Clinical Actions of Specific Agents
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
LA Armamentarium in North America
1) Articaine (Septocaine) with 1:100,000 epinephrine (GOLD)
2) Articaine (Septocaine) with 1:200,000 epinephrine (SILVER)
3) Bupivacaine (Marcaine) with 1:200,000 epinephrine (BLUE)
4) Lidocaine (Xylocaine) with 1:100,000 epinephrine (RED)
5) Lidocaine (Xylocaine) with 1:50,000 epinephrine (GREEN)
6) Mepivacaine (Carbocaine, Polocaine) with 1:20,000 levonordefrin (BROWN)
7) Mepivacaine (Carbocaine, Polocaine) Plain (TAN)
8) Prilocaine (Citanest) with 1:200,000 epinephrine (YELLOW)
9) Prilocaine (Citanest) Plain (BLACK)
Procaine and propoxycaine were withdrawn from the United States market in January 1996
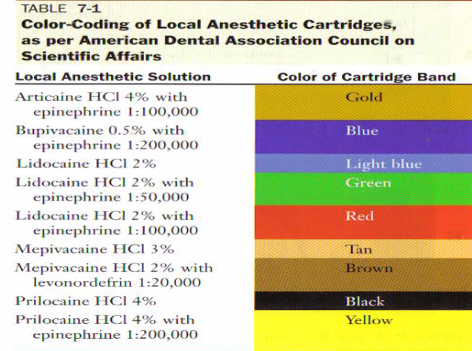
What we Have
• Articaine HCl
4% + epinephrine 1:100,000 (intermediate acting)
4% + epinephrine 1:200,000 (intermediate acting)
• Bupivacaine HCl
0.5% + epinephrine 1:200,000 (long acting)
• Lidocaine HCl
2% + epinephrine 1:50,000 (intermediate acting)
2% + epinephrine 1:100,000 (intermediate acting)
• Mepivacaine HCl
3% Plain (short acting)
2% + levonordefrin 1:20,000 (intermediate acting)
• Prilocaine HCl
4% Plain (short acting for infiltration; intermediate acting for block)
4% + epinephrine 1:200,000 (intermediate acting)
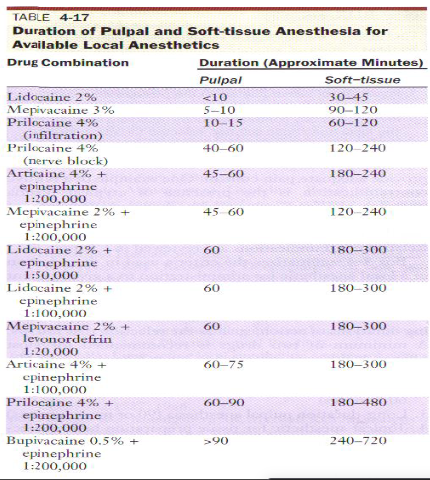
Duration of Action
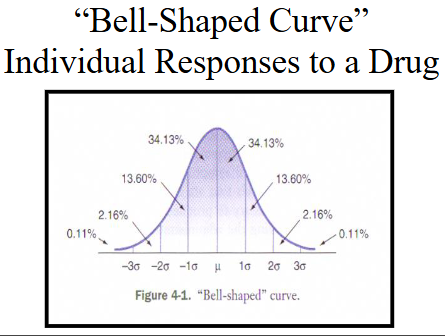
Duration of hard and soft tissue anesthesia is only an approximation; there are many factors that can prolong or decrease the level of anesthesia:
1) Individual response to the drug
-70% normal, 15% hyper-responders and 15% hypo-responders
2) Accuracy of deposition of the drug
-depositing the solution close to the nerve provides greater duration
3) Status of the tissues at the site of drug administration
-inflammation, infection and pain; vascularity of tissues
4) Anatomical variation
-height of mandibular foramen; width of ramus
-position of the palatal root
5) Type of injection administered
-block anesthesia vs. supraperiosteal injection
Maximum Doses of LA (MRD)
Doses of anesthetic drugs are presented in terms of:
Milligrams of drug per unit of body weight, either milligrams per kilogram or milligrams per pound (mg/kg or mg/lb)
Always minimize drug doses and use the smallest clinically effective dose for all individuals: normal, hyper, hypo-responders
MRDs
-The American Council on Dental Therapeutics of the ADA and The United States Pharmacopeial Convention (USP) no longer adjusts them for inclusion of a vasoconstrictor
-Changes in liver function, plasma protein binding, blood volume and other important physiological functions influence the manner in which local anesthetics are distributed and biotransformed in the body
-The half lives of amide local anesthetics are increased in the presence of decreased liver function or perfusion
-When the MRD is exceeded there is no guarantee that an overdose will occur, only that there is a greater likelihood of it arising; in hyper-responders, an overdose may occur under the MRD
The maximum calculated drug dose always should be decreasedi n medically compromised, debilitated, or elderly persons
“How do I determine the maximum recommended dose of each local anesthetic administered in clinical situations where more than one drug is necessary?”
Ensure that the total dose of both local anesthetics not exceed the lower of the two maximum doses for the individual agents
MRDs for Specific LA Agents
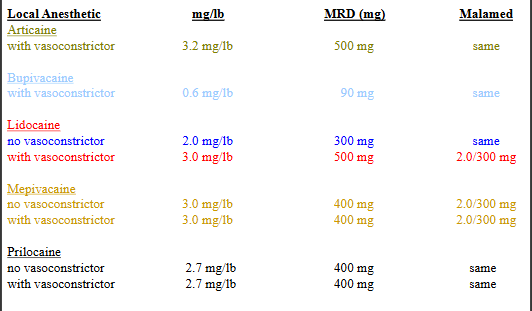
Calculations of Mg of LA per dental cartridge (1.8 mL)
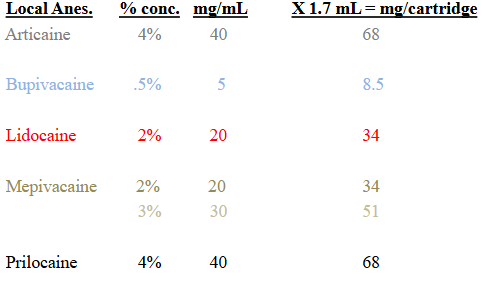
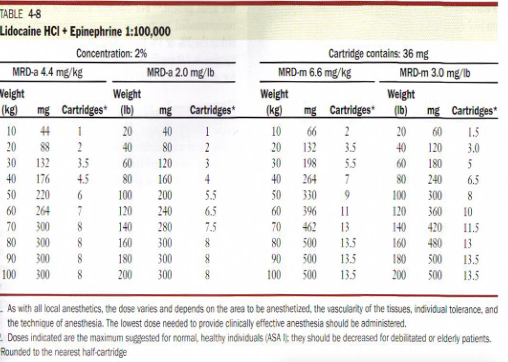
2% Lidocaine 1:100,000 epinephrine MRD
300 mg; that does not mean that anyone can have up to 300 mg; this number is based on a patient’s weight, therefore, a 80 lb. child cannot have 300 mg but instead:
80 lb. X 2.0 mg/lb. = 160 mg MRD
160 mg / 34 mg/ cartridge = 4.7 cartridges
MRD Examples
Patient: 22 year old, healthy, female 110 lbs.
Drug: Lidocaine 2% no vasoconstrictor = 34 mg/cartridge
MaximumRecommendedDose: 110 lbs. x 2.0 mg/lb = 220 mg
NumberofCartridges: 220 mg / 34 mg = 6.5 cartridges maximum
Patient: 6 year old, healthy, male 40 lbs.
Drug: Mepivacaine 3%Plain = 51 mg/cartridge
MaximumRecommendedDose: 40 lbs. x 2.0 mg/lb = 80 mg
NumberofCartridges: 80 mg / 51 mg = 1.6 cartridges maximum
Novocaine
procaine + propoxycaine
1903
Procaine
Ester
-hydrolyzed rapidly in plasma by plasma pseudocholinesterase
-excreted more than 2% unchanged in the urine; 90% as PABAand 8% as diethylaminoethanol
-pKa = 9.1; this is why the onset is very long
-pH of plain solution = 5.0 to 6.5
-pH of vasoconstrictor solution = 3.5 to 5.5
-onset of action = 6 to 10 minutes (very long by amide standards)
-effective dental concentration = 2% to 4%
-half-life = 6 minutes
-topical anesthetic action = none
-produces the greatest vasodilation of all current local anesthetics
the first synthetic injectable local anesthetic proprietary name of Novocain is known around the world
2% procaine plain provides essentially no pulpal anesthesia
provides 15 to 30 minutes of soft tissue anesthesia the short duration of action is due to its profound vasodilating effects its vasodilating properties are used to break arteriospasm metabolized in the blood by plasma cholinesterases hepatic dysfunction is not a problem with procaine
MRD = 1000 mg
pKa of 9.1 means slow onset which is why propoxycaine is added
Lidocaine
(*Xylocaine / Octocaine / Lignospan)
(Amide) (discovered 1943)
metabolized in the liver by microsomal fixed-function oxidases
by products are monoethylglyceine xylidide and glyceine xylidide produce sedationexcreted via the kidneys less than 10% unchanged more vasodilating than Prilocaine or Mepivacaine
pKa = 7.9
pH of plain solution = 6.5
pH of vasoconstrictor solution = 5.0 to 5.5
onset of action = 2 to 3 minutes (rapid)
effective dental concentration = 2%
anesthetic half-life = 90 minutes
-topical anesthetic action = yes; in 5% concentration
-MRD (vasoconstrictor-containing) = 3.2 mg/lb not to exceed 500 mg
-Malamed recommended MRD = 2.0 mg/lb not to exceed 300 mg
-1st amide local anesthetic to be marketed replacing Novocaine
-Lidocaine provides more rapid, more profound anesthesia, longer duration and greater potency than Procaine (Novocain)
-Allergy to amide local anesthetics is virtually nonexistent, although possible
-extremely rare allergy is a major advantage of amides over esters
-2% Lidocaine comes in plain, 1:50,000 epinephrine and 1:100,000 epinephrine
-only recommended use of 2% Lidocaine 1:50,000 epinephrine is toprovide hemostasis by injecting volumes directly into surgical site
-the MRD for epinephrine sensitive individuals is 40 micrograms(.04 mg) per appointment which is equivalent to 2 cartridges of1:100,000 epinephrine (each cartridge contains .018 mg epinephrine)
-the MRD for healthy individuals is .20 mg epinephrine per appointment (.018 mg/cartridge with 1:100,000 epinephrine X 11.1 cartridges = .20 mg epinephrine)
-2% Lidocaine with 1:50,000; 1:100,000; 1:200,000; 1:250,000epinephrine all provide the same depth/duration of soft/hard tissueanesthesia, however, not the same level of hemostasis
-1:50,000 epinephrine is not dangerous to most patients but can be tosome ASA II and ASA III patients and to the very young and elderly
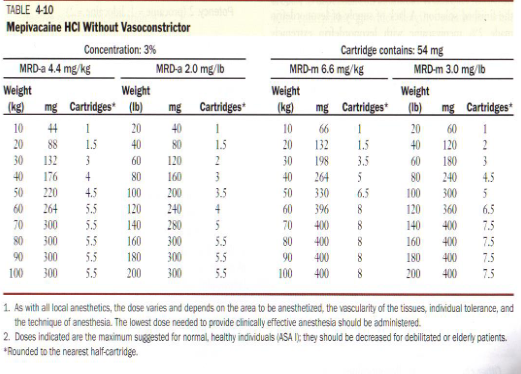
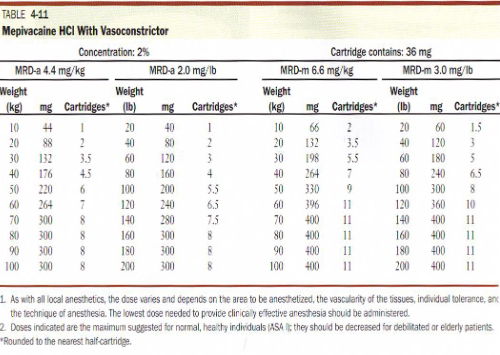
Mepivacain
(*Carbocaine / Polocaine / Isocaine / Scandonest)
(amide)
-metabolized in the liver by microsomal fixed-function oxidases
-hydroxylation and N-Demethylation play roles in the metabolism
-excreted via the kidneys 1% to 16% excreted unchanged
-produces only slight vasodilation (very important)
-produces pulpal anesthesia withouta vasoconstrictor of 20 to 40 minutes
-Lidocaine provides 5 minutes of pulpal anesthesia and Procaine 2 minutes of pulpal anesthesia without a vasoconstrictor
-pKa = 7.6 (faster onset than Lidocaine)*
-pH of plain solution = 4.5
-pH of vasoconstrictor solution = 3.0 to 3.5
-onset of action = 1.5 to 2 minutes (very rapid)
-effective dental concentration = 3% without vasoconstrictor2% with a vasoconstrictor
-anesthetic half-life = 1.9 hours
-MRD = 2.0 mg/lb; not to exceed 300 mg
-the mild vasodilating properties of Mepivacaine provide a longerduration of anesthesia than most other anesthetics when the drug isadministered without a vasoconstrictor
-Mepivacaine 3% Plain provides 20 to 40 minutes of pulpal anesthesia and 2 to 3 hours of soft tissue anesthesia
-Mepivacaine 3% Plain is indicated for patients in whom avasoconstrictor is contraindicated
-Mepivacaine 3% Plain is the most used local anesthetic for pediatric patients when the treating doctor is not a pediatric dentist
-true, documented, reproducible allergy to Mepivacaine, an amidelocal anesthetic, is virtually nonexistent
-two types of vasoconstrictors are used with Mepivacaine;1:20,000 levonordefrin and 1:100,000 epinephrine
Why is Mepivacaine used so often in children
1) pKa is 7.6 which allows for faster onset
2) Slight vasodilation so longer duration
3) 3% affords stronger anesthetic solution
Prilocaine (citanest)
Discovered 1953
-secondary amine
-hydrolyzed straight-forwardly by hepaticamidases into orthotoluidine and
N-Propylalanine is a major byproduct of Prilocaine biotransformation
-extremely small amount of Prilocaine isdetected in the urine
-orthotoluidine can induce the formation ofmethemoglobin
-methemoglobinemia occurs most often withPrilocaine
-Prilocaine consistently reduces the blood’s oxygen carrying capacity enough to produce observablecyanosis
-Limiting the total Prilocaine dose to 400 mg avoidsthis occurrence (4% cartridge = 68 mg / cartridge)(400 mg / 68 mg = 5.9 cartridges maximum)
-methemoglobin levels less than 20% do not produce clinicalsymptoms of cyanosis, i.e., blue lips and nail beds, respiratory distress
-methemoglobinemia can be reversed w/in 15 minutes by administering 1 to 2 mg/kg body weight of 1% methylene blue IV for 5 minutes
-Prilocaine undergoes biotransformation more rapidly and completelythan Lidocaine, taking place in the liver, kidney and lung
-plasma levels of Prilocaine decrease more rapidly than Lidocaine dueto the massive biotransformation thus it is considered less toxic thanother more potent amides
-Prilocaine CNS toxicity is more brief and less severe than Lidocaine
toxicity
-Prilocaine is excreted via the kidneys more rapidly than other amides
-Prilocaine causes vasodilation; albeit less than Lidocaine
-pKa = 7.9 (same as Lidocaine)
-pH of plain solution = 4.5
-pH of vasoconstrictor containing solution = 3.0 to 4.0
-onset of action = 2 to 4 minutes (slightly slower than Lidocaine)
-effective dental concentration = 4%
-half-life = 1.6 hours
-topical anesthetic activity = none (except EMLA- prilocaine + lidocaine)
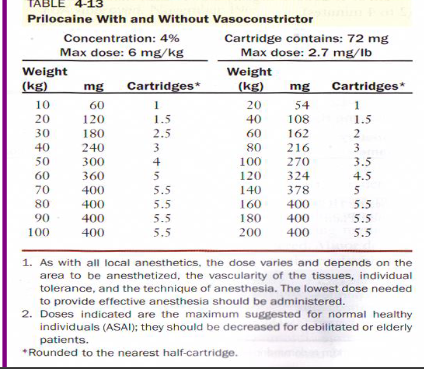
-MRD = 2.7 mg/lb; 400 mg total
-Prilocaine Plain is able to provide anesthesia that is equal in durationto Lidocaine with a vasoconstrictor (nerve block)
-Prilocaine Plain provides 10 to 15 minutes of pulpal anesthesia and1.5 to 2 hours soft tissue anesthesia when given as supraperiosteal
-*Prilocaine Plain provides 60 minutes of pulpal anesthesia and 2 to 4hours soft tissue anesthesia when given as regional nerve block
-epinephrine sensitive patients requiring prolonged pulpal anesthesia(greater than 60 minutes) should receive Prilocaine Plain orPrilocaine 1:200,000 epinephrine (.09 mg epinephrine/cartridge)
-rapid biotransformation makes Prilocaine a relatively safe amide
Prilocaine is relatively contraindicated in patients with idiopathic or congenital methemoglobinemia, sickle cell anemia, anemias and hypoxias
Articaine
(*Septocaine / Articadent / Zorcaine /Orabloc)
Discovered 1969
-1.5 times more potent than Lidocaine
-Articaine is the only amide that contains a thiophene group
-Articaine is the only amide that contains an ester group
-Articaine biotransformation occurs in the plasma and liver degradation of Articaine by hydrolysis of the carboxylic acid ester groups to give free carboxylic acid
excretion via the kidneys with 5% to 10% unchanged
Articaine has vasodilating effects equal to that of Lidocaine
pKa = 7.8; faster onset than Lidocaine
pH of plain solution = not available
-pH of vasoconstricting solution = 4.4 to 5.2
-onset of action = 1 to 3 minutes
-effective dental concentration = 4%
-Half-life = .5 hours*
-topical anesthetic action = none
-topical anesthetic action = none
-MRD = 3.2 mg/lb; 500 mg total
(68 mg per 4% cartridge / 500 =7.4 cartridges maximum)
-Articaine is becoming the most popular amide local anesthetic in countries other than the United States
-Articaine holds 26% of the United States amide local anesthetic sales
-reports of paresthesia have become frequent in the United States
-Articaine and Prilocaine have been associated with reports of parasthesia; they are the only amides with 4% concentrations
-no cases of methemoglobinemia have been reported when Articainehas been used in the normal course of dental anesthesia
-use in children under 4 years of age is not recommended until furtherdata is analyzed about its safety
“minimum contents of each 1.7 mL” which is printed on eachcartridge of Articaine is there only to show that local anestheticcartridges are filled on a conveyor belt by a machine and cannot guarantee that there is 1.8 mL in each cartridge; consider all these cartridges to contain 1.8 mL not 1.7 mL as written on the cartridge by the manufacturer
Local anesthetics linger in the pulp cells of developing permanent teeth for hours after administration and reduced the levels of a protein critical to cell division
Local anesthetics may sometimes lead to the developmental failure of growing permanent teeth
Local anesthetics remained in high concentrations even 16 hours after injection
At low concentration and short time exposure, tooth pulp cells appeared to be able to adapt themselves, but eventually the 'protection mechanism' collapsed if they 'suffered' too long under too high concentration of the drugs
Bupivacaine
(*Marcaine / Vivacaine)
Discovered 1957
-potency = 4 times that of Lidocaine, Mepivacaine or Prilocaine
-toxicity = less than four times that of Lidocaine, Mepivacaine, or Prilocaine
-metabolized in the liver by amidases
-excretion via the kidney; 16% unchanged in urine
-great vasodilating effects; greater than Lidocaine, Mepivacaine and Prilocaine
-pKa = 8.1 (causes longer onset of action)
-pH of plain solution = 4.5 to 6.0
-pH of vasoconstrictor containing solution =3.0 to 4.5
-onset of action = 6 to 10 minutes (much longer than other amides)
-effective dental concentration = 0.5%
-half-life = 2.7 hours
-topical anesthetic action = none
-MRD = 0.6 mg/lb; 90 mg total
(8.5 mg per .5% cartridge / 90 = 10.6 cartridges maximum)
2 Utilizations in Dentistry:
1) lengthy dental procedure where pulpal anesthesia is necessary in excess of 90minutes
2) management of post-operative pain(post-surgical)
-post-operative need for narcoticslessened when you use Bupivacaine; rarely used in children or mentally handicapped
Kovanaze
Nasal spray indicated for regional anesthesia when performing
a restorative procedure on teeth 4-13 and A-J in adults and
children who weigh 40kg (88 lbs.) or more

Topical anesthetics
-topically applied local anesthetic is an important part of atraumatic needle penetration in the oral mucosa; numbs 2 to 3 mm deep
-topical anesthetic concentration is greater than injectable local concentration
-higher concentrations facilitate diffusion through mucous membranes
-topical anesthetics do not contain vasoconstrictors so absorption into the blood stream could be quite rapid
-do not inject topical anesthetics
-Examples: Benzocaine, Butamben, Tetracaine HCl, Cocaine, Dyclonine HCl, and Lidocaine (5% concentration)
-topical anesthetic gel must remain on tissue for at least 1 minute
Eutectic mixture of local anesthetic (EMLA)
-composed of Lidocaine 2.5% and Prilocaine 2.5%
-cream is an emulsion in which the oil phase is a eutectic mixture of Lidocaine and Prilocaine in a ratio of 1:1
-designed to have topical powers on intact skin (venipuncture)
-must be applied 1 hour before the procedure
-patients with a history of methemoglobinemia are contraindicated
-Has eliminated use of a needle in some pediatric procedures
-promising for the future of topical pain resolution in all facets of medicine and dentistry
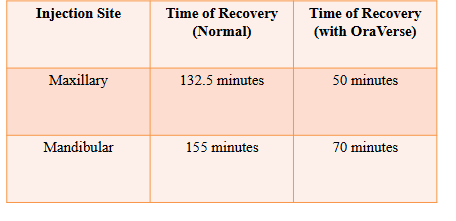
OraVerse (Phentolamine Mesylate)
Alpha adrenergic receptor agonist used for reversal of local anesthesia
Also used for diagnosis and treatment of Pheochromocytoma and Erectile Dysfunction (ED)
Antagonizes Alpha-1 & Alpha-2 receptors which blocks the action of circulating epinephrine and norepinephrine and also stimulates the Beta receptors in the heart and lung (vasodilation)
Each 1.7 mL cartridge contains 0.4 mg of phentolamine mesylate which is about 1/30 the concentration used in medicine
Recommended dose is based on the number of local anesthetic cartridges administered to the patient (up to 2 cartridges)
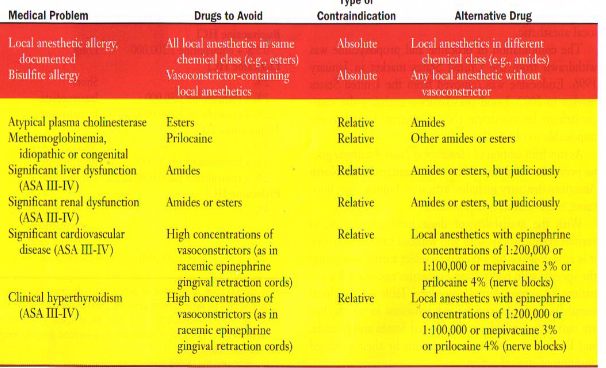
Contraindications
Not recommended for children under age 6 or weighing less than 33 pounds
Caution recommended for patients with cardiovascular disease- can cause tachycardia and cardiac arrhythmias
Consider these points when selecting an anesthetic
1) Length of the procedure; amount of time pain control is necessary
2) The need for post-treatment pain control
3) The need for hemostasis
4) Contraindications of the local anesthetic
Long appointment: .5% Bupivacaine
Intermediate appointment: 2% Lidocaine 1:100,000 epinephrine
Short appointment: 3% Mepivacaine or 4% Prilocaine
Hemostasis recommended: 1:50,000 epinephrine (only used for hemostasis)
Absolute contraindication: true, documented, reproducible allergy
*Short, intermediate and long-action amide local + topical is needed for every dental practice
Contraindications for LA