11/4/25 Psychosis and schizophrenia spectrum disorders pt 1
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
Psychosis definition
trouble distinguishing what is real vs not real
most often, people either develop beliefs that are not real or perceive things that are not real
In what types of conditions can psychotic symptoms occur?
psychotic symptoms can occur in a variety of different disorders and medical conditions (e.g. MDD, bipolar disorder, dementia, infections, vitamin deficiencies)
what’s another name for psychotic disorders, and how are they diagnosed?
psychotic disorders (sometimes also called schizophrenia spectrum disorders) are diagnosed by examining symptoms across 5 domains
psychotic disorder indicators- 5 domains
delusions
hallucinations
disorganized speech and thought
grossly disorganized or abnormal motor behavior
negative symptoms
psychotic disorder domain 1: delusions
intense, intractable beliefs that do not waver even with evidence that conflicts or disconfirms them; tends to follow patterns but content can vary; there are 5 common types of delusions…
persecutory: being harassed or harmed by an individual, group, or organization
referential: gestures, comments, environmental cues are directed towards oneself
grandiose: belief in having exceptional abilities, fame, or wealth
erotomanic: false belief that another person is in love with you
somatic: related to health or organ function (e.g. bones have been replaced by jelly)
delusional content can be bizarre or nonbizarre
bizarre delusions are clearly implausible, do not derive from ordinary life circumstances, and are not easily understood by same culture peers
often centers on a loss of control of body or mind (e.g. an outside force has removed your organs and replaced them with the organs of another person, without leaving marks or scars)
nonbizarre delusions are plausible
e.g. text messages are being monitored by the government
psychotic disorder domain 2: hallucinations
vivid, clear, perceptual-like experiences that occur without an external stimulus
not under voluntary control
auditory are most common form (usually voices), but can also be visual, tactile, olfactory
people think of hallucinations as something very rare, but…
between 10-25% of the general population reports hearing a voice at some point, and a much smaller percent (around 1%) report more frequent recurrent voice hearing
some other stats about hallucinations
66% of people who hear voices recurrently hear more than one voice
71% of voice have a different accent than the voice hearer’s accent
57% of voices are “crowds” of talking, 34% middle aged man, 10% young woman
68% hear the same voice recurrently
68% hear abusive voices
25% hear approving or gentle voices
around 70% of people begin hearing voices after a significant emotional event
where do auditory hallucinations occur?
perception is that the voice is inside the head, not transmitted through the ears
fMRI studies confirm that different neural regions are activated during auditory hallucinations than during hearing normal auditory stimuli
psychotic disorder domain 3: disorganized speech and thought
loose associations: frequently switching from topic to topic
tangentiality: providing unrelated responses to conversational prompts
incoherence: sometimes referred to as “word salad”, words in a string are disconnected from each other (e.g. “purple sky drink balloons elephant crackers”)
mildly disorganized speech is common, in psychosis this disorganization must be severe enough to impair effective communication
psychotic disorder domain 4: grossly disorganized or abnormal motor behavior
silliness, agitation, mutism or lack or verbal response, staring, echoing, grimacing
can also include catatonia, or decrease in reactivity to environment, sometimes to the point of stupor or lack of motion
psychotic domain 5: negative symptoms
similar to operant conditioning definitions of positive vs negative
hallucinations and delusions are referred to as positive symptoms because their presence occurs in addition to more typical, expected perceptions and experiences
negative symptoms are symptoms that are marked by the absence or diminishing of what we would expect to see in someone
flat affect (diminished emotional expression)
avolition (decrease in self-motivated activities)
anhedonia (decrease in interest or pleasure)
asociality (social withdrawal or disinterest in social activities)
What does the term disorganized symptoms refer to in psychopathology?
Illogical speech, erratic behavior, and affect that does not match the situation.
Schizophrenia Spectrum and Other Psychotic Disorders
Brief Psychotic Disorder
Schizophreniform Disorder
Schizophrenia
how are schizophrenia spectrum and other psychotic disorders similar and different?
they all share these core features of psychosis, but are primarily differentiated by number and duration of symptoms
Brief Psychotic Disorder criteria
presence of one or more of the following symptoms, and at least one of these must be (1), (2), or (3):
delusions
hallucinations
disorganized speech (e.g. frequent derailment or incoherence)
grossly disorganized or catatonic behavior
duration of an episode of the disturbance is at least 1 day but less than 1 month, with eventual full return to premorbid level of functioning (not a super long term condition)
disturbance is not better explained by MDD or bipolar disorder with psychotic features or another psychotic disorder (schizophrenia or catatonia) and is not attributable to the physiological effects of a substance or another medical condition
Brief Psychotic Disorder specifiers
with peripartum onset (period immediately surrounding childbirth)
with marked stressor
Schizophreniform Disorder criteria (a step up in intensity from
Two or more of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated), where at least one of them must be (1), (2), or (3):
delusions
hallucinations
disorganized speech (e.g. frequent derailment or incoherence)
grossly disorganized or catatonic behavior
negative symptoms (e.g. diminished emotional expression or avolition)
an episode of the disorder lasts at least 1mo but less than 6mo; when the diagnosis must be made without waiting for recovery, it should be qualified as “provisional”
schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out because either
1) no MDD or manic episodes have occurred concurrently with active-phase symptoms, or
2) if mood episodes have occurred during active-phase symptoms, they have been present for a minority of the total duration of the active and residual periods of the illness
disturbance is not attributable to the physiological effects of a substance or another medical condition
Schizophrenia criteria
Two or more of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated), where at least one of them must be (1), (2), or (3):
delusions
hallucinations
disorganized speech (e.g. frequent derailment or incoherence)
grossly disorganized or catatonic behavior
negative symptoms (e.g. diminished emotional expression or avolition)
for a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas (e.g. work, interpersonal relations, self-care) is markedly below the level achieved prior to the onset (or when childhood/adolescent onset, there is failure to achieve expected level of interpersonal, academic, or occupational functioning)
continuous signs of the disturbance persist for at least 6mo
this 6mo period must include at least 1mo of symptoms (or less if successfully treated) that meet Criterion A (i.e. active-phase symptoms) and may include periods of prodromal or residual symptoms.
during these prodromal or residual periods, the signs of disturbance may be manifested by only only negative symptoms or by 2 or more of the symptoms listed in Criterion A present in an attenuated form (e.g. odd beliefs, unusual perceptual experiences)
Schizophrenia rule-outs
schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out because either
1) no MDD or manic episodes have occurred concurrently with the active-phase symptoms, or
2) if mood episodes have occurred during the active-phase symptoms, they have been present for a minority of the total duration of the active and residual periods of the illness
the disturbance is not attributable to the physiological effects of a substance or another medical condition
if there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations (in addition to the other required symptoms of schizophrenia) are also present for at least 1mo (or less if successfully treated)
Schizophrenia vs Schizophreniform Disorder are very similar (they have the exact same Criterion A), but can be differentiated by…
duration and the impairment of the symptoms
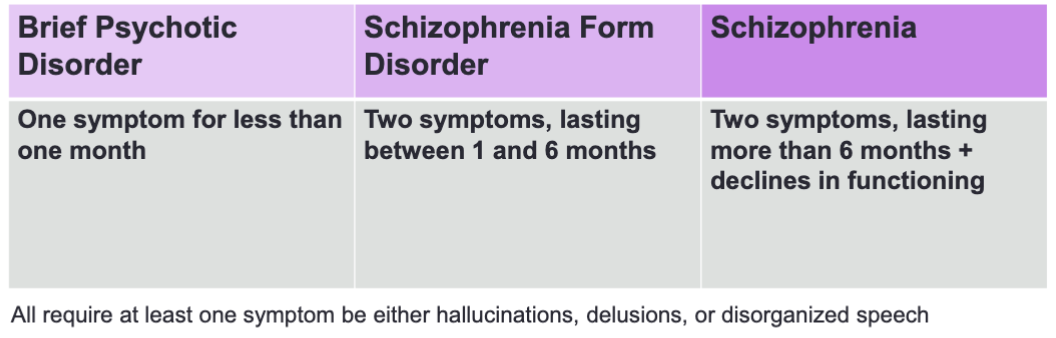
how to differentiate between the 3 psychotic disorders
recap: they are primarily differentiated by number and duration of symptoms
Brief Psychotic Disorder: one symptom for less than 1mo
Schizophrenia Form Disorder: two symptoms, lasting between 1-6mo
Schizophrenia: two symptoms, lasting more than 6mo, and declines in functioning
all require at least one symptom be either hallucinations, delusions, or disorganized speech
two more disorders related to schizophrenia and psychosis in the DSM
delusional disorder
schizoaffective disorder
Delusional Disorder criteria
defined by the presence of one or more delusions with a duration of more than one month, but no disorganized speech. Hallucinations may be present but are not severe and are related to the theme of the delusion
functioning is not impaired and behavior is not unusual/not seen as unusual to other people
some studies show that about ½ of ppl with delusional disorder marry and work
onset tends to be later than with schizophrenia
not due to substance use, brain injury, or another medical condition
Schizoaffective Disorder criteria
a psychotic disorder with symptoms of both schizophrenia and a major mood disorder (e.g. bipolar disorder or MDD)
unlike psychotic symptoms that only occur during a mood disorder, ppl with schizoaffective disorder show delusions and hallucinations for at least 2wks not during mood disruptions
AND they show major mood disruptions for the majority of the time as they experience psychosis
some more facts about schizophrenia
it’s a chronic disorder, full recovery from schizophrenia is rare — once the disorder develops, ppl tend to have symptoms for the rest of their lives
remission is defined by symptoms no longer impairing daily life and functioning
about 50-80% of ppl who are hospitalized for severe symptoms of schizophrenia will be re-hospitalized at some point during their lives
equal prevalence across men and women, although men tend to develop the disorder at younger ages
1% global prevalence estimate
some indicators of schizophrenia are evident early on
ppl who go on to develop schizophrenia show mild motor problems, physical abnormalities or neurological “soft signs,” and mild social problems even in childhood
these are often non-specific and appear in many different types of neurological conditions
schizophrenia prodrome (even before the disorder is fully symptomatic, there’s a period that indicates something may be coming on)
about 1-2 yrs prior to the onset of schizophrenia
positive symptom early indicators: magical thinking (believing in having special abilities or telepathy) or feeling like someone else is present when they are not
negative symptom early indicators: social isolation, anhedonia
although there have been significant intervention efforts (meds, therapy, fish oil), with schizophrenia prodrome, none of them have been able to avert schizophrenia onset
research has shifted to investigating if these can either delay onset or lessen symptoms post-onset
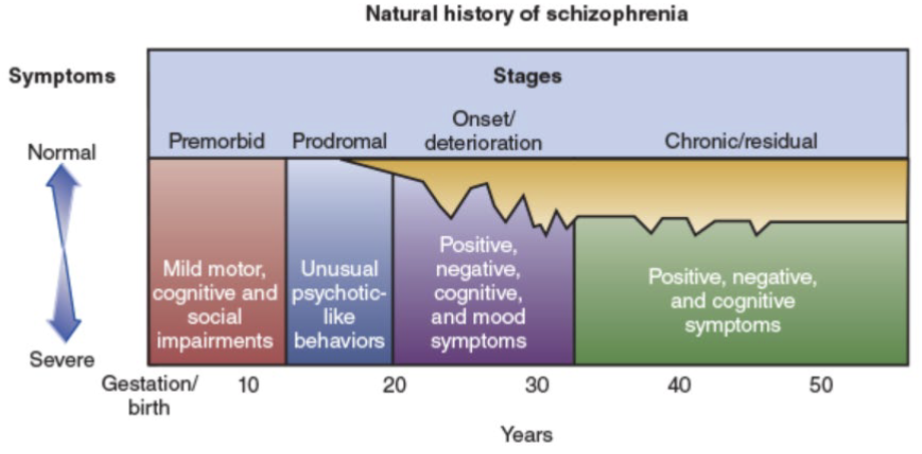
natural history of schizophrenia (table from textbook)
st stage (birth-10yo): premorbid (mild motor, cognitive, and social impairments)
nd stage (10-20yo): prodromal (unusual psychotic-like behaviors)
rd stage (20-30yo): onset/deterioration (positive, negative, cognitive, and mood symptoms)
th stage (30+yo): chronic/residual (positive, negative, and cognitive symptoms)
genetics and schizophrenia + family transmission (all forms of psychopathology are heritable, to a degree)
just like other disorders, schizophrenia is polygenic (there’s no “schizophrenia gene” but it’s related to many different gene variants)
schizophrenia was one of the first disorders clearly shown to be heritable via family transmission
likelihood of developing schizophrenia is higher among biologically related individuals, and higher likelihood is linked to greater/closer genetic relationship
adoption studies show that likelihood of schizophrenia is more strongly related to whether a biological parent has schizophrenia than an adoptive parent
psychosocial antecedents of schizophrenia
prenatal exposure to viruses, infections birth complications (especially those involving loss of oxygen at birth)
chronic stress early in life: childhood stress, “ adversity, “ poverty, “ homelessness, “ immigration
environmental antecedent of schizophrenia- cannabis and the adolescent brain
cannabis can temporarily induce hallucinations, ppl with cannabis-induced psychosis showed elevated rates of later diagnoses of schizophrenia
regular cannabis use during adolescence is associated with a four-fold increase in likelihood of a diagnosis of schizophrenia
this does not seem to be purely a question of selection
cannabis use during adolescence is associated with thinning of cerebral cortex that does not rebound or recover
for ppl with high genetic risk for schizophrenia, avoiding cannabis is often recommended
dopamine hypothesis of schizophrenia
4 main pathways in brain that transmit dopamine (mesolimbic, mesocortical, nigrostriatal, and tuberoinfundibular)
in general, hallucinations and delusions are correlated with excessive dopamine activity in the mesolimbic pathway
negative symptoms seem to result from less dopamine in the mesocortical pathway
antipsychotic medications (two generations)
first line treatment for psychosis
older/typical antipsychotics block dopamine receptors in order to reduce positive symptoms
lessening of dopamine can result in harsh side effects as dopamine is depleted in other pathways
dopamine reduction in nigrostriatal pathway often led to Parkinson’s-like symptoms of tremors, rigidity, slow movement, etc.
tardive dyskinesia (possible side effect): involuntary lip smacking, grimacing, tongue thrusting
dopamine reduction in tuberinfundibular pathways can involve weight gain, lactation, sexual dysfunction
2nd gen/atypical antipsychotics block both dopamine and serotonin receptors
does not have Parkinson’s-like side effects and greatly reduce probability of tardive dyskinesia, but it’s still possible
other serious side effects: primarily cardiometabolic issues (obesity, HBP, diabetes), increased stroke and heart disease risk
ppl on antipsychotics report greatly reduced quality of life
how well do antipsychotic medications work?
about 45% of ppl experience remission of symptoms in 18mo after starting treatment (of these, 12% maintain remission for 6mo)
tends to be much better at reducing positive symptoms than improving negative ones