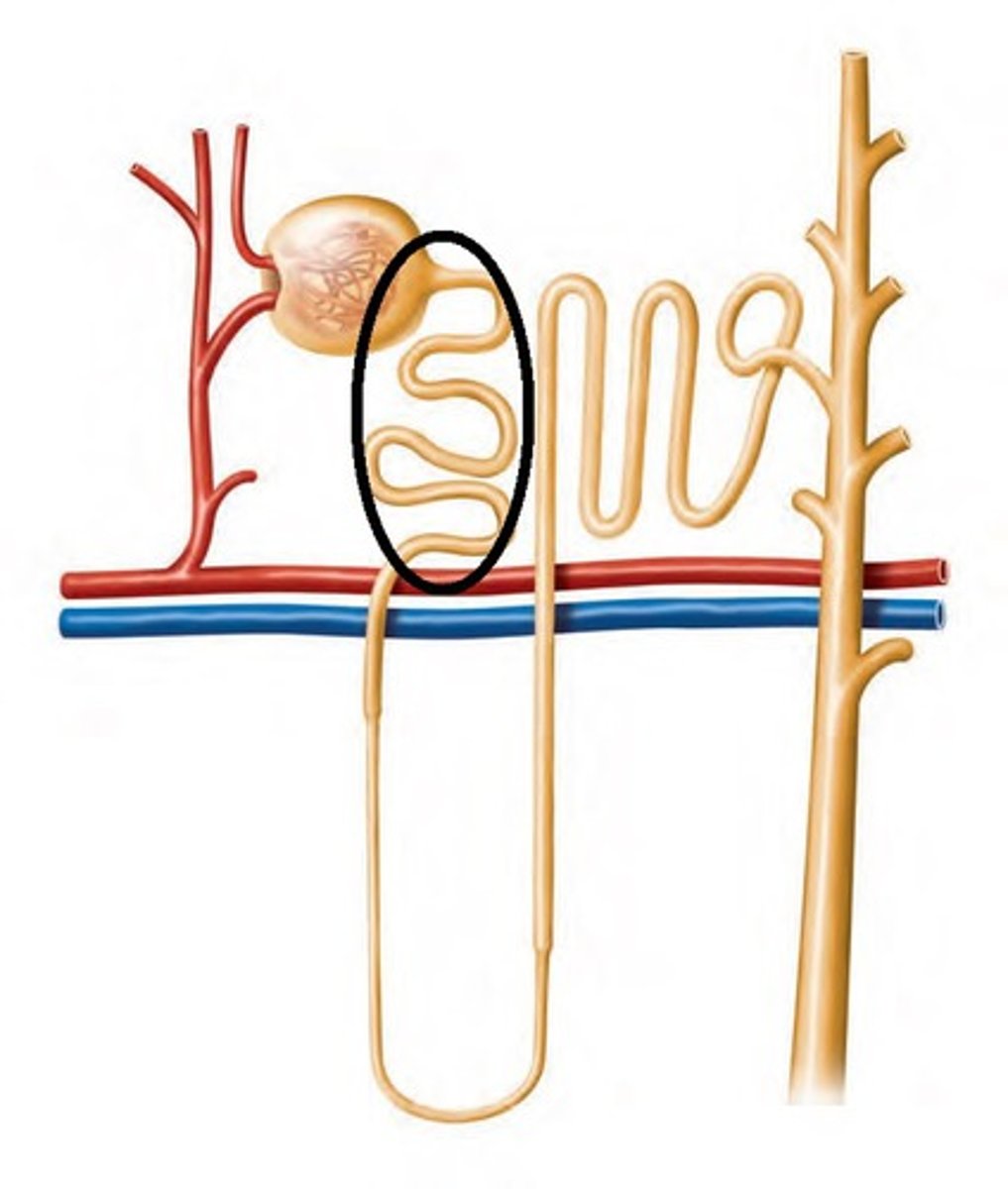
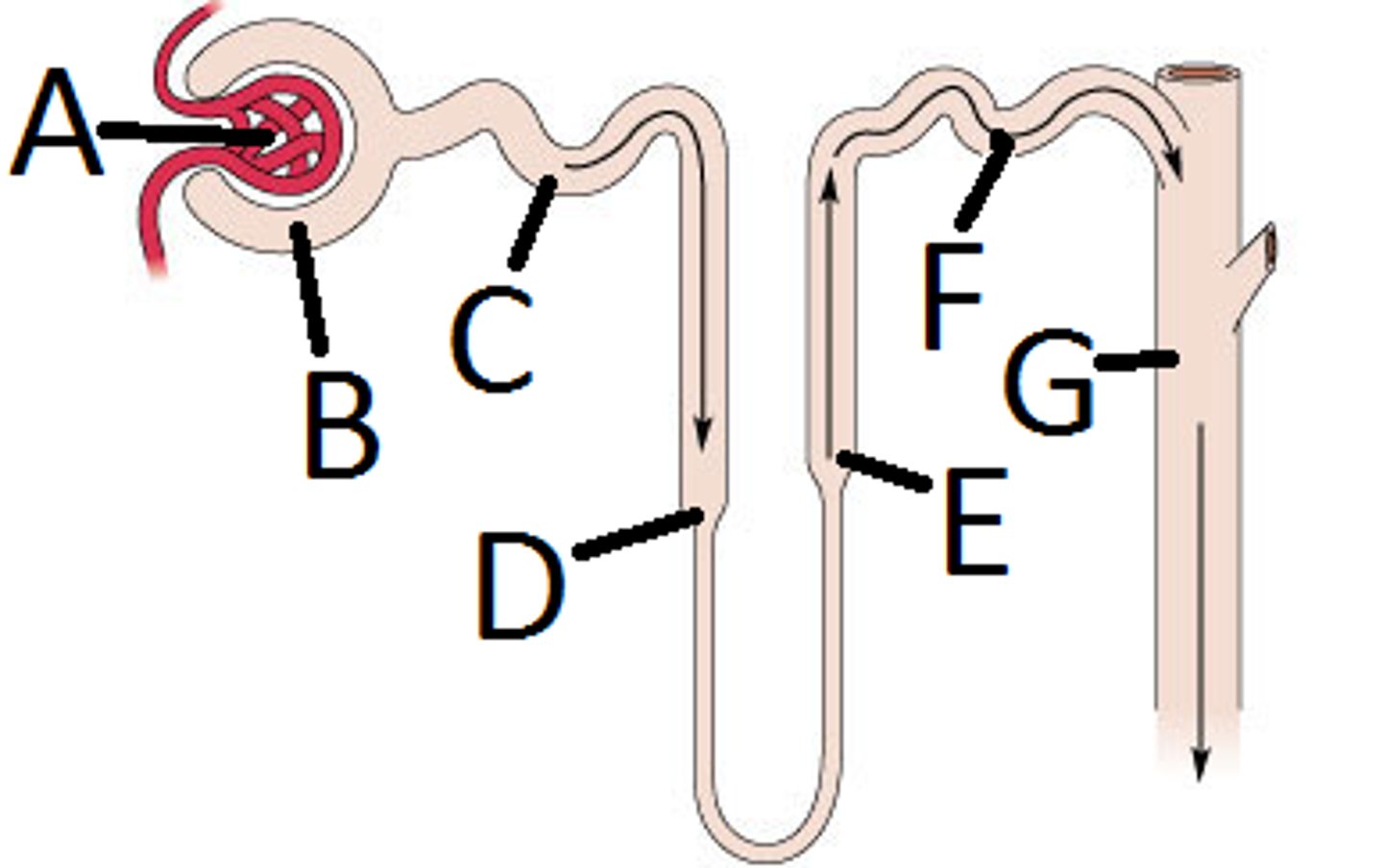
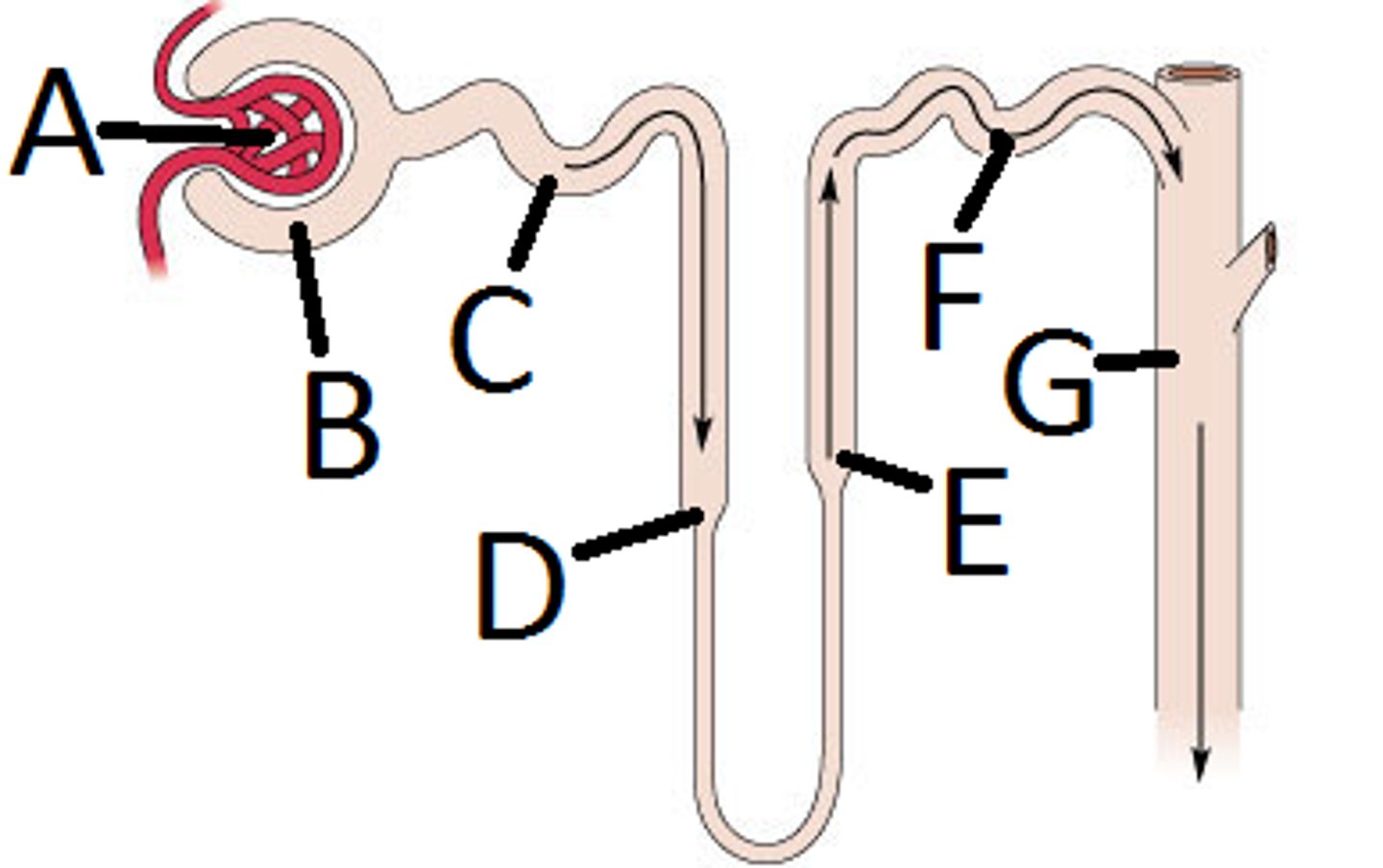
Structure of the nephrons
Bowman's capsule
Proximal convoluted tubule (PCT)
Loop of Henle
Distal convoluted tubule (DCT)
Collecting duct
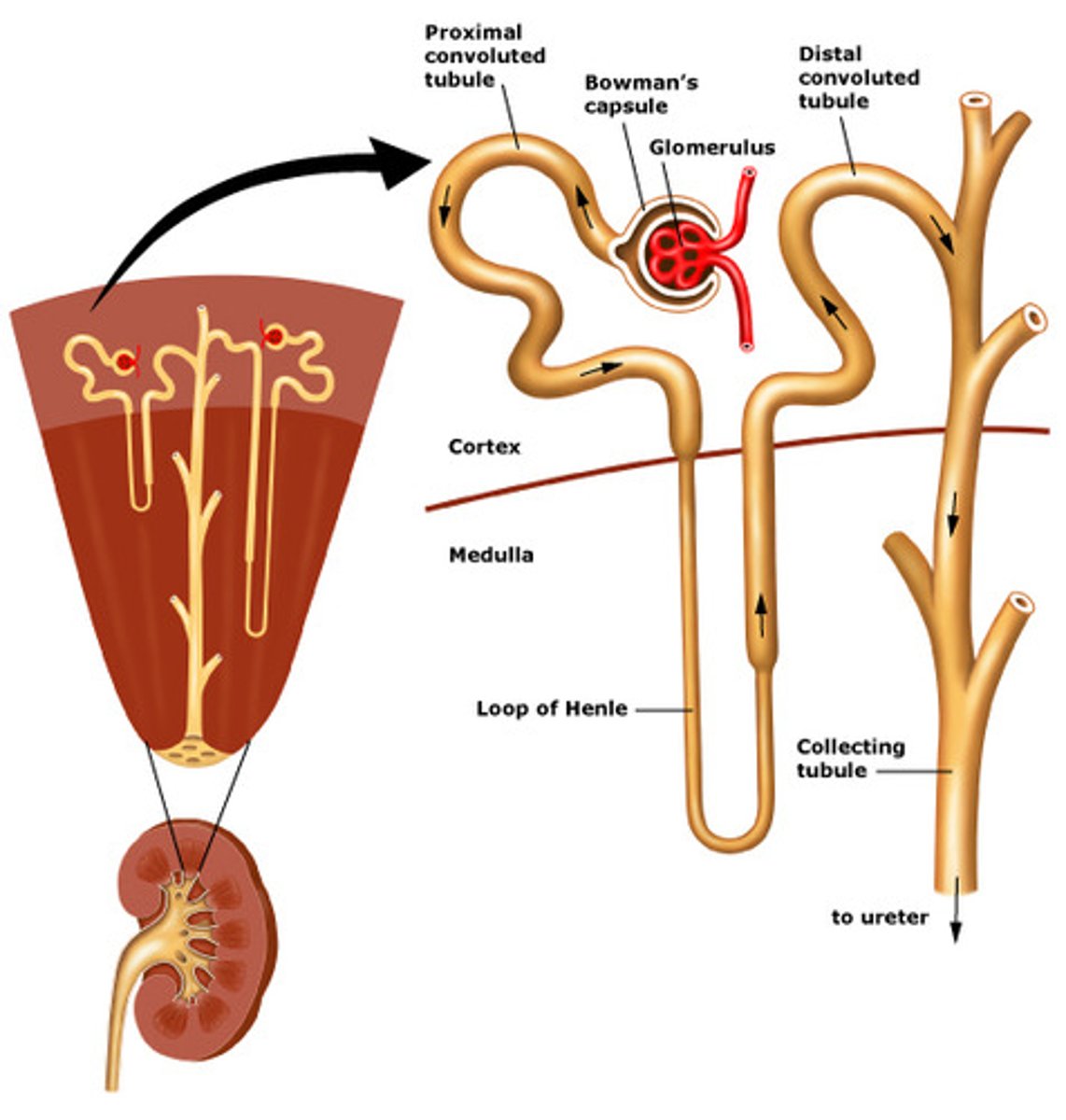
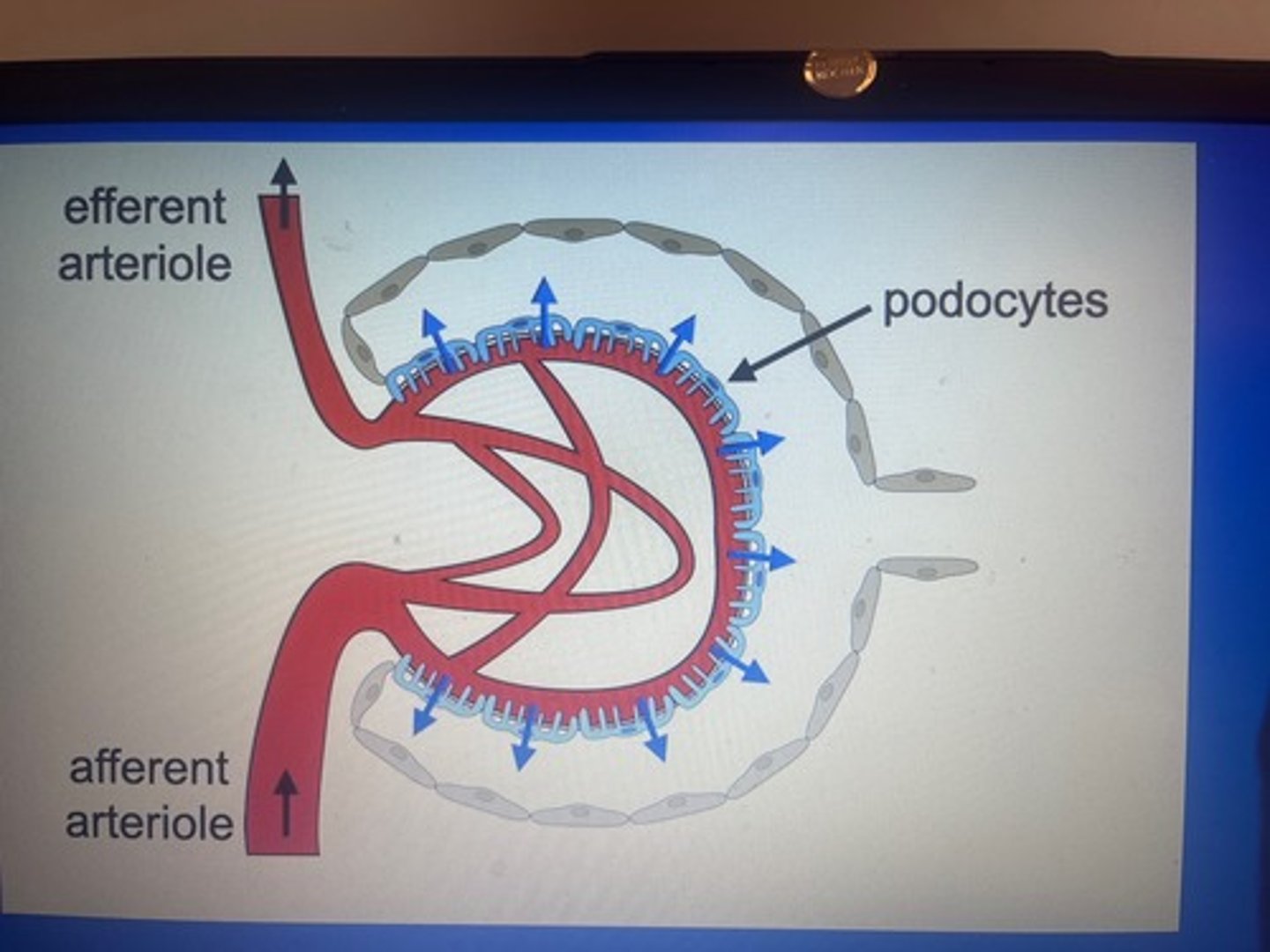
Bowman's capsule
Surrounds glomerulus (where filtrate is formed) and contains podocytes in its inner layer
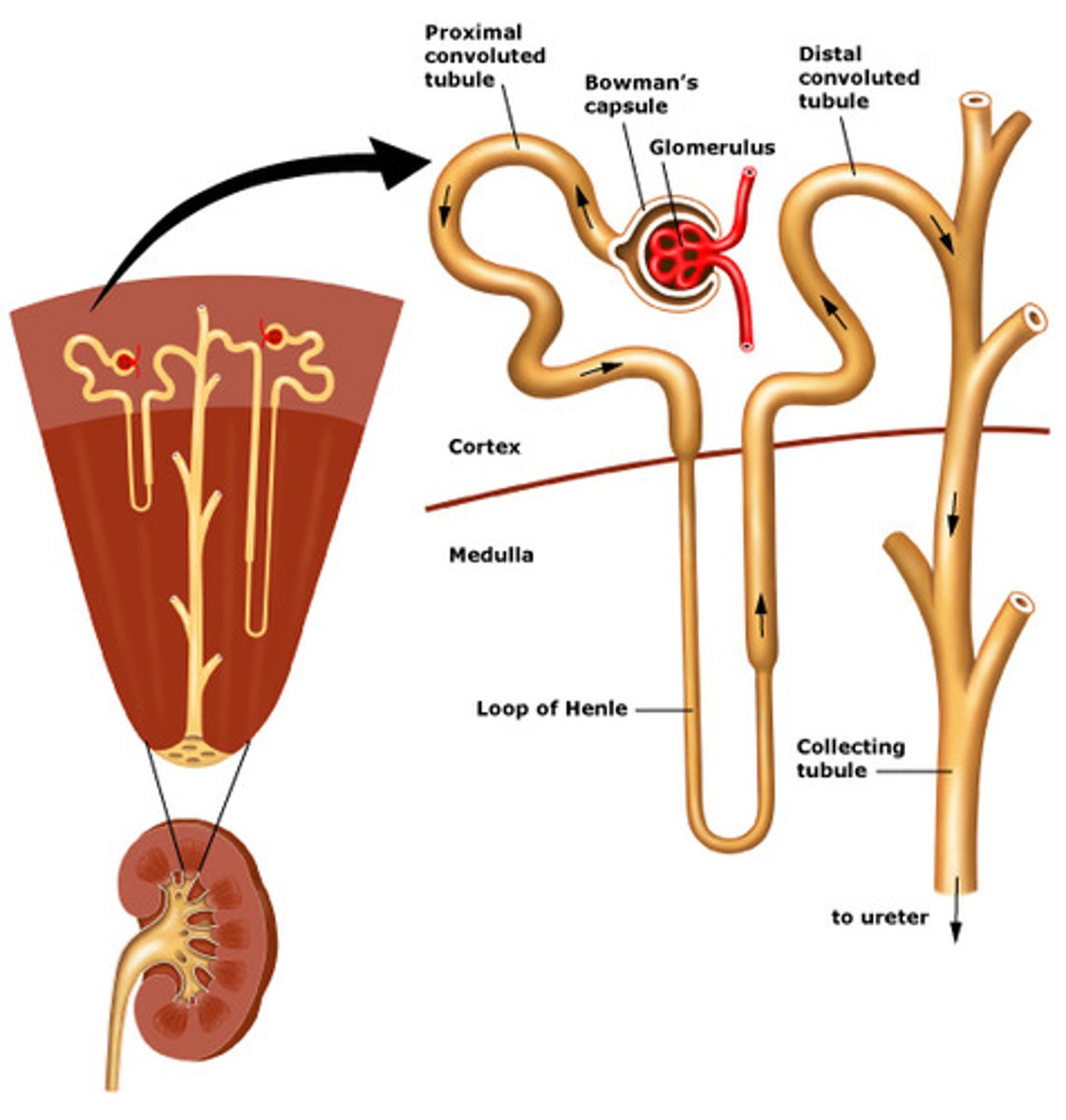
Proximal convoluted tubule (PCT)
Reabsorbs useful substances (eg water, glucose, salts) into surrounding capillaries
* Contains microvilli to increase surface area
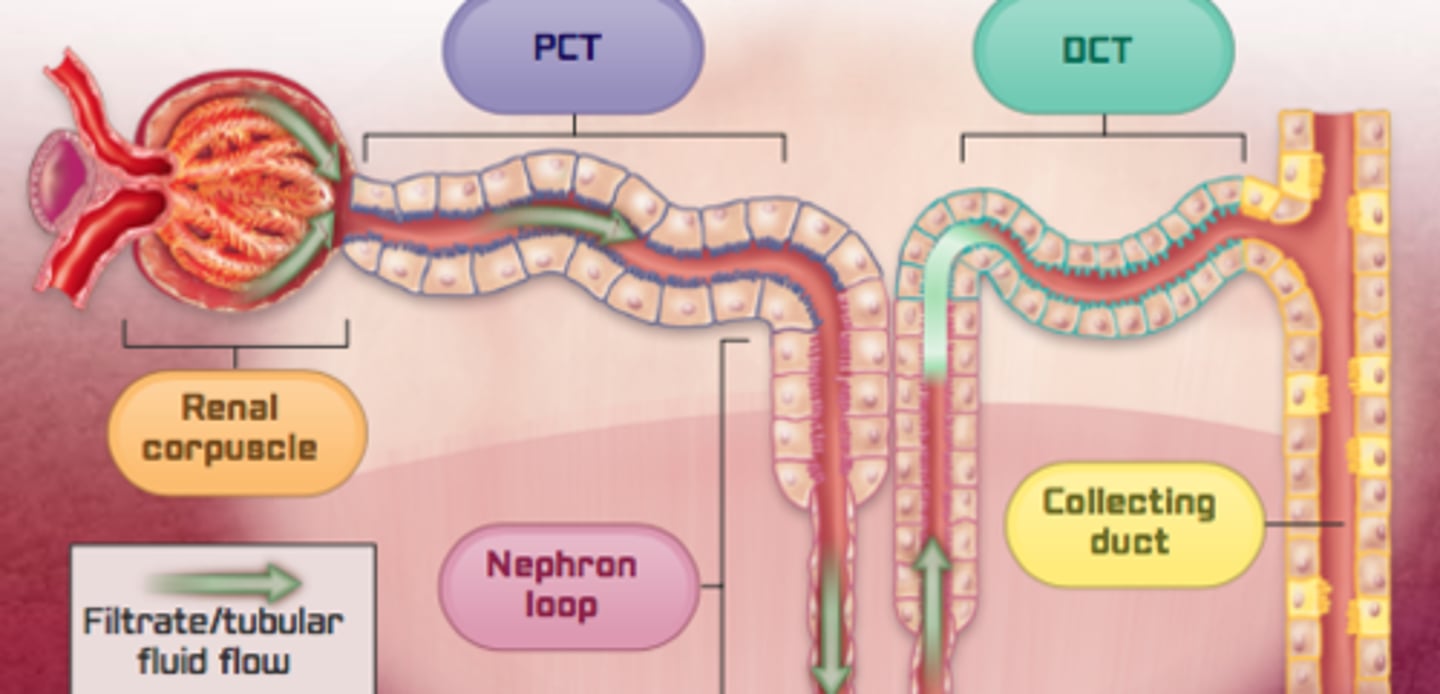
Loop of Henle
Loop that creates a high solute gradient in the medulla, helping with reabsorption
Distal convoluted tubule (DCT)
Reabsorbs water into blood + influenced by ADH
- Surrounded by fewer capillaries than the PCT
Collecting duct
Collects filtrate from nephrons and further alters the water balance, before the urine is passed to the bladder
Role of the blood vessels associated with the nephron
* Afferent arteriole - supplies glomerulus with blood
* Glomerulus - fluid is forced out of the blood inside glomerulus into the Bowman's capsule through ultrafiltration
* Efferent arteriole - carries blood away from glomerulus
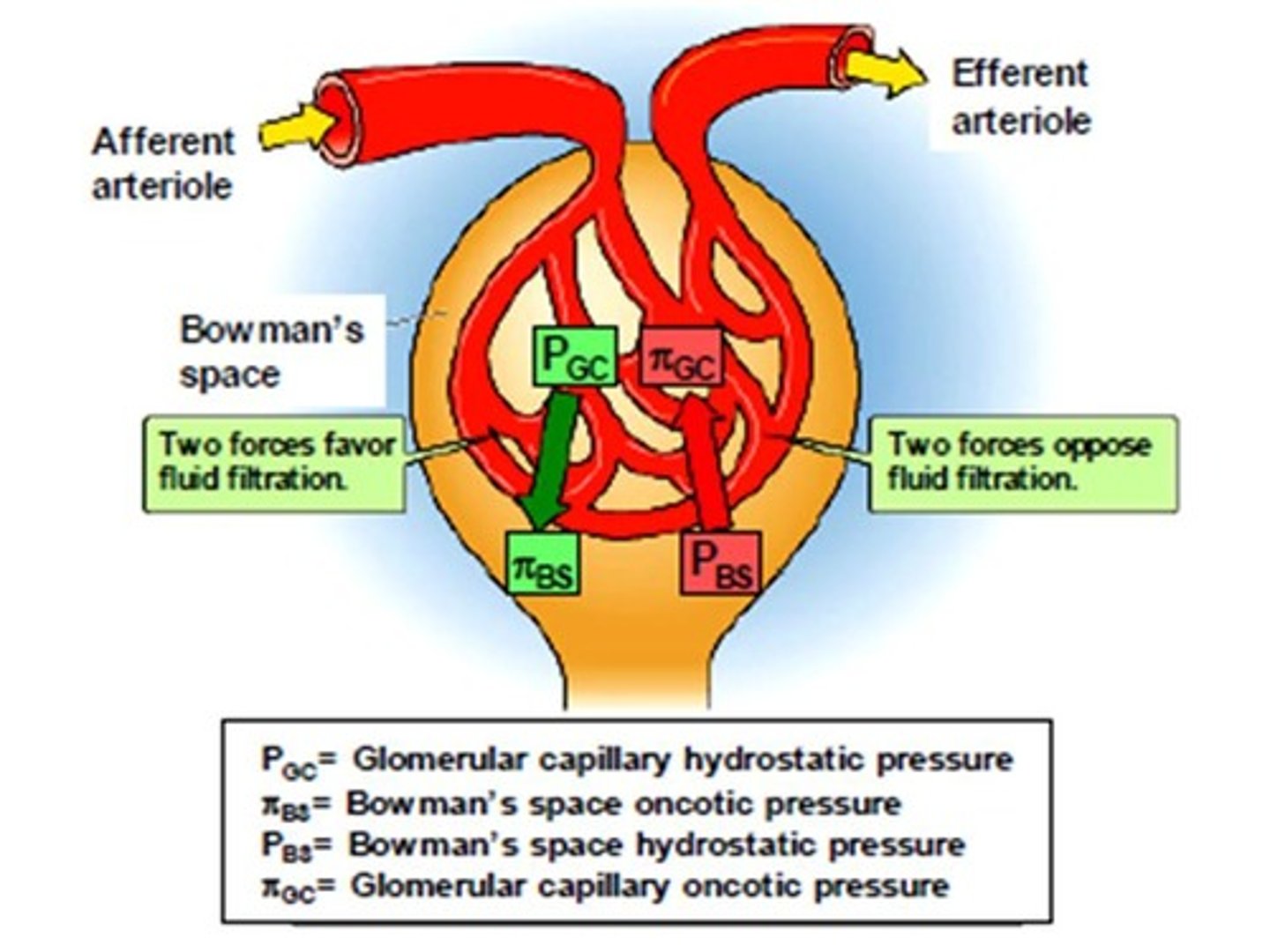
What is ultrafiltration?
Filtering small molecules (eg; H₂O, glucose, urea) out of the blood and into the Bowman's capsule to form glomerular filtrate
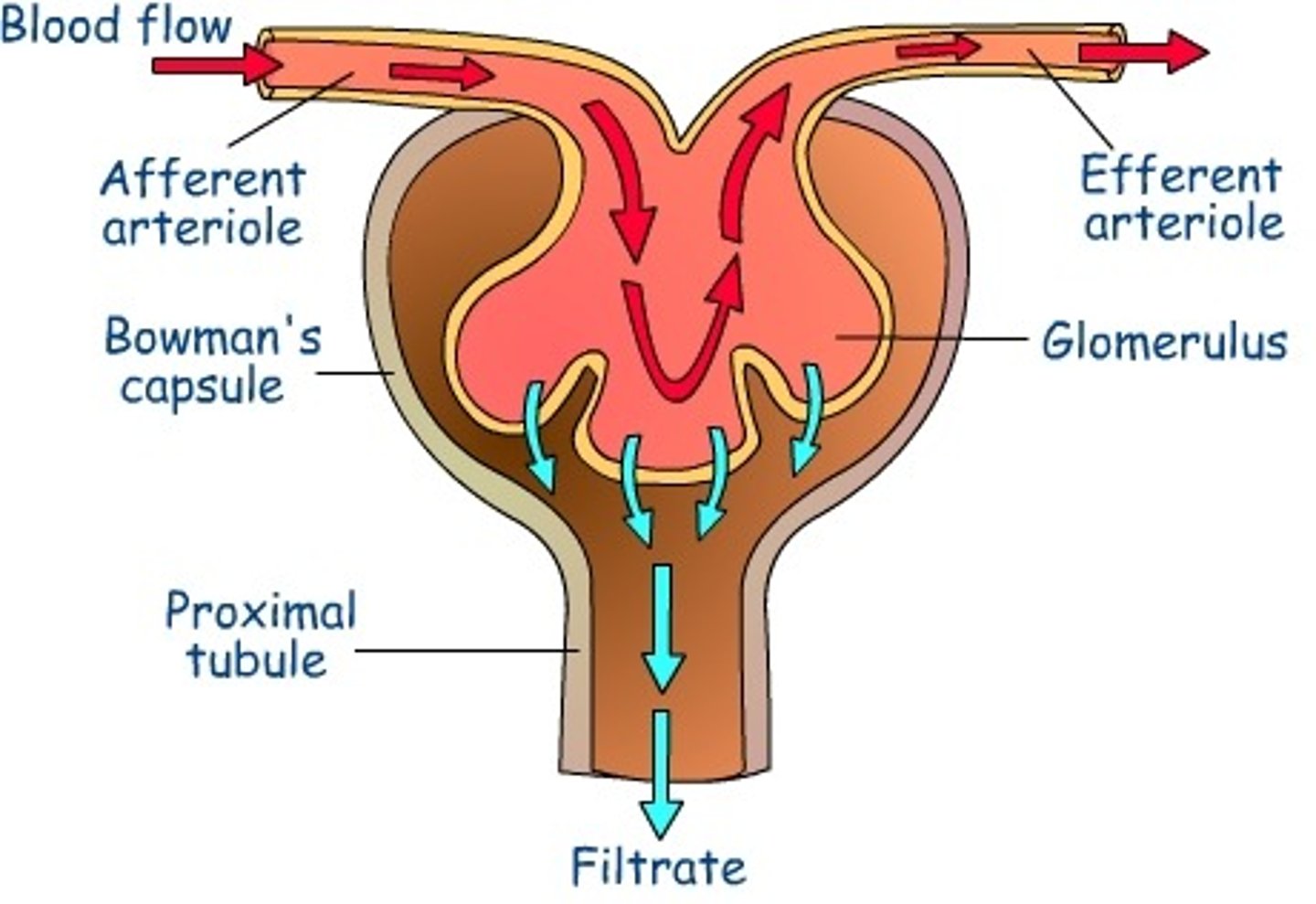
Steps of Ultrafiltration
- Blood enters glomerulus via afferent arteriole
- Afferent arteriole is wider than efferent arteriole (creating a high hydrostatic pressure)
- Pressure forces molecules (eg urea) out of the blood
- These molecules pass through three filtration layers:
* Capillary endothelium (with pores)
* Basement membrane (main filter; stops large proteins)
* Podocytes (with filtration slits)
- Filtered fluid (glomerular filtrate) enters Bowman's capsule
- Large molecules (proteins) remain in blood
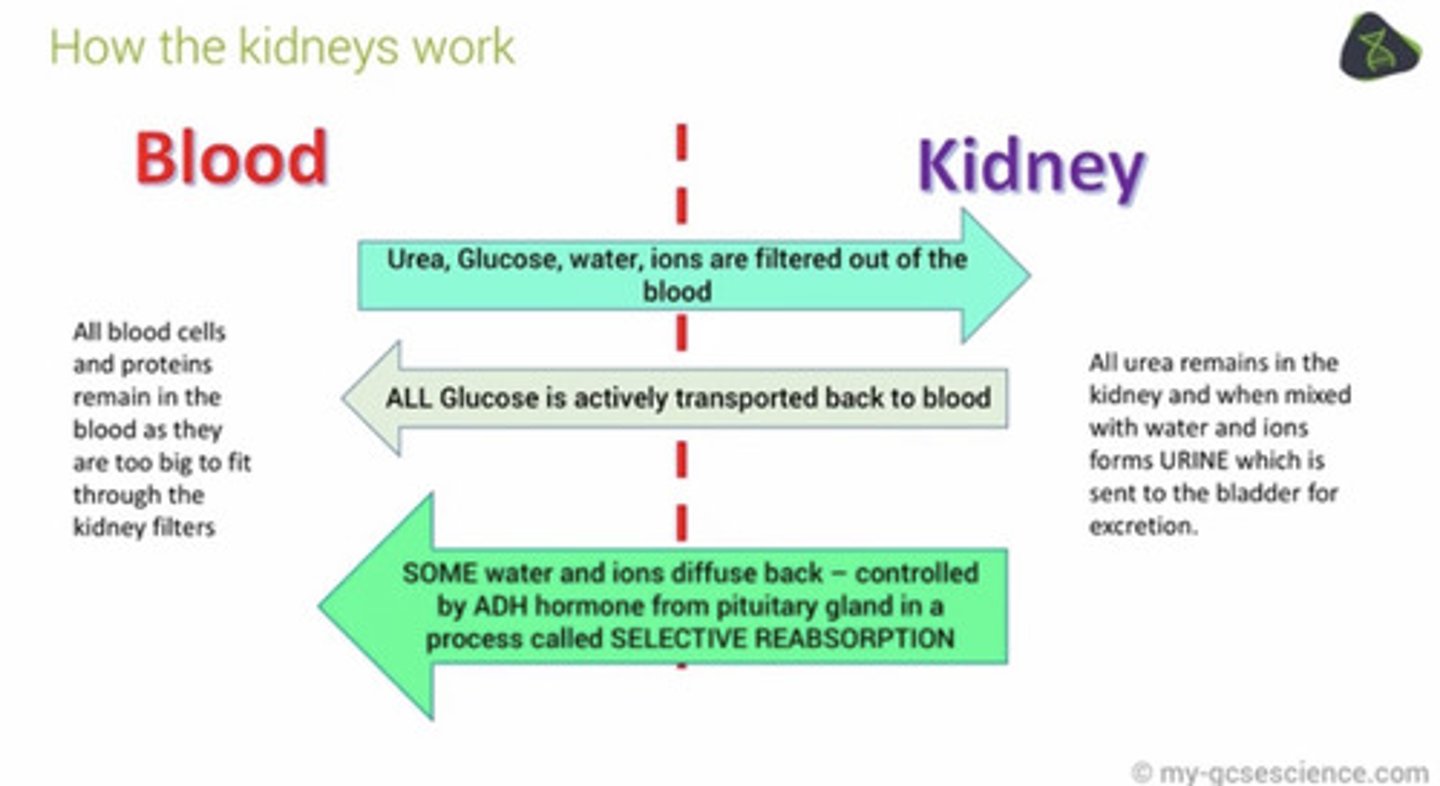
How does the kidney produce urine?
By filtration of the blood and selective reabsorption of useful substances (eg glucose)
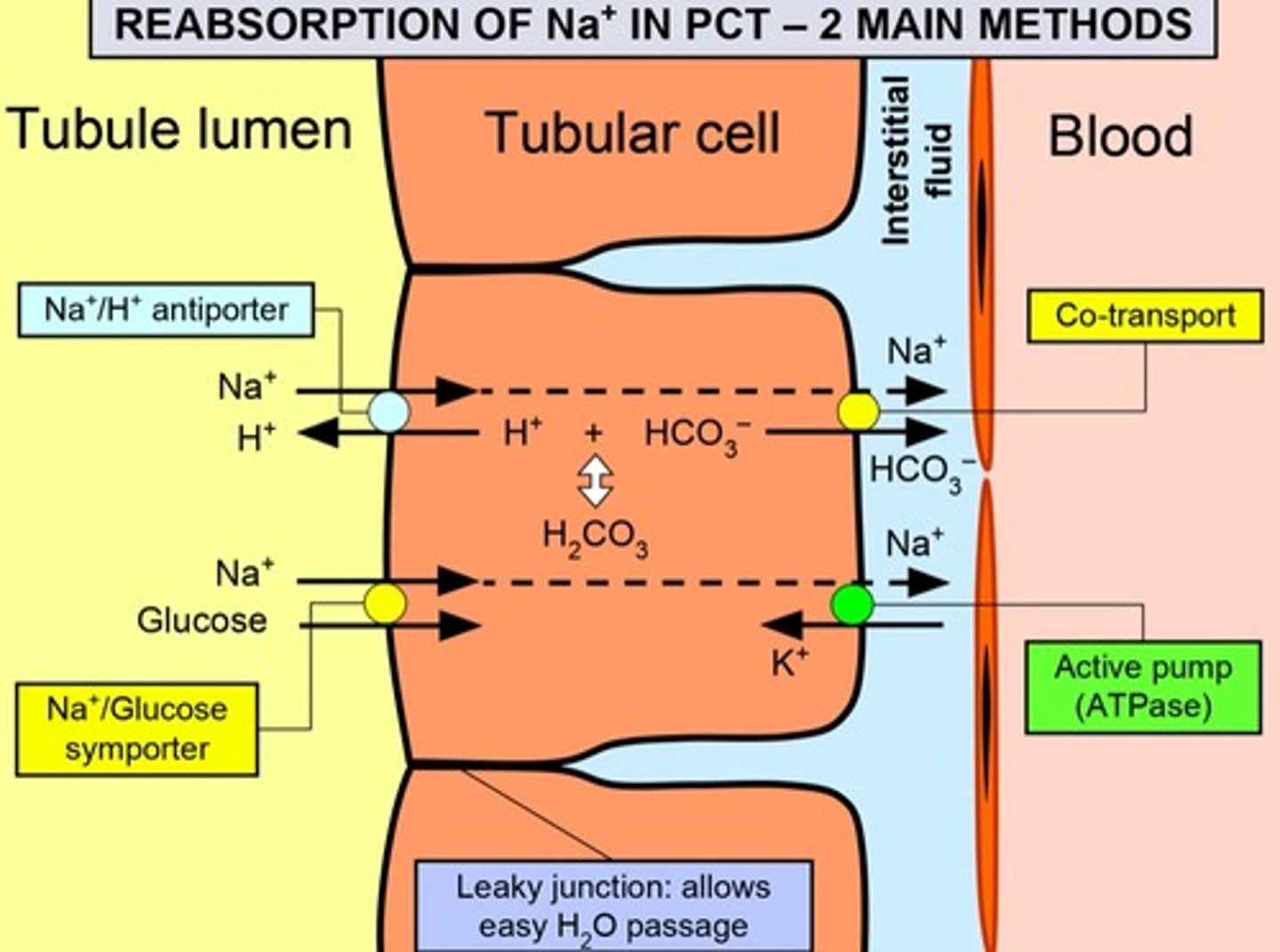
How is the proximal convoluted tubule (PCT) adapted for reabsorption?
Basal infoldings + Microvilli - Increases surface area
Mitochondria - provides ATP for active transport
Co transporter proteins - allows co-transport of substances from filtrate into epithelial cells
Selective reabsorption
- Na⁺ ions are actively transported into blood
- This reduces Na⁺ conc. in epithelial cells lining the PCT
- Na⁺ moves from PCT lumen into epithelial cells, down concentration gradient
- Na⁺ is co-transported with substances (eg glucose) into epithelial cells
- These substances diffuse into blood capillaries
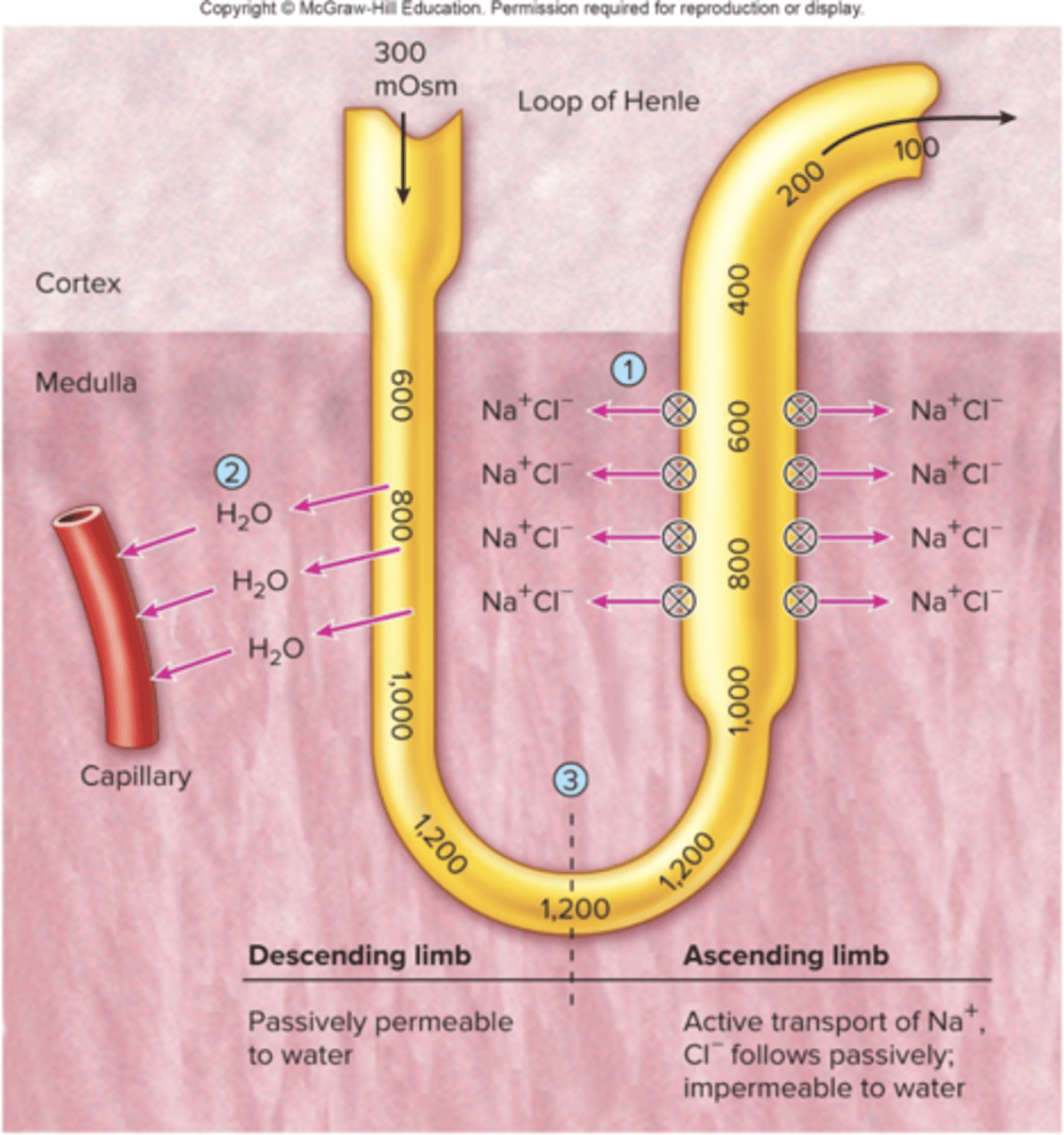
Loop of Henle - Descending limb
- Narrow
- High water permeability
- Impermeable to ions
Loop of Henle - Ascending limb
- Wider
- Impermeable to water
- Permeable to ions
How does the Loop of Henle control water reabsorption?
(Descending Limb)
- As filtrate travels down, solute conc. of medulla increases
- Water leaves filtrate into medulla by osmosis
- Filtrate becomes more concentrated
(Ascending Limb)
- Lower part: Na⁺ and Cl⁻ diffuse into the medulla
- Upper part: ions are actively transported into the medulla
This maintains a high salt concentration in the medulla
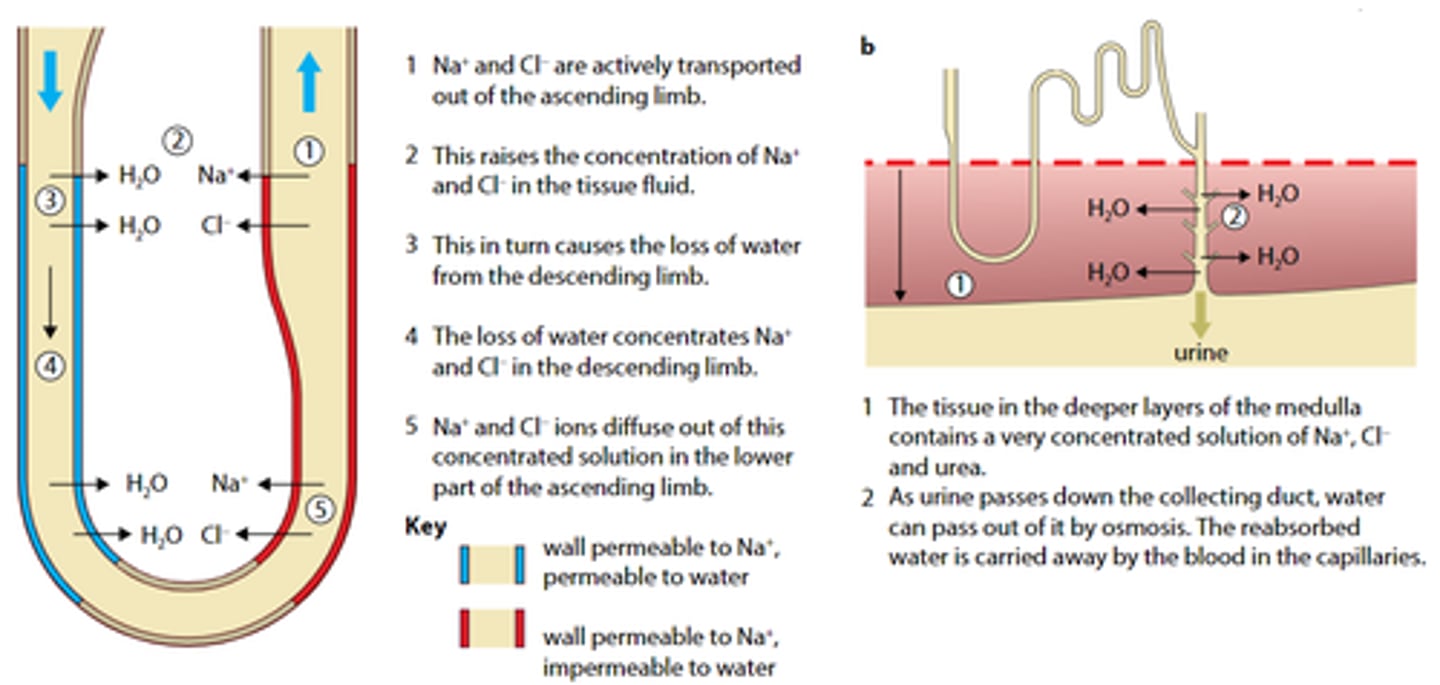
How does the Loop of Henle act as a countercurrent multiplier?
- As filtrate moves down the collecting duct, it loses water, decreasing its water potential.
- However, the water potential of the medulla is even lower than the collecting duct (due to high ion concentration at ascending limb)
- This allows water to continue to move out of filtrate down the whole length of the collecting duct
- This allows urine to be concentrated and ensures there's always a water potential gradient drawing water out of the collecting duct
Role of distal convoluted tube (DCT)
Reabsorption of water and ions through active transport
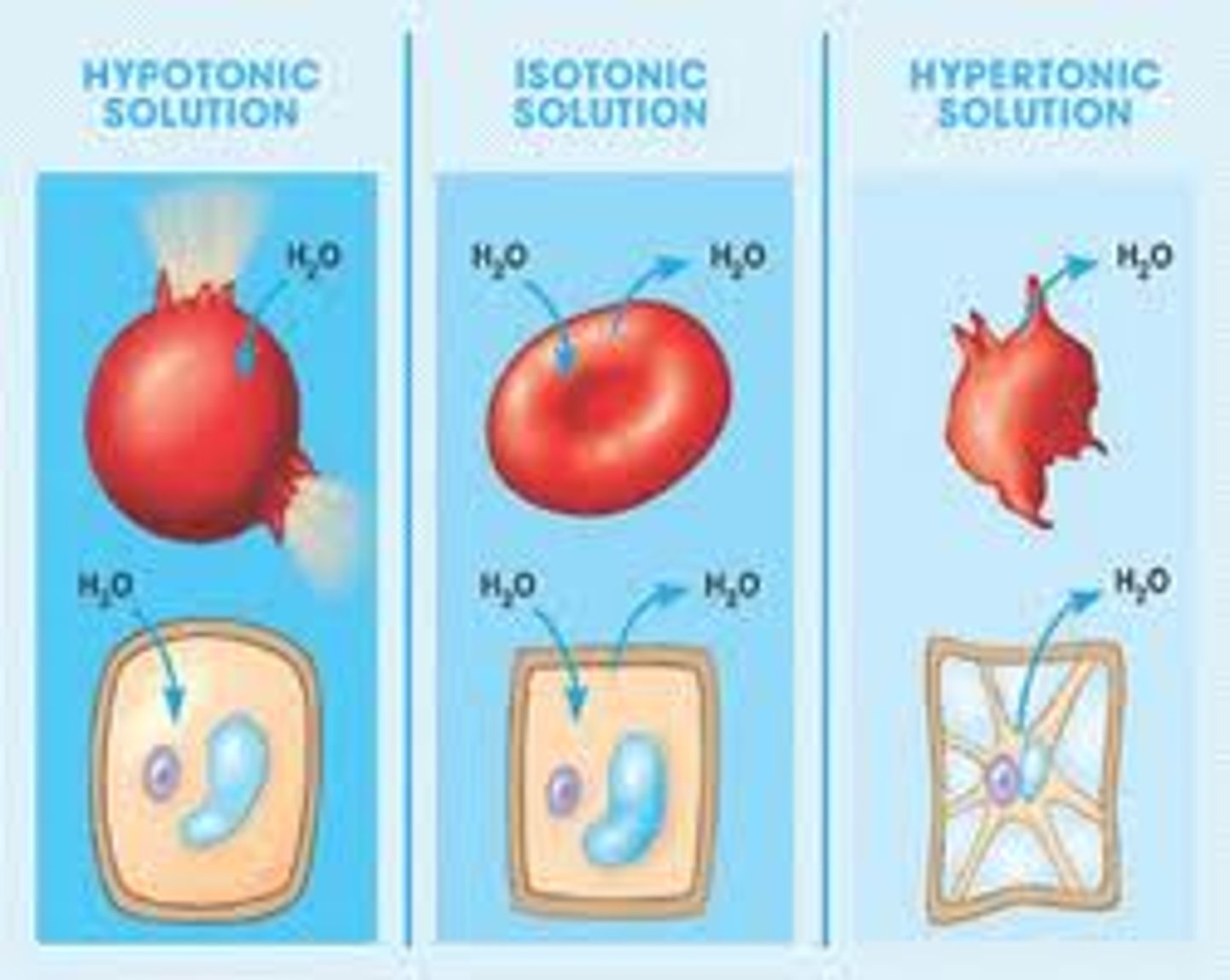
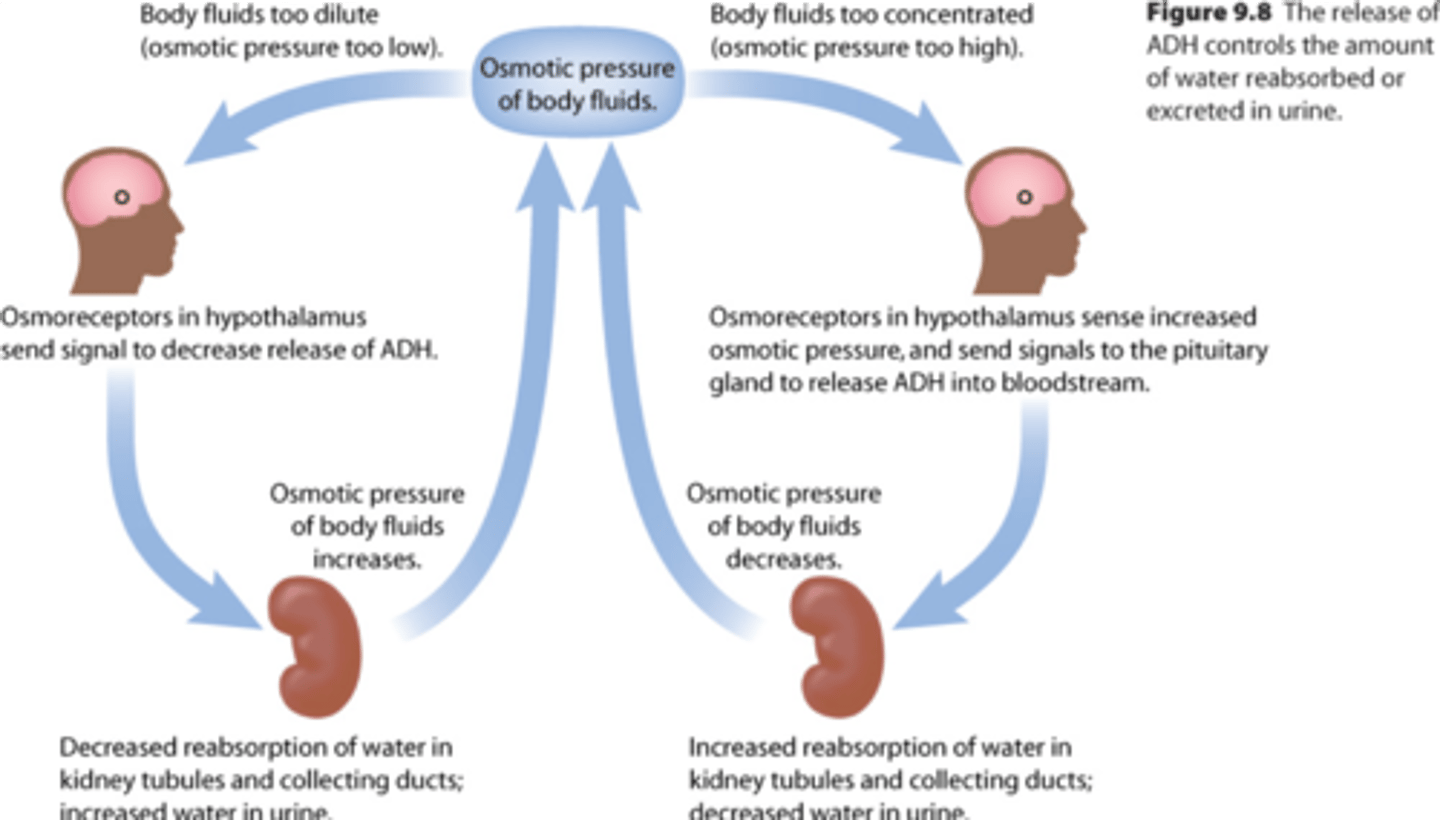
Osmoregulation
Homeostatic control of the water potential of the blood

Why is osmoregulation important?
Prevents cells bursting or shrinking during osmosis
Key features of ADH
- Produced in hypothalamus
- Stored in posterior pituitary gland
- Its target cells: cells lining the DCTs and collecting ducts (in kidneys)
- Controlled by negative feedback
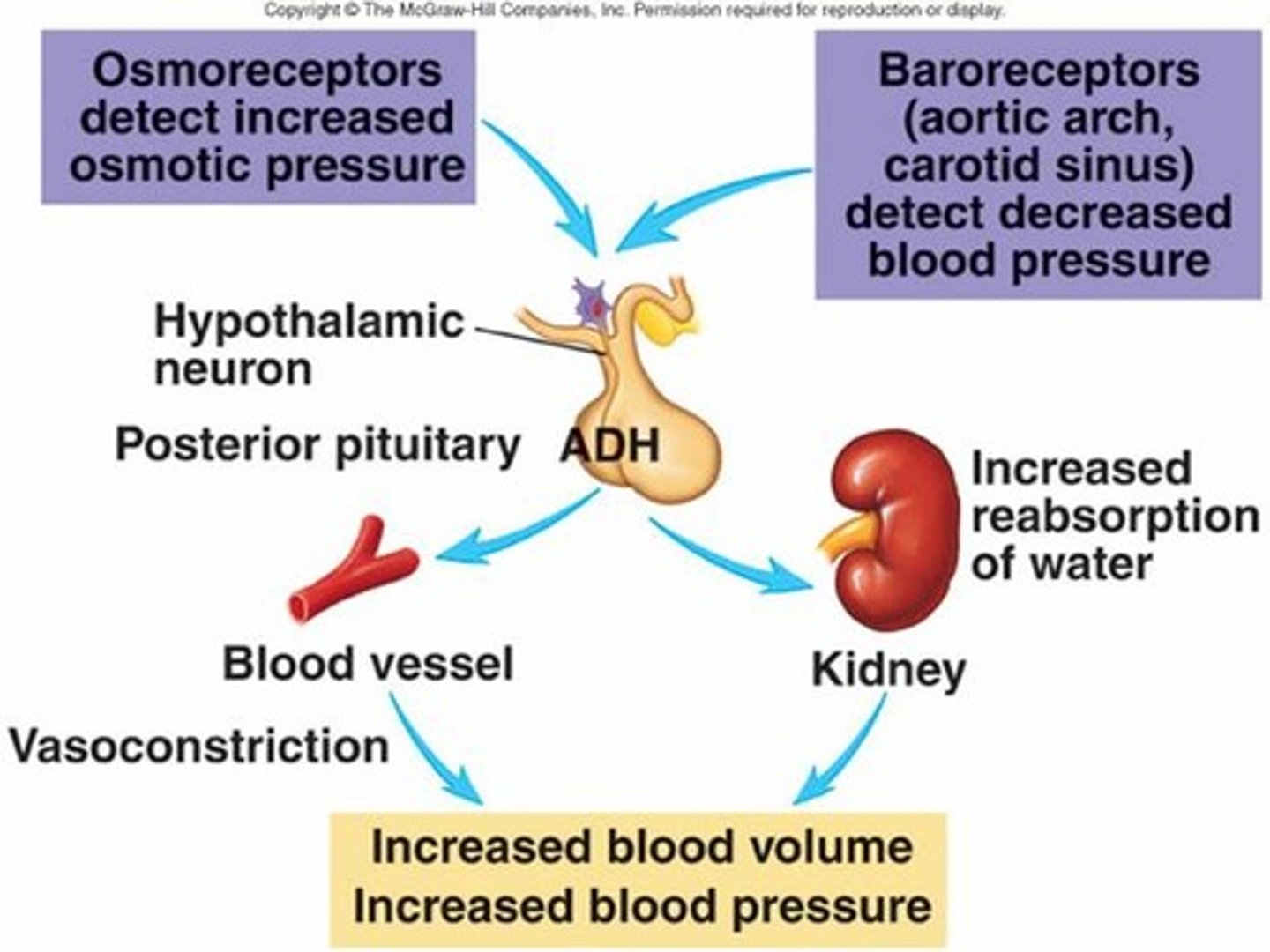
What happens when blood has low water potential?
- Osmoreceptors in the hypothalamus detect decrease in water
- More ADH is released from the pituitary gland
- Increased permeability of collecting duct walls and DCTs
- More water reabsorbed into blood
- Smaller volume of more concentrated urine produced
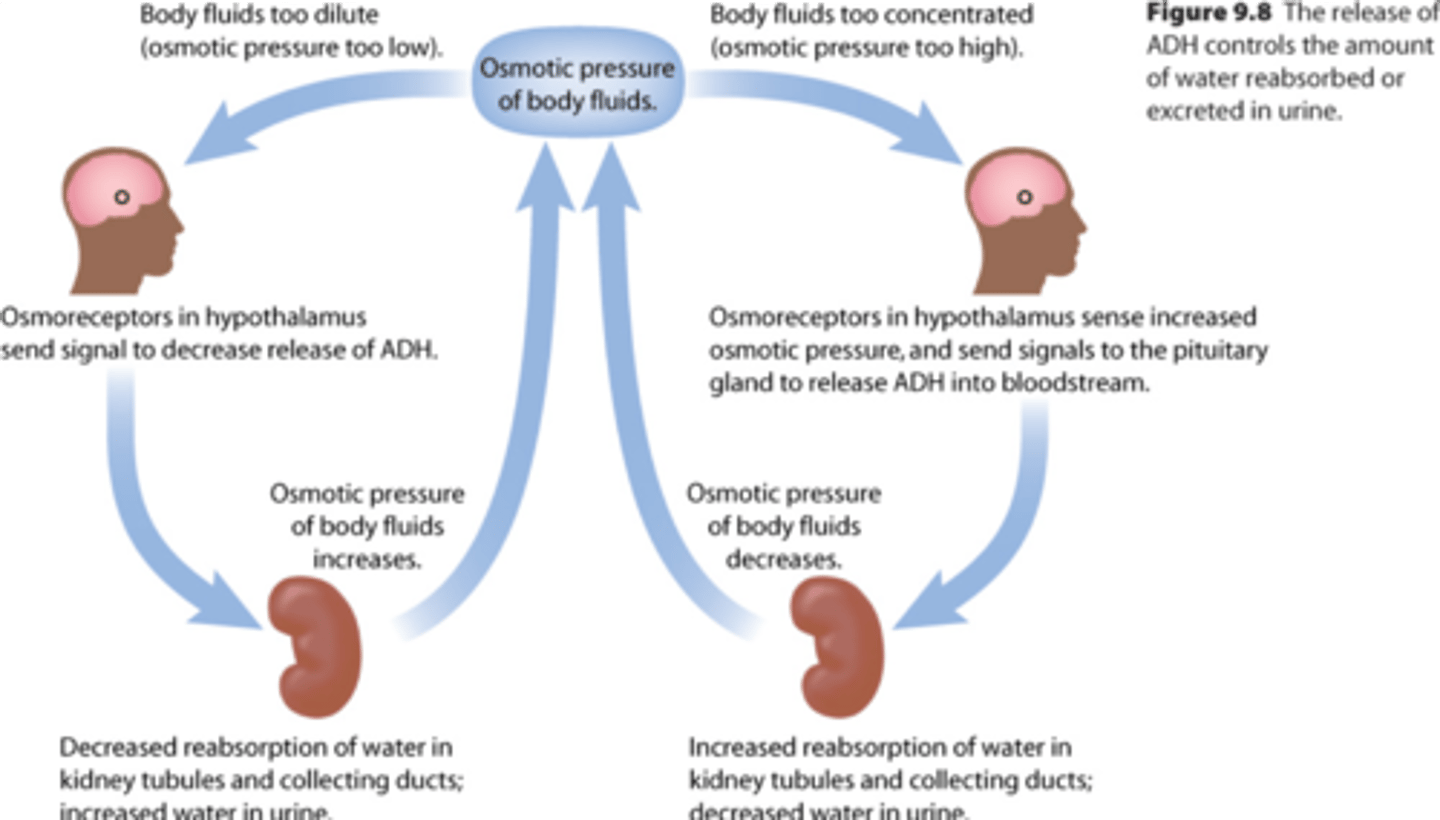
What happens when blood has high water potential?
- Osmoreceptors in the hypothalamus detect increase in water
- Less ADH is released from the pituitary gland
- Decreased permeability of collecting duct walls and DCTs
- Less water reabsorbed into blood
- Larger volume of less concentrated urine produced
How can urine be used to diagnose?
- Glucose in urine suggests diabetes
- High creatinine levels in urine suggests muscle/kidney damage
- Blood/proteins in urine suggests kidney disorders

Monoclonal antibodies
Antibodies from a single clone of cells that are produced to target particular body cells
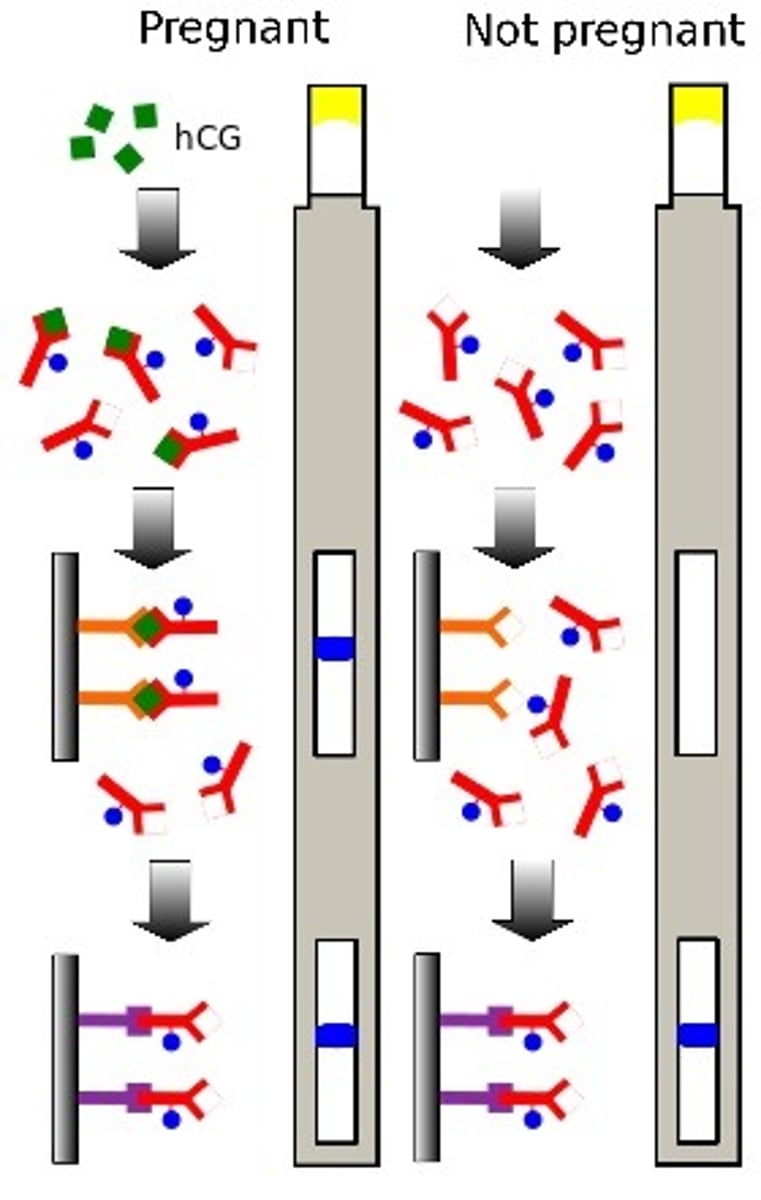
How do pregnancy tests work?
- Antibodies are attached to blue beads
- As urine passes through reaction zone, antibodies bind to any hCG
- In results zone, immobilised antibodies bind to any hCG (if test is positive - blue line appears)
- Other antibodies which don't attach to the hCG bind to antibodies in control zone
- Blue line always appears in control zone, but blue line in result zone means positive test
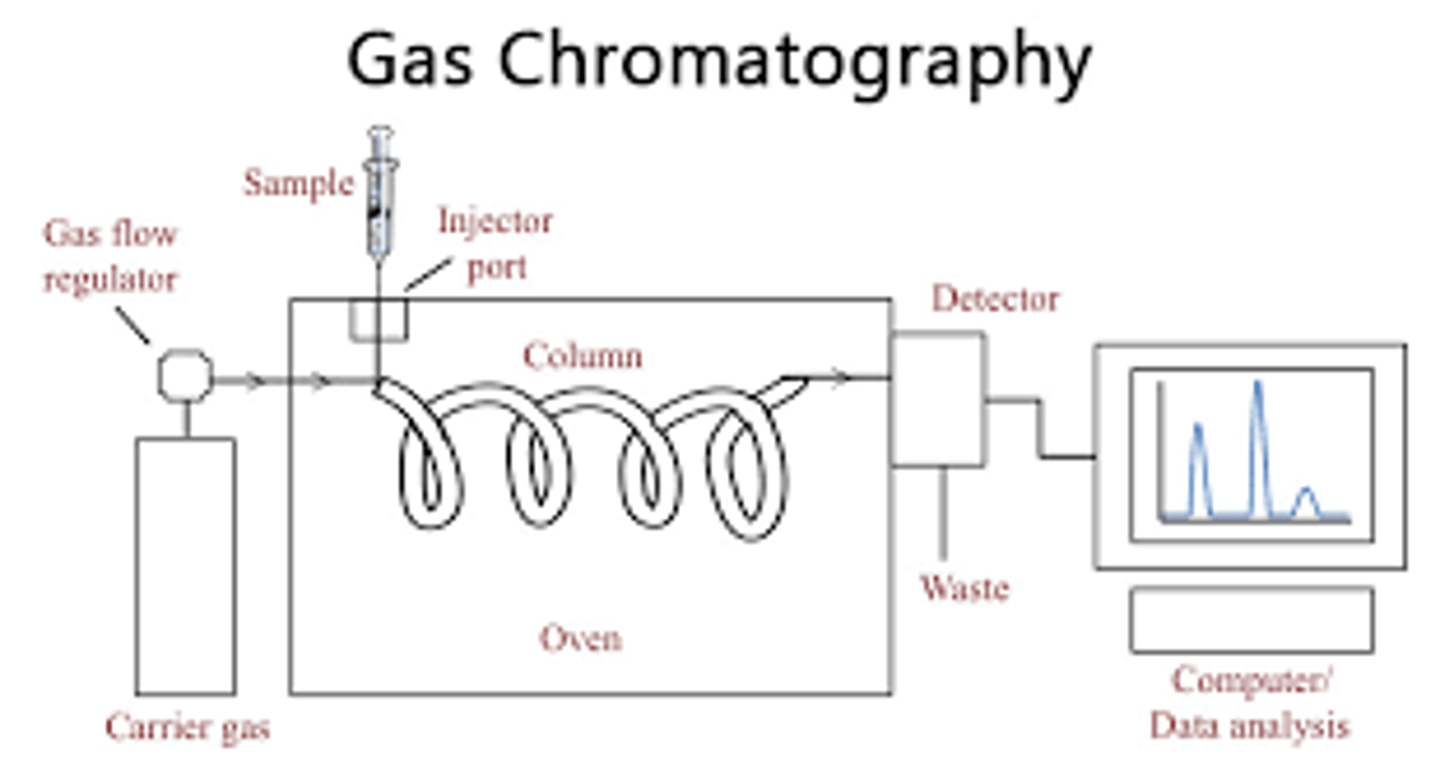
How can urine be used to test for drugs?
Using gas chromatography
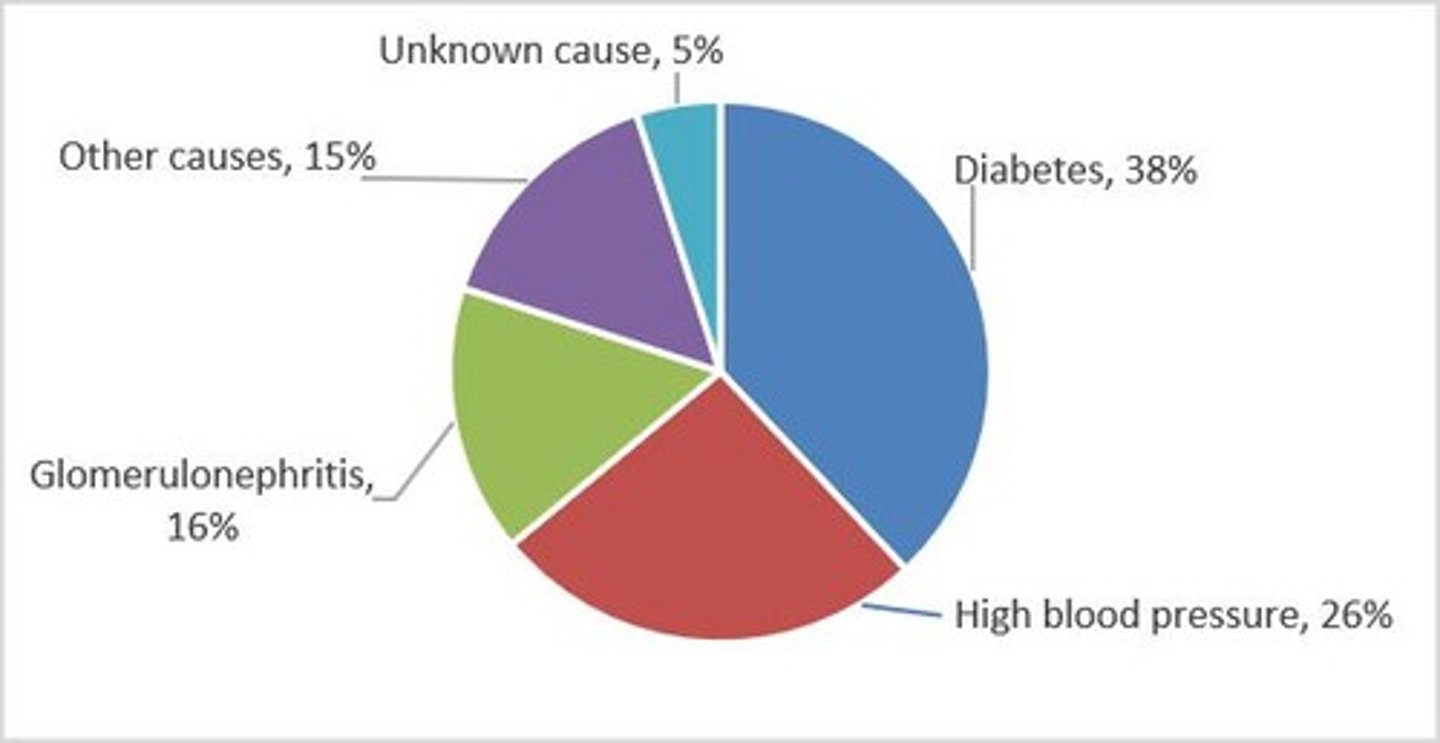
What are some causes of kidney failure?
- Kidney infections
- High blood pressure (hypertension)
- Diabetes
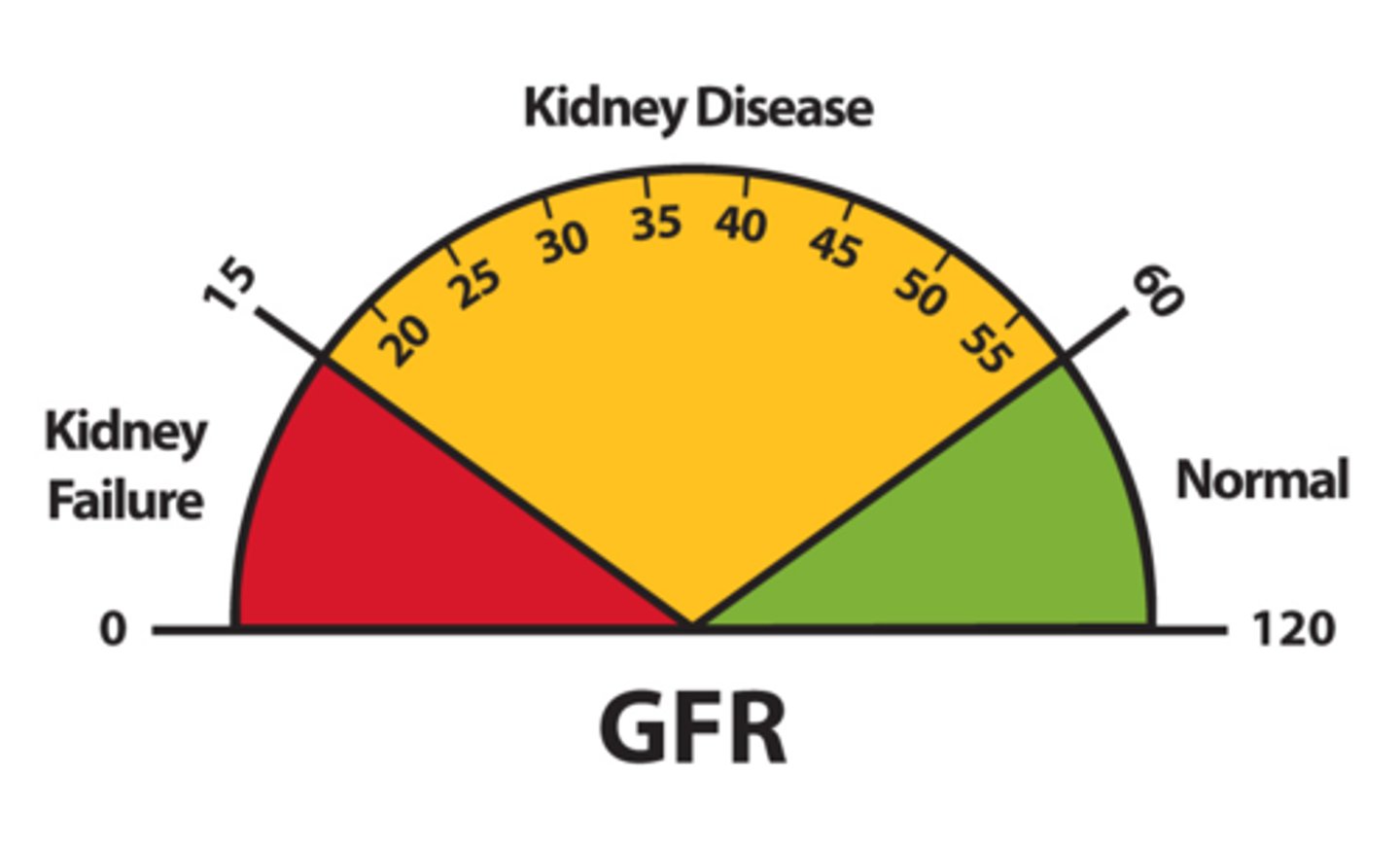
Glomerular filtration rate (GFR)
Measure of how much blood is filtered in the Bowman's capsules
How can GFR be used to detect kidney failure?
- Low GFR indicates less effective blood filtration
- Creatinine level in the blood is used to estimate the GFR
- High creatinine level indicates kidney disease
Effects of kidney failure
* Mineral ions buildup - causes electrolyte + osmotic imbalance
* Toxic waste buildup - poisons cells
* High blood pressure - causes heart problems
* Anaemia - causes fatigue
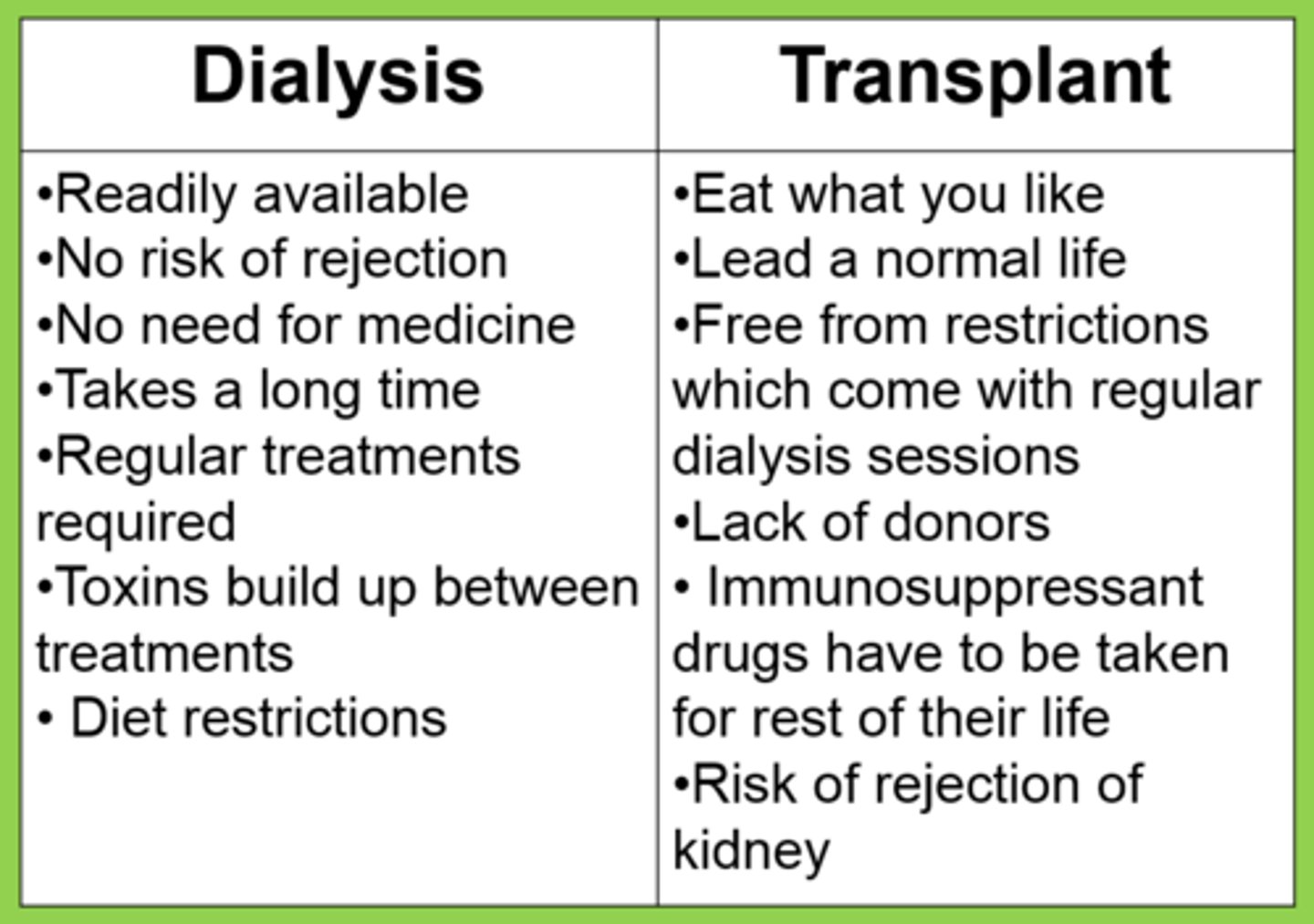
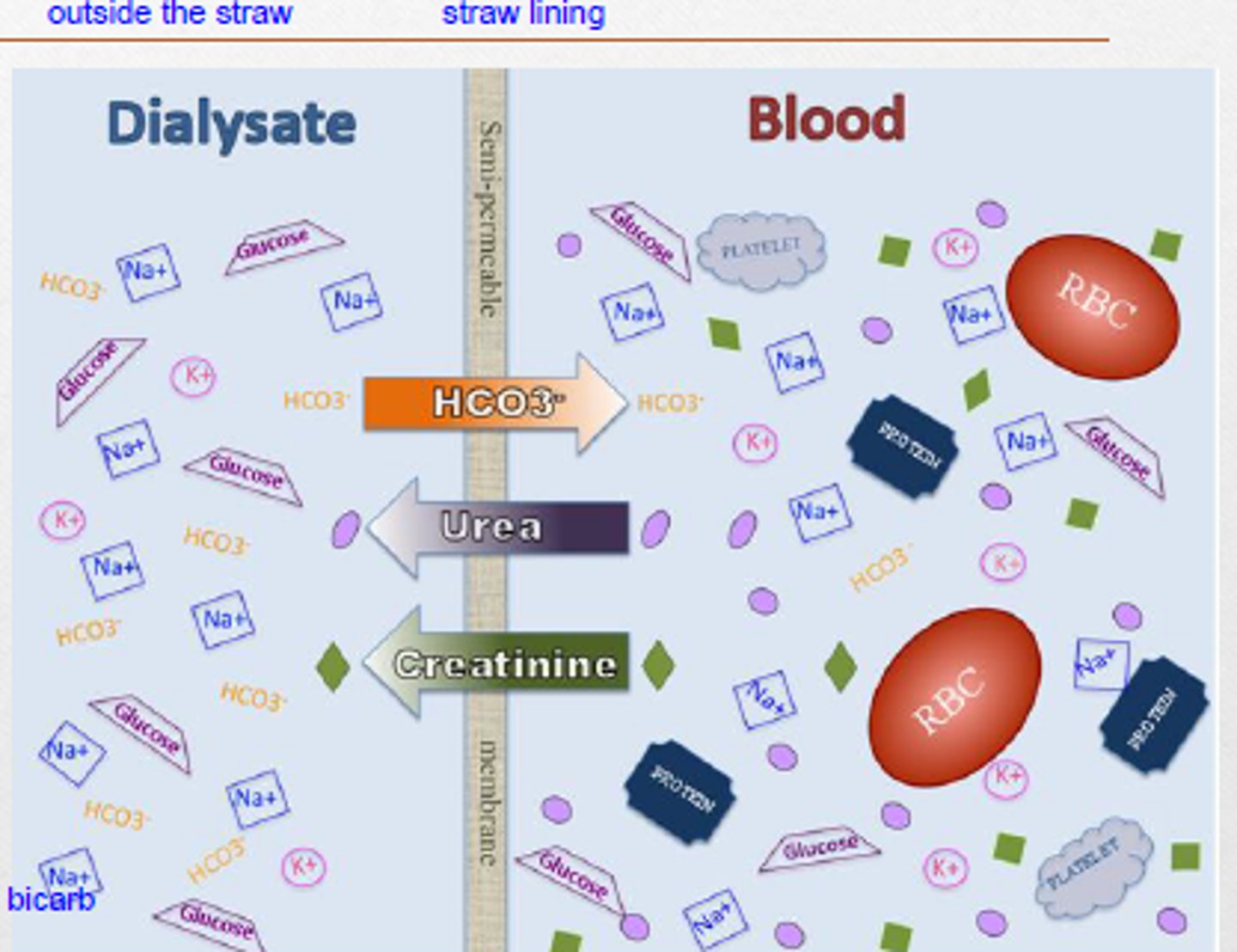
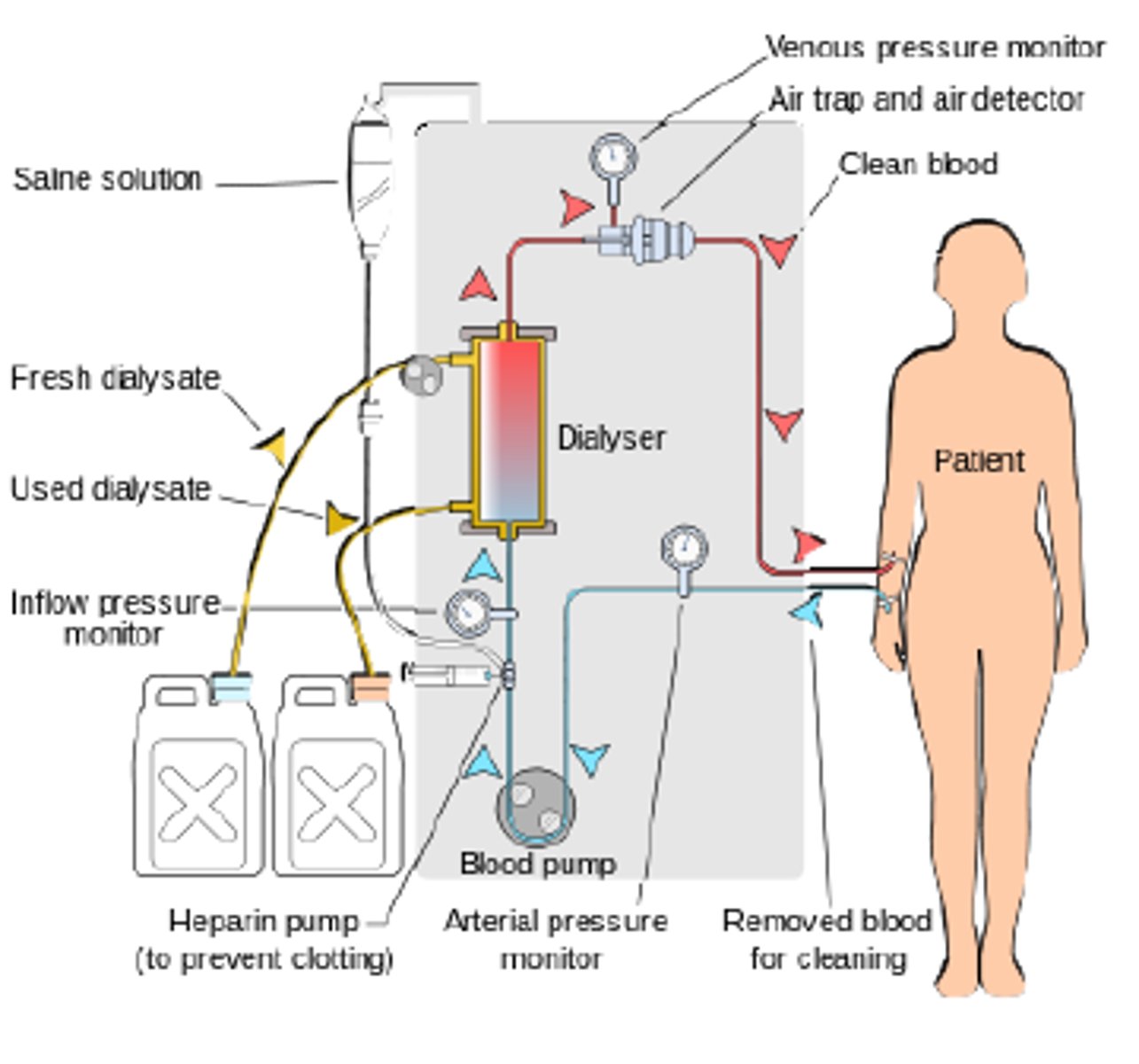
How does dialysis work?
- Blood and dialysis fluid are seperated by a semi-permeable membrane
- Dialysis fluid has normal levels of ions + glucose
- Ions and glucose diffuse across membrane into blood until normal levels are present
- Urea diffuses from blood into the dialysis fluid
- Larger molecules (RBC, proteins) remain in the blood because they're too big to pass membrane
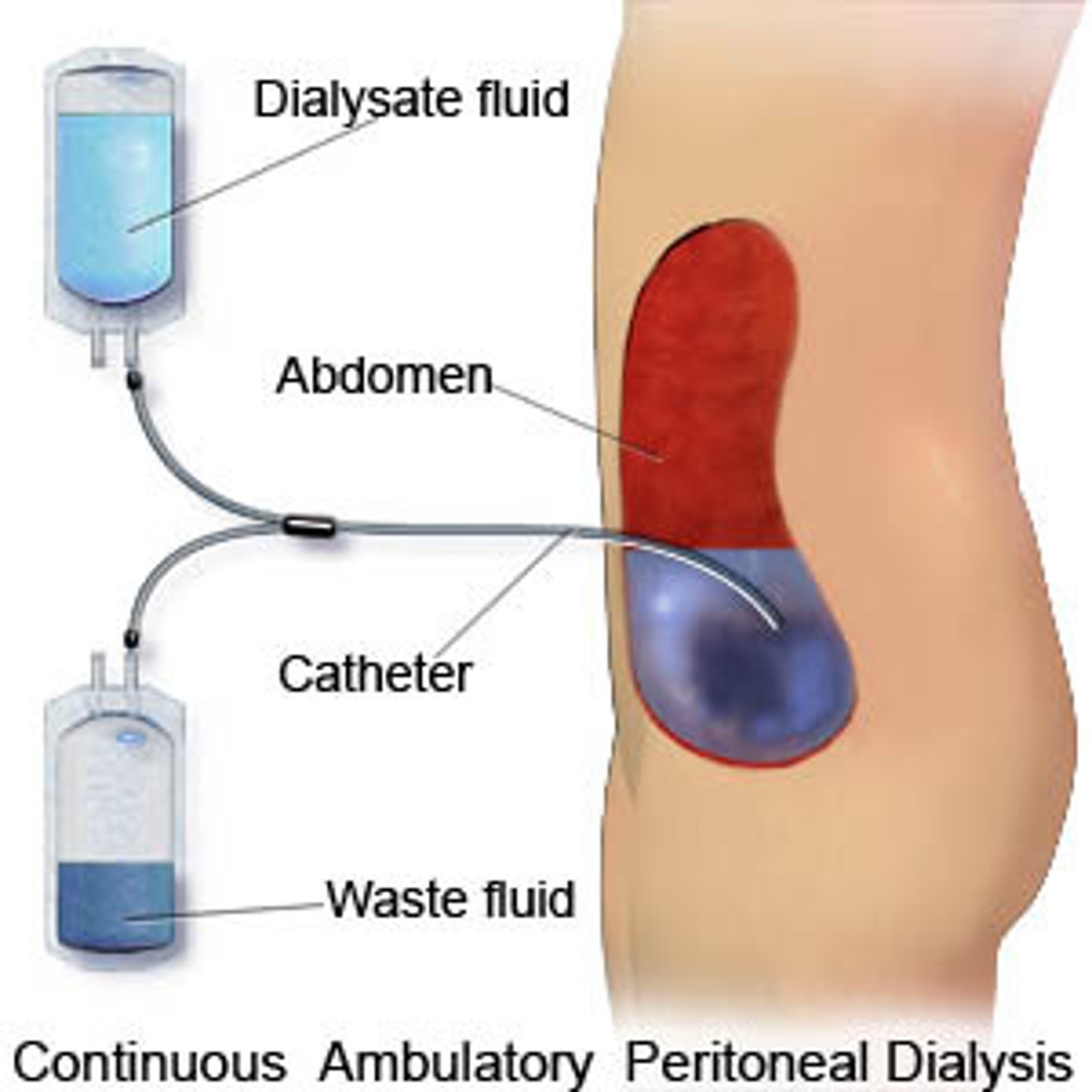
What are the 2 types of dialysis?
* Haemodialysis = blood leaves patient's body and flows into a dialysis machine
* Peritoneal dialysis = dialysis fluid is injected into body and then drained out (happens within the body)
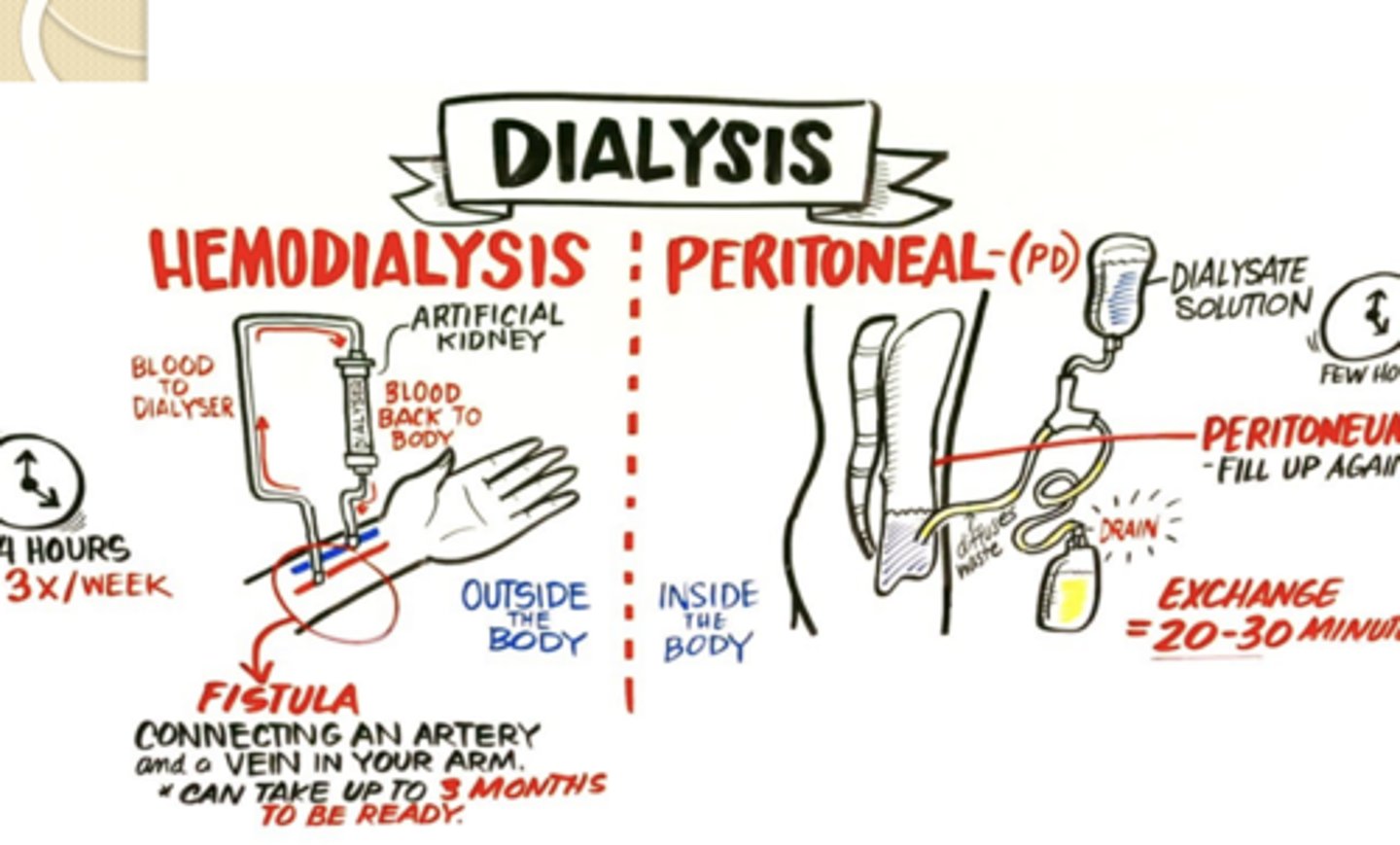
Adv and Disadv of Haemodialysis
A: Lower infection risk
A: Required less often
D: Must be done in hospital
D: Requires specialist equipment
Adv and Disadv of Peritoneal dialysis
A: Can be done at home
A: Can be mobile during it
D: Infection risk
D: Required often
Adv and Disadv of Kidney transplants
A: One off - no dialysis sessions
A: No diet monitoring
A: Improved QOL
D: Rejection risk
D: Donor shortage
D: Must take immunosuppressants