B5: Cell Bio Exam 2 Practice Q's
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
148 Terms
simple cuboidal epithelium
What type of epithelium lines the proximal convoluted tubule (PCT)?
simple cuboidal epithelium with a thick/tall microvilli brush border, glycocalyx
What is the histology of the proximal convoluted tubule (PCT)?
short sparse microvilli
What is the histology of the distal convoluted tubule (PCT)?
HCO3-, H2O, Na+, Cl- (bicarb, water, sodium, chloride), amino acids, and glucose
Which substances are reabsorbed in the proximal convoluted tubule (PCT)?
Hint: most things!
Hint hint: All Brackish Water has Salt and Sugar
creatinine, urea, H+
Which substances are secreted in the proximal convoluted tubule (PCT)?
Bowman’s capsule & thin descending loop of Henle
Which structures of the nephron are made of simple squamous epithelium?
both convoluted tubules (proximal and distal) & thick ascending loop of Henle
Which structures of the nephron are made of simple cuboidal epithelium?
Bowman’s capsule, proximal convoluted tubule, thin descending loop of Henle
Which structures of the nephron are permeable to water?
thick ascending loop of Henle and distal convoluted tubule
Which structures of the nephron are impermeable to water?
hint: if you thicc and far away, you getting no water
Na/K/ATPase, ENaC
aldosterone stimulates _____ and ______ on principal cells in the basolateral collecting duct
principal, basolateral
aldosterone stimulates Na/K/ATPase and ENaC on ______ cells in the ______ collecting duct
H+, Cl-
alpha intercalated cells of the collecting duct are responsible for secretion of:
HCO3-
beta intercalated cells of the collecting duct are responsible for secretion of:
HCO3-, K+
alpha intercalated cells of the collecting duct are responsible for reabsorption of:
H+
beta intercalated cells of the collecting duct are responsible for reabsorption of:
ENaC
potassium sparing diuretics block ______ in the apical collecting duct, leading to decreased Na+ resorption, H2O follows
apical
potassium sparing diuretics block ENaC in the _____ collecting duct
potassium sparing diuretics
amiloride and triamterene (and spironolactone!) are classified as:
ADH/vasopressin
_________ cause an increase in water resorption by acting on aquaporins on the basolateral membrane
basolateral
ADH/vasopressin cause an increase in water resorption by acting on aquaporins on the _______ membrane
reabsorption
_______ occurs from the lumen into the interstitium
transcellular
_____ reabsorption occurs via passive and active transport
paracellular
_____ reabsorption occurs via passive transport
hint: P & P
transcellular, paracellular
Water follows high solute concentration using ______ (AQP4) and _____ transport
reabsorbed, secreted
GFR may not be accurately reflected in the excreted urine if the substance is ______ or _______
inulin
What is the gold standard for measuring GFR, as clearance of this substance is equal to GFR?
it is freely filtered and neither reasorbed nor secreted
Why is inulin the gold standard for measuring GFR?
secreted into the renal tubules
If excretion of a substance is greater than amount filtered, it is being:
absorbed back into blood
If excretion of a substance is less than the amount filtered, it is being:
transporter-mediated diffusion
Glucose uses ________-________ ________ for filtration → as glucose increases, approaches transporter saturation causing increased excretion of glucose
increased excretion of glucose
Glucose uses transporter-mediated diffusion for filtration → as glucose increases, it approaches transporter saturation causing:
filtered
ID purple
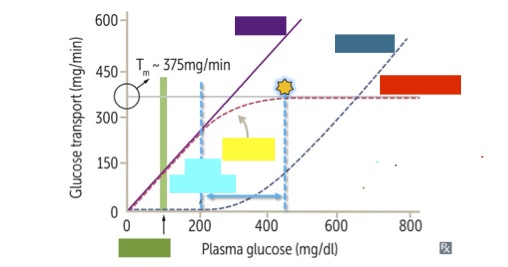
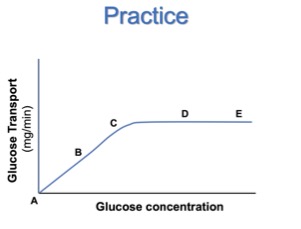
glucose transport graph
What is this graph representing?
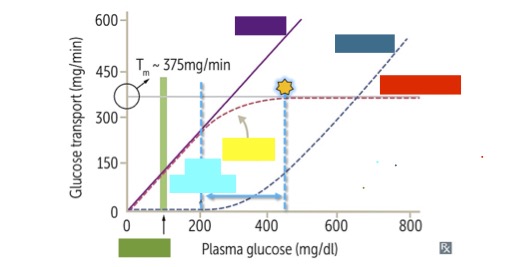
excreted
ID dark blue
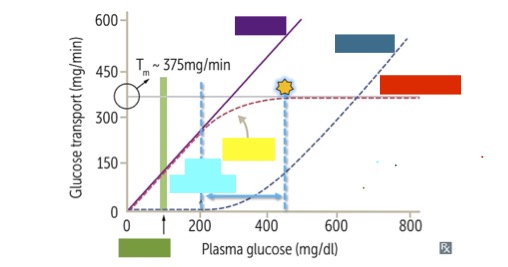
renal threshold
ID light blue
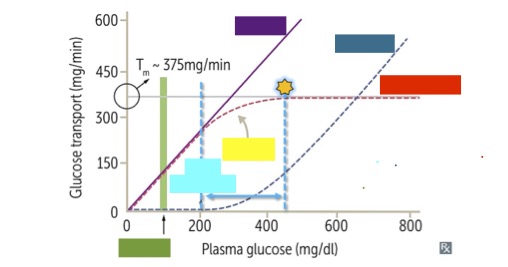
reabsorbed
ID red
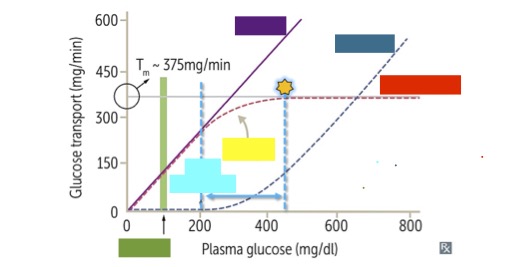
splay
ID yellow
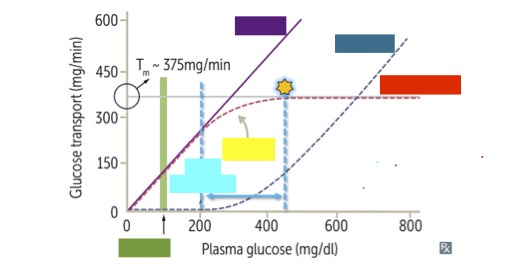
normal
ID green
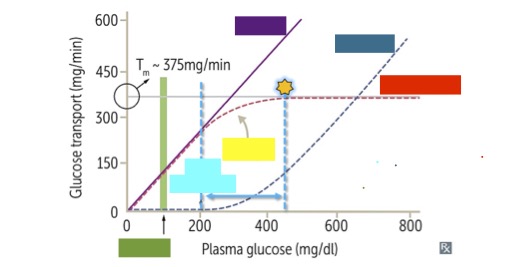
Tmax
_____ is the transport maximum of glucose, aka the maximum rate of glucose reabsorption as plasma glucose increases, at 375 mg/min
hyperglycemia
in ________, glucose exceeds the Tmax, therefore the remaining glucose that cannot be reabsorbed is excreted instead
glucosuria
In _______, the amount of glucose present in the urine depends on the reabsorption rate
PCT
Thin descending LOH
Bowman’s capsule
DCT
Thick ascending LOH
rank the parts of the nephron from most permeable to water to least permeable to water.
transport saturation graph
ID graph
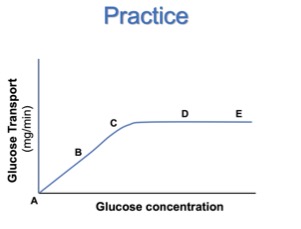
reabsorption
What does this curve represent?
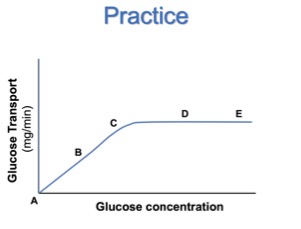
greatest rate of glucose filtration
ID E
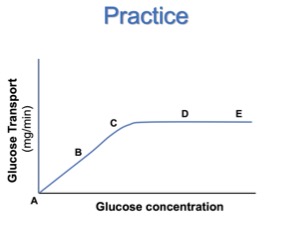
lowest glucose concentration where it starts appearing in the urine
ID C
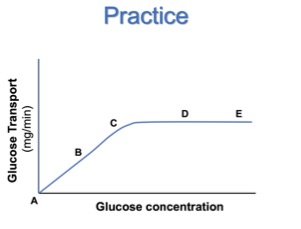
lowest plasma glucose level where you are reabsorbing at Tmax
ID D
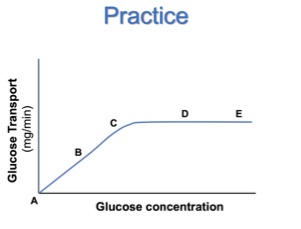
it is constant
What happens to the rate of glucose reabsorption as you move from D to E?
increases
What happens to the rate of glucose excretion as you move from D to E?
increases
What happens to the rate of glucose filtration as you move from A to B?
increases
What happens to the rate of glucose reabsorption as you move from A to B?
proximal convoluted tubule
Where is 65-80% of Na and H2O reabsorbed in the nephron?
thin descending LOH
Where is NO Na reabsorbed in the nephron because it is impermeable to Na?
thick ascending LOH
Where is 10-20% Na reabsorbed in the nephron?
distal convoluted tubule
Where is 5-10% Na reabsorbed in the nephron?
paracellular flux
In pulmonary edema, disruption of ________ _____ causes leakage of fluid/proteins into interstitial space → exacerbates edema
transcellular flux
In pulmonary edema, paracellular flux disruption plays a bigger role than ______ ___ disruption, destroying the gradient
endothelial damage
In pulmonary edema, Kf increases due to _______ ______ causing fluid/protein leakage → exacerbates edema
transcytosis, caveolae-mediated
Increased ______ and ________-_______ transport, causing fluid/protein leakage → exacerbates edema
furosemide
blocks NKCC on apical thick ascending LOH → can cause hypokalemia
hydrochlorothiazide
blocks Na/Cl symporter in DCT → can cause hyponatremia, hypokalemia, hypochlorhydria (the hypo-trio)
Acetazolamide
Carbonic anhydrase inhibitor in PCT → can cause hyponatremia, low bicarb, hypochlorhydria
ARBs
block AngII in apical PCT → cause decreased apical Na/H exchange
nephritic syndrome
inflammation of the glomerulus
-PSGN, IgA nephropathy
Hematuria (gross blood in urine)
Azotemia (increased waste in blood)
Casts (RBC’s in urine sediment)
3 symptoms of nephritic syndrome
nephrotic syndrome
derangement in glomerular capillary walls leading to increased permeability
-minmal change disease, FSGS, membranous nephropathy
Massive proteinuria (>3.5mg)
Hypoalbuminemia
Hyperlipidemia
3 symptoms of nephrotic syndrome
net filtration (+)
what happens in the afferent arteriole end of the glomerular capillary?
net reabsorption
what happens in the efferent arteriole end of the glomerular capillary?
autoregulation
First line of defense against MAP spikes = ________ for MAP within that range
60-140mmHg MAP
autoregulatory range
myogenic response
-CONSTRICTION ONLY
↑ arterial pressure → ↑ flow → vascular smooth muscle contraction → maintains normal flow
metabolic response
CONSTRICT AND DILATE – Tubuloglomerular Feedback
↑ flow/osmolarity = ↑ GFR leads to ATP released by macula densa → inhibition of RAAS → decreased GFR, increased Na excretion
↓ flow/osmolarity = ↓ GFR → NO & prostaglandins released by macula densa → stimulation of RAAS → increased GFR, decreased Na excretion
vasoconstriction in afferent arteriole
↓ RBF
↓ RPF
↓ GFR
-SNS activation, NSAIDs
vasodilation in afferent arteriole
↑ RBF
↑ RPF
↑ GFR
-CA or alpha-1 blockade
vasoconstriction in efferent arteriole
↓ RBF
↑ RPF
no change (or ↑) GFR
-RAAS activation (Ang II)
vasodilation in efferent arteriole
↑ RBF
↓ RPF
no change (or ↓) GFR
-ACEis and ARBs
norepinephrine, epinephrine, endothelin
these substances affect afferent vasoconstriction
eNOS, prostaglandins
these substances affect afferent vasodilation
𝑁𝐹𝑃 = 𝐾f (𝑃c −𝑃b −𝜋c)
net filtration pressure
𝐽v =𝐾f[(𝑃c−𝑃i)−𝜎(𝜋c −𝜋i)]
fluid flux
-if 𝐽v positive → filtration/flux out of capillary
-if 𝐽v negative → reabsorption/flux into capillary
filtration coefficient
𝐾f = 𝐿p ∗ 𝑆𝐴
-Lp = hydraulic conductivity
-SA = surface area
junctional integrity, ionic permissivity, tissue integrity, podocyte health/number
what factors affect hydraulic conductivity (Lp)?
diameter of capillaries, radius of filtration slits, disease (loss of tissue)
What factors affect surface area (SA)?
large size (heavy molecular weight) and negative charge
What factors reduce relative filterability?
(renal) clearance
𝐶𝑥 = ([U]x • V) / [Px] mL/min
Cx = clearance, [U] = urine concentration, V = urine volume/time, Px = plasma concentration
clearance
the rate at which a specific substance is removed and excreted in the urine
-used to measure GFR
-Inulin is GOLD STANDARD for measuring
-Creatinine is most commonly used clinically, tends to overestimate GFR by 10-20%
kidney
Only ______ extracts para-aminohippurate (PAH), so [RA]PAH = [RV]PAH in other organs
glomerular filtration rate
𝐺𝐹𝑅 = ([U]inulin • V) / [P]inulin
renal plasma flow in other organs
RPF = [U]PAH • V / [P]PAH
renal plasma flow in kidney
RPF = ([U]PAH • V) / ([RA]PAH - [RV]PAH)
filtration fraction
FF = GFR / RPF
inulin
filtration mechanics: filtration only
𝐹𝑖𝑙𝑡𝑒𝑟𝑒𝑑 𝐿𝑜𝑎𝑑 = 𝐺𝐹𝑅 (𝑚𝑙/𝑚𝑖𝑛) ∗ [𝑃]x (𝑚𝐸𝑞/𝑚𝐿)
𝐸𝑥𝑐𝑟𝑒𝑡𝑖𝑜𝑛 𝑅𝑎𝑡𝑒 → 𝐶x = 𝑈x ∗ 𝑉
𝑅𝑒𝑠𝑜𝑟𝑝𝑡𝑖𝑜𝑛 𝑜𝑟 𝑆𝑒𝑐𝑟𝑒𝑡𝑖𝑜𝑛 = (𝐺𝐹𝑅 ∗ 𝑃x)−(𝑈x ∗𝑉)
Na, K, Cl
filtration mechanics: filtration & partial reabsorption
𝐹𝑖𝑙𝑡𝑒𝑟𝑒𝑑 𝐿𝑜𝑎𝑑 = 𝐺𝐹𝑅 (𝑚𝑙/𝑚𝑖𝑛) ∗ [𝑃]x (𝑚𝐸𝑞/𝑚𝐿)
𝐸𝑥𝑐𝑟𝑒𝑡𝑖𝑜𝑛 𝑅𝑎𝑡𝑒 → 𝐶x = 𝑈x ∗ 𝑉
𝑅𝑒𝑠𝑜𝑟𝑝𝑡𝑖𝑜𝑛 𝑜𝑟 𝑆𝑒𝑐𝑟𝑒𝑡𝑖𝑜𝑛 = (𝐺𝐹𝑅 ∗ 𝑃x)−(𝑈x ∗𝑉)
glucose, bicarb
filtration mechanics: filtration & complete reabsorption
𝐹𝑖𝑙𝑡𝑒𝑟𝑒𝑑 𝐿𝑜𝑎𝑑 = 𝐺𝐹𝑅 (𝑚𝑙/𝑚𝑖𝑛) ∗ [𝑃]x (𝑚𝐸𝑞/𝑚𝐿)
𝐸𝑥𝑐𝑟𝑒𝑡𝑖𝑜𝑛 𝑅𝑎𝑡𝑒 → 𝐶x = 𝑈x ∗ 𝑉
𝑅𝑒𝑠𝑜𝑟𝑝𝑡𝑖𝑜𝑛 𝑜𝑟 𝑆𝑒𝑐𝑟𝑒𝑡𝑖𝑜𝑛 = (𝐺𝐹𝑅 ∗ 𝑃x)−(𝑈x ∗𝑉)
creatinine
filtration mechanics: filtration and secretion
𝐹𝑖𝑙𝑡𝑒𝑟𝑒𝑑 𝐿𝑜𝑎𝑑 = 𝐺𝐹𝑅 (𝑚𝑙/𝑚𝑖𝑛) ∗ [𝑃]x (𝑚𝐸𝑞/𝑚𝐿)
𝐸𝑥𝑐𝑟𝑒𝑡𝑖𝑜𝑛 𝑅𝑎𝑡𝑒 → 𝐶x = 𝑈x ∗ 𝑉
𝑅𝑒𝑠𝑜𝑟𝑝𝑡𝑖𝑜𝑛 𝑜𝑟 𝑆𝑒𝑐𝑟𝑒𝑡𝑖𝑜𝑛 = (𝐺𝐹𝑅 ∗ 𝑃x)−(𝑈x ∗𝑉)
renal plasma flow
𝑅𝑃𝐹 = ([U]PAH • V) / ([RA]PAH - [RV]PAH)
or
𝑅𝑃𝐹 = [U]PAH • V / [P]PAH
renal blood flow
𝑅𝐵𝐹 = 𝑅𝑃𝐹 / (1−𝐻𝑐𝑡)
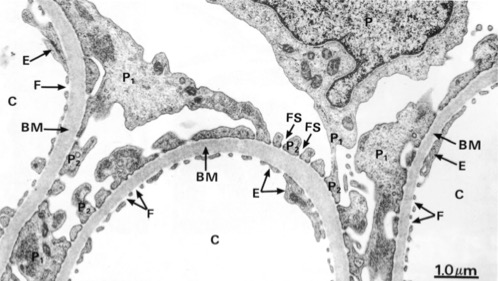
capillary
ID C
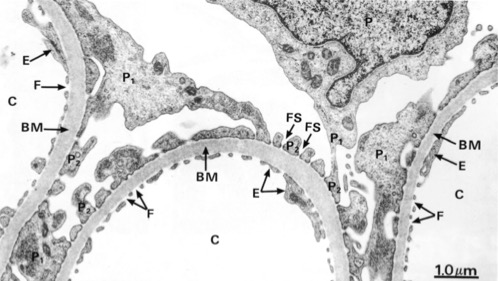
fenestrated endothelium
ID F