Arteries, arterioles & distribution of blood flow
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
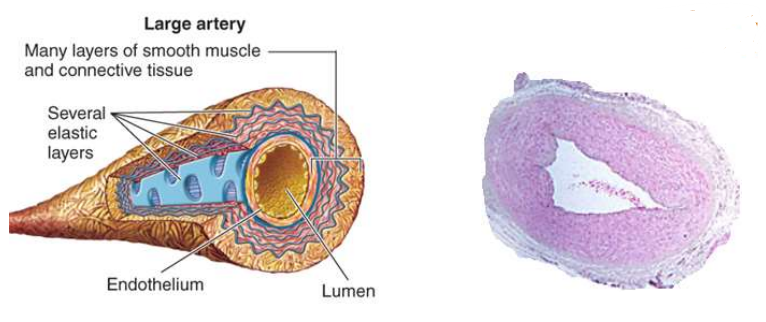
what are some features of arteries
pressure tubes - act as pressure reservoirs to maintain blood flow through tissue during diastole
large diameters - provides low resistance pathway for conducting blood to organs/tissues
most of the artery consists of smooth muscle and connective tissue
why is blood flow out of the heart considered intermittent
the aortic valve (between L.V & aorta) closed upon ventricular repolarisation
however, blood flow through tissues is continuous
what is systolic blood pressure
pressure required to stretch the arteries
about 2/3 of blood flow goes to stretching arteries
about 1/3 of blood flow goes to arterioles & capillaries
what is diastolic blood pressure
the pressure in your arteries when your heart relaxes between beats
the 2/3 of blood flow that stretched the arterial walls now goes to arterioles & capillaries (thus continuous flow)
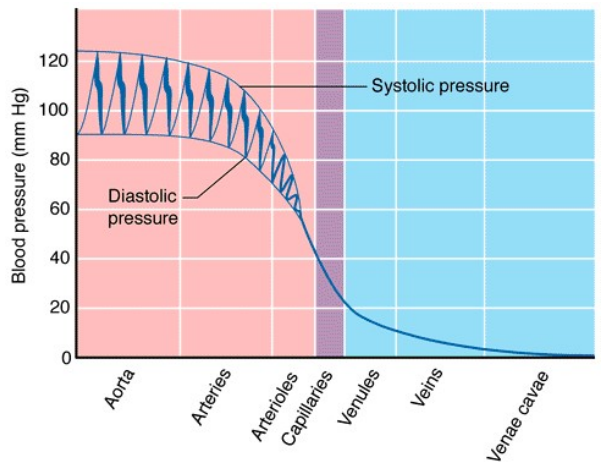
what is an aortic pressure trace
graph that displays key pressure such as:
Systolic blood pressure
diastolic blood pressure
pulse pressure (SBP - DBP)
mean arterial pressure (DBP + 1/3(PP))
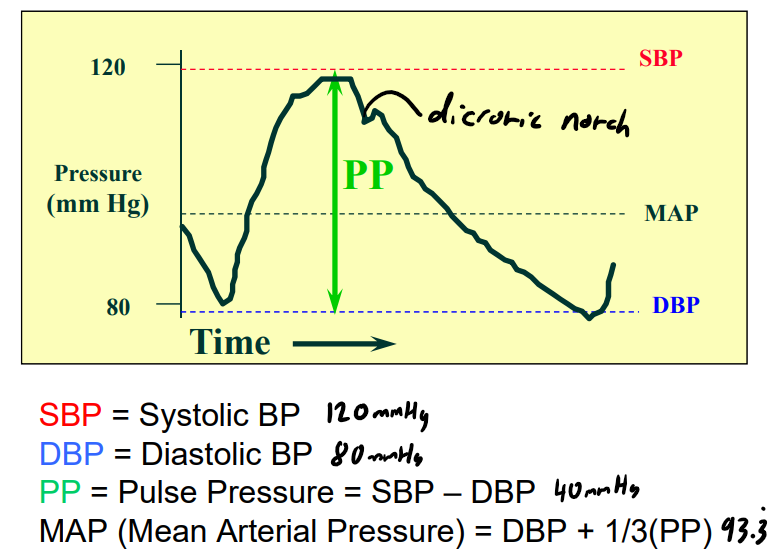
what is a dicrotic notch
a small drop in pressure that represents the closure of the aortic valve upon ventricular repolarisation
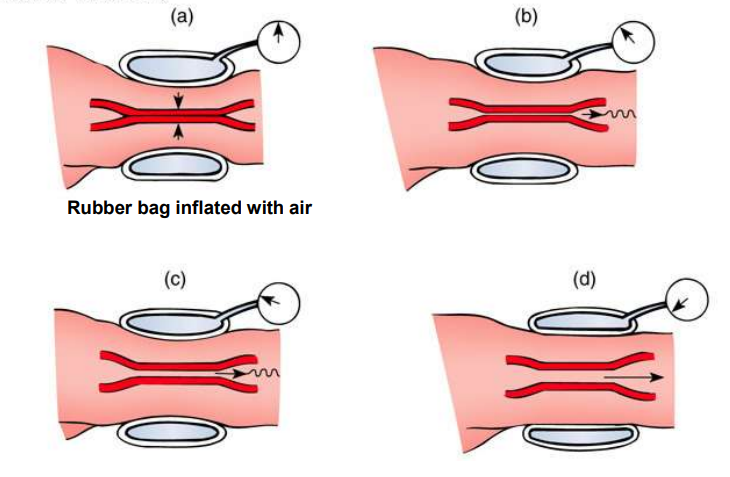
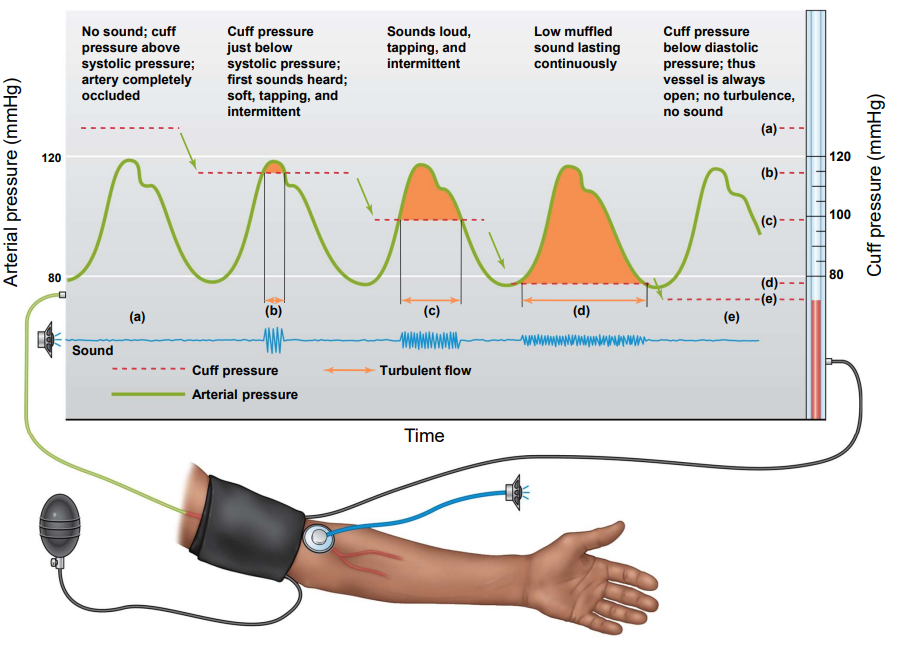
how is blood pressure measured
inflatable cuff is pumped above systolic pressure (120mmHg), cuts off flow through the brachial artery
pressure in cuff is slowly released, thus causing turbulent flow (systolic)
once laminar flow (diastolic) is established recording is finished
what are Korotkoff sounds
sounds heard by stethoscope that indicate turbulent flow of blood through the body
what is hypertension & hypotension
hypertension - higher than normal blood pressure
consistently above about 140/90
hypotension - lower than normal blood pressure
consistently below about 100/60
these conditions are determined via the mean systolic/diastolic pressures
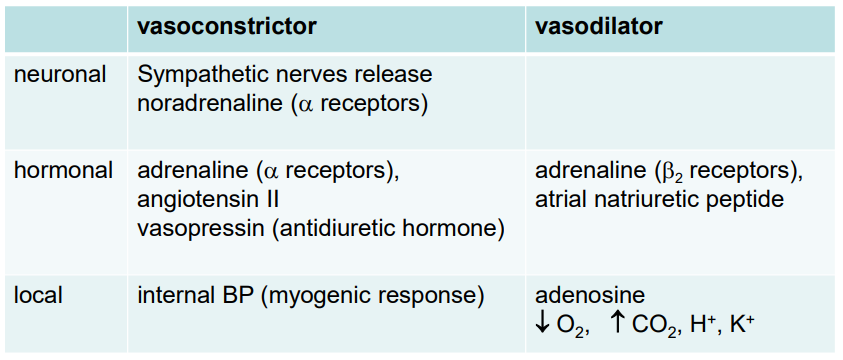
what are arterioles responsible for
controlling the proportional distribution of blood flow to organs by altering diameter of arteries
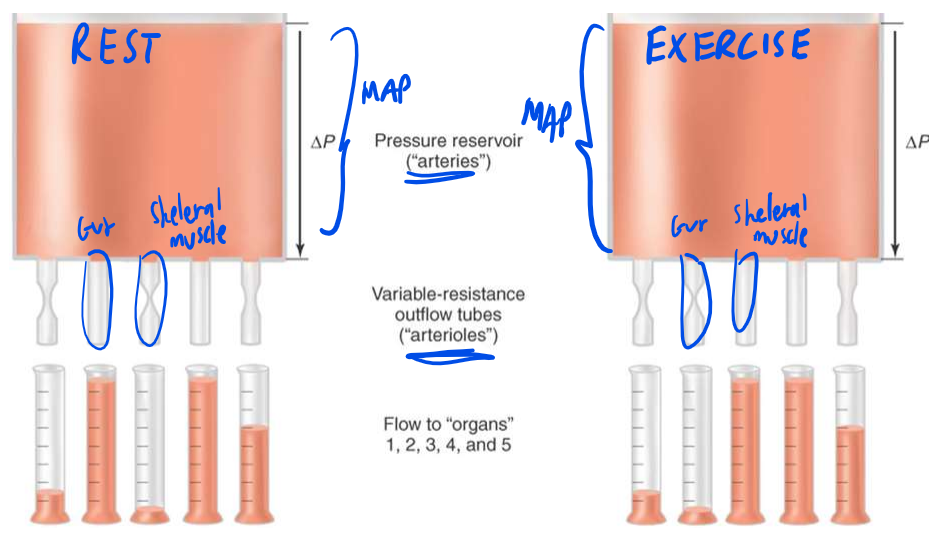
how is the diameter of blood vessel altered by arterioles
smooth muscle wraps around the arteries:
constriction: decreases diameter = decrease blood flow
relaxation: increase diameter = increase blood flow
what are the 2 local mechanisms for changing arteriole diameter
Autoregulation
metabolic control
myogenic mechanism
what is metabolic control
increase in blood flow when metabolic activity is high, occurs by relaxation of arterioles.
↑ adenosine
↑ [CO₂]
↓ [O₂]
↑ [H⁺]
results in “active hyperemia”
what is the myogenic mechanism
refers to a decrease in the pressure of an arteriole, after a sudden increase
this is cause by a constriction in the smooth muscle cells
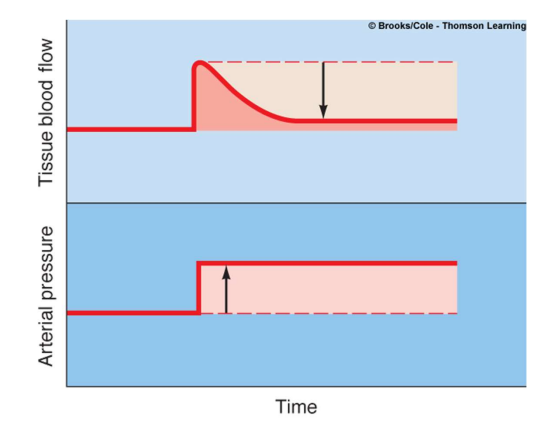
what is the point of the myogenic mechanism
allows organs to maintain constant blood pressure even with a dramatic change in arterial pressure
how are arterioles innervated
mostly innervated by sympathetic nerves
only genitals have significant innervation
noradrenaline acts on arteriolar muscle adreno-receptors (α) = smooth muscle constriction
what does the reflex control of arterioles consists of
some level of resting sympathetic activity, so smooth muscle is partially constricted, therefore:
↑ sympathetic = ↓ blood flow
↓ sympathetic = ↑ blood flow
how can arterioles be controlled by hormones
causes constriction by acting on α-receptors
causes dilation by acting on arterioles with β2-adrenergic adrenoreceptors (e.g. skeletal muscles)
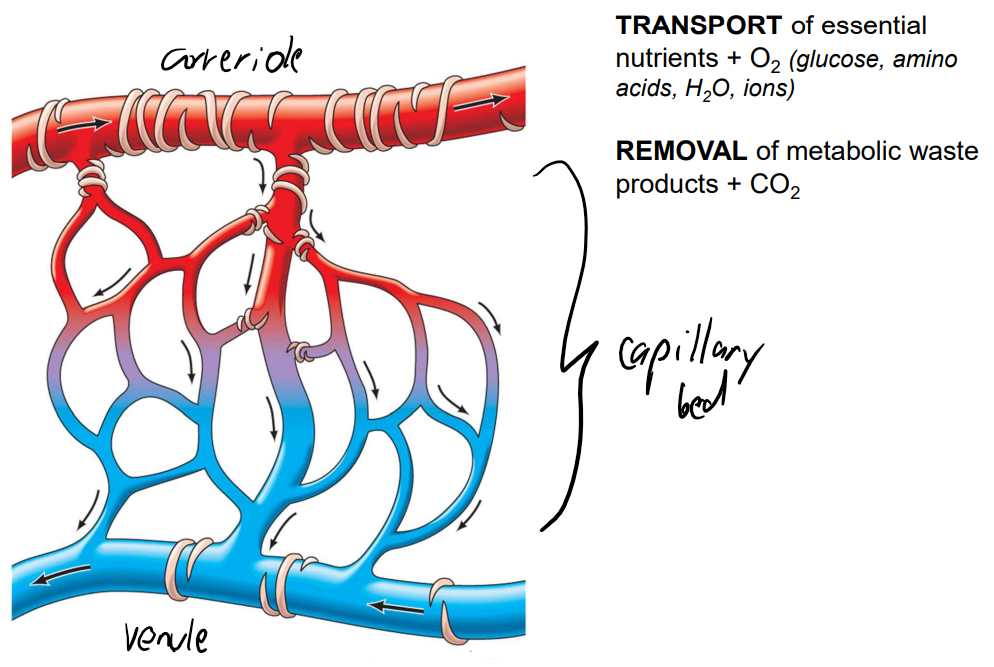
what is microcirculation
blood flow from arteriole to venule, through the capillary beds, in which:
O2 + nutrients is sent
CO2 + waste is collected
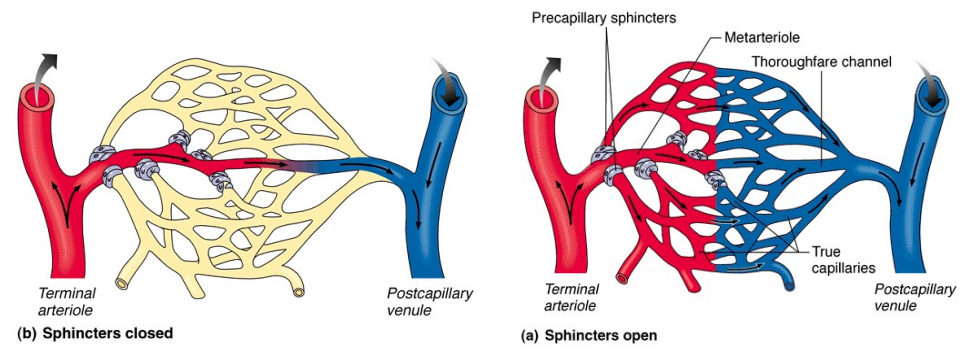
what is some information about capillaries at rest & during exercise
rest = many capillaries are closed
during exercise:
smooth muscle sphincters relax allowing blood to flow through metarteriole & throughfare channel
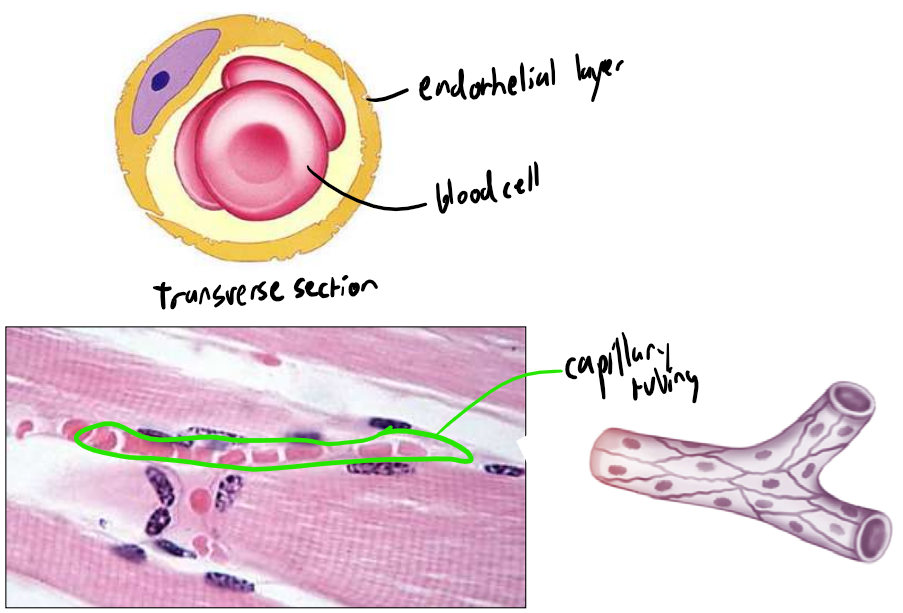
what are some details about the structure of capillaries
thin layer of endothelial cells making exchange across the membrane easy
narrow tube allowing blood cells to flow through in single file
what is the pressure within arterioles & capillaries
arterioles = 40mmHg
capillaries = 20mmHg
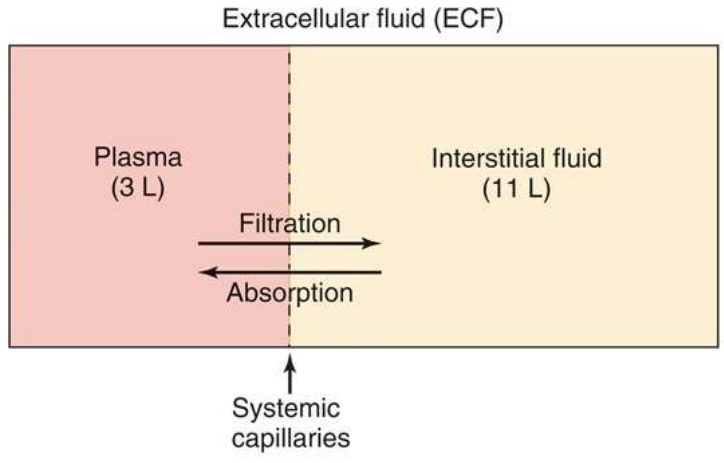
how are the different extracellular body fluids separated from each other
plasma is separated by the endothelial layer of capillaries.
filtration = H2O & solute transfer from plasma → interstitial fluid
Absorption = H2O & solute transfer from interstitial fluid → plasma
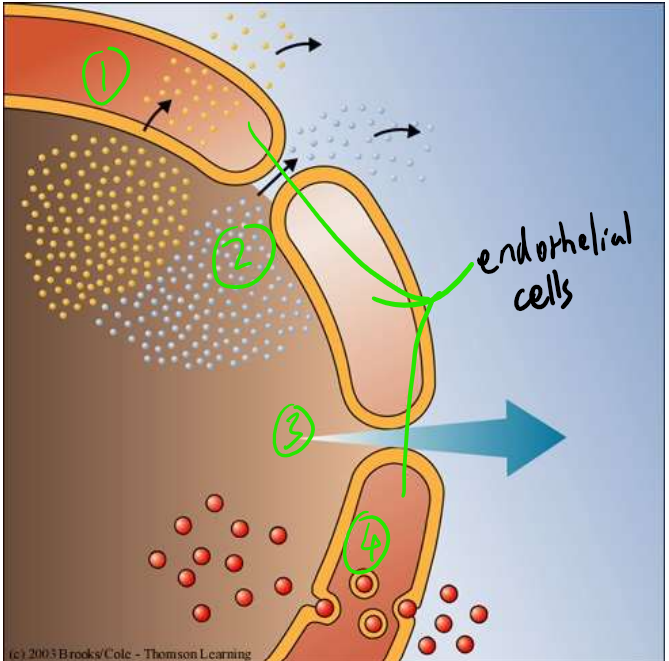
describe the movement of substances from the plasma → interstitial fluids
direct diffusion
lipid soluble / gases (O2, CO2)
diffusion through pores (intercellular clefts)
lipid insoluble = glucose, ions, A.As
Bulk flow
H2O
vesicular transport of large molecules
some hormones
what are the 2 major forces driving & opposing filtration at capillaries
hydrostatic / blood pressure in capillaries
drives filtration
plasma osmotic (colloidal oncotic) pressure
caused by plasma protein
opposes filtration
explain how the functions of arterioles are influenced by pressure
hydrostatic pressure from blood is high at the end near arterioles, with a lower osmotic pressure
hence the net pressure allows for the filtration of nutrients into the interstitial fluid
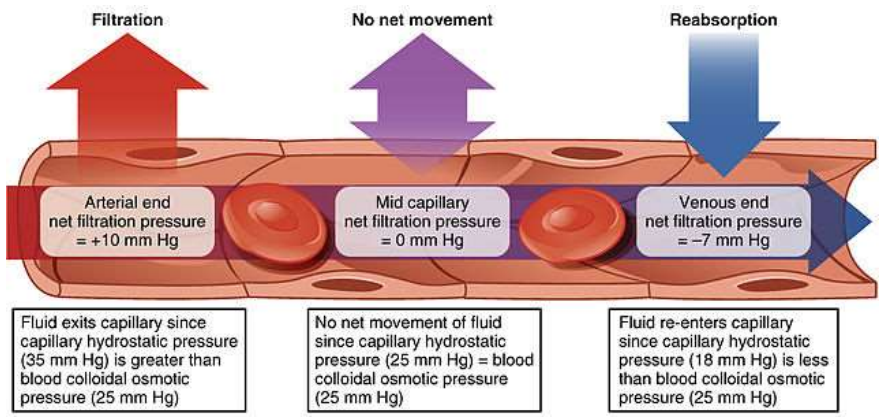
explain how the functions of venules are influenced by pressure
hydrostatic pressure from blood is low at the end near venules, with a higher osmotic pressure
hence the net pressure allows for the absorption of waste from the interstitial fluid
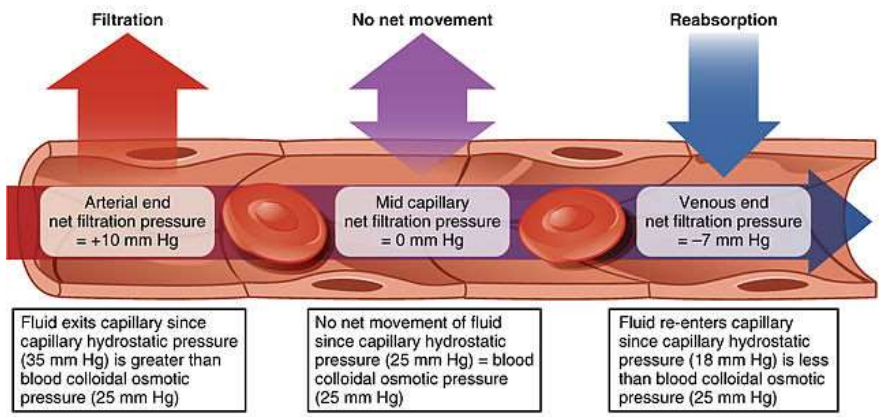
what is important to note about the middle of the capillary bed
equal hydrostatic & osmotic pressure, hence no exchange
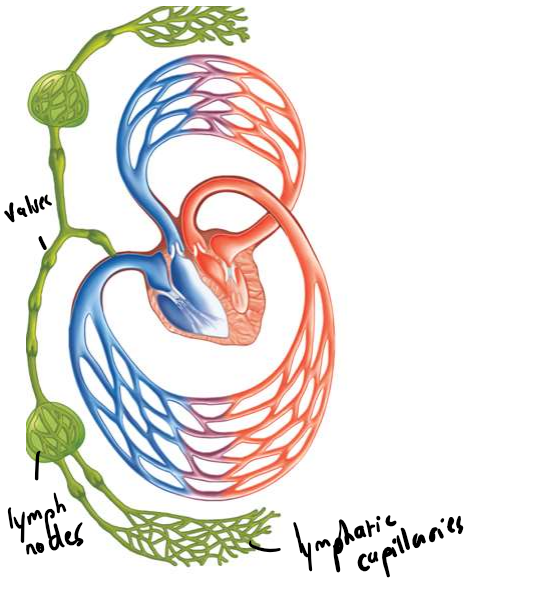
there is a net filtration of ~4L protein-free fluid from plasma into the interstitial fluid, how is this drained
drained by the lymphatic system, by lymphatic capillaries.
it contains blind-ended capillaries that drain fluid through lymphatic veins into subclavian vein of cardiovascular system
what occurs when drainage of extracellular fluids in the body doesn’t occur
results in oedema
failure to maintain distribution of water thus leading to a build-up
what are some causes of oedema
increased hydrostatic pressure of blood (prevents absorption)
heart failure, hypertension
decreased osmotic pressure (prevents filtration), caused by drop in plasma protein levels
malnutrition, liver disease, renal disease
lymphatic drainage disruption (tumors)
disruption on the permeability of capillaries
what is some information about the veins
low pressure
large diameter
low resistance
thin-walled
one-way valves
what is venous return & cardiac output
venous return - refers to the volume of blood that flows back to the heart
cardiac output - refers to the volume of blood pumped throughout the body per minute
venous return effects cardiac output
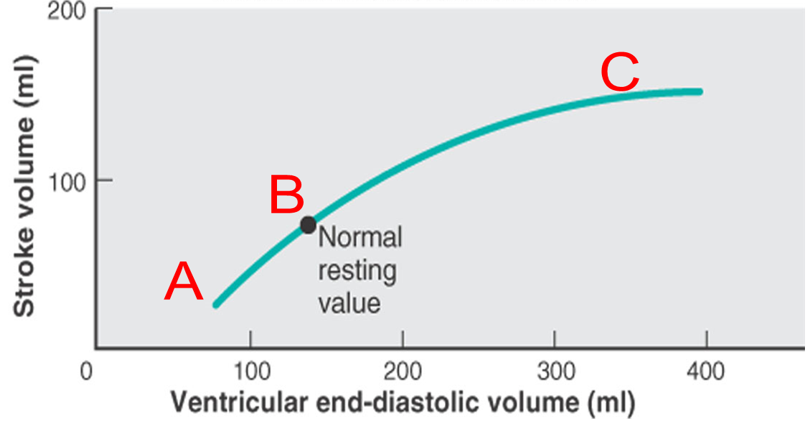
what is the ventricular end diastolic volume
the volume of blood in the ventricle just before a contraction
increase in end diastolic pressure = increase in length of cardiac muscle
what is stroke volume
the amount of blood pumped from the left ventricle throughout the body in one contraction
what are some equations to know regarding the cardiovascular system
cardiac output (CO) = SV x HR
stroke volume (SV) = EDV - ESV
ejection fraction (EF%) = SV/EDV x 100
what are 3 mechanisms that influence venous return
pressure gradient
skeletal muscle ‘pump’
respiratory ‘pump’
how can venous return be increased using a pressure gradient
increasing the pressure of the veins compared to the right atrium will increase venous return
sympathetic activation on smooth muscle around veins stiffens the walls, thus increasing pressure
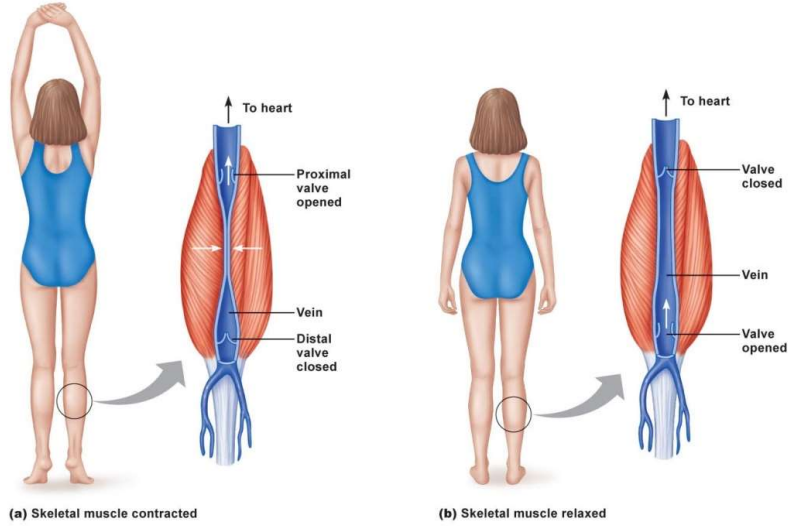
how is venous return increased by skeletal muscle ‘pump’
contraction of certain muscles within the body causes a blockage of veins, this increases the pressure of the veins driving blood back to the heart
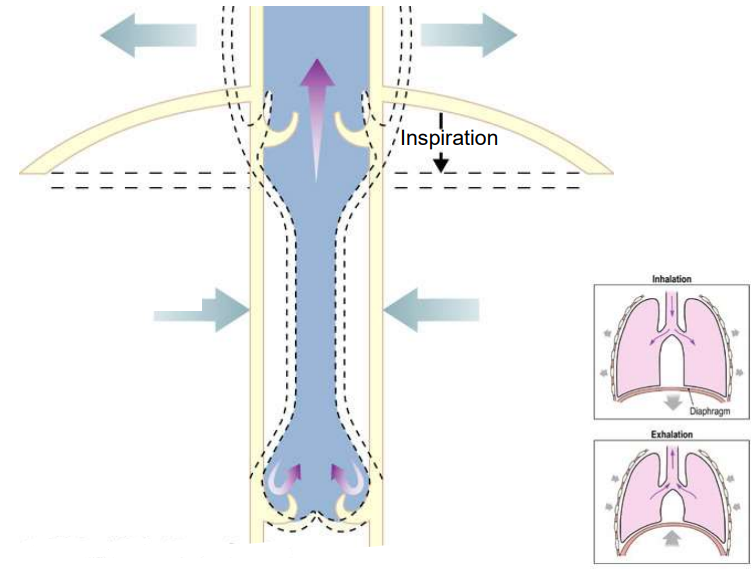
how can venous return be increased by the respiratory ‘pump’
when we breath in (inspiration), the diaphragm move down. This increases the pressure in the abdomen & decreases pressure in the thorax
this pressure gradient drives blood through the abdominal veins back to the heart
what is the Frank-Starling mechanism
the relation between the filling of the ventricle (EDV) and stroke volume
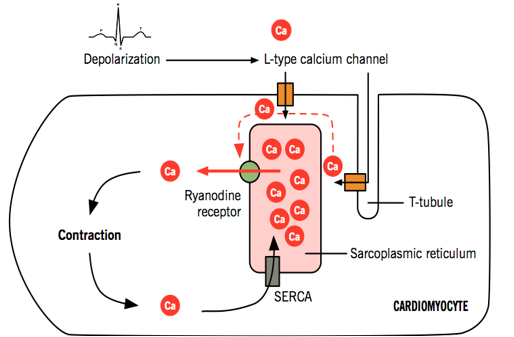
explain the process of muscle contraction
The neurotransmitter noradrenaline from the sympathetic cardiac nerves binds to beta-1 receptors on the heart decrease the depolarisation threshold for the L-type calcium channels, thus more calcium into the cell. Also increases the calcium-induced calcium release as calcium binds to the ryanodine receptor on the surface of the sarcoplasmic reticulum. This allows for more calcium to bind to troponin, this changes the shape of troponin and tropomyosin, thus exposing actin-myosin binding sites. Myosin heads have ATP bound to it causing the formation of a cross-bridge section between the myosin head and actin-myosin binding site. Hydrolysis of the ATP molecule causes the power stroke movement shortening the sarcomere. After which ADP and phosphate are released and a new ATP molecule bind causing the detachment of the myosin head ready for another stroke. SECRA maintains calcium concentration gradient by pumping calcium back into sarcoplasmic reticulum.