bio 224 exam 3
1/81
Earn XP
Description and Tags
digestive system
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
82 Terms
functions of the digestive system (6 items)
ingestion- eating/drinking something
mechanical digestion- does not change what the substance is, but just breaks it into smaller pieces.
Increases the surface area of food so chemical digestion occurs faster.
Includes chewing (also known as mastication), grinding, & churning
chemical digestion- breaking chemical bonds. Makes big molecules into smaller molecules. This actually changes what the substance is
secretion- the job of the accessory organs. Don’t move, but spit on food as it passes by
absorption- the movement of nutrient molecules thru the digestive wall into the blood or lymph
excretion/defecation- getting rid of the waste that couldn’t be absorbed or used
digestive organs & their mucosa (5 items)
(hint: there are mainly 2 types of mucosa for these organs, just know what differentiates the last 3 organs from each other!)
Food passes thru these
oral cavity (strat. squam epi.)
esophagus (strat. squam epi.)
stomach (simp. col. epi / gastric pits)
small intestine (simp. col. epi / plicae / villi / microvilli)
large intestine (simp. col. epi / goblet cells everywhere)
accessory organs (3 items)
These don’t touch the food but secrete on it as it passes by
salivary glands
liver
pancreas
layers of the digestive wall (from inner to outer) (4 layers)
includes definitions of MALT, Peristalsis, Myenteric plexus, & mesenteries
Mucosa- lots of epithelium & touches the food. Modified by the organ (mucosal modifications)
has MALT (mucosa associated lymphoid tissue), which is a lymphoid nodule
Submucosa- areolar conn. tissue. Has blood, lymphatic vessels, & glands
Muscularis externa: smooth muscle
has longitudinal layer & circular layer
Peristalsis- circular & longitudinal contractions. This is how we move food thru these organs.
Myenteric plexus- division of the ANS (works on its own). Aids in control of digestion by controlling the smooth muscle
Serosa- serous membrane. abdomen (peritoneum). These sheets of serous membrane help hold the organs in place
Mesenteries- layers of serous membrane
peritonitis
inflammation of peritoneum. Common cause of death after abdominal surgery
oral cavity (what 3 parts does it include?)
Includes…
hard palate- has bone & allows us to breathe while chewing
soft palate- has no bone
Uvula- end of the soft palate
Substances that make up teeth (3 substances)
Define odontoblasts
enamel- crystalized calcium phosphate. Noncellular & made of dead cells, so it can’t repair itself
dentin- like bone but harder (more hydroxyapatite). NONCELLULAR
Odontoblasts- cells that make dentin. Nucleus in pulp cavity with the “arms” in dentin
cementum- like mortar (dry glue) between bricks. anchors the tooth
Types of teeth (from front to back) (3 types)
incisors- the teeth we cut with.
canines- the “tearing” teeth. Strongly rooted into gums in order to tear with them
molars- grinding/chewing teeth
3rd molars (wisdom teeth)- can cause issues if not removed for most people (depends on the size of teeth or size of mouth)
The mucosa of the oral cavity is what type of tissue?
stratified squamous epithelium
vestibule
the area between the lips & teeth
bolus
the chewed up food that you swallow
Swallowing (aka deglutition) (location & phases)
Takes place between the oral cavity & esophagus
Phases of swallowing (it’s based on where the food is located)
Voluntary phase- can be controlled. Use the tongue to shove bolus to pharynx. (Voluntary because you can still spit out the bolus)
Pharyngeal phase- move the bolus into the esophagus
Esophageal phase- has peristaltic waves. Longest phase due to the long tube (the esophagus)
Esophagus
Has smooth musc. & its mucosa is strat. squam. epi
10 inches long with the top third (3 inches) having skeletal muscle
this allows us to cough stuff out after entering the esophageal phase
Known as the “bolus transport tube” as it takes abt 10 seconds for the bolus to travel to the stomach
chyme
a more liquid form of bolus. Allows for more surface area. This is what bolus becomes when it enters the stomach
Stomach
know its function, the sphincters, what’s special about its muscularis externa, & rugae
Function: changes bolus into chyme
bolus enters the stomach & leaves as chyme
Smooth muscle sphincters:
Gastroesophageal (cardiac) sphincter- guards the entrance into the stomach
Pyloric sphincter- guards the exit from the stomach
The stomach’s muscularis externa has an extra layer known as the inner oblique area.
this is the only digestive organ with this extra layer
Rugae- folds in the organ’s wall that allow it to expand up to about 1 liter (on average for a normal stomach)
Can expand more thru training, as seen with competitive eaters
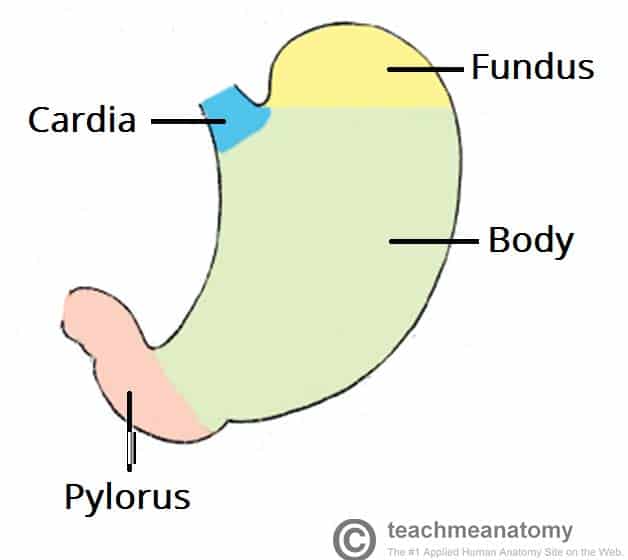
Stomach’s regions
Fundus- the top, dome-shaped part
Cardia region- where the bolus comes in
Body region- the largest, main area of the stomach
Pylorus- end of stomach
Stomach’s mucosa
Know the gastric pit & each type of glandular cell
Stomach’s mucosa is simple columnar epithelium
Gastric pit- permanent pits (inward projections). Very deep & narrow. The stomach is the only one w/ gastric pits
different from rugae bc rugae is much larger
Glandular cells- what the cells turn into at the bottom part of the gastric pit
parietal cells- make stomach acid (HCl)
chief cells- make digestive enzyme, pepsinogen
endocrine cells- make hormones
GERD
gastroesophageal reflux disease.
Stomach contents leak backwards into the esophagus
Includes stomach acid from parietal cells
small intestine & its mucosa
List the sections, its length, function, & the definition of plicae
largest digestive organ (despite the name…)
“small” comes from this having a 1” diameter
mucosa: simple columnar epithelium
Sections:
duodenum - abt 1 ft long
jejunum - abt 8 ft long
ileum - abt 12 ft long (remember e for eat to not confuse it with the ilium bone)
This organ is about 21 ft long while relaxed & 15-16ft long while still alive (bc different sections are contracted)
Plicae- circular, permanent folds inside the small intestine. This is the part that looks wavy on the inside of the small intestine. (think of this as the wavy carpet)
Villi- small, finger-like projections on plicae. Think of this as the carpet fibers
Inside, villi have a cardiovascular capillary & lacteal (lymphatic capillary) for absorption
Microvilli- small, finger-like projections on simple columnar epithelium
This organ deals with ABSORPTION
has large surface area (thanks to folds & villi & microvilli) to do absorption as quickly as possible
What are the accessory organs to the small intestine?
liver & pancreas
Where are the liver, pancreas, & gallbladder located?
Near the small intestine. They’re accessory to the duodenum
In order from superior to inferior:
Liver
Gallbladder
Pancreas
Large intestine
Know its length, function, mucosa, & structures (4 total)
2.5” diameter & 5 ft long
Function: change chyme into feces by pulling water out of chyme. DEHYDRATES THE CHYME
If done too quickly, results in diarrhea (too much water remaining in feces) (watery feces)
If done too slowly, results in constipation (too much water removed from feces)
Mucosa: simple columnar epithelium with LOTS OF GOBLET CELLS “gobs of goblets”
Ileocecal valve- found in lower-right quadrant of abdomen. Sphincter guards the exit from ileum & entrance into colon (large intestine)
Cecum- the “dead end pouch”
if chyme moves up, it continues along the digestive tract. If it moves down, it reaches a dead end into the cecum
Some organisms have multiple of this, but we only have one.
Appendix- hangs off of the cecum
function is mainly unknown since it can be cut out with basically no issues
If inflamed, it can swell & rupture (extremely dangerous!)
Taeniae coli- 3 striped on large intestine. Longitudinal muscle that helps move chyme (becomes harder to move as it becomes dry)
Pulling causes puckered appearance & forms pouches called haustrum
appendicitis
inflammation of the appendix. Can swell & rupture. 50% chance of death when this occurs
Treatment= cut it out
Path of chyme through the large intestine (5 parts)
as chyme moves on this path, it becomes more dry & harder to move
ascending colon
transverse colon
descending colon
sigmoid colon
rectum
enzymes
these are proteins
These are “divas” because they’re picky about how they function (ex. need specific temperature & pH to function)
Some enzymes require coenzymes/vitamins in order to function properly
Other examples of what they may require are proenzymes & the presence of metals (ex. Fe or Zn)
We need enzymes to break polymers into monomers because we can only absorb monomers!!
Enzymes perform chemical digestion by using water to split polymers
If we don’t have a specific enzyme for a food molecule, then we can’t do anything with it.
This is why we can only break down some polysaccharides, proteins, etc.
ex. we can’t break down a plant’s cell wall because we don’t have enzymes for it
vitamins
these are coenzymes. Some enzymes require vitamins/coenzymes to be present in order to function
Hydrolysis
lyse something by adding water to it.
this is NOT dissolving!!!
This is carried out by hydrolase enzymes (our digestive enzymes)
Digestive enzymes that deal with CARBOHYDRATES (3 total)
Name?
Where is it made?
Where does it work?
What’s the reaction it makes happen?
Salivary amylase- salivary glands; oral cavity; breaks polysaccharides into smaller polysaccharides
Pancreatic amylase- pancreatic juice; small intestine; breaks polysaccharides into smaller polysaccharides
Maltase, sucrase, lactase- intestinal brush border (microvilli); small intestine; breaks smaller polysaccharides into monosaccharides
Digestive enzymes that deal with PROTEINS (5 total)
Name?
Where is it made?
Where does it work?
What’s the reaction it makes happen?
Pepsin- chief cells of gastric cells (secreted as prescursor pepsinogen); stomach; changes proteins into polypeptides & smaller polypeptides
this is the 1st enzyme to make polypeptides into smaller polypeptides
Trypsin- pancreatic juice; small intestine; changes small polypeptides into smaller polypeptides (activates itself & other pancreatic enzymes)
Chymotrypsin- pancreatic juice; small intestine; changes small polypeptides into smaller polypeptides
Carboxypeptidase- pancreatic juice; small intestine; changes small polypeptides into smaller polypeptides
Dipeptidase & tripeptidase- intestinal brush border (microvilli); small intestine; breaks small polypeptides into amino acids
Digestive enzymes that deal with LIPIDS (2 total)
Name?
Where is it made?
Where does it work?
What’s the reaction it makes happen?
Gastric lipase- gastric glands; stomach; breaks triglycerides into free fatty acids & diglycerides
Pancreatic lipase- pancreatic juice; small intestine; breaks triglycerides into free fatty acids & monoglycerides
Digestive enzymes that deal with NUCLEIC ACIDS (DNA/RNA) (1 total)
Name?
Where is it made?
Where does it work?
What’s the reaction it makes happen?
Nucleases- pancreatic juice; small intestine; breaks nucleic acids into nitrogenous bases & simple sugars
Digestive enzymes in the ORAL CAVITY
CARBS
polysaccharides —salivary amylase→ smaller polysaccharides
PROTEINS
none
LIPIDS
none
NUCLEIC ACIDS
none
Digestive enzymes in the ESOPHAGUS
trick question! none for the esophagus :)
Digestive enzymes in the STOMACH (hint: only 2)
CARBS
none
PROTEINS
proteins —pepsin→ polypeptides & smaller polypeptides
LIPIDS
triglycerides —gastric lipase→ free fatty acids & diglycerides
NUCLEIC ACIDS
none
Digestive enzymes in the SMALL INTESTINE (hint: there are 8)
CARBS
some polysaccharides —pancreatic amylase→ smaller polysaccharides
maltose, sucrose, & lactose —maltase, sucrase, & lactase→ monosaccharides
PROTEINS
small polypeptides —trypsin, chymotrypsin, & carboxypeptidase→ smaller peptides
dipeptides & tripeptides —dipeptidase & tripeptidase→ amino acids
LIPIDS
triglycerides —pancreatic lipase→ free fatty acids & monoglycerides
NUCLEIC ACIDS
nucleic acids —nuclease→ nitrogenous bases & simple sugars
Digestive enzymes in the LARGE INTESTINE
trick question! none for the large intestine :)
How do we make stomach acid?
Parietal cells in the gastric pit produce HCl (stomach acid). These pump out H+ (hydrogen ions)
Stomach acid is made to change pepsinogen to pepsin
Parietal cells get this H+ thru this equation:
CO2 + H2O → H2CO3 → H+ + HCO3-
the H+ gets pumped out & helps lower pH to 1.5 or 2 to activate pepsin
The problem with lipids (includes definition of emulsified & micelle)
The issue is that lipids can’t be efficiently digested/hydrolyzed until they have been emulsified
emulsified= forced to be in little globs (separated)
Remember, lipids are “snobs” because they only get along with other lipids
Once you stop forcing lipids to be separated, they’ll get together again
We use bile or bile salts (from the liver) to emulsify lipids
remember, liver is accessory to the small intestine
Micelle- a lipid droplet surrounded by bile salts
Dual roles of the liver
Makes bile salts
to emulsify lipids
Detoxifies blood
hepatic portal vein- collects blood from abdominal, digestive organs & goes to the liver.
done to get rid of toxins before sending blood back to general circulation.
tissue in liver is set up with hexagon-shaped cells with a central vein in the middle
Has a trio of vessels on each corner (known as the portal triad)
hepatic arteriole- carries blood up
hepatic portal vein- carries blood up
bile duct- carries bile down
hepatic portal blood & arterial blood will meet & mix on their way to the central vein. Clears out toxins as they pass thru hepatic sinusoids since they’re beside hepatocytes
Dual roles of the pancreas
Make & deliver enzymes
Neutralize the acidic chyme
In other words, inc. its pH
duodenum can’t handle the low pH from stomach acid
uses bicarbonates & shoots it down the duct to neutralize the acidic chyme
Uses same chemical equation as the one to disguise CO2 & make stomach acid
Pancreatic acini cells make the enzymes & bicarbonates
Control of some basic digestive processes (what is it controlled by?)
Controlled by…
Nervous system (ANS Myenteric)
Endocrine system (hormones)
3 phases of digestion (gastric/stomach secretion)
Cephalic phase- takes place in the head. “food is on the way.” Prepares you for food
Triggered by sight, smell, or taste of food (it’s not in your stomach!)
Endocrine cells release gastrin to produce more stomach acid & more stomach churning
Gastric phase- takes place in the stomach. “food is here”
Activated when the bolus arrives in the stomach
MORE GASTRIN!!
Intestinal phase- takes place in the intestines. “food is leaving”
starts when the chyme enters the duodenum
Releases 3 hormones:
Secretin- stimulates secretion from pancreas & liver
Gastric Inhibitory Peptide (GIP)- inhibits acid secretion. slows down stomach activity
CCK (cholecystokinin)- stimulates secretion from pancreas & liver
when CCK hits the gallbladder, it will squeeze the gallbladder (the gallbladder holds bile)
absorption of carbs, proteins, & lipids (includes the definition of a chylomicron)
To get absorbed, must move from chyme to blood or lymph
carbs & proteins: moves into blood. done by pumping monomers into the intestinal cell, then they diffuse out of the cell into blood
Lipids: moves into lymph. Gets into intestinal cell by having micelle separate since bile salts are large proteins that can’t enter the intestinal cell. Bile salts stay left behind
Lipids (the glycerol + fatty acids) enter/diffuse into the intestinal cell easily because the cell membrane is made of lipids
These free lipids attach back together inside the intestinal cell
Throws new proteins (not bile salts) to surround the lipid to form a chylomicron. Gets spit out by exocytosis to enter lacteal
don’t confuse the chylomicron with a micelle!
The micelle has had the lipid hydrolyzed & kept apart thru bile salts
The chylomicron has lipids not separated & surrounded by different proteins
Absorption sites for various chemicals (stomach & large intestine & what they absorb. Everything else would be absorbed in the small intestine)
Absorption occurs in areas other than the small intestine, but not much.
Stomach absorbs…
around 20% ethanol (alcohol from grain, fruit, etc. safer alcohol unlike methanol (wood alcohol)) (as long as there aren’t many lipids present)
a few drugs
Large intestine absorbs…
water
potassium
sodium
a few vitamins or coenzymes
Defecation
Know the definitions for feces & distention (as well as the reflex it causes)
Feces- chyme after pulling out water, nutrients, etc
Distention- feces pushing against the wall once it reaches the rectum
Causes reflex where the rectum & end of the colon contract (do peristalsis) & internal anal sphincter relaxes (opens). The external anal sphincter closes
internal anal sphincter is smooth muscle (involuntary)
External anal sphincter is skeletal muscle (voluntary)
Short loop to spinal cord & back triggers this reflex. The long loop makes you aware of the control of defecation
Action of digestive hormones (site of production: stomach) (only 1)
Gastrin- inc. acid secretion
Action of digestive hormones (site of production: intestines) (only 3)
Cholecystokinin (CCK)- stimulate secretion from pancreas & liver; cause the gallbladder to release bile
Gastric inhibitory peptide- inhibits acid secretion
Secretin- stimulates secretion from pancreas & liver
emesis
Stomach contents move backwards. also known as vomiting.
peptic ulcers
an open sore on the inner lining of the stomach & the upper part of the small intestine
fecal transplant
transferring feces from a healthy donor to introduce them into a patient’s gastrointestinal tract. This is done to help introduce healthy bacteria, which can help control C. diff.
hepatitis
inflammation of the liver
cirrhosis
liver disease. It’s permanent scarring that damages the liver.
colitis
inflammation of the large intestine (colon)
pancreatitis
inflammation of the pancreas
pyloric stenosis
a hardened pyloric sphincter, the stomach’s exit
This narrows the exit, making it difficult for food to move into the intestines
metabolism
the grand total of ALL chemical reactions in the body
anabolic vs. catabolic
Anabolic- putting smaller molecules together to build/make a larger one
Catabolic- breaking larger molecules into smaller ones
Cell metabolism/respiration
Usually refers to the catabolism of nutrient molecules to use energy released to make/anabolize ATP
glucose using energy to make new ATPs
Our cells use ATPs for energy. It’s the “energy currency” for our cells
Uses adenosine & 3 phosphates connected thru high energy phosphate bonds
aerobic vs. anaerobic
anaerobic- oxygen is not required. Produces less ATP
aerobic- oxygen is required. Produces more ATP
Phosphorylation
adding phosphates
substrate level phosphorylation vs. oxidative phosphorylation
substrate level phosphorylation- a simple transfer/handoff of phosphate from one molecule to another.
Occurs in glycolysis & Kreb’s
Easy to do
oxidative phosphorylation- happens in the electron transport system. Needs high energy electrons, membranes, proteins, & O2 (the final electron acceptor)
Uses the energy from high energy electrons to attach phosphates
Harder due to needing more stuff, but this also pays more ATPs
Glycolysis
Know where it occurs & what chemicals enter & exit it.
Occurs in the cytoplasm
Enters: 1 glucose
Exits: 2 pyruvate, 2 ATPs, & 2 NADH
Substrate level phosphorylation
Cells without a mitochondria can only do glycolysis (lower pay rate in ATPs)
Conversion
Know where it occurs & what chemicals enter & exit it
Occurs in the mitochondria
Enters: 2 pyruvates
Exits: 2 acetyl CoA, 2 CO2, & 2 NADH
This is where the CO2 we need to exhale comes from
Citric Acid (Kreb’s) Cycle
Know where it occurs & what chemicals enter & exit it
Occurs in the mitochondria
Enters: 2 acetyl CoA. Goes thru a cycle twice (one for each acetyl CoA)
Exits: 4 CO2, 2 ATPs, & 6 NADH, & 2 FADH2
substrate level phosphorylation
This is where the CO2 we need to exhale comes from
Electron Transport System
Know where it occurs & what chemicals enter & exit it. (Go into more detail for the process here for what happens with the chemicals that enter. Remember “hot potato”)
Occurs in the mitochondria
Enters: all the NADHs & FADH2 & O2
NADH & FADH2: carry lots of high energy electrons & H+ to the electron transport system
Sends these electrons to electron acceptors (proteins) in the inner mitochondrial membrane & “plays hot potato”
As the electron gets passed on to the next protein, it gives up some energy, which is used to pump H+ from one side of the membrane to the other
This is why H+ gets pumped out the other side of the membrane. So it can come back in
H+ comes back in thru ATP synthase. As it comes through, we add a phosphate to make a new ATP
Takes H+ & O2 to make water (metabolic water) (O2 is the final electron acceptor)
Exits: metabolic water & 32 ATPs
oxidative phosphorylation
Grand total of ATPs (starting from one glucose)
glycolysis- 2 ATPs
kreb’s- 2 ATPs
Electron transport system- 32 ATPs
Grand total: 36 ATPs
aerobic respiration vs. anaerobic respiration vs. lactic acid fermentation
anaerobic respiration- oxygen is not required. Produces less ATP (2 ATPs per glucose). This is glycolysis alone
Done for great ATP needs or if there isn’t enough O2
aerobic respiration- oxygen is required. Produces more ATP (36 ATPs per glucose)
Lactic acid fermentation- pyruvate becomes lactic acid. Occurs when pyruvate doesn’t go into Kreb’s cycle. This is a type of anaerobic respiration. It allows for glycolysis to continue (2 ATPs produced)
Lactic acid- what the pyruvates become when they don’t go into Kreb’s cycle
Occurs in muscle cells. Can cause soreness from lactic acid
How lipids are metabolized by the body (generate ATP) & ketoacidosis
Change a fatty acid by removing some carbons to make Acetyl CoA
Using glucose is easier than using lipids
This process results in “garbage,” which is often molecules called ketones (which are acidic).
This is ketoacidosis (the “price tag” of using lipids instead of glucose for ATP)
How proteins are metabolized by the body (generate ATP)
Take the aminos off the amino acid, & the carbon skeleton can be used to make ATP
carbs are still easier to use than proteins
gluconeogenesis
Converting amino acids or fatty acids into glucose. The creation of glucose molecules from a non-carbohydrate precursor
Not easy, but can be good since carbs are easier to use than lipids or proteins
This is a type of nutrient molecule interconversion
Nutrient molecule interconversion
switching from one molecular group into another. Like translating
ex. changing a lipid into a carb
Not easy since something can get lost in translation
nutrients
nutrient molecules are the things we absorb (monosaccharides, amino acids, etc.)
We could make these, but we aren’t plants (can’t make our own food)
essential nutrients (includes essential amino acids)
nutrients that must be eaten (your body can’t make them).
ex. essential amino acids must be supplied through a diet.
minerals
substances we eat known by their element names (ex. zinc, iron, calcium, etc.)
BMR (basal metabolic rate) & factors that can influence it (5 factors)
the amount of energy (Calories) per day/hour that the body uses at rest
Factors include hormones, fever, nutritional status, physical activity, & certain drugs
Calorie vs. calorie (capitalized vs uncapitalized)
calorie- energy unit
Calorie- Kilocalorie or food calorie (1000 calories)
complete protein
a dietary protein that supplies all the essential amino acids
fat soluble vitamins vs. water soluble vitamins
fat soluble vitamins- a vitamin with a structure similar to cholesterol, making it nonpolar, hydrophobic, & soluble in other lipids
water soluble vitamins- a vitamin with predominantly polar bonds, are hydrophilic, & are soluble in water
free radicals
highly reactive, unstable molecules with at least 1 unpaired electron in its outer shell.
1 function for each vitamin: A, B1, B2, Niacin (B3), B12, C, D, E, & K & vitamin deficiency symptoms
A- growth & development.
Deficiency=delayed growth
B1- coenzyme in many catabolic pathways.
Deficiency= disease beriberi (peripheral nerve disfunction & heart disease)
B2- component of FAD & catabolic pathways.
Deficiency= skin disorders
Niacin (B3)- component of NAD & catabolic pathways.
Deficiency= disease pellagra (CNS, GI, & skin disfunction)
B12- needed for development of erythrocytes.
Deficiency= disease pernicious anemia
C- coenzyme in collagen synthesis.
Deficiency= disease scurvy (deterioration of skin & epithelial membranes)
D- needed for calcium ion homeostasis & bone growth.
Deficiency=osteoporosis
E- antioxidant.
Deficiency= anemia
K- Needed for synthesis of clotting factors.
Deficiency=bleeding disorders
Thermoregulation (including heat transfer, gain & loss, & variation)
Thermoregulation- body temperature regulation. Metabolism is the primary source of body heat
Heat transfer: a form of convection (heat is transferred through a liquid or gaseous medium).
Body heat rises away from the body and is replaced by falling cooler, denser air
Gain & loss: how the body gains/loses heat thru heat transfer
Variation: thermoregulation can vary based on factors like activity & air temperature
hypothermia
an abnormal decrease in body temperature, often due to prolonged exposure to decreased temperatures.