41. Primary and secondary bone healing. Complications of the fractures treatment and therapy. Arthrodesis.
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
What is required for direct/primary bone healing?
Rigid stabilisation with compression of bone ends (contact healing)
How can different types of primary healing be classified?
Gap healing
Contact healing
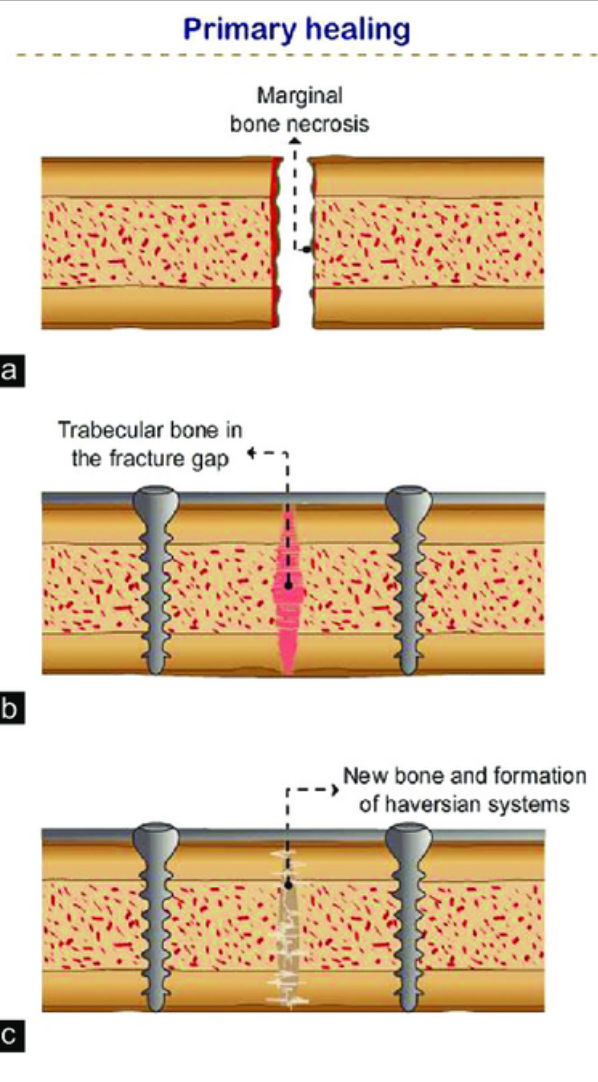
What are the two stages of gap healing (a type of primary bone healing)?
Filling of gap (less than 1mm) by direct bone formation, no connective tissue or fibrocartilage w/i gap preceding production of bone.
Longitudinal haversian remodelling reconstructs necrotic fracture ends & newly formed bone is resorbed & replaced w/osteons of original orientation
What characterises contact healing (a type of primary bone healing)?
Direct apposition of fragments, osteons grow across the fracture site, parallel to the long axis of the bone
What are the stages of indirect/secondary bone healing?
Haematoma and inflammation
Reparative phase
Bone remodelling
What occurs during the haematoma and inflammation phase of secondary bone healing?
Haematoma formation → attraction of inflammatory cells → swelling, vasodilation
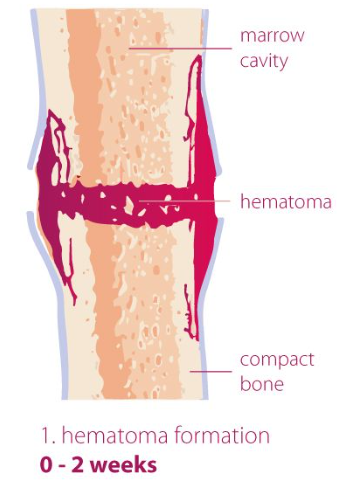
Which inflammatory cells are involved in the haematoma and inflammation phase of bone healing?
Platelets, neutrophils, macrophages & mesenchymal stem cells
What are the stages of the reparative phase of bone repair?
Soft callus formation
Cartilaginous callus
Hard callus formation
What occurs during the soft callus formation phase?
Granulation tissue forms a fibrous callus to stabilise the area as inflammation subsides
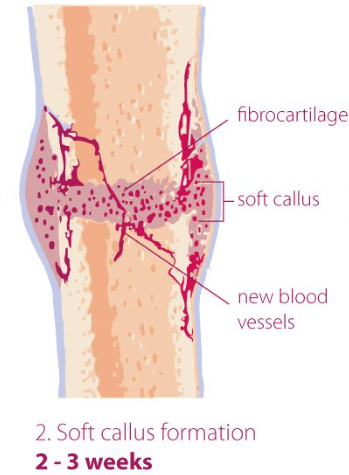
Which cells are involved in the soft callus phase?
Fibrocytes
What occurs during the cartilaginous callus formation phase?
Fibrous callus undergoes chondrogenesis → cartilage in the intercortical region
Which cells are involved in the cartilaginous callus phase?
Chondrocytes
What occurs during the hard callus formation phase?
Cartilaginous callus ossifies (endochondral ossification) into woven bone → osseous callus forms reinforcing the fracture
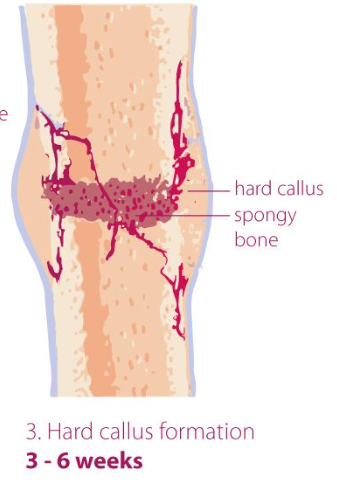
Which cells are involved in the hard callus phase?
Osteoblasts, osteoclasts
What occurs during the remodelling phase?
Woven bone is replaced by lamellar bone, excess callus is resorbed to match the original bone structure, restoring function
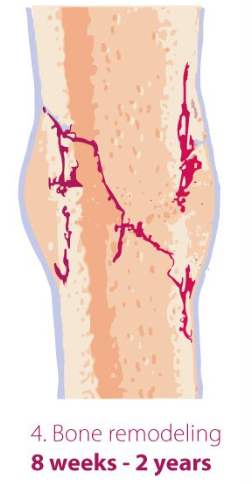
Which cells are involved in the remodelling phase?
Osteoblasts, osteoclasts & osteocytes
What are examples of complications of fracture treatment and therapy?
Delayed union
Malunion
Non-union
Excessive callus formation
Fracture disease
Pseudoarthrosis
Osteomyelitis
Others
What is delayed union?
Normal stages of fracture healing occur at a slower rate than normal.
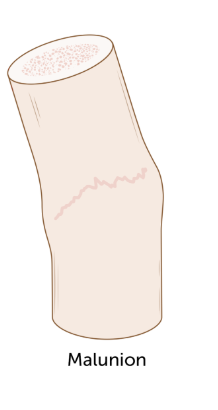
What is malunion?
Normal fracture healing stages with malalignment.
What is non-union?
Failure of a fracture to heal.
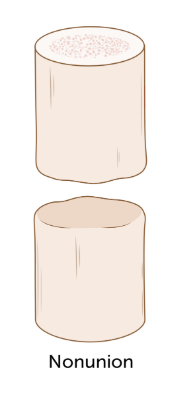
What is the aetiology of non-union of bones?
Inadequate immobilisation of fracture ends, resulting in movement of bones or disruption of blood supply
What are the two types of non-union?
Viable (biologically active; hypertrophic) and non-viable (biologically inactive; atrophic).
What characterises hypertrophic non-union?
Excessive fracture mobility with adequate blood supply → Excessive callus formation, "elephant's foot" sign.
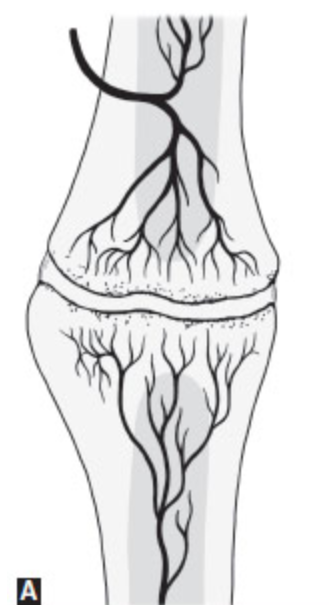
What characterises atrophic non-union?
Reabsorption and rounding of bone ends due to inadequate blood supply & excessive mobility of bones.

What is pseudoarthrosis?
A false joint that forms due to a failure of fracture healing.

What is osteomyelitis?
Inflammation of bone and bone marrow. May result in delayed union or non-union
What are clinical signs of osteomyelitis?
Lameness, inflammation, swelling, redness → necrosis and fistula
What are some treatment options for osteomyelitis?
Drainage, necrotic bone removal, lavage, stabilisation, antibiotics (Amoxicillin/Clavulanate, G+ clindamycin or G- enrofloxacin).
What is arthrodesis?
Surgical fusion of a joint to form one bone.
How is arthrodesis performed?
Bone grafts either from a donor or from patients own body is put between two bones being fused, often w/ help of supporting metal implants to hold them together (screws, plates, fixators)
After surgery & healing (months to years…), two adjoining bones are fused & no motion takes place between them.
What is important for successful arthrodesis?
Removal of all cartilage
Alignment of joint surfaces.
Which fractures are most likely to become infected?
Open fracture with skin penetration.