OB Hemorrhage Relias 2025–2026: 40+ Expert-Curated Verified Q&A with Emergency Response Protocols, Pharmacological Management & Postpartum Clinical Scenarios (RN/NP/CNM Aligned + Instant Digital Access)
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
What percentage of births are affected by OB hemorrhage?
OBH is responsible for how many pregnancy related deaths worldwide?
11% of births
25% of pregnancy deaths worldwide, 10.7% in the US
4 domains of care?
- Readiness (hemorrhage cart, training, protocols)
- Recognition/prevention (risk assessment, accurate EBL)
- Response (standard plan)
- Reporting (debriefs/reviews)
OB Hemorrhage protocols have been shown to decrease maternal death rate by ___ and maternal morbidity by ___.
OB Hemorrhage protocols have been shown to decrease maternal death rate by 50% and maternal morbidity by 21%.
Stages of Hemorrhage
Stage 0 - active mgt 3rd stage
Stage 1 - >500 vaginal, >1000 CS: activate OBH protocol
Stage 2 - 1000 - 1500 QBL, advance through protocol sequentially
Stage 3 - >1500QBL: activate MTP, move to OR
Stage 4 - cardiovascular collapse
Uterotonics and dosages
TXA
Oxytocin: 10-40 units per 500-1000cc IV, or 10 units IM.
Methergine: 0.2mg IM q2-4h (avoid if HTN)
Carboprost: 0.25mg IM q15-90 min, no more than 8 doses =2mg. (avoid if significant asthma)
Misoprostol: 800mcg SL or PO x 1
TXA (not uterotonic): 1g (100mg/mL) infused over 10 min, can repeat at 30 min
Risk factors for OB Hemorrhage
-History of OBH
-Uterine overdistension (multiple gestation, large fibroids, macrosomia, polyhydramnios)
-Grand multiparity or Primiparity
-Obesity (inc atony)
-Prior CS / Uterine surgery
-Abnormal placentation
-Abruption
-Coagulopathy/ Bleeding Disorder
-Personal or FHx OBH in a 1st degree relative
Platelets <100k
-Prolonged or augmented labor
-Prolonged third stage
-Operative Delivery
-Connective tissue disorders
-Preeclampsia/HELLP
-Use of MgSO4
-Malpresentation (inc risk of trauma)
-General anesthesia
Recurrence risk of OBH?
ranges 8-28% depending on contributing factors
May be as high as 80% in patients with vWF disease
High risk factors for OBH include:
Previa/low lying placenta
Accreta spectrum
Hct <30 + other risk factor
Platelets <100k
Active bleeding on admission
Known bleeding d/o
Multiple lower level risk factors
TYPE AND CROSS these peeps
Signs/symptoms of hypovolemia and concealed hemorrhage to tell patients?
dizziness, rapid HR, fatigue, rectal or pelvic pressure, abdominal pain
Atony is the cause of OBH at delivery in about ___% of cases.
About ____% of OBH is secondary (late).
80% atony
1-3%, rarely atony
When does primary and secondary hemorrhage occur?
Primary (early): within 24h of delivery
Secondary (late): 24h - 12 weeks after delivery
Women who deliver by primary CS have a ___% chance of subsequent CS.
90%
Women over 40 statistics:
2x as likely as moms <20yo to have a CS.
death rate 81.9 per 100k births
7.7x more likely to die of pregnancy than women <25yo
Physiologic cardiovascular changes of pregnancy peak at ___weeks.
Plasma volume expands by ____% while red cell volume increases by ____%, resulting in maternal ______.
Physiologic cardiovascular changes of pregnancy peak at 32 weeks.
Plasma volume expands by 40-50% while red cell volume increases by 20-30%, resulting in maternal anemia.
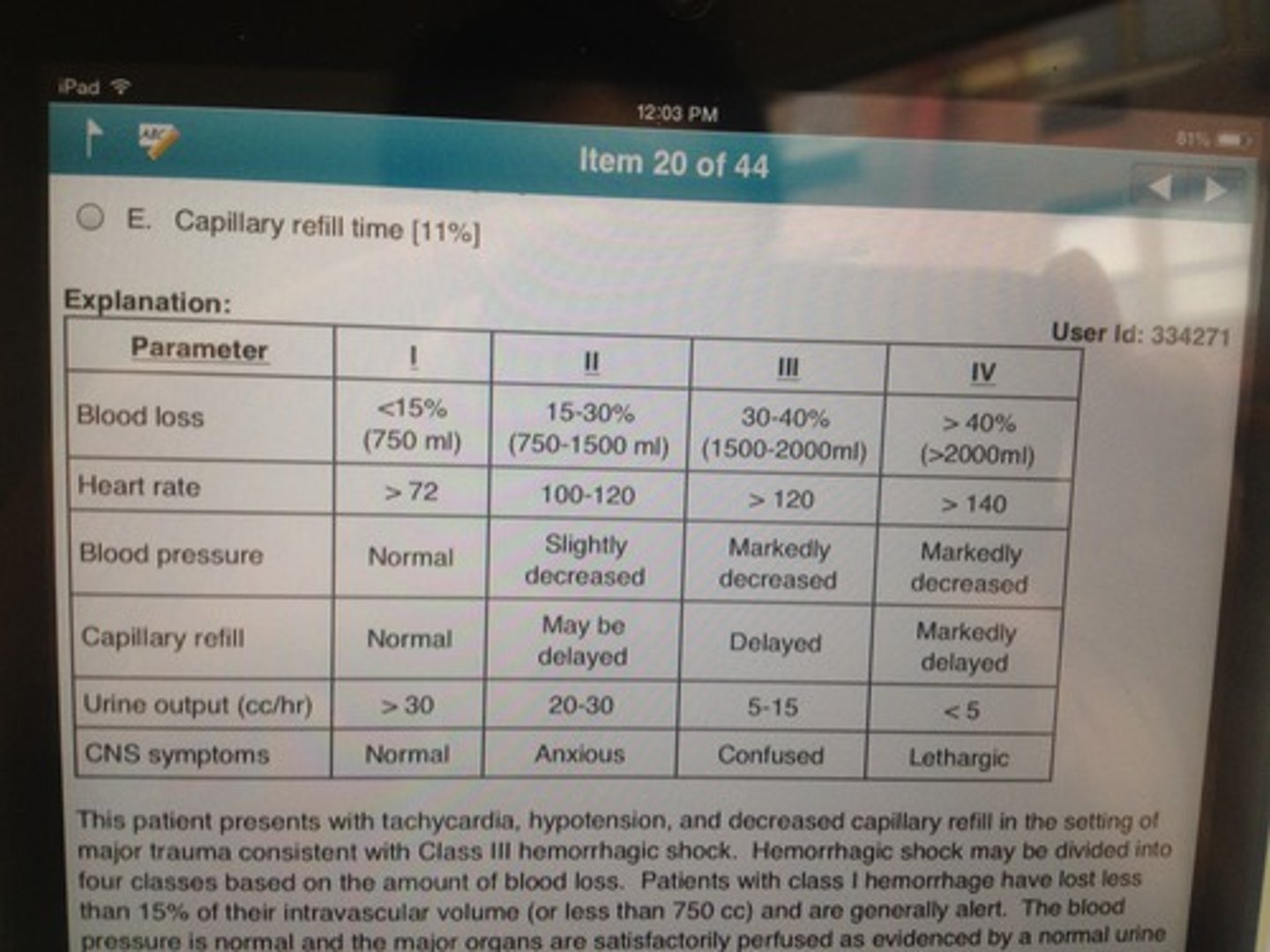
Clinical signs of maternal blood loss such as tachycardia and hypotension may not appear until _____% of circulating blood volume is lost.
Tachycardia: 15-20%
(1000-1500cc)
Hypotension w/tachycardia: 25-40%
(>2000cc)
What is the rate of uterine blood flow at term?
up to 750cc/min
(10-15% of maternal cardiac output)
3 mechanisms that control uterine bleeding at delivery:
-Contractions compress blood vessels
- Tissue factor is released from the decidua (combines with FVIIa to initiate the extrinsic clotting cascade)
- Circulating clotting factors including platelets, fibrinogen form clots at the uterine blood supply
What factors increase clotting?
What factors decrease clotting?
Increase: 5,7,8,9 and thrombin
Decrease: C, S, plasmin, antifactor Xa, antithrombin 3
What makes pregnancy a hypercoagulable state?
Increased clotting factors
Decreased anti-clotting factors
What is the shock index and its relevant cutoff?
Shock index = HR/SBP
Sensitive indicator of blood loss
>=1.4 requires urgent intervention
What is the lethal triad of excessive hemorrhage?
Hypothermia (halts coagulation)
Coagulopathy (increases lactic acidosis)
Acidosis (decreases myocardial performance)
Calcium, lactate, base deficit, temperature goals?
Ca >2
Lactate <2
Base Deficit <3
T 96.8-99.5
1 cc blood weighs ___.
1 cc blood = 1 gm
Types of peripartum hematoma?
Risk factors for developing?
Vulvar, vulvovaginal, paravaginal, retroperitoneal
Risks: nulliparity, episiotomy, forceps delivery
What are the processes in DIC?
Consumptive coagulopathy:
- Triggering event releases TF (thromboplastin), activating clotting cascade
- Platelets and clotting factors are used up > Bleeding
- Intravascular clots cause end-organ damage
Amniotic fluid embolism is also called ______.
What is the cause?
What is the maternal triad?
What are the two phases?
AFE = ASP (Anaphylactoid syndrome of pregnancy)
- maternal immunologic reaction to fetal antigens entering maternal circulation during labor/delivery, causing release of excessive catecholamines
Triad: hypovolemia, hypotension, coagulopathy
Phase 1 - cardiopulmonary phase
Phase 2 - late hemorrhagic phase (DIC)
How should oxytocin be used for active management of the third stage?
Give 10 units within 30 min (can be diluted in IVF or given IM)
Continue at 10 units per hour for 4 hours
Can give 10 - 40 units in 1000 mL saline
Up to 80 units in 1000mL can be given, but no extra benefit is shown
What is the mechanism of methergine?
Dosing?
Contraindications?
Alpha-adrenergic agonist that causes vasoconstriction
IM - 0.2mg, 2-5 min effect
PO - 0.2mg, 5-10 min effect
Intrauterine (can be transabominal) - 0.2mg, 2-5 min
AVOID IF: preeclampsia/HTN, Raynauds, scleroderma, CAD, or on protease inhibitors
What is the mechanism of prostaglandin F2-alpha?
Dosing?
AKA Hemabate / carboprost
IM or Intrauterine - 0.25mg
Given every 15 - 90 min to a max of 2 mg (up to 8 doses)
Must be refrigerated
AVOID if active asthma requiring treatments
What is the mechanism of prostaglandin E1?
Dosing?
AKA Cytotec / misoprostol
SL, PO, Rectal - 400-800mcg
How does TXA work? Dosing?
inhibits fibrinolysis by competitively blocking plasminogen activation on the surface of fibrin (clots can't break down)
Opposite of tPA, which activates plasmin from plasminogen
1g in 100mL over 10 min, can give another 1g after 30 min
What is a uterine tourniquet?
A method to reduce blood loss at the time of laparotomy
A foley catheter is tied tightly around the lower uterine segment for vascular occlusion
What is a good indicator that uterine compression sutures will be effective?
If manual compression of the uterus slows bleeding
What is an O'Leary stitch?
Compresses the uterine artery to the uterine wall just above the level of the cervix
What is a pelvic pressure pack?
A sterile tamponade device used after hysterectomy in the setting of coagulopathy, placed into the general pelvis through the open vaginal cuff
What vital signs criteria are used to transfuse prior to return of labs?
QBL 1000cc or more
HR 110 or more
BP < 85/45
Ongoing bleeding with a negative clot tube
Unstable vitals
What is the transfusion Hb level for a patient who has STOPPED bleeding?
8 mg/dL
What does the INR tell you about clotting factors?
INR 1.6 suggests that clotting factors are at 30% of their normal level, and FFP may be needed
3-6 units of FFP required to increase clotting factors by 20%
1 unit FFP raises fibrinogen 10mg/dL
What is the usual dosing of cryoprecipitate?
1 unit per 10kg body weight
Criteria for activating MTP?
Stage 3 cumulative blood loss >1500cc
2u PRBC given with persistent hemodynamic instability
Coagulopathy
Anticipated EBL 50% or more of total blood volume in 2h
Persistent bleeding after 4u PRBC
Uncontrolled bleeding with maternal hypovolemia
What is ANH?
Acute normovolemic hemodilution
1L blood drawn immediately before surgery and replaced with 1L crystalloid
Person's own blood transfused back after surgery
Point is to reduce loss of RBCs by diluting