Seminar 4 anti-racism and anti-oppression
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Trauma - Fight, flight, freeze, fawn response
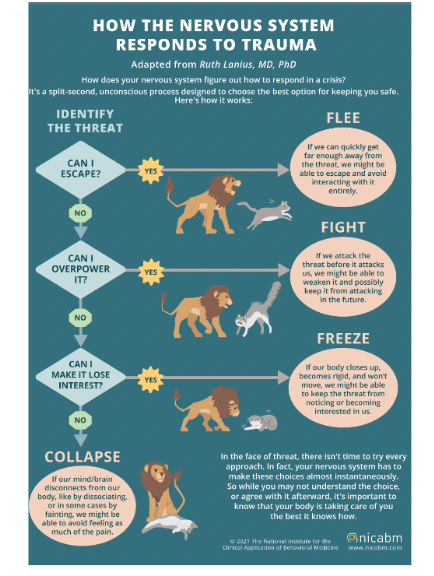
Self-care: Fight, flight, freeze, fawn respons
BREATHE to soothe the sympathetic nervous system
RESPOND to address action/comment when in a parasympathetic state (e.g., feeling more relaxed).
RECOGNIZE the comment as it is
PROVIDE SPACE for learning from comment
ADDRESS the need to create a safer workspace (e.g., what might we do…)
ACKNOWLEDGING the emotional burden that some people may experience over others
Historical Development of Nursing Theory
Nursing theories focusing on illness in clinical settings are not always easily adapted to practice of CHN
More recent developments include nursing theories being adapted specifically to CHN
Most nurse theorists assumed that community health nursing theories and models were relevant to practice with a range of populations and communities.
Theories did not explicitly draw on Indigenous perspectives and may have been the result of very few Indigenous nurses as community health nursing scholars, researchers, and leaders (due to racism and exclusion).
Theoretical perspectives are broadening (i.e., complexity science theory, social ecological theory, feminist theory, postcolonial theory, intersectional feminist theory) have been added to the nursing literature
Importance of Theory
Theory, research and practice are reciprocal
Theory provides roots that anchor both practice and research in the nursing discipline
Practice and research in diverse settings contribute to development of new theories
Theory assists practitioners, decision-makers, educators, and researchers to explain what they experience, inform their actions and decisions, and articulate possible outcomes
For CHNs, theory may guide practice in situations where rigorous research-based evidence is not available
Theories can support understanding of why things are the way they are.
Nursing theories are integrated with theories developed in public health and the social sciences to guide the practice, research, and education of CHNs.
Definitions: Privilege
Societally granted, unearned advantages accorded to some people and not others. These systemic or structural advantages impact people based on identity factors such as race, gender, sex, religion, nationality, disability, sexuality, class, and body type.
Definitions: Oppression
Societally constructed disadvantages and disenfranchisement due to holding a marginalized identity (an identity not part of the dominant group/culture). These systemic or structural disadvantages impact people based on the same identity factors of privilege.
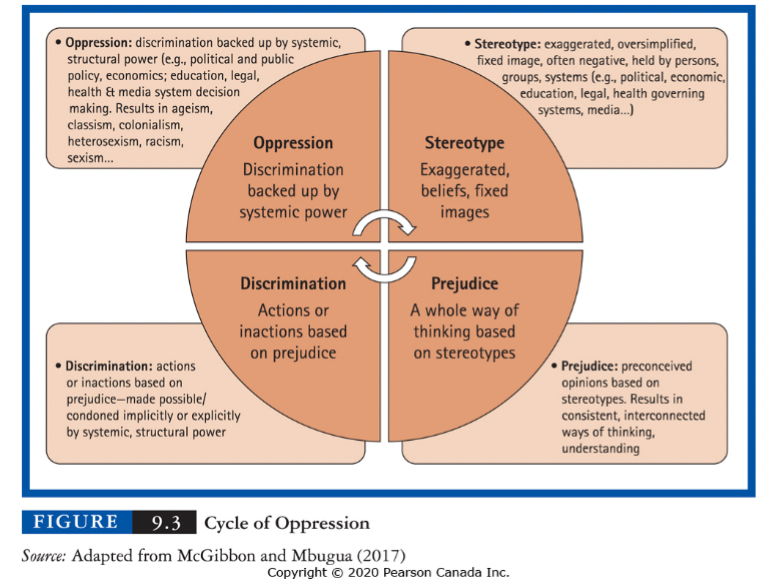
Cycle of Oppression
Fig 6.1 & 9.3
(p. 97 & p. 174)
False Ideas: Biological Racial Hierarchies
Nursing theory developed within the context of nation-building in Canada (& racial hierarchies developed by British empire)
Those who support racial hierarchies believe in the superiority of one ‘race’ over others, which contributes to the devaluing and dehumanizing of certain people
In Canada, race-based policies were experienced through slavery, segregation (e.g., IRS, Indian Hospitals), & citizenship / immigration (e.g., Komagata Muru, Japanese internment camps, Chinese head tax) and ongoing experiences of race-based inequities
Racial hierarchies vary across societies; they are sometimes instituted into law (e.g., Apartheid in South Africa, Nuremberg Laws in Nazi Germany).
Definitions: Race
Race is used to categorize people (by phenotypes like hair, nose, skin colour).
Race is a social construct:
99.9% of our genetic codes are similar
Most genetic variation arises within groups
Little genetic variation exists between groups
All populations represent a long history of migration and mixing
There is no ‘pure’ racial group
“It remains the case that western lowland gorillas show a higher overall level of genetic diversity than humans.”
Definitions: Social Construct
a concept that exists not in objective reality but because of human interaction over time and reinforced through ideas (p. 368).
Racial groups are socially constructed through the process of racialization.
Definition: Racialization
assigning people of colour into racial groups based on imposed beliefs about the person’s body (like skin tone and physical appearance) (p. 173).
Racism
Racism — not race — creates biological consequences & different health outcomes
Definitions: Ethnicity
is about cultural identity and shared heritage
Definitions: Nationality
Nationality is about legal status and political affiliation with a country.
important terms for understanding cultural contexts
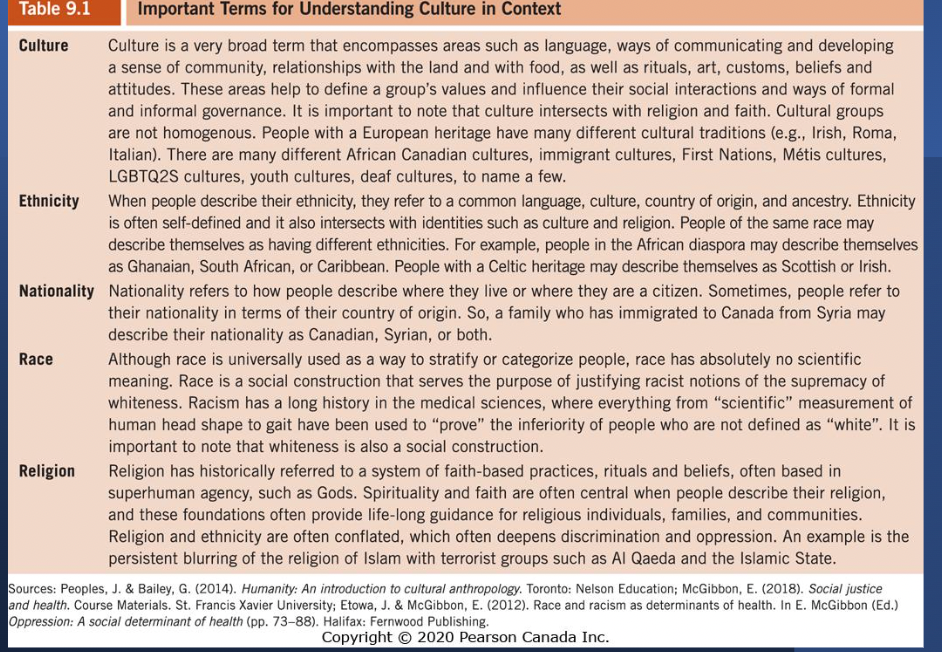
Definitions: Diversity
Diversity is described as encompassing a range of characteristics including but not limited to race, ethnicity, culture, socioeconomic status, gender, sexual orientation, and disability.
Recognizing these differences and reflecting upon biases is crucial for providing holistic and effective care.
What is intersectionality?
An approach to understand how systems of inequities, such as sexism, racism and ableism, interact with each other to produce complex patterns of privilege and oppression.
The result is not additive; finding oneself on the same side of two coins does not mean that one is twice as privileged or twice as oppressed.
Rather, intersecting systems of inequality produce new and complex patterns of advantage and disadvantage.
The relevance and impact of these positions varies according to context, and so one’s positions on these multiple coins need to be analyzed together.
Intersectionality
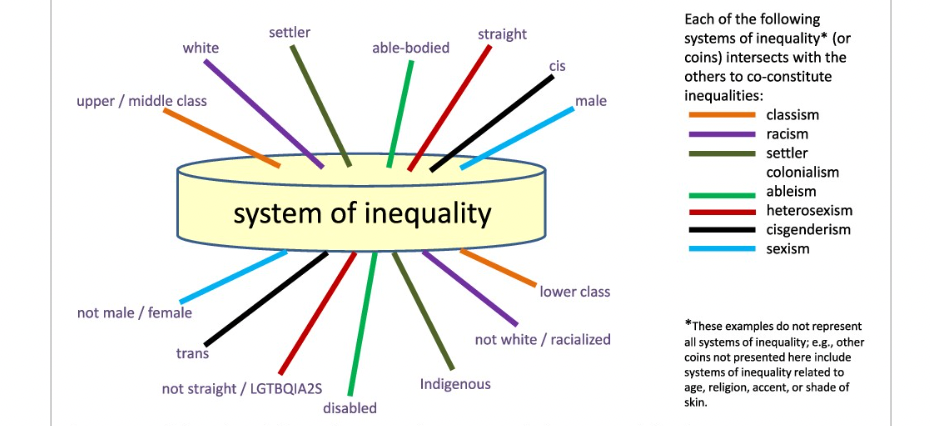
What is intersectionality? 2
We all hold multiple social identities simultaneously, such as ethnic background, gender, ability, and sexuality.
Jordan’s Principle – was created due to the overlapping and intersecting identities of First Nations children (e.g., age, Indigeneity, ability) and how systems of oppression differentially impact them.
Definition: Culture
Culture: language, gestures, tools, customs & traditions defining a group’s values and organize social interactions
Culture is a social construction – norms, behavior and values are learned through socialization (family, community)
Culture is integrated and embedded in everyday life – beliefs and healthcare practices are consistent with overall paradigms used to make sense out of the world.
Culture is shared – beliefs are shared by a group (cultural values) that guide members about what to believe and how to act
Culture shapes us at an unconscious level
Culture is fluid and dynamic (always adapting and changing)
Continuum for cultural safety and humility
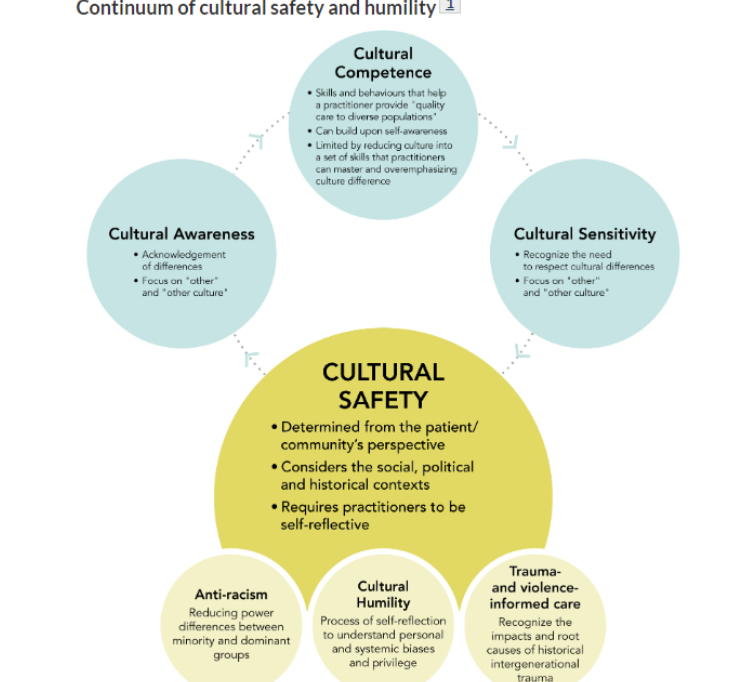
Cultural awareness & Cultural sensitivity:
Steps toward cultural safety
Cultural awareness = An initial understanding that variations exist
Cultural sensitivity = Showing respect and valuing cultural diversity
Cultural competence: is an ongoing process not an outcome
Process of respecting, accepting, and applying knowledge and skills appropriate to client interactions without allowing a nurse's personal beliefs to influence the clients’ differing views
Examples = paying attention to:
dietary practices; attitudes toward pain; beliefs about death and dying; modesty; eye contact; closeness and physical contact

Cultural Competence
An ongoing process not an outcome
Process of respect, accept, and apply knowledge and skill appropriate to client interactions without allowing their personal beliefs to influence the clients’ differing views
Examples = paying attention to:
dietary practices
attitudes toward pain
beliefs about death and dying
modesty
eye contact
closeness and physical contact.
Applying Cultural Competence to Community Health Nursing
Culturally competent CHNs may:
Use cultural brokering (bridging the difference)—can be intersectoral partners or someone from your organization
Know if there are specific risk factors for a given cultural population—understand that those risk factors are probably due to the SDoH
Understanding that context may adjust one’s culture—migration, etc.
Be willing to learn your clients’ healing practices
Are aware of cultural values, beliefs, and practices to guide them in delivering culturally appropriate care
Two-Eyed Seeing
Cultural Humility
A commitment to actively taking responsibility for seeking to understand the culture and experiences of others.
Being comfortable not being the expert
Knowing one can never fully understand the experience, history, and background of another
Inhibitors to Developing Cultural Competence & Safety
A narrow view of culture may:
exclude history & context, drawing attention away from the wider social, historical and economic contexts that shape peoples’ lives
create assumptions about so-called cultural characteristics & may feed into stereotypes about a groups’ values, beliefs, lifestyles
stereotype rather than create understanding on how oppression (e.g., patriarchy, racism, colonialism) impact health access
prevent understanding of your privilege(s)
provide a tick box approach to assessment, rather than a relational & wholistic approach
Cultural Safety
Cultural safety is based on the following three premises:
Respect for cultural identity: Recognize one’s own unique cultural self and its influence on client interactions.
Power imbalances: Acknowledgement of the power imbalance that favour the health professional; address the imbalance so that the client feels safe.
Self reflection & continuous improvement: HCP learns and applies new skills; reflects on biases, privileges & attempts to improve approach to care
All three premises work together to help remove the barriers of “power” and “authority” and promote inequities.
Cultural safety is determined by the client, patient, member.
Cultural Nursing Assessment
A systematic way to identify people’s beliefs, values, meanings, and behaviours, while considering their history, life experiences, and the social and physical context in which they live. (Think of the continuum of cultural safety & humility not just cultural competence).
CHNs must conduct a cultural assessment for all clients (individuals, families, or communities) when they first contact them.
If clients are reluctant to answer questions, CHNs should seek information from sources such as family members, interpreters, traditional cultural health practitioners, and educational resources.
When conducting a cultural assessment, consider:
Communication/language, space, social organization, history, time and environment
Summary
To be “culturally- competent” or culturally humble & safe in practice, we need to:
think about how we are conceptualizing “culture”
Move beyond a narrow view of culture to a “lens with multiple filters” with a view toward history, politics, the SDoH--& uniqueness of the individual/family/population
Be vigilant about understanding our privilege and how that might shape our interactions with our patients, families, and communities
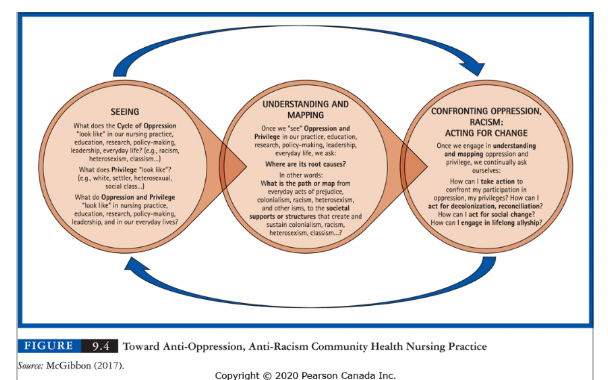
Toward Anti-Oppression in CHN practice
Seeing
What might the cycle of oppression “look like” at your clinical site?
What does privilege look like?
What do oppression and privilege look like in nursing practice?
Understanding and mapping
What are the root causes?
What creates structural oppression?
Confronting oppression
How can I take action?